Abstract
Background
Few studies have compared change in the health-related quality of life (HRQL) following treatment of non-ST-elevation acute coronary syndrome (NSTE-ACS) with either percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). This study is to compare changes in HRQL six months after hospital discharge between NSTE-ACS patients who underwent either PCI or CABG.
Methods
HRQL was assessed using the Seattle angina questionnaire at admission and six months after discharge in 1012 consecutive patients with NSTE-ACS. To assess associations of PCI and CABG with HRQL changes, logistic regression models were constructed treating changes in the score of each dimension of the Seattle angina questionnaire as dependent variables.
Results
Although both the PCI and CABG groups experienced angina relief and other improvements at 6-month follow-up (P < 0.001), the CABG relative to PCI group showed more significant improvements in angina frequency (P = 0.044) and quality of life (P = 0.028). In multivariable logistic analysis, CABG also was an independent predictor for both improvement of angina frequency (OR: 1.62, 95%CI: 1.09−4.63, P = 0.042) and quality of life (OR: 2.04, 95%CI: 1.26−6.92, P = 0.038) relative to PCI.
Conclusions
In patients with NSTE-ACS, both PCI and CABG provide great improvement in disease-specific health status at six months, with that of CABG being more prominent in terms of angina frequency and quality of life.
Keywords: Non-ST elevation acute coronary syndrome, Quality of life, Therapeutic strategy
1. Introduction
Non-ST-elevation acute coronary syndrome (NSTE-ACS) is an acute severe cardiac disorder whose manifestations include unstable angina and non-ST-segment elevation myocardial infarction.[1] Registry data consistently show that NSTE-ACS is more common than ST-elevation acute coronary syndrome (STE-ACS) with an annual incidence of around 3 per 1000 inhabitants, which varies among countries.[2] Revascularization procedures, including percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), have proven effective in angina relief.[3]
Thanks to improved therapy, more patients are living with coronary heart disease (CHD). The goal of treating patients with ACS, therefore, is not only to prolong life but also to relieve symptoms and improve coronary function. Measures of mortality and morbidity, traditionally used as hard primary endpoints, have lost weight with the increased recognition that in the management and care of ACS patients merely focusing on assessment of physical outcomes is insufficient. Accordingly, assessment of well-being and health-related quality of life is also considered important.
Despite its significance as a public health problem, there are few reports examining and comparing revascularization strategies, namely PCI and CABG, in terms of improvement of quality of life for patients with NSTE-ACS in the Chinese population. Therefore, we used the Seattle angina questionnaire to evaluate the effect of therapy on health-related quality of life (HRQL) in a prospective observational study on a population of Chinese NSTE-ACS patients.
2. Methods
2.1. Study design
This follow-up study was carried out between July 2010 and December 2013 in the Cardiology Unit of Anzhen Hospital in Beijing, where consecutive patients admitted for NSTE-ACS diagnosis were identified on the basis of clinical, biochemical and electrocardiographic criteria. Patients with non-ischemic or non-cardiac precordial pain were excluded. All patients had an indication for revascularization and were suitable candidates for both PCI and CABG procedures. All procedures were performed using standard techniques. Following revascularization, optimal medical therapy was recommended for both groups. The patients' information (obtained three to seven days after admission, when the patient was clinically stable and six months after discharge) was obtained by a single previously-trained interviewer; clinical evaluation was made concurrently. All demographic, clinical, and health status data were collected. Specific variables included demographic characteristics (age, gender, marital status, insurance, and education level), cardiac risk factors (diabetes, hypertension, hyperlipidemia and smoking history), and cardiovascular disease severity (congestive heart failure, previous coronary revascularization procedure, and previous myocardial infarction). Before inclusion, all patients were asked for their informed consent and all agreed to participate.
2.2. Measurement of disease-specific health status
Health status assessments were performed using standardized, written questionnaires administered to each patient at baseline and six months after therapy. The Seattle angina questionnaire (SAQ) was a 19-item self-administered, well-validated questionnaire that had well-established validity, reliability, sensitivity to clinical change and prognostic value.[3]–[9] The SAQ quantified five clinically relevant domains of cardiac-related health status: physical limitation, angina frequency, angina stability, treatment satisfaction, and quality of life. Scores range from 0 to 100 for each domain with higher scores indicating better function and fewer symptoms. Questionnaires were administered using linguistically and culturally validated translations in Chinese.
We defined clinically meaningful changes in each of the Seattle angina questionnaire scales according to criteria developed by Wyrwich, et al.,[10] i.e., a difference of 8 or more points on the physical-limitation scale, 20 or more on the angina-frequency scale and 16 or more on the quality of life scale.
