Abstract
Dermoid cysts are malformations that are rarely seen in the oral cavity. An intraoral dermoid cyst grows slowly, but may enlarge and interfere with deglutition and speech, or can pose a critical risk to the airway and therefore require immediate surgical intervention. Dermoid cysts may develop above or below the mylohyoid muscle, causing a submental or submandibular swelling. Surgical excision is the treatment of choice and recurrence is rare. An intraoral approach for the treatment of large lesions presenting above the mylohyoid muscle provides good cosmetic and functional results. We report a case of a 26-year-old female who developed an epidermoid cyst presenting as a large sublingual swelling causing speech and swallowing difficulties. The lesion was surgically excised using an intraoral approach. Microscopic examination revealed a dermoid cyst of the epidermoid type. This case shows that dermoid cysts may be successfully diagnosed and managed using a series of simple yet effective clinical procedure.
Keywords: Dermoid cyst, epidermoid cyst, floor of mouth
INTRODUCTION
Dermoid cysts are development lesions found inside normal organs or tissues as a result of the inclusion of tissue from diverse sources (ectoblastic, mesoblastic, or endoblastic) caused by a defect in the fusion of the embryonic lateral mesenchymatic mass (mainly the first and second arcs) during the fifth week of embryological development.[1] Depending on their location, dermoid cysts are divided into medial and lateral cysts. Dermoid cysts on the floor of the mouth are often relatively soft unfluctuating masses, frequently adhered to the child's hyoid bone. In adults, the cyst on the floor of the mouth is located between the geniohyoid and mylohyoid muscles. It brings about an upward displacement of the tongue, slurred speech, and difficulty in swallowing. When the cyst locates itself between the mylohyoid muscle and the neck's cutaneous muscle, it is referred to as a geniohyoid cyst with displacement outward and resembling a double chin.[2]
In 1955, Meyer[3] updated the concept of dermoid cyst to describe three histological variants: The true dermoid cyst, the epidermoid cyst, and the teratoid variant. True dermoid cysts are cavities lined with epithelium showing keratinization and with identifiable skin on the cyst wall. Epidermic cysts are lined with simple squamous epithelium with a fibrous wall and no attached structures. The lining of teratoid cysts varies from simple squamous to a ciliate respiratory epithelium containing derivatives of ectoderm, mesoderm, and/or endoderm. All three histological types contain a thick, greasy-looking material.
CASE REPORT
We present here the case of a 26-year-old female who attended the outpatient department seeking consultation for a growth in the floor of the mouth that had existed for about 3 years, although she had not noted any significant increase in size over the last few years. She had been having altered speech and functional difficulty since last two years and she believes that the tumoration on the floor of his mouth was the cause of it all. On extraoral inspection, her neck appeared short and thick, giving a double chin appearance [Figure 1]. There was no cervical lymphadenopathy. Intraoral examination showed a large swelling involving the submental, submandibular, and sublingual areas measuring 3 × 3 cm2 in diameter, adhered to the deep planes, painless, and displacing her tongue upward. The tongue was elevated to the extent that the soft palate could not be visualized. The swelling was found to be smooth, nontender, and the mucosa on the floor of the mouth was normal [Figure 2]. On application of pressure in the submental region, the growth was getting displaced upward. The size and appearance of the orifices of Wharton's ducts were normal.
Figure 1.

Extraoral appearance of double chin in the patient
Figure 2.
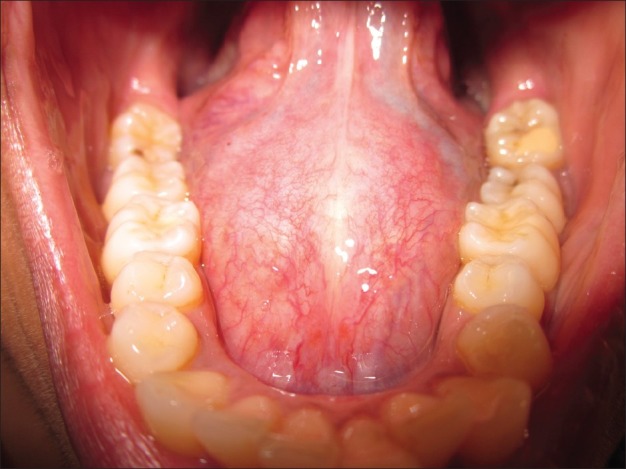
Intraoral appearance of dermoid cyst
An ultrasonography was performed, which revealed cystic area with echogenic material and internal echoes within it. There was no evidence of flow within the cystic area on the color doppler [Figure 3]. MRI showed an encapsulated cystic mass without any calcification [Figure 4].
