Abstract
The expression of transient receptor potential cation channel V5 (TRPV5) in articular cartilage cells under normal and exercise loading conditions was measured, and the clinical significance, in order to define its role in the formation of articular cartilage tissues was analyzed. In normal and osteoarthritis (OA) Sprague Dawley rats the severity of injury was observed, TRPV5 expression was measured by immunohistochemistry following exercise loading, and its association with clinical pathological characteristics (including articular lesions) was analyzed. The results of the immunohistochemical assay showed that the percentage of positive expression areas in the normal articular cartilage and loading articular cartilage groups was 34.3±5.8 and 18.1±4.9%, respectively. In the OA articular cartilage and OA loading articular cartilage groups, the positive expression areas were 13.17±4.2 and 6.4±2.7%, respectively. There was a statistically significant difference in TRPV5 expression levels between the normal articular cartilage and loading articular cartilage groups, and between the OA articular cartilage and OA loading articular cartilage groups (P<0.001). TRPV5 is expressed in all bone cartilage tissues and its expression level depends on the load of the bone and joint. Therefore, this indicates that TRPV5 may play a role in the formation and development processes of cartilage tissues.
Keywords: osteoarthritis, cartilage cell, exercise load, transient receptor potential cation channel V5, transient receptor potential channel, immunohistochemistry
Introduction
Osteoarthritis (OA), a common chronic joint disease, is frequently observed in middle-aged and elderly patients, and is also an important factor influencing the quality of life in these age groups. Joints are load-bearing and their surfaces are covered by articular cartilages. The layer of articular cartilages is a significant component of the motor system, and can reduce the friction coefficient of articular surfaces and disperse the pressure load on the articular surface (1). With the progression of OA, the injury of cartilage cells becomes aggravated. Investigating the changes of cartilage cells is an important process to explore the etiopathogenesis and therapy of OA. Currently, studies are focusing on interpreting and clarifying the pathogenesis and biological behaviors of OA in molecular and genetic perspectives, which is also the premise and foundation of developing an effective and precisely targeted treatment for OA in the future. Transient receptor potential (TRP) channels are a group of important cation channels located in the cell membrane, and can respond to temperature, touch, pain, osmotic pressure, taste and other stimuli (2,3).
TRP cation channel V5 (TRPV5) is one of the TRP channel subtypes, and was cloned from rabbit proximal tubular kidney epithelial cells. TRPV5 is a highly selective receptor-activated ion channel; the current is highly selective for Ca2+ via active TRPV5 and is feedback-regulated by Ca2+ (4). TRPV5 is expressed in the kidneys, duodenum, pancreas, prostate, placenta, colon and rectum, and is highly expressed in distal convoluted renal tubules and collecting tubules. In the human body, TRPV5 is usually co-existent and co-expressed with active calcium-resorption proteins, such as calcium binding proteins and the Na+/Ca2+ exchanger. The expression level of TRPV5 in channel mediating Ca2+ transmembrane transport is regulated by vitamin D3, Ca2+ concentration, estrogen and parathyroid hormone. TRPV5 can be opened or closed by conformational change, thereby controlling the transmembrane flow of Ca2+ and maintaining the balance of Ca2+ in vivo (5). Studies have shown that TRPV5 may be associated with inflammation, endocrine and other pathological processes (6), and closely correlates with the occurrence of idiothic hypercalciuria, osteoporosis and bone tumors (7,8). Thus far, there are few studies regarding the association between TRPV5 and articular cartilage cells. The expression of TRPV5 in articular cartilage cells and its mechanism of action in the development of diseases have not been clarified.
A suitable exercise load can provide stress stimulation for the proliferation, differentiation and functional phenotype of articular cartilages. By contrast, an improper mechanical load causes and even aggravates the degeneration of articular cartilages, directly influencing and damaging joint functions and eventually inducing OA. The aim of the present study was to preliminarily investigate the protein expression characteristics of TRPV5 in rat articular cartilage cells and its biological significance under different exercise load modes, to analyze the association between TRPV5 expression levels and different exercise loads, and to preliminarily explore and analyze the possible role of TRPV5 in chondrogenesis.
