Abstract
The dual global epidemics of crack cocaine use and HIV have resulted in a large number of people living with HIV who use crack cocaine, many of whom continue to engage in unprotected sex. Crack use also increases the rate of HIV progression. Consequently, there is an urgent need for effective interventions to decrease crack use and unprotected sex and to improve antiretroviral therapy (ART) adherence in this population. This article reviews the recent published literature on interventions for reducing crack use and unprotected sex among people living with HIV. Only a few intervention outcome studies targeting exclusively HIV positive crack cocaine users were identified, whereas other studies used a mixed sample. Some interventions focused on reducing crack use and several focused on reducing sex-risk behaviors. Consequently, there is a critical need for efficacious interventions that address crack use, risky sex and ART adherence among people living with HIV.
Keywords: HIV-positive crack users, interventions, outcomes, substance abuse, sexual risk, Behavioral Aspects of HIV Management, antiretroviral therapy, sexual risk behaviors
Introduction
In the early 1980s, the United States experienced an epidemic of crack cocaine use [1, 2]. Although currently it receives less media attention [3], crack cocaine use has not only become endemic in inner cities [1, 2], it has spread to rural areas in the United States [4] as well as to European [5, 6], African [7, 8] and South American countries [9]. Early in the epidemic, the trajectories of crack-using careers were undocumented. However, research has shown that for many users, crack use becomes a chronic relapsing condition [10, 11], with some similarities to opioid dependence [12]. Crack use, particularly as a chronic relapsing condition, also is associated with a broad range of physical, neurological and mental illnesses, as well as social instability [13, 14].
In addition, crack use has been linked to a variety of risky sex practices [15, 16] that place users at high risk of HIV [17, 18] and other sexually transmitted infections (STIs) [19, 18]. Some of the highest risk practices involve transactional sex in exchange for crack [20]. Male crack users tend to trade crack for sex [21], whereas female crack users tend to trade sex for crack [22, 23, 20]. However, it is not uncommon for male crack users, many of whom identify as heterosexual, to trade sex to other males for crack [24]. Crack use is also common among some groups of HIV-positive males who identify as gay or bisexual [25, 26]. In some areas, HIV prevalence among non-injecting crack users is higher than it is among people who inject drugs [27].
Polydrug use also is common among crack users and users of other drugs [28]. In addition to illegal drugs, there is considerable overlap between crack use and heavy alcohol use [29]. Using crack alone or in combination with other drugs has been associated with increased sex risk [30] and a variety of health problems [31], including the risk of HIV infection and in combination with alcohol a more rapid disease progression [32, 33]. It also has been associated with decreased adherence to antiretroviral therapy (ART) among people living with HIV [34].
As noted above, crack use has spread extensively over the past 30 years and continues to be an important driver of the HIV epidemic in many populations, including people living with HIV. During the late 1990s, a number of behavioral interventions were developed to reduce HIV risk behaviors among people who used crack cocaine [35, 36]. However, these interventions did not specifically target crack users who were HIV positive. Consequently, there is a critical need for efficacious interventions to reduce crack use and sexual risk behaviors and to improve ART adherence among people living with HIV.
Review of Recent Literature
To identify articles, we searched PubMed, CINAHL, Cochrane Library reviews, PsychInfo, and Sociological Abstracts for recently published articles that evaluated sexual risk reduction and crack cocaine reduction interventions for people living with HIV/AIDS (PLWHA). The search terms included a combination of the following: “HIV,” “HIV infections,” “HIV-seropositivity, “HIV-infected,” “interventions,” “prevention and control,” “primary prevention,” “sexual risk reduction,” “Crack Cocaine,” “Cocaine,” “Substance use,” “sexual behavior,” “risk reduction behavior.” We used the following criteria to limit our search findings: 1) the article must have been published in 2010 or later, 2) only PLWHA were included in the intervention sample, 3) the sample included at least some crack cocaine users or included participants that had (studies in which a urine positive drug screen for cocaine, 3) sex risk and/or drug use reduction were targeted as the interventions’ primary or secondary outcome measure. A thorough review of the abstracts eliminated articles which did not fit these criteria, and left 8 manuscripts to be included in this review. We also searched Elsevier’s SciVerse Scopus database to find additional articles that had cited the relevant articles that we located in the initial search. Additionally, we utilized the authors’ professional contacts to determine if we had missed any articles These approaches s did not yield any additional articles.
Our review of HIV prevention intervention studies published in 2010, 2011 or 2012 did not identify any reports of HIV prevention interventions designed to reduce both sexual risk and crack use in HIV-seropositive persons. Rather, the published reports on behavioral risk-reduction intervention studies described interventions that focused either exclusively on drug-use reduction or sex-risk reduction outcomes. The studies in this review are grouped and presented accordingly.
Evaluations of Substance Use Reduction Interventions with HIV- Positive Crack Users, Including Adherence Measures
We found three studies that reported the results of interventions which specifically targeted reducing drug use among HIV-positive people who use crack cocaine [37•, 38••, 39••]. Two of these tested approaches that targeted individual-level risk factors [37••, 39••]. One of these studies [39••] included measures of HIV medication adherence as an outcome. The third study tested an intervention that intervened on women’s social environment [38••]. The two studies that targeted individual factors are described first.
The first study was a pilot study that used a randomized controlled trial (RCT) to test “HealthCall,” an automated interactive voice response (IVR) system that collects participant information via touchtone or voice recognition response [37•]. The investigators hypothesized that this system would enhance the motivational interviewing (MI) [40] intervention by generating accurate personalized feedback based on participants’ daily self-reports on drug use and health behaviors. To test the efficacy of “MI+Health Call” as compared with “MI-only” in reducing non-injecting drug use, the study enrolled a racially mixed group of 40 HIV-positive, non-injecting drug-using males (n=20) and females (n=20) who were receiving primary care in an urban clinic. All participants received one, 20- to 25-minute MI session. In addition, the participants in the MI+HealthCall condition were instructed to call the HealthCall daily for the next 30 days. These data were then recorded, summarized, and provided as personalized feedback during the 3- and 6-month follow-up visits.
