Abstract
Background
Methylenetetrahydrofolate reductase (MTHFR) is a key enzyme of folate metabolic pathway which catalyzes the irreversible conversion of 5, 10-methylenetetrahydrofolate to 5-methyltetrahydrofolate. 5-methyltetrahydrofolate donates methyl group for the methylation of homocysteine to methionine. Several studies have investigated maternal MTHFR C677T polymorphism as a risk factor for DS, but the results were controversial and inconclusive. To come into a conclusive estimate, authors performed a meta-analysis.
Aim
A meta-analysis of published case control studies was performed to investigate the association between maternal MTHFR C677T polymorphism and Down syndrome.
Methods
PubMed, Google Scholar, Elsevier, Springer Link databases were searched to select the eligible case control studies using appropriate keywords. The pooled odds ratio (OR) with 95%confidence interval were calculated for risk assessment.
Results
Thirty four studies with 3,098 DS case mothers and 4,852 control mothers were included in the present meta-analysis. The pooled OR was estimated under five genetic models and significant association was found between maternal MTHFR 677C>T polymorphism and Down syndrome under four genetic models except recessive model (for T vs. C, OR = 1.26, 95% CI = 1.09–1.46, p = 0.001; for TT vs. CC, OR = 1.49, 95% CI = 1.13–1.97, p = 0.008; for CT vs. CC, OR = 1.29, 95% CI = 1.10–1.51, p = 0.001; for TT+CT vs. CC, OR = 1.35, 95% CI = 1.13–1.60, p = 0.0008; for TT vs. CT+CC, OR = 0.76, 95% CI = 0.60–0.94, p = 0.01).
Conclusion
The results of the present meta-analysis support that maternal MTHFR C677T polymorphism is a risk factor for DS- affected pregnancy.
Introduction
Down syndrome (DS) is the most common chromosomal disorder with the prevalence of 1/700–1000 live birth. It is characterized by the trisomy 21, which results from maternal meiotic nondisjunction in majority (90%) of cases. The established risk factor for DS is advanced (>35 years) maternal age at the time of conception. However, a fairly high number of DS children born to younger mothers suggest that risk factors other than advanced maternal age might be involved in predisposing younger mothers to DS-affected pregnancy [1], [2]. The molecular and biochemical mechanism of maternal meiotic non-disjunction is still not known. James et al. [3] reported that methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism might be a risk factor for maternal meiotic non-disjunction. Since then several studies have investigated the risk of DS to variants of folate pathway genes like MTHFR, Methionine synthase (MTR) and Methionine synthase reductase (MTRR) in Asian [1], [2], [4], [5] and Caucasian [6]–[8] populations. Folate deficiency and dysfunctional MTHFR causes abnormal DNA methylation [9], [10] and chromosomal segregation [11], [12]. Hypomethylation of the centromeric DNA has been suggested as the causative mechanism of meiotic non-disjunction. Abnormal DNA methylation of centromere lead to aberrant kinetochore formation that results into abnormal segregation of chromosomes during meiosis [3], [13].
MTHFR is a key enzyme in folate metabolism, which catalyzes the reduction of 5, 10-methylenetetrahydrofolate to the predominant circulating form of folate i.e. 5-methyltetrahydrofolate (5-THF). 5-THF donates methyl group for the conversion of homocysteine to methionine, which is further converted into S-adenosylmethionine (SAM). SAM is the main methyl group donor for all cellular methylation reactions. Folate deficiency and/or dysfunctional MTHFR reduces the conversion of 5, 10-methylene THF to 5-methyl THF, and elevates plasma homocysteine concentration. Both folate and MTHFR are involved in many complex biochemical reactions like DNA synthesis, repair and methylation.
There are more than 40 polymorphisms reported in MTHFR gene and among them C677T variant is the most studied and clinically important. The C677T variant (rs 1801133; Ala 222 Val) has been associated with a decreased activity of MTHFR, and increased homocysteine level [14]–[16]. Mutant homozygous (TT) individuals have a decreased enzymatic activity ∼ 70% and the heterozygote by 40%. A dysfunctional MTHFR leads to lower levels of SAM resulting into DNA hypomethylation. DNA hypomethylation increases the risk of many diseases and disorders like- neural tube defects [17], cleft lip and palate [18], Alzheimer disease [19], cardiovascular diseases [14], diabetes [20] and psychiatric disorders [21] etc. Several epidemiological studies have investigated the associations of the maternal MTHFR C677T polymorphism with Down syndrome. However, the results were conflicting and inconclusive. In light of the above facts, we conducted a meta-analysis of published case control studies relating the C677T polymorphism of the maternal MTHFR gene to the risk of having DS offspring.
