Abstract
Objective: The relationship between specific distributions of isolated soleal vein thrombosis (SVT) and risk factors was investigated.
Subjects and Methods: The subjects included 93 patients with SVT diagnosed with ultrasonography.
Results: In the acute thrombus distribution, the thrombi of central veins were significantly more frequent than the thrombi of medial veins in the unilateral SVT. The thrombi of central veins were not more significantly frequent than the thrombi of medial veins in the bilateral SVT.
Conclusion: The risk factors of bilateral SVT are considered to be different from that of the unilateral SVT. (*English translation of J Jpn Coll Angiol 2013; 53: 159-166)
Keywords: soleal vein classification, isolated soleal vein thrombosis, ultrasonography, risk factor, recurrent factor
Introduction
Thrombi localized in the soleal veins (isolated thrombosis), which are the main sites of origination of lower limb deep vein thrombosis, disappear and recur depending on changes in risk factors, and secondarily propagate proximally and cause pulmonary embolism.1–3) Therefore, countermeasures against secondary diseases should be taken upon the diagnosis of isolated thrombosis,1,4–6) but these have not yet been presented in practical guidelines.7,8) To promote studies and treatment of isolated thrombosis, we proposed a soleal vein classification (vein classification) in 2009.9,10) The pathogenesis of recurrent isolated thrombosis has not yet been fully elucidated.11) Determination of an accurate vein classification-based relationship between the distribution characteristics and risk factors may lead to the identification of risk factors involved in recurrence (recurrent factors).
In this study, the association between the vein classification-based distribution characteristics and risk factors was investigated in patients with isolated thrombosis.
Subjects and Methods
The subjects were 93 patients with isolated thrombosis who underwent lower limb ultrasonography between June 2009, when the vein classification was initiated, and July 2011. Forty-one patients were diagnosed before June 2009, and examination was performed to evaluate thrombi after the initiation of treatment (treatment group). Fifty-two patients were diagnosed after June 2009, and examination was performed to evaluate thrombi before the initiation of treatment (pre-treatment group). In the pre-treatment group, the mean age was 71 ± 11 years old, male:female sex ratio was 16:36, and acute:chronic ratio was 26:26. In the treatment group, the mean age was 69 ± 10 years old, male:female sex ratio was 16:25, and acute:chronic ratio was 10:31, showing no significant differences between the 2 groups. The examination was performed for local and related symptoms and asymptomatic conditions in 40%, 60%, and 0% in the pre-treatment group (Table 1), and in 20%, 49%, and 31% in the treatment group, respectively. Significantly more patients had local symptoms in the pre-treatment group (P <0.05), whereas significantly more patients were asymptomatic in the treatment group (P <0.001).
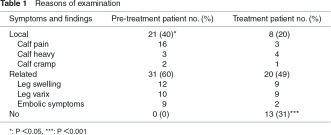
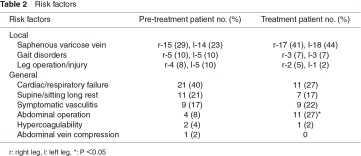
Risk factors of isolated thrombosis were divided into local risk factors influencing only the unilateral leg and systemic factors influencing bilateral legs (general factors) (Table 2). Of the local factors, varicose vein was most frequently noted, and no significant difference was noted in its incidence between the pre-treatment and treatment groups. Of the general factors, heart/respiratory failure was most frequently noted, followed by long rest, symptomatic vasculitis, and abdominal surgery in this order in the pre-treatment group, but the frequency of these factors decreased in the order of abdominal surgery, symptomatic vasculitis, and long rest in the treatment group, and abdominal surgery was significantly more frequent in the treatment group (P <0.05).
