Abstract
Objective:
To develop and evaluate new thin and light glasses for the examination of patients with nystagmus and to compare them with Frenzel goggles.
Methods:
First, we designed new examination glasses: a Fresnel-based device with a short focal length that is not as heavy or bulky as Frenzel goggles. Second, visual-fixation suppression of postrotatory nystagmus with Frenzel goggles and the Fresnel-based device, the latter with 2 different magnifications (2- and 4-fold), was compared in 13 healthy subjects. Third, the intensity of the peripheral vestibular spontaneous nystagmus—in 6 patients with acute vestibular neuritis—with the Frenzel goggles and the Fresnel-based device with the 4-fold magnification was compared. Fourth, the visibility and clinical applicability were evaluated.
Results:
The Fresnel-based device weighs 6 g (dimensions 12 × 8 × 0.3 cm). There was no significant difference in the intensity of postrotatory nystagmus between the Fresnel-based device with 4-fold magnification (37.3 ± 17.9°/s) and the Frenzel goggles (39.0 ± 18.3°/s). There was also no significant difference between the intensity of peripheral vestibular spontaneous nystagmus in the patients with acute vestibular neuritis. The Fresnel-based device can be easily applied.
Conclusion:
For suppression of nystagmus, the new Fresnel-based device or so-called M glasses is not inferior to Frenzel goggles. Doctors can carry it in their pocket, it is inexpensive, and easy to handle and to fix to the patient's nose so that it can be used in daily practice for the bedside examination.
Classification of evidence:
This study provides Class III evidence that, in subjects with nystagmus, a Fresnel-based device identifies a similar intensity of nystagmus as that identified by Frenzel goggles.
One of the crucial clinical signs for differentiation between acute peripheral and central vertigo is whether the spontaneous nystagmus can be suppressed by visual fixation (see reference 1). This is particularly relevant for the diagnosis of “vestibular pseudoneuritis” vs vestibular neuritis.2,3 Frenzel goggles reduce visual fixation by means of the magnification glasses of about 16 diopters (D) (table 1) and also allow a better examination of the eye movements. They were described by the German otolaryngologist Hermann Frenzel from Göttingen in the 1950s4 and have been used as an examination tool since then. The major disadvantages of Frenzel goggles (figure 1A) are as follows: first, they are heavy (approximately 500 g); second, they are large (20 × 13 × 7 cm), consisting of 2 glass spectacle lenses (+15 to +18 D), fixed in a compact, fully closed frame; third, they need an electrical power supply for the small lights; and fourth, they need to be held in front of the patient's eyes, which limits the flexibility of the examiner.
Table 1.
Technical information about the different glasses

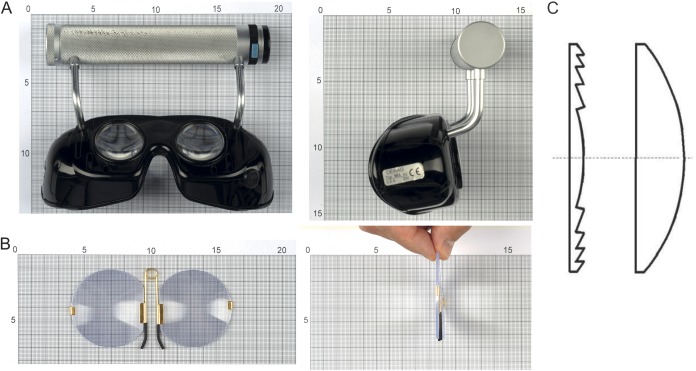
Figure 1. Frenzel goggles, takeaway Frenzel goggles, and construction of the Fresnel lenses.
(A) Frenzel goggles, a commercially available tool for the examination of nystagmus: magnification by glass spectacle lenses about 16 diopters, dimensions approximately 20 × 13 × 7 cm, and weight approximately 500 g. (B) The takeaway Frenzel goggles, a Fresnel-based device, is a newly designed tool for the bedside examination of nystagmus: magnification by Fresnel plastic lenses about 16 diopters, dimensions 12 × 8 × 0.3 cm, and weight 6 g. (C) Schematic drawing showing comparison of Fresnel lenses (left) and regular lenses (right) to illustrate the basic principle of Fresnel lenses, which leads to the smaller dimensions.