Materials and Methods
Selection of studies
Electronic searches were conducted using PubMed, Google Scholar, Elsevier and Springer link and all published manuscripts up to January, 2014 were considered in present meta-analysis. The following index terms were used for search ‘MTHFR’ ‘Methylenetetrahydrofolate reductase’, and ‘C677T polymorphism’, ‘maternal risk’ and ‘Down syndrome’. In addition, bibliographies of all articles and reviews were hand searched for additional suitable studies.
Inclusion criteria
Included studies had to meet the following criteria: (1) article should be published; (2) article should have sufficient data to calculate the odds ratio with 95% CI; (3) article should be case control association study; and (4) author should describe the genotyping protocols.
Data extraction
The following data were extracted from each study: first author’s name, publication year, journal name, country name, genotyping method, and different MTHFR genotype numbers.
Meta-analysis
Statistical analysis of maternal MTHFR C677T polymorphism and DS risk was estimated by Odds ratio (ORs) with 95% confidence intervals (CIs). The heterogeneity was tested by the Q-statistics with p-values <0.05. Subgroup analysis was done to know the source of heterogeneity. If higher heterogeneity (I2>50%) would be observed, the random effect model [22] would be applied. Otherwise, fixed-effect model [23] was applied to obtain the summary OR and 95% CI. All p values were two-sided and a p value of less than 0.05 was considered statistically significant. All analyses were performed using the computer program MIX version 1.7 [24]. The control genotypes were tested for Hardy-Weinberg equilibrium (HWE) using the Goodness of fit Chi-square test. The quality of the included studies was measured according to the scoring system for randomized controlled association studies proposed by Clark and Baudouin [25]. Case control studies scoring <5 were defined as low quality study and those ≥5 were defined as high quality study.
Publication bias
Funnel plots of precision by log (OR) and standard error by log (OR) were plotted to determine publication bias and asymmetrical funnel plots represent publication bias. Begg and Mazumdar rank correlation [26] and Egger’s regression intercept [27] tests were adopted to assess the publication bias.
Results
Eligible Studies
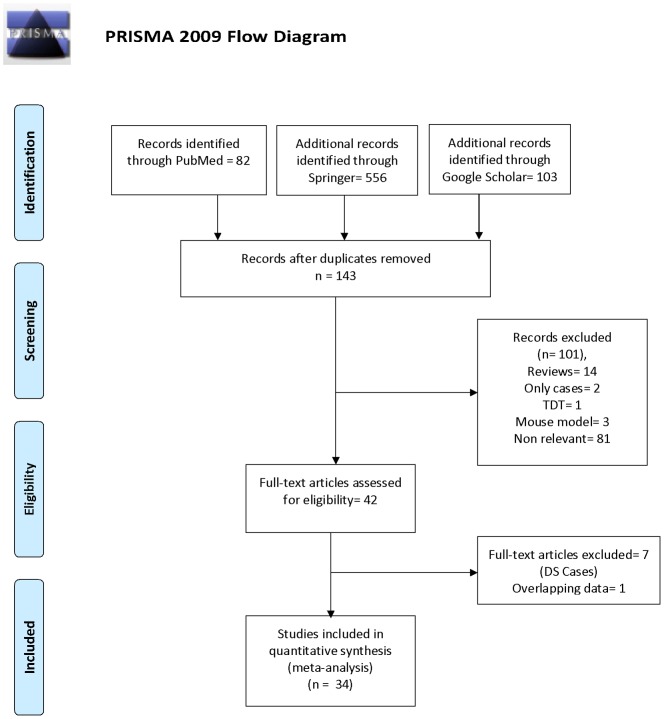
With our original search criterion, 85 articles were found. After reviewing each original article, 50 publications were excluded including reviews, case studies, editorials etc. (Figure 1). Following these exclusions, 34 individual case-control studies with a total of 3,098 cases and 4,852 controls were found to be suitable for inclusion into meta-analysis and listed in Table 1 (Figure 1).
Figure 1. Flow Diagram of Study Searching and Selection Process.
Table 1. Characteristics of the eligible studies included in the meta-analysis.
