ABSTRACT
Alphavirus replicons were evaluated as potential vaccine candidates for Venezuelan equine encephalitis virus (VEEV), western equine encephalitis virus (WEEV), or eastern equine encephalitis virus (EEEV) when given individually or in combination (V/W/E) to mice or cynomolgus macaques. Individual replicon vaccines or the combination V/W/E replicon vaccine elicited strong neutralizing antibodies in mice to their respective alphavirus. Protection from either subcutaneous or aerosol challenge with VEEV, WEEV, or EEEV was demonstrated out to 12 months after vaccination in mice. Individual replicon vaccines or the combination V/W/E replicon vaccine elicited strong neutralizing antibodies in macaques and demonstrated good protection against aerosol challenge with an epizootic VEEV-IAB virus, Trinidad donkey. Similarly, the EEEV replicon and V/W/E combination vaccine elicited neutralizing antibodies against EEEV and protected against aerosol exposure to a North American variety of EEEV. Both the WEEV replicon and combination V/W/E vaccination, however, elicited poor neutralizing antibodies to WEEV in macaques, and the protection conferred was not as strong. These results demonstrate that a combination V/W/E vaccine is possible for protection against aerosol challenge and that cross-interference between the vaccines is minimal.
IMPORTANCE Three related viruses belonging to the genus Alphavirus cause severe encephalitis in humans: Venezuelan equine encephalitis virus (VEEV), western equine encephalitis virus (WEEV), and eastern equine encephalitis virus (EEEV). Normally transmitted by mosquitoes, these viruses can cause disease when inhaled, so there is concern that these viruses could be used as biological weapons. Prior reports have suggested that vaccines for these three viruses might interfere with one another. We have developed a combined vaccine for Venezuelan equine encephalitis, western equine encephalitis, and eastern equine encephalitis expressing the surface proteins of all three viruses. In this report we demonstrate in both mice and macaques that this combined vaccine is safe, generates a strong immune response, and protects against aerosol challenge with the viruses that cause Venezuelan equine encephalitis, western equine encephalitis, and eastern equine encephalitis.
INTRODUCTION
Three positive-stranded RNA viruses found in the Americas belonging to the family Togaviridae and genus Alphavirus cause encephalitic disease in mammals, particularly in equids and humans (1). They are roughly designated by geographical location, with Venezuelan equine encephalitis virus (VEEV) found in South and Central America while western equine encephalitis virus (WEEV) is found along the western half of North America. Eastern equine encephalitis virus (EEEV) was originally thought to be primarily restricted to the eastern coast of North America; but it has been found as far west as Louisiana in North America, and isolates have been found in South America. Unlike the highly virulent isolates of EEEV found in North America, South American isolates are considered avirulent in humans. Naturally transmitted by mosquitoes, all three viruses are highly infectious by the aerosol route and can cause significant morbidity and mortality. For these reasons they are considered potential biological weapons, and licensed medical countermeasures that can prevent or treat the diseases caused by these viruses are considered highly desirable.
Early attempts to develop vaccines for VEEV, WEEV, and EEEV focused on classical approaches. The TC-83 vaccine strain for VEEV, the only live alphavirus vaccine currently available for limited human use, was derived by serial passage of virulent virus in cell culture. However, TC-83 has a high potential for reversion and offers poor protection against enzootic subtypes of VEEV (2–4). Killed whole-virus vaccines have been developed for VEEV (C-84), WEEV, and EEEV by formalin treatment, and while these vaccines are safe, they also have a high failure rate for seroconversion (2, 5–7). All four vaccines have been used successfully for veterinary applications for several decades but are available only on a limited basis for human use. Based on nonhuman primate (NHP) data with TC-83 and C-84 as well as human cases of VEEV in vaccinated individuals, none of the current vaccines is thought to offer good protection against aerosol exposure, particularly against enzootic subtypes of VEEV.
A variety of approaches have been used to generate candidate vaccines to replace the current vaccines. Subunit vaccines derived from a variety of expression systems have shown efficacy in rodent models (8–11). DNA vaccines, administered by several means, have also shown efficacy in rodents and nonhuman primates (12–14). Live attenuated vaccines developed using modern molecular techniques provided good immunogenicity, safety, and protection in rodents and nonhuman primates although in phase I clinical trials mild fever responses were seen at very low dosages (15–17). Other approaches using live attenuated vaccines are being evaluated and have shown promise in mice and nonhuman primates (18–20). However, the public perception of the risk associated with live vaccines in general has created great resistance to their potential use. An additional concern for alphavirus vaccines is cross-interference with other alphavirus vaccines (21–24).
As an alternative to conventional live attenuated vaccines, alphavirus replicons have been proposed to circumvent some of the concerns regarding potential reversion to virulence surrounding live vaccines. An alphavirus replicon is derived by deletion of the genes encoding viral structural proteins from full-length genomic cDNA clones (25). The replicon retains all of the machinery necessary for its replication and transcription once it is introduced into an appropriate cell type (26). Placement of an alternative gene(s) encoding an immunogen at the site of the deleted structural proteins results in its expression in lieu of the viral structural proteins (25, 27). Alphavirus replicons have been used successfully to express immunogens for a number of pathogens (28–34). We report here efforts to develop a combination vaccine that would protect against all three encephalitic alphaviruses (VEEV, WEEV, and EEEV).
MATERIALS AND METHODS
Ethics statement.
Research was conducted in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals. All research described herein adhered to the principles stated in the Guide for the Care and Use of Laboratory Animals. All research described herein adhered to the principles stated in the Public Health Services (PHS) Policy on Humane Care and Use of Laboratory Animals. The research described herein was approved by the U.S. Army Medical Research Institute of Infectious Disease (USAMRIID) Laboratory Animal Care and Use Committee, protocol AP-07-12. The facility where this research was conducted is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International (Rockville, MD). NHPs were housed in an air-conditioned facility with an ambient temperature of 21 to 25°C, a relative humidity of 40% to 60%, and a 12-h light/dark cycle. All NHPs were housed in individual cages and provided a commercial primate diet. Enrichment was provided in accordance with AAALAC or PHS guidelines. NHPs were anesthetized with tiletamine-zolazepam (6 mg/kg) or ketamine (9 mg/kg) given intramuscularly (i.m.) before any procedures (cage change, phlebotomy, surgery, aerosol exposure, or euthanasia). Isoflurane gas was used for maintenance of the anesthetized state during surgical implantation of telemetry devices. All efforts were made to minimize pain and distress after exposure to alphaviruses; however, analgesics were not given as this could mask clinical signs of the disease, a critical piece of these studies. All NHPs were monitored at least twice daily after aerosol exposure to alphaviruses, with an increased frequency of observation at the onset of neurological signs (every 6 to 8 h). When clinical signs indicated that NHPs were moribund, euthanasia was performed promptly by injection of anesthetic followed by intravenous (i.v.) injection of a barbiturate overdose once the animal was anesthetized.
Cells.
African green monkey (Vero) and baby hamster kidney (BHK) cells were grown in minimal essential medium supplemented with 5% Cosmic calf serum, 1% antibiotics (100 U/ml penicillin, 100 μg/ml streptomycin, and 50 μg/ml gentamicin), and 1× nonessential amino acids at 37°C with 5% CO2.
Viruses.
The following viruses were used in these studies: VEEV subtype IAB (VEEV-IAB) (strains TrD and TC-83) (35, 36), VEEV-IC (strain P676) (37), VEEV-ID (strain 3880) (38), VEEV-IE (strain 68U201) (39), VEEV-IIIA (Mucambo) (4), WEEV (strain CBA-87) (40), and EEEV (strain FL91-4679) (41). All viruses were passaged in Vero cells and stored at −80°C until use. For aerosol exposures, viruses were diluted to the appropriate concentration in Hanks' balanced salt solution (HBSS) containing 1% fetal bovine serum.
Construction of replicon vectors.
Glycoprotein (GP) genes for VEEV (strain V3014) (25, 42), EEEV (strain FL91-4679), or WEEV (strain CBA-87) were constructed that lacked furin cleavage sites between the E3 and E2 proteins (Fig. 1). The furin cleavage site deletion resulted in expression of an unprocessed form of the E2 glycoprotein (PE2). Optimized replicon vectors expressing the furin cleavage site mutant GP genes were constructed as previously described (27). The VEEV, EEEV, and WEEV GP genes were derived from plasmid DNAs pV3014, pE4200, and pW2130, respectively (25). DNA containing the GP genes was provided by Michael Parker, USAMRIID.
FIG 1.