The first aim of this study was to develop a new type of examination tool for nystagmus to overcome the limitations of Frenzel goggles. This type of glasses is based on thin Fresnel lenses. These lenses were described by the French physicist Augustin-Jean Fresnel in 1822.5 He developed lighter and smaller glasses based on an optical system in which a series of small base-in prisms replaced a large convex lens; the use of plastics instead of glass was also examined, demonstrating the same optical properties.6 The second aim of the current study was to compare this Fresnel-based device with Frenzel goggles for suppression of peripheral nystagmus and applicability.
METHODS
Level of evidence.
The primary aim of this class III evidence study was to evaluate whether the suppression of spontaneous nystagmus (measured by mean peak slow-phase velocity [mSPV]) and its visibility were equal with the Fresnel-based device and Frenzel goggles.
Standard protocol approvals, registrations, and patient consents.
This study was approved by the local ethics committee. All patients gave their written informed consent. The patient shown in the videos on the Neurology® Web site at Neurology.org also gave his written consent for the videos to be posted online and he had the opportunity to review the manuscript.
Designing and manufacturing the Fresnel-based device.
We developed new small, thin, light examination glasses (figure 1B). They consist of thin Fresnel plastic lenses with a series of small base-in prisms (figure 1C), which replace a large convex lens. They can be held in place on the nose by a metal clamp (for details, see the results section). A comparison was made between Frenzel goggles and the new Fresnel-based device. The Fresnel-based device was designed by 2 of the authors (M.S. and C.F.) and manufactured by Hans Hintermaier, technician at the Department of Neurology. Frenzel goggles were purchased from DEHAG, Rosdorf, Germany.
Postrotatory nystagmus.
To induce peripheral vestibular nystagmus, the semicircular canals were stimulated using a rotatory chair. For stimulation, we used a standard program with a velocity of 3°/s/s in the acceleration phase, a plateau phase (120°/s for 100 seconds), and a sudden stop performed within about 2 seconds to zero (deceleration 100°/s/s). This induced postrotatory nystagmus. Eye movements were recorded with an electronystagmography device (DC-coupled) (Maastricht Instruments BV, Maastricht & Ekida GmbH Denzlingen), and mSPV in degrees/second was measured. We compared the mSPV in subjects with Frenzel goggles and the Fresnel-based device with a 2-fold and 4-fold magnification (see below). There was at least 24 hours between each experiment because of an adaption of the postrotatory nystagmus after repeated stimulations with short intervals.
Peripheral vestibular spontaneous nystagmus.
In addition, we examined patients presenting with spontaneous peripheral vestibular nystagmus caused by acute vestibular neuritis according to diagnostic criteria described before.7 Here, we measured and compared the mSPV (°/s) using the Fresnel-based device with the 4-fold magnification and the Frenzel goggles with a 4-fold magnification. Eye movements were recorded by electronystagmography (same device as described above) for 30 seconds. The recordings with the 2 different glasses were performed immediately after each other in the same visual environment (see below), in a sitting position with the head fixed in the same upright position.
Visibility of nystagmus, general comfort, and handling quality.
In addition to measurements of the slow-phase velocity, we performed a video documentation of the nystagmus. An assessment of the nystagmus visibility was conducted independently by C.F. and L.H.; they evaluated the coverage of the eyes by the sheets/glasses, the conspicuity of the eye movements (nystagmus), the clouding, specular reflexion, and brightness. The aim was to evaluate and compare the general visual quality of the different tools under standardized conditions. Therefore, we used the setting with the healthy subjects.
To measure the general comfort and handling quality, we examined the 13 participants using the rotational chair test. With the help of a short questionnaire, they evaluated various aspects, including the comfort of the Fresnel-based device and the Frenzel goggles, coverage, and visibility of objects in the visual environment. The grading for both evaluations was based on the school grade system: 1 = very good/absolutely; 2 = good/much; 3 = moderate; 4 = less good/less/fewer; 5 = bad/much less/much fewer; and 6 = very bad/not at all.
Illumination and visual background.
All experiments were performed in the same examination room with artificial light from the ceiling and no daylight with an identical visual background for all measurements. The aim was to have conditions similar to those found in most examination rooms.
Data analysis and statistics.