2.3. Statistical analysis
Categorical data are reported as frequency and percentage and compared by chi-square test. Continuous variables are expressed as mean ± SD and compared by t-test. The chi-square test was used to compare the proportions of patients in each treatment group with significant improvement as defined by the angina frequency score on the SAQ. Mean observed data for each of the SAQ domains were analyzed with the use of unpaired t-tests comparing the scores of patients treated with PCI or CABG. Multivariable logistic regressions were used to evaluate the independent predictors of significant improvement of angina frequency (difference of 20 or more) and quality of life (difference of 16 or more), which were both significantly improved by CABG versus PCI in unadjusted analyses. Covariates used in each of the adjusted models included baseline SAQ scores, gender, age as a continuous variable, and coexisting medical conditions and risk factors including history of myocardial infarction, hypertension, diabetes, hyperlipidemia, current use of tobacco, and history of cardiovascular disease. All statistical analyses were two-tailed, and P < 0.05 was considered statistically significant. Analyses were performed with SPSS software, version 17.0 for windows (SPSS, Inc., Chicago, IL, USA).
3. Results
3.1. Patient population
Of the 1050 patients who were initially included in this study, 1012 (96.3%) remained in the study after the six-month follow-up after undergoing either PCI (n = 510) or CABG (n = 502) procedures; and 38 withdrew from the trial or died before six months. Of the 1012 patients, the majority was male (706, 69.8%). Socio-demographic and clinical characteristics of the treatment groups are shown in Table 1. There were no significant differences in most of these baseline characteristics except health insurance rates and education level, which were lower in the CABG group.
Table 1. Baseline sociodemographic and clinical characteristics.
| PCI (n = 510) | CABG (n = 502) | P value | |
| Age | 67.63 ± 11.98 | 67.13 ± 8.94 | 0.07 |
| Gender (male) | 358 (70.2) | 348 (69.3) | 0.76 |
| Marital status (married) | 462 (90.6) | 449 (89.3) | 0.48 |
| Education (> 12 yrs) | 170 (33.3) | 156 (31.1) | 0.44 |
| Medical insurance | 407 (79.8) | 390 (77.87 | 0.41 |
| HBP | 377 (73.9) | 370 (73.8) | 0.94 |
| DM | 212 (41.6) | 205(40.8) | 0.81 |
| Lip | 266 (52.2) | 261 (52.0) | 0.96 |
| Smoker | 198 (38.8) | 219 (43.6) | 0.12 |
| UA-ACS | 388 (76.1) | 405 (80.7) | 00.076 |
| PMI | 94 (18.4%) | 106 (21.1) | 00.284 |
| LVEF < 40% | 72 (14.1%) | 064 (10.5) | 00.061 |
Data are presented as mean ± SE or n (%). ACS: acute coronary syndrome; CABG: coronary artery bypass grafting; DM: diabetes mellitus; HBP: high blood pressure; Lip: hyperlipidemia; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention; PMI: previous myocardial infarction; UA: unstable angina.
3.2. The use of antianginal medications
As summarized in Table 2, using of antianginal medications at baseline was similar between groups. Use of calcium channel blocker did not differ between the two groups. Use of nitrates and β-blockers was much less frequent, but was numerically higher after PCI than after CABG.
Table 2. Antianginal medications.
| PCI (n = 510) | CABG (n = 502) | P value | ||
| β-blockers | Baseline | 433 (84.9) | 441 (87.8) | 0.172 |
| 6 months | 398 (78.0) | 381 (75.9) | 0.418 | |
| Nitrates | Baseline | 434 (85.0) | 442 (88.0) | 0.169 |
| 6 months | 286 (56.1) | 256 (51.0) | 0.105 | |
| Calcium channel blockers | Baseline | 158 (30.9) | 140 (27.9) | 0.281 |
| 6 months | 112 (21.9) | 108 (21.5) | 0.863 |
Data are presented as mean ± SE or n (%). CABG: coronary artery bypass grafting; PCI: percutaneous coronary intervention.
