Abstract
Objectives
Determine if patients prefer multi-vessel percutaneous coronary intervention (mv-PCI) over coronary artery bypass graft surgery (CABG) for treatment of symptomatic multi-vessel coronary artery disease (mv-CAD) despite high 1-year risk.
Background
Patient risk perception and preference for CABG or mv-PCI to treat medically refractory mv-CAD is poorly understood. We hypothesize that patients prefer mv-PCI instead of CABG even when quoted high mv-PCI risk.
Methods
585 patients and 31 physicians were presented standardized questionnaires with a hypothetical scenario describing chest pain and medically refractory mv-CAD. CABG or mv-PCI were presented as treatment options. Risk scenarios included variable 1-year risks of death, stroke and repeat procedures for mv-PCI and fixed risks for CABG. Participants indicated their preference of revascularization method based on the presented risks. We calculated the odds that patients or physicians would favor mv-PCI over CABG across a range of quoted risks of death, stroke and repeat procedures.
Results
For nearly all quoted risks, patients preferred mv-PCI over CABG, even when the risk of death was double the risk with CABG or the risk of repeat procedures was more than three times that for CABG (p<0.0001). Compared to patients, physicians chose mv-PCI less often than CABG as the risk of death and repeat procedures increased (p<0.001 and p=0.004, respectively).
Conclusion
Patients favor mv-PCI over CABG to treat mv-CAD, even if 1-year risks of death and repeat procedures far exceed risk with CABG. Physicians are more influenced by actual risk and prefer mv-PCI less than patients despite similarly quoted 1-year risks.
Indexing Words: coronary atherosclerosis, myocardial revascularization, percutaneous transluminal coronary angioplasty
INTRODUCTION
For decades, coronary artery bypass graft surgery (CABG) has been the treatment of choice for symptomatic patients with medically refractory multi-vessel coronary artery disease (CAD) (1). Recently, drug-eluting stents were shown to reduce the incidence of in-stent restenosis and target lesion revascularization (2–6). The SYNTAX trial is the first randomized-controlled trial comparing CABG with multi-vessel percutaneous coronary intervention (mv-PCI) utilizing drug-eluting stents for multi-vessel CAD (7). The combined primary endpoint was death, stroke, myocardial infarction or repeat revascularization at 12-months. The composite outcome was reached in 12.3% with CABG and 17.6% with mv-PCI suggesting that CABG remained superior for multi-vessel CAD revascularization. Despite these findings, CABG rates continue to decline (8,9). While cardiologists and surgeons debate on optimal revascularization method (10–12), little is understood of the patient viewpoint.
Sub-analyses of SYNTAX composite endpoints suggested no statistically significant difference between CABG and mv-PCI for the risk of death or myocardial infarction, and a lower risk of stroke with mv-PCI at 12 months. The overall composite outcome was driven primarily by the risk of repeat procedures at 1-year (5.9% vs. 13.5% for CABG and mv-PCI revascularization, respectively). Based on these findings, some have suggested that i) mv-PCI could still be recommended due to reduced stroke risk compared to CABG, and ii) the increased risk of repeat procedures may be tolerable as they are mostly repeat PCI which is associated with less morbidity than CABG (13). In this context, patient perceptions of the risks associated with CABG and mv-PCI remain poorly understood. We hypothesize that patients will choose mv-PCI over CABG for symptomatic, medically refractory mv-CAD, even if quoted 1-year mv-PCI risks in excess of those observed in the SYNTAX trial.
METHODS
Study Design
GUIDE (Generating Useful Information on patient-based Decisions for method of complex rEvascularization) was a prospective study conducted from July 1, 2009 through July 31, 2010, at a large academic medical center. The protocol was approved by the local Human Subjects Institutional Review Board. Informed consent was obtained from all subjects.
Patients enrolled into the study were asked to imagine that they had chest pain due to multi-vessel coronary artery disease that was refractory to medical therapy. CABG or mv-PCI were treatment options. A standardized script describing CABG and mv-PCI was verbally recited to patients (see Appendix). The script was developed based on typical consent practice at our institution, and was pre-approved by all interventional cardiologists and all cardiothoracic surgeons as an accurate and unbiased explanation for each procedure and associated risks. The script described i) standard on-pump CABG with open sternotomy and standard PCI via a femoral approach, ii) length of in-hospital stay of 4–5 days with CABG and one day with PCI, and iii) need for at least one year of clopidogrel following PCI. Patients were then quoted hypothetical risks of death, stroke and need for repeat procedures at 1-year for CABG and mv-PCI revascularization, and then asked to choose which procedure they would prefer based on the presented risks. The hypothetical risk scenarios were presented to patients verbally and on paper, in short text phrases and in a tabular format.