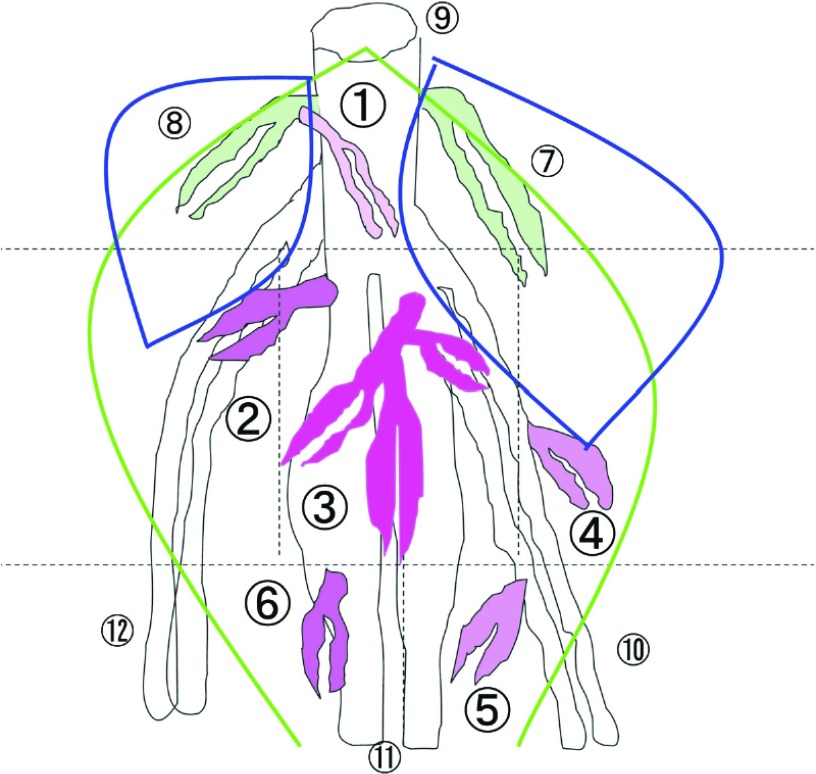
On the first visit, consultation and examination were performed. Lower limb ultrasonography and blood tests (D dimer and anti-nuclear antibody) were performed for isolated thrombosis, and echocardiography and contrast computed tomography (CT) were additionally performed for pulmonary embolism. For lower limb ultrasonography, an ultrasonograph of Toshiba (SSA-660A) and a 7.5-MHz linear probe were used. Combining the B-mode imaging with color Doppler method, the target veins were identified employing the squeezing and compression techniques, and thrombi were judged. The posture was set as sitting with the calf dropped. The bilateral thighs (common, deep, and superficial femoral veins) and bilateral calfs (popliteal, peroneal, posterior tibial, anterior tibial, gastrocnemial, and soleal veins) were examined.7) In the vein classification, the soleus muscle was divided into six circulatory regions, and intramuscular veins were divided into six groups: proximal, lateral, central, medial, distal medial, and distal lateral veins, based on the circulatory regions and deep veins communicated with intramuscular veins in these regions10) (Fig. 1). The soleal veins were investigated in this order. Isolated thrombosis was evaluated with regard to the location (uni- or bilateral and right or left leg), distribution (six vein groups), property (acute or chronic), and the total number of thrombi and numbers of chronic and acute thrombi were analyzed using the numbers of patients, legs, and vein groups as indices. In blood tests, D dimer was measured employing latex immune turbidimetry, and a level of 1 µg/mL or higher was regarded as abnormal. Anti-nuclear antibody was measured using the fluorescent antibody method, and an antibody titer of 40 times or higher was judged as positive.
Fig. 1.
Six groups of soleal veins in the right leg.  : proximal soleal vein,
: proximal soleal vein,  : lateral soleal vein,
: lateral soleal vein,  : central soleal vein,
: central soleal vein,  : medial soleal vein,
: medial soleal vein,  : distal medial soleal vein,
: distal medial soleal vein,  : distal lateral soleal vein,
: distal lateral soleal vein,  : medial gastrocnemial vein,
: medial gastrocnemial vein,  : lateral gastrocnemial vein,
: lateral gastrocnemial vein,  : popliteal vein,
: popliteal vein,  : posterior tibial veins,
: posterior tibial veins,  : peroneal veins,
: peroneal veins,  : anterior tibial veins.
: anterior tibial veins.
Regarding the course, the patients were periodically consulted (1 and 3 months after the initial examination and every 3 months thereafter) and additionally examined. Lower limb ultrasonography and blood tests were performed at 1, 3, and 6 months and every 6 months thereafter. Echocardiography was performed at 6 and 12 months and every 12 months thereafter.