| Study | Year | Country | Case | Control | Quality Score | Reference |
| James et al. | 1999 | Canada | 50 | 57 | 7 | Am J Clin Nutr 70∶495-50 |
| Hobbs et al. | 2000 | America | 157 | 140 | 7 | Am J Hum Genet 67∶623–630 |
| Chadeaux-Vekemans et al. | 2002 | France | 85 | 70 | 5 | Pediatr Res 51∶766–767 |
| O’Leary et al. | 2002 | Ireland | 41 | 192 | 5 | Am J Med Genet A 107∶151–155 |
| Stuppia et al. | 2002 | Italy | 64 | 112 | 7 | Eur J Hum Genet 10∶388–390 |
| Boduroglu et al. | 2004 | Turkey | 158 | 91 | 5 | Am J Med Genet 127A: 5–10 |
| Acacio et al. | 2005 | Brazil | 70 | 88 | 8 | Prenat Diagn 25∶1196–1199 |
| Da Silva et al. | 2005 | Brazil | 154 | 158 | 7 | Am J Med Genet Part A 135A: 263–267 |
| Coppede et al. | 2006 | Italey | 79 | 111 | 7 | Am J Med Genet A 140(10): 1083–1091 |
| Liang et al. | 2006 | China | 30 | 70 | 7 | China J Modern Medicine 20∶011 |
| Rai et al. | 2006 | India | 149 | 165 | 6 | J Hum Genet 51∶278–283 |
| Scala et al. | 2006 | Italy | 94 | 256 | 8 | Genet Med 8∶409–416 |
| Wang et al. | 2007 | China | 100 | 100 | 8 | Zhonghua Yi Xue Yi Chuan Xue Za Zhi 24∶533–537 |
| Biselli et al. | 2008 | Brazil | 82 | 134 | 8 | Genet Mol Res 7∶33–42 |
| Kohli et al. | 2008 | India | 103 | 109 | 6 | Downs Syndr Res Pract 12∶133–137 |
| Martinez-Frias et al. | 2008 | Spain | 146 | 188 | 4 | Am J Med Genet A 146A(11): 1477–1482 |
| Meguid et al. | 2008 | Egypt | 42 | 48 | 7 | Dis Markers 24∶19–26 |
| Santos-Reboucas et al. | 2008 | Brazil | 103 | 108 | 7 | Dis Markers 25∶149–157 |
| Wang et al. | 2008 | China | 64 | 70 | 8 | J Zhejiang Univ Sci B 9(2): 93–99 |
| Brandalize et al. | 2009 | Brazil | 239 | 197 | 6 | Am J Med Genet 149A (10): 2080–2087 |
| Coppede et al. | 2009 | Italy | 94 | 113 | 8 | Neurosci Lett 449∶15–19 |
| Cyril et al. | 2009 | India | 36 | 60 | 6 | Indian J Hum Genet 15∶60–64 |
| Kokotas et al. | 2009 | Denmark | 177 | 984 | 6 | Dis Markers 27∶279–285 |
| Pozzi et al. | 2009 | Italy | 74 | 184 | 8 | Am J Obstet Gynecol 63: e1–e6 |
| Coppede et al. | 2010 | Italy | 29 | 32 | 5 | BMC Med Genomics 3∶42 |
| Liao et al. | 2010 | China | 60 | 68 | 7 | Yi Chuan 32(5): 461–466 |
| Vranekoviz et al. | 2010 | Croatia | 111 | 141 | 7 | Dis Markers 28∶293–298 |
| Bozovic et al. | 2011 | Croatia | 112 | 221 | 7 | Pediatr Int 53(4): 546–550 |
| Sadiq et al. | 2012 | Jordan | 53 | 29 | 6 | Genet Test Mol Biomarker 15∶1–7 |
| Tayeb | 2012 | Saudi Arabia | 30 | 40 | 5 | Egyptian J Med Hum Genet 13(3): 263–268 |
| Zampieri et al. | 2012 | Brazil | 105 | 185 | 8 | Dis Markers 32(2): 73–81 |
| Kaur and Kaur | 2013 | India | 110 | 111 | 6 | Indian J Hum Genet 19(4): 412–414 |
| Pandey et al. | 2013 | India | 81 | 99 | 6 | Int J Pharm Bio Sci; 4(2):(B)249–256 |
| Elsayed et al. | 2014 | Egypt | 26 | 61 | 9 | The Egyptian J Med Hum Genet 15(1): 39–44 |
These studies were published between 1999 and 2013. All these thirty four studies were performed in different countries- Brazil [28]–[33], China [4], [34]–[36], Croatia [8], [37], Egypt [38], [39], France [40], India [1], [5], [41]–[43], Ireland [44], Italy [7], [13], [45]–[48], Jordan [49], Netherlands [50], Saudi Arabia [2], Spain [51], Turkey [52] and USA [3], [6] (Table 1).
Characteristics of included studies
In thirty four studies included in the present meta-analysis, the smallest case sample size was 26 [39] and highest sample size was 239 [32]. ORs for more than one were reported in twenty four articles [1], [2], [4]–[6], [8], [13], [28]–[30], [32], [33], [35]–[39], [42], [43], [46]–[49], [51], [52]. Except two studies [28], [43], control populations of all articles were in Hardy-Weinberg equilibrium.
In all thirty four studies, total cases were 3,098 with CC (1,396), CT (1,326) and TT (376), and controls were 4,852 with CC (2,329), CT (2,015), and TT (508) genotypes. In controls genotypes, percentage of CC, CT and TT were 48.00%, 41.53%, and 10.47% respectively. In total cases, genotype percentage of CC, CT, and TT was 45.06%, 42.8% and 12.14% respectively. Frequencies of CC and CT genotypes were highest in both cases and controls (Table 2). In cases and controls, the allele C was the most common. All five genetic models; -allele contrast (T vs C) homozygote (TT vs CC), codominant (CT vs CC), dominant (TT+CT vs CC) and recessive (TT vs CT+CC) models were used to evaluate C677T polymorphism as DS risk.