Crack cocaine use was the primary substance reported by the majority of the sample (76%), followed by heroin (15%) and methamphetamine (9%). Participants in the MI-only condition reported reducing their drug use from a mean of 10.2 days at baseline to 4.1 days at the 60-day follow-up interview, whereas participants in the HealthCall+MI condition reduced their drug use from a mean of 9.2 days at baseline to 2.0 days at the 60-day follow-up. Group differences in drug use were not statistically significant at P < 0.05; however, this was expected given the small sample size. The investigators observed moderate effect size, which provides some evidence that technologies such as IVR may a useful adjunct to substance use reduction interventions for HIV-positive people in a primary care setting.
The second study used a randomized design to examine whether or not a MI intervention enhanced with personalized feedback and relapse prevention skills (MI+) would be more efficacious than a video-delivered informational intervention at reducing drug use and improving highly active antiretroviral therapy (HAART) adherence [39••]. A majority of the 54 participants in the sample (28 men, 25 women, and 1 transgender person), were African American (82%), heterosexual (59%), and crack-cocaine dependent (92%). At baseline, adherence to HAART was less than 90%.
The MI+ intervention was based on the Informational Motivation Behavioral Skills (IMB) model [41]. Participants attended six, therapist-guided, individual MI sessions over a 5- to 6-week period. During these sessions, therapists trained in MI reviewed strategies such as selfmonitoring, exploring drug use and nonadherence triggers, and creating problem-solving plans with participants. Additionally, participants’ baseline data were used to tailor personalized feedback for use during discussions around goal setting, personal control and choices, and change planning. The participants in the comparison intervention (Video+) viewed six, 30- to 45-minute informational videos on crack cocaine and other drug use or HAART adherence. They attended a 10-minute debriefing session after each video.
Participants in both intervention conditions reported significant decreases in drug-related problems and days of cocaine use. Both groups maintained positive improvements on drug-related problems from the 3- to 6-month follow-up sessions. There were no significant differences between groups on drug use outcomes. The results of this study suggest that additional research should be conducted to investigate the efficacy of video-based interventions in this population. Considering the medium’s relative cost-effectiveness and portability, video-based interventions could potentially be disseminated widely.
The third study used an RCT design to test the hypothesis that an intervention which addressed psychosocial factors associated with HIV disease progression and substance use relapse, would reducel substance use and improve HAART adherence in HIV-positive females who were currently in recovery from substance abuse as compared with “Health Group,” a standard psychoeducational comparison condition[38••]. The sample consisted of 126 primarily of low-income minority women. The RCT tested Structural Ecosystems Therapy (SET) [42], a family-centered, eco-systemic intervention designed to target women’s social environment to improve drug use and HIV medication adherence outcomes by improving “adaptive” behaviors and reducing “maladaptive” interactions between the participant, her family, and other systems (i.e., substance abuse treatment and health care systems). Participants had to meet DSM-IV criteria for substance use diagnosis, and cocaine had to either be their primary or secondary drug of choice. Females in the intervention condition attended weekly, 50-minute sessions for up to 4 months after randomization, whereas females in the comparison, condition, Health Group (HG), attended eight, bi-weekly 90-minute sessions..
The primary outcomes included substance use,. Substance use did not differ by condition, and remained relatively high; 56% of the study population either reported substance use or had a positive urine drug screen at 12-month follow-up. However, participants in the SET condition were more likely than participants in the HG condition to report utilization of substance abuse treatment.
Table 1 reviews these previous studies and also the studies with secondary goals to reduce crack use.
Table 1.
Review of Recent Studies
| Authors | Sample | Intervention Components |
Delivery Mode |
Number & Duration of Sessions |
% Crack Cocaine Users |
Primary Outcome Measures |
Primary Outcomes |
|---|---|---|---|---|---|---|---|
| I. Evaluations of substance use reduction interventions with HIV-positive crack users, including adherence measures | |||||||
| Aharonovich et al. (2012) [37]• | 40 New York City based, HIV+, non-injection drug users in primary care |
MI session; telephone-based interactive voice response (IVR) system |
In-person counseling supplemented with IVR calls |
One, 20–25 min session; automated calls for 30 days |
76% | Days used primary non-injection drug |
Significant within group pre-post differences; Between group differences not significant |
| Ingersoll et al. (2011) [39]•• | 54 HIV+ adults with current crack cocaine use disorder |
“MI+” MI plus feedback and skills building |
In-person, individual counseling |
Five or Six, 30–45 min sessions |
100% | Addiction Severity Index Drug Composite Scores |
Significant within group pre-post differences; Between group differences not significant |
| Feaster et al. (2010) [38••] | 126 HIV+ women who met DSM-IV criteria for cocaine abuse/dependence and criteria for ART |
A family, eco-systemic intervention |
In-person counseling/ individual and family |
16, 50-min sessions |
94% | Self- reported substance use/ urine screens |
Between group differences not significant. |
| II. Studies with secondary goals to reduce crack use | |||||||
| Meade et al. (2010) [43] | 117 male and 130 female, HIV+ adults with childhood sexual abuse history |
Group coping intervention that utilized cognitive-behavioral treatment strategies |
Group counseling |
15, 90-min sessions |
26%** | Frequency of cocaine use in the past month |