The clinical disease stage (stage) was diagnosed as acute or chronic based on the findings on lower limb ultrasonography in consideration of symptoms and the D dimer level. In treatment, the acute stage was treated with anticoagulant therapy, and the chronic stage was treated with compression therapy (elastic bandage, elastic stocking), as a rule. All patients received instruction in physical therapy (crural muscle massage, ankle joint movement, and promotion of walking). Anticoagulant therapy was introduced with heparin or fondaparinux, and warfarin treatment was continued for 3 months or longer adjusting PT-INR to 1.5–2.0 (preventive administration) for cases without pulmonary embolism and 2.0–2.5 (therapeutic administration) for cases with pulmonary embolism. For recurrence after the initiation of treatment, warfarin was administered for one year or longer adjusting PT-INR to 2.0–2.5.
In terms of the statistical analysis, the results are presented as mean ± standard deviation. For between-group comparison with homogeneity of variance, the t-test was employed. For between-group comparison with heterogeneity of variance, the Cochran-Cox test was employed. For between-group comparison of rates, the χ2 test was performed. The significance level was set at P <0.05.
Results
1. Treatment
Of the 41 patients in the treatment group, 9 (22%), 21 (51%), and 11 (27%) were treated with anticoagulant, compression, and physical (alone) therapies, respectively.
2. Thrombus location
The thrombus locations and numbers of patients in the pre-treatment and treatment groups are shown in Table 3.
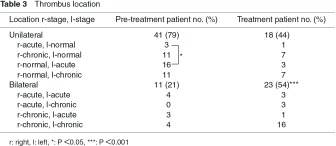
In the pre-treatment group, thrombi were noted in uni- and bilateral legs in 41 (79%) and 11 (21%) patients, respectively. The stage of unilateral thrombi was acute in 19 (46%) and chronic in 22 (54%) patients, and thrombi were present in the right leg in three and left leg in 16 in the acute cases, showing that the frequency was significantly higher in the left leg (P <0.05). The stage of bilateral thrombi was acute in 7 (64%) and chronic in 4 (36%). In the acute cases, thrombi were present in both legs in four and one leg in three, and in the right and left legs in 0 and 3 patients with thrombi in only one leg, respectively, but the difference was not significant.
In the treatment group, uni- and bilateral thrombi were noted in 18 (44%) and 23 (54%) patients, respectively. The stage of unilateral thrombi was acute in four (22%) and chronic in 14 (78%), and thrombi were noted in the right leg in one and left leg in three in the acute cases, showing no significant difference. The stage of bilateral thrombi was acute in 7 (30%) and chronic in 16 (70%). In the acute cases, thrombi were present in both legs in three and one leg in four, and in the right and left legs in three and 1 patient with acute thrombi in only one leg, respectively, showing no significant difference.
On comparison between the pre-treatment and treatment groups, the frequency of unilateral thrombi was not significantly different between the two groups, but that of bilateral thrombi was significantly higher in the treatment group (P <0.001).
3. Thrombus distribution
The uni- and bilateral thrombus distributions in the pre-treatment group are shown based on the number of legs in Table 4. Unilateral thrombi were noted in 41 patients (41 legs), and they were noted in single and multiple veins in 95% and 5%, respectively. In the single vein group, thrombi were present in the proximal, central, medial, and distal lateral veins in 3%, 82%, 12%, and 3%, respectively, showing that the frequency of central vein thrombus was significantly higher than that of medial vein thrombus (P <0.001). Bilateral thrombi were noted in 11 patients (22 legs), and these were present in single and multiple veins in 82% and 18%, respectively. In the single vein group, thrombi were present in the central, medial, distal medial, and distal lateral veins in 44%, 39%, 6%, and 11%, respectively, showing no significant difference between the central and medial veins. On comparison between the uni- and bilateral thrombus groups, no significant differences were noted in the rate of patients with single or multiple vein thrombi. However, in the single vein group, the incidence of central vein thrombus was significantly higher in the unilateral thrombus group (P <0.01), whereas the incidence of medial vein thrombus was significantly higher in the bilateral thrombus group (P <0.05). In all unilateral and bilateral thrombus patients, thrombi were present in single and multiple veins in 90% and 10% (57 and 6 legs), respectively. In the single vein group, thrombi were present in the proximal vein in one leg (2%), central vein in 40 legs (70%), medial vein in 12 legs (21%), lateral vein in 0 legs (0%), distal medial vein in one leg (2%), and distal lateral vein in three legs (5%).
