Abstract
BACKGROUND AND OBJECTIVE:
There is ongoing concern that stimulant medications may adversely affect growth. In a sample of attention-deficit/hyperactivity disorder (ADHD) cases and controls from a population-based birth cohort, we assessed growth and the association between stimulant treatment and growth.
METHODS:
Subjects included childhood ADHD cases (N = 340) and controls (N = 680) from a 1976 to 1982 birth cohort (N = 5718). Height and stimulant treatment information were abstracted from medical records and obtained during a prospective, adult follow-up study. For each subject, a parametric penalized spline smoothing method modeled height over time, and the corresponding height velocity was calculated as the first derivative. Peak height velocity (PHV) age and magnitude were estimated from the velocity curves. Among stimulant-treated ADHD cases, we analyzed height Z scores at the beginning, at the end, and 24 months after the end of treatment.
RESULTS:
Neither ADHD itself nor treatment with stimulants was associated with differences in magnitude of PHV or final adult height. Among boys treated with stimulants, there was a positive correlation between duration of stimulant usage before PHV and age at PHV (r = 0.21, P = .01). There was no significant correlation between duration of treatment and change in height Z scores (r = −0.08 for beginning vs end change, r = 0.01 for end vs 24 months later change). Among the 59 ADHD cases treated for ≥3 years, there was a clinically insignificant decrease in mean Z score from beginning (0.48) to end (0.33) of treatment (P = .06).
CONCLUSIONS:
Our findings suggest that ADHD treatment with stimulant medication is not associated with differences in adult height or significant changes in growth.
Keywords: attention-deficit/hyperactivity disorder, stimulant medications, adult outcomes, height, growth
What’s Known on This Subject:
Stimulant medications are indicated for treatment of childhood attention-deficit/hyperactivity disorder (ADHD), but there is concern that stimulants may negatively affect growth. However, no longitudinal, population-based studies have examined height into adulthood for childhood ADHD cases.
What This Study Adds:
This longitudinal, population-based study shows that neither childhood ADHD itself nor treatment with stimulants is associated with significant deficits in height into adulthood.
Attention-deficit/hyperactivity disorder (ADHD) is the most commonly diagnosed childhood neurodevelopmental disorder.1,2 Treatment with stimulant medication reduces the core symptoms of ADHD and may improve school, social, and behavioral functioning.3–7 However, the chronicity of ADHD7,8 and persistent concerns about the effect of stimulant treatment on growth9,10 necessitate a deeper understanding of how ADHD and stimulant treatment may affect growth.
ADHD may be associated with dysregulated growth.11–13 Early adolescents with ADHD may have small but significant height deficits compared with controls.14 In contrast, among stimulant-naive patients with ADHD, baseline height may be slightly greater than population norms,9 and children referred for ADHD treatment are reportedly taller at baseline than those not referred.9,15,16 The Multimodal Treatment Study of Children With ADHD Cooperative Group reported that untreated prepubertal children with ADHD had average height Z scores that increased over time, suggesting faster growth than population norms.17 More research is needed to assess associations between ADHD and dysregulated growth.
The potential adverse effect of stimulants on growth may be due to both their anorexic effect and an increase in synaptic dopamine, which acutely inhibits growth hormone.9,18 Although studies in the 1970s reported reductions in height in children treated with stimulant medication,10,19 subsequent studies have been mixed, with some reporting growth reductions16,20–22 and others finding no significant growth changes.23–26 Higher dosages of stimulants may cause more growth attenuation.9,19,27,28 Growth deficits may differ based on type,9,19,28–30 age of initiation,31–34 or duration16,35,36 of stimulant medications. Specifically, stimulant treatment duration >3 years may be associated with decreased height velocity throughout adolescence.36 Limitations in the existing literature include small sample sizes, lack of controls, referred samples limiting generalizability, and paucity of information about adult growth outcomes.
In this study, we report on the long-term associations between ADHD case status, stimulant treatment, and height in a large, population-based cohort of adults with childhood ADHD and without childhood ADHD. We compared height velocity, height Z scores before and after stimulant treatment, and adult height for subjects with versus without ADHD and, among ADHD cases, for those treated with stimulants versus those not treated. We examined the effect of stimulant medication by analyzing the impact of duration of stimulant treatment on height-for-age Z scores at the beginning, the end, and 24 months after the end of stimulant treatment.
Methods
Study Setting
The Rochester Epidemiology Project provided the infrastructure for this research.37 Almost all medical care for residents of Rochester, Minnesota is provided by Mayo Clinic, Olmsted Medical Center, and their 3 affiliated hospitals. Through the Rochester Epidemiology Project, all medical diagnoses and surgical procedures are recorded and indexed for computerized retrieval. The medical records contain detailed history of all medical encounters. For this project, all 41 public and private schools in Minnesota Independent School District 535 (Rochester, MN) participated in a contractual research agreement providing access to cumulative educational records for every child in the 1976 to 1982 Rochester, Minnesota birth cohort. The institutional review boards of both Mayo Clinic and Olmsted Medical Center approved this study.
Subjects
Birth Cohort
This study used a birth cohort consisting of all children born between January 1, 1976 and December 31, 1982 to mothers residing in the townships in Minnesota Independent School District 535, who continued to live in Rochester until at least age 5 years and who granted permission for research use of their medical records (N = 5718). The cohort was initially identified through computerized birth certificate information obtained from the Minnesota Department of Health, Division of Vital Statistics.38 The birth certificate information included characteristics of both the child (eg, birth length and weight) and the mother (eg, age and education).