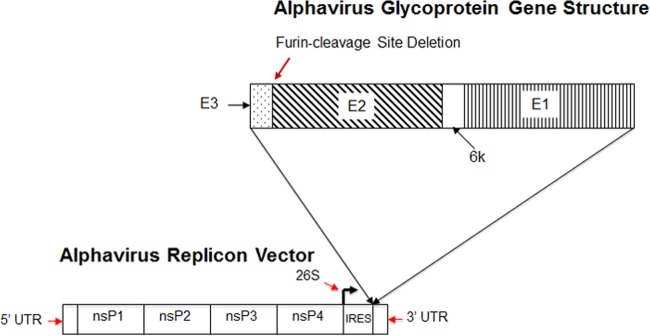
Schematic of an equine encephalitis GP furin cleavage site deletion mutant gene cloned into an optimized alphavirus replicon vector. nsP1 to nsP4, nonstructural proteins 1 to 4; UTR, untranslated region; IRES, internal ribosome entry site; 26S, alphavirus subgenomic promoter.
Electroporation.
Vero cells grown in minimal essential medium supplemented with 5% Cosmic calf serum, 1% antibiotics (100 U/ml penicillin, 100 μg/ml streptomycin, and 50 μg/ml gentamicin), and 1× nonessential amino acids (complete medium) were harvested by trypsinization. Harvested cells were washed twice with 200 ml of cold wash buffer (5% sucrose, 60 mM NaCl, 10 mM Na3PO4, pH 7.3) and then suspended in wash buffer at a final density of 1.3 × 108 cells/ml. An aliquot (600 μl) of prepared cells (7.8 × 107 cells) was combined with 30 μg of in vitro-transcribed replicon RNA containing either the VEEV, EEEV, or WEEV GP coding region with the furin deletion mutation. The cells and RNA were transferred to a 0.4-cm gap cuvette and pulsed four times at a voltage of 580 V and a capacitance of 25 μF in a Gene Pulser XCell (Bio-Rad). Electroporated cells were incubated at room temperature for 5 min; then one half of the cells were transferred to 50 ml of complete medium. Both 48-well plates and 6-well plates were seeded from the cell suspension with 200 μl and 3 ml, respectively. The electroporated cells were incubated overnight at 37°C with 5% CO2 and were then used to examine GP expression by immunofluorescence and Western blotting as described below.
Immunofluorescence.
At 18 h postelectroporation, cells from the 48-well plate were washed twice in phosphate-buffered saline (PBS) and then fixed for 5 min at room temperature with cold acetone-methanol (1:1). Fixed cells were washed three times with PBS and then incubated with respective antibodies. The cells electroporated with VEEV replicon were stained with a goat anti-VEEV GP (1:1,000) prepared at AlphaVax, Inc. (Research Triangle Park, NC). Cells electroporated with EEEV and WEEV replicons were stained with mouse monoclonal EEEV-specific (1:200) and WEEV-specific (1:200) antibodies provided by the National Veterinary Diagnostic Lab in Ames, IA. Cells were also stained with a goat anti-nsP2 antibody as a positive control. Secondary antibodies were either anti-goat or anti-mouse Alexa Fluor 288 (1:500).
Western blotting.
At 18 h postelectroporation, cells from a single well of a six-well plate were lysed in 500 μl of a Triton X-100 lysis buffer per sample for 15 min at room temperature. Nuclei were removed by centrifugation, and the supernatant containing the soluble protein was retained. Total protein concentration was determined using a bicinchoninic acid (BCA) kit (Pierce). Deglycosylation was carried out on 15 μg of total cellular protein with 2,000 units of peptide-N-glycosidase F (PNGase F; NEB). An aliquot (10 μg) of either untreated or deglycosylated total cellular protein was run on a 4 to 12% gradient bis-Tris polyacrylamide gel. Separated proteins were transferred to a polyvinylidene difluoride (PVDF) membrane via a semidry electroblotting method (Bio-Rad). Membranes were blocked and probed with the same antibodies described in the immunofluorescence method. Antibody dilutions were as follows: goat anti-VEEV GP, 1:2,000; mouse anti-EEEV, 1:400; and mouse anti-WEEV, 1:100. VEEV, EEEV, and WEEV GPs were detected using horseradish peroxidase (HRP)-labeled anti-goat or anti-mouse antibody (Kirkegaard and Perry Laboratories) and visualized by chemiluminescence using an HRP substrate kit (ECL Western blotting substrate; Pierce).
VRP production.
The procedures used for making virus-like replicon particles (VRP), based on a two-helper system, are described in detail in Kamrud et al. (27). Briefly, Vero cells (1 × 108 cells) suspended in PBS were combined with 30 μg of replicon, 20 μg of capsid helper, and 60 μg of GP helper RNA in 0.4-cm electroporation cuvettes and electroporated using a Bio-Rad Gene Pulser (Bio-Rad). The capsid and GP helper RNAs were derived from the V3014 strain of VEEV (25). The cells and RNA were pulsed four times with electroporator settings of 580 V and 25 μF. Electroporated cell suspensions were seeded into individual roller bottles containing 150 ml of OptiPro medium (Invitrogen) supplemented with antibiotics and incubated at 37°C in 5% CO2 for 16 to 24 h. VRP were harvested, and the titers of the VRP were determined by immunofluorescence assay (IFA) using goat anti-VEEV nsP2-specific polyclonal antiserum as the primary antibody and donkey anti-goat Alexa Fluor 488 (Invitrogen) as the secondary antibody on methanol-fixed cells using a Nikon Eclipse TE300 fluorescence microscope. The VRP were tested for the presence of contaminating replication-competent VEEV (RCV) following two blind passages on Vero cells, as described previously (27). The VRP titers are expressed as infectious units (IU). VRP were purified by affinity column chromatography using Cellufine sulfate resin (Chisso Corporation, Tokyo, Japan) as described previously (27) and formulated in 10 mM Na3PO4 buffer, pH 7.3, containing 1% normal serum, 5% sucrose, 200 mM NaCl. The VRP were stored at −80°C until used.
PRNT.
To determine the plaque reduction neutralization titer (PRNT), 2-fold dilutions of serum starting at 1:20 were mixed with equal volumes of medium containing 200 PFU of virus and incubated overnight at 4°C. The following day, six-well plates containing confluent monolayers of Vero cells were incubated at 37°C for 1 h with the virus-antibody mixtures, after which a medium-agarose overlay was added. One day later, 1 ml of a solution of 5 to 6% neutral red in 1× HBSS (without phenol red) was added to each well, and plaques were counted 24 h later.
ELISA.
Enzyme-linked immunosorbent assays (ELISA) were done using standard ELISA procedures. Briefly, dilutions of primate serum were incubated for 1 h at room temperature on Microlite 2+ 96-well plates (Thermo Labsystems, Waltham, MA) coated with sucrose gradient-purified, γ-irradiated VEEV. After plates were washed with PBS-Tween, secondary goat anti-monkey IgG-HRP (Research Diagnostics, Flanders, NJ) was added to the plates, and they were incubated for an additional hour at room temperature; next, the plates were washed again, and BM chemiluminescence substrate (Roche Applied Sciences, Brandford, CT) was added for 30 min before the plate was read on an Lmax plate reader (Molecular Devices, Sunnyvale, CA).
Testing vaccine candidates in rodents.
Groups of 10 female BALB/c mice approximately 6 to 8 weeks of age (National Cancer Institute, Frederick, MD) were inoculated subcutaneously (s.c.) with 1 × 107 IU of each vaccine on day 0 and day 28. Mice vaccinated with a mixture of VEEV-GP, EEEV-GP, and WEEV-GP (V/E/W GP) VRP received a total of 3 × 107 IU (1 × 107 IU of each VRP). Mice were challenged with VEEV (1 × 104 PFU of TrD), WEEV (2 × 104 PFU) or EEEV (1 × 105 PFU) by the subcutaneous or aerosol route of exposure at various times postvaccination depending on the animal study. Two independent mouse studies were conducted. The first study examined immunogenicity and efficacy of the vaccines either alone or in a mixture containing all three VRP vaccines. Serum was collected from all mice at 4 weeks post-priming vaccination (postprime) and again prior to virus challenge on day 63. The second study examined the duration of immunity provided by each vaccine either alone or in a mixture containing all three VRP. In the second study, mice were vaccinated on day 0 and day 28. Mice were challenged with virus at 1.5 months postprime, 2 months postprime, 6 months postprime, or 12 months postprime by either the subcutaneous or aerosol route of exposure as previously described (16, 43).
Testing vaccine candidates in macaques.
