Abstract
A human-systems perspective is a fruitful approach to understanding home health care because it emphasizes major individual components of the system – persons, equipment/technology, tasks, and environments –as well as the interaction between these components. The goal of this research was to apply a human-system perspective to consider the capabilities and limitations of the persons, in relation to the demands of the tasks and equipment/technology in home health care. Identification of challenges and mismatches between the person(s) capabilities and the demands of providing care provide guidance for human factors interventions. A qualitative study was conducted with 8 home health Certified Nursing Assistants and 8 home health Registered Nurses interviewed about challenges they encounter in their jobs. A systematic categorization of the challenges the care providers reported was conducted and human factors recommendations were proposed in response, to improve home health. The challenges inform a human-systems model of home health care.
Keywords: Healthcare, Human-Systems, Human Factors
1 Introduction
Health care is moving from the hospital to the home. Home health care is described as a range of medical and therapeutic services delivered at a care recipient’s home for the purpose of promoting, maintaining, or restoring health or maximizing the level of independence, while minimizing the effects of disability and illness, including terminal illness (Jones et al., 2012). Providing health care services in the care recipient’s home is becoming a necessity due to expedited hospital discharge and ongoing care plans. With the aging of the baby boomer generation (Administration on Aging, 2006), and the increasing life expectancy for people in developed countries (National Center for Health Statistics, 2005) t people are at risk for experiencing chronic age-related health declines for an extended period of time.
Home health care offers advantages over hospital-based health care, for example home health care may be more cost effective than that provided in a hospital (Naylor et al., 1999) and may reduce exposure to hospital-associated infections (Leff et al., 2005). Furthermore, home health care supports aging in place and independence, which are important for the quality of life for older adult care recipients.
However, understanding the needs of care providers and care recipients is necessary to optimize the health care services provided in the home. The goal of this work was to use qualitative methods to explore home health care from a human-systems perspective. Improvements to home health care will contribute to the health care system as a whole, but also hold the promise of providing effective treatment, quality of life, and comfort for care recipients.
2 A Human-Systems Approach to Understanding Home Health Care
A human-systems perspective is a beneficial approach to understanding home health care. This approach emphasizes the interaction between individual components of the system, specifically persons, tasks, equipment/technology, and environments –as well as the interaction between these components. A human-systems perspective also considers safety, effectiveness, and efficiency of the system as a whole, which is particularly applicable due to the complexity of the components that comprise home health care.
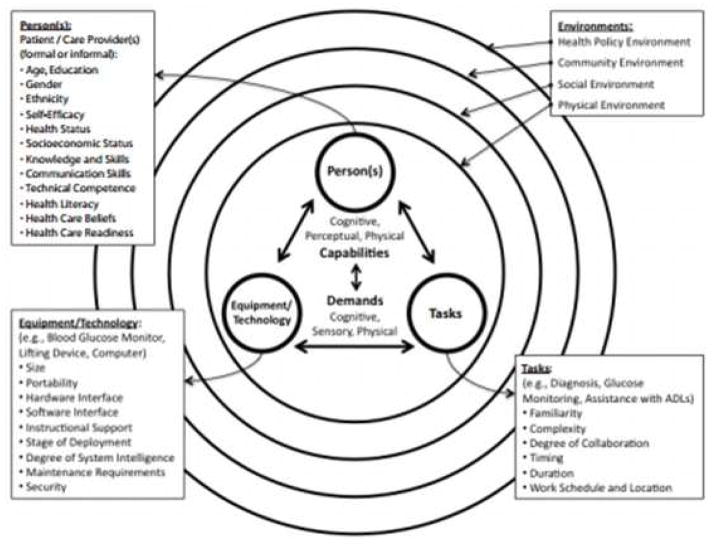
There has been limited application of human-systems knowledge to the home health care domain; however, the National Research Council (2011) released a proposal to apply human-systems and human factors to home health care, recommending the model presented in Figure 1. The model categorizes the components of the system – persons, tasks, and equipment/technology – with the multiple environments represented by overlapping circles (e.g., health policy, community, social, and physical). Persons, task, equipment/technology, and environments have characteristics that act as barriers and facilitators to the interaction of all of the components (represented by double arrows). A human-system perspective will consider the capabilities and limitations of the persons, in relation to the demands of the tasks and equipment/technology; thus, identification of mismatches between the person’s capabilities and the demands of providing care will provide a basis for proposing human factors interventions. The following sections provide an overview of each of these components.
Figure 1.
Model of human factors of health care in the home (National Research Council, 2011).
2.1 Persons
The primary persons involved in home health care can be subdivided into two groups: the health care provider (formal or informal individuals providing health care) and the health care recipient (individuals receiving care). Note that family and friends who are not primary care givers are included within the social environment. In 1990, there were an estimated 288,000 professional home health care providers in the USA; in 2010 that number had increased to 1,081,000 (U.S. Census Bureau, 2012). There is a variety of formal care giver occupations, such as home health aides, nurses, physicians, pharmacists, therapists, and social workers. In particular, home health aides and home health registered nurses represent a significant proportion of all health care support occupations, comprising approximately 27% and 14%, respectively (US Bureau of Labor Statistics, 2012). Some home health aides are Certified Nursing Assistants (CNAs); their job requirements include primarily personal care tasks, such as assistance with bathing, toileting, and medication reminders/encouragement. Registered nurses (RNs) perform skilled nursing tasks, such as using medical devices and equipment, wound care, and medication management.
The number of home health care recipients (i.e., patients) has increased from 2.5 million in 2002 to 3.4 million in 2010 (Medicare Payment Advisory Commission, 2012). The majority (70%) are 65 years of age and older (U.S. Dept. of Health and Human Services, 2000). The consequences of the growing older adult population for the health care system are substantial. With the aging of the baby boomer generation, more services will be required for the treatment and management of chronic and acute health conditions at home, especially those most prevalent with aging (CDC, 2004): hypertension, arthritis, heart disease, cancer, diabetes, and stroke.
2.2 Tasks
A variety of tasks are performed in home health care, with their successful completion dependent on the capabilities of the care provider to handle the task demands. Home health care tasks range in complexity, from simple tasks such as taking a care recipient on a walk to cognitively-challenging tasks (e.g., managing complex medication regimens) and physically-challenging tasks (e.g., bathing, toileting, transfer). Home health care tasks can be broadly categorized as health maintenance, episodic care, chronic care, and end of life care (The National Research Council, 2011). A description of these types of care and examples are provided in Table 1.
Table 1.
Home health care task descriptions and examples.
| Type of care | Description | Examples tasks required for care |
|---|---|---|
| Health Maintenance | Self-help and self-care activities that promote general health and well being |
|
| Episodic Care | Medical care required for short-term illness or condition |
|
| Chronic Care | Medical care required for long-term illness or condition; requires long-term lifestyle changes |
|
| End of Life Care | Medical care required when care recipient is dying; focus on maintaining comfort |
|
Tasks commonly performed for older home health care recipients included skilled nursing services, physical therapy, assistance with activities of daily living (ADLs), homemaker services, occupational therapy, wound care, and dietary counseling (CDC, 2012). These tasks require physical, cognitive, and perceptual skills on the part of the care provider. These tasks also require communication skills, including the ability to provide emotional support to the care recipient. For example, medication management is cognitively demanding (Lippa et al., 2008), compounded by multiple medications, side effects, and schedules. Unfortunately, many older adults have multiple health problems, and therefore have complex medication regimens. Bathing and wound care require simultaneous physical actions to promote balance, reach, flexibility, and proper hygiene (Murphy et al., 2007; The National Research Council, 2011). Given the challenges of health care tasks, it is necessary to evaluate both the task demands and the capability of the care providers to determine potential for adverse outcomes.