Relative to participants in the support group, those in the coping group reported significantly greater reductions in any cocaine use |
| III. Interventions studies targeting sexual risk reduction among HIV+ populations that include all or some crack cocaine users | |||||||
| Williams et al. (2012) [46]•• | 183 female and 164 male, HIV+ African American crack cocaine users |
Node link mapping |
Mixed-gender, group counseling |
6, 60-min sessions |
100% | Condom use | Condom use increased significantly in the intervention group. Between group differences not significant. |
| Lovejoy et al. (2011) [49] | 54 male, 44 female, HIV+ late middle-age (≥45 years) adults |
Telephone-administered, individual MI session(s) |
Telephone-based counseling |
4 sessions OR 1 session/ 40-min |
Not Specified |
Unprotected anal and vaginal sex |
Unprotected sex significantly lower in 4-session intervention vs. controls. No difference seen between controls and 1 MI session. |
| Cosio et al. (2010) [51] | 55 male, 24 female HIV+ persons ≥ 18 in rural areas |
MI plus skills building intervention |
Telephone-based counseling |
2 sessions; length not specified |
36%** | Condom use during vaginal, anal, or oral sex |
Intervention resulted in significantly better condom use outcomes. |
| Golin et al. 2012 [61] | 315 HIV+ males and 168 HIV+ females in three HIV clinics in North Carolina |
MI supplemented with CD and 4 booster letters |
Individual, in-person counseling sessions |
4, 40–60 min sessions |
19% | Number of unprotected intercourse acts |
SafeTalk intervention significantly reduced unprotected sex acts. Between-group differences significant. |
| IV. Evaluations of substance use reduction interventions with HIV-positive crack users, including adherence measures | |||||||
| Aharonovich et al. (2012) [37] | 40 New York City based, HIV+, non-injection drug users in primary care |
MI session; telephone-based interactive voice response (IVR) system |
In-person counseling supplemented with IVR calls |
One, 20–25 min session; automated calls for 30 days |
75.8%** | Days used primary non-injection drug |
MI Only—mean of 10.2 days to 4.1 at 60-days (SD=4.95); HealthCall + MI mean 9.2 day to 2.0 at 60 days (SD=4.35); Group differences not significant |
| Ingersoll et al. (2011) [39] | 54 HIV+ adults with current crack cocaine use disorder |
“MI+” MI plus feedback and skills building |
In-person, individual counseling |
Five or Six, 30–45 min sessions |
100% | Addiction Severity Index Drug Composite Scores |
Both conditions significantly decreased drug-related problems and days of cocaine use. Group differences not significant. |
| Feaster et al. (2010) [38] | 126 HIV+ women who met DSM-IV criteria for cocaine abuse/dependence and criteria for ART |
A family, eco-systemic intervention |
In-person counseling/ individual and family |
16, 50-min sessions |
94.44%** | Self- reported substance use/ urine screens |
Levels of drug use did not differ by condition; 56% of females either reported substance use or had positive urine drug screen at 12 months. |
| V. Studies with secondary goals to reduce crack use | |||||||
| Meade et al. (2010) [43] | 117 male and 130 female, HIV+ adults with childhood sexual abuse history |
Group coping intervention that utilized cognitive-behavioral treatment strategies |
Group counseling |
15, 90-min sessions |
26%** | Frequency of cocaine use in the past month |
Relative to participants in the support group, those in the coping group had greater reductions in any cocaine use (Wald χ2(4)= 9.81, P < .05). |
| VI. Interventions studies targeting sexual risk reduction among HIV+ populations that include all or some crack cocaine users | |||||||
| Williams et al. (2012) [46] | 183 female and 164 male, HIV+ African American crack cocaine users |
Node link mapping |
Mixed-gender, group counseling |
6, 60-min sessions |
100% | Condom use | Condom use increased significantly in the intervention group. Between group differences not significant. |
| Lovejoy et al. (2011) [49] | 54 male, 44 female, HIV+ late middle-age (≥45 years) adults |
Telephone-administered, individual MI session(s) |
Telephone-based counseling |
4 sessions OR 1 session/ 40-min |
Not Specified |
Unprotected anal and vaginal sex |
Unprotected sex significantly lower in 4-session intervention vs. controls. No difference seen between controls and 1 MI session. |
| Cosio et al. (2010) [51] | 55 male, 24 female HIV+ persons ≥ 18 in rural areas |
MI plus skills building intervention |
Telephone-based counseling |
2 sessions; length not specified |
36%** | Condom use during vaginal, anal, or oral sex |
Intervention resulted in significantly better condom use outcomes. |
| Golin et al. 2012 [61] | 315 HIV+ males and 168 HIV+ females in three HIV clinics in North Carolina |
MI supplemented with CD and 4 booster letters |
Individual, in-person counseling sessions |
4, 40–60 min sessions |
19.06% | Number of unprotected intercourse acts |
SafeTalk intervention significantly reduced unprotected sex acts. Between-group differences significant. |
Studies with Secondary Goals to Reduce Crack Use
In addition to the three studies in which reductions in crack and other substance use were primary outcomes, the literature search identified one article that reported on an intervention in which reduction in crack use was a secondary outcome. This article described secondary analysis of data collected as part of an intervention to build adaptive coping skills among HIV-positive people with a history of childhood sexual abuse [43]. The analyses examined the efficacy of “Living in the Face of Trauma” (LIFT), a group-coping intervention that integrates the cognitive theory of stress and coping [44] and effective cognitive-behavioral treatment strategies for sexual trauma among a sample of people who were HIV-positive [45]. Participants in the time and attention matched comparison group attended support group meetings during which they discussed issues surrounding HIV and child sexual abuse (CSA). Although substance use reduction was not a primary outcome of interest in the intervention, substance use was addressed in two of the intervention sessions and referred to throughout the LIFT intervention as a potential maladaptive strategy that could be a source of stress. The intervention consisted of 15 weekly, 90-minute group sessions.
