Abstract
A 28-year-old man presented with a 2-week history of red eye, photophobia, pain and decreased visual acuity of the right eye. The ophthalmological examination revealed hypertensive non-granulomatous panuveitis, retinal vasculitis with focus of retinochoroiditis with pigmented central area suggestive of ocular toxoplasmosis in the active phase. He started treatment with azithromycin, pyrimethamine, topical steroids and measures for control of intraocular pressure. Serology for Toxoplasma gondii was positive and for HIV, negative. For headache and vomiting, he was hospitalised in order to exclude cerebral toxoplasma. The cerebral CT scan, MRI and lumbar puncture were negative and treatment was changed to pyrimethamine, sulfadiazine and prednisolone. For persistence of vomiting he started clindamycin with clinical and ophthalmological improvement. The patient is currently under prophylaxis with co-trimoxazol for 1 year, and maintains clinical improvement. This case illustrates the rarity of presentation of ocular toxoplasmosis, without cerebral in an immunocompetent patient.
Background
Toxoplasmosis is a worldwide zoonosis caused by the protozoal organism Toxoplasma gondii, an obligatory parasite of the cat. Infection is acquired by ingestion of oocysts in cat faecal matter or bradyzoits in undercooked meat. In an immunocompetent host, it is generally a benign self-limited infection; nevertheless, severe complications, such as retinochoroidal involvement, have been known to occur.
Central nervous system toxoplasmosis is almost always seen in patients severely immunosuppressed. Ocular toxoplasmosis can be seen even in immunocompetent patients.
The authors present this case to highlight the possibility of ocular toxoplasmosis in immunocompetent patients and the potential for severe disease.
Case presentation
A 28-year-old man from Brazil, who worked with horses, presented with a 2-week history of red eye, photophobia, pain and decreased visual acuity (VA) of the right eye (RE). He denied trauma or similar episodes as relevant ophthalmological history. The ophthalmic test revealed decreased VA of the RE of 7/10 and normal VA of the left eye (LE) of 10/10, as well as a hypertensive non-granulomatous panuveitis of the RE, retinal vasculitis (figure 1) with focus of retinochoroiditis (figure 2) with the pigmented central area having an appearance suggestive of ocular toxoplasmosis in the active phase (headlight in the fog sign).
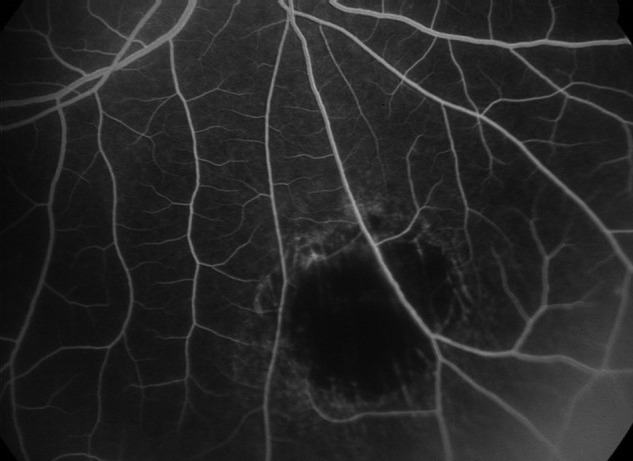
Figure 1.

Angiography of the right eye showing areas of exudation and vasculitis.
Figure 2.
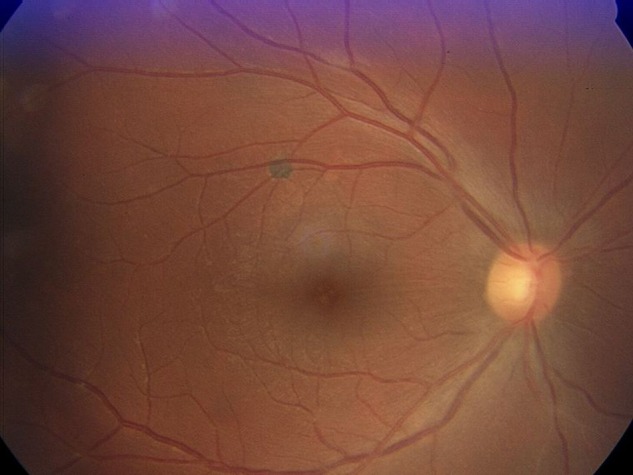
Retinography of the right eye showing toxoplasma focus.
Serology for T. gondii serology was positive (IgG+/IgM−) and for HIV, negative.
Outcome and follow-up
The patient started treatment with azithromycin, pyrimethamine, topical steroids and measures for control of intraocular pressure. One week later, he was re-evaluated and presented partial improvement of intraocular pressure and continued medication.