For CABG, patients were quoted a hypothetical 1-year risk of death, stroke, and need for a repeat procedures of 3%, 2% and 5%, respectively, based on the 1-year point estimate results of the SYNTAX trial, rounded to the lowest whole number (7). Repeat procedures were described as either PCI or repeat CABG surgery. The CABG risk estimates remained fixed across all hypothetical risk scenarios.
For mv-PCI, patients were also quoted hypothetical risks of death, stroke, and need for repeat revascularization procedures at 1-year. Repeat procedure was defined as either repeat PCI or CABG. However, unlike with CABG where quoted risks remained fixed for all presented scenarios, the quoted risk estimates for mv-PCI were altered with each risk scenario. Each mv-PCI risk scenario was randomly generated choosing one of three possible 1-year risk estimates of death (2%, 4% or 6%), one of two possible 1-year risk estimates of stroke (1% or 2%) and one of four possible 1-year risk estimates of repeat procedures (7%, 11%, 15% or 17%). Therefore, there were a total of 24 possible risk scenarios each containing fixed 1-year risk estimates for CABG revascularization and one randomly chosen risk estimate for mv-PCI revascularization.
Each patient was presented with six randomly generated, non-consecutively ordered risk scenarios. For each risk scenario, patients recorded their preference of CABG or mv-PCI before proceeding to the next risk scenario. For example, a subset of patients would have been asked to choose their preferred revascularization method based on the following risk scenario: mv-PCI (6%, 2%, 17%) compared to CABG (3%, 2%, 5%) for (death, stroke, repeat procedures respectively).
Interviews were conducted by eight 1st and 2nd year Medical Students, as well as one 1st year and one 2nd year Internal Medicine Resident. All interviewers were formally trained to uniformly apply the questionnaires. Clear instructions were given to interviewers to strictly follow the approved script to avoid unintentional bias. Independent personnel monitored interviewers at random intervals throughout the study to ensure consistent application of the survey. The questionnaires were administered both verbally (face-to-face) and on paper, in a private clinic room or inpatient room.
Patient choice of revascularization method based on hypothetical risk scenarios could potentially be influenced by an aversion bias to any type of risk. To explore this, general risk aversion was investigated using a Holt and Laury lottery choice task. This widely used experiment is designed to capture risk preference in healthcare and non-healthcare scenarios (14,15).
Patient Enrollment Criteria
Study enrollment included clinically stable patients, age 40–80 years old with angiographically proven CAD or with suspected CAD due to anginal symptoms and two or more risk factors such as hypertension, diabetes mellitus, dyslipidemia, tobacco abuse, and peripheral arterial disease. Applying a research questionnaire quoting unrealistic risks to patients who actually have refractory multi-vessel CAD and who are facing mv-PCI or CABG was considered unethical by the investigators and the institutional review board. These vulnerable patients could potentially confuse the unrealistic hypothetical risks posed in the questionnaire with their own personal risk, which could jeopardize actual medical decision-making. Therefore, our assumption in this study was that patients with established CAD or who are at high risk for CAD have a health care perception that would be reasonably similar to those patients with medically refractory multi-vessel CAD actually facing mv-PCI or CABG.
Patients were recruited from ambulatory cardiovascular medicine/surgery clinics; the cardiac catheterization lab; and the general medicine, cardiology and cardiovascular surgery ward services. Patients were excluded if they had a documented history of cognitive decline, altered mental status, Alzheimer’s disease, did not speak English, were incarcerated, were clinically unstable or were presently being treated in an ICU.
Physician Enrollment Criteria
Cardiovascular Medicine and Cardiac Surgery physicians were presented with the hypothetical risk questionnaires and risk aversion survey to compare patient and physician responses. Unlike patients, physicians were presented with all 24 hypothetical risk scenarios.
Statistical Analysis
Each risk scenario response was treated as a separate observation. Each patient contributed six observations and each physician contributed twenty-four observations to the overall data. Mixed-effects logistic regression analysis was performed in which procedure choice (mv-PCI versus CABG) was the dependent variable and risk of death (2%, 4% or 6%), stroke (1% or 2%), and repeat procedure (7%, 11%, 15% or 17%) were the independent variables. A random effect for the subject was included in the model to account for the correlation between multiple observations from the same subject. Differences between patients and physicians were tested in a combined model that included interactions between respondent type (patients versus physicians) and each of the risk types (death, stroke and repeat procedure). Subsequent sub-analyses examined the effects of CABG/PCI history, gender, age and stroke history on procedure choice.