Identification of Childhood ADHD Cases and Controls
The identification of childhood ADHD incident cases (N = 379) in this birth cohort has been described elsewhere39 and was based on combinations of the following 3 categories of information from school and medical records: behavioral symptoms consistent with criteria for ADHD from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision; positive ADHD questionnaire results; and documented clinical diagnosis of ADHD. Research ADHD criteria were met at a mean age of 10.4 years. At the time of this study, 340 ADHD cases continued to allow use of their records for research. For each case, we randomly selected 2 age- and gender-matched controls without ADHD (n = 680) from the birth cohort.
Height Measurements
This study used both a retrospective phase and a prospective follow-up of subjects into adulthood.2,8 We retrospectively obtained height from medical records for each subject from birth through August 2010. We also prospectively obtained height measurements using a stadiometer during the prospective phase of a research study using this same cohort.8 During the retrospective phase of the study, height measurements were obtained by clinical staff and recorded in inches or centimeters rounded to the nearest 0.5. For our analyses, all measurements were converted to centimeters. During the prospective phase of the study, trained research staff obtained height measurements during study visits from 8 am to 5 pm, to the nearest millimeter, using a Seca stadiometer (Seca Corporation, Issaquah, WA).
Stimulant Medication Treatment
In a previous study, we reviewed medical records of all ADHD cases for documentation about stimulant treatment.40 For each documented stimulant treatment episode, we abstracted the dosage and associated start and stop dates, based on the dates of visits at which medications were prescribed and when prescription refills were written. The cumulative duration of stimulant treatment was derived by summating the durations of the individual treatment episodes. ADHD cases were considered “stimulant treated” if treated for a cumulative duration of ≥3 months between 2 and <21 years of age; otherwise they were considered stimulant naive.
Data Analysis
Analyses were performed with the SAS version 9.2 software package (SAS Institute, Inc, Cary, NC). All calculated P values were 2-sided; P values <.05 were considered statistically significant. We used standard statistical methods to summarize the data: frequencies and percentages for nominal scaled variables and means and standard deviations or medians and interquartile ranges for continuously scaled variables. Comparisons between groups (ADHD cases versus controls, stimulant treated versus not-treated ADHD cases) were evaluated by using the χ2 test for gender, the 2-sample t test for birth length, birth weight, and age, and the Wilcoxon rank-sum test for maternal education categories and number of height measurements.
Height Velocity
Because height was measured during clinic visits, the number of measurements and spacing over time varied by subject. To obtain estimates of height continuously from infancy through early adulthood separately for each subject, we used a parametric penalized spline smoothing method proposed and implemented in MATLAB by Cao, Cai, and Wang41 to model height over time. This method combines the advantages of a parametric growth model based on expert knowledge42 with the flexibility of nonparametric smoothing methods. For each subject, we separately predicted the height and height velocity (by taking the first derivative of the function) from age 0 to 30 years at 0.1 increments. For each subject, we determined the peak height velocity (PHV) based on the point of maximal height velocity during the pubertal growth phase. We used the 2-sample t test (unadjusted for multiple comparisons) to compare the age at PHV and the magnitude of PHV between groups, separately by gender. We estimated the correlation between the cumulative stimulant duration before PHV and the age at PHV by using the Pearson correlation coefficient. To adequately estimate the height velocity continuously throughout the key periods of puberty and stimulant use, we restricted this analysis to use all available height measurements for subjects with ≥1 recorded height measurement during each of 3 following time intervals: 6 to <9, 9 to <12, and 12 to <15 years of age.
Height Z Scores Before and After Stimulant Treatment
We determined gender-specific height-for-age Z scores using the 2000 Centers for Disease Control and Prevention growth chart.43 Among the ADHD cases treated with stimulants for ≥3 months, we identified the gender-specific height-for-age Z scores at the beginning, the end, and 24 months after the end of stimulant treatment as follows: The Z score at the beginning of treatment was defined as the closest height within 6 months before or up to 3 months after treatment with stimulants started, the Z score at the end of treatment was defined as the closest height recorded within 3 months before or 3 months after treatment with stimulants ended, and the Z score 24 months after the end of treatment was defined as the closest height at 24 months recorded between 21 and 27 months after treatment with stimulants ended. The relationship between change (post–pre) in Z scores and the total cumulative stimulant duration was depicted graphically as a scatterplot using a loess smoother, and we estimated the correlation by using the Pearson correlation coefficient. We evaluated paired comparisons of Z scores by using the paired t test.
Adult Height
We defined adult height as the average of all height measurements performed at age ≥18 years for women and at age ≥20 years for men, consistent with criteria used in other studies.44–46 Adult height was compared between groups, separately by gender, using the 2-sample t test.
Results
Characteristics of ADHD Cases and Controls
Of the 340 ADHD cases and 680 age- and gender-matched non-ADHD controls, 339 cases and 674 controls had ≥2 height measurements recorded. The 339 ADHD cases had a median of 36 (interquartile range, 25–54) height measurements per subject over an average of 26.2 years of follow-up. The 674 controls had a median of 28 (interquartile range, 18–41) height measurements per subject over an average of 23.1 years of follow-up. To adequately estimate the height velocity continuously throughout the key periods of puberty and stimulant treatment, we restricted the cohort to 637 subjects (243 ADHD cases, 394 controls) with ≥1 recorded height measurement during each of following 3 time intervals: 6 to <9, 9 to <12, and 12 to <15 years of age. Table 1 summarizes the baseline and follow-up characteristics of these 637 subjects.
