Abstract
Machupo virus (MACV) is the etiologic agent of Bolivian hemorrhagic fever (BHF). Utilizing a reverse-genetics system recently developed, we report the rescue of a rationally modified recombinant MACV containing a single mutation in the transmembrane region of the glycoprotein. Following challenge of susceptible mice, we identified a significant reduction in virulence in the novel virus. We also identified an instability leading to reversion of the single mutation to a wild-type genotype.
TEXT
The etiologic agent of Bolivian hemorrhagic fever (BHF), Machupo virus (MACV), is classified as a Tier 1 Select Agent by the Centers for Disease Control and Prevention (CDC), requiring a biosafety level 4 (BSL4) laboratory environment (1). First identified during an outbreak in the Beni district of Bolivia, MACV has a reported case mortality rate of 25 to 35% (2–6). Since 2007, reports of MACV have increased dramatically, with a peak of over 200 human cases in 2008 (7). Exposure to the aerosolized excreta and secreta of the natural rodent reservoir Calomys callosus is predicted to be the primary route of exposure (3, 8, 9). However, nosocomial spread within family groups and at the hospital have been reported but are not believed to be the primary method of spread during an outbreak (10–12).
A member of the family Arenaviridae, MACV is a single-stranded, negative-sense RNA virus that utilizes an ambisense encoding strategy (2). The two segments, small (S [∼3.3 kb]) and large (L [∼7.2 kb]), encode four viral proteins (Fig. 1A). The S segment encodes the nucleoprotein (NP) and glycoprotein precursor (GPC), which is posttranslationally cleaved into GP1, GP2, and stable signal peptide (SSP). The L segment encodes the RNA-dependent RNA polymerase (L protein) and a RING finger matrix protein (Z) (13–18). The genes are separated by an intergenic region (IGR) serving as the transcription terminator and flanked by untranslated regions (UTR) at the 5′ and 3′ ends of each segment (2, 19, 20). The 19-nucleotide (nt) termini of each UTR are highly conserved across members of the Arenaviridae (21–23).
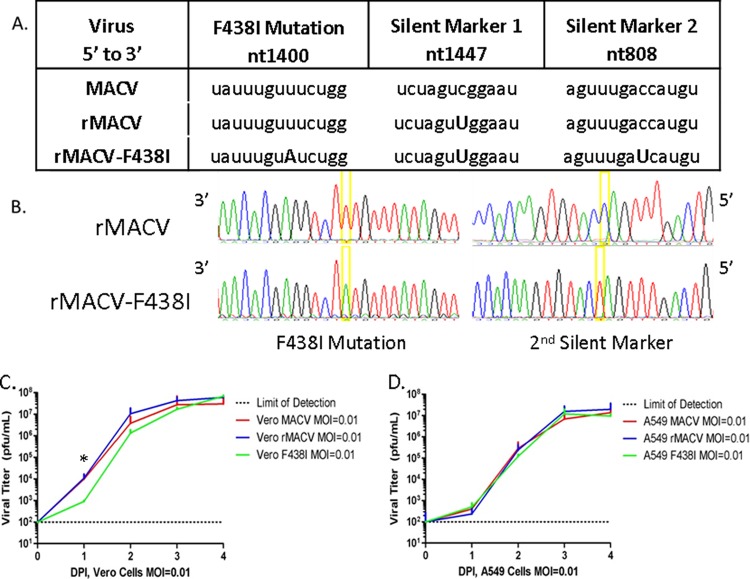
FIG 1.
Schematic representation of arenavirus genome and processed glycoprotein. (A) Schematic of the small and large segments of Machupo virus with each gene separated by the IGR. Each open reading frame (ORF) is preceded by an untranslated region, denoted by the bold squares, which plays a pivotal role in secondary structure and polymerase binding. (B) Sequence analysis of the glycoprotein membrane region of MACV, JUNV-Romero, and Candid#1. There is a single amino acid difference of an isoleucine versus a valine between MACV and JUNV-Romero/Candid#1 at amino acid residues 442 and 431, respectively. The box around the residues identifies phenylalanines that are identical in MACV and JUNV but different in Candid#1. Sequence analysis is based upon published online sequences (GenBank accession no. JN794584.1, AY619640, and AY746353.1). The schematic identifies the transmembrane region, which spans the region of GP2 within the cellular membrane.