Differences between patients and physicians in total Holt and Laury risk aversion scores were examined using linear regression. In addition, the difference between patient and physician probability of being risk neutral/seeking versus risk adverse were compared using logistic regression. The direct effect of risk aversion on procedure choice was investigated by including the respondent’s categorized Holt and Laury risk aversion score (risk averse and risk neutral/risk seeking) in the model with risk type and level.
The authors are responsible for the design of the study. The authors wrote the manuscript and vouch for completeness and accuracy of the data, the analyses and presentation.
RESULTS
Participant Demographics
Five hundred and eight-five patients met entry criteria and were enrolled in the study. Thirty-four patients expressed an inability to complete all aspects of the survey due to time constraints. These incomplete surveys were excluded from the final analysis. One patient requested that their information be removed from the study. Therefore, a total of 550 patients were included in the final analysis. Thirty-one physicians were enrolled in the study and 100% were included in the final analysis. All physicians were familiar with the 1-year results of the SYNTAX trial. Demographic characteristics of patients and physicians can be seen in Table 1.
Table 1.
Baseline characteristics
| Patients (n=550) | |
| Age | |
| Mean | 62.4 years +/− 10 years |
| Median | 63 years |
| Gender | |
| Male | 69.6% |
| Female | 30.4% |
| Active Tobacco Use | 19.1% |
| Diabetes | 32.0% |
| Hypertension | 82.5% |
| Dyslipidemia | 80.0% |
| Ischemic Symptoms | |
| Asymptomatic | 70.3% |
| Stable Angina | 13.8% |
| Unstable Angina | 15.9% |
| Angiographically proven CAD | 55.2% |
| Prior PCI only | 29.5% |
| Prior CABG only | 9.5% |
| Prior CABG and PCI | 13.5% |
| No prior CABG or PCI | 47.6% |
| Prior MI | 43.6% |
| Prior Stroke | 7.1% |
| Prior TIA | 8.2% |
| Location of interview | |