2.3 Equipment and Technology
Many home health care tasks require the use of technology and equipment by the health care providers as well as the care recipients. Innovations in technology have allowed a range of health care devices and tasks to move from the hospital to the home. However, much of the medical equipment used in home health care was designed by manufacturers to be used only in clinical settings by trained professionals (U.S. Food and Drug Administration, 2010). Examples include medication administration equipment, durable medical devices (i.e., hospital beds, wheelchairs), infusion pumps, dialysis machines, feeding tubes, catheters, Hoyer lifts, defibrillators, ambulation aids, blood glucose meters, and oxygen tanks. In an analysis of adverse events in the home (Marion, 2007), problems with infusion pumps, hospital beds, ventilators, and powered wheelchairs were reported – suggesting that the most complex medical equipment carried the highest risk of injury.
2.4 Environment
Finally, it is impossible to consider the interaction of persons, tasks, and equipment/technology without consideration of the environment in which these components are interacting; namely, the home. The home environment differs in many ways from the controlled environment of a hospital or clinic. This imposes unique challenges, because each home a health care worker visits is different and may hinder their ability to provide adequate care. Many homes may not meet electrical codes, controlled temperature, lighting, or sanitary requirements critical in providing safe and effective care. Interview with home health care subject matter experts revealed that challenges in the home environment not only included environmental factors (i.e., crowded or dimly lit surroundings), but also socio-environmental factors such as family over- or under-involvement or access to support from other professional caregivers (McBride et al., 2011).
3 Goals of Research
A human-systems perspective, such as the one provided in Figure 1, is a fruitful approach to understanding home health care because it emphasizes individual components of the system – persons, equipment/technology, tasks, and environments –as well as the interaction between these components. To date, there has been limited application of human-systems knowledge to the home health care domain. The overarching aim of this research was to use the systems model to frame the challenges discussed by the health care providers in the interviews. The intention was not to validate or test the model; rather this qualitative research was conducted to investigate in depth the trends patterns of challenges, and add to the conceptual framework. In other words, the purpose of this research was to provide a descriptive account of how the human-systems perspective provides structure and insight into challenges related to home health care. Specific goals were to:
Goal 1: Identify challenges home health care providers encounter in the home.
Goal 2: Consider how these challenges fit within a human factors and systems model of home health care.
Goal 3: Propose potential human factors solutions for those challenges.
We designed a structured interview, wherein professional home health care providers reported challenges they encountered within the context of seven tasks: medication management, transfer (sometimes ambulation was also discussed in relation to this task), bathing, toileting, wound care, infusion pump, and device use. This research is part of a large project, and preliminary results have been published (Beer et al., 2011; McBride et al., 2011, 2012; Mitzner et al., 2009). The current report differs from previous publications by:
including additional data, particularly data collected from interviews with RNs, and discussion of device use;
reporting additional analyses to assess artifact-specific challenges, the role of affect, and differences between RNs and CNAs;
including the results from seven commonly performed care tasks to move toward a more complete understanding of home health care;
synthesizing the results to add to the human factors model in Figure 1;
and, discussing the identified challenges and the potential for human factors interventions.
In sum, the results contribute to a better understanding of home health care from a human-systems perceptive, and provide potential human factors interventions supported by data collected from professional home health care providers.
4 Method
4.1 Home Health Care Providers
We interviewed eight CNAs and eight RNs, which is a reasonable sample size for our research goals and qualitative methodology (Marshall, 1996). The providers were recruited via word of mouth and study advertisements from local home health care agencies and Craigslist.org postings. They were given monetary compensation for their participation. The providers represent home health workers from an urban area of the southeast United States. Approval was obtained for the sessions to be audio recorded, and providers were aware that no information about their participation in the study was to be shared with their managers or supervisors.
For care providers to be eligible for the study they had to have at least one year of experience in home health care with older adults, and speak English as their primary language. The care providers were diverse in gender (12 female, 4 male) and race (4 Caucasian, 10 Black/African American, 1 multi-racial, and 1 unreported). Details regarding their education and job experience are reported in Table 2. Most of the home health care providers worked full time, and one provider was recently retired.
Table 2.
Demographics for Home Health Care Providers
| Provider | Age (years) M (SD) | Education | # Care recipients per week | Home health experience (years) M (SD) |
|---|---|---|---|---|
| Certified Nursing Assistants | 37.50 (10.36) | Vocational training or higher | 1–5 | 4.25 (3.69) |
| Registered Nurses | 47.25 (12.85) | Associates degree or higher | 6+ | 8.88 (7.49) |
4.2 Materials
4.2.1 Questionnaires
Standard materials (Czaja et al., 2006) were used for collecting demographic and health information. Additional questions were added to collect specific information related to the provider’s training, education, and employment history.
Providers also completed questionnaires to collect information on the frequency with which they performed various home health care tasks and challenges encountered for each task (the full set of these questionnaires can be requested from the first author).
4.2.2 Semi-structured interview script
The interview script was designed to assess challenges the home health care providers encountered when performing their job. A needs assessment (i.e., literature review, interviews with subject matter experts, and pilot testing) provided the basis for the script development by suggesting relevant tasks to discuss and wording for questions. The script was piloted with four CNAs to ensure that the discussion questions were clear and prompted discussion relevant to the issues of immediate interest (see McBride et al., 2011, for an overview of the needs assessment).
We chose seven home health care tasks to serve as context for the interview. These tasks were carefully chosen to represent the range of home health task types: health maintenance, episodic care, and chronic care. Additionally, they were chosen based on the frequency with which they are performed, as well as the likelihood they prove to be challenging for the providers (McBride et al., 2011). Each health care provider discussed only five of the seven tasks. The tasks of medication management, device use, and ambulation/transfer were discussed by both CNAs and RNs. The remaining two tasks were either CNA or RN specific, with CNAs discussing toileting and bathing, and RNs discussing wound care and infusion pumps. The counterbalancing of these tasks is displayed in Table 3.
Table 3.
Counterbalancing of tasks included in structured interview.
| Task | Task | Task | Task | Task | |
|---|---|---|---|---|---|
|
| |||||
| CNA1 | Bathing | Toileting | Med management | Device use | Transfer |
| CNA2 | Toileting | Bathing | Transfer | Med management | Device use |
| CNA3 | Bathing | Toileting | Device use | Transfer | Med management |
| CNA4 | Toileting | Bathing | Med management | Device use | Transfer |
| CNA5 | Bathing | Toileting | Transfer | Med management | Device use |
| CNA6 | Toileting | Bathing | Device use | Transfer | Med management |
| CNA7 | Bathing | Toileting | Med management | Device use | Transfer |
| CNA8 | Toileting | Bathing | Transfer | Med management | Device use |
| RN1 | Wound care | IV/ Infusion pump | Med management | Device use | Transfer |
| RN2 | IV/ Infusion pump | Wound care | Transfer | Med management | Device use |
| RN3 | Wound care | IV/ Infusion pump | Device use | Transfer | Med management |
| RN4 | IV/ Infusion pump | Wound care | Med management | Device use | Transfer |
| RN5 | Wound care | IV/ Infusion pump | Transfer | Med management | Device use |
| RN6 | IV/ Infusion pump | Wound care | Device use | Transfer | Med management |
| RN7 | Wound care | IV/ Infusion pump | Med management | Device use | Transfer |
| RN8 | IV/ Infusion pump | Wound care | Transfer | Med management | Device use |
For each task, the same set of questions was asked (the full script is available upon request). We first asked:
“What is the perfect process or procedure for completing the task of ________?”
The purpose of this question was to gain an understanding of the steps required to complete the task. We then asked:
“Please think about each step of the process or procedure. What frustrations or challenges did you encounter when performing the task of ________?”
