Abstract
Previous reports suggest that Black breast cancer patients receive less patient-centered cancer care than their White counterparts. Interventions to improve patient-centered care (PCC) in Black breast cancer patients are lacking. Seventy-six women with histologically confirmed breast cancer were recruited from the Washington, DC area. After a baseline telephone interview, women received an in-person decision support educational session led by a trained survivor coach. The coach used a culturally appropriate guidebook and decision-making model—TALK Back!© A follow-up assessment assessed participants’ acceptability of the intervention and intermediate outcomes. After the intervention, participants reported increased: self-efficacy in communicating with providers (70 %) and self-efficacy in making treatment decisions (70 %). Compared to baseline scores, post-intervention communication with providers significantly increased (p=.000). This is the first outcome report of an intervention to facilitate PCC in Black breast cancer patients. Testing this intervention using RCTs or similar designs will be important next steps.
Keywords: African-American, Black, Adjuvant therapy, Decision support
Introduction
Patient-centered care is an essential aspect of quality care recognized by The Institute of Medicine [1]. Attributes of patient-centered care (PCC) are consideration of patients’ needs, perspectives, and individual experiences; provision of opportunities to patients to participate in their care; and enhancement of the patient–clinician relationship. Nowhere is patient-centered care more necessary than in the delivery of cancer care. Unlike most chronic diseases, the diagnosis of cancer typically poses an immediate threat to the life of the patient, requires decisions about complex therapies, and often requires interactions with multiple providers. Thus, ensuring that breast cancer patients receive care according to these attributes of care is essential.
Patients who receive PCC are more likely to be more satisfied and adhere to their treatment [2]. Communication is central to PCC and may have a role in reducing health disparities [3]. This is because prescription of cancer treatments such as adjuvant therapy takes place within the context of the patient–provider relationship. Good communication and participatory encounters may increase rates of optimal treatment and may improve cancer outcomes. Some data suggest that Black breast cancer patients have less participatory encounters than Whites and receive less information about their breast [4–6]. Few interventions have been developed to empower Black women in their patient–provider interactions.
Skill-based interventions have shown promise in non-cancer settings for increasing patients’ skills in communicating with their providers [7]. However, these approaches have shown less favorable results in Blacks suggesting that these strategies may work best when combined with other culturally acceptable intervention approaches [7]. To fill this gap, in interventions focused on decision support, we developed an intervention to facilitate patient–provider communication in Black breast patients by improving women’s self-efficacy in interacting with providers and in their treatment knowledge. Our formative work noted that Black survivors were viewed as trusted information sources among newly diagnosed Black patients [8, 9]. Black women were targeted given the persistent reported disparities in breast cancer outcomes and in processes of care. We integrated theoretical constructs from Social Cognitive Theory [10], the Decision Support Framework, and the PEN-3 cultural model of health behavior [11]. Intervention approaches and messages were developed based on a review of published interventions, a review of existing patient education booklets and pamphlets, and formative data from Black breast cancer patients in active treatment, survivors, and cancer providers. Details of these developmental steps are described elsewhere [12]. A brief overview of the intervention, Sisters Informing SistersSM intervention, is discussed below.