The study enrolled 247 participants, of which 130 were female and 117 were male. Of the males, 100% reported that they were gay or had sex with men, whereas 24% of females reported that they were lesbian/bisexual. Among the sample, 41% of the participants reported a drug use disorder (30% abuse, 11% dependence) and 26% of the participants had used cocaine in the past month prior to baseline. The primary outcomes, examined were frequency of alcohol, cocaine, and marijuana use. Measurements were taken every 4 months through the 12-month post-intervention follow-up period.
The proportion of the participants in the coping condition that reported using cocaine at follow-up was significantly less than proportion in the comparison condition that reported using cocaine at their 12-month follow-up interview.
Intervention Studies Targeting Sex-Risk Reduction that Include Some Crack Cocaine Users
This review only identified one study that specifically targeted sex-risk reduction among HIV-positive people who were using crack [46••]. This study compared the Positive Choices Intervention (PCI), which consisted of six, 60-minute, mixed-gender group session, with a standard risk reduction intervention.. PCI was based on social cognitive theory [47] and the content was delivered using node link mapping, a method of using visual representations to help connect intervention ideas and concepts [48]. The standard risk reduction intervention consisted of five-sessions that provided participants with information about safer sex and drug use practices in a group format.
The study enrolled 347 heterosexual, African American female (183) and male (164) crack cocaine users into an RCT. The primary outcome was consistent condom use, during vaginal sex in the past 30 days. Both groups showed positive changes at 3-month follow-up. Participants in both groups increased consistent condom use and condom use during last sex, and both groups showed significant differences in mean condom use, condom use self-efficacy, and condom use attitudes between baseline and the 9-month follow-up. The findings suggest that the SI condition continued to improve or maintained their level of change after 3 months, whereas the PCI condition’s sex-risk reduction outcomes generally degraded between the 3-month follow-up and 9-month follow-up appointments.
This study demonstrates that a brief intervention can lead to behavior change. However, it calls into question whether content and method of delivery are more important than simply participating in some type of intervention.
Three other studies that used MI to reduce sex risk among people who are HIV positive also merit mentioning. In the first study, Lovejoy and colleagues [49] utilized an RCT to evaluate the effect of MI session dosage on sex-risk reduction outcomes among 100 HIV-positive older adults. Three conditions were compared: a four-session, telephone-delivered MI counseling intervention, a one-session telephone delivered MI counseling intervention, and a control condition that received no active intervention session. MI intervention components were based on the Transtheoretical Model of behavior change [50].
Participants in the control condition reported three times as many occasions of unprotected sex at 3-month follow-up (compared with participants in the four-session MI condition. Intervention outcomes were more pronounced for participants with the riskiest behavior, and greater MI treatment fidelity resulted in greater reductions in sex-risk behavior. No differences were seen between participants in the control condition and participants in the condition that received one MI session.
In the second study, Cosio and colleagues [51] compared the effects of a two-session telephone-administered MI intervention, the “integrated intervention” group, with the effects of an attention equivalent, skill-building intervention condition in reducing risky sex behaviors among HIV-positive people living in rural areas in the United States. The investigators recruited a sample of 55 males and 24 females living in rural areas in 27 states. The majority of the sample was white (67%), and self-identified as gay men (54%). Neither crack cocaine nor substance use was listed as a criterion to participate in this study. However, 36% of the participants reported using cocaine in the 2 months prior to baseline data collection. The investigators used the IMB model to develop the integrated intervention [41].
Prior to their study sessions, participants in the integrated intervention condition were sent a survey related to sex-risk behaviors. Information from these surveys was then aggregated to create personalized feedback to use during the two telephone MI sessions. The primary behavioral outcome was number of unprotected anal and vaginal sex acts in the past 3 months. Participants in the integrated intervention reported significantly greater increases in the proportion of vaginal sex partners with whom condoms were used “all the time” (16.7% [pre], 22.5% [post]), whereas participants in the skills-building condition reported decreases (25.8% [pre], 22.5% [post] (p < 0.05).
The third study, Project SafeTalk, used an RCT design to compare the efficacy of an MI-based, multicomponent program to enhance safer sex practices among people living with HIV [52] with a heart healthy comparison condition. This intervention had a similar format and materials to those used in the Safe Talk intervention, and was adopted from a nutrition and physical activity counseling intervention to include information for HIV-positive individuals. The SafeTalk intervention was developed by taking into account factors identified in previous research as associated with practicing risky sex among people living with HIV, including health beliefs about HIV treatment [53, 54], experiencing ongoing stressful life events [55, 56] and perceived stigma [57], lower self-efficacy and behavioral control to practice safer sex and use condoms [55, 56], and substance use [57, 58], as well as having a better health status [56, 57] or a committed relationship [53, 59]. Because a safer sex program for people living with HIV would need to consider multiple individualized risk factors, MI was used because it allows individualized counseling.
Based on social cognitive theory [47] and Rogerian psychology [60], the SafeTalk program consisted of four structured monthly MI sessions with booster letters, a series of four booklet-CD pairs that helped prepare patients for each MI session, with a fifth pair providing tailored safer sex information. SafeTalk’s short-term and long-term efficacy on behavioral outcomes was tested in an RCT among 490 men and women living with HIV, 20% of whom reported crack cocaine use in the past 3 months. In the primary test of efficacy, which controlled for baseline transmission risk behavior (TRB, the number of acts of unprotected sex with a negative or unknown serostatus partner), SafeTalk reduced the average number of TRB acts at 8- month follow-up by 87% compared with controls (p < 0.001). SafeTalk significantly reduced TRB rates at 8 and 12 months. In multivariable analyses, the duration of MI counseling and number of provided sessions increased, participants' sex-risk behavior decreased. The effect of MI time and number of sessions on sex behavior was mediated by self-efficacy but not by motivation to practice safer sex [52].