Table 2. Distributions of MTHFR C677T genotypes and allele frequencies in DS case mothers and control mothers reported in different included studies.
| CC | CT | TT | C | T | |||||||
| Study | Country | Case | Control | Case | Control | Case | Control | Case | Control | Case | Control |
| James et al., 1999 | Canada | 24 | 15 | 22 | 34 | 4 | 8 | 70 | 64 | 30 | 50 |
| Hobbs et al., 2000 | America | 51 | 67 | 84 | 59 | 22 | 14 | 186 | 193 | 128 | 87 |
| Chadeaux-Vekemans et al., 2002 | France | 36 | 29 | 42 | 30 | 7 | 11 | 114 | 88 | 56 | 52 |
| O’Leary et al., 2002 | Ireland | 18 | 90 | 21 | 84 | 2 | 18 | 57 | 264 | 25 | 120 |
| Stuppia et al., 2002 | Italy | 20 | 27 | 32 | 62 | 12 | 23 | 72 | 116 | 56 | 108 |
| Boduroglu et al., 2004 | Turkey | 86 | 58 | 55 | 30 | 17 | 3 | 227 | 146 | 89 | 36 |
| Acacio et al., 2005 | Brazil | 35 | 54 | 30 | 25 | 5 | 9 | 100 | 133 | 40 | 43 |
| Da Silva et al., 2005 | Brazil | 67 | 84 | 72 | 67 | 15 | 7 | 206 | 235 | 102 | 81 |
| Coppede et al., 2006 | Italey | 20 | 39 | 43 | 54 | 16 | 18 | 83 | 132 | 75 | 90 |
| Liang et al., 2006 | China | 7 | 16 | 20 | 34 | 3 | 20 | 34 | 66 | 26 | 74 |
| Rai et al., 2006 | India | 97 | 124 | 40 | 39 | 12 | 2 | 234 | 287 | 64 | 43 |
| Scala et al., 2006 | Italy | 31 | 74 | 39 | 125 | 24 | 57 | 101 | 273 | 87 | 239 |
| Wang et al., 2007 | China | 28 | 48 | 52 | 42 | 20 | 10 | 108 | 138 | 92 | 62 |
| Biselli et al., 2008 | Brazil | 29 | 100 | 35 | 77 | 8 | 17 | 93 | 229 | 71 | 39 |
| Kohli et al., 2008 | India | 74 | 71 | 29 | 32 | 0 | 6 | 177 | 174 | 29 | 44 |
| Martinez-Frias et al., 2008 | Spain | 61 | 76 | 61 | 85 | 24 | 27 | 183 | 237 | 109 | 139 |
| Meguid et al., 2008 | Egypt | 20 | 33 | 17 | 12 | 5 | 3 | 57 | 78 | 27 | 18 |
| Santos-Reboucas et al., 2008 | Brazil | 51 | 49 | 43 | 47 | 9 | 12 | 145 | 145 | 61 | 71 |
| Wang et al., 2008 | China | 14 | 36 | 32 | 29 | 18 | 5 | 60 | 101 | 68 | 39 |
| Brandalize et al., 2009 | Brazil | 94 | 86 | 113 | 93 | 32 | 18 | 301 | 265 | 177 | 129 |
| Coppede et al., 2009 | Italy | 25 | 40 | 52 | 55 | 17 | 18 | 102 | 135 | 86 | 91 |
| Cyril et al., 2009 | India | 33 | 60 | 3 | 0 | 0 | 0 | 69 | 120 | 3 | 0 |