Healthy, adult cynomolgus macaques (Macaca fascicularis) of both sexes were obtained from the USAMRIID nonhuman primate colony for use in these studies. Before macaques were assigned to these studies, blood samples from each macaque were screened for PRNT for any evidence of previous exposure to VEEV-IA/B, VEEV-IE, VEEV-IIIA, WEEV, and EEEV. Telemetry implants (TA10TA-D70; Data Sciences International, St. Paul, MN) were implanted s.c. on the dorsal surface to monitor body temperature and activity. Macaques were allowed to recover from surgery prior to study initiation. Body temperature and activity were recorded every 15 min by the DataQuest A.R.T. Gold system (Data Sciences International). Using data collected prior to challenge, an autoregressive integrated moving-average model for each macaque was developed and used to forecast body temperature during the postexposure period (15, 44–47). Residual temperature changes postexposure were determined by subtracting the predicted temperature from the actual temperature recorded for each point. Residual temperature changes greater than 3 standard deviations above the training period level were used to compute fever duration (number of hours or days of significant temperature elevation) and fever-hours (sum of the significant temperature elevations).
Macaques were randomly divided into groups (n = 6), and each macaque received a single s.c. inoculation of a vaccine candidate or culture medium, followed by a second inoculation 28 days later. The projected replicon dose was 2 × 108 IU per vaccine candidate (V/W/E total dosage 6 × 108 IU). On day 60 (VEEV and EEEV) or day 109 (WEEV) after vaccination, macaques were anesthetized with tiletamine-zolazepam (6 mg/kg, i.m.; Aveco Co., Fort Dodge, IA) and exposed for 10 min to an aerosol containing virulent VEEV TrD, WEEV, or EEEV at dosages previously determined to be sufficient to cause disease (15, 16, 44, 45, 47, 48). Blood samples were collected on days 14, 42, 56, 77, and 109 to evaluate changes in PRNTs. Macaques were bled daily beginning 3 days prior to challenge up to 10 days postchallenge to monitor viremia and changes in leukocytes as previously described (15, 44, 45, 47, 48).
RESULTS
Expression analysis of VEEV, EEEV, and WEEV GP replicon vectors.
Vero cells electroporated with VEEV-GP, EEEV-GP, or WEEV-GP replicon RNA were used to generate cell lysates that were analyzed by Western blotting using antibodies that recognize the E2 protein of each virus. Cell lysates were also treated with PNGase F to evaluate the glycosylation state of each of the expressed proteins. All three GP replicons expressed proteins of the expected molecular mass for their respective PE2 proteins (Fig. 2). This result indicated that the furin cleavage site mutation ablated the cleavage of E3 from E2. In addition, PNGase F treatment demonstrated that the PE2 protein was being processed correctly; treated samples showed a reduction in molecular mass equivalent to the cleavage of glycosylated residues (Fig. 2).
FIG 2.
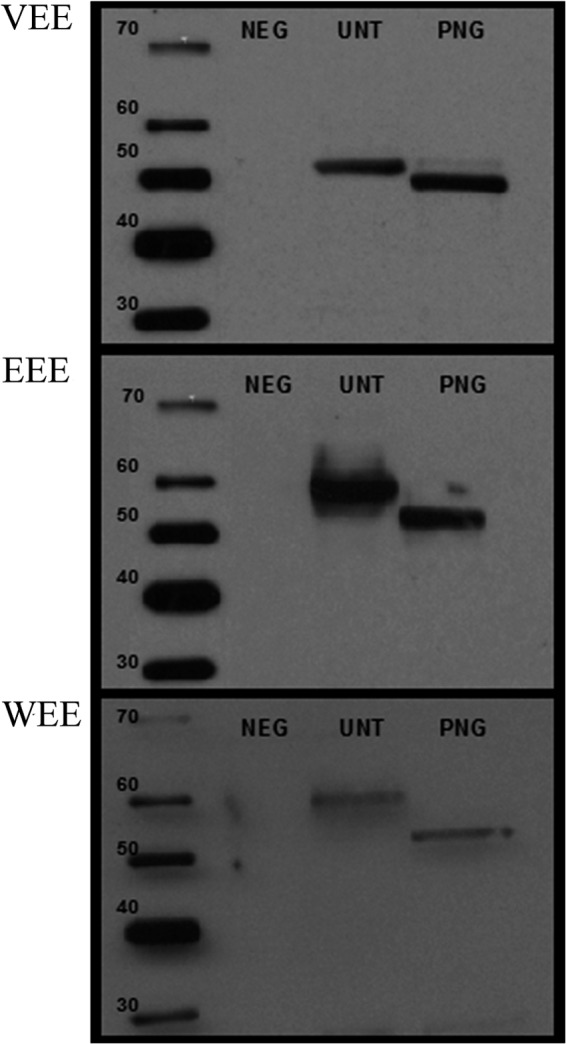
Western blot analysis of VEEV, WEEV, and EEEV GP replicon vectors. Vero cells were electroporated with VEEV, EEEV, or WEEV GP replicon RNA. At 18 h postelectroporation, cells were lysed in Triton X-100 lysis buffer. Nuclei were removed, and total protein concentration was determined. Samples were deglycosylated with PNGase F. Following treatment, samples were separated in a 4 to 12% gradient bis-Tris polyacrylamide gel and transferred to PVDF membrane. Western blotting was performed using VEEV-, EEEV-, or WEEV-specific GP serum and HRP-labeled secondary antibody. Proteins were visualized by addition of chemiluminescence substrate. The unglycosylated (PNG column) molecular mass for the PE2 proteins is predicted to be 53.7 kDa. NEG, control Vero cell lysate; UNT, VEEV, WEEV, or EEEV GP replicon electroporated cells untreated with PNGase F enzyme; PNG, VEEV, WEEV, or EEEV GP replicon electroporated cell lysates treated with PNGase F enzyme.
VEEV, EEEV, and WEEV GP expression was also analyzed by immunofluorescence assay (IFA). Vero cells electroporated with VEEV-GP, EEEV-GP, or WEEV-GP replicon RNA were fixed and analyzed with the same antibodies used for Western blotting. Each replicon expressed protein recognized specifically by the respective anti-VEEV, anti-EEEV, and anti-WEEV antibodies (Fig. 3).
FIG 3.
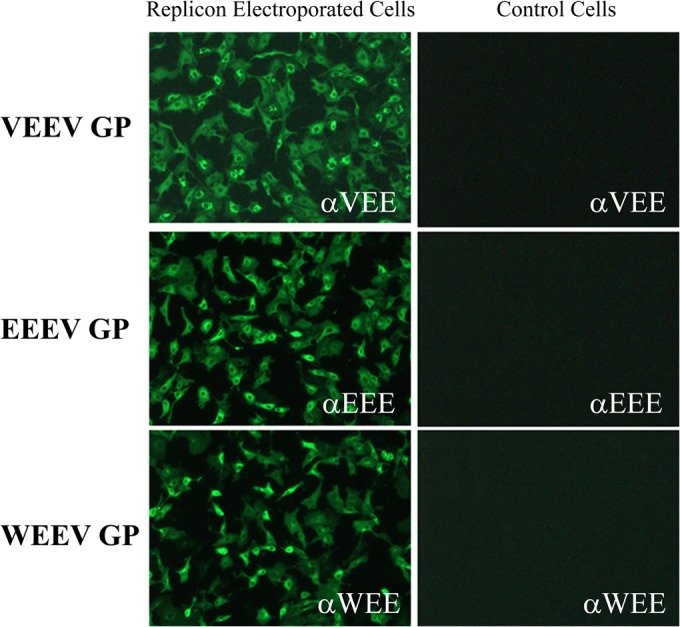
Immunofluorescence analysis of VEEV-GP, EEEV-GP, and WEEV-GP replicon electroporated Vero cells. Vero cells were electroporated with VEEV-GP, EEEV-GP, or WEEV-GP RNA. Following electroporation, cells were seeded in a 48-well plate. At 18 h postelectroporation, cells were fixed with acetone-methanol (1:1), and IFA was performed. E2 protein was detected using anti-VEEV, anti-EEEV, or anti-WEEV E2-specific monoclonal antibodies and visualized by Alexa Fluor 288-labeled secondary antibody. Control cells received no RNA at electroporation and show no specific fluorescence with any of the antibodies in the assay. α, anti.
Immunogenicity, efficacy, and duration of immunity of VEEV-GP, EEEV-GP, and WEEV-GP VRP vaccines in mice.
