Abstract
Bile duct injuries are a recognised complication of cholecystectomy and a number of options exist for their evaluation. A 44-year-old woman presented with a suspected biliary leak 11 days following an open cholecystectomy. Her medical history was significant for biliopancreatic diversion 2 years previously. An ultrasound scan demonstrated a perihepatic collection but no dilation of the biliary tree was observed. The patient's surgical history and the lack of biliary dilation precluded an endoscopic retrograde cholangiopancreatography or percutaneous transhepatic cholangiography, and she could not undergo an MR cholangiopancreatography due to claustrophobia. A CT cholangiogram was performed and clarified the location of the injury, facilitating operative identification and repair of the bile duct. CT cholangiography performed as a dynamic procedure is useful as a means of identifying bile duct injuries.
Background
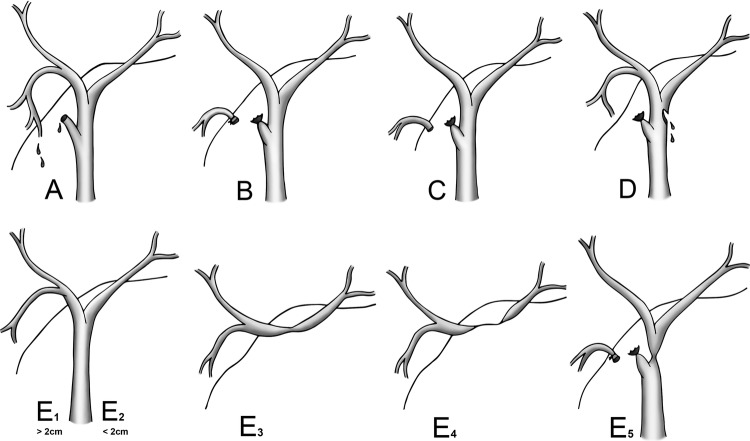
Iatrogenic bile duct injuries are an important complication of cholecystectomy, since despite being a rare occurrence, at 0.2% following open cholecystectomy, they are associated with significant morbidity and mortality.1 Bile duct injuries are classified according to the system devised by Strasberg et al2 into five types (A–E) with type E injuries being further divided 1–5.
Diagnosis of an iatrogenic bile duct injury is usually based on clinical suspicion and confirmed by means of ultrasound (USS) that would demonstrate a collection, and allow for targeted drainage. Endoscopic retrograde cholangiopancreatography (ERCP) is often used to define the type of injury, and dependent on the severity, may allow stent insertion and drainage of bile as definitive treatment. Our patient's previous surgery prohibited an endoscopic approach. Likewise the lack of biliary dilation made percutaneous transhepatic cholangiography (PTC) unfeasible.
An alternative approach would be an MR cholangiopancreatography (MRCP) although the presence of metallic clips in the postoperative state may have impaired the image quality. In the current case MRCP was not possible due to the patient's claustrophobia.
Case presentation
A 44-year-old woman was admitted as an emergency with acute onset diffuse right upper quadrant abdominal pain and vomiting. She had undergone a routine open cholecystectomy 11 days prior to her emergency admission at another institution. This had been noted to be a difficult procedure as a result of an open biliopancreatic diversion for morbid obesity 2 years previously. There had been a ‘minor injury’ to the common duct at the time of cholecystectomy that had been identified and immediately repaired with an absorbable suture.
On examination she was tender, mainly in the right upper quadrant with evidence of peritonism. An USS confirmed a large perihepatic collection extending into the subphrenic and subhepatic spaces, consistent with a collection or biloma. No intrahepatic or extrahepatic duct dilation was noted. The collection was drained with a pigtail catheter and bile obtained. The complex anatomy made ERCP impossible, and the non-dilated biliary system ruled out a PTC.
Furthermore, she was claustrophobic and had failed to tolerate an MRI during a previous hospital episode. In view of these difficulties, a CT cholangiogram (figure 1) was performed which demonstrated a high bile duct injury running from just below the confluence of the hepatic ducts into the common hepatic duct, a Strasberg type D injury (figure 2). Contrast was noted to be flowing freely through a defect in the wall of the duct into the subhepatic space and out through the drain.