3.3. Health status outcomes
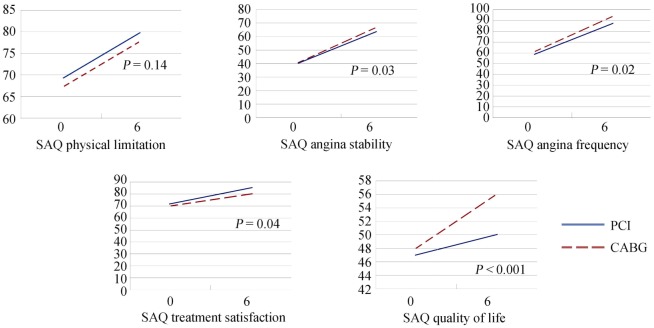
The rate of response in quality of life assessments among follow-up patients was 96.3%. Figure 1 summa rizes SAQ score results for the domains of physical limitation, angina frequency, angina stability, treatment satisfaction and quality of life. Baseline health status scores were similar between the two treatment groups. At the sixth months, we examined five domains for differences between treatment groups. Patients having either PCI or CABG procedures experienced significant improvements after treatment in the five SAQ domains (P < 0.001). There were no differences in improvement between the PCI and CABG groups (P = 0.359) in physical limitation (P = 0.14) and angina stability (P = 0.12); however, the CABG group had more pronounced improvements than the PCI group in angina frequency (P = 0.02), treatment satisfaction (P = 0.04), and quality of life (P < 0.001). In the PCI group, angina frequency scores improved from 58 ± 18 to 79 ± 14, treatment satisfaction scores from 72 ± 17 to 76 ± 13, and quality of life scores improved from 40 ± 23 to 43 ± 17. In the CABG group, angina frequency scores improved from 61 ± 17 to 93 ± 9, treatment satisfaction scores from 70 ± 12 to 80 ± 9, and quality of life scores improved from 48 ± 14 to 56 ± 11. The improvement in angina frequency scores in the CABG group was markedly different to that of the PCI group, demonstrating that angina was relieved more significantly in the CABG group. The difference between the groups was much more obvious in quality of life scores, the CABG group improved significantly more than the PCI group (P < 0.001). Table 3 shows the proportion of patients with a clinically significant improvement (as defined in the Methods section) within each domain. Both PCI and CABG groups had clinically significant improvements in the scores for all five domains to a certain extent.
Figure 1. Scores on the Seattle angina questionnaire from baseline to six months.
CABG: coronary artery bypass grafting; PCI: percutaneous coronary intervention; SAQ: Seattle angina questionnaire.
Table 3. Patients with clinically significant improvement from baseline in scores on the Seattle angina questionnaire.
| Domain | PCI | CABG | P value |
| PL | 68% | 71% | 0.708 |
| AS | 66% | 69% | 0.707 |
| AF | 59% | 80% | 0.044 |
| TS | 40% | 41% | 0.849 |
| QL | 22% | 38% | 0.028 |
AF: angina frequency; AS: angina stability; CABG: coronary artery bypass grafting; PCI: percutaneous coronary intervention; PL: physical limitation; QL: quality of life; TS: treatment satisfaction.
Multivariable logistic analysis showed that CABG was an independent predictor for both improvement of angina frequency (OR: 1.62, 95% CI: 1.09−4.63, P = 0.042) and quality of life (OR: 2.04, 95% CI: 1.26−6.92, P = 0.038) when compared with PCI.
4. Discussion
The main findings of this observational study are that PCI and CABG improve disease-specific health status in NSTE-ACS. Improvement was greater for CABG in angina frequency, treatment satisfaction and quality of life domains of the SAQ. A greater proportion of the CABG group had clinically significant improvements in the scores for angina frequency and quality of life after six months, the extent of improvement being slightly greater with CABG than with PCI. It is worth remembering that therapeutic procedures are performed not only to prevent events but also improve disease-specific health status.
Several previous studies have evaluated the HRQL of patients with coronary heart disease.[11]–[15] These studies have tended to show that compared with PCI, CABG results in superior angina relief over the first three years after initial revascularization. The RITA (Randomized Intervention Treatment of Angina) and BARI15 (Bypass Angioplasty Revascularization Intervention) trials had similar findings.[16],[17] In the RITA trial, there was a 9.8% difference in the prevalence of angina at one year in favour of CABG vs. balloon angioplasty; in the BARI trial, the difference in angina relief was even larger at one year in favour of CABG.