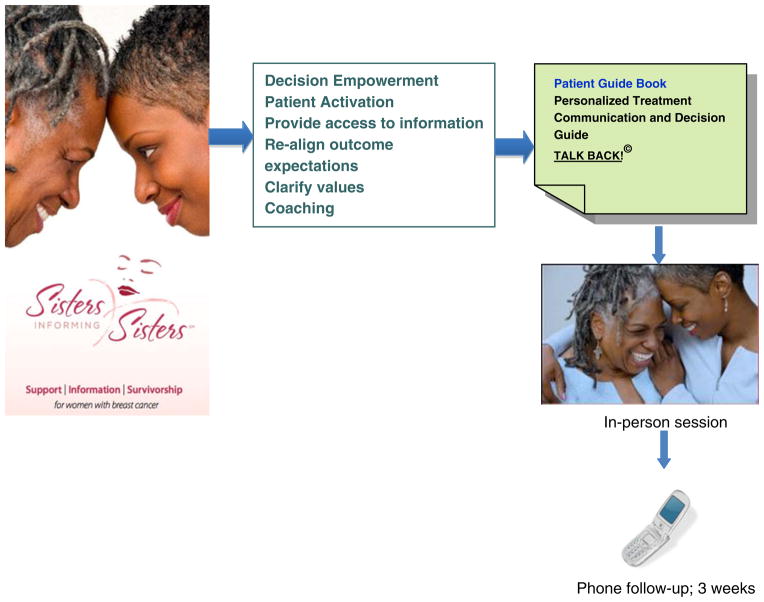
Sisters Informing SistersSM began implementation in 2005 and pairs a newly diagnosed African-American breast cancer patient with a trained survivor for an in-person patient skills education session (Fig. 1). The primary purpose of the session is to assist participants in obtaining necessary information from their providers and to get them more involved in their encounters so that they will ultimately make guideline-appropriate decisions that are in line with their preferences, values, and needs. The intervention focuses on patient activation and centers on enhancing key communication skills of information seeking and question asking [13, 14]. The one-on-one session which provides women with access to information incorporates the sharing of personal stories, communication skills training, and decision support through the use of facilitator and patient guidebooks, which were organized around the TALK Back!© framework developed for this intervention [12]. The mnemonic TALK represents the framework to facilitate good communication with providers: Tell your story, Ask questions, Listen actively, and Know your options. In this report, we: (1) assess the acceptability of the intervention as measured by women’s satisfaction with their interactions with their survivor coach, decision support print materials, and overall rating of intervention; (2) examine the impact of the intervention on patient-reported outcomes of: (a) self-efficacy in communicating with providers, (b) decision making, treatment knowledge; and (3) assess improvements in patient-centered care.
Fig. 1.
Overview of the intervention process
Methods
Setting, Population, and Recruitment
This study was approved by the Institutional Review Board and conducted in the Washington, DC metropolitan area. Given the need to identify and recruit women to the study after a confirmed diagnosis, we focused efforts on recruiting women primarily from cancer surgeons. The clinical staff who helped identify eligible patients received training about the study, which included the purpose, general research questions, and eligibility criteria. They were also provided with study brochures to distribute to potentially eligible patients. The brochures that described the study and included a study voicemail number, e-mail, and phone numbers for other resources were mailed to local support groups, cancer providers, and mammography clinics.
Eligible women were those who self-identified as being Black, had histologically confirmed breast cancer, were 21 years of age or older, and were diagnosed with any stage of breast cancer. Women with recurrent breast cancer or second primary cancers were excluded, as decision making is more complex for this group. For women referred by medical providers, medical staff obtained verbal consent for the potential participant to be contacted by our research staff. All women were informed that their decision to participate would not affect their medical care. A research assistant obtained verbal consent, scheduled the face-to-face coaching session, and conducted baseline and follow-up patient interviews.
Patients returned consent forms by mail and received a $25 American Express® gift cheque for their time, following their coaching session. Women were contacted again within 3 months of seeing the survivor coach to complete a telephone follow-up survey to assess intervention outcomes. Participants received a $15 grocery store gift card.
Study Measures
Implementation
Coaches completed a brief contact form after the intervention session which captured the start and end time of the session, observed mood of the participant (optimistic, anxious, sad, afraid), referrals made (if any), and any specific concerns that women mentioned.
Satisfaction with survivor coaches was measured using six Likert-formatted items that captured participants’ ratings of interpersonal and technical skills (alpha=.985). Lower scores represented higher levels of satisfaction with the survivor coach. Women’s perception of the effectiveness of their coach was measured on a five-point Likert-type scale (1=not at all to 5=a great deal). Women also rated their overall quality of communication with their coach on a scale from 0 to 10, with a higher score representing better communication (m=9.39, SD=1.48).
Satisfaction with print materials was measured using a six-item scale. Patients answered yes or no to the items regarding the usefulness of the guidebook (alpha=.814; range 1.02–23.67) For example, patients were asked if they found the guidebook easy to read and if it helped them.