Figure 3.
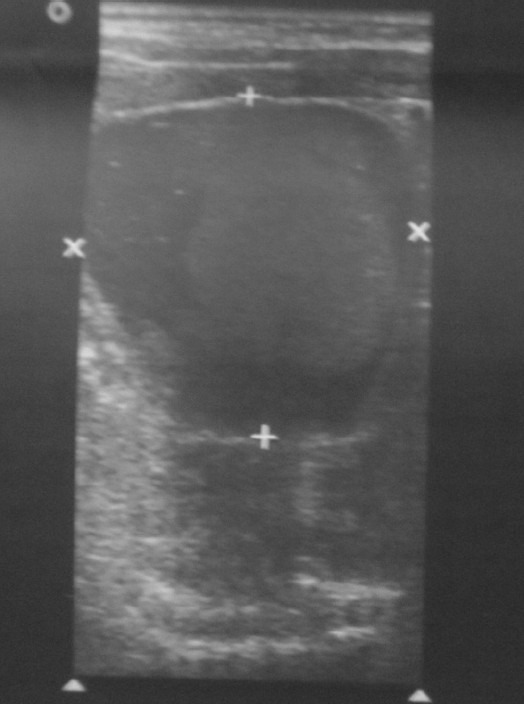
Ultrasonographic appearance of dermoid cyst
Figure 4.
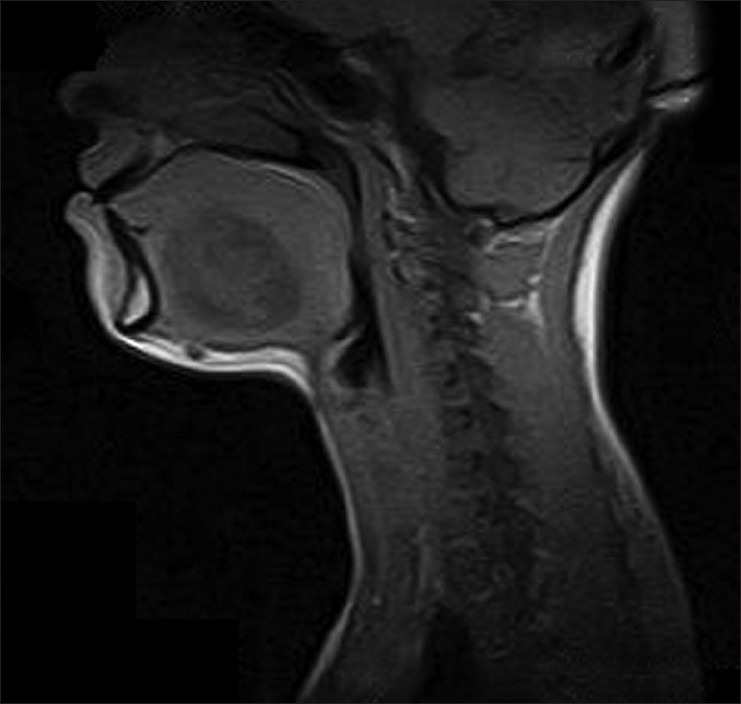
MRI image of dermoid cyst
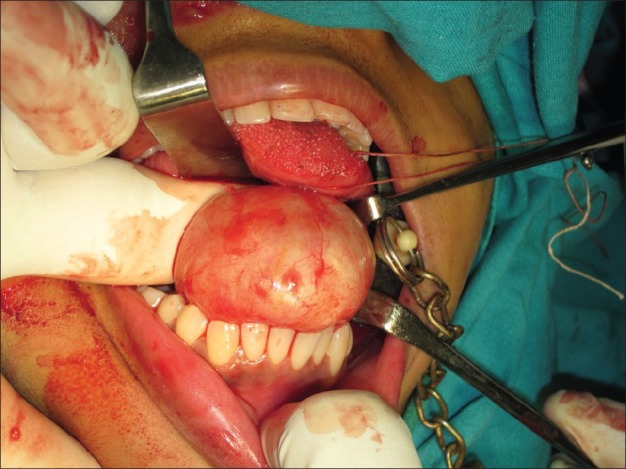
The differential diagnosis included lipoma, ranula, thyroglossal duct cyst, cystic hygroma, branchial cleft cysts, and benign and malignant tumors of the floor of the mouth and adjacent salivary glands. Surgical excision of the lesion was performed through an intraoral midline incision under general anesthesia [Figure 5]. Blunt dissection was utilized to free and remove the mass, and then the wound was sutured in layers with a corrugated rubber drain placed in position. Macroscopically, the lesion appeared encapsulated and contained a keratin-like yellow material [Figure 6]. The anatomical pathology diagnosis was a dermoid cyst. Histopathology revealed that it is an epidermal cyst lined by stratified squamous epithelium with the lumen containing kerati [Figure 7] histopathology course was uneventful, and there was no evidence of recurrence at a period of 4 months after surgery].