Clinically, BHF development is similar to that of Argentine hemorrhagic fever (AHF), caused by Junin virus (JUNV) (24). The disease incubation period after exposure to MACV is 3 to 16 days (25). The prodromal phase lasts from 1 to 5 days, from which one-third of patients progress into the hemorrhagic/neurological phase (25–28). Recovering patients have an extended 1- to 3-month convalescence period, during which hair loss, dizziness, and fatigue are reported.
There are no licensed or approved treatments for MACV. Immune plasma and ribavirin have been utilized in a limited number of cases, but no trials have been completed (10, 11). Candid#1, the attenuated vaccine strain of JUNV, is licensed for use in the region of endemicity of Argentina (29–31). Recent reports have identified a single mutation in the glycoprotein transmembrane region, F427I, of Candid#1 as playing a key role in attenuating JUNV in a murine model (32, 33). This transmembrane region is highly conserved between MACV, JUNV, and Candid#1 (Fig. 1B) (32, 34, 35). Utilizing a reverse-genetics system our laboratory published previously, we generated a rationally designed recombinant MACV (rMACV) strain containing a single F438I mutation at the GPC transmembrane region (referred to as rMACV-F438I here) by introducing a U-to-A mutation at nucleotide (nt) 1400 in the S segment (36). The rational generation of rMACV-F438I builds upon the first-generation methodology of reassortment used to generate the Lassa virus (LASV) vaccine candidate ML29 (37–39). The following report describes the in vitro and in vivo characterization of rMACV-F438I. Additionally, we identified instability of the single mutation following in vivo challenge, leading to a reversion to the wild-type genotype.
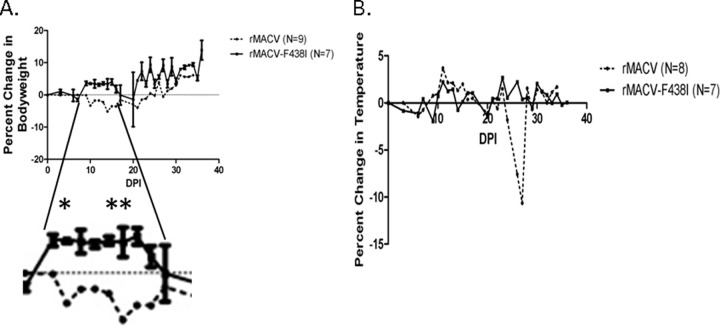
Following the rescue and single passage in Vero cells, the rMACV-F438I titer was 4 × 107 PFU/ml, comparable to those of MACV and rMACV (23, 36, 40). Sequencing of the stock virus confirmed the presence of the single mutation at nt 1400 along with two silent genetic markers at nt 808 and nt 1447 on the S segment: the first allows us to distinguish all recombinant viruses from MACV, and the second distinguishes rMACV-F438I from rMACV (Fig. 2A and B). To determine if the F438I mutation had an impact on viral growth in vitro, we infected interferon (IFN)-incompetent Vero cells and IFN-competent A549 cells at a multiplicity of infection (MOI) of 0.01. Tissue culture supernatant (TCS) was collected in triplicate at 0, 24, 48, 72, and 96 h postinfection. The growth curve of rMACV-F438I was similar to those of MACV and rMACV in both cell types (Fig. 2C and D).
FIG 2.
Rescue and in vitro analysis of rMACV-F438I. (A) The mutation to generate the F438I amino acid change was accomplished through target PCR mutagenesis by changing the adenosine to a uracil at nt 1400. The addition of a silent mutation at nt 1407 distinguishes all rMACVs from the wild-type virus. The addition of the second marker distinguishes rMACV-F438I from rMACV. Differences between sequences are denoted by a capital letter. (B) Chromatography sequence analysis of viral cDNA confirms the presence of the F438I mutation and both silent markers. (C) TCSs from cells infected at an MOI of 0.01 with MACV, rMACV, or rMACV-F438I in triplicate (n = 3) were plaque analyzed to calculate viral titers from 0 to 4 dpi. TCSs collected from IFN-incompetent Vero cells showed similar growth of all three viruses. By 3 dpi, all three viruses reached comparable viral peaks, which were maintained at 4 dpi. (D) TCS collected from IFN-competent A549 cells had no significant difference in viral titers between all three viruses (P > 0.05, two-way ANOVA, n = 3).