Materials and methods
Exercise-load models of normal rats
Sprague Dawley (SD) rats, aged 50 days, were forced to exercise for 30 min, twice a day for 8 weeks on a self-made animal treadmill (independently developed based on the Junxia treadmill). During the exercise, the rats were stimulated with sound or by prodding with a small wooden stick. No load was used in the control group. There were 12 rats in each group. The rats were maintained in a specific, pathogen-free environment. All the animal procedures were performed according to the protocol approved by the Experiment Animal Center of China Medical University (Shenyang, Liaoning, China) in accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health.
Exercise-load models of OA rats
SD rats, aged 50 days, were orally administered monosodium iodoacetate to induce OA, and following this they underwent treadmill exercise. The method and intensity of exercise and grouping were the same as with the normal rats.
Main reagents
Rabbit polyclonal antibody against human TRPV5 (Santa Cruz Biotechnology, Inc, Dallas, TX, USA) was used as the primary antibody, and the immunohistochemistry Substance P secondary antibody kit (Gene Technologies Ltd., Shanghai, China) was used.
Macroscopic grading of experimental samples
After 8 weeks of exercise, the experimental animals were sacrificed by spine dislocation. The knee articular cartilages were exposed and the cartilage lesions were graded according to the Outerbridge Grading Standard (9) by visual observation. The grading standard was as follows: Grade 0, normal articular cartilage; grade 1, mild OA; grade 2, moderate OA; grades 3 and 4, severe OA. Subsequently, the cartilage tissues were sampled.
Histopathology
The resected surgical samples were fixed in 10% neutral formalin-buffered solution, gradient-dehydrated with alcohol, embedded in paraffin and cut into 4-μm tissue sections. The sections were dried, dewaxed, gradient-hydrated with alcohol, stained with hematoxylin and eosin (H&E) and observed for pathological characteristics under a microscope.
Immunohistochemistry
Immunohistochemical staining was performed with the Elivision™ tool kit (Maxim Corp., Fuzhou, China) according to the manufacturer’s instructions. The anti-TRPV5 antibody was diluted by 1:50 with 0.01 mol/l phosphate-buffered solution (PBS), and added onto the sections as a primary antibody. In the negative controls, 0.01 mol/l PBS was used instead of the primary antibody to exclude false-positive results caused by non-specific antibody reactions. All the samples were tested twice as described above to exclude possible technical errors. The experimental steps are described as follows: The sections were dewaxed, hydrated, blocked for 10 min in 3.0% H2O2, incubated with 0.01 mol/l sodium citrate solution and placed into a microwave oven for high-temperature antigen retrieval. Subsequently, these sections were blocked in normal goat serum blocking buffer for 20 min at 37°C, incubated overnight at 4°C with primary antibody (1:50 anti-TRPV5 antibody), rewarmed for 45 min and washed with 0.01 mol/l PBS. The sections were incubated with biotinylated secondary antibody for 20 min at 37°C, washed with 0.01 mol/l PBS, developed with diaminobenzidine and counterstained with hematoxylin. Following this, the above sections were dehydrated, vitrified and mounted. Finally, the sections were photographed under a microscope (×400 power) and five fields were randomly selected. The integrated optical density of positive units was measured using the Olympus BX52 microscopic image acquisition system (Olympus, Tokyo, Japan) and the results were evaluated.
Statistical analysis
Data are expressed as (mean ± standard deviation). SPSS 16.0 software (SPSS, Inc., Chicago, IL, USA) was used for independent sample t-test. P<0.05 was considered to indicate a statistically significant difference and P<0.01 were highly statistically significant.