“Please describe an example where the perfect process or procedure did not occur when performing ________?”
These questions were designed to encourage providers to discuss the nature of the challenges encountered on the job for each task. Finally we asked:
“Do you have any ideas about how this task could be made easier?”
The purpose of this question was to assess the providers’ perceptions of how the task could be improved and challenges alleviated. This question was followed up by a discussion of instruction/training, which is not the focus of the present paper (discussed in McBride et al., 2012).
4.3 Procedure
Prior to participation, the health care providers completed a telephone prescreening interview, which included questions about their home health experience with older adults and education to ensure they met study requirements. When eligible, providers were mailed the questionnaire set to complete prior to the interview.
The structured interviews took place either in person in a university conference room or over the telephone, and lasted a maximum of three hours. Providers gave informed consent. Next, the interviewer summarized the general goals of the study and nature of the discussion. Then, each provider discussed a total of five tasks1 (counterbalanced). After completion of each task discussion, providers were provided a break. When discussion was completed, the providers were debriefed and paid $66 for participation. Discussions were audio recorded for later transcription.
5 Results
5.1 Overview of coding and analysis of interview data
The audio recordings were professionally transcribed verbatim with personal information omitted. Transcripts were segmented into units of analysis by the primary coders. The focus of the segmentation was to identify difficulties encountered in the job. A segment was defined as a statement or description that included the following dimensions: 1) Goal, for example to transfer a person from a bed to a wheelchair; 2) Challenge, for example the care recipient was too heavy to move; and/or 3) Solution, for example the care provider asked another person to help. For a statement or description to be segmented into a unit of analysis, two of the three aforementioned dimensions had to have been mentioned. Each segment was coded on each of the three dimensions: goal, challenge, and solution (if one of the dimensions was not present, then it was coded as “not mentioned”).
The challenges were coded by categories derived from the human-systems perspective (Figure 1); specifically persons, artifacts (equipment/technology), tasks, and environment. The coding scheme was developed by reviewing a random sample of the transcripts and extracting common themes, as well as including themes from previous studies (Beer et al., 2011; McBride et al., 2011, 2012; Mitzner et al., 2009). Coders were calibrated by conducting 2 rounds of independent coding on the same 4 randomly selected transcripts, and then a third round of coding on 2 new randomly selected transcripts. Each round was followed by discussion of discrepancies and revision to the coding definitions. The final round of reliability resulted in an average of 75% agreement between the 3 coders. The remaining transcripts were divided among the 3 coders to code independently.
The dimension “challenge” yielded the majority of the results. These comments captured well the difficulties of the health care providers’ job from a human-systems perspective and the potential for human factors interventions. Therefore, the reported challenges are the focus of the results presented here. The following results are organized based on the human-systems coding scheme. First, challenges related to persons are reported, split between the care recipient and the care provider. Next, artifacts (i.e., equipment/technology) are presented. Lastly, the challenges related to the environment and the broader health care systems are reported. Interactions between these categories are presented throughout. For example, tasks, part of the human-system model (Figure 1), were used as context in the structured interviews; thus, the impact of task is discussed in each section.
5.2 Challenges Related to the Care Recipient
The “Care Recipient” category was used when the care recipients’ health-related declines or emotional stress were stated as the source of the difficulty. Such challenges were coded as affect, cognitive lack of knowledge, cognitive impairment, or physical limitation (see Table 4 for definitions, examples, and frequency). These challenges do not suggest that the care recipient themselves is the source of the challenge. Rather, the care recipients have particular needs related to their state of health, which they have no control over. Thus, these challenges are reported as the care recipient needs, and the providers’ reported attempts at meeting these needs within the context of home health care.
Table 4.
Recipient codes.
| Recipient Code Category | Definition | Examples | # of Codes Among CNAs | # of Codes Among RNs |
|---|---|---|---|---|
| Affective | The care recipient’s experience of mood or feelings | Care recipient’s frustration, preferences, attitudes, or embarrassment | 70 | 21 |
| Cognitive lack of knowledge | Information and skills acquired through the care recipient’s experience or education | Care recipient’s experience of confusion (not cognitive impairment), or not understanding terminology, steps, or procedure. | 4 | 11 |
| Cognitive impairment /memory limitation | The care recipient’s cognitive state and ability to remember | Care recipients dementia, cognitive impairment, or some other limitation in mental action | 7 | 8 |
| Physical | The care recipient’s fitness and ability to exert physical actions | Care recipient’s limitations in the recipient’s strength, reach, or balance | 68 | 46 |
When the source of the difficulty was related to the care recipient needs, both RNs and CNAs attributed the difficulty most often to the care recipient’s affective and/or physical limitations. CNAs reported almost twice as many difficulties stemming from the care recipient needs as RNs, yet the pattern was similar across code categories. Difficulties attributed to a characteristic of the care recipient needs were reported across all of the tasks discussed in the interviews, which is an important point because these are frequently performed tasks.
5.2.1 Affective Challenges
An unexpected finding was the frequency of challenges related to the care recipient’s affect. Affective challenges included instances where the care recipient’s emotions (e.g., fear), preferences (i.e., preference for hot bathing water), or attitudes (e.g., noncompliance) were discussed by the care provider. Affective challenges undoubtedly emerge because of the emotional aspects of care giving. Care recipients not only need to heal physically, but also deal with the emotional ramifications of health issues, as illustrated by these comments:
“Depression…interferes with them doing anything, so you know based on where is that patient coming from. They’ve just been told they have cancer...”
“Depression is I don’t want to get up. I don’t care. I’m going to die anyway you know.”
“Depression is a big factor in a lot of these situations.”
The providers reported that in addition to care recipients being upset about their condition, they may also become combative or noncompliant. While noncompliance was mentioned for many of the tasks in the interview, it was particularly evident in the discussions of medication management, where care recipients were resistant to taking their prescribed medication. The providers indicated that to overcome this challenge, they relied on encouragement and positive feedback.
“There’s a lot of patients that they do not want to take the medication because they think that you’re -- they don’t trust you, they think you’re trying to poison them, um, whatever is in their mind.”
“The only frustration I have is when they just don’t want to take it [medication]. They say it makes them sick. Some of them say it makes them sick and you know -- or they just don’t want to take it... So just try to encourage them...”
Care recipient affective challenges were more often reported by the CNAs compared to the RNs. This may be due, in part, to the fact the CNAs generally perform tasks that are more physical in nature. Physical challenges were often compounded by the care recipient’s fear and/or depression and physical weakness (e.g., resulting from long hospital stays, lack of ambulation when caregiver is not present).
“The willingness …to do what they need to do [for task of transfer]. And they’re afraid they’re going to fall or something, so they don’t want to try because of that fear or that type thing.”
“I encourage. I encourage. I encourage and I say well you know I know you don’t feel well today, but I think if you sit up...you’ll feel a little bit better... So again you’re back to kind of forcing them, but they have rights if they don’t want to get up, they don’t have to get up. But it’s our job to try to get them out of that bed or at least get them sitting up in bed.”
The CNAs also reported that comfort and preferences play a role in the task of bathing. Because bathing is a private task, some care recipients may be uncomfortable with receiving care. Additionally, providers reported that some older adults have very specific preferences for water temperature, soap or shampoo preferences, or a fear of water.
“Trying to get them in the bathtub. That is the most problem because some of them are afraid of water.”
“And you know if they’re comfortable with you, the task is easy you know. But if they’re not comfortable or you’re new or they’re use to one particular caregiver, then it’s difficult because they’re not comfortable. So they’re not going to make your job easier at all.”
5.2.2 Cognitive Challenges
Cognitive challenges related to the care recipients needs include both cognitive impairment and cognitive lack of knowledge. Cognitive impairment included comments related to the care recipient having dementia. This created challenges related to the care recipient being unable to understand care tasks.