The mSPV under the different conditions, i.e., Frenzel goggles and the Fresnel-based device with 2- and 4-fold magnification, was compared using paired t tests on a 2-sided α level of 0.10. The use of a lower α and Bonferroni correction for multiplicity would be “anticonservative” in the sense that existing differences to the reference method (Frenzel goggles) would be less likely to be detected. Statistical computation was done using R version 2.15 (http://www.R-project.org) and StatWeave version 0.90 (http://www.stat.uiowa.edu/∼rlenth/StatWeave).
RESULTS
Design of Fresnel-based device.
The Fresnel-based device was constructed from round, milled polyvinyl chloride sheets (figure 1B); each sheet was about 0.03 cm thick. The milling causes a light refraction and therefore a magnification. We used lenses with a 2-fold and a 4-fold magnification. The latter was achieved by bonding 2 lenses with 2-fold magnification and attaching them to a covered metal clamp that holds the new glasses in place on the bridge of the patient's nose. The overall size of the Fresnel-based device is 12 × 8 × 0.3 cm; the weight is 6 g (for a comparison with regular Frenzel goggles, see table 1).
The focal distance was 134 mm for the Fresnel-based device with the 2-fold magnification and 63 mm with the 4-fold magnification, corresponding to approximately 8 and 16 D. The focal distance of the Frenzel goggles was 61 mm, corresponding to +16 D (conventional Frenzel goggles have +15 to +18 D).
Postrotatory nystagmus.
Thirteen healthy subjects (1 male, mean age 26.5 years) were examined using a rotatory chair. The mSPV ± SD of the postrotatory nystagmus with the Frenzel goggles was 39.0 ± 18.3°/s. It was 37.3 ± 17.9°/s with the Fresnel-based device with the 4-fold magnification and 16.6 ± 6.7°/s with the 2-fold magnification. The paired t test revealed no statistically significant differences between Frenzel goggles and the Fresnel-based device with the 4-fold magnification (−1.7°/s, 90% confidence interval [CI] −6.7 to 3.4°/s, p = 0.56). There were statistically significant differences between the Fresnel-based device with the 2-fold magnification and the Frenzel goggles (−22.4°/s, 90% CI −29.9 to −14.9°/s, p = 0.0002), as well as between the Fresnel-based device with the 2-fold and the 4-fold magnification (−20.7°/s, 90% CI −27.9 to −13.5°/s, p = 0.0003).
Peripheral vestibular spontaneous nystagmus.
In the 6 patients with acute vestibular neuritis (3 male, mean age 46.4 years), the mSPV of the peripheral vestibular spontaneous nystagmus was 9.1 ± 3.7°/s for the Frenzel goggles compared with 8.2 ± 3.2°/s for the Fresnel-based device with the 4-fold magnification. Plotting the mSPV values measured with the Fresnel-based device against those measured with Frenzel goggles showed a linear relation with a slope of 0.69 (95% CI −0.04 to 1.41) (figure 2; see also videos 1–3, which show a comparison of the intensity and visibility of peripheral vestibular spontaneous nystagmus in a patient with acute vestibular neuritis).
Figure 2. Plot of mean slow-phase velocity of the different goggles.

Plotting the mean peak slow-phase velocity (mSPV) measured with the Fresnel-based device with the 4-fold magnification (y) and Frenzel goggles in 6 patients with spontaneous peripheral nystagmus suggests a linear relation. This indicates that the fixation suppression achieved by the Fresnel-based device is constantly 0.69 times that of the Frenzel goggles, irrespective of the intensity (mSPV) of the spontaneous nystagmus.
Visibility of nystagmus, rating of general comfort, practical use, and durability of the Fresnel-based device.