Intervention Outcomes
Women’s self-efficacy in communication with their providers was measured on using two items that assessed communication with doctors and ability to prepare for follow-up appointments (alpha=.92). Participants also rated their improvements in shared decision making using a three-item scale (alpha=.78). Self-efficacy in treatment knowledge was assessed with two items on a five-point Likert scale that assessed participants’ perceptions of their knowledge about their treatments and confidence in making informed decisions (alpha=.90). The primary outcome, patient-centered communication was measured using the 13-item patient perceived involvement in care (PICS) (alpha=.51) [15].
Analysis
Descriptive statistics were used to describe demographic, clinical, and psychosocial characteristics of the study participants. Chi-square tests for categorical variables and Student’s t tests and correlations for continuous variables were used to determine associations between intervention status and the study variables. Paired t tests were used to assess differences in baseline and follow-up patient involvement in care (PICS) scores. Analyses were conducted using SPSS version 19 software.
Results
A total of 76 women enrolled in the study (see Table 1). Participants were primarily referred to this study by surgeons (n=45), medical oncologists (n=6), and from community sources (n=22). Three women (n=3) were referred by friends or self-referred to the study by calling the study voicemail line. The ages of participants ranged from 31 to 85 (m=51.9; SD=10.6). More than (70 %) of the women had above high school education. More than one third (36 %) of the women had at least a college degree or more and most were insured (95 %). Almost 70 % of study participants were unmarried/not partnered. In comparison, the three survivor coaches all held advanced degrees, were insured, similarly employed, and most were unmarried (66 %). Seventy-five percent of the study participants who completed baseline interviews met with a survivor coach. There were no significant differences in demographic factors or clinical factors between those women who did or did not meet with a coach (p>.05).
Table 1.
Demographic, clinical, and psychosocial characteristics of the study patients by intervention status (N=76)
| Total N=76 | Intervention Session
|
p value | |||||
|---|---|---|---|---|---|---|---|
| Yes, 47 (61.8) | No 29 (38.2) | ||||||
|
|
|
|
|||||
| n | % | n | % | n | % | ||
| Demographic characteristics | |||||||
| Age: mean (SD) | 51.9 (10.60) | 51.9 (11.58) | 51.8 (9.17) | .953 | |||
| ≤50 years | 33 | 43.4 | 21 | 63.6 | 12 | 36.4 | .492 |
| >50 years | 43 | 56.6 | 24 | 55.8 | 19 | 44.2 | |
| Education | |||||||
| ≤HS | 21 | 28.4 | 14 | 66.7 | 7 | 33.3 | .348 |
| >HS | 53 | 71.6 | 29 | 54.7 | 24 | 45.3 | |
| Marital status | |||||||
| Married/living as married | 26 | 34.2 | 17 | 65.4 | 9 | 34.6 | .430 |
| Currently single | 50 | 65.8 | 28 | 56.0 | 50 | 44.0 | |
| Employment | |||||||
| Full-time employed | 32 | 45.1 | 17 | 53.1 | 15 | 46.9 | .475 |
| Other | 39 | 54.9 | 24 | 61.5 | 15 | 38.5 | |
| Insurance | |||||||
| Yes | 72 | 94.7 | 42 | 58.3 | 30 | 41.7 | .641 |
| No | 4 | 5.3 | 3 | 3.9 | 1 | 25.0 | |
| Clinical characteristics | |||||||
| HR status | |||||||
| HR positive | 42 | 75.0 | 24 | 57.1 | 18 | 42.9 | .642 |
| HR negative | 14 | 25.0 | 7 | 50.0 | 7 | 50.0 | |
| Stage | |||||||
| I | 21 | 39.6 | 11 | 52.4 | 10 | 47.6 | .958 |
| II and III | 32 | 60.4 | 17 | 53.1 | 15 | 46.9 | |
| Surgery | |||||||
| Lumpectomy | 35 | 60.3 | 18 | 51.4 | 17 | 48.6 | .479 |
| Mastectomy | 23 | 39.7 | 14 | 60.9 | 9 | 39.1 | |
| Psychosocial factors | |||||||