TABLE 1.
Baseline and Follow-up Characteristics of Non-ADHD Controls and ADHD Cases; ADHD Cases Separately by Treatment Status
| Characteristic | ADHD Case Status | Pa | ADHD Cases Treated With Stimulants for ≥3 Monthsb | Pa | ||
|---|---|---|---|---|---|---|
| Non-ADHD Controls (N = 394) | ADHD Cases (N = 243) | Yes (N = 171) | No (N = 65) | |||
| Baseline | ||||||
| Gender, n (%) | .88 | .027 | ||||
| Male | 286 (72.6) | 175 (72.0) | 130 (76.0) | 40 (61.5) | ||
| Female | 108 (27.4) | 68 (28.0) | 41 (24.0) | 25 (38.5) | ||
| Birth length (cm), mean (SD) | 51.8 (2.8) | 51.7 (2.9) | .73 | 51.7 (3.0) | 51.8 (2.7) | .83 |
| Birth wt (g), mean (SD) | 3522 (560) | 3456 (566) | .15 | 3449 (547) | 3472 (619) | .78 |
| Maternal age at subject’s birth, mean (SD) | 26.4 (4.7) | 26.1 (4.9) | .47 | 26.2 (4.7) | 26.1 (5.4) | .87 |
| Maternal education at subject’s birth, n (%) | .011 | .29 | ||||
| Not available, n | 42 | 19 | 15 | 4 | ||
| Less than high school | 26 (7.4) | 14 (6.3) | 9 (5.8) | 5 (8.2) | ||
| High school graduate | 106 (30.1) | 97 (43.3) | 72 (46.2) | 21 (34.4) | ||
| Some college | 130 (36.9) | 71 (31.7) | 48 (30.8) | 21 (34.4) | ||
| College graduate | 90 (25.6) | 42 (18.8) | 27 (17.3) | 14 (23.0) | ||
| Follow-up | ||||||
| Age at last recorded height measurement (y), mean (SD) | 24.6 (5.8) | 26.8 (5.0) | <.001 | 26.8 (4.8) | 26.7 (5.7) | .91 |
| Number of height measurements per subject in 3-y age windows, median (IQR) | ||||||
| Birth to <3 y | 9 (7, 12) | 8 (6, 12) | 8 (6, 12) | 8 (6, 9) | ||
| 3 to <6 y | 3 (2, 6) | 4 (2, 7) | 4 (2, 7) | 3 (2, 4) | ||
| 6 to <9 y | 3 (2, 6) | 4 (2, 7) | 5 (3, 8) | 4 (2, 6) | ||
| 9 to <12 y | 4 (2, 6) | 5 (3, 8) | 5 (3,8) | 5 (4, 7) | ||
| 12 to <15 y | 4 (2, 6) | 5 (3, 8) | 5 (3, 8) | 4 (3, 7) | ||
| 15 to <18 y | 3 (1, 5) | 3 (2, 6) | 4 (2, 7) | 3 (1, 5) | ||
| ≥18 y | 5 (1, 12) | 8 (3, 18) | 8 (3, 18) | 9 (2, 18) | ||
| Overall | 35 (26, 49) | 44 (33, 60) | <.001 | 46 (34, 62) | 41 (33, 53) | .16 |
| Age met ADHD research criteria (y), mean (SD) | n/a | 10.3 (3.6) | n/a | 9.9 (3.4) | 11.3 (3.8) | .006 |
IQR, interquartile range.
Comparisons between groups were evaluated by using the χ2 test for gender, the 2-sample t test for birth length, birth wt, and age, and the Wilcoxon rank-sum test for the maternal education categories and number of height measurements.
Duration of stimulant treatment was unknown for 7 of the 243 ADHD cases.
Among these 243 childhood ADHD cases, 171 (70.4%) were treated with stimulants for ≥3 months (Table 2). ADHD cases were prescribed methylphenidate (N = 152) and dextroamphetamine (N = 70) most commonly. Many ADHD cases (N = 67, 39.2%) were prescribed >1 type of stimulant medication over time.
TABLE 2.
Details About Age at Onset, Duration, and Average Daily Dosage of Stimulant Treatment of the 171 Stimulant-Treated ADHD Cases, Separately by Gender
| Male (N = 130) | Female (N = 41) | Total (N = 171) | |
|---|---|---|---|
| Age at onset of stimulant treatment (y) | |||
| Mean (SD) | 10.1 (3.6) | 10.4 (3.4) | 10.2 (3.5) |
| Median (IQR) | 9.8 (7.5–12.8) | 9.4 (7.9–13.3) | 9.8 (7.5–12.8) |
| Cumulative duration of stimulant treatment (m) | |||
| Mean (SD) | 54.4 (37.2) | 48.3 (37.9) | 53.0 (37.4) |
| Median (IQR) | 45.9 (27.3–77.0) | 35.5 (16.9–72.2) | 44.8 (22.6–76.9) |
| Average daily dosage (in MEUa) | |||
| Mean (SD) | 27.8 (11.1) | 21.3 (7.4) | 26.2 (10.7) |
| Median (IQR) | 26.6 (20.0–33.1) | 20.0 (17.3–25.0) | 24.5 (19.9–31.5) |
IQR, interquartile range; MEU = methylphenidate equivalent units.