| Kokotas et al., 2009 | Denmark | 92 | 445 | 72 | 449 | 13 | 90 | 256 | 1339 | 98 | 629 |
| Pozzi et al., 2009 | Italy | 28 | 62 | 30 | 93 | 16 | 29 | 86 | 217 | 62 | 151 |
| Coppede et al., 2010 | Italy | 5 | 11 | 19 | 17 | 5 | 4 | 29 | 39 | 29 | 25 |
| Liao et al., 2010 | China | 12 | 23 | 26 | 33 | 22 | 12 | 50 | 79 | 70 | 57 |
| Vranekoviz et al., 2010 | Croatia | 49 | 66 | 49 | 64 | 13 | 11 | 147 | 196 | 75 | 86 |
| Bozovic et al., 2011 | Croatia | 46 | 101 | 55 | 97 | 11 | 23 | 147 | 299 | 77 | 143 |
| Sadiq et al., 2011 | Jordan | 23 | 23 | 27 | 5 | 3 | 1 | 73 | 51 | 33 | 7 |
| Tayeb, 2012 | Saudi Arabia | 16 | 22 | 10 | 14 | 4 | 4 | 42 | 58 | 18 | 22 |
| Zampieri et al., 2012 | Brazil | 40 | 94 | 55 | 73 | 10 | 18 | 135 | 261 | 75 | 109 |
| Kaur & Kaur, 2013 | India | 86 | 89 | 22 | 22 | 2 | 0 | 194 | 200 | 26 | 22 |
| Pandey et al., 2013 | India | 67 | 87 | 12 | 9 | 2 | 3 | 146 | 183 | 16 | 15 |
| Elsayed et al., 2014 | Egypt | 11 | 30 | 12 | 24 | 3 | 7 | 34 | 84 | 18 | 38 |
Meta-analysis
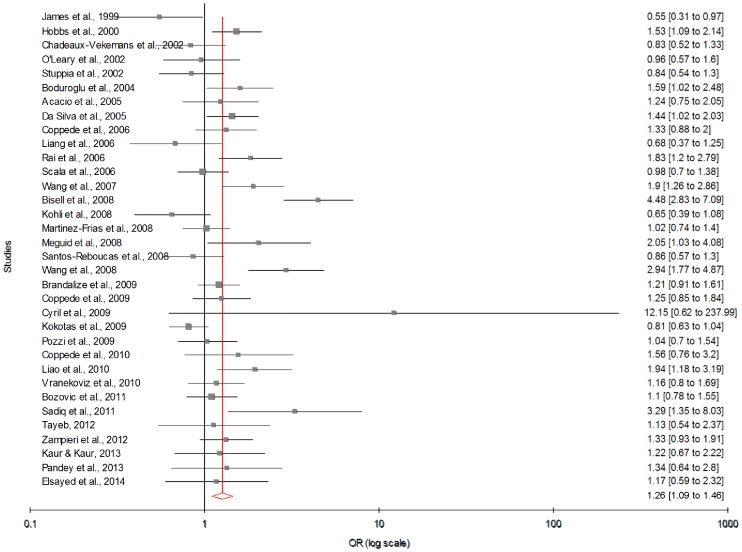
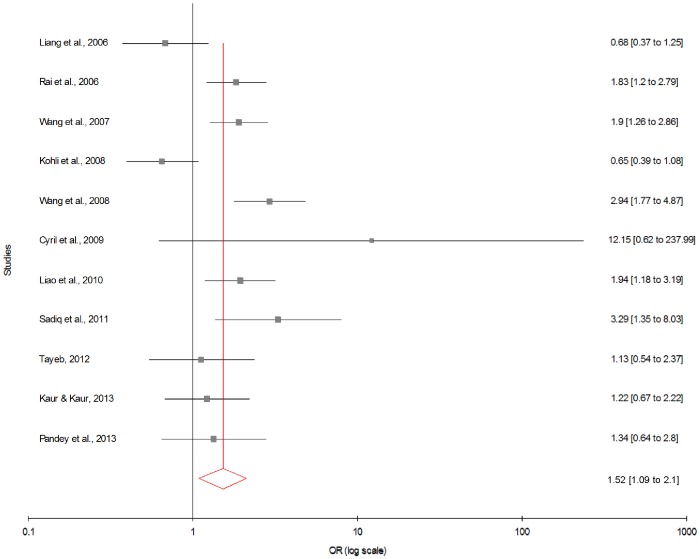
Meta-analysis with allele contrast showed significant association between maternal 677T allele and DS with both fixed effect (ORTvsC = 1.22; 95% CI = 1.13–1.31; p = <0.0001) and random effect models (ORTvsC = 1.26; 95% CI = 1.09–1.45; p = 0.001) (Figure 2) (Table 3). In cumulative meta-analysis using random effect model, the association of maternal T allele with DS turned statistically significant with the addition of study of Wang et al. (2008) and remained significant thereafter.
Figure 2. Forest plots (Random effect) showed significant association between MTHFR C677T polymorphism and risk of Down syndrome using allele contrast model (C versus T).
Results of individual and summary OR estimates and 95% CI of each study were shown. Horizontal lines represented 95% CI, and dotted vertical lines represent the value of the summary OR.
Table 3. Summary estimates for the odds ratio (OR) of MTHFR C677T in various allele/genotype contrasts, the significance level (p value) of heterogeneity test (Q test), the I2 metric and publication bias p-value (Egger Test) in total studies, Asian, American and European studies.