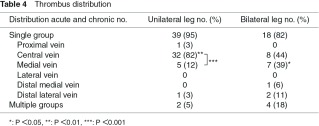
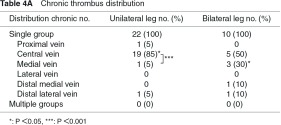
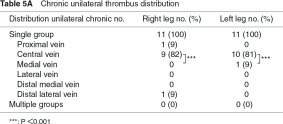
The chronic thrombus distribution is shown in Table 4A. In the unilateral thrombus group, thrombi were present in 22 patients (22 legs), in single veins in all patients. Thrombi were present in the proximal, central, medial, and distal lateral veins in 5%, 85%, 5%, and 5%, respectively, showing that the frequency in the central vein was higher than that in the medial vein (P <0.001). In the bilateral thrombus group, thrombi were noted in 10 legs (5 patients), and all were noted in single veins. Thrombi were present in the central, medial, distal medial, and distal lateral veins in 50%, 30%, 10%, and 10%, respectively, showing no significant difference between the central and medial veins. On comparison between the uni- and bilateral thrombus groups, there was no significant difference in the rate of patients with single or multiple vein thrombi, but the frequency in the central vein was significantly higher in the unilateral thrombus group (P <0.05), while that in the medial vein was significantly higher in the bilateral thrombus group (P <0.05).
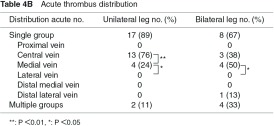
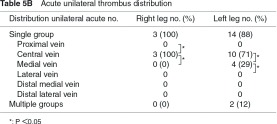
The acute thrombus distribution is shown in Table 4B. In the unilateral thrombus group, thrombi were present in 19 legs (19 patients), and they were present in single and multiple veins in 89% and 11%, respectively. In the single vein group, thrombi were present in the central and medial veins in 76% and 24%, respectively, and these were significantly higher than the frequencies in the other veins (P <0.05). The frequency in the central vein was significantly higher than that in the medial vein (P <0.01). Bilateral thrombi were noted in 6 patients (12 legs), and thrombi were present in single and multiple veins in 67% and 33%, respectively. In the single vein group, thrombi were present in the central, medial, and distal lateral veins in 38%, 50%, and 13%, respectively, showing that the frequencies in the central and medial veins were significantly higher than those in the proximal, lateral, and distal medial veins (P <0.05), and no significant difference was noted between the central and medial veins. On comparison between the uni- and bilateral thrombus groups, no significant difference was noted in single, multiple, or individual single group.
4. Unilateral thrombus distribution
The unilateral thrombus distributions in the right and left legs in the pre-treatment group are shown in Table 5. Thrombi were present in 14 right legs (14 patients) and all were present in single veins. Thrombi were present in the proximal, central, medial, and distal lateral veins in 7%, 86%, 0%, and 7%, respectively, showing that the frequency in the central vein was significantly higher than that in the medial vein (P <0.001). Thrombi were present in 27 left legs (27 patients), and these were present in single and multiple veins in 93% and 7%, respectively. In the single vein group, thrombi were present in the central and medial veins in 80% and 20%, respectively, showing that the frequency in the central vein was significantly higher than that in the medial vein (P <0.05). On comparison between the right and left legs, no significant difference was noted in single, multiple, or individual single group.
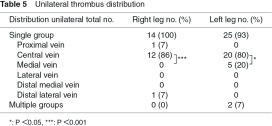
The chronic unilateral thrombus distributions in the right and left legs are shown in Table 5A. Thrombi were present in 11 right legs (11 patients), and all were present in single veins. Thrombi were present in the proximal, central, and medial veins in 9%, 82%, and 0%, respectively, showing that the frequency was significantly higher in the central than in the medial vein (P <0.001). Thrombi were present in 11 left legs (11 patients), and all were present in single veins. Thrombi were present in the central and medial veins in 81% and 9%, respectively, showing a significant difference (P <0.001). On comparison between the right and left legs, no significant difference was noted in single, multiple, or individual single group.