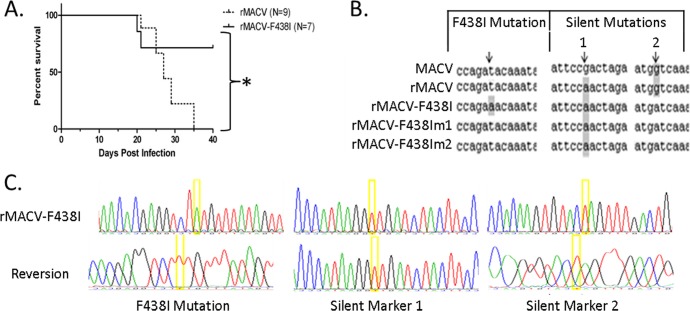
To examine the impact of the single mutation on the virulence of rMACV-F438I, we challenged IFN-αβ/γ receptor knockout (IFN-αβ/γ R−/−) mice with 10,000 PFU of rMACV (n = 9) or rMACV-F438I (n = 7) through intraperitoneal injection (36, 41). Changes in body temperature, weight, and disease development were monitored throughout the study. Animals challenged with rMACV followed a similar disease progression as described previously (36). A period of significant (P < 0.01, two-way analysis of variance [ANOVA]) weight loss at 10, 12, 14, and 15 days postinfection (dpi) was identified in rMACV-challenged animals compared to animals challenged with rMACV-F438I (Fig. 3A). Hypothermia was observed in animals 1 to 2 days prior to death (Fig. 3B).
FIG 3.
Change in weight and temperature of rMACV and rMACV-F438I-infected mice. (A) Daily collection of weight data from mice infected intraperitoneally with 10,000 PFU of MACV identified a significant difference in weight change during the period from 10 to 15 dpi between the rMACV-F438I- and the rMACV-challenged mice. The only period of significant weight loss identified in the rMACV-F438I-infected mice was 1 to 2 days prior to the two mice succumbing to disease. Asterisks denote significant differences at 9, 13, and 14 dpi (P < 0.05, two-way ANOVA). (B) Daily collection of temperature data from infected mice identified no development of febrile disease throughout the study in either group of mice. Hypothermia was commonly identified in rMACV-infected mice 1 to 2 days prior to death.
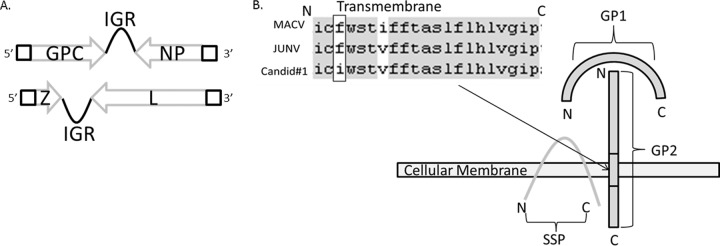
Starting at ∼20 dpi, neurological impairment and clinical disease were identified in all rMACV-infected mice. Interestingly, two of the seven animals challenged with rMACV-F438I developed disease symptoms, including scruffed fur and hunched postures at 19 and 20 dpi, which progressed to rear limb paralysis by 20 and 21 dpi, at which point both animals were euthanized following IACUC protocol requirements. The remaining five animals did not show any observable symptoms. All animals challenged with rMACV developed severe disease starting at 21 dpi and succumbed to disease or were euthanized with a mean time to death (MTD) at 27 dpi. Challenge with rMACV-F438I resulted in a significant reduction in mortality compared to that of rMACV-infected animals (P = 0.024, log rank test) (Fig. 4A), suggesting attenuation of this virus.
FIG 4.
Survival curves of rMACV- and rMACV-F438I-infected mice and sequencing identifying reversion of rMACV-F438I. (A) All mice challenged with rMACV succumbed to disease with an MTD of ∼27 dpi, while only 28% of animals challenged with rMACV-F438I succumbed to disease. Mice that succumbed following rMACV-F438I challenge had an MTD of 20.5 dpi. Asterisks denote a significant difference in survival between the two viruses (P < 0.05, Mantel Cox). (B) Graphical sequence analysis and comparison of cDNA generated from MACV, rMACV, and rMACV-F438I isolates. rMACV and MACV maintain the wild-type genotype at the nucleotide coding for F438. The nucleotide change coding for I438 is present in the stock of rMACV-F438I, while a reversion has occurred in the viral RNA isolated from mice 1 and 2. The presence of the second silent marker confirms that both animals were challenged with rMACV-F438I. (C) Chromatography analysis of sequenced viral cDNA confirming the reversion of the mutation in the consensus sequence and the presence of both silent markers.