Two mouse studies were conducted to examine the candidate VEEV-GP, EEEV-GP, and WEEV-GP VRP vaccines. The first mouse study evaluated the immunogenicity and efficacy of the individual VRP vaccines and an equimolar mixture of all three. Immunogenicity was measured by virus-specific ELISA and by virus neutralization assay. For VEEV analysis, viruses from three different subtypes were used to examine both homologous (VEEV-IAB) and heterologous (VEEV-IIIA and -IE) reactivity and protection from challenge. A summary of the ELISA results and 80% plaque reduction neutralization titers (PRNT80) are presented in Table 1. VEEV-GP VRP-vaccinated mouse samples were tested against the homologous VEEV-IAB subtype as well as VEEV-IE and -IIIA subtypes by both PRNT80 and ELISA. While low or undetectable neutralizing responses were noted after the prime vaccination, strong homologous VEEV-IAB virus neutralization titers were detected after mice were boosted. All VEEV-GP VRP-vaccinated mice demonstrated both homologous and heterologous VEEV ELISA reactivity after the priming vaccination, and these titers uniformly increased for the different VEEV strains after the boost (Table 1). Complete protection from homologous or heterologous VEEV challenge was demonstrated in all groups vaccinated with VEEV-GP VRP alone or with a mixture of VEEV-GP, EEEV-GP, and WEEV-GP VRP (V/E/W VRP) by both the s.c. and aerosol challenge routes. Interestingly, mice that received the control VRP vaccination (VRP expressing the HIV Gag gene) also demonstrated some protection from VEEV challenge even though virus neutralization by PRNT80 was not detected (Table 1). This phenomenon was most evident in mice challenged with VEEV by the s.c. route, suggesting that the aerosol route is a more stringent challenge (49). The groups challenged with EEEV and WEEV used only the aerosol route of exposure because adult mice are less susceptible to s.c. challenge with these viruses and because the aerosol challenge route provided a more stringent evaluation of vaccine efficacy.
TABLE 1.
Summary of VEEV-GP immunogenicity and efficacy mouse study
| Challenge virus and route | VRP type | PRNT80a |
IgG titera |
Survival rateb | % survival | ||
|---|---|---|---|---|---|---|---|
| Day 28 | Day 63 | Day 28 | Day 63 | ||||
| VEEV-IAB | |||||||
| Subcutanteous | VEEV | 23 | 686 | 3,051 | 113,130 | 10/10 | 100 |
| V/W/E | 30 | 844 | 1,005 | 52,431 | 10/10 | 100 | |
| Mock | 20 | 20 | 33 | 33 | 2/5 | 40 | |
| HIV Gag | 20 | 20 | 33 | 33 | 10/10 | 100 | |
| Aerosol | VEEV | 25 | 46 | 4,677 | 90,814 | 10/10 | 100 |
| V/W/E | 26 | 92 | 2,167 | 90,814 | 10/10 | 100 | |
| Mock | 20 | 20 | 33 | 33 | 0/5 | 0 | |
| HIV Gag | 20 | 20 | 33 | 41 | 1/10 | 10 | |
| VEEV-IE | |||||||
| Subcutanteous | VEEV | 20 | 21 | 3,014 | 65,315 | 10/10 | 100 |
| V/W/E | 20 | 25 | 1,251 | 58,520 | 10/10 | 100 | |
| Mock | 20 | 20 | 33 | 33 | 0/5 | 0 | |
| HIV Gag | 20 | 21 | 33 | 33 | 4/10 | 40 | |
| Aerosol | VEEV | 34 | 130 | 466 | 19,507 | 10/10 | 100 |
| V/W/E | 33 | 121 | 300 | 17,477 | 10/10 | 100 | |
| Mock | 33 | 20 | 33 | 41 | 0/5 | 0 | |
| HIV Gag | 33 | 23 | 33 | 64 | 3/10 | 30 | |
| VEEV-IIIA, aerosol | VEEV | 20 | 28 | 1,740 | 90,814 | 10/10 | 100 |
| V/W/E | 20 | 25 | 647 | 46,976 | 10/10 | 100 | |
| Mock | 20 | 20 | 33 | 80 | 0/5 | 0 | |
| HIV Gag | 20 | 25 | 33 | 173 | 0/10 | 0 | |
PRNT80 and IgG titer are the reciprocal of the endpoint dilution.
Number of survivors/total number of mice in group.
Mice vaccinated with EEEV-GP VRP either alone or in a mixture of V/E/W VRP demonstrated anti-EEEV immunity 28 days after a single vaccination by both ELISA and virus neutralization assays (Table 2). These immune responses uniformly increased after the boost, and all mice that received the EEEV-GP VRP (alone or in a mixture of V/E/W VRP) were protected from EEEV aerosol challenge; all control mice succumbed to infection (Table 2).
TABLE 2.
Summary of EEEV-GP and WEEV-GP immunogenicity and efficacy mouse studies
| Challenge virusb | VRP type | PRNT80b |
IgG titerb |
Survival ratec | % survival | ||
|---|---|---|---|---|---|---|---|
| Day 28 | Day 63 | Day 28 | Day 63 | ||||
| EEEV | EEEV | 640 | 11,763 | 5,826 | 81,365 | 10/10 | 100 |
| V/W/E | 2,229 | 12,607 | 9,146 | 65,315 | 10/10 | 100 | |
| HIV Gag | 20 | 20 | 33 | 33 | 0/10 | 0 | |
| WEEV | WEEV | 28 | 485 | 2,167 | 113,130 | 10/10 | 100 |
| V/W/E | 20 | 139 | 647 | 3,027 | 10/10 | 100 | |
| HIV Gag | 20 | 20 | 33 | 37 | 0/10 | 0 | |
Aerosol route.
PRNT80 and IgG titer listed are the reciprocal of the endpoint dilution.
Number of survivors/total number of mice in group.
Mice vaccinated with WEEV-GP VRP either alone or in a mixture of V/E/W VRP demonstrated low or undetectable neutralizing responses after the prime vaccination while anti-WEEV antibodies were detected by ELISA at this time point (Table 2). Both ELISA results and virus neutralization activity were noted after mice were boosted prior to WEEV aerosol challenge. The virus neutralizing titers noted in mice that received the V/E/W VRP mixture were lower than in mice vaccinated with WEEV-GP VRP alone, but this difference did not influence the outcome of challenge as all mice receiving WEEV-GP VRP survived; none of the control mice survived challenge (Table 2).
The second set of murine studies examined the duration of immunity induced by VEEV-GP, EEEV-GP, and WEEV-GP VRP vaccines either alone or in a mixture. Mice were vaccinated two times at day 0 and day 28; groups were then challenged by the aerosol route with the respective viruses at 2 weeks postprime, 1 month postboost, 6 months postprime, and 12 months postprime.
Incomplete protection from aerosol challenge was noted 2 weeks after a single vaccination in all groups receiving VEEV-GP, EEEV-GP, WEEV-GP, or the V/E/W VRP mixture (Tables 3 and 4). However, complete protection from homologous or heterologous VEEV challenge as well as EEEV or WEEV challenge was demonstrated in all groups by 1 month postboost (Tables 3 and 4). Mice in the EEEV-GP VRP 1-month postboost group were not challenged with EEEV due to the presence of a pregnant mouse in the cohort; the mice were removed from the study. Although this group was lost for the duration of the immunity study, the mice whose data are reported in Table 2 represent a similar cohort, and that study demonstrated complete protection from EEEV aerosol challenge 1 month after a boost. Groups of mice were next challenged at 6 months postprime (5 months postboost).
TABLE 3.
Summary of VEEV-GP VRP duration of protection study
| Challenge virus and VRP typea | No. of survivors/total no. of mice in group by time of challenge (mos.)b |
|||
|---|---|---|---|---|
| 1.5 | 2 | 6 | 12 | |
| VEEV-IAB | ||||
| VEEV | 1/10 | 10/10 | 10/10 | 10/10 |
| V/W/E | 1/10 | 10/10 | 6/10 | 8/9 |
| Control | 0/5 | 0/5 | 0/5 | 0/4 |
| Mock | 0/5 | 0/5 | 0/5 | 0/5 |
| VEEV-IE | ||||
| VEEV | 2/10 | 10/10 | 9/10 | 10/10c |
| V/W/E | 3/10 | 10/10 | 10/10 | 7/9c |
| Control | 0/5 | 0/5 | 0/5 | 0/5 |
| Mock | 0/5 | 0/5 | 0/5 | 0/5 |
| VEEV-IIIA | ||||
| VEEV | 4/10 | 9/9 | 10/10 | 10/10c |
| V/W/E | 1/10 | 11/11 | 10/10 | 9/9c |
| Control | 0/5 | 0/5 | 0/5 | 0/5 |
| Mock | 0/5 | 0/5 | 0/5 | 0/5 |
Aerosol challenge.
Time of challenge is indicated as time post-priming vaccination.
Nonlethal illness observed.
TABLE 4.