Figure 5.
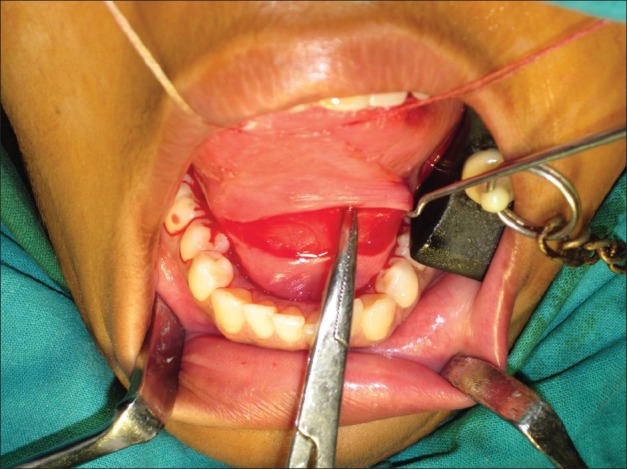
Intraoral surgical approach for the excision of dermoid cyst
Figure 6.
Macroscopic appearance of dermoid cyst
Figure 7.
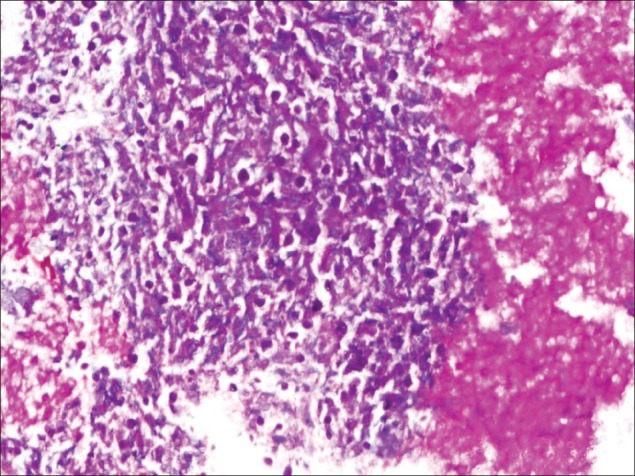
Histopathological appearance of dermoid cyst
DISCUSSION
The floor of the mouth and submandibular area may be affected by numerous pathologic conditions, which can be broadly classified as developmental, inflammatory, obstructive, or neoplastic in origin. Lesions in this area may be present for a prolonged period of time before the patient seeks medical advice, usually as a result of interference with swallowing or speech. The floor of the mouth is the most common intraoral location for developmental lesions of the oral soft tissues, particularly dermoid cysts, lipoma, branchial cleft cysts, and thyroglossal duct cysts.[4]
Dermoid cysts are considered to be a variation of teratomas and are thought to arise from entrapment of epithelial remnants during closure of the branchial arches or as a result of trauma.[5,6] Almost one-fifth of the dermoid cysts that occur in the head and neck area are located on the floor of the mouth where they may cause tongue elevation, submental protrusion, or both. They are predominantly seen in young persons, presenting as soft to rubbery swellings in the midline or laterally.