| GeneticContrast | Fixed effect OR(95% CI), p | Random effect OR(95% CI), p | Heterogeneityp-value (Q test) | I2 (%) | Publication Bias(p of Egger’s test) | |
| All | Allele Contrast (T vs. C) | 1.22 (1.13−1.31), <0.0001 | 1.26 (1.09−1.46), 0.001 | <0.0001 | 69.42 | 0.14 |
| Co-dominant (CT vs. CC) | 1.23 (1.11−1.36), <0.0001 | 1.29 (1.10−1.51), 0.001 | 0.0002 | 52.49 | 0.02 | |
| Homozygote (TT vs. CC) | 1.44 (1.22−1.69), <0.0001 | 1.49 (1.13−1.97), 0.008 | <0.0001 | 57.3 | 0.56 | |
| Dominant (TT+CT vs. CC) | 1.28 (1.16−1.41), <0.0001 | 1.35 (1.13−1.60), 0.0008 | <0.0001 | 63.56 | 0.05 | |
| Recessive (CT+CC vs. TT) | 0.76 (0.65−0.88), 0.0004 | 0.76 (0.60−0.94), 0.01 | 0.0044 | 43.68 | 0.926 | |
| Asian | Allele Contrast (T vs. C) | 1.53 (1.29−1.82), <0.0001 | 1.52 (1.09−2.1), 0.01 | 0.0003 | 69.43 | 0.82 |
| Co-dominant (CT vs. CC) | 1.52 (1.21−1.91), 0.0003 | 1.57 (1.14−2.14), 0.005 | 0.09 | 38.05 | 0.11 | |
| Homozygote (TT vs. CC) | 2.41 (1.62−3.59), <0.0001 | 2.21 (1.03−4.74), 0.0411 | 0.0074 | 60.04 | 0.204 | |
| Dominant (TT+CT vs. CC) | 1.64 (1.32−2.0), <0.0001 | 1.70 (1.18−2.4), 0.004 | 0.01 | 56.67 | 0.30 | |
| Recessive (CT+CC vs. TT) | 0.54 (0.37−0.78), <0.0001 | 0.58 (0.29−1.16), 0.12 | 0.0094 | 58.77 | 0.334 | |
| American | Allele Contrast (T vs. C) | 1.23 (1.07−1.39), 0.003 | 1.19 (0.99−1.44), 0.06 | 0.06 | 47.69 | 0.11 |
| Co-dominant (CT vs. CC) | 1.42 (1.17−1.71), 0.0002 | 1.42 (0.97−2.06), 0.066 | 0.0005 | 73.15 | 0.908 | |
| Homozygote (TT vs. CC) | 1.68 (1.24−2.28), 0.0008 | 1.58 (0.84−2.95), 0.148 | 0.0007 | 72.07 | 0.667 | |
| Dominant (TT+CT vs. CC) | 1.48 (1.24−1.76), <0.0001 | 1.44 (0.95−2.19), 0.078 | <0.0001 | 80.11 | 0.782 | |