The acute unilateral thrombus distributions in the right and left legs are shown in Table 5B. Thrombi were present in three right legs (3 patients), and all were present in single veins. Thrombi were present in the central and medial veins in 100% and 0%, respectively, showing a significant difference (P <0.05). Thrombi were present in 16 left legs (16 patients), and these were present in single and multiple veins in 88% and 12%, respectively. In the single group, thrombi were present in the central and medial veins in 71% and 29%, respectively. The frequencies in the central and medial veins were significantly higher than those in the other veins (P <0.05), and the frequency in the central vein was significantly higher than that in the medial vein (P <0.05). On comparison between the right and left legs, no significant difference was noted in single, multiple, or individual single group.
5. Bilateral thrombus distribution
The thrombus distributions in the right and left legs were analyzed in the bilateral thrombus cases in the pre-treatment group. Thrombi were present in 11 right legs (11 patients), and these were present in single and multiple veins in 10 (91%) and one leg (9%), respectively. In the single vein group, thrombi were present in the central, medial, distal medial, and distal lateral veins in three (30%), five (50%), one (10%), and one (10%), respectively, and no significant difference was noted between the central and medial veins. Thrombi were present in 11 left legs (11 patients), and these were present in single and multiple veins in eight (73%) and three legs (27%), respectively. In the single vein group, thrombi were present in the central, medial, and distal lateral veins in five (63%), two (25%), and one (13%), respectively, and there was no significant difference between the central and medial veins. On comparison between the right and left legs, no significant difference was noted in single, multiple, or individual single group.
The chronic thrombus distributions in the right and left legs were analyzed. Thrombi were present in six right legs (6 patients), and all were present in single veins. These were present in the central, medial, distal medial, and distal lateral veins in two (33%), two (33%), one (17%), and one (17%), respectively, and no significant difference was noted between the central and medial veins. Thrombi were present in four left legs (4 patients) and all were present in single veins. These were present in the central and medial veins in three (75%) and one (25%), respectively, and no significant difference was noted between the central and medial veins. On comparison between the right and left legs, no significant difference was noted in single, multiple, or individual single group.
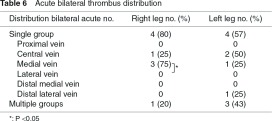
The acute thrombus distributions in the right and left legs are shown in Table 6. Thrombi were present in five right legs (5 patients), and 80% and 20% were present in single and multiple veins, respectively. In the single vein group, thrombi were present in the central and medial veins in 25% and 75%, respectively, showing no significant difference between these two veins, but the frequency in the medial vein was significantly higher in those in the other veins excluding the central vein (P <0.05). Thrombi were present in seven left legs (7 patients), and 57% and 43% were present in single and multiple veins, respectively. In the single vein group, thrombi were present in the central, medial, and distal lateral veins in 50%, 25%, and 25%, respectively, and there was no significant difference between the central and medial veins. On comparison between the right and left legs, no significant difference was noted in single, multiple, or individual single group.
Discussion
1. Diagnosis of isolated thrombosis
To analyze the characteristics of thrombi in the soleal veins, accurate definition and terminology of the veins and branches are necessary.6,11) In the vein classification, the soleus muscle was divided into six circulatory regions, and six vein groups were established based on these circulatory regions and deep veins communicated with intramuscular veins in these regions.9,10) Thrombi were diagnosed after the vein groups in the soleus muscle had been identified in the bilateral legs.7,12)
The identification of the vein groups was interfered with by displaced inflow due to differences in circulatory regions and venous joining sites from the definition and obstruction by chronic thrombi. When the central vein present in the largest circulatory region is obstructed or small, the lateral and central branches join the peroneal vein and the central and medial branches join the posterior tibial vein, which makes the identification difficult.9,10) If greater importance is attached to inflow veins, the lateral and medial veins can be called, but we should call the central vein due to displacement of the inflow sites, attaching greater importance to the circulatory regions. When the posterior tibial, medial, and distal medial veins are obstructed, their differentiation from the surrounding muscle may be difficult depending on the brightness of chronic thrombi, making the identification difficult.9,10) However, obstruction of the entire length of the vein is rare, and the veins were identified by applying ultrasonography through patent regions.