Results
Histopathology
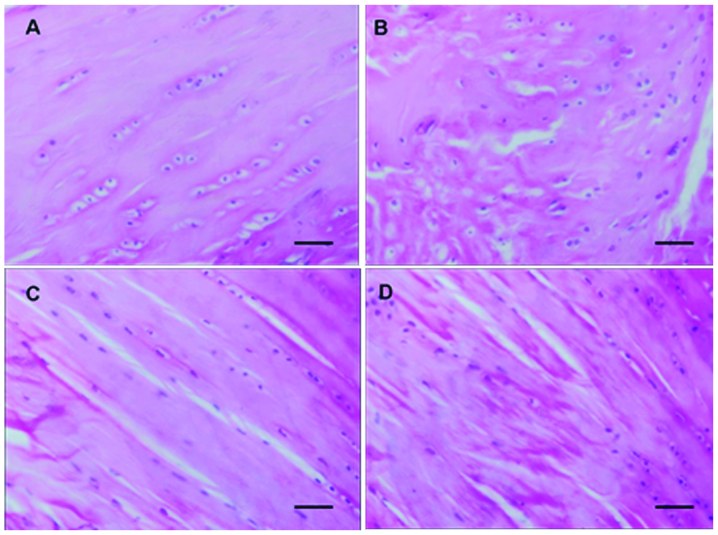
In the normal control group, the surface of rat articular cartilages was smooth. The superficial cartilage cells were fusiform and arranged intensely, and their long axis was parallel to the cartilage surface. The intermediate cartilage cells were round, arranged irregularly and distributed in a double-cell back-to-back manner. The mast cells were gradually distributed from double-cell to multi-cell mass, without a visible tidal line. There were no significant pathological changes in the calcified cartilage layer and subchondral bone. In the normal loading group, the ulcer defects and minor fissures were observed on the surface of articular cartilages, and the cartilage cells were reduced in number, in a disorderly arrangement, and clustered. In the normal control group, there were 1–2 layers of rat synovial tissues and cells. The cells were distributed regularly and the synovial tissues had no signs of chronic inflammation (Fig. 1A). In the normal loading group, there was significant hyperplasia of rat synovial tissues, the synovial cell layer changed into 3–5 layers due to hyperplasia, the synovial cells were arranged irregularly and there was hyperplasia of subsynovial fibrous tissues and blood capillaries, infiltration of monocytes and lymphocytes, and synovial lipedema (Fig. 1B). In the OA group, the surface of the cartilage tissues was coarse and uneven, the cartilage cells were in a disorderly arrangement, decreased in number and clustered, and there was degeneration and necrosis of cartilage cells, decreased cartilage thickness, unevenly stained matrix and metachromasia (Fig. 1C). In the OA loading group, the cartilage cells were arranged extremely irregularly and were significantly decreased in number. There was also cell clustering and a larger number of cartilage cells became degenerative and necrotic (Fig. 1D).
Figure 1.
Hematoxylin and eosin (H&E) staining of normal and osteoarthritis (OA) articular cartilage tissue (magnification, ×200; scale bar, 50 μm). (A) Normal articular cartilage tissue. (B) Normal loading articular cartilage tissue. (C) OA articular cartilage tissue. (D) OA loading articular cartilage tissue.
Immunohistochemistry of TRPV5
TRPV5 expression was mainly located at the membrane of articular cartilage cells. The surface of clustered cartilage cells demonstrated brown positive staining (Fig. 2). In the normal articular cartilage group, there was a rich cartilage matrix, the cartilage cells increased and were clearly distributed. The positive protein expression of TRPV5 was observed in the superficial immature cartilage cells and the deep isogenous cartilage cell clusters, typically in the articular cartilage load-bearing region (Fig. 2A). In the normal loading group, there was degeneration of articular cartilages, thinned cartilage matrix, a decreased number of articular cartilage cells and decreased brown TRPV5 protein-positive cells in the cartilage cell clusters (Fig. 2B). The percentage of positive expression areas in the normal articular cartilage and normal loading articular cartilage groups was 34.3±5.8 and 18.1±4.9%, respectively (P<0.01). In the OA articular cartilage group, there was a thin cartilage matrix, the number of cartilage cells decreased significantly, the cartilage cells degenerated and were irregular in morphology and distributed in disorderly fashion, and the brown TRPV5 protein-positive cells in the cartilage cell clusters were markedly reduced (Fig. 2C). In the OA loading articular cartilage group, the cartilage matrix was injured and ulcerated, the subchondral bone was exposed and sclerotized, the articular cartilage cells were significantly decreased and were mainly present in the periarticular non-load-bearing region, degenerated, irregular in morphology and distributed in an extremely disorderly fashion. A small amount of brown TRPV5 protein-positive expression was found in some of the surviving articular cartilage cells (Fig. 2D). The percentage of positive expression areas in the OA articular cartilage and OA loading articular cartilage groups was 13.17±4.2 and 6.4±2.7%, respectively (P<0.01).