| Recessive (CT+CC vs. TT) | 0.69 (0.51−0.92), 0.0136 | 0.72 (0.44−1.18), 0.203 | 0.0159 | 59.42 | 0.753 | |
| European | Allele Contrast (T vs. C) | 1.03 (0.93−1.15), 0.482 | 1.04 (0.93−1.16), 0.451 | 0.3576 | 8.81 | 0.084 |
| Co-dominant (CT vs. CC) | 0.99 (0.85−1.16), 0.956 | 1.00 (0.85−1.17), 0.992 | 0.3774 | 6.87 | 0.050 | |
| Homozygote (TT vs. CC) | 1.09 (0.87−1.37), 0.422 | 1.09 (0.85−1.40), 0.455 | 0.3715 | 7.45 | 0.329 | |
| Dominant (TT+CT vs. CC) | 1.02 (0.88−1.17), 0.787 | 1.03 (0.87−1.21), 0.704 | 0.308 | 13.58 | 0.041 | |
| Recessive (CT+CC vs. TT) | 0.90 (0.73−1.10), 0.322 | 0.90 (0.72−1.11), 0.339 | 0.570 | 0 | 0.948 |
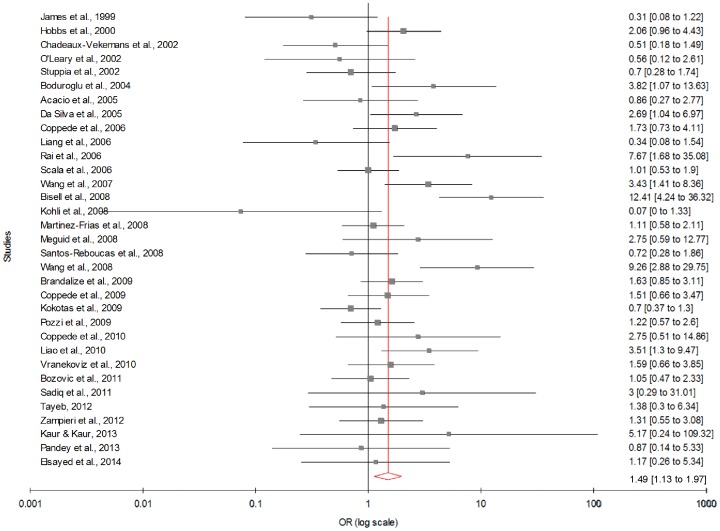
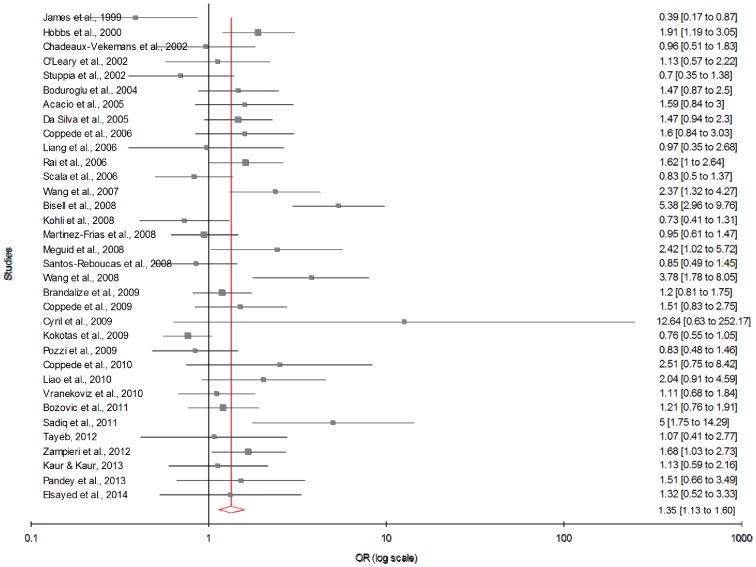
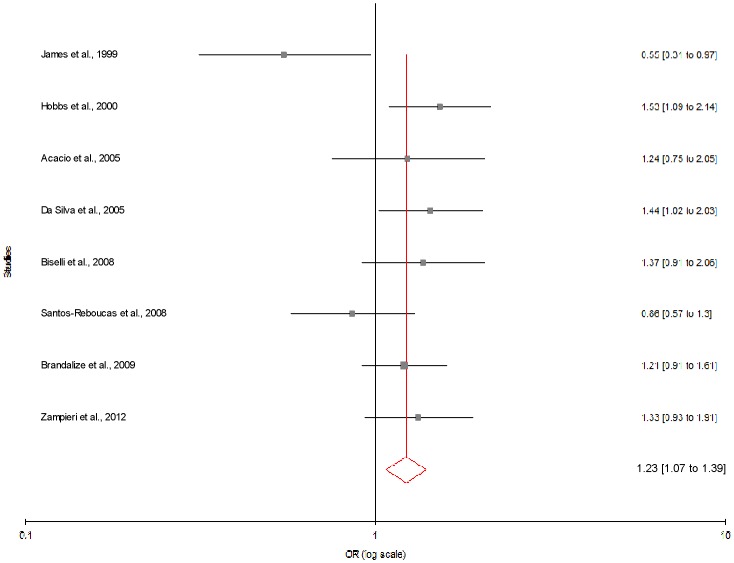
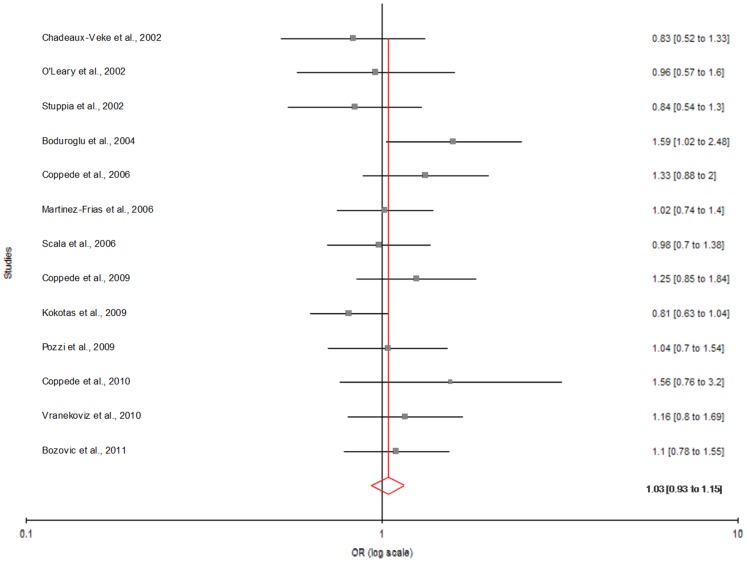
Table 3 summarizes the ORs with corresponding 95% CIs for association between maternal C677T polymorphism and risk of DS in dominant, recessive, homozygote and co-dominant models. With our primary analysis, there was an increased risk of DS among mutant homozygote variants (TT), with both fixed (ORTTvs.CC = 1.44; 95% CI = 1.22−1.69, p = <0.0001) and random (ORTTvs.CC = 1.49; 95% CI = 1.13−1.97, p = 0.008) effect models with moderate statistical heterogeneity between-study (Figure 3). Association of mutant heterozygous genotype (CT vs. CC) was observed significant with fixed (ORCTvs.CC = 1.23; 95% CI = 1.11−1.36; p = <0.0001) and random (ORCTvs.CC = 1.29; 95% CI = 1.10−1.51; p = 0.001) effect models. Similarly combined mutant genotypes (TT+CT vs. CC) showed significant association with DS using both fixed (ORTT+CTvs.CC = 1.28; 95% CI = 1.16−1.41; p = <0.0001) and random (ORTT+CTvs.CC = 1.35; 95% CI = 1.13−1.60; p = 0.0008) effect models (Figure 4).