The RN providers mentioned difficulties that fell in all of the code categories, suggesting that there is a range of challenges that are caused by care recipient’s cognitive characteristics. In particular, the cognitive challenges of medication management were primarily related to the care recipient’s lack of knowledge (e.g., lack of knowledge with medication regimen, side effects).
“It’s just hard to teach people to throw medications away that are expired, [and to not] duplicate what they’re taking.”
“[The] biggest problem is I guess trying to get people to understand that there’s a brand name and a generic name for drugs and that they cannot base the purpose of their drugs on colors. I think that is especially with the older adults they learn their medications well they think they learn their medications by colors... you have to really really really stress to them that that is not the appropriate way to learn their medications because with your different manufacturers come different colors and different colors for the same drug.”
5.2.3 Physical Challenges
The physical challenges were those the providers perceived or observed the care recipients encountering. Not surprisingly, more physical challenges were reported by the CNAs than the RNs, as CNAs typically perform more physically challenging tasks.
Of the reported challenges mostly attributed to physical needs of the care recipient, CNAs mentioned that they occurred in relation to bathing, toileting, and transfer. This was particularly evident, for example, when the care recipient was obese; “Turning them on their side if they’re obese for example.” The size and weight of the older adult influenced the ease with which they could easily move or transfer for these tasks.
One theme that emerged was that challenging affective and physical needs of the care recipient often occurred in tandem, particularly for the tasks of transfer and bathing. For example, affective reactions such as fear or noncompliance would lead to physical challenges, such as tensing of muscles, less focus on balance, or stiffness. One CNA described:
“Back to rejections if they reject you when you try to get them cleaned up, they get very stiff and they won’t move their arms or legs or anything and that’s the challenging part. You know, not want to move, but like I said you’ve got to get them calm and let them know you are there for them, and you won’t leave them or harm them or anything.”
For the RNs, challenges during wound care were mostly attributed to physical needs of the care recipient. Providers spoke of challenges caused by the size of the care recipient with respect to being able to reach wound sites, secure bandages or position them correctly for a wound to heal. For example,
“You get a lot of obese patients or if the wound is in a difficult area to get to.”
“The wound [is] progressing, getting worse because [the family members] are not making the [care recipient] roll off of it, because they are uncomfortable when they have to lay on their left or right side.”
Device use challenges were mostly attributed to physical needs of the care recipient for both CNAs and RNs. They expressed difficulties due to the weight/size of the care recipients, lack of care recipient mobility, compounded by risks due to using a device in isolation, for example:
“You really don’t know that you have that client’s weight until you’re both standing up and the [wheel]chair is not around you know. So sometimes you think you got them, and you’re standing up and you’re like okay, well he’s a little bit heavier than I thought.”
“And they taught me when I got my first CNA job you’re not supposed to use that Hoyer lift by yourself because it could very easily -- the patient could drop from the Hoyer…if a patient is not movable whether it be because of their legs or whatever...you know the Hoyer lift is a challenge because you’re there by yourself. If you drop that patient, you’re in trouble.”
Finally, physical challenges related to the care recipient needs were also discussed by the RNs in relation to medication management. However, these physical characteristics were related to vision impairment or tremors.
“Now whether people can read it or see it, you know, because some of them have the vision problems and some of your elderly can’t read...”
“This one particular person had Parkinson’s. And you’d go back and he would have spilled all the pills and have them all messed up and stuff.”
5.3 Challenges Related to the Care Provider
The “Provider” category was used when a characteristic of the care provider was identified as the source of the difficulty. Similar to the “Care Recipient” category, any mention of a challenge associated with the care provider was assigned one of four codes (i.e., affect, cognitive lack of knowledge, cognitive impairment, or physical limitations; see Table 5).
Table 5.
Provider codes.
| Provider Code Category | Definition | Examples | # of Codes Among CNAs | # of Codes Among RNs |
|---|---|---|---|---|
| Affective | The care provider’s experience of mood or feelings | Care provider’s frustration, preferences, attitudes, or embarrassment | 8 | 7 |
| Cognitive lack of knowledge | Information and skills acquired through the care provider’s experience or education | Care provider’s experience of confusion (not cognitive impairment), or not understanding terminology, steps, or procedure. | 2 | 11 |
| Cognitive impairment / memory limitation | The care provider’s cognitive state and ability to remember | Care provider’s dementia, cognitive impairment, or some other limitation in mental action | 0 | 0 |
| Physical | The care and ability to exert physical actions | provider’s fitness the recipient’s strength, reach, or balance | Care provider’s limitations in 13 | 5 |
Challenges related to the provider (whether it be affect, cognition, or physical limitations) were infrequently mentioned. This may be due, in part, to the provider’s sense of duty towards the job. When providers were discussing challenges, comments such as “But that’s my job”, “You do the best you can”, and “…but as long as the patient gets what they need you just go through it and you don’t think about it” suggested that the care-providers considered some of these types of challenges as a necessary aspect of their job rather than an issue to be remedied.
5.3.1 Affective Challenges
With regard to challenges related to the care provider’s affective state, the nature and number were similar for CNAs and RNs. They discussed affective challenges related to the task of transfer with both providers discussing fear and frustration associated with using a Hoyer lift. In particular, fear was associated with dropping a care recipient and causing bodily harm. This fear was linked, in part, to the fact that the providers work in isolation. If a fall were to happen, then help may not be readily available, thus increasing the frustration and fear associated with the task.
“But he [the care recipient] would just keep wiggling and keep wiggling [out of Hoyer lift] until he would be on the floor and I find situations like that frustrating because - especially when you have no one - I would have to call downstairs and get some[one]...”
5.3.2 Cognitive Challenges
The care providers did not mention cognitive challenges regarding their own cognitive impairment or memory limitations. However, there were mentions related to lack of knowledge, which is a cognitive issue. Lack of knowledge was mentioned more frequently by RNs than CNAs, with most comments being device use related. Specifically, RNs reported issues related to not knowing how a particular device functioned or was operated.
“...there are so many different kinds on the market and you don’t always know what type of infusion pump you’re going to be involved with until you get to the home.”
“... usually when your trained on a device the rep that comes in will show you that one particular device ... as you encounter new devices they basically have the same [use] but you can read the instructions quickly teach you how to get it started.”
“...depending on where you’re working, the pump can be different than what the company used so basically you just have to familiarize yourself with the equipment that you were using... and it’s not that same one, you run into problems so you just have to know the equipment that you are working with and operate it accordingly.”
Another example of lack of knowledge was linked to a lack of communication between providers. The providers reported that at times they were unaware of a care recipient’s medication regimen, prescriptions, therapy, capabilities, or special doctor orders. One provider stated:
“I had a ... patient who was just getting out of the hospital who hadn’t walked, and I wasn’t aware that she hadn’t walked and at least about three weeks prior to me coming over for the admission….”
5.3.3 Physical Challenges
Again, the CNA providers discussed physical challenges more frequently than the RNs, which reflects the physically demanding nature of the tasks CNAs routinely perform. In particular, for bathing and transfer, CNAs mentioned challenges regarding limitations in their own physical stature, strength, and balance. CNAs reported concern of physically injuring their back while lifting or turning care recipients, particularly if the recipient was obese.
“It could be made easier if it was a two-person transfer you know versus a one ‘cause a one person transfer could easily hurt your back.”
“You wait until you get help because the patient’s safety is the most important thing and I’m a small type person...”
Physical challenges were also mentioned related to using devices for the task of transfer, for example Hoyer lifts. Although these transfer devices are intended to make the task easier, the CNAs reported that the devices are physically cumbersome to use without a second caregiver to assist with the task.