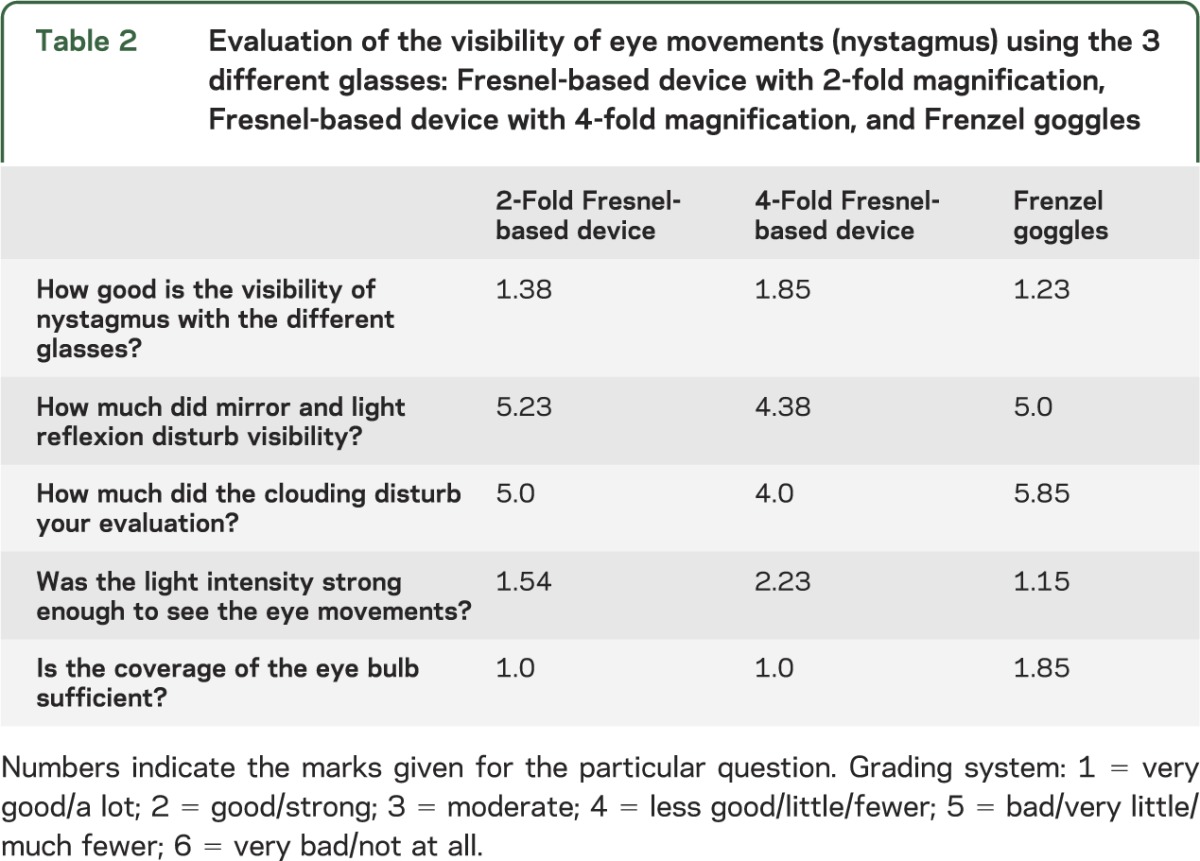
The assessment of the video documentation revealed “fewer” difficulties because of clouding for the Fresnel-based device with the 4-fold magnification and “much fewer” problems for the Frenzel goggles. The mean visibility of the nystagmus was “good” with the Fresnel-based device with the 4-fold magnification compared with a “good to very good” rating for the Frenzel goggles. There were no problems concerning the evaluation of eye movements because of the unequal light conditions (table 2).
Table 2.