Our study focused on the NSTE-ACS population. The lessons from epidemiological observations are that treatment strategies for NSTE-ACS not only need to address the acute phase, but with the same intensity impact on longer term management. Consistent with previous studies,[18]–[21] we also found significant improvements. Despite inclusion of patients with more complex coronary artery disease than those in previous trials, the SYNTAX[22] and FREEDOM[23] trials showed that continued evolution of PCI techniques, including stenting, has narrowed the gap in health related quality of life between patients who undergo PCI and those who undergo CABG. Our results demonstrated a slight benefit of CABG over PCI in patients with NSTE-ACS. The responses to the Seattle angina questionnaire in the PCI and CABG groups showed that the improvement in rates of angina were lower in the PCI group than in the CABG group during follow-up. This result shows that revascularization treatment is beneficial for the relief of symptoms in patients with NSTE-ACS, and that CABG as compared to PCI patients had significantly greater improvement in this SAQ score. CABG group had a better health status than the PCI group may be explained by the bypass grafts to the mid-coronary vessel treating both the culprit lesion and also offering prophylaxis against new proximal disease. However, stents in the proximal coronary artery cannot protect against new disease, and there is a significantly higher risk of revascularization with PCI.[24],[25] Another possible reason might be CABG has some of the antianginal benefits unrelated to relief of myocardial ischemia (e.g., denervation, placebo effects). Although the difference was largely driven by repeat revascularization there was no significant difference in mortality.
Quality of life scores improved less than previous studies, the average age of our study is older than these studies, elderly patients improve little in quality of life. According to some studies, elderly patients experience worse HRQL than younger patients after PCI and CABG.[26]
To our knowledge, few studies have focused on the health status changes in a Chinese NSTE-ACS population after different revascularization treatments. Because of the economic, cultural, health and other reasons, Chinese people have their own specialty. An initial strategy of PCI or CABG relieved angina and improved the NSTE-ACS patients' health status. A greater benefit from CABG was observed in those patients with NSTE-ACS.
There are inherent limitations to our study. First, this was a single center non-randomized, observational study. This nonrandomized nature may lead to several potential forms of bias. The choice of revascularization was at the discretion of the treating physician or patient. This indication bias may affect the results of our study in that the indication for treatment may affect outcomes and answers to the SAQ. Although this bias may not be entirely obviated, it was minimized by the adjustment of factors such as patient demographics and coexisting medical conditions by using multivariable logistic modeling. Future randomized prospective studies are warranted. Furthermore, the small sample and short follow-up period in the study could diminish the statistical power and underestimate differences at follow-up.
In conclusion, in this observational study, we found that revascularization treatment including PCI and CABG provides large gains in disease-specific quality of life in patients with NSTE-ACS, and that CABG improved the quality of life slightly better than PCI.
Acknowledgments
We declare that all the authors have no conflict of interest. We appreciate the help provided by Dr. John Spertus for language polishing.
References
- 1.Kushner FG, Hand M, Smith SC, Jr, et al. Focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2009;120:2271–2306. doi: 10.1161/CIRCULATIONAHA.109.192663. [DOI] [PubMed] [Google Scholar]
- 2.Hamm CW, Bassand JP, Agewall S, et al. ESC Committee for practice guidelines. ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 3.Hamm CW, Bertrand M, Braunwald E. Acute coronary syndrome without ST elevation: implementation of new guidelines. Lancet. 2001;358:1533–1538. doi: 10.1016/S0140-6736(01)06585-0. [DOI] [PubMed] [Google Scholar]
- 4.Spertus J, McDonell M, Fihn S. Association between depression and worse disease-specific functional status in outpatients with coronary artery disease. Am Heart J. 2000;140:105–110. doi: 10.1067/mhj.2000.106600. [DOI] [PubMed] [Google Scholar]
- 5.Spertus JA, Jones P, McDonell M, et al. Health status predicts long-term outcome in outpatients with coronary disease. Circulation. 2002;106:43–49. doi: 10.1161/01.cir.0000020688.24874.90. [DOI] [PubMed] [Google Scholar]
- 6.Spertus JA, Winder JA, Dewhurst TA, et al. Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol. 1994;74:1240–1244. doi: 10.1016/0002-9149(94)90555-x. [DOI] [PubMed] [Google Scholar]