All abstracted stimulant dosages were converted into MEUs with the following formula: 20 mg methylphenidate = 10 mg dextroamphetamine = 56.25 mg pemoline = 10 mg methamphetamine = 10 mg levoamphetamine plus dextroamphetamine.34
Estimated Peak Height Velocity
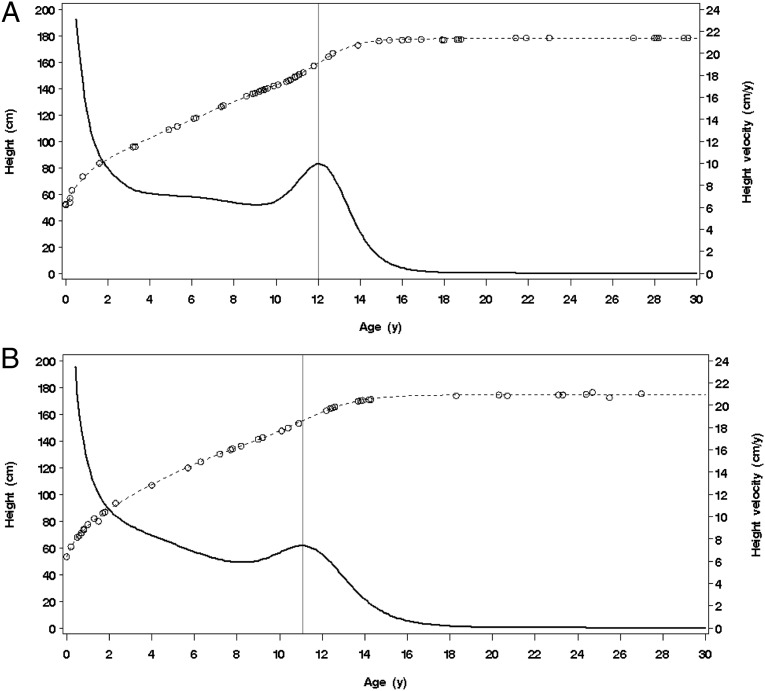
For each of the 637 subjects (243 ADHD cases, 394 controls), all recorded height measurements were used to predict their height and height velocity from 0 to 30 years of age using the parametric penalized spline smoothing method. As an example, Fig 1 depicts recorded height measurements, estimated height, derived height velocity, and PHV for 2 non-ADHD subjects. For 77 subjects (26 [10.7%] of ADHD cases and 51 [12.9%] of non-ADHD controls), there was no apparent PHV, based on visual inspection of the velocity curves; therefore, they were excluded from PHV analyses. The mean age at PHV and magnitude of PHV were not significantly different between ADHD cases and non-ADHD controls, either among male or female subjects (Figs 2 and 3, Table 3). There was no statistically significant difference between stimulant-naive ADHD cases at the time of the PHV and non-ADHD controls in age at PHV (male subjects, P = .08; female subjects, P = .41) or magnitude of PHV (male subjects, P = .28; female subjects, P = .83). However, among male ADHD cases, the mean age at PHV was significantly later among those treated with stimulants for ≥3 months by the time of their PHV compared with stimulant-naive cases (mean [SD], 13.5 years [1.0] vs. 12.9 years [1.2]; P = .002). Furthermore, among the male ADHD cases, there was a positive correlation between duration of stimulant usage before PHV and the age at PHV (r = 0.21, P = .01). Despite the later mean age at PHV for male ADHD cases treated ≥3 months, there was no difference in magnitude of PHV for stimulant-naive and stimulant-treated ADHD cases for male or female subjects.
FIGURE 1.
Measured (open circles) height, estimated (dashed line) height, and estimated height velocity (solid bold line) from the parametric penalized spline smoothing method for 2 non-ADHD subjects. A, Male subject with peak height velocity = 12 years. B, Female subject with peak height velocity = 11.1 years.
FIGURE 2.
Box plots of the estimated age at PHV, by ADHD case status and cumulative stimulant duration. Among the 217 ADHD cases with a PHV, 6 had unknown information on stimulant duration and are not displayed.
FIGURE 3.
Box plots of the estimated magnitude of PHV, by ADHD case status and cumulative stimulant duration. Among the 217 ADHD cases with a PHV, 6 had unknown information on stimulant duration and are not displayed.
TABLE 3.
Comparison of Age at PHV and Magnitude of PHV Between ADHD Cases and Non-ADHD Controls and by Cumulative Stimulant Duration
| No. of Subjects | Age at PHV (y) | Magnitude of PHV (cm/y) | ||||
|---|---|---|---|---|---|---|
| Mean (SD) | Pa | Mean (SD) | Pa | |||
| Male subjects | ADHD cases | 158 | 13.3 (1.1) | .96 | 8.2 (1.5) | .71 |
| Non-ADHD controls | 256 | 13.3 (1.3) | 8.3 (1.6) | |||
| Female subjects | ADHD cases | 59 | 11.0 (1.4) | .87 | 7.5 (1.4) | .80 |
| Non-ADHD controls | 87 | 11.0 (1.1) | 7.4 (1.2) | |||
| ADHD cases only | Cumulative stimulant duration before PHV | |||||
| Male subjects | Stimulant naiveb | 65 | 12.9 (1.2) | .002 | 8.0 (1.5) | .22 |
| Stimulant treatedc | 88 | 13.5 (1.0) | 8.3 (1.5) | |||
| 3 m–3 y | 27 | 13.3 (0.9) | 8.4 (1.8) | |||
| ≥3 y | 61 | 13.6 (0.9) | 8.3 (1.5) | |||
| Female subjects | Stimulant naiveb | 36 | 10.8 (1.5) | .36 | 7.5 (1.5) | .99 |
| Stimulant treatedc | 22 | 11.2 (1.0) | 7.5 (1.4) | |||
| 3 m–3 y | 16 | 11.1 (1.1) | 7.4 (1.4) | |||
| ≥3 y | 6 | 11.3 (0.9) | 7.7 (1.5) | |||
2-sample t test comparing ADHD cases with non-ADHD controls and, among the ADHD cases, stimulant naive with stimulant treated.