Lipoma[7] is a slow growing benign tumor with intraoral incidence as low as 1%. Lipids unavailability for metabolism, coupled with autonomous growth of a lipoma, have rendered it to be a true neoplasm. Cheek is the most common intraoral site followed by floor of the mouth. Branchial cleft cysts[8] are developmental anomalies which arise from incomplete closure of branchial arches. They usually appear in relatively young patients as fluctuant swellings located anteriorly to the sternocleidomastoid muscle.
Heterotopic gastrointestinal cysts are choristomas of head and neck and mostly affect the sublingual area or the floor of the mouth. They appear to have a male preponderance and are usually lined with gastric mucosa.[9]
Thyroglossal duct cysts[10] arise from remnants of the embryonic thyroid. They typically present in the midline in close contact to the hyoid bone, often producing a characteristic movement during swallowing. Developmental lesions present a relatively silent course before causing any symptoms, as with the present patient. However, this patient's age made the probability of such an entity less likely.
Congenital lesions, such as vascular malformation or lymphangioma (cystic hygroma), are generally included in the differential diagnosis of neck masses extending to the floor of the mouth. Both lesions are most commonly seen in childhood, with 90% of lymphangiomas of the head and neck diagnosed by the age of 2 years.[11]
Infections and inflammatory lesions of perioral tissues may also present as a swelling of the submandibular area extending to the floor of the mouth.[12] Acute infections may derive from an odontogenic focus of infection but were not considered in the differential diagnosis, because of the chronic nature of the condition. In addition, fever, malaise, and pain would normally accompany the clinical presentation of an acute infection, and tenderness to palpation and fixed or fluctuant overlying skin would be apparent in the clinical examination.
Another entity which should be considered is lymphadenitis of different causes. Submandibular lymph nodes may commonly be affected by cat-scratch disease, tuberculosis (scrofula), or actinomycosis.[13] The present patient's noncontributory medical history ruled out this possibility. Additionally, lymphadenitis typically does not produce this degree of intraoral swelling.
Salivary gland lesions are commonly seen intraorally and in the submandibular triangle. The ranula is located exclusively on the floor of the mouth. It appears as an enlargement of normal to bluish color, varying from a fluctuant process to a lesion of soft consistency, depending on the thickness of the overlying tissues. Children and young adults are more frequently affected, and a history of repetitive rupture and recurrence is a common finding. Plunging ranula is a variation of the ranula, produced by dissection of extravasated mucin through the mylohyoid muscle. It appears as a lump in the submandibular neck area, with or without intraoral signs.[14]
Inflammatory disorders of the salivary glands merited consideration in the differential diagnosis of the present lesion. Acute sialadenitis of the submandibular gland usually presents with swelling associated with meals and pain and purulent discharge from the Wharton duct,[15] and chronic sialadenitis runs a prolonged course of remissions and exacerbations. Both conditions are more frequent in the sixth decade of life and present no gender predilection. Moreover, both conditions usually involve a number of predisposing factors.
Acute sialadenitis of the submandibular gland usually presents with swelling associated with meals and pain and purulent discharge from the Wharton duct which was not seen in the present case and hence was ruled out. Chronic sialadenitis runs a prolonged course of remissions and exacerbations. Both conditions are more frequent in the sixth decade and usually involve a number of predisposing factors, such as sialolithiasis, chronic illness, hospitalization, or medications, all of which may be associated with xerostomia.
Pleomorphic adenoma and monomorphic adenoma are usually included in the differential diagnosis of painless and slowly growing intraoral masses.[16] However, salivary gland neoplasms of the floor of the mouth are more often malignant than benign. The present patient's age does not conform the incidence of salivary gland neoplasms.
Malignant soft tissue tumors were considered to be a remote possibility. Rapid growth, lack of circumscription, fixation to adjacent structures, and ulceration of the overlying mucosa are common features of malignancy that were not noted in the present patient.