Summary of EEEV-GP and WEEV-GP VRP duration of protection study
| Challenge virus and VRP typea | No. of survivors/total no. of mice in group by time of challenge (mos.)b |
|||
|---|---|---|---|---|
| 1.5 | 2 | 6 | 12 | |
| EEEV | ||||
| EEEV | 0/10 | —c | 10/10 | 10/10 |
| V/W/E | 0/10 | 10/10 | 9/9 | 9/10 |
| Control | 0/10 | 0/10 | 0/9 | 0/9 |
| WEEV | ||||
| WEEV | 2/10 | 10/10 | 10/10 | 9/9 |
| V/W/E | 1/10 | 10/10 | 9/10 | 7/8 |
| Control | 0/10 | 0/10 | 0/10 | 0/10 |
Aerosol challenge.
Time of challenge is indicated as time post-priming vaccination.
Experimental group removed from study due to pregnancy in cohort of animals.
For VEEV challenge, mice receiving the VEEV-GP VRP vaccine alone demonstrated 90% protection or better from homologous or heterologous VEEV challenge (Table 3). The same result was noted in mice receiving the V/E/W VRP mixture, with the exception of mice challenged with the homologous VEEV-IAB subtype; this group demonstrated 60% protection at the 6-month postprime time point (Table 3). Mice receiving the VEEV-GP VRP alone demonstrated complete protection from homologous or heterologous VEEV challenge at the 12-month postprime (11 months postboost) time point (Table 3). Mice receiving the V/E/W VRP mixture demonstrated between 77% and 100% protection at the 12-month postprime time point (Table 3). No clinical signs of illness were observed following homologous challenge; however, nonlethal illness was noted in mice receiving either VEEV-GP VRP alone or the V/E/W VRP mixture following heterologous challenge.
Mice vaccinated with EEEV-GP VRP alone demonstrated complete protection from EEEV challenge at both the 6-month and 12-month postprime time points (Table 4). Mice vaccinated with the V/E/W VRP mixture demonstrated complete protection at 6 months postprime and 90% protection at the 12-month postprime time point (Table 4). As noted for EEEV-GP VRP-vaccinated groups, mice vaccinated with WEEV-GP VRP alone demonstrated complete protection from WEEV challenge at both the 6-month and 12-month postprime time points (Table 4). Mice vaccinated with the V/E/W VRP mixture demonstrated 90% protection at 6 months postprime and 87.5% protection at the 12-month postprime time point (Table 4). No clinical signs of illness were observed in any of the vaccinated mice.
Protection of nonhuman primates against aerosol challenge with VEEV, EEEV, or WEEV.
Cynomolgus macaques (n = 6 per group) were vaccinated twice, 4 weeks apart, by s.c. inoculation with either individual replicon vaccines or in combination (V/W/E). A separate group of macaques was vaccinated with process control medium (mock-vaccinated group). On day 56, PRNT80 values were assessed against both epizootic and enzootic subtypes of VEEV as well as EEEV and WEEV (Table 5). Vaccination of macaques with individual replicon vaccines generated neutralizing antibody titers against their respective virus. The V/W/E combination vaccine also elicited neutralizing antibodies against all three viruses; against epizootic VEEV-IAB and EEEV, the combination vaccine elicited higher titers than did their respective individual vaccines in 12 out of 12 macaques tested. Against WEEV, the V/W/E combination vaccine elicited neutralizing antibody in only half of the macaques tested (9/18). Against the epizootic VEEV-IC and enzootic VEEV-ID and VEEV-IE subtypes, the VEEV VRP elicited neutralizing antibody responses in all 6 macaques. The V/W/E VRP combination vaccine also elicited responses against VEEV-IC, VEEV-ID, and VEEV-IE but not in all of the macaques tested, ranging from 25% (3 of 12 for VEEV-ID) to 75% (9 of 12 for VEEV-IC). The response to VEEV-IC, VEEV-ID, and VEEV-IE was lower in the V/W/E group than to VEEV alone, but the differences were only significant for VEEV-IE (P = 0.0702, 0.3976, 0.0250 for VEEV-IC, -ID, and -IE, respectively, using an unpaired t test with Welch's correction).
TABLE 5.
VRP immunogenicity in macaques on day 56 postvaccination
| VRP type | Mean PRNT80 (no. of animals responding/no. of animals tested)a |
|||||
|---|---|---|---|---|---|---|
| VEEV-IAB | VEEV-IC | VEEV-ID | VEEV-IE | WEEV | EEEV | |
| VEEV | 3,200 (6/6) | 667 (6/6) | 43 (6/6) | 307 (6/6) | <20 (0/6) | <20 (0/6) |
| WEEV | ND | ND | ND | ND | 80 (4/6) | ND |
| EEEV | 160 (1/6) | 50 (1/6) | <20 (0/6) | 20 (1/6) | <20 (0/6) | 163 (6/6) |
| V/W/E | 5,647 (12/12) | 142 (9/12) | 87 (3/12) | 57 (6/12) | 53 (9/18) | 417 (12/12) |
| Mock | <20 | <20 | <20 | <20 | <20 | <20 |
Values are reciprocals of the endpoint dilution. ND, not determined.
On day 60 after the initial vaccination, 6 macaques vaccinated with VEEV were aerosol challenged with 1 × 108 PFU of TrD, a virulent VEEV-IAB virus (1). Six macaques vaccinated with V/W/E and 6 mock-vaccinated macaques were also challenged with 1 × 108 PFU of aerosolized TrD. Fever responses in both vaccine groups were significantly lower in than the mock-vaccinated group (Table 6). Further, while 4 of 6 mock-vaccinated macaques were viremic, none of the VEEV-vaccinated and only 1 of the V/W/E-vaccinated macaques had detectable viremia after challenge. No difference was observed between the three groups in terms of lymphopenia.
TABLE 6.
VRP-induced protection and clinical observations in macaques challenged by aerosol with encephalitic alphaviruses
| Challenge virus and group | Survivala | MTDb | Viremiag | Feverf |
% change in lymphocyte countf | % change in granulocyte countf | ||
|---|---|---|---|---|---|---|---|---|
| TMaxc | Duration (h)d | Fever-hourse | ||||||
| VEEV-IAB | ||||||||
| VEEV | NAh | NA | 0/6 | 3.7 | 69.9* | 89.4* | −12.8 | NA |
| V/W/E | NA | NA | 1/6 | 4.0 | 58.3* | 90.8* | −13.9 | NA |
| Mock | NA | NA | 4/6 | 4.1 | 140.2 | 245.4 | −15.4 | NA |
| WEEV | ||||||||
| WEE | 5/6 | 6.0 | NDi | 38.7 | 24.3 | 29.1 | NA | 52.7 |
| V/W/E | 4/6 | 6.0 | ND | 39.2 | 57.6 | 95.9 | NA | 75.3 |
| Mock | 3/6 | 7.3 | ND | 39.3 | 64.8 | 109.7 | NA | 65.6 |
| EEEV | ||||||||
| EEE | 11/12 | 6 | ND | 3.8 | 40.9 | 71.1 | NA | 5.9* |
| V/W/E | 12/12 | >28 | ND | 3.3* | 37.4 | 46.0* | NA | 6.3 |
| Mock | 6/12 | 6 | ND | 4.6 | 54.7 | 114.9 | NA | 11.1 |
Number of surviving animals/number of animals in group.
MTD, mean time to death in days.
TMax, maximum temperature deviation from predicted.
Number of hours of significant temperature elevation.
Sum of significant temperature elevations.
Values are the mean for the group. *, significantly different from controls (P < 0.05) as determined by one-way analysis of variance.
Number of animals with viremia/number of animals in group.
NA, not applicable.
ND, not determined.
On day 60 after the initial vaccination, 6 macaques vaccinated with EEEV were aerosol challenged with 1 × 108 PFU of EEEV. Six macaques vaccinated with V/W/E and 6 mock-vaccinated macaques were also challenged with 1 × 108 PFU of aerosolized EEEV. In the initial experiment, only 2 of the 6 mock-vaccinated controls succumbed to infection; therefore, the experiment was repeated with an additional 6 macaques per group. The results are shown in Table 6. Six of 12 (50%) of the mock-vaccinated macaques succumbed to infection while only 1 of 12 EEEV-vaccinated macaques and none of the V/W/E-vaccinated macaques succumbed to infection. Fever responses were milder in vaccinated macaques. It was previously noted that an increase in granulocyte counts predicted outcome in naive macaques; the data here support that finding as vaccinated macaques had a smaller increase in granulocyte counts than observed in the mock-vaccinated group.
For the WEEV challenge in macaques, the challenge was delayed because of issues in developing the challenge stock of WEEV. On day 109 after the initial vaccination, six macaques vaccinated with WEEV were aerosol challenged with 1 × 108 PFU of WEEV. Six macaques vaccinated with V/W/E and six mock-vaccinated macaques were also challenged with 1 × 108 PFU of aerosolized WEEV. Three of six mock-vaccinated macaques succumbed to challenge while one of six WEEV-vaccinated and two of six V/W/E-vaccinated macaques also succumbed (Table 6). Fever responses in the V/W/E group were only slightly less than those of the mock-vaccinated group while the granulocyte increase was actually higher. Macaques given the WEEV vaccine alone had a lower fever response and smaller granulocyte increase.