| Clinic | 23.4% |
| Catheterization Lab | 11.5% |
| Hospital ward | 65.1% |
| Physicians (n=31) | |
| Age | |
| Mean | 42.1 +/− 10 years |
| Median | 40 years |
| Gender | |
| Male | 68.8% |
| Female | 31.3% |
| Field of Practice | |
| Cardiac Surgery | 9.4% |
| Invasive Cardiology | 15.6% |
| Non-invasive Cardiology | 75.0% |
| Level of Training | |
| Attending | 71.0% |
| Cardiology/Cardiothoracic Surgery Fellow | 29.0% |
Patient Preferences
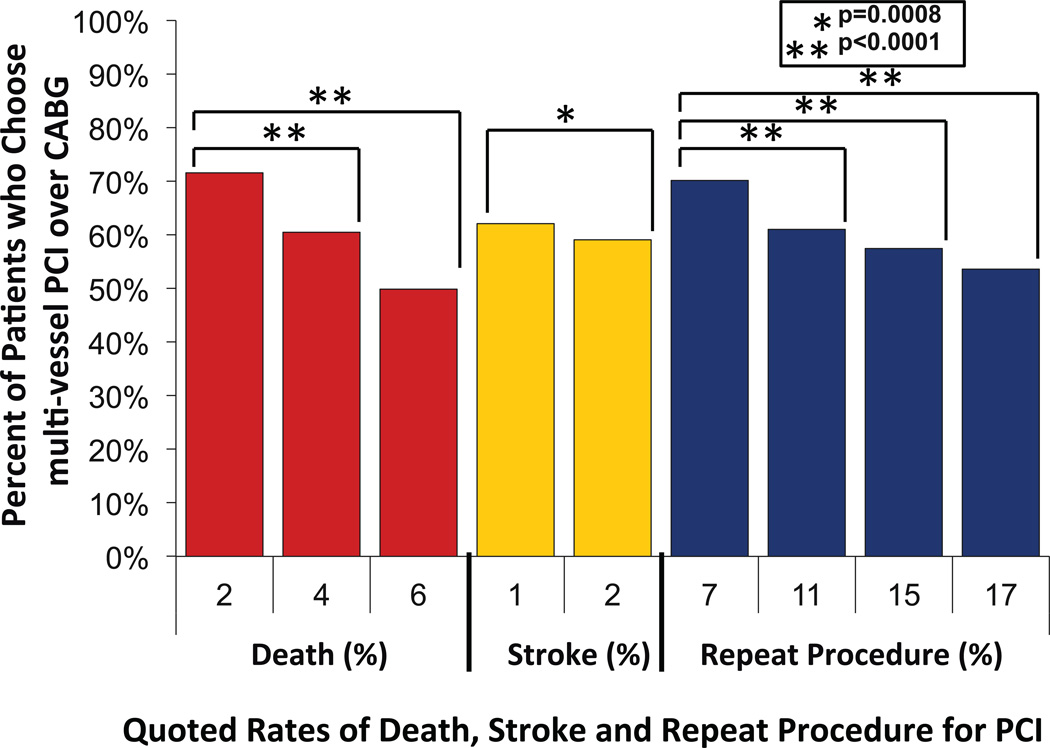
Figure 1 describes patient preference of CABG versus mv-PCI over the range of hypothetical PCI risk scenarios. These data show that patients chose mv-PCI more than CABG across nearly all hypothetical PCI risk scenarios. The percent of patients who chose mv-PCI significantly declined as the hypothetical risks of death, stroke and repeat procedures increased. The odds that a patient would favor mv-PCI over CABG was 74% lower (OR=0.26, 95% CI: 0.19, 0.37) when the risk of death was 4% rather than 2%, and 93% lower (OR=0.07, 95% CI: 0.05, 0.11) when the risk of death was 6% rather than 2%. Similarly, the odds that a patient would favor mv-PCI declined by 37% (OR=0.63, 95% CI: 0.48, 0.82) when the risk of stroke increased from 1% to 2%.
Figure 1.
Patient Preference of mv-PCI over CABG across Hypothetical Risk Scenarios. Percent of patients who chose mv-PCI over CABG across the quoted 1-year risk of death, stroke, and repeat procedure for mv-PCI. p-values indicate significance level of comparisons across for each percent risk within each risk factor. mv-PCI= multi-vessel percutaneous coronary intervention, CABG= coronary artery bypass graft surgery.
As the risk of repeat procedure increased, the favorability of mv-PCI over CABG declined. The odds that a patient would favor mv-PCI declined by 55% (OR=0.45, 95% CI: 0.30, 0.65) when the risk of repeat procedure increased from 7% to 11%. When the risk increased from 7% to 15% the odds that the patients favored mv-PCI declined by 75% (OR=0.25, 95% CI: 0.17, 0.37), and when the risk increased from 7% to 17% the odds declined by 79% (OR=0.21, 95% CI: 0.14, 0.31). Overall, patients placed greatest decisional weight on death, compared to repeat procedure and stroke when choosing mv-PCI versus CABG.