| Perceived discrimination | |||||||
| Yes | 27 | 43.5 | 14 | 51.9 | 13 | 48.1 | .521 |
| No | 35 | 56.5 | 21 | 60.0 | 14 | 40.0 | |
| Collectivism (mean (SD)) | 9.3 (3.22) | 9.1 (2.32) | 9.6 (4.16) | .564 | |||
| Worldview (mean (SD)) | 7.3 (1.42) | 7.4 (1.47) | 7.3 (1.38) | .909 | |||
| Religiosity scale (mean (SD)) | 30.7 (4.98) | 30.4 (5.26) | 31.1 (4.68) | .603 | |||
p values were obtained from chi-square and t tests. Percentages add up to 100 along the rows for intervention groups and along columns for the “total” category
Implementation of Survivor–Survivor Coaching Sessions
The in-person survivor-to-survivor intervention sessions were held in mutually agreed upon locations (e.g., coffee shops, participants’ homes, hospitals) and ranged from 30 to 120 min in length (m=60 min). Most participants attended sessions alone (74 %); 20 % brought family members and/or friends. At the session, coaches observed that more than half of the patients appeared to be optimistic (55 %) in the face of their diagnosis, whereas others were perceived to be anxious (20 %), afraid (20 %), or sad (10 %). Survivor coaches used the patient guidebook and TALK Back!© model to facilitate intervention sessions. Time spent on model steps was tailored to each woman’s case (e.g., emphasis on treatment options versus emphasis on getting certain questions answered by providers). Core discussion elements included addressing common myths about breast cancer, terminology, and adjuvant therapies. Other issues/questions raised by participants were: the long-term effects of adjuvant therapy, ability to conceive, and benefits of mastectomy versus lumpectomy. When requested or deemed necessary, survivor coaches made referrals to nutritionists and patient navigators to assistance women with transportation or insurance issues.
Acceptability and Process Outcomes
Satisfaction with Survivor Coach
Figure 2 displays responses to ratings of individual items of ratings of a survivor coach. Most women had high ratings of their survivor coach and either strongly agreed or agreed that she was courteous (93.6 %), sensitive (91.5 %), respectful (93.6 %), and thorough (89.3 %). Most (87 %) women valued working with the coach and 89 % stated that they would refer other women to the intervention. The average rating of satisfaction was 27.2 (SD=6.3). Women’s overall rating of communication with their coach was high (m=9.4; SD=1.5). Ratings of the survivor coach did not vary according to patient characteristics (e.g., demographic, psychosocial; p>.05; data not shown).
Fig. 2.
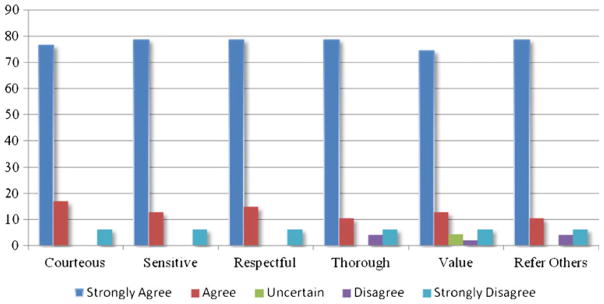
Intervention participants’ ratings of survivor coach
Decision Model Print Materials
Most (87 %) patients reported that the steps in the TALK Back!© model helped them communicate better with their provider. After using the guidebook, 98 % of participants were more informed about breast cancer, and 96 % reported increased knowledge about their treatment options. In open-ended comments, women described the patient guide as “helpful to realizing that you are not alone.” Ninety-eight percent of the participants reported finding the guidebook helpful, yet only 12 % took their guidebooks to their medical appointments. Further understanding was gained from women’s open-ended comments that pointed to the size of the book as reasons not to carry their guidebooks (e.g., “cannot fit in my purse” and “holding capacity in purse”). Suggested improvements for the guidebook were that it be made “easier to open” and include more information on survivor stories. There were no differences in ratings of the materials by women’s demographic, clinical, or psychosocial factors (p>.05; data not shown).