To diagnose thrombi, the thrombus detection limit and judgment of the thrombus properties were important. The thrombus detection limit was set at 2.0 mm based on the compressibility of veins on the compression techniques.11) The acute and chronic properties of thrombi were determined based on the venous thrombus ratio, brightness, and hardness.7) For acute thrombi, it is important to judge the possibility of recurrence based on the mixture of low (fresh) and high (funicular or calcified) brightness.6)
2. Evaluation of isolated thrombosis
The distribution and property of thrombi were investigated as their characteristics. The thrombus distribution was categorized based on differences of location in the bilateral legs (location characteristics) and differences in the distribution in each leg (distribution characteristics),6) and analyzed based on the numbers of total, chronic, and acute thrombi. Regarding the thrombus property, component differences in the forming process (composition characteristics) and age-related differences in the retracting process (structural characteristics) are involved,6,13) and chronic and acute thrombi were analyzed based on these.
In the analysis of acute thrombi, the location and distribution characteristics may reflect the frequency of thrombus formation at the time of examination, that is, the tendency for thrombosis.6,11) Accordingly, there is a possibility to identify recurrent factors in individual cases by selecting general factors from the location characteristics of the bilateral legs and local factors from the distribution characteristics of each leg in consideration of the living conditions and blood test findings.6,7,11) In addition, the risks for local and propagating recurrence may be predicted by considering recurrent factors with the composition and structural characteristics of thrombi in the individual vein groups.6,7)
3. Characteristics of isolated thrombosis
The frequency of bilateral thrombi was lower than that of unilateral thrombi in the pre-treatment group, as a location characteristic.6) However, it was revealed that the frequency of bilateral thrombi significantly rose in the treatment group compared with that in the pre-treatment group. This recurrence of bilateral thrombi may have involved blood-borne endothelial disorder, in addition to the low rate of patients treated with anticoagulant therapy.6,11)
Differences were also noted in the distribution characteristics between bilateral and unilateral thrombi. In acute thrombus distribution, the frequency of acute thrombi was higher in the central and medial veins than in the other veins. The frequency in the central vein was higher than that in the medial vein in unilateral thrombus cases, but no significant difference was noted between the two veins in bilateral thrombus cases. In addition, no difference in the incidence in the central or medial vein was noted between the unilateral and bilateral cases, nor was there laterality.
On the basis of these findings, the association between the thrombus characteristics and risk factors is discussed as follows: Strong general risk factors for recurrence may be involved in bilateral thrombi based on the location characteristics, and these may be different from those involved in unilateral thrombi.11) On the other hand, on the basis of the distribution characteristics, central and medial vein thrombi may involve larger diameters of these veins than those of the others as a local risk factor.9,10) Furthermore, on the basis of the differences between central and medial vein thrombi, local factors may be more strongly involved than general factors in unilateral thrombi,6,11) whereas the influence of general factors may be stronger than that of local factors for bilateral thrombi.