Figure 2.
Immunohistochemical staining showing transient receptor potential cation channel V5 (TRPV5) expression (magnification, ×200; scale bar, 50 μm). TRPV5 was expressed in the cell membrane, and the intensity varied significantly among the pathological groups. (A) Normal articular cartilage tissue. (B) Normal loading articular cartilage tissue. (C) Osteoarthritis (OA) articular cartilage tissue. (D) OA loading articular cartilage tissue.
Discussion
Based on the encoding amino acid sequences, the TRP gene family is divided into seven subfamilies, which are TRPC, TRPV, TRPM, TRPA, TRPP, TRPML and TRPN (10). TRPs are a group of voltage-independent cation channels that are widely expressed on cell membranes of various organisms, and can respond to several intra- and extra-cellular stimuli (4). The subtypes, such as TRPV, TRPM8, TRPC3 and TRPC6, have been demonstrated to be correlated to the occurrence of malignant tumors (11,12). In the present study, TRPV5 was found to be expressed in the articular cartilage cells to different extents, and its expression level was associated with the severity of joint injury (including the downregulation of TRPV5 expression level with an increase of injury severity). TRPV5 expression has been indicated to possibly play a role in the articular chondrogenesis process.
Thus far, TRP channels are a commonly used molecular entity model used to study store-operated calcium channels (SOCs) (13). The opening of SOCs is triggered by calcium store depletion and SOCs are the major channels for Ca2+ influx in non-excitable cells (14). Ca2+, as the most important second messenger in the body, is a necessary component of several transmembrane signaling pathways (such as the phosphatidylinositol-3-kinase messenger system). All the phases of cell proliferation are associated with Ca2+ regulation (15,16) and Ca2+ can extensively participate in cell proliferation, differentiation and migration by influencing cell volume, controlling cell membrane potential, and contributing to cytoskeletal formation and intercellular responses. Furthermore, the increased Ca2+ concentration in cells can activate the endogenous endonuclease that segmentalize DNA, is dependent on Ca2+/Mg2+, and plays an important role in apoptosis (17). In the TRP family, TRPV5 is a transient receptor potential channel with high selectivity to Ca2+, and plays a critical role in maintaining Ca2+ concentration in cells. The TRPV5 expression level influences intracellular Ca2+ homeostasis and thus, it may participate in the proliferation and apoptosis of cartilage cells. In fact, studies indicate that TRPV5 is expressed in giant cell tumor tissues of the bone and may be involved in the transmembrane transport of Ca2+ in tumor cells (8). TRPV5 is co-expressed with the majority of calcium-binding proteins in tissues, among which Annexins (ANXs) are closely associated with cell growth, differentiation and infiltration. Annexin A10 expression is a sign of histocyte differentiation and growth arrest, which is closely associated with the malignant phenotype of histocytes, vascular invasion and tumor progression (18). Annexin A2 downregulation can block TRPV5-mediated current. The aforementioned findings demonstrate that ANXs may play a role by regulating TRPV5 (19). The present study confirms that TRPV5 is highly expressed in normal articular cartilage tissues and injured articular cartilage tissues, but its expression level varies among different pathological types. In addition, the expression level of TRPV5 in cartilage tissues is associated with the injury severity of cartilage histocytes. This suggests that TRPV5 expression may play a role in the formation and development of cartilage, and indicates that the TRPV5 expression level may be helpful for prognosis prediction, although the specific mechanism underlying its role in these processes requires further study.
Acknowledgements
The present study was supported by the National Natural Scientific Foundation of China (grant no. 81272050) to L.B.