Communication and Decision Outcomes
Most participants (91 %) reported improvements in self-efficacy regarding their skills to communicate with their provider after receiving the intervention. Additionally, 77 % reported improved self-efficacy to participate in the treatment decision-making process. Similarly, 96 % reported that they were more informed about their cancer, and 92 % were more informed about their treatment options after the coaching session. Eighty percent of women indicated greater participation in the treatment decision-making process (data not shown). These outcomes did not vary by demographic, clinical, or psychosocial factors (p>.05; Table 2). Finally, we found a significant improvement in participants’ rating of their involvement in their care from their baseline assessment (m=19.2; SD=1.9) to follow-up (m=21.0; SD=1.7; p=.000). No other factors were associated with PICS scores (data not shown).
Table 2.
Associations between participant characteristics and intervention outcomes (N=47)
| Satisfaction with coach, m=27.2; SD=6.3 | Communication with coach, m=9.4; SD=1.5 | Effectiveness: decision support m=10.6; SD=2.7 | Self-efficacy: communication, m=7.5; SD=2.0 | Self-efficacy decision, m=7.9; SD=1.6 | PICS post-intervention, m=20.7; SD=1.9 | |
|---|---|---|---|---|---|---|
| Age, r (p values) | .02 (.87) | .17 (.26) | .09 (.55) | .18 (.24) | 15 (.33) | −.47 (.07) |
| Education: >HS versus ≤HS | −2.29 (.25) | −.27 (.54) | −1.31 (.12) | −.81 (.20) | −.40 (.41) | .97 (.35) |
| Marital/living: married versus single | −.92 (.63) | .31 (.50) | 1.05 (.20) | .76 (.20) | .05 (.92) | −.37 (.73) |
| Employment: full time versus other | −.89 (.60) | −.64 (.20) | −.08 (.92) | −.81 (.22) | −.15 (.78) | −.24 (82) |
| Hormonal receptor (positive versus negative) | −.81 (.50) | .21 (.75) | .36 (.77) | .32 (.72) | .59 (.40) | −1.17 (.30) |
| Surgery (mastectomy versus lumpectomy) | .89 (.60) | −.44 (.42) | .46 (.65) | .05 (.95) | .26 (.65) | −.71 (49) |
| Tumor stage: (stages II and III versus I) | −1.16 (.53) | −.21 (.48) | .94 (.38) | .25 (.72) | .29 (.55) | −.67 (.58) |
| Collectivism, r (p values) | .22 (.20) | −.12 (.48) | −.17 (.31) | −.13 (.46) | −.20 (.26) | .20 (.49) |
| World view, r (p values) | .07 (.70) | .04 (.84) | −.02 (.90) | .13 (.46) | .02 (.90) | −.11 (.71) |
| Discrimination, r (p values) | −.09 (.55) | .05 (.73) | −.04 (.82) | −.10 (.50) | −.00 (.99) | .29 (.28) |
| Religiosity, r (p values) | −.18 (.30) | .09 (.60) | .12 (.48) | .07 (.67) | −.05 (.78) | −.184 (53) |
Values are given as (mean difference, p value) or r (p value)
Discussion and Conclusion
This study found that it was feasible to recruit newly diagnosed Black patients into a decision support intervention. The intervention approach was acceptable as demonstrated by women’s high level of satisfaction with their coach, the print materials, and overall rating of the intervention. Participants reported improved communication with providers, increased knowledge, and increased shared decision making (SDM). Finally, we found a significant improvement in participant’s scores of patient-centered communication (p<.05). Results did not vary by women’s demographic, clinical, or psychosocial characteristics. Taken together, these data provide support for the acceptance and value of a peer-delivered culturally relevant decision support intervention for Black women with breast cancer. To our knowledge, this study is the first to describe process outcomes related to a decision support intervention developed specifically for Black breast cancer patients.