Figure 1.
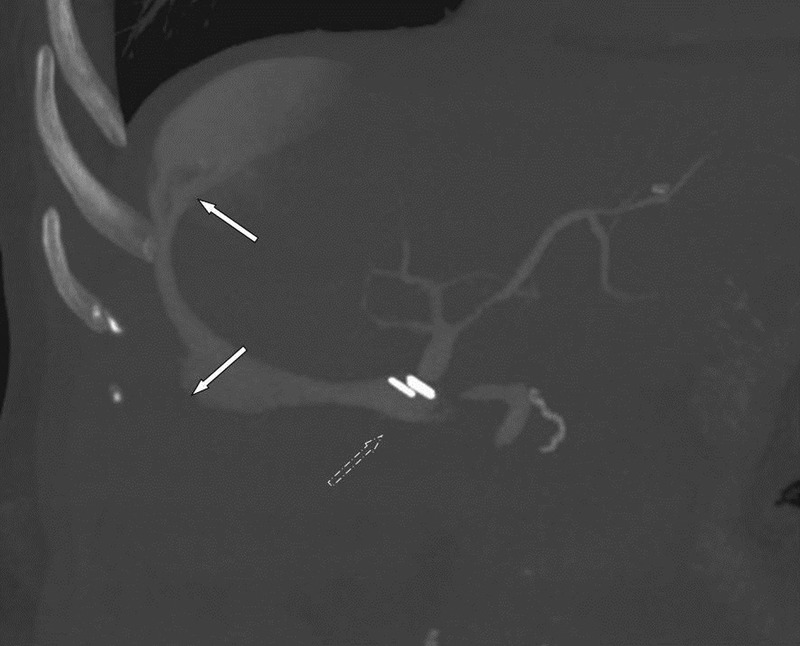
CT cholangiogram demonstrating a leak from the lateral wall of the common duct (broken arrow), with a large biloma extending laterally up to the subphrenic space also clearly identified (white arrows).
Figure 2.
Strasberg classification of bile duct injuries.
At laparotomy the defect was identified and corresponded exactly to the CT images. A Roux-en-Y hepaticojejunostomy was constructed and the peritoneal cavity thoroughly irrigated. Her postoperative recovery was uneventful and she remains asymptomatic at follow-up.
Discussion
There is very little literature on the role of CT cholangiography in the detection of bile leaks.3 4 Dinkel et al3 examined the role of CT cholangiography in nine patients who had undergone hepatobiliary surgery or sustained trauma. CT cholangiography confirmed biliary injury in seven patients and excluded bile duct trauma in two cases. Only one patient in the series went on to ERCP. In a more recent study, Kirk et al4 assessed 20 suspected bile leaks occurring following cholecystectomy. CT cholangiography was used as the primary investigation in seven cases, identifying the leak in six and excluding biliary injury thus allowing conservative management in the final patient. CT cholangiography also confirmed the anatomical location of the leak in five of six individuals. Unlike the clinical scenario we faced in the current case, none of the cases reported to date had any anatomical or psychological contraindication to ERCP, MRCP or PTC documented.
Interestingly, in patients such as those undergoing liver transplantation in whom, as in our case, ERCP and PTC are not always applicable due to postoperative anatomical changes; CT cholangiography has already proved to be a valued option for the demonstration of biliary integrity and bile duct patency.5
While ERCP and PTC have traditionally been the modalities of choice for evaluation of injuries of the biliary tree, the major complication rates are in the order of 6.85% for ERCP6 (pancreatitis, bleeding, infection and perforation) and 2% for PTC7 (sepsis, cholangitis, bile leak, haemorrhage and pneumothorax). Furthermore for ERCP, there is a procedure-related mortality of around 0.33%.6 In the case of CT cholangiography, the only potential complication is contrast allergy, which is seen in around 1 in 5000 patients.8
Another option for patients undergoing laparoscopic cholecystectomy is diagnostic laparoscopy and washout as this provides the potential for both diagnosis and management.9 If a leak is identified, depending on the type of defect observed, a direct repair may be attempted or the patient referred to a hepatobiliary surgeon for definitive management. Unfortunately, this approach was not appropriate in this case.