Abbreviations
- OA
osteoarthritis
- SD
Sprague Dawley
- TRPV5
transient receptor potential cation channel V5
- H&E
hematoxylin and eosin
- PBS
phosphate-buffered solution
References
- 1.Ruiz-Romero C, López-Armada MJ, Blanco FJ. Proteomic characterizeation of human normal articular chondrocytes: a novel tool for the study of osteoarthritis and other rheumatic diseases. Proteomics. 2005;5:3048–3059. doi: 10.1002/pmic.200402106. [DOI] [PubMed] [Google Scholar]
- 2.Bang S, Yoo S, Oh U, Hwang SW. Endogenous lipid-derived ligands for sensory TRP ion channels and their pain modulation. Arch Pharm Res. 2010;33:1509–1520. doi: 10.1007/s12272-010-1004-9. [DOI] [PubMed] [Google Scholar]
- 3.Patel A, Sharif-Naeini R, Folgering JR, et al. Canonical TRP channels and mechanotransduction: from physiology to disease states. Pflugers Arch. 2010;460:571–581. doi: 10.1007/s00424-010-0847-8. [DOI] [PubMed] [Google Scholar]
- 4.Clapham DE. TRP channels as cellular sensors. Nature. 2003;426:517–524. doi: 10.1038/nature02196. [DOI] [PubMed] [Google Scholar]
- 5.Yang Z, Qin DM, Gu GS, et al. The correlations between TRPV5 and bone metabolism. J Jilin Univ Health Sci. 2005;31:645–648. [Google Scholar]
- 6.Topala CN, Bindels R, Hoenderop J. Regulation of the epithelial calcium channel TRPV5 by extracellular factors. Curr Opin Nephrol Hypertens. 2007;16:319–324. doi: 10.1097/MNH.0b013e3281c55f02. [DOI] [PubMed] [Google Scholar]
- 7.Liu Y, Zhang B. New progress in the study of idiopathic hypercalciuria. Medical Recapitulate. 2010;16:2969–2972. [Google Scholar]
- 8.Li FC, Gu GS, Jin CH, et al. Expression of TRPV5 and TRPV6 in osteosarcoma and giant cell tumor of bone. Shandong Med J. 2007;47:73–74. [Google Scholar]
- 9.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–775. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 10.Montell C, Birnbaumer L, Flockerzi V, et al. A unified nomenclature for the superfamily of TRP cation channels. Mol Cell. 2002;9:229–231. doi: 10.1016/s1097-2765(02)00448-3. [DOI] [PubMed] [Google Scholar]
- 11.Santoni G, Farfariello V. TRP channels and cancer: new targets for diagnosis and chemotherapy. Endocr Metab Immune Disord Drug Targets. 2011;11:54–67. doi: 10.2174/187153011794982068. [DOI] [PubMed] [Google Scholar]
- 12.Sun H, Shen F, Wu M. TRPC Mediates the proliferation of hepatocellular carcinoma cell. Tumor. 2006;26:396–401. [Google Scholar]
- 13.Putney JW., Jr New molecular players in capacitative Ca2+ entry. J Cell Sci. 2007;120:1959–1965. doi: 10.1242/jcs.03462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rychkov G, Brereton HM, Harland ML, Barritt GJ. Plasma membrane Ca2+ release-activated Ca2+ channel with a high selectivity for Ca2+ identified by patch-clamp recording in rat liver cells. Hepatology. 2001;33:938–947. doi: 10.1053/jhep.2001.23051. [DOI] [PubMed] [Google Scholar]
- 15.Xue Q, Wang Z. Ca2+ apoptosis and drug regulation. Chin Gen Pract. 2009;12:1126–1127. [Google Scholar]
- 16.Berridge MJ, Lipp P, Bootman MD. The versatility and universality of calcium signaling. Nat Rev Mol Cell Biol. 2000;1:11–21. doi: 10.1038/35036035. [DOI] [PubMed] [Google Scholar]
- 17.Wang J, Sun Y, Song R, et al. Cadmium induced apoptosis in rat hepatocytes by calcium overloading. Acta Veterinaria et Zootechnica Sinica. 2011;42:1168–1174. [Google Scholar]
- 18.Liu SH, Lin CY, Peng SY, et al. Down-regulation of annexin A10 in hepatocellular carcinoma is associated with vascular invasion, early recurrence, and poor prognosis in synergy with p53 mutation. Am J Pathol. 2002;160:1831–1837. doi: 10.1016/S0002-9440(10)61129-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van de Graaf SF, Hoenderop JG, Gkika D, et al. Functional expression of the epithelial Ca2+ channels (TRPV5 and TRPV6) requires association of the S100A10-annexin 2 complex. EMBO J. 2003;22:1478–1487. doi: 10.1093/emboj/cdg162. [DOI] [PMC free article] [PubMed] [Google Scholar]