To investigate if any mutation could account for the differential outcome observed in rMACV-F438I-infected mice, we purified viral RNA from the homogenate of the brains, lungs, kidneys, and spleens of the mice. Amplification of viral RNA into cDNA was accomplished utilizing primers designed previously (36). Whole-genome sequencing of viral RNA purified from the lung, kidney, and brain homogenates of both sick mice uniformly identified an A-to-U reverse mutation at nt 1400 of the S segment, resulting in a reversion to the wild-type GPC F438 genotype (Fig. 4B and C). As rMACV contains only one of the silent mutation markers, the presence of both silent genetic markers in these two rMACV-F438I isolates further excluded a possibility of cross-contamination with rMACV and confirmed that they were indeed the MACV-F438I revertants.
The similar growth curves of rMACV-F438I, rMACV, and MACV, as well as the similar stock virus titers between rescued rMACV-F438I and rMACV, indicated that the single mutation did not noticeably impact virus replication in cell culture. This result is comparable to the reports of rJUNV and rJUNV-F427I viral growth kinetics as reported previously but not that of LASV (33).
To identify if the single mutant virus is genetically stable in vitro, we serially passaged rMACV-F438I in Vero cells in duplicate. The serial passage was performed at an estimated MOI of 0.01 based on Fig. 2C. At each passage, virus was collected at 3 or 4 dpi followed by infection of fresh Vero cells for five passages. Viral RNAs were prepared from cellular lysate and supernatant and sequenced as described previously (36). Following partial GPC sequencing of all passaged viruses, we observed that the virus maintained the single mutation for the GPC I438 residue as well as both silent markers. No additional mutations were detected in the fifth passage of the virus following whole-genome sequencing, demonstrating the genetic stability of the rMACV-F438I virus in vitro.
Challenge of IFN-αβ/γ R−/− mice with rMACV resulted in a biphasic disease, clinical signs, and MTD similar to what our laboratory reported previously when characterizing the model (36). Of the seven animals challenged with rMACV-F438I, two developed severe disease and succumbed to disease. The other five had no identifiable disease throughout the study. The diverse outcomes from these animals are interesting, especially as the two animals had such a rapid decline in health. A significant difference in the mortality rates between rMACV- and rMACV-F438I-infected animals indicated that the single mutation in the GPC transmembrane region could lead to MACV attenuation, the same as JUNV.
Based on the sequence analysis of virus collected from the two animals that succumbed to rMACV-F438I challenge, the phenotypic reversion of rMACV-F438I to the virulent infection was determined by the genotypic reversion of the attenuating GPC mutation at amino acid 438 to the wild type. This reversion was confirmed in all organs examined from both lethally infected mice. The apparent instability of the single mutation in vivo leads us to presume that additional mutations are necessary for maintaining attenuation. Introduction of the single GPC F427I mutation in mouse-pathogenic XJ13 JUNV further reduced the virulence; however, no previous reports exist that describe a reversion to wild-type sequence. Taken together with the results from passaging of rMACV-F438I, the single mutant attenuated MACV-F438I strain is genetically stable in vitro but not in vivo, and hence, the single mutant strain is not sufficient in and of itself as a vaccine candidate.
In summary, in this article we have identified that a single mutation in the glycoprotein transmembrane region of MACV does not change its replication in vitro, while it significantly attenuates the virus in vivo. This is the first report of a rationally attenuated MACV and provides further evidence of the utility of the reverse-genetics system and mouse model our laboratory has developed to study MACV. The significant role that the F438I mutation plays in attenuating MACV and JUNV leads us to believe that further elucidation of its role will allow for future development of rationally designed vaccines against New World hemorrhagic arenaviruses.
Nucleotide sequence accession numbers.
The reference sequences for MACV S and L were submitted to GenBank under accession numbers KM198593 and KM198592.