DISCUSSION
The primary objective of the studies reported here was to evaluate whether alphavirus-based replicons could serve as vaccines against the encephalitic alphaviruses providing strong durable immunity that could protect against s.c. or aerosol challenge with virulent viruses. As shown in the experiments reported here, these vaccines generated strong, durable immune responses in mice against VEEV, WEEV, and EEEV as measured by both ELISA and neutralizing antibody assays and provided good protection out to 1 year postvaccination. In cynomolgus macaques, the VRP also induced strong neutralizing antibody responses against VEEV and EEEV while the response to WEEV was not as strong. In subsequent evaluation against aerosol challenge, the macaque studies demonstrated good protection against VEEV and EEEV. The protection against WEEV afforded by either WEEV VRP or the combination vaccine was not significantly different from that of mock-vaccinated controls although it was suggestive of protection.
A secondary objective was to evaluate whether these three vaccines could be given simultaneously and whether coadministration would interfere with the resulting immunogenicity and protection conferred against one or all of the vaccines. In a prior study it was shown that human volunteers vaccinated with a live attenuated chikungunya virus (CHIKV) did not respond to a live attenuated VEEV vaccine, and conversely humans vaccinated against VEEV did not respond to the CHIKV vaccine (21). It was speculated that the interference was a result of cross-reactivity between CHIKV and VEEV which prevented development of neutralizing antibody against the vaccine given second. Similarly, prior administration of a VEEV vaccine has been shown to suppress antibody responses to formalin-inactivated WEEV and EEEV vaccines in humans and equines (23, 24). A more recent report found that inactivated WEEV and EEEV vaccines can interfere with one another when administered simultaneously to people (22). In the murine studies reported here, interference between the VEEV, WEEV, and EEEV VRP did not occur, as measured by either antibody responses or the protection afforded against challenge even in the duration studies.
In macaques, antibody responses were lower in the combination V/W/E vaccine to VEEV-IC, VEEV-ID, and VEEV-IE than in the macaques vaccinated with VEEV alone, but the difference in titers was only significant for VEEV-IE. This would suggest that interference caused by the EEEV and WEEV vaccines may have reduced the response to VEEV-IE in the combination vaccine. It is not clear whether this interference would impact protection; in a prior study with a live attenuated VEEV vaccine, no neutralizing antibody to VEEV-IE was generated, yet macaques were protected against VEEV-IE challenge (15). It is possible that this is a result of the furin cleavage deletion, which can alter immunogenicity of the surface GPs, but this requires further investigation. The failure of the WEEV VRP in the NHP model to provide significant protection was not a result of interference as the antibody responses and protection afforded were not significantly different between groups given the WEEV VRP individually or in combination with EEEV and VEEV. Neutralizing antibody responses to WEEV were weak overall in both vaccine groups, with only one NHP achieving a PRNT80 higher than 160 (data not shown). The data suggest that further study is needed to improve responses to WEEV in NHP.
Neutralizing antibody has long been considered a correlate of protection for many viral vaccines, including the encephalitic alphaviruses (1). The experiments reported here, in agreement with other prior reports, demonstrated robust antibody responses in mice against all three VRP, whether given individually or in combination. In nonhuman primates, responses were generally stronger against VEEV-IAB than the other viruses, with the response to WEEV being the weakest, and only four of six macaques vaccinated with the WEEV VRP alone were seropositive on day 56. Neutralizing antibody titers failed to correlate with protection against EEEV in macaques vaccinated with Sindbis (SIN)/EEE virus (18). As previously mentioned, a live attenuated VEEV-IAB virus failed to generate neutralizing antibody against VEEV-IE in NHP while still protecting against aerosol challenge against VEEV-IE (15). For WEEV and EEEV, we also failed to see a correlation between PRNT80 and protection in macaques although this could be a reflection of weaker antibody responses against WEEV and EEEV than against VEEV. Schmaljohn et al. reported in 1982 that VEEV can induce nonneutralizing but cross-protective antibody responses (50). It is worth noting that neutralization assays are done in vitro and may not correspond with in vivo function. Though it is no longer a requirement for laboratory access, previous reports indicate postvaccination clearance titers of ≥1:20 for VEEV and ≥1:40 for EEEV and WEEV (51). A better understanding of the immunological mechanisms involved in protection against encephalitic alphaviruses, particularly in nonhuman primates, is necessary.
An additional objective with the protection against VEEV was the ability to protect against other epizootic (VEEV-IC) and enzootic (VEEV-ID, VEEV-IE, and VEEV-IIIA) subtypes as the current investigational new drug (IND) vaccines do not protect well against aerosol exposure to these subtypes. In the mice, the VEEV VRP and combined V/W/E VRP stimulated neutralizing antibody against both VEEV-IE and VEEV-IIIA subtypes and protected against subsequent aerosol challenge. In macaques, the VEEV VRP elicited neutralizing antibodies against all four subtypes tested in all six macaques. The combination V/W/E VRP elicited neutralizing antibodies against the VEEV-IC, VEEV-ID, and VEEV-IE subtypes although not consistently in every macaque. The ability of the VEEV VRP to stimulate neutralizing antibodies across all subtypes in macaques was somewhat surprising as this has not been seen with the live attenuated TC-83 or V3526 vaccines in macaques, particularly against the VEEV-ID (D. S. Reed, unpublished observations) and VEEV-IE (15) subtypes. Considering that the IND vaccines given to at-risk personnel do not protect well against these subtypes (3, 4; P. T. Franck, presented at the Workshop-Symposium on Venezuelan Equine Encephalitis Virus, Washington, DC, 14 to 17 September 1971), the VEEV VRP warrants further investigation as a pan-VEEV vaccine.
It should be noted that a number of other vaccine approaches against alphaviruses have been reported in recent years. A live, attenuated VEEV was shown to generate neutralizing antibody responses in mice and macaques while offering good protection against epizootic and enzootic VEEV subtypes (15, 16, 43, 52). Chimeric VEEV and EEEV vaccines have been generated using a Sindbis (SIN) virus vector and have been shown to be safe and immunogenic in mice and to protect mice against VEEV and EEEV challenge (19, 20, 53). The SIN/EEE vaccine was the first to demonstrate good protection in macaques against aerosol challenge with EEEV (18). The potential for reversion makes the hurdle of safety much more difficult to achieve with approaches using live attenuated vaccines, particularly given public perception of adverse events associated with biological products and the associated risk/benefit of the product. A DNA vaccine has shown promise against aerosol challenge with VEEV in macaques although neutralizing antibody responses were low (13). In a number of systems, replicon-based vaccines have been shown to induce stronger immune responses than DNA or subunit approaches but are safer than approaches using live attenuated vaccines due to the limited replication that can occur in vivo.
This is the first report to demonstrate that combined VRP against all three encephalitic alphaviruses could offer good protection against all three viruses by either s.c. or aerosol challenge in both mice and macaques. The studies further indicate that interference between these vaccines is not a concern as there was no difference in antibody responses or protection afforded between the combination vaccine and the vaccines given individually. Similar results have been demonstrated in animals vaccinated with VRP expressing multiple smallpox virus antigens; immune responses to individual antigens were not significantly different in animals receiving a combination of VRP from those receiving a single VRP vaccination (54). The WEEV VRP stimulated weak neutralizing antibody responses in both mice and macaques relative to the other VRP although the protection in mice was good. In macaques, the WEEV VRP vaccine did not provide statistically significant protection although the response was suggestive of protection. These data suggest that further study is needed to identify the immunological mechanisms responsible for protection and improve the response against WEEV but that the VRP approach overall is safe and immunogenic and provides good protection against challenge with encephalitic alphaviruses.
ACKNOWLEDGMENTS
The views, opinions, and/or findings contained herein are those of the authors and should not be construed as an official Department of Army position, policy, or decision unless so designated by other documentation.
We thank the technicians in the Center for Aerobiological Sciences for their assistance in the aerosol exposures and collection of telemetry data for these studies.
The National Institutes of Health (grant U01 A|056438-04) and Department of Defense (grant H.H.0003_07_RD_B) funded this work.