Stimulant naive was defined as subjects on stimulants for <3 mo before the time of the PHV.
6 ADHD cases had an unknown duration of stimulant medication treatment and were not included in this subanalysis.
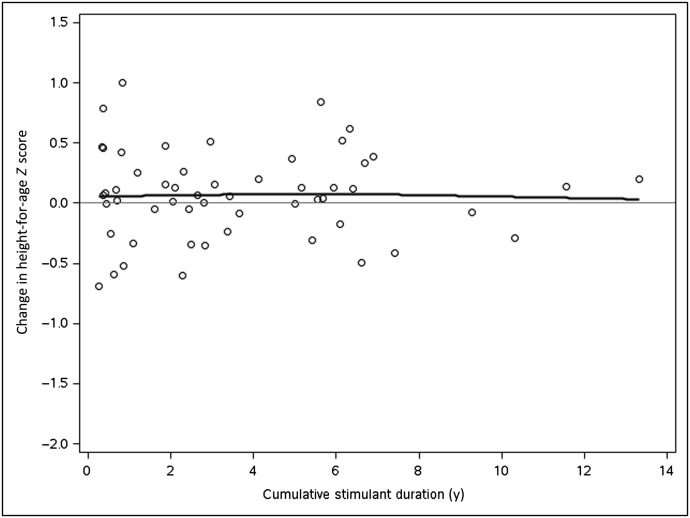
Effect of Stimulant Treatment on Height Z Scores
We included all ADHD cases treated with stimulants for ≥3 months (N = 219 of the original 340) in this analysis. Stimulant treatment details for these 219 (data not shown) are very similar to those presented in Table 2. Fig 4 depicts the relationship between the change in the gender-specific height-for-age Z score from the beginning to the end of stimulant treatment and the cumulative duration of stimulant treatment among the cases with height measurements at both time points (n = 111, r = −0.08, P = .42). Among the 20 cases with a cumulative stimulant duration of <1 year, there was a slight decrease in Z scores between the 2 time points (mean = 0.19 and 0.12 at the beginning and end, respectively; P = .26). However, among the 59 cases with a cumulative stimulant duration of ≥3 years, the mean Z score decreased from 0.48 at the beginning of treatment to 0.33 at the end of treatment (P = .06).
FIGURE 4.
Relationship between change in gender-specific height-for-age Z scores before and after stimulant treatment and cumulative stimulant duration.
Fig 5 depicts the relationship between the change in the gender-specific height-for-age Z score from the end to 24 months after treatment and the duration of treatment among cases with height measurements at both time points. Overall, there was a small increase in Z scores between the 2 time points (mean = 0.07 and 0.14, respectively, P = .18), but the change in Z score was not associated with cumulative stimulant treatment duration (r = 0.01, P = .94).
FIGURE 5.
Relationship between change in gender-specific height-for-age Z scores after stimulant treatment and 24 months later and cumulative stimulant duration.
Adult Height
Among the initial cohort of 340 ADHD cases and 680 age- and gender-matched non-ADHD controls, 742 subjects (285 cases, 457 controls) had ≥1 recorded adult height measurement available. Of these 742 subjects, 503 were included in the cohort of 637 patients summarized in Table 1. There was no difference in adult height between ADHD cases and controls for male subjects (mean difference = −0.4 cm, P = .56) or female subjects (mean difference = −1.1 cm, P = .29), or between stimulant-treated and stimulant-naive ADHD male subjects (mean difference = 0.6 cm, P = .64) or female subjects (mean difference = 0.2 cm, P = .93) (Table 4). Furthermore, there was no correlation between cumulative duration of stimulant treatment and adult height (male subjects: r = −0.02, P = .83; female subjects: r = 0.03, P = .84).
TABLE 4.
Comparison of Adult Height Between ADHD Cases and Non-ADHD Controls and by Cumulative Stimulant Duration
| No. of Subjects | Adult Height (cm), Mean (SD) | Pa | ||
|---|---|---|---|---|
| Male subjects | ADHD cases | 208 | 178.7 (7.6) | .56 |
| Non-ADHD controls | 309 | 179.1 (6.8) | ||
| Female subjects | ADHD cases | 77 | 164.6 (7.5) | .29 |
| Non-ADHD controls | 148 | 165.7 (6.6) | ||
| ADHD cases only | Cumulative stimulant duration | |||
| Male subjects | Stimulant naiveb | 58 | 178.2 (9.8) | .64 |
| Stimulant treatedc | 144 | 178.8 (6.7) | ||
| 3m to <1 y | 27 | 177.5 (4.6) | ||
| 1 to <3 y | 35 | 180.0 (8.0) | ||
| ≥3 y | 82 | 178.7 (6.6) | ||
| Female subjects | Stimulant naiveb | 31 | 164.6 (9.0) | .93 |
| Stimulant treatedc | 44 | 164.8 (6.4) | ||
| 3m to <1 y | 6 | 166.3 (6.2) | ||
| 1 to <3 y | 17 | 164.2 (6.7) | ||
| ≥3 y | 21 | 165.7 (6.4) |
2-sample t test comparing ADHD cases with non-ADHD controls and, among the ADHD cases, stimulant naive with stimulant treated.