ACKNOWLEDGMENTS
This work was performed in part to complete the dissertation requirements for Michael Patterson.
This work was partially supported by the Institute of Human Infections and Immunity at UTMB.
Footnotes
Published ahead of print 16 July 2014
REFERENCES
- 1.Department of Agriculture. 2012. Agricultural Bioterrorism Act of 2002. Biennial review and republication of the Select Agent and Toxin List; amendments to the Select Agent and Toxin Regulations; final rule. Fed. Regist. 77:61056–61081 http://www.gpo.gov/fdsys/pkg/FR-2012-10-05/pdf/2012-24434.pdf [Google Scholar]
- 2.Buchmeier M, de la Torre J, Peters C. 2007. Arenaviridae: the viruses and their replication, p 1791–1827 In Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, Roizman B, Straus SE. (ed), Fields virology, 5th ed. Lippincott Williams & Wilkins, Philadelphia, PA [Google Scholar]
- 3.Johnson KM. 1965. Epidemiology of Machupo virus infection. Am. J. Trop. Med. Hyg. 14:816–818 [DOI] [PubMed] [Google Scholar]
- 4.Johnson KM, Wiebenga NH, Mackenzie RB, Kuns ML, Tauraso NM, Shelokov A, Webb PA, Justines G, Beye HK. 1965. Virus isolations from human cases of hemorrhagic fever in Bolivia. Proc. Soc. Exp. Biol. Med. 118:113–118. 10.3181/00379727-118-29772 [DOI] [PubMed] [Google Scholar]
- 5.Webb PA, Johnson KM, Mackenzie RB, Kuns ML. 1967. Some characteristics of Machupo virus, causative agent of Bolivian hemorrhagic fever. Am. J. Trop. Med. Hyg. 16:531–538 [DOI] [PubMed] [Google Scholar]
- 6.Patterson M, Grant A, Paessler S. 2014. Epidemiology and pathogenesis of Bolivian hemorrhagic fever. Curr. Opin. Virol. 5:82–90. 10.1016/j.coviro.2014.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aguilar PV, Camargo W, Vargas J, Guevara C, Roca Y, Felices V, Laguna-Torres VA, Tesh R, Ksiazek TG, Kochel TJ. 2009. Reemergence of Bolivian hemorrhagic fever, 2007–2008. Emerg. Infect. Dis. 15:1526–1528. 10.3201/eid1509.090017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson KM, Kuns ML, Mackenzie RB, Webb PA, Yunker CE. 1966. Isolation of Machupo virus from wild rodent Calomys callosus. Am. J. Trop. Med. Hyg. 15:103–106 [DOI] [PubMed] [Google Scholar]
- 9.Fulhorst CF, Bowen MD, Ksiazek TG, Rollin PE, Nichol ST, Kosoy MY, Peters CJ. 1996. Isolation and characterization of Whitewater Arroyo virus, a novel North American arenavirus. Virology 224:114–120. 10.1006/viro.1996.0512 [DOI] [PubMed] [Google Scholar]
- 10.Stinebaugh BJ, Schloeder FX, Johnson KM, Mackenzie RB, Entwisle G, De Alba E. 1966. Bolivian hemorrhagic fever: a report of four cases. Am. J. Med. 40:217–230. 10.1016/0002-9343(66)90103-3 [DOI] [PubMed] [Google Scholar]
- 11.Kilgore PE, Ksiazek TG, Rollin PE, Mills JN, Villagra MR, Montenegro MJ, Costales MA, Paredes LC, Peters CJ. 1997. Treatment of Bolivian hemorrhagic fever with intravenous ribavirin. Clin. Infect. Dis. 24:718–722. 10.1093/clind/24.4.718 [DOI] [PubMed] [Google Scholar]
- 12.Peters CJ, Kuehne RW, Mercado RR, Le Bow RH, Spertzel RO, Webb PA. 1974. Hemorrhagic fever in Cochabamba, Bolivia, 1971. Am. J. Epidemiol. 99:425–433 [DOI] [PubMed] [Google Scholar]