5.4 Challenges Related to Artifacts (Equipment/Technology and Supplies)
The “Artifacts” category was used when providers identified challenges associated with the devices and supplies being used by themselves or care recipients to complete care tasks. Although the model (Figure 1) defines this component as equipment/technology (i.e., medical devices), we broaden this term to artifacts, to not only include equipment and technological medical devices, but also supplies. For example, devices included products that were designed to be used repeatedly by providers or patients, and were not disposable. This included durable medical equipment (e.g., wheelchair, walker) or monitoring/measurement technologies (e.g., blood pressure monitor, blood glucose meter). Supplies included all the non-reusable or disposable products that may be used by providers and/or care recipients. This category included items such as medication, adult diapers, incontinence pads, and bandaging. Challenge associated with artifacts was assigned to a code category depending upon the specific nature of the challenges (see Table 6).
Table 6.
Artifact Codes
| Artifact Code Category | Definition | Examples | # of Codes Among CNAs | # of Codes Among RNs |
|---|---|---|---|---|
| Function and Design Features | The product does not function appropriately, or is lacking functions or design features | Wheelchair has little lift, shower chair uncomfortable, bed pads tear easily, diapers fit poorly | 18 | 5 |
| Setup | Some aspect of setting up the device or system for use is not done correctly, resulting in complications | Battery died, humidifier bottle is cross-threaded, infusion pump signals air in the line, medication reconciliation lacking, missing needed medication | 7 | 35 |
| Degraded Quality | The quality of the device or supply has deteriorated in some way | Device inaccurate or malfunctioning, medication expired | 14 | 12 |
| Other | Devices or supplies too expensive | 4 | 1 |
5.4.1 Function and Design Features
Comments in this category reflected that the design of the artifact did not sufficiently allow the provider to perform the task. The majority of comments was made by CNAs, and covered a wide range of devices and supplies. The most discussed issue centered on difficulties encountered using wheelchairs. Transferring care recipients into and out of wheelchairs was often reported as being complicated by the fact that the wheelchairs often had no lift or the wheelchair arms did not come off, making it difficult to safely get care recipients out of a seated position. For example, CNAs made comments such as:
“Some of them [wheelchairs] sit real low. …to get down that low and to get somebody who is maybe a lot heavier than you, you know, up and out of that chair, it’s kind of hard.”
“You know the arm rest was that high, and just imagine what the process is trying to like, you know, assist her with one arm to stand up, you know, from something so low…so it was like I don’t have no balance and no strength trying to lift you up this low.”
Another artifact that presented providers with numerous challenges was toileting supplies, such as incontinence undergarments and disposable bed pads. Providers discussed how care recipients were embarrassed and rejected wearing adult diapers because of their design, including their resemblance to infant diapers, the sound they made, and their bulky shape. One CNA also mentioned that even for care recipients who do wear adult diapers, some brands are poor quality and will seep feces into bed when worn overnight. The durability of the disposable bed pads used was also an issue. One CNA described the process of cleaning up after a care recipient had an accident in bed:
“And then the clean-up process is so hard. You know, trying to depend on really the bed pad and you know they rip and tear easy.”
The other comments related to the function and design of artifacts spanned multiple products and issues, such as the appearance and softness of shower chairs, the lack of stickiness in some tape used for wound care, the complexity and danger of transferring a person using a Hoyer lift, and blood pressure cuffs that could not fit on certain care recipients.
5.4.2 Setup
For many artifacts, some type of setup is required, either by the provider or by an outside third party, such as a device distributor. One of the primary devices for which setup was problematic was infusion pumps. Providers described situations in which an infusion pump signaled that air was present in the line, but they struggled to determine where in the line the air was because of a lack of feedback from the device. In some cases, they had to bleed medication through the line repeatedly, resulting in wasted medication. In other cases, providers indicated that they thought the pump alarm was a false-alarm, that there was no air in the line, but they still had to bleed the medication through until the alarm deactivated. For example, providers commented:
“The machine kept reading air in the line and I had to keep taking it down and thumping the line and trying to see where the air was and in fact I didn’t see any at all but I had to keep going through the process again probably about two or three good times before the system finally allowed for me to hang the fluid.”
“You think you’ve done it right but […] it keeps beeping because the machines are so sensitive that it keeps beeping and you have to try to figure it out or start all over or sometimes even change the tubing just to get it to work.”
Many devices also came pre-programmed from other organizations, such as a pharmacy, and providers had to double check the devices were correctly setup. As one provider described:
“It’s usually programming error or programming issues that we have if it’s set up by the pharmacy when they send them to us, sometimes it’s not the same as what’s on the bag, so you have to make sure that the order is what the doctor ordered, that it matches what the pump actually is than what the bag says it is.”
The other predominant issue related to setup was that providers did not have the required devices or supplies to perform their care tasks. For instance, one provider remarked:
“If a patient is on a special oral care protocol and they need a certain type of dressing, that dressing either hasn’t arrived in the mail or no one ordered it or they did not send them home from the hospital with it, so it’s just not available and you’re having to use something different…and do something different than what you were expecting to do when you got there.”
The majority of challenges with not having the appropriate supplies involved medication. Providers reported that in some cases the care recipient were missing or had too much medication or they were taking medication that they were no longer supposed to be taking. Providers reported that medication reconciliation, or the process of comparing a person’s new medication orders with all of the medications that the patient has been taking, was very difficult in the home setting. For example, providers commented:
“When you get to a patient’s home and you find out that they’ve been seeing 4 different doctors and none of the doctors know what each of the other doctors are prescribing and you have 50 different prescriptions and 4 of them are for the same thing...”
“The hospital doesn’t reconcile what they need to and they put them on something different and send them home then the patient feels like they’ve got to take what the hospital sent them home with along with everything they still had at home to begin with...”
“What the doctor is sending home as a list that they want the patient on, and this patient has maybe 10 or 12 more medicines that he has been taking up until the time he went to the hospital. So trying to get some sort of a list that’s appropriate for the patient to be taking and getting the doctor to understand that these other medicines were already here or the patient’s totally confused about what to take.”
5.4.3 Degraded Quality
Providers also described situations in which using an artifact was problematic because the item had deteriorated or failed in some way. For instance, some of the provider’s frustrations were that devices were simply, old, broken, or malfunctioning in some way. One provider described how many care recipients often have old, out of date equipment that is more likely to have problems:
“You know they’re going to get the oldest thing that’s out because most of the time most of the clients are on Medicare and Medicaid. So they’re going to get the oldest thing they have. So you know it could be something wrong with it. You never know.”
One specific device that numerous providers commented on was digital blood pressure cuffs. Many providers had the perception that the digital blood pressure cuffs gave less accurate readings compared to taking blood pressure manually with a stethoscope. For example, providers remarked:
“I kind of like the old manual kind. I feel like that’s a better reading to me. Most of my clients have the digital kind…I’ll use theirs, and if it doesn’t look right to me, then I’ll use mine that I have in my bag.”
“Well, because it’s electronic for one and you know, with electronic, it’s really not accurate.”
In addition to faulty devices, providers discussed cases in which the supplies provided by the care recipient and/or their family were unusable because they had not been properly stored and were contaminated:
“You’re having to try to remove, you know, a good dressing out of a box that’s, you know, practically contaminated with pests and you’ve already instructed the patient and the family members that you have to keep this in a clean and enclosed environment.”
The other type of supply that was often degraded was medication. Providers reported that many care recipients had expired medication that they continued to take. One provider reported:
“So it’s like a mess that muddling through to try to straighten so the patient won’t be taking all these duplicate medications or medications that have expired. They don’t understand they need to throw those away and get them in the toilet and flush them down, whatever.”