- 7.Kimble LP, Dunbar SB, Weintraub WS, et al. The Seattle angina questionnaire: reliability and validity in women with chronic stable angina. Heart Dis. 2002;4:206–211. doi: 10.1097/00132580-200207000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dougherty CM, Dewhurst T, Nichol WP, et al. Comparison of three quality of life instruments in stable angina pectoris: Seattle angina questionnaire, short form health survey (SF-36), and quality of life index-cardiac version III. J Clin Epidemiol. 1998;51:569–575. doi: 10.1016/s0895-4356(98)00028-6. [DOI] [PubMed] [Google Scholar]
- 9.Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle angina questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 10.Wyrwich KW, Spertus JA, Kroenke K, et al. Clinically important differences in health status for patients with heart disease: an expert consensus panel report. Am Heart J. 2004;147:615–622. doi: 10.1016/j.ahj.2003.10.039. [DOI] [PubMed] [Google Scholar]
- 11.Perers E, Caidahl K, Herlitz J, et al. Spectrum of acute coronary syndromes: history and clinical presentation in relation to sex and age. Cardiology. 2004;102:67–76. doi: 10.1159/000077907. [DOI] [PubMed] [Google Scholar]
- 12.Beck CA, Joseph L, Belisle P, et al. Predictors of quality of life 6 months and 1 year after acute myocardial infarction. Am Heart J. 2001;142:271–279. doi: 10.1067/mhj.2001.116758. [DOI] [PubMed] [Google Scholar]
- 13.Veenstra M, Pettersen KI. Association of changes in health-related quality of life in coronary heart disease with coronary procedures and sociodemographic characteristics. Health Qual Life Outcomes. 2004;2:56. doi: 10.1186/1477-7525-2-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Failde II, Soto MM. Changes in health related quality of life 3 months after an acute coronary syndrome. BMC Public Health. 2006;6:18. doi: 10.1186/1471-2458-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Five-year clinical and functional outcome comparing bypass surgery and angioplasty in patients with multivessel coronary disease. A multicenter randomized trial. Writing Group for the Bypass Angioplasty Revascularization Investigation (BARI) Investigators. JAMA. 1997;277:715–721. [PubMed] [Google Scholar]
- 16.Henderson RA, Pocock SJ, Sharp SJ, et al. Long-term results of RITA-1 trial. Lancet. 1998;352:1419–1425. doi: 10.1016/s0140-6736(98)03358-3. [DOI] [PubMed] [Google Scholar]
- 17.Fox KA, Poole-Wilson P, Clayton TC, et al. 5–year outcome of an interventional strategy in non-ST-elevation acute coronary syndrome: the British Heart Foundation RITA 3 randomised trial. Lancet. 2005;366:914–920. doi: 10.1016/S0140-6736(05)67222-4. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Z, Spertus JA. The impact of acute coronary syndrome on clinical, economic, and cardiac-specific health status after coronary artery bypass surgery versus stent-assisted percutaneous coronary intervention: 1-year results from the stent or surgery (SoS) trial. Am Heart J. 2005;150:175–181. doi: 10.1016/j.ahj.2005.01.019. [DOI] [PubMed] [Google Scholar]
- 19.Serruys PW, Morice MC, Kappetein P. Percutaneous coronary Intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–972. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 20.Norris CM, Saunders LD, Ghali WA, et al. Health related quality of life outcomes of patients with coronary artery disease treated with cardiac surgery, percutaneous coronary intervention or medical management. Can J Cardiol. 2004;20:1259–1266. [PubMed] [Google Scholar]
- 21.Favarato ME, Hueb W, Boden WE, et al. Quality of life in patients with symptomatic multivessel coronary artery disease: a comparative post hoc analyses of medical, angioplasty or surgical strategies-MASS II trial. Int J Cardiol. 2007;116:364–370. doi: 10.1016/j.ijcard.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 22.Cohen DJ, Van Hout B, Serruys PW, et al. Synergy between PCI with taxus and cardiac surgery investigators. quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N Engl J Med. 2011;364:1016–1026. doi: 10.1056/NEJMoa1001508. [DOI] [PubMed] [Google Scholar]
- 23.Mouin S, Kaijun Wang, Elizabeth A, et al. Quality of life after PCI vs. CABG among patients with diabetes and multivessel coronary artery disease. JAMA. 2013;310:1581–1590. doi: 10.1001/jama.2013.279208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wahrborg P. Quality of life after coronary angioplasty or bypass surgery.1-year follow-up in the coronary angioplasty versus bypass revascularization investigation (CABRI) trial. Eur Heart J. 1999;20:653–658. doi: 10.1053/euhj.1998.1237. [DOI] [PubMed] [Google Scholar]
- 25.Glaser R, Herrmann HC, Murphy SA, et al. Benefit of an early invasive management strategy in women with acute coronary syndromes. JAMA. 2002;288:3124–9. doi: 10.1001/jama.288.24.3124. [DOI] [PubMed] [Google Scholar]
- 26.Taggart DP. PCI or CABG in coronary artery disease? Lancet. 2009;373:1150–1152. doi: 10.1016/S0140-6736(09)60574-2. [DOI] [PubMed] [Google Scholar]