- 13.Bradfute SB, Dye JM, Jr, Bavari S. 2011. Filovirus vaccines. Hum. Vaccin. 7:701–711. 10.4161/hv.7.6.15398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beyer WR, Pöpplau D, Garten W, von Laer D, Lenz O. 2003. Endoproteolytic processing of the lymphocytic choriomeningitis virus glycoprotein by the subtilase SKI-1/S1P. J. Virol. 77:2866–2872. 10.1128/JVI.77.5.2866-2872.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lenz O, ter Meulen J, Klenk H-D, Seidah NG, Garten W. 2001. The Lassa virus glycoprotein precursor GP-C is proteolytically processed by subtilase SKI-1/S1P. Proc. Natl. Acad. Sci. U. S. A. 98:12701–12705. 10.1073/pnas.221447598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.York J, Nunberg JH. 2007. A novel zinc-binding domain is essential for formation of the functional Junin virus envelope glycoprotein complex. J. Virol. 81:13385–13391. 10.1128/JVI.01785-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.York J, Romanowski V, Lu M, Nunberg JH. 2004. The signal peptide of the Junin arenavirus envelope glycoprotein is myristoylated and forms an essential subunit of the mature G1-G2 complex. J. Virol. 78:10783–10792. 10.1128/JVI.78.19.10783-10792.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.York J, Nunberg JH. 2007. Distinct requirements for signal peptidase processing and function in the stable signal peptide subunit of the Junin virus envelope glycoprotein. Virology 359:72–81. 10.1016/j.virol.2006.08.048 [DOI] [PubMed] [Google Scholar]
- 19.Tortorici MA, Albarino CG, Posik DM, Ghiringhelli PD, Lozano ME, Rivera Pomar R, Romanowski V. 2001. Arenavirus nucleocapsid protein displays a transcriptional antitermination activity in vivo. Virus Res. 73:41–55. 10.1016/S0168-1702(00)00222-7 [DOI] [PubMed] [Google Scholar]
- 20.Meyer BJ, Southern PJ. 1994. Sequence heterogeneity in the termini of lymphocytic choriomeningitis virus genomic and antigenomic RNAs. J. Virol. 68:7659–7664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Auperin DD, McCormick JB. 1989. Nucleotide sequence of the Lassa virus (Josiah strain) S genome RNA and amino acid sequence comparison of the N and GPC proteins to other arenaviruses. Virology 168:421–425. 10.1016/0042-6822(89)90287-0 [DOI] [PubMed] [Google Scholar]
- 22.Auperin DD, Compans RW, Bishop DHL. 1982. Nucleotide sequence conservation at the 3′ termini of the virion RNA species of new World and Old World arenaviruses. Virology 121:200–203. 10.1016/0042-6822(82)90130-1 [DOI] [PubMed] [Google Scholar]
- 23.Emonet SF, Seregin AV, Yun NE, Poussard AL, Walker AG, de la Torre JC, Paessler S. 2011. Rescue from cloned cDNAs and in vivo characterization of recombinant pathogenic Romero and live-attenuated Candid #1 strains of Junin virus, the causative agent of Argentine hemorrhagic fever dis. J. Virol. 85:1473–1483. 10.1128/JVI.02102-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charrel RN, Lamballerie XD. 2003. Arenaviruses other than Lassa virus. Antiviral Res. 57:89–100. 10.1016/S0166-3542(02)00202-4 [DOI] [PubMed] [Google Scholar]
- 25.American Academy of Pediatrics. 2009. Hemorrhagic fevers caused by Arenaviruses, p 325–334 In Pickering LK. (ed), Red book: report of the Committee on Infectious Diseases, 28th ed. American Academy of Pediatrics, Elk Grove Village, IL [Google Scholar]
- 26.Child PL, MacKenzie RB, Valverde LR, Johnson KM. 1967. Bolivian hemorrhagic fever. A pathologic description. Arch. Pathol. 83:434–445 [PubMed] [Google Scholar]
- 27.Kuns ML. 1965. Epidemiology of Machupo virus infection. Am. J. Trop. Med. Hyg. 14:813–816 [DOI] [PubMed] [Google Scholar]
- 28.Acha P, Szyfres B. 2003. Machupo hemorrhagic fever, p 200–205 In Zoonoses and communicable diseases common to man and animals, 3rd ed, vol 2 Pan American Health Organization, Washington, DC [Google Scholar]
- 29.Maiztegui JI, McKee KT, Jr, Barrera Oro JG, Harrison LH, Gibbs PH, Feuillade MR, Enria DA, Briggiler AM, Levis SC, Ambrosio AM, Halsey NA, Peters CJ. 1998. Protective efficacy of a live attenuated vaccine against Argentine hemorrhagic fever. AHF Study Group. J. Infect. Dis. 177:277–283. 10.1086/514211 [DOI] [PubMed] [Google Scholar]