Stimulant naive was defined as ADHD cases on stimulants for <3 mo before the time of the PHV.
8 ADHD cases had an unknown duration of stimulant medication treatment and were not included in this subanalysis.
Discussion
In this longitudinal, population-based study, neither ADHD nor treatment with stimulants was associated with differences in magnitude of PHV during adolescence. However, among boys treated with stimulants, the age of PHV was slightly later (12.9 years for stimulant-naive, 13.6 years for ADHD cases treated ≥3 years). There was no significant correlation between duration of treatment and change in height-for-age Z scores at the beginning, the end, or 24 months after the end of stimulant treatment. However, among the cases with a cumulative stimulant duration of ≥3 years, the mean change in Z scores over the course of treatment approached statistical significance (P = .06), although the magnitude of change was clinically insignificant (mean change, 0.15). Neither ADHD nor treatment with stimulants was associated with differences in final adult height.
ADHD was not associated with age or magnitude of PHV or final adult height. Previous studies have been contradictory,9 with reports of both decreased14 and increased14,47 growth among adolescent ADHD cases. However, these studies followed subjects during childhood but not to adulthood. In a study of clinically referred subjects followed into their early 20s, there were no differences in growth between ADHD cases and controls,25 and our findings, using non-referred ADHD cases and controls from a population-based birth cohort, provide additional evidence that ADHD itself does not negatively affect growth.
The similarity in final adult height between ADHD cases treated with stimulants and those not treated is reassuring. This finding could reflect catch-up growth occurring after stimulant treatment was discontinued, as suggested by the Multimodal Treatment Study of Children With ADHD.5 However, consistent with Biederman et al,25 we found no significant difference in the magnitude of PHV between stimulant-treated and stimulant-naive ADHD cases. We also examined height-for-age Z scores in relation to stimulant treatment because previous research suggests that a child’s age and timing of treatment may matter.32–34 Overall, we found no significant difference in height Z scores at the beginning and at the end of stimulant treatment. Although the decrease in Z scores from the beginning to end of treatment among the ADHD cases treated for ≥3 years approached statistical significance (P = .06), the difference was clinically insignificant. For example, in an 18-year-old man with height ranging from 5 feet 9 inches to 6 feet 3 inches, a change in Z score of 0.16 equates to slightly <0.5 inches. There was a small, clinically insignificant increase in height Z scores between the end and 24 months after the end of stimulant treatment that does not suggest significant catch-up growth after stimulants were discontinued. There were no differences in adult height outcomes, either overall or based on duration of stimulant treatment, indicating that even for those treated for ≥3 years there was no overall impact on final adult height.
Our findings should be interpreted with some potential limitations. These data are from a clinical setting. Clinicians were probably reviewing growth curves and may have made treatment decisions, such as cessation of stimulants or dietary recommendations, based on the child’s growth. Despite our findings, clinicians should continue to carefully monitor growth when making medication management decisions. The initial retrospective identification of ADHD cases may have been incomplete; however, our comprehensive access to all medical and school records for every birth cohort member makes it unlikely that we missed a significant number of cases.39 ADHD cases were not all treated with stimulant medications throughout adolescence, potentially accounting for the lack of differences in adult height between treated and untreated cases. However, we found no significant adverse impact of treatment on magnitude of PHV, growth during treatment, or adult height. It was impossible to assess the precision of growth measurements obtained during clinical visits. The setting of this study may limit generalizability, given that the population is largely white and middle class.37
Conclusions
Childhood ADHD is not associated with dysregulated growth. Furthermore, in this population-based cohort, stimulant treatment of childhood ADHD is not associated with deficits in adult height nor with a significant adverse impact on growth throughout childhood and adolescence.
Acknowledgments
We thank study coordinators Candice Klein and Ann Van Oosten for their efforts in subject recruitment and conduct of the study assessments. We are also indebted to Brad Lewis for the MATLAB programming.