4. Recurrence of isolated thrombosis
Recurrence factors were investigated among the three local factors and 6 general factors determined based on the history of illness and examinations.6,7,11,14) Although the frequency of bilateral thrombi is low, the tendency for recurrence is strong, and the frequencies of the central and medial vein thrombi were equivalent, based on which enhanced coagulation and vasculitis are selected as general factors. Enhanced coagulation is a recurrence factor when female hormones and steroids are continuously administered, and vasculitis is a recurrence factor when Raynaud’s phenomenon is present.11) In cancer-bearing patients, cancer-derived coagulation-promoting substances, such as tissue factors, are tested.15) When enhanced coagulation and vasculitis are absent, coagulation inhibitors and autoantibodies are tested.7) In isolated thrombosis patients, coagulation inhibitor deficiency was noted in 5%, lupus anticoagulant was positive in 0%, and anti-nuclear antibody was positive in 63%.11) Anti-nuclear antibody was positive in 31.7% of normal subjects, and recurrence factors were suspected.16) When anti-nuclear antibody is negative, Burger disease is considered.11)
In unilateral thrombi, the frequency is high but the tendency for recurrence is weak, and thrombi are more likely to appear in the central vein than in the medial vein, based on which varicose vein and gait disturbance are selected as local factors.6,14) Heart/respiratory failure and long rest are also considered as additional general factors.6) For the left leg, involvement of left iliac vein compression is considered as an uneven factor.17,18) Additional general factors and uneven factors are considered to be involved complementarily to local factors and promote recurrence.6,11) Varicose vein and gait disturbance are judged as recurrence factors associated with crural muscle pump dysfunction. Regarding the volume load, the influence of primary non-saphenous varicose vein is weak, but the saphenous type promotes recurrence.14) Regarding pump failure, primary deep venous valve dysfunction may promote recurrence. More than 10 mm dilation or valve incompetence of the soleal veins, acting as the pump, is also considered to be involved in recurrence.2,9,11,14) Regarding crural muscle pump dysfunction, pump failure is more important than the volume load.14,19)
5. Origination and propagation of isolated thrombosis
The mechanism of the origination and propagation of soleal vein thrombi has not yet been fully elucidated.1–3) It is discussed as follows based on the vein classification and thrombus characteristics.
In isolated thrombosis patients, in addition to the causes of the initial onset, such as abdominal surgery, additional recurrence factors, such as gait disturbance, can be pointed out based on the history of illness. In addition, mixed presence of new and old thrombi is observed on lower limb ultrasonography, and isolated thrombosis may be mostly due to repetitive recurrence.6,11) The origin of isolated thrombosis in the vein classification may be the confluence of branches in the central vein, at which the frequency of thrombi is the highest, and the intermuscular membrane passage in the medial vein with the second highest frequency. For repetitive local recurrence, it is hypothesized that compression of veins by the crural muscles during sleep is also involved, in addition to the capture of veins by the arteries of the same name during walking.6,11)
Propagation recurrence and embolization are influenced by anatomical differences in the vein groups in the soleus muscle. On the basis of the vein classification, there are 3 pathways of proximal propagation from isolated thrombosis: the central pathway from the central and proximal veins to the popliteal vein, the medial pathway from the medial and distal medial veins to the posterior tibial vein, and the lateral pathway from the lateral and distal lateral veins to the peroneal vein.2,9,20) The frequencies of single venous thrombi were 72% in the central and proximal veins, 23% in the medial and distal medial veins, and 5% in the lateral and distal lateral veins, suggesting that the central pathway is the most frequent. However, central vein thrombi frequently propagated to the peroneal vein,1,3,6) suggesting that the lateral pathway is the most important.
6. Countermeasures against isolated thrombosis
When isolated thrombosis is diagnosed, countermeasures should be taken in consideration of the risk of recurrence based on evaluation of the properties and analysis of the characteristics.6,7) The stage is first judged based on the properties. When it is acute, the risk of recurrence is predicted based on analysis of the characteristics. In unilateral thrombi, the risks of local and propagation recurrence are low in medial vein thrombi, but central vein thrombi may have a risk of propagation recurrence. On the other hand, in bilateral thrombi, medial vein thrombi may have a risk of local recurrence, and central vein thrombi are at high risk of local and propagation recurrence. Effective treatment can be selected for isolated thrombosis patients by considering the risk of recurrence.
Conclusion
On the basis of the vein classification of isolated thrombosis, the frequencies of unilateral and bilateral single vein thrombi were 68% and 32%, and those of central, medial, and other veins were 70%, 21%, and 9%, respectively, in the pre-treatment group.
Regarding the acute thrombus distribution, the frequency of central vein thrombi was higher than that of medial vein thrombi in the unilateral thrombus cases, but there was no difference in the frequency between the central and medial veins in the bilateral thrombus cases.
It was suggested that bilateral thrombi involve risk factors different from those involved in unilateral thrombi in isolated thrombosis patients.
Disclosure Statement
The authors have no potential conflict of interest to be disclosed.
Footnotes
This article is English translation of J Jpn Coll Angiol 2013; 53: 159-166.