Recently, several reports have noted that Black and other minority women are less likely to have important adjuvant systemic therapies compared to Whites [16]. Some potential explanations include provider factors (e.g., lack of a recommendation), patient factors (limited understanding of treatment benefits), and system factors (referrals) [5, 16, 17]. Improving patient-centered care may alleviate some of the barriers to adjuvant systemic therapy. Unfortunately, there are few interventions in this area [18]. Bickell developed a systems-based tracking and feedback registry to increase the likelihood that breast cancer surgery patients would connect with an oncologist [19]. After initiation of the patient-tracking system, the number of completed oncology consultations increased, and the racial disparity in adjuvant underuse was eliminated [20]. Ell used a sociomedical model of case management and provided assistance with scheduling child and elderly care to increase the number of patients who received breast cancer treatment within 20 days of their diagnosis [20]. Though not significant, data suggest trends in improving initiation of treatment among minority women [20]. Other strategies have focused on increasing women’s involvement in consultations or providing case management, but these studies did not focus on minority women [20, 21]. Further these studies did not directly focus on increasing patients’ ability to effectively communicate with their providers and included limited numbers of minority women. Although knowledge and communication with providers have been identified as important factors that may influence treatment disparities, there is limited intervention information about how to address these issues [22, 23]. Post and colleagues have shown that patient-training interventions improve patient satisfaction, health outcomes, and increase patient participation in their healthcare [24]. However, when they compared intervention outcomes for Blacks and Whites, Blacks did not have the same degree of favorable outcomes regarding print-oriented interventions [24]. Kreling and colleagues suggest that utilizing peer counselors may enhance the acceptability and effectiveness of interventions with breast cancer patients [25]. Our report is among the first to describe process outcomes for an intervention designed to facilitate communication and knowledge among Black women with breast cancer. Interestingly, self-reported outcomes did not vary according to participants’ sociodemographic or clinical factors suggesting that this intervention may benefit Black women with breast cancer from varying sociodemographic backgrounds. Additionally, in this sample, there were high ratings of spirituality.
Like most women facing a breast cancer diagnosis, women in our study were concerned about their children, treatment side effects, and finances. Using the facilitator’s guide, the survivor coach assessed women’s values, preferences, and cancer beliefs and subsequently guided them in an exercise to clarify values, obtain information, and learn the steps of decision making and communicating with their providers using motivational interviewing techniques. Most patients reported reading the print materials and listed specific areas (e.g., writing questions, help with chemotherapy decisions) that were informed by the print materials.
Strengths and Limitations
This study fills a gap in the literature regarding potential strategies to inform Black women about their breast cancer treatment options and to improve their decision-making skills, SDM, and communication with their providers. There are, however, several limitations to our findings. First, while this study provides important information regarding Black women’s satisfaction with the intervention, outcomes regarding knowledge, SDM, communication, and self-efficacy were based on self-report. Future studies that include audio or video recordings of patient–provider interactions will be important. Additionally, this process-focused feasibility pilot did not employ a randomized control trial design, which limits our ability to draw conclusions regarding the intervention’s effectiveness compared to another strategy or usual care. It will be important in the future to assess the effectiveness of the intervention in a more rigorous design.
Practical considerations are that not all women enrolled in the study met with an interventionist (38 % attrition rate). We are unable to report the reasons for their lack of participation. Thus, women who participated may differ from those who did not on parameters not collected as part of this study (e.g., mental health, social support, etc.). However, we noted that we did not find significant differences in demographic or clinical factors between women who did or did not receive the intervention. Because participants were drawn from a variety of locations, we were unable to track women through the system. Therefore, we could not assess whether women who did not meet with a coach had withdrawn from the medical system altogether. Future interventions that are nested within a clinical setting may reduce the percentage of patients who are lost to follow-up. Additionally, collection of information beyond demographics may help to better understand characteristics of women who were unable to be reached by survivor interventionists. Nevertheless, the high participation rate in this study suggests that most women were willing to follow through with an in-person appointment.