One week later, he came to the emergency department after suffering 3 days of an intense periocular headache and vomiting, as well as decrease of VA of the RE (6/10).
He was hospitalised for suspicion of cerebral toxoplasmosis. The laboratory results were normal, the cerebral CT scan showed a doubtful right frontal subcortical hypodensity and the MRI revealed only non-specific aspects suggestive of microvascular leucoencephalopathy. For the persistent headache he was submitted to a lumbar puncture, which was normal with a negative toxoplasma antigen titre.
Therapy was changed to pyrimethamine, sulfadiazine and prednisolone. For vomiting, he was started on clindamycin (as it is the only intravenous drug indicated for the treatment of toxoplasmosis) and continued pyrimethamine. The ophthalmological re-evaluation showed improvement of VA of the RE (10/10), and maintained VA of the LE (10/10), resolution of tyndall and keratic precipitates, a slight posterior vitritis with peripheral vasculitis and chorioretinal focus and control of the intraocular tension, whereby corticosteroid was reduced (figure 3).
Figure 3.
Angiography of the right eye showing clear improvement of the vasculitis and exudates.
Acquired immunosuppression was excluded.
Clinically, the refractory headache was found to be related to the ocular inflammatory process and improved with salicylates and pregabalin.
After 9 days of hospitalisation, the patient continued medication with pyrimethamine, sulfadiazine, prednisolone, folic acid and analgaesics.
Three weeks later, the patient showed improvement of the vitritis and vasculitis.
The patient completed 8 weeks of the referred treatment and is now under treatment with co-trimoxazol (trimethoprim/sulfamethoxazole) 3×/week for 1 year to prevent relapse of ocular toxoplasmosis.
He underwent an angiography that revealed improvement of the lesions.
Clinically, the patient is doing well and is under prophylaxis with trimethoprim/sulfamethoxazole.
Discussion
Ocular toxoplasmosis does not need immune suppression to occur. It is thought to represent either a reactivation of congenital infection or a postnatally acquired infection by a parasite.1 In some areas, such as Brazil,2 it is the most common form of posterior uveitis in immunocompetent patients. The variable prevalence is thought to reflect geographic variation of the strains of T. gondii. Toxoplasmic chorioretinitis presents as a focal posterior uveitis sometimes with vitreous flocculation and extension to the anterior chamber showing the classic aspect of ‘headlight in the fog’. Unilateral lesions are more common with acquired toxoplasmosis. In contrast, congenital disease is bilateral in three quarters of patients and has a propensity to involve the macular region. When the lesion is characteristic, the demonstration of IgG serum antibody3 gives a presumptive diagnosis and allows initiation of specific therapy. In doubtful cases, it is possible to detect the parasite DNA by vitreous puncture and PCR for T. gondii.
Classic therapy is sulfadiazine and pyrimethamine. Folinate must be given in order to prevent pyrimethamine-induced pancytopenia and steroids can be given for sight-threatening lesions in order to control inflammation.
Some authorities advocate the addition of clindamycin to the protocol. Clindamycin is also an alternative therapy when sulfa drugs are not tolerated. Other effective drugs are spiramycin, atavaquone or azithromycin with or without pyrimethamine. Recent studies show that co-trimoxazole is also an effective therapy.4
Learning points.
Toxoplasmic chorioretinitis does not need immunocompromising to occur.
It is the most common cause of posterior uveitis in some countries, such as Brazil.
The aspect of the typical chorioretinal lesion along with a positive IgG for Toxoplasma allows the diagnosis.
In doubtful cases PCR can be performed to confirm diagnosis.
Footnotes
Contributors: MM and TM were involved in conception and design, drafting and revising, and final approval of the article. AG was involved in revising and final approval of the article. ACF was involved in collection of images and final approval of the article.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Perkins ES Ocular toxoplasmosis. Br J Ophthalmol 1973;57:1–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glasner PD, Silveira C, Kruszon-Moran D, et al. An unusually high prevalence of ocular toxoplasmosis in Southern Brazil. Am J Ophthalmol 1992;114:136–44 [DOI] [PubMed] [Google Scholar]
- 3.Ongkosuwito JV, Bosch-Driessen EH, Kijlstra A, et al. Serologic evaluation of patients with primary and recurrent ocular toxoplasmosis for evidence of recent infection. Am J Ophthalmol 1999;128:407–12 [DOI] [PubMed] [Google Scholar]
- 4.Opremcak EM, Scales DK, Sharpe MR, Trimethoprim-sulfamethoxazole therapy for ocular toxoplasmosis. Ophthalmology 1992;99:920–5 [DOI] [PubMed] [Google Scholar]