Physician Preferences
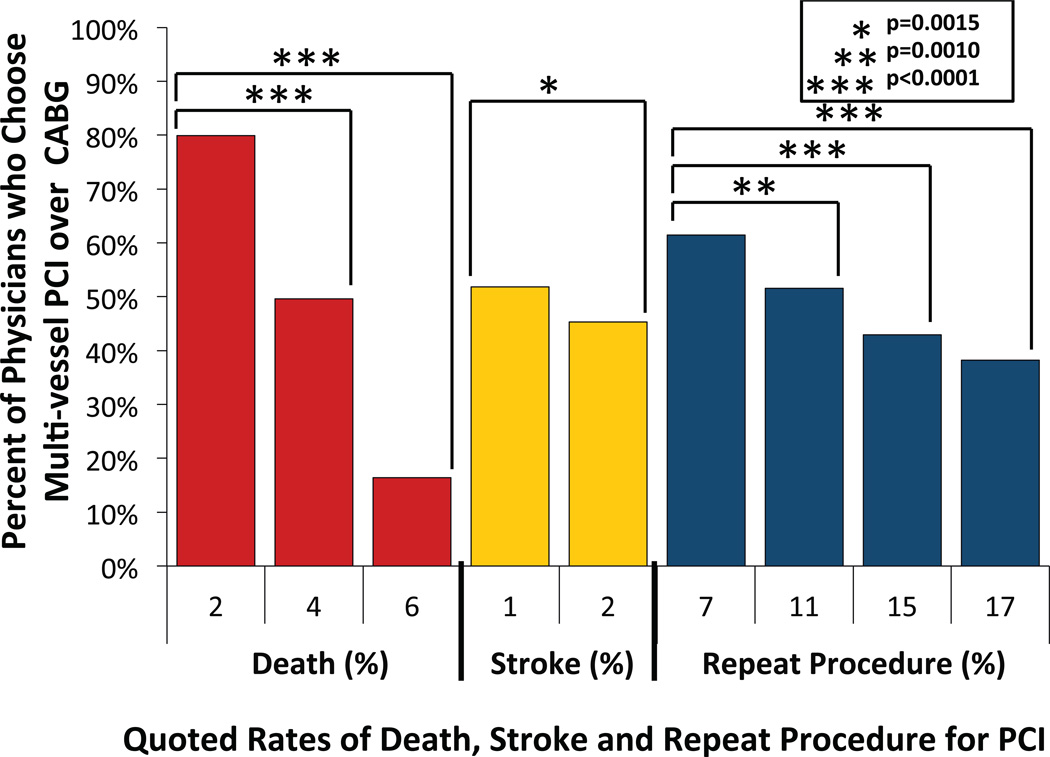
Figure 2 describes physician preference of CABG versus mv-PCI across all tested risk scenarios. Overall, physician preference of mv-PCI over CABG declined as hypothetical mv-PCI risk increased. The percent of physicians who chose mv-PCI over CABG declined by 95% (OR=0.05, 95% CI: 0.02, 0.10) when the risk of death increased from 2% to 4%; and 99% (OR=0.001, 95% CI: 0.001, 0.004) when the risk of death increased from 2% to 6%. The percent of physicians who chose mv-PCI over CABG declined by 55% (OR: 0.45, 95% CI: 0.16, 0.63) when the risk of stroke increased from 1% to 2%. As mv-PCI hypothetical risks increased, the greatest decline in favorability of mv-PCI over CABG was seen for death, followed by repeat procedure and stroke in that order. Similar to patients, physicians placed greatest decisional weight on death, compared to repeat procedure and stroke when choosing mv-PCI versus CABG.
Figure 2.
Physician Preference of mv-PCI over CABG across Hypothetical Risk Scenarios. Percent of physicians choosing mv-PCI over CABG across the quoted 1-year risk of death, stroke, and repeat procedure for mv-PCI. p-values indicate significance level for comparisons across each percent risk within each risk factor. Abbreviations as in Figure 1.
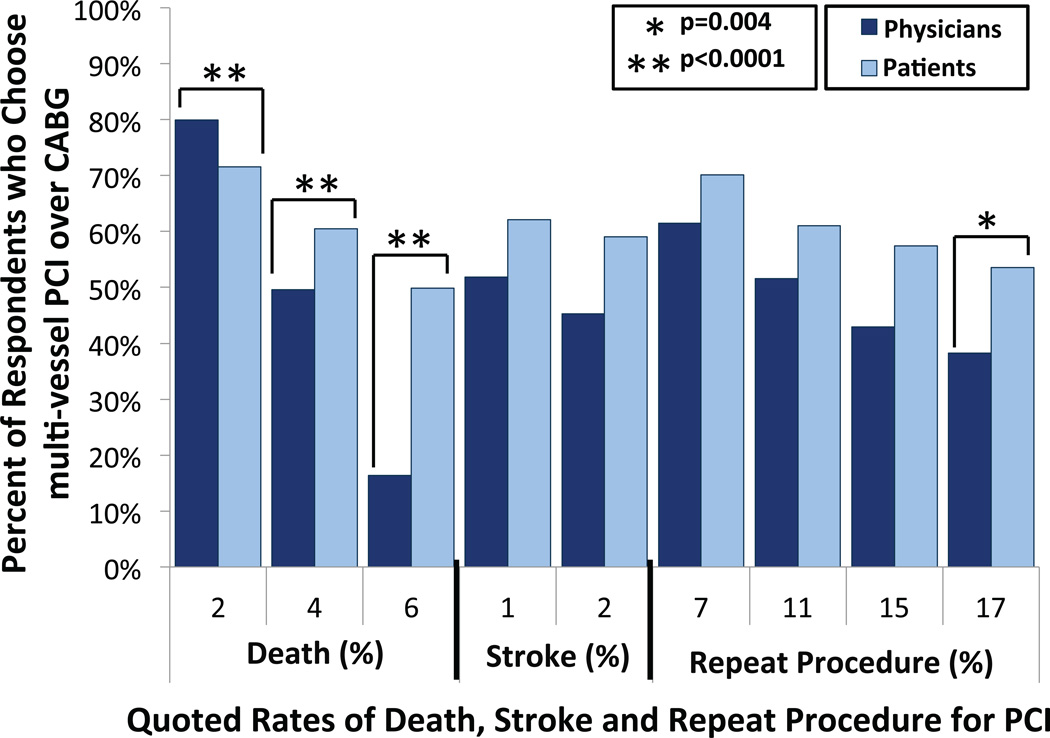
Comparing Patient and Physician Preferences
Comparing patient and physician responses, physicians chose mv-PCI over CABG significantly less than the patients when risk of death was quoted as 4% and 6% (p<0.0001) and repeat revascularization procedures at 15% (p=0.0326) and 17% (p=0.0038). Although a similar trend was seen for stroke, this difference was not statistically significant (Figure 3).