Evaluation of the visibility of eye movements (nystagmus) using the 3 different glasses: Fresnel-based device with 2-fold magnification, Fresnel-based device with 4-fold magnification, and Frenzel goggles
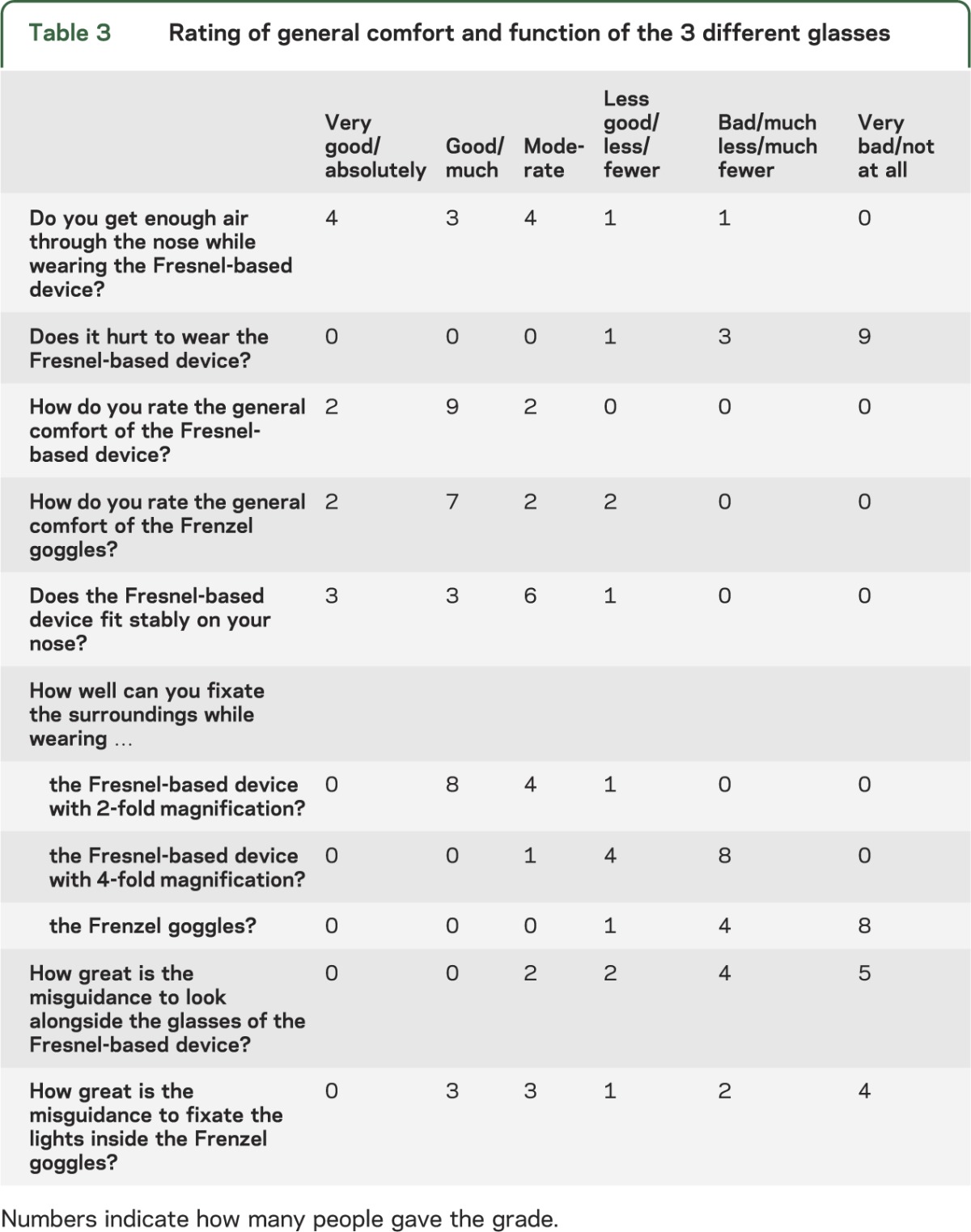
The 13 test persons evaluated the overall comfort of the new Fresnel-based device as “good” with an acceptable firmness, similar to Frenzel goggles. On average, the “ability to breathe through the nose” with the new glasses was rated as “good” and the question about whether the Fresnel-based device hurt was answered with “much less” to “not at all.” The Fresnel-based device could be fixed on the patient's nose in a “good” and stable way. The misguidance of looking alongside the Fresnel-based device was judged as “much less.” Fixation of the lamps inside the Frenzel goggles was mainly judged as “less.” Regarding fixation of the surroundings, the Fresnel-based device with the 4-fold magnification and the Frenzel goggles reached values from “bad” to “not at all” (table 3).
Table 3.
Rating of general comfort and function of the 3 different glasses
The Fresnel-based device has been used for more than a year by the authors and their colleagues in daily practice. A special case for carrying is not necessary. The Fresnel-based device has proven to be very practical, robust, and durable. Its durability is attributable to its simple construction (made of plastic and steel), low weight, and small dimensions; none of the devices have ever broken even when they were dropped.