Glossary
- ADHD
attention-deficit/hyperactivity disorder
- PHV
peak height velocity
Footnotes
Dr Harstad participated in the design of this analysis and drafted the initial manuscript; Ms Weaver participated in the design of this study and analysis, conducted the statistical analyses, and drafted portions of the initial manuscript; Drs Katusic, Colligan, Kumar, and Voigt participated in the design of this study and analysis; Dr Chan participated in the design of this analysis; Dr Barbaresi participated in the design of this study and analysis and edited the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The study was supported by Public Health Service research grants MH076111, HD29745, and AG034676. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention (CDC) . Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children: United States, 2003 and 2007. MMWR Morb Mortal Wkly Rep. 2010;59(44):1439–1443 [PubMed] [Google Scholar]
- 2.Barbaresi W, Katusic S, Colligan R, et al. How common is attention-deficit/hyperactivity disorder? Towards resolution of the controversy: results from a population-based study. Acta Paediatr Suppl. 2004;93(445):55–59 [DOI] [PubMed] [Google Scholar]
- 3.Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Modifiers of long-term school outcomes for children with attention-deficit/hyperactivity disorder: does treatment with stimulant medication make a difference? Results from a population-based study. J Dev Behav Pediatr. 2007;28(4):274–287 [DOI] [PubMed] [Google Scholar]
- 4.Kaplan G, Newcorn JH. Pharmacotherapy for child and adolescent attention-deficit hyperactivity disorder. Pediatr Clin North Am. 2011;58(1):99–120, xi [DOI] [PubMed] [Google Scholar]
- 5.MTA Cooperative Group . National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: 24-month outcomes of treatment strategies for attention-deficit/hyperactivity disorder. Pediatrics. 2004;113(4):754–761 [DOI] [PubMed] [Google Scholar]
- 6.Biederman J, Monuteaux MC, Spencer T, Wilens TE, Faraone SV. Do stimulants protect against psychiatric disorders in youth with ADHD? A 10-year follow-up study. Pediatrics. 2009;124(1):71–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown RT, Amler RW, Freeman WS, et al. American Academy of Pediatrics Committee on Quality Improvement. American Academy of Pediatrics Subcommittee on Attention-Deficit/Hyperactivity Disorder . Treatment of attention-deficit/hyperactivity disorder: overview of the evidence. Pediatrics. 2005;115(6). Available at: www.pediatrics.org/cgi/content/full/115/6/e74915930203 [Google Scholar]
- 8.Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131(4):637–644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faraone SV, Biederman J, Morley CP, Spencer TJ. Effect of stimulants on height and weight: a review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(9):994–1009 [DOI] [PubMed] [Google Scholar]
- 10.Safer D, Allen R, Barr E. Depression of growth in hyperactive children on stimulant drugs. N Engl J Med. 1972;287(5):217–220 [DOI] [PubMed] [Google Scholar]
- 11.Ptacek R, Kuzelova H, Paclt I, Zukov I, Fischer S. ADHD and growth: anthropometric changes in medicated and non-medicated ADHD boys. Med Sci Monit. 2009;15(12):CR595–CR599 [PubMed] [Google Scholar]
- 12.Ptacek R, Kuzelova H, Paclt I, Zukov I, Fischer S. Anthropometric changes in non-medicated ADHD boys. Neuroendocrinol Lett. 2009;30(3):377–381 [PubMed] [Google Scholar]
- 13.Hanć T, Cieślik J, Wolańczyk T, Gajdzik M. Assessment of growth in pharmacological treatment-naïve Polish boys with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2012;22(4):300–306 [DOI] [PubMed] [Google Scholar]
- 14.Spencer TJ, Biederman J, Harding M, O’Donnell D, Faraone SV, Wilens TE. Growth deficits in ADHD children revisited: evidence for disorder-associated growth delays? J Am Acad Child Adolesc Psychiatry. 1996;35(11):1460–1469 [DOI] [PubMed] [Google Scholar]
- 15.Bereket A, Turan S, Karaman MG, Haklar G, Ozbay F, Yazgan MY. Height, weight, IGF-I, IGFBP-3 and thyroid functions in prepubertal children with attention deficit hyperactivity disorder: effect of methylphenidate treatment. Horm Res. 2005;63(4):159–164 [DOI] [PubMed] [Google Scholar]
- 16.Poulton A, Cowell CT. Slowing of growth in height and weight on stimulants: a characteristic pattern. J Paediatr Child Health. 2003;39(3):180–185 [DOI] [PubMed] [Google Scholar]
- 17.Swanson JM, Elliott GR, Greenhill LL, et al. Effects of stimulant medication on growth rates across 3 years in the MTA follow-up. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1015–1027 [DOI] [PubMed] [Google Scholar]
- 18.De Zegher F, Van Den Berghe G, Devlieger H, Eggermont E, Veldhuis JD. Dopamine inhibits growth hormone and prolactin secretion in the human newborn. Pediatr Res. 1993;34(5):642–645 [DOI] [PubMed] [Google Scholar]
- 19.Safer DJ, Allen RP. Factors influencing the suppressant effects of two stimulant drugs on the growth of hyperactive children. Pediatrics. 1973;51(4):660–667 [PubMed] [Google Scholar]
- 20.Post FA, Willcox PA, Mathema B, et al. Genetic polymorphism in Mycobacterium tuberculosis isolates from patients with chronic multidrug-resistant tuberculosis. J Infect Dis. 2004;190(1):99–106 [DOI] [PubMed] [Google Scholar]
- 21.Zhang H, Du M, Zhuang S. Impact of long-term treatment of methylphenidate on height and weight of school age children with ADHD. Neuropediatrics. 2010;41(2):55–59 [DOI] [PubMed] [Google Scholar]