Figure 3.
Patient and Physician Risk Acceptance for Revascularization with mv-PCI over CABG- The percentage of patients and physicians who chose mv-PCI over CABG across the quoted 1-year risk of death, stroke, and repeat procedure for mv-PCI. p-values indicate significance level for comparisons between patients’ and physicians’ response rates within each risk factor percent. Abbreviations as in Figure 1.
Comparing Preferences based on General Risk Aversion
Patients and physicians were stratified into i) risk averse or ii) risk neutral/ risk seeking categories based on the results of the general risk aversion questionnaire. Physicians scored 19% (or 0.80 points) higher than patients on the risk aversion questionnaire which corresponds with increased risk aversion, but this difference did not reach statistical significance (95% CI: −0.33, 1.92). Fifty-seven percent of physicians were risk averse compared to 42% of patients, although this difference did not reach statistical significance (OR=1.84, 95% CI: 0.88, 3.82).
Patients who were risk neutral/risk seeking were not more likely to choose mv-PCI over CABG than patients who were averse (OR=1.46, 95% CI: 0.64, 3.31). Similarly, physicians who were risk neutral/risk seeking were not more likely to choose mv-PCI over CABG than physicians who were risk averse (OR=1.41, 95% CI: 0.10, 20.70). Thus, general risk aversion did not appear to influence patient or physician preferences for method of revascularization.
Sub-Groups
Patients who actually had a previous history of PCI-only strongly preferred mv-PCI over CABG compared with patients who did not have a history of either procedure (OR=24.38, 95% CI: 8.69, 68.34). Patients who had a previous history of CABG-only, modestly preferred CABG over mv-PCI (OR=0.01, 95% CI: 0.00, 0.04). The preferences of patients who previously had both CABG and PCI were similar to those with no history of these procedures (OR=1.02, 95% CI: 0.28, 3.73). Therefore, patient history of PCI and CABG did not influence their choice of mv-PCI or CABG across the hypothetical risk scenarios.
Compared to younger patients, those over age 63 (median age) tended to prefer mv-PCI over CABG (OR=2.11, 95% CI: 0.89, 5.00), but this difference did not reach statistical significance. Similarly, women were more likely than men to choose mv-PCI over CABG (OR=1.97, 95% CI: 0.78, 5.00), and patients with a history of stroke were less likely than those without this history to choose mv-PCI (OR=0.40, 95% CI: 0.11, 1.45); however, neither of these differences reached statistical significance. Therefore, age, gender and history of stroke did not influence patient preference of mv-PCI or CABG across the hypothetical risk scenarios.
DISCUSSION
In this prospective study, patients and physicians were asked to imagine they had symptomatic, medically refractory multi-vessel coronary artery disease, and then choose either mv-PCI or CABG when the 1-year risks associated with these procedures were varied. Patients generally chose mv-PCI over CABG across the hypothetical risk scenarios, which may not be surprising given patients’ perception of morbidity and prolonged recovery associated with CABG. However, patients preferred mv-PCI over CABG even when the hypothetical 1-year risk of repeat procedure was three times the actual risk of repeat procedure observed in the CABG arm in the SYNTAX trial. Moreover, a similar number of patients chose mv-PCI over CABG even when the hypothetical 1-year risk of death with mv-PCI was double the actual 1-year risk of death observed in the CABG arm in the SYNTAX trial. Overall, patient choice of revascularization method was most influenced by the risk of death, and modestly influenced by risk of repeat procedure or stroke.
The SYNTAX trial demonstrated that mv-PCI was inferior to CABG for the 1-year composite outcome of major adverse cardiac and cerebrovascular events (7). Despite this published and widely presented information, CABG rates continue to decline (8,9). Subsequent opinion statements have referenced sub-groups of the SYNTAX PCI cohort where mv-PCI may still be an option, such as those with discrete lesions and other indices of ideal coronary anatomy (i.e. low SYNTAX score) (16–18). Some have pointed to the reduced 1-year risk of stroke with mv-PCI compared to CABG as a reason to still consider mv-PCI in many situations (10–12). An element missing in this debate is actual patient preferences and their valuation of individual risk outcomes such as death, stroke and repeat revascularization. Our data suggest that patients are willing to assume considerable risk with mv-PCI in order to avoid CABG revascularization of multi-vessel CAD. Patients place greatest weight on the risk of death, compared to repeat revascularization or stroke, when making treatment decisions. Investigators designing multi-vessel revascularization trials may consider a separate “patient-oriented” composite endpoint consisting of weighted risk endpoints deemed most important by patients (19). Additional studies are needed to test the reliability and impact of weighted endpoints in clinical trials.