Discussion
Very few reports of interventions for HIV-positive people who use crack cocaine have been published within the past 2 years. Nonetheless, these few studies highlight important progress in behavioral HIV prevention strategies for HIV-positive males and females who use crack. There was a strong emphasis in the interventions on the unique needs of HIV-positive crack users and on addressing the relationships between individual, interpersonal, and contextual factors. Moreover, the use of technology in delivering HIV prevention has been increasing. Video and telephone delivery of interventions appeared to be efficacious methods of delivering brief behavioral HIV prevention for HIV-positive people who use or abuse crack cocaine. Important characteristics of the studies reviewed here are categorized in Table 1.
HIV positive people who use crack may or may not be aware of their HIV status. Interventions for people who are not aware of their status need to include a seek component (e.g. outreach, media campaigns, etc.) to reach people in the community who use crack, an HIV testing component to identify people who are positive and a component that links people who test positive for HIV to care and treatment. Interventions for people who know that they are HIV positive and are already linked to care and treatment need to focus on improving medication adherence and retention in treatment. The importance of interventions that link to people to treatment and improve adherence for those who are on treatment has increased tremendously with the new focus on HIV treatment as prevention.
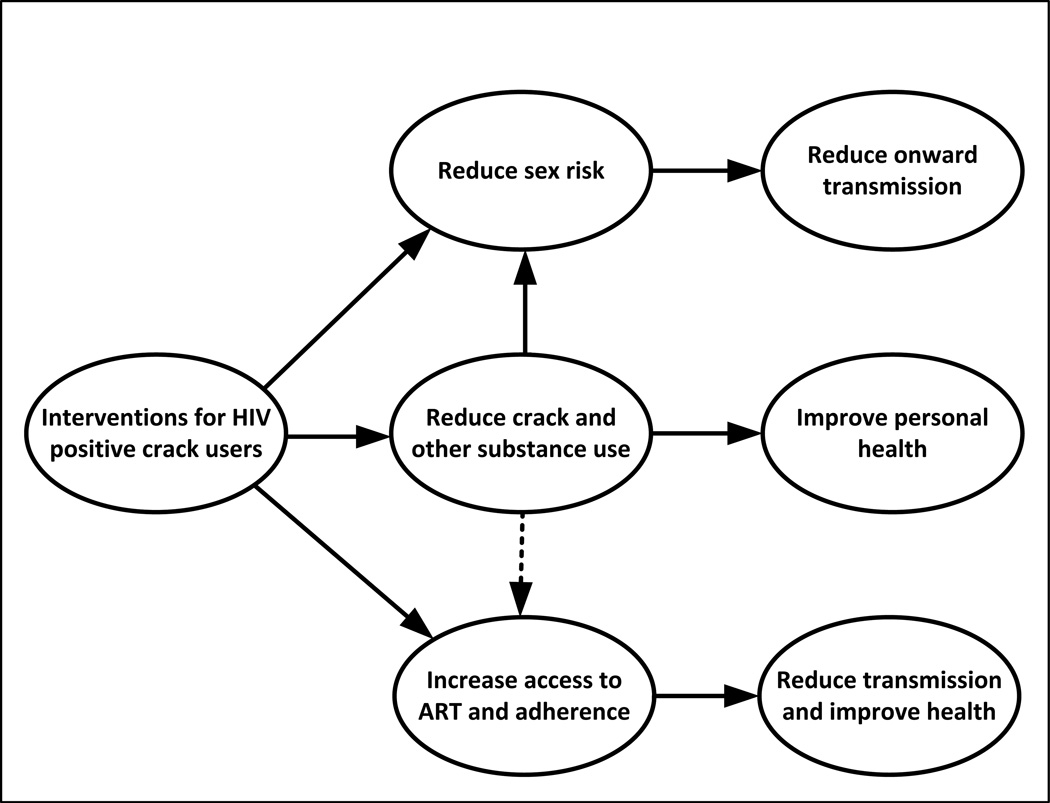
Interventions are most likely to be most efficacious and cost-effective if they target multiple factors. Interventions that address substance use, ART adherence, and safer sex behavior must take into account biomedical and interrelated sociobehavioral factors that influence health and transmission. Many approaches, such as MI, that have been successful in treating substance abuse also show promise in addressing ART adherence and safer sex behaviors. Consequently, they may be particularly adaptable to multipronged approaches. For example, MI could be coupled with less labor intensive methods such as tailored intervention booster sessions that are delivered via-kiosks in clinic waiting rooms or via the internet to sustain reductions in crack use and sex risk and with text messaging interventions to improve adherence. Figure 1 presents a conceptual model of what interventions could target and what their biobehavioral outcomes could be. Approaches that integrate behavior change techniques into technology-based interactive multimedia programs pique interest and increase sustainability, and they may become increasingly important as the penetration of smartphone technology continues to grow globally. In addition to interventions that target HIV positive people who use crack cocaine, structural interventions to reduce onset of crack use by targeting upstream factors (e.g. social inequality, gender discrimination, limited job opportunities) are also needed.
Figure 1.
Intervention targets for expected outcomes
Scientists and policy makers need to find ways to collaborate and coordinate efforts so that research findings are translated into effective and sustainable programs. HIV infection and crack use are global problems. For interventions to have widespread impact, they will need to be adaptable to different sociocultural environments sensitive to gender and traditions. Polydrug use is now the norm; consequently, crack is rarely used in isolation. Therefore, new interventions will need to address the needs and risks associated with polydrug use.
Conclusions
While definitive conclusions cannot be drawn based on current studies, it appears that more intensive interventions may be more effective. If this turns out to be the case, the need for greater intensity will have to be balanced against cost and practicality of widely disseminated intensive interventions given resource constraints and creative approaches to enhancing efficiency, such as integration with existing clinical relationships and integrating the use of technology. Overall, policy-level and structural-level interventions that reduce poverty, increase jobs with health insurance, create access to substance abuse treatment, and reduce the availability of crack in communities may have the broadest impact on the HIV epidemic. However, these efforts will take a tremendous commitment on the part of all levels of stakeholders, which is often difficult to achieve. With economies at a breaking point, research may also be hard pressed to offer singular solutions for HIV-positive crack cocaine users. Nor is there truly much homogeny in substance use among crack users with the need to come down after a long crack high, often by using alcohol or marijuana. Collectively, researchers, clinicians, and stakeholders need to work creatively toward advancing innovative solutions that will have a cost-benefit and high impact for substance-abusing people living with HIV.