CONCLUSION
Floor of the mouth has always remained a challenging site for diagnosis and management of lesions pertaining to that site. Range of lesions that are seen in this region extends from mucocele to malignancy and hence it is prudent to investigate with recent modalities before final diagnosis and surgical exploration. Tightly netted vital structures can route infections till the mediastinum and can contribute to morbidity and mortality in these cases.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Containment P. Medical-Encyclopedie chirurgicale-E-20-860-A-10. Paris: Elsevier; 2000. Congenital fistulas and cysts of the neck. [Google Scholar]
- 2.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2nd ed. Philadelphia: Saunders; 2002. [Google Scholar]
- 3.Meyer I. Dermoid cysts (dermoids) of the floor of the mouth. Oral Surg Oral Med Oral Pathol. 1955;27:1149–64. doi: 10.1016/0030-4220(55)90380-7. [DOI] [PubMed] [Google Scholar]
- 4.Longo F, Maremonti P, Mangone GM, De Maria G, Califano L. Midline (dermoid) cysts of the floor of the mouth: Report of 16 cases and review of surgical techniques. Plast Reconstr Surg. 2003;112:1560–5. doi: 10.1097/01.PRS.0000086735.56187.22. [DOI] [PubMed] [Google Scholar]
- 5.Pryor SG, Lewis JE, Weaver A, Orvidas LJ. Pediatric dermoid cysts of the head and neck. Otolaryngol Head Neck Surg. 2005;132:938–42. doi: 10.1016/j.otohns.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Lian TS. Benign tumors and tumor-like lesions of the oral cavity. In: Flint P, Haughey B, Robbins KT, Thomas JR, editors. Cummings’ otolaryngology: Head and neck surgery. 4th ed. Philadelphia: Mosby; 2005. pp. 1574–7. [Google Scholar]
- 7.El-Momen MH, Gaafar AH, Magdy EA. Lipomas of the head and neck: Presentation variability and diagnostic work-up. J Laryngol Otol. 2006;120:47–55. doi: 10.1017/S0022215105004597. [DOI] [PubMed] [Google Scholar]
- 8.Glosser JW, Pires CA, Feinberg SE. Branchial cleft or cervical lymphoepithelial cysts: Etiology and management. J Am Dent Assoc. 2003;134:81–6. doi: 10.14219/jada.archive.2003.0020. [DOI] [PubMed] [Google Scholar]
- 9.Coriæ M, Seiwerth S, Bumber Z. Congenitaloral gastrointestinal cyst: An immunohistochemical analysis. Eur Arch Otorhinolaryngol. 2000;257:459–61. doi: 10.1007/s004050000255. [DOI] [PubMed] [Google Scholar]
- 10.Ellis PD, van Nostrand AW. The applied anatomy of thyroglossal tract remnants. Laryngoscope. 1977;87:765–70. doi: 10.1002/lary.5540870512. [DOI] [PubMed] [Google Scholar]
- 11.Gharaibeh TM, Safadi RA, Rawashdeh MA, Hammad HM. Plunging arteriovenousmal formation in the floor of the mouth: A case report. Br J Oral Maxillofac Surg. 2010;48:e35–7. doi: 10.1016/j.bjoms.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 12.Tosios K, Rallis G, Vallianatou D, Vlachodimitropoulos D. Yellow-white tumor on the floor of the mouth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:701–4. doi: 10.1016/j.tripleo.2005.10.066. [DOI] [PubMed] [Google Scholar]
- 13.King RC, Smith BR, Burk JL. Dermoid cyst in the floor of the mouth. Review of the literature and case reports. Oral Surg Oral Med Oral Pathol. 1994;78:567–76. doi: 10.1016/0030-4220(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 14.Mosier KM. Nononcologic imaging of the oral cavity and jaws. Otolaryngol Clin North Am. 2008;41:103–37. doi: 10.1016/j.otc.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 15.Huang C, Damrose E, Bhuta S, Abemayor E. Kuttner tumor (chronic sclerosingsialadenitis) Am J Otolaryngol. 2002;23:394–7. doi: 10.1053/ajot.2002.126855. [DOI] [PubMed] [Google Scholar]
- 16.Munir N, Bradley PJ. Diagnosis and management of neoplastic lesions of the submandibular triangle. Oral Oncol. 2008;44:251–60. doi: 10.1016/j.oraloncology.2007.02.004. [DOI] [PubMed] [Google Scholar]