Patients and physicians viewed the proposed hypothetical risks differently when choosing mv-PCI or CABG for revascularization of multi-vessel CAD. Compared to physicians, patients appear willing to accept considerable risk with mv-PCI to avoid CABG. This has important implications for how physicians counsel patients on risks associated with either revascularization approach, as well as how they make recommendations regarding the most appropriate method of revascularization. Frank exchange of accurate information is essential to each counseling practice.
There are several limitations to our study. Patients and physicians were studied from a single, large academic institution preventing applicability across other populations with different ethnic and socio-economic proportions. The SYNTAX trial included myocardial infarction in the overall composite outcome, but this was not included in the risk scenarios applied to patients in our study. One reason was to simplify the questionnaire to study three risk outcome variables instead of four, which would have resulted in significantly more hypothetical risk scenarios and a prohibitively longer questionnaire. In SYNTAX, the authors defined myocardial infarction as the finding of a new Q wave on the ECG and a creatine kinase MB fraction that was five times the upper limit of normal (7). Since the majority of the infarctions during the first year were peri-procedural, the implication of this biochemical and ECG event may not to be immediately tangible to patients, as it is with death, stroke, and repeat revascularization. Additionally, angina and quality of life metrics were not included, since the degree of angina relief and quality of life with CABG and PCI from the SYNTAX trial was unknown at the time of our study initiation. Actual patients facing the decision of CABG or mv-PCI were not included in this study in order to avoid jeopardizing actual medical decisions with hypothetical risks. Finally, we cannot exclude the possibility that patients would have different responses if questions were posed in-hospital, in an outpatient clinic or at home.
Our hypothetical risk scenario questionnaire fixed the one year composite event rates for CABG based on the original SYNTAX trial results, which was designed and powered to detect differences in events at one year. Since our study initiation, a three year follow-up study of SYNTAX participants was published. Not surprisingly, this study demonstrated increased rates of death, stroke, myocardial infarction, and repeat procedure in both PCI and CABG arms, compared to the results from one year. The risk of death and repeat revascularization following CABG or mv-PCI did not change in relative terms; however, three-year stroke outcome was similar between the two revascularization methods (20). The possibility that some physicians and perhaps patients would shift their responses based on these follow-up data cannot be excluded.
CONCLUSIONS
Patients appear willing to accept high 1-year risk in choosing mv-PCI compared to CABG for the treatment of symptomatic, medically refractory multi-vessel coronary artery disease. Patients are more influenced by risk of death compared to repeat procedure or stroke when choosing revascularization method. A disparity exists between physicians and patients for preferred coronary revascularization method when viewing the same risk estimates. Physicians are more influenced by actual risk and prefer mv-PCI less often than patients. These findings may give clinicians additional perspective when counseling patients on risks and benefits of mv-PCI or CABG.
ACKNOWLEDGEMENTS
Andrew Redmann, Angel Matos, Jeff Swick, Lisa Maurer, Lisa Klesius, Nicholas Coorough, and Raj Rangarajan helped with data collection. This project was supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021.