References
- Lohr JM, Kerr TM, Lutter KS, et al. Lower extremity calf thrombosis: to treat or not to treat. J Vasc Surg 1991; 14: 618-23 [DOI] [PubMed] [Google Scholar]
- Ohgi S, Tachibana M, Ikebuchi M, et al. Pulmonary embolism in patients with isolated soleal vein thrombosis. Angiology 1998; 49: 759-64 [DOI] [PubMed] [Google Scholar]
- Ro A, Kageyama N, Tanifuji T, et al. Pulmonary thromboembolism: overview and update from medicolegal aspects. Leg Med (Tokyo) 2008; 10: 57-71 [DOI] [PubMed] [Google Scholar]
- Gillet JL, Perrin MR, Allaert FA. Short-term and mid-term outcome of isolated symptomatic muscular calf vein thrombosis. J Vasc Surg 2007; 46: 513-9; discussion 519 [DOI] [PubMed] [Google Scholar]
- Lautz TB, Abbas F, Walsh SJ, et al. Isolated gastrocnemius and soleal vein thrombosis: should these patients receive therapeutic anticoagulation? Ann Surg 2010; 251: 735-42 [DOI] [PubMed] [Google Scholar]
- Ohgi S, Ohgi N. The relationship between isolated soleal vein thrombosis and pulmonary hypertension. J Jpn Coll Angiol 2012; 52: 353-9 (in Japanese) [Google Scholar]
- Ando M, Ito M, Ohgi S, et al. Guidelines for the Diagnosis, Treatment and Prevention of Pulmonary Thromboembolism and Deep Vein Thrombosis (JCS 2009). Tokyo: The Japanese Circulation Society, 2009: 41-9 (in Japanese) [DOI] [PubMed] [Google Scholar]
- Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141: e419S-94S [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohgi S, Iwai T, Ando M, et al. Frequency and normal size of soleal vein groups. Jpn J Phlebol 2011; 22: 263-9 (in Japanese) [Google Scholar]
- Ohgi S, Iwai T, Ando M, et al. Agreements on research commitee regarding the soleal intra-muscular veins. Jpn J Phlebol 2010; 21: 77-81 (in Japanese) [Google Scholar]
- Ohgi S, Ohgi N. Relation between isolated venous thrombi in soleal muscle and positive anti-nuclear antibody. Ann Vasc Dis 2012; 5: 321-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates SM, Jaeschke R, Stevens SM, et al. Diagnosis of DVT: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141: e351S-418S [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohgi S, Ito K, Tanaka K, et al. Echogenic types of venous thrombi in the common femoral vein by ultrasonic B-mode imaging. Vasc Surg 1991; 25: 253-8 [Google Scholar]
- Ohgi S. Intractable recurrence of isolated thrombi in soleal veins. Ann Vasc Dis 2010; 3: S205 [Google Scholar]
- Ohgi S, Kanaoka Y, Mori T, et al. Recurrent and multiple deep venous thrombosis due to high tissue factor activity in two patients with cancer. Jpn J Phlebol 1992; 3: 39-45 (in Japanese) [Google Scholar]
- Tan EM, Feltkamp TE, Smolen JS, et al. Range of antinuclear antibodies in “healthy” individuals. Arthritis Rheum 1997; 40: 1601-11 [DOI] [PubMed] [Google Scholar]
- Mitsuoka H, Ohta T, Hayashi S, et al. Histological study on the left common iliac vein spur. J Jpn Coll Angiol 2013; 53: 43-7 (in Japanese) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevitt S, Gallagher N. Venous thrombosis and pulmonary embolism. A clinico-pathological study in injured and burned patients. Br J Surg 1961; 48: 475-89 [DOI] [PubMed] [Google Scholar]
- Tachibana M, Hiroe T, Kanaoka Y, et al. Quantitative air-plethysmographic venous function and ambulatory venous pressure in patients with primary varicose vein. Int Angiol 2004; 23: 213-7 [PubMed] [Google Scholar]
- Ohgi S, Kanaoka Y, Maeda T, et al. Genesis of pulmonary embolus in lower limbs of deep vein thrombosis. Jpn J Phlebol 1994; 5: 211-6 (in Japanese) [Google Scholar]