- 30.Ambrosio AM, Riera LM, Saavedra Mdel C, Sottosanti MJ. 2005. Preclinical assay of Candid #1 vaccine against Argentine hemorrhagic fever made in Argentina. Medicina (B. Aires) 65:329–332 (In Spanish.) [PubMed] [Google Scholar]
- 31.Contigiani M, Medeot S, Diaz G. 1993. Heterogeneity and stability characteristics of Candid 1 attenuated strain of Junin virus. Acta Virol. 37:41–46 [PubMed] [Google Scholar]
- 32.Droniou-Bonzom ME, Reignier T, Oldenburg JE, Cox AU, Exline CM, Rathbun JY, Cannon PM. 2011. Substitutions in the glycoprotein (GP) of the Candid#1 vaccine strain of Junin virus increase dependence on human transferrin receptor 1 for entry and destabilize the metastable conformation of GP. J. Virol. 85:13457–13462. 10.1128/JVI.05616-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Albariño CG, Bird BH, Chakrabarti AK, Dodd KA, Flint M, Bergeron É, White DM, Nichol ST. 2011. The major determinant of attenuation in mice of the Candid1 vaccine for Argentine hemorrhagic fever is located in the G2 glycoprotein transmembrane domain. J. Virol. 85:10404–10408. 10.1128/JVI.00856-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.York J, Agnihothram SS, Romanowski V, Nunberg JH. 2005. Genetic analysis of heptad-repeat regions in the G2 fusion subunit of the Junin arenavirus envelope glycoprotein. Virology 343:267–274. 10.1016/j.virol.2005.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agnihothram SS, York J, Trahey M, Nunberg JH. 2007. Bitopic membrane topology of the stable signal peptide in the tripartite Junin virus GP-C envelope glycoprotein complex. J. Virol. 81:4331–4337. 10.1128/JVI.02779-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patterson M, Seregin A, Huang C, Kolokoltsova O, Smith J, Miller M, Yun N, Poussard A, Grant A, Tigabu B, Walker A, Paessler S. 2014. Rescue of a recombinant Machupo virus from cloned cDNAs and in vivo characterization in interferon (αβ/γ) receptor double knockout mice. J. Virol. 88:1914–1923. 10.1128/JVI.02925-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lukashevich IS, Patterson J, Carrion R, Moshkoff D, Ticer A, Zapata J, Brasky K, Geiger R, Hubbard GB, Bryant J, Salvato MS. 2005. A live attenuated vaccine for Lassa fever made by reassortment of Lassa and Mopeia viruses. J. Virol. 79:13934–13942. 10.1128/JVI.79.22.13934-13942.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lukashevich IS, Vasiuchkov AD, Stel'makh TA, Scheslenok EP, Shabanov AG. 1991. The isolation and characteristics of reassortants between the Lassa and Mopeia arenaviruses. Vopr. Virusol. 36:146–150 (In Russian.) [PubMed] [Google Scholar]
- 39.Lukashevich IS. 1992. Generation of reassortants between African arenaviruses. Virology 188:600–605. 10.1016/0042-6822(92)90514-P [DOI] [PubMed] [Google Scholar]
- 40.Huang C, Kolokoltsova OA, Yun NE, Seregin AV, Poussard AL, Walker AG, Brasier AR, Zhao Y, Tian B, de la Torre JC, Paessler S. 2012. Junín virus infection activates the type I interferon pathway in a RIG-I-dependent manner. PLoS Negl. Trop. Dis. 6:e1659. 10.1371/journal.pntd.0001659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kolokoltsova OA, Yun NE, Poussard AL, Smith JK, Smith JN, Salazar M, Walker A, Tseng C-T, Aronson JF, Paessler S. 2010. Mice lacking alpha/beta and gamma interferon receptors are susceptible to Junin virus infection. J. Virol. 84:13063–13067. 10.1128/JVI.01389-10 [DOI] [PMC free article] [PubMed] [Google Scholar]