With the recent proliferation seen in hepatobiliary surgery, including a more than doubling of cholecystectomy rates in the laparoscopic era,10 the importance of developing a safe and reliable means of diagnosing bile leaks is becoming increasingly important. Leak rates following laparoscopic cholecystectomy are now around 0.2% and so similar to the open area.10 Although less commonly performed operations, the rates of biliary leaks following liver resection and transplantation are reported to be in the order of 5% and 2–25% respectively.11 12
While the literature on CT cholangiography in the evaluation of bile leaks is limited, the investigation would appear to provide a complication free means of evaluating patients. Of particular interest, is that the dynamic nature of CT cholangiography can demonstrate whether or not the leak is ‘on-going’ and thus further aid in guiding treatment.
Learning points.
CT cholangiography is effective in demonstrating the presence and site of a bile leak.
CT cholangiography can show whether or not the bile leak is ‘on-going’.
For patients with claustrophobia or with a contraindication to endoscopic retrograde cholangiopancreatography and percutaneous transhepatic cholangiography, CT cholangiography is the ideal investigation for demonstrating a bile leak.
Footnotes
Competing interests: None.
Patient consent: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Roslyn JJ, Binns GS, Hughes EF, et al. Open cholecystectomy: a contemporary analysis of 42,474 patients. Ann Surg 1993;218:129–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 1995;180:102–25 [PubMed] [Google Scholar]
- 3.Dinkel HP, Moll R, Gassel HJ, et al. Helical CT cholangiography for the detection and localization of bile duct leakage. Am J Roentgenol 1999;173:613–17 [DOI] [PubMed] [Google Scholar]
- 4.Kirk M, Kaplan E, Udayasiri R, et al. The Role of CT cholangiography in the detection and localisation of suspected bile leakage following cholecystectomy. Gastroenterol Res 2012;5:215–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller GA, Yeh BM, Breiman RS, et al. Use of CT cholangiography to evaluate the biliary tract after liver transplantation: initial experience. Liver Transpl 2004;10:1065–70 [DOI] [PubMed] [Google Scholar]
- 6.Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 2007;102:1781–8 [DOI] [PubMed] [Google Scholar]
- 7.Saad WEA, Wallace MJ, Wojak JC, et al. Quality improvement guidelines for percutaneous transhepatic cholangiography, biliary drainage, and percutaneous cholecystotomy. J Vasc Interv Radiol 2010;21:789–95 [DOI] [PubMed] [Google Scholar]
- 8.Gibson RN, Vincent JM, Speer T, et al. Accuracy of computed tomographic intravenous cholangiography (CT-IVC) with iotroxate in the detection of choledocholithiasis. Eur Radiol 2005;15:1634–42 [DOI] [PubMed] [Google Scholar]
- 9.Ahmad F, Saunders RN, Lloyd GM, et al. An algorithm for the management of bile leak following laparoscopic cholecystectomy. Ann R Coll Surg Engl 2007;89:51–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmad J, McElvanna K, McKie L, et al. Biliary complications during a decade of increased cholecystectomy rate. Ulster Med J 2012;81:79–82 [PMC free article] [PubMed] [Google Scholar]
- 11.Hoekstra LT, van Gulik TM, Gouma DJ, et al. Posthepatectomy bile leakage: how to manage. Dig Surg 2012;29:48–53 [DOI] [PubMed] [Google Scholar]
- 12.Ayoub WS, Esquivel CO, Martin P. Biliary complications following liver transplantation. Dig Dis Sci 2010;55:1540–6 [DOI] [PubMed] [Google Scholar]