5.5 Challenges Related to the Health Care Environment
5.5.1 The Home Environment
Although the providers did not explicitly mention the home environment often, there were a number of themes related to the home that were discussed as interacting with persons, artifacts, and tasks. We provide an overview here of emerging themes. First, each home that the CNAs and RNs reported visiting is different and may hinder their ability to provide care. For example, CNAs expressed the need to maintain a sanitary environment. Whether the patient soiled the bathwater or soiled the bed during a bed bath, the goal of ensuring proper hygiene was reported as challenging. RNs discussed similar issues in regard to wound care, where an unclean environment could increase the risk of infection. Furthermore, the layout of the home placed temporal demand on already time-consuming tasks. In particular, bathing was reported as very time consuming, due, in part, to the amount of time required to transfer a patient from their bedroom to the bathroom, which may not be located near one another. One CNA provided an example of working with a patient during a three hour shift. If that patient needed a bath, then bathing had to be the first task completed because it took nearly two hours.
As health care moves from the hospital to the home, the interactions between a patient’s family and the health care providers become increasingly dynamic and complex. Family members at home have a greater influence, either positive or negative, on the patient’s daily activity and health care plan. CNAs and RNs described examples in which family members made home care difficult. For example, some family members were reported to make distracting comments and demands on the care recipient, such as “stop acting like this,” which can distract patients or even make them more upset. Similarly, there are times when the family members were too demanding on the care providers, expecting difficult tasks, such as bathing, to be performed every visit.
However, it should also be stressed that families can also serve a beneficial role. CNAs and RNs mentioned that a patient who does not want to comply with their medication regimen can sometimes be persuaded by a family member to take the medication.
5.5.2 Work Environment
It is important to consider the culture of home health work environment within the context of the larger health care system. Physical and emotional support systems provided by other health care professionals are inherent in hospitals and assisted living facilities. However, the home health care providers reported often working in isolation – an aspect of the work environment specific to home health care. In particular, many CNAs reported that they often need help, especially with physically demanding tasks such as lifting or moving patients, but there is no help available to them, oftentimes because agencies are understaffed or because the patient load is just too high to assign multiple CNAs to a single home patient.
Many of the CNAs reported using Hoyer lifts to reduce the physical challenge of transfer. However, the use of these devices was mentioned as being a challenge in itself, particularly when working alone.
“…and they taught me when I got my first CNA job you’re not supposed to use that Hoyer lift by yourself because it could very easily -- the patient could drop from the Hoyer…You know it’s very scary when you’re doing it by yourself because it could not work. It could fail.”
“If you don’t feel comfortable in that particular situation doing it by yourself, we just don’t do it [referring to ambulation].”
Additionally, Hoyer lifts are expensive and usually the patient could not afford to own or maintain one. Moreover, for many home health devices, providers mentioned the challenge ‘different home, different device.’ This requires the providers to learn how to use each device, particularly considering the likelihood of missing documentations, manuals, and guides. One CNA stated,
“…being that these devices [Hoyer lifts] are in the client’s home, they’re not going to get the new products. You know they’re going to get the oldest thing that’s out because most of the time most of the clients are on Medicare and Medicaid.”
An additional theme related to education about medications such the side effects or specifics of the regimen, which should fall under the responsibility of the care recipients’ physician/pharmacist. However, many CNAs reported not having enough training to provide adequate medication education they felt was needed by the care recipients.
6 Discussion
6.1 Considering Challenges in Home Health Care within a Human-Systems Approach
The original model of human factors of health care in the home (Figure 1, National Research Council, 2011) was not meant to be an exhaustive depiction of factors and characteristics to consider in home health care; not enough research had yet been conducted on this topic to create a comprehensive and complete model. However, it is important to build and contribute to existing models, to reflect the growing human-systems knowledge on and study of home health care. Our research provides a rich dataset of challenges in home health care by providing a vivid account of the front lines of home health care. A striking finding was the variability of the challenges the providers reported, providing insight into the demands of the job. Although there are many routine elements of the work, the care tasks discussed in this study do provide a surprising amount of challenges, complexity, and variability (Beer et al. 2011).
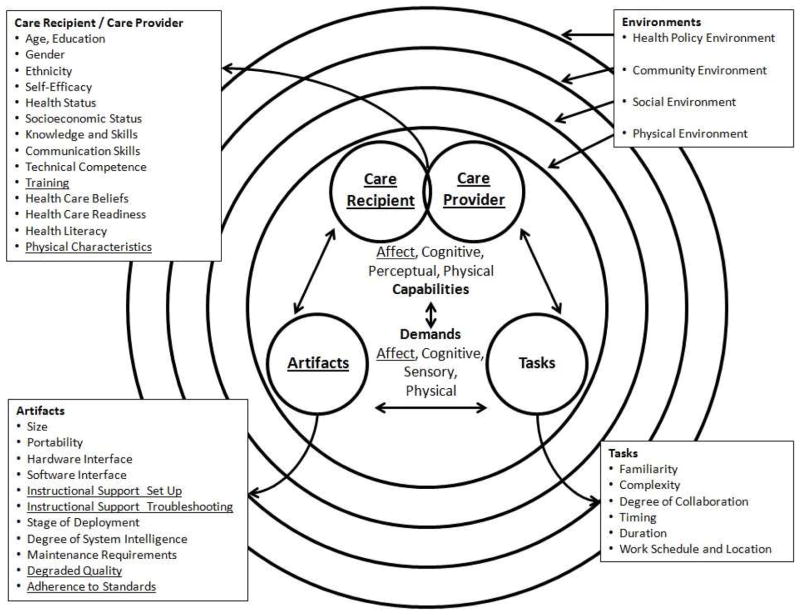
Many of the themes discussed in our results provide insight into the components of person(s) and equipment/technology, and can contribute additional factors to the human factors of health care model (Figure 1). A revised version of the model is depicted in Figure 2. The additions and modifications, based on the current research, are indicated by underlined text in the model. First, the person(s) component of the model has been divided into two circles to represent the care provider and the care recipient. It is important to differentiate these two primary person roles because person characteristics (e.g., education, knowledge and skills, communication) differ significantly between them (National Research Council, 2011). In addition person capabilities of the care recipient and provider interact with one another, as well as with other components of the model (e.g., tasks, environment).
Figure 2.
Updated Model of human factors of health care in the home (National Research Council, 2011). Additions indicated by underlined text.
Additionally, affect was added to the model as a care recipient and provider capability and demand. The role of affect as a care recipient or provider capability refers to their ability to convey and manage their mood or feelings (e.g., fear, frustration, preferences, cooperation). Affect also plays a role as a demand related to the task and artifacts used for that task. For example, bathing and toileting are highly emotional and intimate tasks, which provide additional privacy, confidentiality, and communication demands and challenges. Our data illustrate the emotional toll of home health care; suggesting the importance of health providers’ recognizing and handling one’s own and others’ emotions (Davies, Jenkins, & Mabbett, 2010). We found that health care providers interact with care recipients, often quite intensively, eliciting emotional attachment, as well as strife. Our findings contribute to previous literature investigating care providers’ relationships with care recipients; when direct care givers were asked what they find most satisfying about their job they said “the residents”, particularly the close, personal relationships (Kemp, Ball, Hollingsworth, & Lepore, 2010). Thus, managing and maintaining affective relationships and dynamics with care recipients was an important theme in our data.
The role of affect interacted with the fact that the care providers reported working in isolation. Both CNAs and RNs reported working alone, lacking in affective support from other care providers. This finding provides insight to the challenges in communication between home care providers and the rest of the health care system. Both RNs and CNAs often need to communicate with other health care providers, or with each other. However, lack of face-to-face contact with one another, as well as HIPPA regulations on communication of health information create challenges specific to home health care. Working in isolation also contributed to the physical strain care providers experienced. Physical characteristics of both the care provider and recipient were common trends in our data (see addition of physical characteristics in Figure 2). For example, the physical characteristics of the provider (e.g., strength) and the care recipient (e.g., weight) played a role in how difficult a task (e.g., transfer) was to complete, particularly when working alone. Physical and affective strain on the job has been cited as a contributor to high turnover, burnout, and lack of job satisfaction (Delp, Wallace, Geiger-Brown, & Muntaner, 2010; Erickson & Grove, 2007).