REFERENCES
- 1.Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner TJ, Hart JC, Herrmann HC, Hillis LD, Hutter AM, Jr, et al. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery) Circulation. 2004;110(14):e340–e437. [PubMed] [Google Scholar]
- 2.Serruys PW, Degertekin M, Tanabe K, Abizaid A, Sousa JE, Colombo A, Guagliumi G, Wijns W, Lindeboom WK, Ligthart J, et al. Intravascular ultrasound findings in the multicenter, randomized, double-blind RAVEL (RAndomized study with the sirolimus-eluting VElocity balloon-expandable stent in the treatment of patients with de novo native coronary artery Lesions) trial. Circulation. 2002;106(7):798–803. doi: 10.1161/01.cir.0000025585.63486.59. [DOI] [PubMed] [Google Scholar]
- 3.Moses JW, Leon MB, Popma JJ, Fitzgerald PJ, Holmes DR, O'Shaughnessy C, Caputo RP, Kereiakes DJ, Williams DO, Teirstein PS, et al. Sirolimus-Eluting Stents versus Standard Stents in Patients with Stenosis in a Native Coronary Artery. New England Journal of Medicine. 2003;349(14):1315–1323. doi: 10.1056/NEJMoa035071. [DOI] [PubMed] [Google Scholar]
- 4.Schofer J, Schluter M, Gershlick AH, Wijns W, Garcia E, Schampaert E, Breithardt G. Sirolimus-eluting stents for treatment of patients with long atherosclerotic lesions in small coronary arteries: double-blind, randomised controlled trial (E-SIRIUS) Lancet. 2003;362(9390):1093–1099. doi: 10.1016/S0140-6736(03)14462-5. [DOI] [PubMed] [Google Scholar]
- 5.Stone GW, Ellis SG, Cox DA, Hermiller J, O'Shaughnessy C, Mann JT, Turco M, Caputo R, Bergin P, Greenberg J, et al. A Polymer-Based, Paclitaxel-Eluting Stent in Patients with Coronary Artery Disease. New England Journal of Medicine. 2004;350(3):221–231. doi: 10.1056/NEJMoa032441. [DOI] [PubMed] [Google Scholar]
- 6.Fajadet J, Wijns W, Laarman GJ, Kuck KH, Ormiston J, Munzel T, Popma JJ, Fitzgerald PJ, Bonan R, Kuntz RE. Randomized, double-blind, multicenter study of the Endeavor zotarolimus-eluting phosphorylcholine-encapsulated stent for treatment of native coronary artery lesions: clinical and angiographic results of the ENDEAVOR II trial. Circulation. 2006;114(8):798–806. doi: 10.1161/CIRCULATIONAHA.105.591206. [DOI] [PubMed] [Google Scholar]
- 7.Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961–972. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 8.Adult Cardiac Surgery Database Executive Summary 10 Years. The Society of Thoracic Surgeons. 2010 [Google Scholar]
- 9.Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. JAMA. 2011;305(17):1769–1776. doi: 10.1001/jama.2011.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee TH, Hillis LD, Nabel EG. CABG vs. stenting--clinical implications of the SYNTAX trial. N Engl J Med. 2009;360:e10. doi: 10.1056/NEJMp0900462. United States. [DOI] [PubMed] [Google Scholar]
- 11.Schachinger V, Herdeg C, Scheller B. Best way to revascularize patients with main stem and three vessel lesions: patients should undergo PCI! Clin Res Cardiol. 2010;99(9):531–539. doi: 10.1007/s00392-010-0189-8. [DOI] [PubMed] [Google Scholar]
- 12.Kawasuji M. Debate over patient-centered care: percutaneous coronary intervention or coronary artery bypass grafting? Surg Today. 2011;41(4):459–462. doi: 10.1007/s00595-010-4452-4. [DOI] [PubMed] [Google Scholar]
- 13.Gulati R, Rihal C, Gersh B. The SYNTAX trial: a perspective. Circulation Cardiovascular Intervention. 2009;2(5):463–467. doi: 10.1161/CIRCINTERVENTIONS.109.882670. [DOI] [PubMed] [Google Scholar]
- 14.Holt CA, Laury SK. Risk Aversion and Incentive Effects. The American Economic Review. 2002;92(5):1644–1655. [Google Scholar]
- 15.Anderson LR, Mellor JM. Predicting health behaviors with an experimental measure of risk preference. J Health Econ. 2008;27(5):1260–1274. doi: 10.1016/j.jhealeco.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Capodanno D, Capranzano P, Di Salvo ME, Caggegi A, Tomasello D, Cincotta G, Miano M, Patane M, Tamburino C, Tolaro S, et al. Usefulness of SYNTAX score to select patients with left main coronary artery disease to be treated with coronary artery bypass graft. JACC Cardiovasc Interv. 2009;2(8):731–738. doi: 10.1016/j.jcin.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, et al. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5(1):50–56. doi: 10.4244/eijv5i1a9. [DOI] [PubMed] [Google Scholar]
- 18.Kim YH, Park DW, Kim WJ, Lee JY, Yun SC, Kang SJ, Lee SW, Lee CW, Park SW, Park SJ. Validation of SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) score for prediction of outcomes after unprotected left main coronary revascularization. JACC Cardiovasc Interv. 2010;3(6):612–623. doi: 10.1016/j.jcin.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Wilson RF, Berger AK. Are all end points created equal? The case for weighting. J Am Coll Cardiol. 2011;57(5):546–548. doi: 10.1016/j.jacc.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Kappetein AP, Feldman TE, Mack MJ, Morice MC, Holmes DR, Stahle E, Dawkins KD, Mohr FW, Serruys PW, Colombo A. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur Heart J. 2011;32(17):2125–2134. doi: 10.1093/eurheartj/ehr213. [DOI] [PubMed] [Google Scholar]