Footnotes
Disclosure: W. M. Weschberg: none; C. Golin: NIH grant; N. El-Bassel: none; J. Hopkins: none; Zule: none.
References
Papers of particular interest, published recently have been highlighted as:
• Of importance
•• Of major importance
- 1.Inciardi JA. Editor's introduction. The crack epidemic revisited. J Psychoactive Drugs. 1992;24(4):305–306. doi: 10.1080/02791072.1992.10471655. [DOI] [PubMed] [Google Scholar]
- 2.Washton AM, Gold MS. Crack. JAMA. 1986;256(6):711. doi: 10.1001/jama.1986.03380060037008. [DOI] [PubMed] [Google Scholar]
- 3.Fischer B, Coghlan M. Crack use in North American cities: the neglected 'epidemic'. Addiction. 2007;102(9):1340–1341. doi: 10.1111/j.1360-0443.2007.01963.x. [DOI] [PubMed] [Google Scholar]
- 4.Draus PJ, Carlson RG. Change in the scenery: an ethnographic exploration of crack cocaine use in rural Ohio. J Ethn Subst Abuse. 2007;6(1):81–107. doi: 10.1300/J233v06n01_06. [DOI] [PubMed] [Google Scholar]
- 5.Ilse J, Prinzleve M, Zurhold H, et al. Cocaine and crack use and dependence in Europe—Experts view on an increasing public health problem. Addiction Research and Theory. 2006;14(5):437–452. [Google Scholar]
- 6.Vivancos R, Maskrey V, Rumball D, Harvey I, Holland R. Crack/cocaine use in a rural county of England. J Public Health. 2006;28(2):96–103. doi: 10.1093/pubmed/fdl010. [DOI] [PubMed] [Google Scholar]
- 7.Needle R, Kroeger K, Belani H, et al. Sex, drugs, and HIV: Rapid assessment of HIV risk behaviors among street-based drug using sex workers in Durban, South Africa. Soc Sci Med. 2008;67(9):1447–1455. doi: 10.1016/j.socscimed.2008.06.031. [DOI] [PubMed] [Google Scholar]
- 8.Parry CDH, Bhana A, Plüddemann A, et al. The South African Community Epidemiology Network on Drug Use (SACENDU): description, findings (1997–99) and policy implications. Addiction. 2002;97(8):969–976. doi: 10.1046/j.1360-0443.2002.00145.x. [DOI] [PubMed] [Google Scholar]
- 9.Pechansky F, Woody G, Inciardi J, et al. HIV seroprevalence among drug users: an analysis of selected variables based on 10 years of data collection in Porto Alegre, Brazil. Drug Alcohol Depend. 2006;82(Suppl. 1):S109–S113. doi: 10.1016/s0376-8716(06)80017-7. [DOI] [PubMed] [Google Scholar]
- 10.Falck RS, Wang J, Carlson RG. Crack cocaine trajectories among users in a midwestern American city. Addiction. 2007;102(9):1421–1431. doi: 10.1111/j.1360-0443.2007.01915.x. [DOI] [PubMed] [Google Scholar]
- 11.Wechsberg WM, Novak SP, Zule WA, et al. Sustainability of intervention effects of an evidence-based HIV prevention intervention for African American women who smoke crack cocaine. Drug Alcohol Depend. 2010;109(1–3):205–212. doi: 10.1016/j.drugalcdep.2010.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hser YI, Huang D, Brecht ML, Li L, Evans E. Contrasting trajectories of heroin, cocaine, and methamphetamine use. J Addict Dis. 2008;27(3):13–21. doi: 10.1080/10550880802122554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Falck RS, Wang J, Siegal HA, Carlson RG. The prevalence of psychiatric disorder among a community sample of crack cocaine users: an exploratory study with practical implications. J NervMent Dis. 2004;192(7):503–507. doi: 10.1097/01.nmd.0000131913.94916.d5. [DOI] [PubMed] [Google Scholar]
- 14.Fischer B, Rudzinski K, Ivsins A, et al. Social, health and drug use characteristics of primary crack users in three mid-sized communities in British Columbia, Canada. Drugs: Education, Prevention & Policy. 2010;17(4):333–353. [Google Scholar]
- 15.Logan TK, Leukefeld C. Sexual and drug use behaviors among female crack users: a multi-site sample. Drug Alcohol Depend. 2000;58(3):237–245. doi: 10.1016/s0376-8716(99)00096-4. [DOI] [PubMed] [Google Scholar]
- 16.Wechsberg WM, Dennis ML, Stevens SJ. Cluster analysis of HIV intervention outcomes among substance-abusing women. Am J Drug Alcohol Abuse. 1998;24(2):239–257. doi: 10.3109/00952999809001711. [DOI] [PubMed] [Google Scholar]
- 17.Edlin BR, Irwin KL, Faruque S, et al. Intersecting epidemics-—crack cocaine use and HIV infection among inner-city young adults. New Eng J Med. 1994;331(21):1422–1427. doi: 10.1056/NEJM199411243312106. [DOI] [PubMed] [Google Scholar]
- 18.Wilson T, DeHovitz JA. STDs, HIV, and crack cocaine: a review. AIDS Patient Care STDS. 1997;1(2):62–66. doi: 10.1089/apc.1997.11.62. [DOI] [PubMed] [Google Scholar]
- 19.Marx R, Aral SO, Rolfs RT, Sterk CE, Kahn JG. Crack, sex, and STD. Sex Trans Dis. 1991;18(2):92–101. doi: 10.1097/00007435-199118020-00008. [DOI] [PubMed] [Google Scholar]
- 20.Inciardi JA. Crack, crack house sex, and HIV risk. Arch Sex Behav. 1995;24(3):249–269. doi: 10.1007/BF01541599. [DOI] [PubMed] [Google Scholar]
- 21.Inciardi J. HIV/AIDS risks among male, heterosexual noninjecting drug users who exchange crack for sex. NIDA Res Monogr. 1994;143:26–40. [PubMed] [Google Scholar]