- 22.Faraone SV, Spencer TJ, Kollins SH, Glatt SJ. Effects of lisdexamfetamine dimesylate treatment for ADHD on growth. J Am Acad Child Adolesc Psychiatry. 2010;49(1):24–32 [DOI] [PubMed] [Google Scholar]
- 23.Hechtman L, Weiss G, Perlman T. Young adult outcome of hyperactive children who received long-term stimulant treatment. J Am Acad Child Psychiatry. 1984;23(3):261–269 [DOI] [PubMed] [Google Scholar]
- 24.Kramer JR, Loney J, Ponto LB, Roberts MA, Grossman S. Predictors of adult height and weight in boys treated with methylphenidate for childhood behavior problems. J Am Acad Child Adolesc Psychiatry. 2000;39(4):517–524 [DOI] [PubMed] [Google Scholar]
- 25.Biederman J, Spencer TJ, Monuteaux MC, Faraone SV. A naturalistic 10-year prospective study of height and weight in children with attention-deficit hyperactivity disorder grown up: sex and treatment effects. J Pediatr. 2010;157(4):635–640, e631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Biederman J, Faraone SV, Monuteaux MC, Plunkett EA, Gifford J, Spencer T. Growth deficits and attention-deficit/hyperactivity disorder revisited: impact of gender, development, and treatment. Pediatrics. 2003;111(5 pt 1):1010–1016 [DOI] [PubMed] [Google Scholar]
- 27.Charach A, Figueroa M, Chen S, Ickowicz A, Schachar R. Stimulant treatment over 5 years: effects on growth. J Am Acad Child Adolesc Psychiatry. 2006;45(4):415–421 [DOI] [PubMed] [Google Scholar]
- 28.Pliszka SR, Matthews TL, Braslow KJ, Watson MA. Comparative effects of methylphenidate and mixed salts amphetamine on height and weight in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2006;45(5):520–526 [DOI] [PubMed] [Google Scholar]
- 29.Sund AM, Zeiner P. Does extended medication with amphetamine or methylphenidate reduce growth in hyperactive children? Nord J Psychiatry. 2002;56(1):53–57 [DOI] [PubMed] [Google Scholar]
- 30.Schertz M, Adesman AR, Alfieri NE, Bienkowski RS. Predictors of weight loss in children with attention deficit hyperactivity disorder treated with stimulant medication. Pediatrics. 1996;98(4 pt 1):763–769 [PubMed] [Google Scholar]
- 31.Swanson J, Greenhill L, Wigal T, et al. Stimulant-related reductions of growth rates in the PATS. J Am Acad Child Adolesc Psychiatry. 2006;45(11):1304–1313 [DOI] [PubMed] [Google Scholar]
- 32.Faraone SV, Biederman J, Monuteaux M, Spencer T. Long-term effects of extended-release mixed amphetamine salts treatment of attention-deficit/hyperactivity disorder on growth. J Child Adolesc Psychopharmacol. 2005;15(2):191–202 [DOI] [PubMed] [Google Scholar]
- 33.Spencer TJ, Faraone SV, Biederman J, Lerner M, Cooper KM, Zimmerman B, Concerta Study Group . Does prolonged therapy with a long-acting stimulant suppress growth in children with ADHD? J Am Acad Child Adolesc Psychiatry. 2006;45(5):527–537 [DOI] [PubMed] [Google Scholar]
- 34.Vincent J, Varley CK, Leger P. Effects of methylphenidate on early adolescent growth. Am J Psychiatry. 1990;147(4):501–502 [DOI] [PubMed] [Google Scholar]
- 35.Satterfield JH, Cantwell DP, Schell A, Blaschke T. Growth of hyperactive children treated with methylphenidate. Arch Gen Psychiatry. 1979;36(2):212–217 [DOI] [PubMed] [Google Scholar]
- 36.Poulton AS, Melzer E, Tait PR, et al. Growth and pubertal development of adolescent boys on stimulant medication for attention deficit hyperactivity disorder. Med J Aust. 2013;198(1):29–32 [DOI] [PubMed] [Google Scholar]
- 37.Melton LJ, III. History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71(3):266–274 [DOI] [PubMed] [Google Scholar]
- 38.Katusic SK, Colligan RC, Barbaresi WJ, Schaid DJ, Jacobsen SJ. Potential influence of migration bias in birth cohort studies. Mayo Clin Proc. 1998;73(11):1053–1061 [DOI] [PubMed] [Google Scholar]
- 39.Katusic SK, Barbaresi WJ, Colligan RC, Weaver AL, Leibson CL, Jacobsen SJ. Case definition in epidemiologic studies of AD/HD. Ann Epidemiol. 2005;15(6):430–437 [DOI] [PubMed] [Google Scholar]
- 40.Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Leibson CL, Jacobsen SJ. Long-term stimulant medication treatment of attention-deficit/hyperactivity disorder: results from a population-based study. J Dev Behav Pediatr. 2006;27(1):1–10 [DOI] [PubMed] [Google Scholar]
- 41.Cao J, Cai J, Wang L. Estimating curves and derivative with parametric penalized spline smoothing. Stat Comput. 2012;22(5):1059–1067 [Google Scholar]
- 42.Jolicoeur P, Pontier J, Abidi H. Asymptotic models for the longitudinal growth of human stature. Am J Hum Biol. 1992;4(4):461–468 [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. A SAS program for the CDC growth charts. 2011. Available at: www.cdc.gov/nccdphp/dnpa/growthcharts/resources/sas.htm. Accessed April 11, 2013
- 44.Lee JJ, Escher JC, Shuman MJ, et al. Final adult height of children with inflammatory bowel disease is predicted by parental height and patient minimum height Z-score. Inflamm Bowel Dis. 2010;16(10):1669–1677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fine RN, Sullivan EK, Tejani A. The impact of recombinant human growth hormone treatment on final adult height. Pediatr Nephrol. 2000;14(7):679–681 [DOI] [PubMed] [Google Scholar]
- 46.Kelly HW, Sternberg AL, Lescher R, et al. CAMP Research Group . Effect of inhaled glucocorticoids in childhood on adult height. N Engl J Med. 2012;367(10):904–912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hanć T, Cieślik J. Growth in stimulant-naive children with attention-deficit/hyperactivity disorder using cross-sectional and longitudinal approaches. Pediatrics. 2008;121(4). Available at: www.pediatrics.org/cgi/content/full/121/4/e967 [DOI] [PubMed] [Google Scholar]