Study findings should be regarded within the context that some patients learned about the intervention from their provider. We were unable to detect whether providers tended to refer patients who they perceived to be adherent or nonadherent. The use of an RCT in the future would help to control for this potential bias. Women in the study were from a metropolitan area and were largely well educated, which may not be representative of women with less education or from other non-urban areas. However, the education levels of our sample reflect national data: 83 % of Black women in the USA have a high school diploma, and 19 % have college degrees.
Conclusion
Racial and ethnic disparities in patient–provider communication are well documented. Yet, there is a shortage of interventions focused to improve this process of care overall and more specifically in Blacks. Assistance with preparing for interactions with their providers may be useful to improving women’s intermediate outcomes. These intermediate outcomes, in turn, may lead to reduced disparities in treatment and ultimately cancer outcomes.
Contributor Information
Vanessa B. Sheppard, Email: vls3@georgetown.edu, Georgetown University Medical Center, Washington, DC 20007, USA. Department of Oncology, Cancer Prevention and Control Program Georgetown University Medical Center, 3300 Whitehaven Street, NW, Suite 4100, Washington, DC 20007, USA
Sherrie F. Wallington, Georgetown University Medical Center, Washington, DC 20007, USA
Shawna C. Willey, Georgetown University Medical Center, Washington, DC 20007, USA
Regina M. Hampton, Signature Breast Care, Lanham, MD 20706, USA
W. Lucas, Georgetown University Medical Center, Washington, DC 20007, USA
Y. Jennings, Georgetown University Medical Center, Washington, DC 20007, USA
S. Horton, Howard University, Washington, DC 20060, USA
N. Muzeck, Georgetown University, Washington, DC 20057, USA
C. Cocilovo, Inova Breast Care Center, Fairfax, VA 22031, USA
C. Isaacs, Georgetown University Medical Center, Washington, DC 20007, USA
References
- 1.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. 2. National Academy Press; Washington: 2001. pp. 1–337. [Google Scholar]
- 2.Epstein RM, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, US Department of Health and Human Services, National Institutes of Health; 2007. p. 07-6225. [Google Scholar]
- 3.Sheppard VB, Figueiredo M, Canar J, Goodman M, Caciedo L, Kaufman A, et al. Latina a Latina: developing a breast cancer decision support intervention. Psychooncology. 2007;17(4):383–391. doi: 10.1002/pon.1239. [DOI] [PubMed] [Google Scholar]
- 4.Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J Gen Intern Med. 2008;23:654–671. doi: 10.1007/s11606-008-0521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gordon HS, Street RL, Jr, Sharf BF, Souchek J. Racial differences in doctors’ information-giving and patients’ participation. Cancer. 2006;107:1313–1320. doi: 10.1002/cncr.22122. [DOI] [PubMed] [Google Scholar]
- 6.Cooper LA, Roter DL. Unequal treatment: confronting racial and ethnic disparities in health care. National Academies of Science; Washington: 2003. Patient–provider communication: the effect of race and ethnicity on process and outcomes of healthcare; pp. 552–593. [Google Scholar]
- 7.Cegala DJ, Post DM, McClure L. The effects of patient communication skills training on the discourse of older patients during a primary care interview. J Am Geriatr Soc. 2001;49:1505–1511. doi: 10.1046/j.1532-5415.2001.4911244.x. [DOI] [PubMed] [Google Scholar]
- 8.Sheppard VB, Wallington SF, Williams KP, Lucas W. Decision-support intervention for black women eligible for adjuvant systemic therapy: sisters informing sisters about breast cancer treatment disparities. In: Elk R, et al., editors. Cancer disparities causes and evidence-based solutions. Springer; New York: 2010. pp. 367–392. [Google Scholar]