- 22.Draus PJ, Carlson RG. “The game turns on you”: Crack, sex, gender, and power in small-town Ohio. J Contemp Ethnogr. 2009;38(3):384–408. [Google Scholar]
- 23.El-Bassel N, Schilling RF, Irwin KL, et al. Sex trading and psychological distress among women recruited from the streets of Harlem. American Journal of Public Health. 1997;87(1):66–70. doi: 10.2105/ajph.87.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deren S, Stark M, Rhodes F, et al. Drug-using men who have sex with men: sexual behaviours and sexual identities. Cult Health Sex. 2001;3(3):329–338. [Google Scholar]
- 25.Hatfield LA, Horvath KJ, Jacoby SM, Simon Rosser BR. Comparison of substance use and risky sexual behavior among a diverse sample of urban, HIV-positive men who have sex with men. J Addict Diss. 2009;28(3):208–218. doi: 10.1080/10550880903014726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tobin KE, German D, Spikes P, Patterson J, Latkin C. A comparison of the social and sexual networks of crack-using and non-crack using African American men who have sex with men. J Urban Health. 2011;88(6):1052–1062. doi: 10.1007/s11524-011-9611-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuo I, Greenberg AE, Magnus M, et al. High prevalence of substance use among heterosexuals living in communities with high rates of AIDS and poverty in Washington, DC. Drug Alcohol Depend. 2011;117(2–3):139–144. doi: 10.1016/j.drugalcdep.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 28.Brecht ML, Huang D, Evans E, Hser YI. Polydrug use and implications for longitudinal research: ten-year trajectories for heroin, cocaine, and methamphetamine users. Drug Alcohol Depend. 2008;96(3):193–201. doi: 10.1016/j.drugalcdep.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Staines GL, Magura S, Foote J, Deluca A, Kosanke N. Polysubstance use among alcoholics. J Addict Dis. 2001;20(4):53–69. doi: 10.1300/j069v20n04_06. [DOI] [PubMed] [Google Scholar]
- 30.Harrell PT, Mancha BE, Petras H, Trenz RC, Latimer WW. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug Alcohol Depend. 2012;122(3):220–227. doi: 10.1016/j.drugalcdep.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garrity TF, Leukefeld CG, Carlson RG, et al. Physical health, illicit drug use, and demographic characteristics in rural stimulant users. J Rural Health. 2007;23(2):99–107. doi: 10.1111/j.1748-0361.2007.00076.x. [DOI] [PubMed] [Google Scholar]
- 32.Baum MK, Rafie C, Lai S, et al. Crack-cocaine use accelerates HIV disease progression in a cohort of HIV-positive drug users. J Acquir Immune Defic Syndr. 2009;50(1):93–99. doi: 10.1097/QAI.0b013e3181900129. [DOI] [PubMed] [Google Scholar]
- 33.Baum MK, Rafie C, Lai S, et al. Alcohol use accelerates HIV disease progression. AIDS Res Hum Retroviruses. 2010;26(5):511–518. doi: 10.1089/aid.2009.0211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sharpe TT, Lee LM, Nakashima AK, Elam-Evans LD, Fleming PL. Crack cocaine use and adherence to antiretroviral treatment among HIV-infected black women. J Community Health. 2004;29(2):117–127. doi: 10.1023/b:johe.0000016716.99847.9b. [DOI] [PubMed] [Google Scholar]
- 35.McCoy CB, Weatherby NL, Metsch LR, et al. Effectiveness of HIV interventions among crack users. Drugs and Society. 1996;9(1–2):137–154. [Google Scholar]
- 36.Wechsberg WM, Lam WK, Zule WA, Bobashev G. Efficacy of a woman-focused intervention to reduce HIV risk and increase self-sufficiency among African American crack abusers. Am J Public Health. 2004;94(7):1165–1173. doi: 10.2105/ajph.94.7.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Aharonovich E, Greenstein E, O’Leary A, et al. HealthCall: technology-based extension of motivational interviewing to reduce non-injection drug use in HIV primary care patients—a pilot study. AIDS Care. 2012 Mar 20; doi: 10.1080/09540121.2012.663882. [Epub ahead of print] This pilot study assessed the impact of adding automated interactive voice response (IVR), a telephone-based technology, to a brief motivational interviewing (MI) intervention on drug use outcomes among a sample of HIV-positive, non-injecting drug users. At 60-day follow-up, the effect size for between-group differences moderate (d = 0.62; P = 0.13) that favored the technology-enhanced arm. Adding IVR to a brief MI intervention may be a feasible low-cost way to improve outcomes in this population.
- 38. Feaster DJ, Mitrani VB, Burns MJ, et al. A randomized controlled trial of Structural Ecosystems Therapy for HIV medication adherence and substance abuse relapse prevention. Drug Alcohol Depend. 2010;111(3):227–234. doi: 10.1016/j.drugalcdep.2010.04.017. This study described a family-based, structural intervention designed to improve drug use and medication adherence outcomes in HIV-positive, drug-using females (cocaine had to be either the women’s primary or secondary drug of choice). Females in the intervention condition did not show positive improvements in either outcome.