Training was also added to the list of characteristics in Figure 2. Training certainly impacts knowledge and skills (also listed as a characteristic), but refers specifically to the formal or informal instruction received by either the care provider and/or recipient. Finally, equipment/technology was renamed as artifacts. We propose this change because our results indicate that much of the apparatus the care providers and recipients interacted with include both equipment/technology as well as non-reusable supplies (e.g., bed pads, adult diapers, medication). The term ‘artifacts’ encompasses a broader array of such technology and supplies required for home health care. Under artifact characteristics, instructional support was split between set up and troubleshooting. Our results suggest that unique challenges arose for both set up and troubleshooting, and the steps required for these two processes differed. Degraded quality was also added to the model. This differs from maintenance, because eventually many artifacts decay in quality despite strict maintenance, such as expired medications, or general wear and tear on durable medical equipment. Finally adherence to standards was added to highlight the need for federal standardization in medical devices, and the adherence to such standards will be likely to impact the usability of the device itself.
6.2 Proposed Human Factors Interventions for Home Health care Challenges
When the providers were asked to describe current or future solutions to the challenges they encounter, a variety of answers were provided. Ideas such as new technology, better training, and standardized/professional instruction manuals (i.e., instead of hand-creating instructions for patients) were proposed. However, in general, the provider recommendations were very broad and thus will not be presented in detail. The providers recognized the potential for interventions, but lacked experience in providing specificity for exactly what would be of help. By taking a systems approach to understanding the challenges in home health care we, as researchers and human factors specialists, can provide preliminary guidelines for potential human factors interventions.
When considering human factors interventions, sometimes tasks can be modified to reduce demands, the technology design itself can be modified for safety and ease of use, or in other cases training can augment an individual’s knowledge and skills. Based on the challenges identified in this research, we identified interventions that could be particularly beneficial.
Physical, physical, and isolation supports
Many types of supports can reduce or mitigate physical, affect, and isolation challenges. Regarding physical support, proper use of Hoyer lifts, braces, and ergonomic lifting procedures (Owen, 2000) should be enforced. Furthermore, technology such as mechanical or robotic supports (e.g., mechanical hospital beds, chair lifts) could ease the physical strain of transfer tasks. Affect and isolation challenges could be addressed through use of telesupport systems. For example, telephone support groups, teleconferencing, or even telepresence systems (Beer & Takayama, 2011) have potential to promote communication between patients, health care providers, and their supervisors during home visits.
Home modification
Although the providers did not explicitly mention the home environment often, many of the challenges reported in this research can be mitigated through proper environmental design. Ensuring the home is modified for the purposes of health care is a beneficial approach to solving safety related issues. For example ensuring there is proper space (i.e., removing hazards), installing grab bars, stair lifts, ramps, and appropriate furnishings are examples of home modifications that can ease challenges encountered by both the care provider and recipient (Sanford, 2012).
Instructional material
Our data suggested that instructional material for set up and troubleshooting artifacts is largely lacking. No matter how much training a care provider receives on medical devices, new or unexpected complications can arise. Instructional material could be provided by the manufacturer to provide step-by-step instructions on how to deal with such events. Furthermore, instructional material could also be useful in assisting the care providers in training the care recipients. The providers in this study reported instructing and educating recipients on device use, medication side effects, and proper procedures for certain tasks (e.g., step-by-step procedure for getting in and out of bed). If instructional material was lacking, the providers reported they would sometimes create their own handmade instructions or diagrams. Proper human factors principles in both training and instructional design (Czaja & Sharit, 2012) can ensure that the providers are not misrepresenting a task or misinforming a care recipient with their custom made instructions. Creation of pamphlets, online instruction material, and “cheat sheets” are recommended. However, providers mentioned that sometimes instruction material can become lost; therefore, offering these materials online or physically connected to the device would be ideal.
Manufacturer standardization and regulations
One challenge repeatedly mentioned by providers was the notion of ‘different home, different device’. Care recipients may purchase medical devices themselves, and these products are available from a variety of Internet sources. The providers reported that artifacts (devices and supplies) were out of date, had missing instructions, or did not work properly. Few regulations address medical devices in the home (National Research Council, 2011). Thus adequate and standardized warning labels, icons, and design features are needed to ensure proper use. Furthermore, such warning labels, icons, and product design features should be developed with proper human factors for the aging population in mind (Fisk et al. 2009).
Training
The National Research Council report stated that “some device users in the home are formally trained caregivers, who have knowledge and expertise of and experience with such medical devices” (2011, p. 113), thus they should know how to properly use devices. Moreover, a CDC report (2011) stated that 82.2% of home health aides thought their initial training prepared them for their jobs. However our data suggested that the formally trained care providers interviewed in this study still encountered problems using devices. In fact, our data suggest that there is not enough training on device use for these professionals, particularly due to the variability in device design between different manufacturers. Untrained caregivers or novices (such as care recipients or family members) are more likely to misinterpret visual information and audible signals/warning emitted by a medical device. This places them at a higher risk of making an incorrect or inappropriate judgment in how to operate the malfunctioning device, or make an error in maintenance/repair to the devices. Training and continued education on how to set up and troubleshoot devices would be particularly beneficial to home health providers who encounter a wide range of devices from home to home.
6.3 Scope and Future Directions
In summary, a human-systems approach was a beneficial way to assess home health care. A goal of human-systems design is to achieve an ideal fit between artifact and task demands, and the human capabilities. When demands exceed an individual’s affective, cognitive, perceptual, and physical capabilities, then the likelihood of adverse events increase. Identifying exactly where these challenges exist makes possible the opportunity to develop human factors interventions, as we proposed. Improvements in home health care have the potential to provide increased well-being, comfort, and safety to both care givers and recipients alike. Through this research, we have identified a number of challenges in home health care, and opportunities for human factors researchers and developers to implement interventions.
This research took a qualitative approach to understanding home health care from a systems perspective. However, qualitative research has both strengths and weaknesses. Although our data provide an in-depth and insightful account of the challenges encountered by providers on the job, follow up research should investigate beyond self-report. Critical next steps to further develop the model in Figure 2 could include observational data and analysis of incident reports. Home health providers may only be self-reporting a fraction of challenges they encounter, or leaving out critical details. Furthermore, our study investigated two types of health care providers: CNAs and RNs. Both types of providers contribute greatly to the home health care system, but are only a portion of persons involved. Further research, taking a human-systems perspective, to identify human factors challenges encountered by physical and occupational therapists, speech therapists, and informal/family care givers would contribute greatly to the model. Finally, the human factors interventions, as proposed in this discussion, need to be thoroughly tested to ensure greater job performance, safety, and satisfaction. Nonetheless, the model presented in Figure 2 moves us a step closer to understanding home health. Further consideration of home health care from a human-systems approach holds promise of promoting positive change toward successful care.
Highlights.
We use a human-systems perspective to understand home health care
We qualitatively assess challenges home health care providers encounter
Affect was a commonly mentioned challenge, as well as a high level of uncertainty
These findings inform a revised human-systems model of home health care
Acknowledgments
This research was supported in part by a grant from the National Institutes of Health (National Institute on Aging) Grant P01 AG17211 under the auspices of the Center for Research and Education on Aging and Technology Enhancement (CREATE; www.create-center.org).