- 9.Sheppard VB, Adams IF, Lamdan R, Taylor KL. The role of patient-provider communication for black women making decisions about breast cancer treatment. Psychooncology. 2010;20:1309–1316. doi: 10.1002/pon.1852. [DOI] [PubMed] [Google Scholar]
- 10.Bandura A. Social foundations of thought and action: a social cognitive theory. Prentice Hall; Englewood Cliffs: 1986. [Google Scholar]
- 11.O’Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G, McPherson R, Bunn H, Graham I, Drake E. A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Educ Couns. 1998;33:267–279. doi: 10.1016/s0738-3991(98)00026-3. [DOI] [PubMed] [Google Scholar]
- 12.Sheppard VB, Williams KP, Harrison TM, Jennings Y, Lucas W, Stephen J, Robinson D, Mandelblatt JS, Taylor KL. Development of decision-support intervention for Black women with breast cancer. Psychooncology. 2010;19:62–70. doi: 10.1002/pon.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Epstein R, Street RL. Patient-centered communication in cancer care. NIH; Bethesda: 2007. [Google Scholar]
- 14.Arora NK, Weaver KE, Clayman ML, Oakley-Girvan I, Potosky AL. Physicians’ decision-making style and psychosocial outcomes among cancer survivors. Patient Educ Couns. 2009;77:404–412. doi: 10.1016/j.pec.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lerman CE, Brody DS, Caputo GC, Smith DG, Lazaro CG, Wolfson HG. Patients’ perceived involvement in care scale: relationship to attitudes about illness and medical care. J Gen Intern Med. 1990;5:29–33. doi: 10.1007/BF02602306. [DOI] [PubMed] [Google Scholar]
- 16.Bickell NA, Wang JJ, Oluwole S, Schrag D, Godfrey H, Hiotis K, Mendez J, Guth AA. Missed opportunities: racial disparities in adjuvant breast treatment. J Clin Oncol. 2006;24:1357–1362. doi: 10.1200/JCO.2005.04.5799. [DOI] [PubMed] [Google Scholar]
- 17.Frederick Schneiders Research. Perceptions of how race and ethnic background affect medical care. 1999 http://www.kff.org/uninsured/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=13290.
- 18.Bickell NA, Cohen A. Understanding reasons for underuse: an approach to improve quality and reduce disparities in breast cancer treatment. Mt Sinai J Med. 2008;75:23–30. doi: 10.1002/msj.20013. [DOI] [PubMed] [Google Scholar]
- 19.Bickell NA, Shastri K, Fei K, Oluwole S, Godfrey H, Hiotis K, Srinivasan A, Guth AA. A tracking and feedback registry to reduce racial disparities in breast cancer care. J Natl Cancer Inst. 2008;100:1717–1723. doi: 10.1093/jnci/djn387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ell K, Padgett D, Vourlekis B, Nissly J, Pineda D, Sarabia O, Walther V, Blumenfield S, Lee PJ. Abnormal mammogram follow-up: a pilot study women with low income. Cancer Pract. 2002;10:130–138. doi: 10.1046/j.1523-5394.2002.103009.x. [DOI] [PubMed] [Google Scholar]
- 21.Sepucha KR, Belkora J, Mutchnick S, Esserman LJ. Consultation planning to help breast cancer patients prepare for medical consultations: effect on communication and satisfaction for patients and physicians. J Clin Oncol. 2002;20:2695–2700. doi: 10.1200/JCO.2002.10.068. [DOI] [PubMed] [Google Scholar]
- 22.Stewart MA. Effective physician–patient communication and health outcomes: a review. CMAJ. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 23.Maly RC, Leake B, Silliman RA. Health care disparities in older patients with breast carcinoma: informational support from physicians. Cancer. 2003;97:1517–1527. doi: 10.1002/cncr.11211. [DOI] [PubMed] [Google Scholar]
- 24.Post D, Cegala D, Marinelli T. Teaching patients to communicate with physicians: the impact of race. J Natl Med Assoc. 2001;93:6–12. [PMC free article] [PubMed] [Google Scholar]
- 25.Kreling B, Figueiredo M, Sheppard V, Mandelblatt J. A qualitative study of factors affecting chemotherapy use in older women with breast cancer: barriers, promoters, and implications for intervention. Psycho-Oncology. 2006;15(12):1065–1076. doi: 10.1002/pon.1042. [DOI] [PubMed] [Google Scholar]