- 39. Ingersoll KS, Farrell-Carnahan L, Cohen-Filipic J, et al. A pilot randomized clinical trial of two medication adherence and drug use interventions for HIV+ crack cocaine users. Drug Alcohol Depend. 2011;116(1–3):177–187. doi: 10.1016/j.drugalcdep.2010.12.016. This study compared the effects of a counseling intervention with a video-based control group on reducing crack cocaine use and increasing highly active antiretroviral therapy (HAART) adherence in a small sample of HIV-positive people who used crack cocaine. Crack cocaine use decreased and HAART adherence increased in both groups, but there were no significant between-group differences. Video-based interventions, which require fewer resources than traditional counseling interventions, should be further explored as a potential method to improve medication adherence and reduce drug use in HIV-positive crack cocaine users.
- 40.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- 41.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 42.Szapocznik J, Feaster DJ, Mitrani VB, et al. Structural ecosystems therapy for HIV-seropositive African American women: effects on psychological distress, family hassles, and family support. J Consult Clin Psychol. 2004;72(2):288–303. doi: 10.1037/0022-006X.72.2.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Meade CS, Drabkin AS, Hansen NB, et al. Reductions in alcohol and cocaine use following a group coping intervention for HIV-positive adults with childhood sexual abuse histories. Addiction. 2010;105(11):1942–1951. doi: 10.1111/j.1360-0443.2010.03075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Folkman S. Personal control and stress and coping processes: a theoretical analysis. J Pers Soc Psychol. 1984;46(4):839–852. doi: 10.1037//0022-3514.46.4.839. [DOI] [PubMed] [Google Scholar]
- 45.Sikkema KJ, Hansen NB, Kochman A, et al. Outcomes from a group intervention for coping with HIV/AIDS and childhood sexual abuse: reductions in traumatic stress. AIDS Behav. 2007;11(1):49–60. doi: 10.1007/s10461-006-9149-8. [DOI] [PubMed] [Google Scholar]
- 46. Williams M, Bowen A, Atkinson JS, et al. An assessment of brief group interventions to increase condom use by heterosexual crack smokers living with HIV infection. AIDS Care. 2012;24(2):220–231. doi: 10.1080/09540121.2011.597707. This intervention had the largest sample of crack cocaine users among all of the interventions reviewed in this article. Both the intervention group and the control group (a standard, informational intervention) saw initial significantly positive changes in condom use outcomes. However, improvement in condom use decayed over time in the intervention group, whereas improvements in the control group were sustained.
- 47.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 48.Dees SM, Dansereau DF, Simpson DD. Mapping-enhanced drug abuse counseling: urinalysis results in the first year of methadone treatment. J Subst Abuse Treat. 1997;14(1):45–54. doi: 10.1016/s0740-5472(96)00163-8. [DOI] [PubMed] [Google Scholar]
- 49.Lovejoy TI, Heckman TG, Suhr JA, et al. Telephone-administered motivational interviewing reduces risky sexual behavior in HIV-positive late middle-age and older adults: a pilot randomized controlled trial. AIDS Behav. 2011;15(8):1623–1634. doi: 10.1007/s10461-011-0016-x. [DOI] [PubMed] [Google Scholar]
- 50.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. American Psychologist. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 51.Cosio D, Heckman TG, Anderson T, et al. Telephone-administered motivational interviewing to reduce risky sexual behavior in HIV-infected rural persons: a pilot randomized clinical trial. Sex Transm Dis. 2010;37(3):140–146. doi: 10.1097/OLQ.0b013e3181c18975. [DOI] [PubMed] [Google Scholar]
- 52.Chariyeva Z, Golin CE, Earp JA, et al. The role of self-efficacy and motivation to explain the effect of motivational interviewing time on changes in risky sexual behavior among people living with HIV: a mediation analysis. AIDS Behav. 2012 Jan 7; doi: 10.1007/s10461-011-0115-8. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Milam J, Richardson JL, Espinoza L, Stoyanoff S. Correlates of unprotected sex among adult heterosexual men living with HIV. J Urban Health. 2006;83(4):669–681. doi: 10.1007/s11524-006-9068-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kalichman SC, Eaton L, White D, et al. Beliefs about treatments for HIV/AIDS and sexual risk behaviors among men who have sex with men, 1997–2006. J Behav Med. 2007;30(6):497–503. doi: 10.1007/s10865-007-9123-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Crepaz N, Hart T, Marks G. Highly active antiretroviral therapy and sexual risk behavior: a meta-analytic review. JAMA. 2004;292:224–236. doi: 10.1001/jama.292.2.224. [DOI] [PubMed] [Google Scholar]
- 56.van Kesteren NM, Hospers HJ, Kok G. Sexual risk behavior among HIV-positive men who have sex with men: a literature review. Patient Educ Couns. 2007;65:5–20. doi: 10.1016/j.pec.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 57.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Metsch LR, Pereyra M, Messinger S, et al. HIV transmission risk behaviors among HIV infected persons who are successfully linked to care. Clin Infect Dis. 2008;47(4):577–584. doi: 10.1086/590153. [DOI] [PubMed] [Google Scholar]
- 59.Kalichman SC. Psychological and social correlates of high-risk sexual behaviour among men and women living with HIV/AIDS. AIDS Care. 1999;11(4):415–427. doi: 10.1080/09540129947794. [DOI] [PubMed] [Google Scholar]
- 60.Rogers CR. The necessary and sufficient conditions of therapeutic personality change. J Consult Psychol. 1957;21(2):95–103. doi: 10.1037/h0045357. [DOI] [PubMed] [Google Scholar]
- 61.Golin CE, Earp JA, Grodensky CA, et al. Longitudinal effects of SafeTalk, a motivational interviewing-based program to improve safer sex practices among people living with HIV/AIDS. AIDS Behav. 2011;6(5):1182–1191. doi: 10.1007/s10461-011-0025-9. [DOI] [PMC free article] [PubMed] [Google Scholar]