Footnotes
Published ahead of print 13 August 2014
REFERENCES
- 1. Steele KE, Reed DS, Glass PJ, Hart MK, Ludwig GV, Pratt WD, Parker MD, Smith JF. 2007. Alphavirus encephalitides, p 241–270 In Dembek ZF. (ed), Medical aspects of biological warfare. Borden Institute, Washington, DC [Google Scholar]
- 2. Pittman PR, Makuch RS, Mangiafico JA, Cannon TL, Gibbs PH, Peters CJ. 1996. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine 14:337–343 [DOI] [PubMed] [Google Scholar]
- 3. Dietz WH, Jr., Peralta PH, Johnson KM. 1979. Ten clinical cases of human infection with Venezuelan equine encephalomyelitis virus, subtype I-D. Am. J. Trop. Med. Hyg. 28:329–334 [DOI] [PubMed] [Google Scholar]
- 4. De Mucha-Macias J, Sanchez-Spindola I. 1965. Two human cases of laboratory infection with Mucambo virus. Am. J. Trop. Med. Hyg. 14:475–478 [PubMed] [Google Scholar]
- 5. White A, Berman S, Lowenthal JP. 1971. Inactivated eastern equine encephalomyelitis vaccines prepared in monolayer and concentrated suspension chick embryo cultures. Appl. Microbiol. 22:909–913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Robinson DM, Berman S, Lowenthal JP. 1972. Mouse potency assay for Western equine encephalomyelitis vaccines. Appl. Microbiol. 23:104–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bartelloni PJ, McKinney RW, Calia FM, Ramsburg HH, Cole FE., Jr. 1971. Inactivated western equine encephalomyelitis vaccine propagated in chick embryo cell culture. Clinical and serological evaluation in man. Am. J. Trop. Med. Hyg. 20:146–149 [DOI] [PubMed] [Google Scholar]
- 8. Hodgson LA, Ludwig GV, Smith JF. 1999. Expression, processing, and immunogenicity of the structural proteins of Venezuelan equine encephalitis virus from recombinant baculovirus vectors. Vaccine 17:1151–1160 [DOI] [PubMed] [Google Scholar]
- 9. Das D, Nagata LP, Suresh MR. 2007. Immunological evaluation of Escherichia coli expressed E2 protein of Western equine encephalitis virus. Virus Res. 128:26–33. 10.1016/j.virusres.2007.03.030 [DOI] [PubMed] [Google Scholar]
- 10. Das D, Gares SL, Nagata LP, Suresh MR. 2004. Evaluation of a Western equine encephalitis recombinant E1 protein for protective immunity and diagnostics. Antiviral Res. 64:85–92. 10.1016/j.antiviral.2004.06.008 [DOI] [PubMed] [Google Scholar]
- 11. Toth AM, Geisler C, Aumiller JJ, Jarvis DL. 2011. Factors affecting recombinant Western equine encephalitis virus glycoprotein production in the baculovirus system. Protein Expr. Purif. 80:274–282. 10.1016/j.pep.2011.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dupuy LC, Richards MJ, Ellefsen B, Chau L, Luxembourg A, Hannaman D, Livingston BD, Schmaljohn CS. 2011. A DNA vaccine for Venezuelan equine encephalitis virus delivered by intramuscular electroporation elicits high levels of neutralizing antibodies in multiple animal models and provides protective immunity to mice and nonhuman primates. Clin. Vaccine Immunol. 18:707–716. 10.1128/CVI.00030-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dupuy LC, Richards MJ, Reed DS, Schmaljohn CS. 2010. Immunogenicity and protective efficacy of a DNA vaccine against Venezuelan equine encephalitis virus aerosol challenge in nonhuman primates. Vaccine 28:7345–7350. 10.1016/j.vaccine.2010.09.005 [DOI] [PubMed] [Google Scholar]
- 14. Dupuy LC, Locher CP, Paidhungat M, Richards MJ, Lind CM, Bakken R, Parker MD, Whalen RG, Schmaljohn CS. 2009. Directed molecular evolution improves the immunogenicity and protective efficacy of a Venezuelan equine encephalitis virus DNA vaccine. Vaccine 27:4152–4160. 10.1016/j.vaccine.2009.04.049 [DOI] [PubMed] [Google Scholar]
- 15. Reed DS, Lind CM, Lackemeyer MG, Sullivan LJ, Pratt WD, Parker MD. 2005. Genetically engineered, live, attenuated vaccines protect nonhuman primates against aerosol challenge with a virulent IE strain of Venezuelan equine encephalitis virus. Vaccine 23:3139–3147. 10.1016/j.vaccine.2004.12.023 [DOI] [PubMed] [Google Scholar]
- 16. Pratt WD, Davis NL, Johnston RE, Smith JF. 2003. Genetically engineered, live attenuated vaccines for Venezuelan equine encephalitis: testing in animal models. Vaccine 21:3854–3862. 10.1016/S0264-410X(03)00328-1 [DOI] [PubMed] [Google Scholar]
- 17. Martin SS, Bakken RR, Lind CM, Reed DS, Price JL, Koeller CA, Parker MD, Hart MK, Fine DL. 2009. Telemetric analysis to detect febrile responses in mice following vaccination with a live-attenuated virus vaccine. Vaccine 27:6814–6823. 10.1016/j.vaccine.2009.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Roy CJ, Adams AP, Wang E, Leal G, Seymour RL, Sivasubramani SK, Mega W, Frolov I, Didier PJ, Weaver SC. 2013. A chimeric Sindbis-based vaccine protects cynomolgus macaques against a lethal aerosol challenge of eastern equine encephalitis virus. Vaccine 31:1464–1470. 10.1016/j.vaccine.2013.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paessler S, Ni H, Petrakova O, Fayzulin RZ, Yun N, Anishchenko M, Weaver SC, Frolov I. 2006. Replication and clearance of Venezuelan equine encephalitis virus from the brains of animals vaccinated with chimeric SIN/VEE viruses. J. Virol. 80:2784–2796. 10.1128/JVI.80.6.2784-2796.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Paessler S, Fayzulin RZ, Anishchenko M, Greene IP, Weaver SC, Frolov I. 2003. Recombinant Sindbis/Venezuelan equine encephalitis virus is highly attenuated and immunogenic. J. Virol. 77:9278–9286. 10.1128/JVI.77.17.9278-9286.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McClain DJ, Pittman PR, Ramsburg HH, Nelson GO, Rossi CA, Mangiafico JA, Schmaljohn AL, Malinoski FJ. 1998. Immunologic interference from sequential administration of live attenuated alphavirus vaccines. J. Infect. Dis. 177:634–641. 10.1086/514240 [DOI] [PubMed] [Google Scholar]
- 22. Reisler RB, Gibbs PH, Danner DK, Boudreau EF. 2012. Immune interference in the setting of same-day administration of two similar inactivated alphavirus vaccines: eastern equine and western equine encephalitis. Vaccine 30:7271–7277. 10.1016/j.vaccine.2012.09.049 [DOI] [PubMed] [Google Scholar]
- 23. Pittman PR, Liu CT, Cannon TL, Mangiafico JA, Gibbs PH. 2009. Immune interference after sequential alphavirus vaccine vaccinations. Vaccine 27:4879–4882. 10.1016/j.vaccine.2009.02.090 [DOI] [PubMed] [Google Scholar]
- 24. Calisher CH, Sasso DR, Sather GE. 1973. Possible evidence for interference with Venezuelan equine encephalitis virus vaccination of equines by pre-existing antibody to eastern or western equine encephalitis virus, or both. Appl. Microbiol. 26:485–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pushko P, Parker M, Ludwig GV, Davis NL, Johnston RE, Smith JF. 1997. Replicon-helper systems from attenuated Venezuelan equine encephalitis virus: expression of heterologous genes in vitro and immunization against heterologous pathogens in vivo. Virology 239:389–401. 10.1006/viro.1997.8878 [DOI] [PubMed] [Google Scholar]
- 26. Rayner JO, Dryga SA, Kamrud KI. 2002. Alphavirus vectors and vaccination. Rev. Med. Virol. 12:279–296. 10.1002/rmv.360 [DOI] [PubMed] [Google Scholar]