Footnotes
Except one provider who did not discuss all tasks due to time limitations
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Administration on Aging. A Profile of Older Americans: 2006. 2006 Retrieved from http://www.aoa.gov/PROF/Statistics/profile/2006/2006profile.pdf.
- Beer JM, Springman JM, McBride SE, Mitzner TL, Rogers WA. Needs assessment for certified nursing assistants providing personal care. Proceedings of the Human Factors and Ergonomics Society 55th Annual Meeting; Santa Monica, CA: Human Factors and Ergonomics Society; 2011. pp. 291–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beer JM, Takayama L. Mobile Remote Presence Systems for Older Adults: Acceptance, Benefits, and Concerns. Proceedings of the Human-Robot Interaction Conference; 2011. pp. 19–26. [Google Scholar]
- Centers for Disease Control and Prevention (CDC), National Center for Health Statistics, United States Department of Health and Human Services. Health Data Interactive. 2004 Retrieved January 7, 2008, from www.cdc.gov/nchs/hdi.htm.
- Centers for Disease Control and Prevention (CDC), National Center for Health Statistics, United States Department of Health and Human Services. Bercovitz A, Moss A, Sengupta M, Park-Lee EY, Jones A, Harris-Kojetin LD, Squillace MR. National health statistics reports: An overview of home health aides: United States, 2007. 2011 Retrieved from http://www.cdc.gov/nchs/data/nhsr/nhsr034.pdf.
- Centers for Disease Control and Prevention (CDC), National Center for Health Statistics, United States Department of Health and Human Services. Jones AL, Harris-Kogetin L, Valverde R. Characteristics and use of home health care by men and women aged 65 and over. 2012;52:1–8. Retrieved 27 June 2013 from: http://www.cdc.gov/nchs/data/nhsr/nhsr052.pdf. [Google Scholar]
- Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, Sharit J. Factors predicting the use of technology: Findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE) Psychology and Aging. 2006;21(2):333–352. doi: 10.1037/0882-7974.21.2.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czaja SJ, Sharit J. Aging and skill acquisition: Designing training programs for older adults. Boca Raton, FL: CRC Press; 2012. [Google Scholar]
- Davies S, Jenkins E, Mabbet G. Emotional intelligence: District nurses’ lived experiences. British Journal of Community Nursing. 2010;15(3):141–146. doi: 10.12968/bjcn.2010.15.3.46903. [DOI] [PubMed] [Google Scholar]
- Delp L, Wallace SP, Geiger-Brown J, Muntaner C. Job stress and job satisfaction: Home care workers in a consumer-directed model of care. Health Services Research. 2010;45(4):922–940. doi: 10.1111/j.1475-6773.2010.01112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson R, Grove W. Why emotions matter: Age, agitation, and burnout among registered nurses. Online Journal of Issues in Nursing. 2007;13(1) [Google Scholar]
- Fisk AD, Rogers WA, Charness N, Czaja SJ, Sharit J. Designing for Older Adults: Principles and Creative Human Factors Approaches. 2. Boca Raton, FL: CRC Press; 2009. [Google Scholar]
- Jones AL, Harris-Kojetin L, Valverde R. Characteristics and use of home health care by men and women aged 65 and older. United States Department of Health and Human Services - National Health Statistics Report. 2012;52:1–7. Retrieved from http://www.cdc.gov/nchs/data/nhsr/nhsr052.pdf. [PubMed] [Google Scholar]
- Kemp CL, Ball MM, Hollingsworth C, Lepore MJ. Connections with residents: “It’s all about the residents for me”. In: Ball MM, Perkins MM, Hollingsworth C, Kemp CL, editors. Frontline workers in assisted living. Baltimore, MD: The Johns Hopkins University Press; 2010. pp. 147–170. [Google Scholar]
- Leff B, Burton L, Mader SL, Naughton B, Burl J, Inouye SK, Greenough WB, Guido S, Langston C, Frick KD, Steinwachs D, Burton JR. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Annals of Internal Medicine. 2005;143(11):798–808. doi: 10.7326/0003-4819-143-11-200512060-00008. [DOI] [PubMed] [Google Scholar]
- Lippa KD, Klein HA, Shalin VL. Everyday expertise: Cognition and decision making in diabetes self-management. Human Factors. 2008;50:112–120. doi: 10.1518/001872008X250601. [DOI] [PubMed] [Google Scholar]
- Marion J. Medsun adverse event reports related to home health care devices. Medsun Newsletter. 2007:17. Retrieved from http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/medsun/news/newsletter.cfm?news=17.
- Marshall MN. Sampling for qualitative research. Family Practice. 1996;13(6):522–525. doi: 10.1093/fampra/13.6.522. [DOI] [PubMed] [Google Scholar]
- McBride SE, Beer JM, Mitzner TL, Rogers WA. Challenges for home health care providers: A needs assessment. Physical & Occupational Therapy in Geriatrics. 2011;29:5–22. doi: 10.3109/02703181.2011.552170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride SE, Beer JM, Mitzner TL, Springman JM, Rogers WA. Challenges of training older adults in a home health care context. Proceedings of the Human Factors and Ergonomics Society 56th Annual Meeting; Santa Monica, CA: Human Factors and Ergonomics Society; 2012. pp. 2492–2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy. 2012:211–206. Retrieved 6 June 2013 from the Medicare Payment Advisory Commission website: http://medpac.gov/documents/Mar12_EntireReport.pdf.
- Mitzner TL, Beer JM, McBride SE, Rogers WA, Fisk AD. Older adults’ needs for home health care and the potential for human factors interventions. Proceedings of the Human Factors and Ergonomics Society 53rd Annual Meeting; Santa Monica, CA: Human Factors and Ergonomics Society; 2009. pp. 718–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SL, Gretebeck KA, Alexander NB. The bath environment, the bathing task, and the older adult: A review and future directions for bathing disability research. Disability and Rehabilitation. 2007;29:1067–1075. doi: 10.1080/09638280600950694. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2005. 2005 Retrieved from http://www.cdc.gov/nchs/data/hus/hus05.pdf.
- National Research Council. Health care comes home: The human factors. Committee on the Role of Human Factors in Home Health Care, Board on Human-Systems Integration, Division of Behavioral and Social Sciences and Education; Washington, DC: The National Academies Press; 2011. [Google Scholar]
- Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA: The Journal of the American Medical Association. 1999;281(7):613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- Owen BD. Preventing injuries using an ergonomic approach. Official Journal of Association of periOperative Registered Nurses (AORN) 2000;72(6):1031–1036. doi: 10.1016/s0001-2092(06)61908-x. [DOI] [PubMed] [Google Scholar]
- Sanford J. Universal Design as a Rehabilitation Strategy: Design for the Ages. New York, New York: Springer Publishing; 2012. [Google Scholar]
- United States Bureau of Labor Statistics. May 2012 national industry-specific occupational employment and wage estimates: NAIS 621600-Home health care services. 2012 Retrieved 6 June 2013 from the Bureau of Labor Statistics website: http://www.bls.gov/oes/current/naics4_62100.htm.
- United States Census Bureau. Statistical abstract of the United States: Health and nutrition-Employment in the health service industries. 2012:162. Retrieved from http://www.census.gov/compendia/statab/cats/health_nutrition.html.
- United States Department of Health and Human Services. National home and hospice survey: Current home health care patients. 2000 Retrieved January 7, 2008, from http://www.cdc.gov/nchs/data/nhhcsd/curhomecare00.pdf.
- United States Food and Drug Administration, Center for Devices and Radiological Health. Medical Device Home Use Initiative. Washington, DC: 2010. Retrieved from http://www.fda.gov/downloads/MedicalDevices/ProductsandMedicalProcedures/HomeHealthandConsumer/HomeUseDevices/UCM209056.pdf. [Google Scholar]