DISCUSSION
The aim of this study was to develop and test a new doctor- and patient-friendly examination tool for nystagmus—a Fresnel-based device. For suppression of postrotatory nystagmus and peripheral vestibular spontaneous nystagmus, the Fresnel-based device with a 4-fold magnification was not inferior to Frenzel goggles. This study provides Class III evidence that, in subjects with nystagmus, a Fresnel-based device identifies a similar intensity of nystagmus as that identified by Frenzel goggles. This simple tool for the examination of eye movements is similar to another examination tool developed, tested, and established in the past—the so-called bucket test for the measurement of the subjective visual vertical.8
The major advantages of the Fresnel-based device are as follows: first, the lower weight (6 g vs 500 g) and smaller dimensions; second, no need for a power supply, meaning that the examiners can carry the glasses with them in the pocket of their coat; third, the glasses can be fastened to the patient's nose, so that examiner has both hands free; fourth, the good durability of the Fresnel-based device due to its simple construction, robust material (plastic and steel), and low weight; and finally, the price advantage of the Fresnel-based device, which costs only approximately US $60 in comparison to US $500 to $800 for the conventional Frenzel goggles.
This study, however, has limitations: first, the low number of patients with acute vestibular neuritis; second, patients with a low mSPV (<4°/s) were not examined; and third, the power to detect a difference of 5°/s in mSPV between the Fresnel-based device with 4-fold magnification and the Frenzel goggles on an α level of 0.10 was 0.51 in our sample.
In summary, the Fresnel-based device—the new takeaway or so-called M glasses—can be easily used, is always ready to use, is light, thin, and inexpensive, and the distribution of this important examination tool should be much higher in the future. Doctors and medical students can take them with them in their coat pocket. In clinical practice, they should be used in all patients with vertigo, dizziness, postural imbalance, and blurred vision (oscillopsia).
ACKNOWLEDGMENT
The authors thank Judy Benson and Katie Ogston for copyediting the manuscript and Richard John Leigh for his critical and very helpful comments. They thank Hans Hintermaier for his contribution to the design and the construction of the Fresnel-based device. They also thank the subjects for their contribution to the study.
GLOSSARY
- CI
confidence interval
- D
diopter
- mSPV
mean slow-phase velocity
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
M.S.: concept and construction of tool, study concept, drafting/revising the manuscript for content, including medical writing for content, critical revision of the manuscript for important intellectual content. C.F.: construction of tool, study concept/design, drafting/revising the manuscript for content, acquisition of data, analysis and interpretation of data, medical writing, statistical analysis. L.H.: acquisition and analysis of data. O.B.: statistical analysis of the data, drafting/revising the manuscript for content, critical revision of the manuscript for important intellectual content.
STUDY FUNDING
Supported by a grant from the BMBF to the IFB (grant code 01 EO 0901).
DISCLOSURE
M. Strupp is joint chief editor of the Journal of Neurology, editor-in-chief of Frontiers of Neuro-otology, and section editor of F1000. He has received speakers honoraria from Abbott, Actelion, UCB, GSK, TEVA, Biogen Idec, Pierre Fabre, Eisai, and Hennig Pharma. C. Fischer reports no disclosures relevant to the manuscript. L. Hanß and O. Bayer report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Leigh RJ, Zee D. The Neurology of Eye Movements, 4th ed New York: Oxford University Press; 2006 [Google Scholar]
- 2.Cnyrim CD, Newman-Toker D, Karch C, Brandt T, Strupp M. Bedside differentiation of vestibular neuritis from central “vestibular pseudoneuritis.” J Neurol Neurosurg Psychiatry 2008;79:458–460 [DOI] [PubMed] [Google Scholar]
- 3.Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke 2009;40:3504–3510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frenzel H. Practical methods of a systematic study of otorhinolaryngology. Munch Med Wochenschr 1956;98:972–975 [PubMed] [Google Scholar]
- 5.Fresnel AJ. Mémoire sur un nuveau système d'éclairage des phares. Imprimerie Royale Lu à L’académie Des Sciences; 1822 [Google Scholar]
- 6.Harle GA. Use of plastics in the Fresnel rhomb. Nature 1950;166:149–150 [DOI] [PubMed] [Google Scholar]
- 7.Strupp M, Brandt T. Vestibular neuritis. Semin Neurol 2009;29:509–519 [DOI] [PubMed] [Google Scholar]
- 8.Zwergal A, Rettinger N, Frenzel C, Frisen L, Brandt T, Strupp M. A bucket of static vestibular function. Neurology 2009;72:1689–1692 [DOI] [PubMed] [Google Scholar]