- 27. Kamrud KI, Custer M, Dudek JM, Owens G, Alterson KD, Lee JS, Groebner JL, Smith JF. 2007. Alphavirus replicon approach to promoterless analysis of IRES elements. Virology 360:376–387. 10.1016/j.virol.2006.10.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hubby B, Talarico T, Maughan M, Reap EA, Berglund P, Kamrud KI, Copp L, Lewis W, Cecil C, Norberg P, Wagner J, Watson A, Negri S, Burnett BK, Graham A, Smith JF, Chulay JD. 2007. Development and preclinical evaluation of an alphavirus replicon vaccine for influenza. Vaccine 25:8180–8189. 10.1016/j.vaccine.2007.09.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Herbert AS, Kuehne AI, Barth JF, Ortiz RA, Nichols DK, Zak SE, Stonier SW, Muhammad MA, Bakken RR, Prugar LI, Olinger GG, Groebner JL, Lee JS, Pratt WD, Custer M, Kamrud KI, Smith JF, Hart MK, Dye JM. 2013. Venezuelan equine encephalitis virus replicon particle vaccine protects nonhuman primates from intramuscular and aerosol challenge with Ebolavirus. J. Virol. 87:4952–4964. 10.1128/JVI.03361-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Heise MT, Whitmore A, Thompson J, Parsons M, Grobbelaar AA, Kemp A, Paweska JT, Madric K, White LJ, Swanepoel R, Burt FJ. 2009. An alphavirus replicon-derived candidate vaccine against Rift Valley fever virus. Epidemiol. Infect. 137:1309–1318. 10.1017/S0950268808001696 [DOI] [PubMed] [Google Scholar]
- 31. Lee JS, Groebner JL, Hadjipanayis AG, Negley DL, Schmaljohn AL, Welkos SL, Smith LA, Smith JF. 2006. Multiagent vaccines vectored by Venezuelan equine encephalitis virus replicon elicits immune responses to Marburg virus and protection against anthrax and botulinum neurotoxin in mice. Vaccine 24:6886–6892. 10.1016/j.vaccine.2006.06.004 [DOI] [PubMed] [Google Scholar]
- 32. Olinger GG, Bailey MA, Dye JM, Bakken R, Kuehne A, Kondig J, Wilson J, Hogan RJ, Hart MK. 2005. Protective cytotoxic T-cell responses induced by Venezuelan equine encephalitis virus replicons expressing Ebola virus proteins. J. Virol. 79:14189–14196. 10.1128/JVI.79.22.14189-14196.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee JS, Hadjipanayis AG, Welkos SL. 2003. Venezuelan equine encephalitis virus-vectored vaccines protect mice against anthrax spore challenge. Infect. Immun. 71:1491–1496. 10.1128/IAI.71.3.1491-1496.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hevey M, Negley D, Pushko P, Smith J, Schmaljohn A. 1998. Marburg virus vaccines based upon alphavirus replicons protect guinea pigs and nonhuman primates. Virology 251:28–37. 10.1006/viro.1998.9367 [DOI] [PubMed] [Google Scholar]
- 35. Kubes V. 1944. Venezuelan-type equine encephalomyelitis virus in Trinidad. Science 99:41–42. 10.1126/science.99.2559.41 [DOI] [PubMed] [Google Scholar]
- 36. Cole FE, Jr., May SW, Robinson DM. 1973. Formalin-inactivated Venezuelan equine encephalomyelitis (Trinidad strain) vaccine produced in rolling-bottle cultures of chicken embryo cells. Appl. Microbiol. 25:262–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wang E, Bowen RA, Medina G, Powers AM, Kang W, Chandler LM, Shope RE, Weaver SC. 2001. Virulence and viremia characteristics of 1992 epizootic subtype IC Venezuelan equine encephalitis viruses and closely related enzootic subtype ID strains. Am. J. Trop. Med. Hyg. 65:64–69 [DOI] [PubMed] [Google Scholar]
- 38. Kinney RM, Tsuchiya KR, Sneider JM, Trent DW. 1992. Genetic evidence that epizootic Venezuelan equine encephalitis (VEE) viruses may have evolved from enzootic VEE subtype I-D virus. Virology 191:569–580. 10.1016/0042-6822(92)90232-E [DOI] [PubMed] [Google Scholar]
- 39. Scherer WF, Dickerman RW, Ordonez JV. 1970. Discovery and geographic distribution of Venezuelan encephalitis virus in Guatemala, Honduras, and British Honduras during 1965–68, and its possible movement to Central America and Mexico. Am. J. Trop. Med. Hyg. 19:703–711 [DOI] [PubMed] [Google Scholar]
- 40. Bianchi TI, Aviles G, Monath TP, Sabattini MS. 1993. Western equine encephalomyelitis: virulence markers and their epidemiologic significance. Am. J. Trop. Med. Hyg. 49:322–328 [DOI] [PubMed] [Google Scholar]
- 41. Mitchell CJ, Niebylski ML, Smith GC, Karabatsos N, Martin D, Mutebi JP, Craig GB, Jr., Mahler MJ. 1992. Isolation of eastern equine encephalitis virus from Aedes albopictus in Florida. Science 257:526–527. 10.1126/science.1321985 [DOI] [PubMed] [Google Scholar]
- 42. Davis NL, Willis LV, Smith JF, Johnston RE. 1989. In vitro synthesis of infectious Venezuelan equine encephalitis virus RNA from a cDNA clone: analysis of a viable deletion mutant. Virology 171:189–204. 10.1016/0042-6822(89)90526-6 [DOI] [PubMed] [Google Scholar]
- 43. Hart MK, Lind C, Bakken R, Robertson M, Tammariello R, Ludwig GV. 2001. Onset and duration of protective immunity to IA/B and IE strains of Venezuelan equine encephalitis virus in vaccinated mice. Vaccine 20:616–622. 10.1016/S0264-410X(01)00337-1 [DOI] [PubMed] [Google Scholar]
- 44. Reed DS, Larsen T, Sullivan LJ, Lind CM, Lackemeyer MG, Pratt WD, Parker MD. 2005. Aerosol exposure to western equine encephalitis virus causes fever and encephalitis in cynomolgus macaques. J. Infect. Dis. 192:1173–1182. 10.1086/444397 [DOI] [PubMed] [Google Scholar]
- 45. Reed DS, Lackemeyer MG, Garza NL, Norris S, Gamble S, Sullivan LJ, Lind CM, Raymond JL. 2007. Severe encephalitis in cynomolgus macaques exposed to aerosolized eastern equine encephalitis virus. J. Infect. Dis. 196:441–450. 10.1086/519391 [DOI] [PubMed] [Google Scholar]
- 46. Reed DS, Lackemeyer MG, Garza NL, Sullivan LJ, Nichols DK. 2011. Aerosol exposure to Zaire Ebolavirus in three nonhuman primate species: differences in disease course and clinical pathology. Microbes Infect. 13:930–936. 10.1016/j.micinf.2011.05.002 [DOI] [PubMed] [Google Scholar]
- 47. Reed DS, Lind CM, Sullivan LJ, Pratt WD, Parker MD. 2004. Aerosol infection of cynomolgus macaques with enzootic strains of Venezuelan equine encephalitis viruses. J. Infect. Dis. 189:1013–1017. 10.1086/382281 [DOI] [PubMed] [Google Scholar]
- 48. Pratt WD, Gibbs P, Pitt ML, Schmaljohn AL. 1998. Use of telemetry to assess vaccine-induced protection against parenteral and aerosol infections of Venezuelan equine encephalitis virus in non-human primates. Vaccine 16:1056–1064 [DOI] [PubMed] [Google Scholar]
- 49. Jahrling PB, Stephenson EH. 1984. Protective efficacies of live attenuated and formaldehyde-inactivated Venezuelan equine encephalitis virus vaccines against aerosol challenge in hamsters. J. Clin. Microbiol. 19:429–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Schmaljohn AL, Johnson ED, Dalrymple JM, Cole GA. 1982. Non-neutralizing monoclonal antibodies can prevent lethal alphavirus encephalitis. Nature 297:70–72. 10.1038/297070a0 [DOI] [PubMed] [Google Scholar]
- 51. Rusnak JM, Kortepeter MG, Aldis J, Boudreau E. 2004. Experience in the medical management of potential laboratory exposures to agents of bioterrorism on the basis of risk assessment at the United States Army Medical Research Institute of Infectious Diseases (USAMRIID). J. Occup. Environ. Med. 46:801–811. 10.1097/01.jom.0000135539.99691.4e [DOI] [PubMed] [Google Scholar]
- 52. Hart MK, Caswell-Stephan K, Bakken R, Tammariello R, Pratt W, Davis N, Johnston RE, Smith J, Steele K. 2000. Improved mucosal protection against Venezuelan equine encephalitis virus is induced by the molecularly defined, live-attenuated V3526 vaccine candidate. Vaccine 18:3067–3075. 10.1016/S0264-410X(00)00042-6 [DOI] [PubMed] [Google Scholar]
- 53. Wang E, Petrakova O, Adams AP, Aguilar PV, Kang W, Paessler S, Volk SM, Frolov I, Weaver SC. 2007. Chimeric Sindbis/eastern equine encephalitis vaccine candidates are highly attenuated and immunogenic in mice. Vaccine 25:7573–7581. 10.1016/j.vaccine.2007.07.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hooper JW, Thompson E, Wilhelmsen C, Zimmerman M, Ichou MA, Steffen SE, Schmaljohn CS, Schmaljohn AL, Jahrling PB. 2004. Smallpox DNA vaccine protects nonhuman primates against lethal monkeypox. J. Virol. 78:4433–4443. 10.1128/JVI.78.9.4433-4443.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]