Figure 3. Forest plots (Random effect) showed significant association between MTHFR C677T polymorphism and risk of Down syndrome.
Results of individual and summary OR estimates and 95% CI of each study were shown using homozygote model (TT versus CC).
Figure 4. Forest plots (Random effect) showed significant association between MTHFR C677T polymorphism and risk of Down syndrome using dominant model (TT+CT versus CC).
Results of individual and summary OR estimates and 95% CI of each study were shown.
Stratified analysis
We also performed sub-group analysis which is based on geographic distribution of population. Out of 34 studies included in present meta-analysis, 11 studies were from Asia, 13 from Europe, 8 from America and 2 from Africa. The subgroup analysis by geographical regions revealed that the significant association between the maternal MTHFR C677T polymorphism and DS existed in Asian population (for T vs. C: OR = 1.51; 95% CI = 1.09−2.10; p = 0.01; I2 = 69.43%; Pheterogeneity = 0.0003; PPb = 0.82) (Figure 5; Table 3). Except allele contrast model of American population (T vs. C: OR = 1.23; 95% CI = 1.07−1.39; p = 0.003; I2 = 47.69%; Pheterogeneity = 0.06; PPb = 0.11) (Figure 6) no significant association was found in American and European population (for T vs. C: OR = 1.03; 95% CI = 0.93−1.15; p = 0.482; I2 = 8.81%; Pheterogeneity = 0.357; PPb = 0.084) (Figures 7; Table 3).
Figure 5. Forest plots (Random effect) showed significant association between MTHFR C677T polymorphism and risk of Down syndrome in Asian studies using allele contrast model (T versus C).
Results of individual and summary OR estimates and 95% CI of each study were shown.
Figure 6. Forest plots (Random effect) showed no association between MTHFR C677T polymorphism and risk of Down syndrome in American studies using allele contrast model (T versus C).
Results of individual and summary OR estimates and 95% CI of each study were shown.
Figure 7. Forest plots (Fixed effect) showed no association between MTHFR C677T polymorphism and risk of Down syndrome in European studies using allele contrast model (T versus C).
Results of individual and summary OR estimates and 95% CI of each study were shown. Horizontal lines represented 95% CI, and dotted vertical lines represent the value of the summary OR.
Heterogeneity and Sensitive analysis
A true heterogeneity existed between studies for allele (Pheterogeneity = <0.0001, Q = 107.92, df = 33, I2 = 69.42%, t2 = 0.12) and mutant genotypes (Pheterogeneity = <0.0001, Q = 74.90, df = 32, I2 = 57.3%, t2 = 0.10) comparisons. The ‘I2’ value of more than 50% for between studies comparison in both allele and genotype analysis shows high level of true heterogeneity. In Asian (Pheterogeneity = 0.0003, I2 = 67.43%) and American (Pheterogeneity = <0.0001, I2 = 83.25%) allele contrast meta-analysis significant high heterogeneity was observed, in European sub-group meta-analysis low heterogeneity was observed (Pheterogeneity = 0.357, I2 = 8.81) in allele contrast model.
In allele contrast meta-analysis, sensitivity analysis performed by exclusion of the studies in which control population was not in Hardy Weinberg equilibrium, studies with small sample size and studies with high p values. Control population of only two studies [28], [43] were not in HW equilibrium and heterogeneity did not decreased after exclusion of these studies (p = <0.0001, I2 = 70.00%). Exclusion of seven studies with small sample size, less than 50 (O’Leary et al. [44], n = 41; Liang et al. [34], n = 30; Mequid et al [38], n = 42; Cyril et al. [42], n = 36; Coppede et al. [48], n = 29; Tayeb [2], n = 30; Elsayed et al. [39], n = 26), also did not decreased heterogeneity (Pheterogeneity = <0.0001, I2 = 72.98%). Similarly exclusion of eleven studies with very high p value (O’Leary et al. [44], p = 0.87; Acacio et al. [28], p = 0.40; Scala et al. [7], p = 0.91; Martinez-Frias et al. [51], p = 0.90; Pozzi et al. [13], p = 0.84;Vranekoviz et al. [37], p = 0.43; Bozovic et al. [8], p = 0.58; Tayeb [2], p = 0.74; Elsayed et al. [39], p = 0.65; Kaur and Kaur [5], p = 0.52; Pandey et al. [43], p = 0.44) did not decrease heterogeneity but increased odds ratio (OR = 1.29, 95% CI = 1.18−1.41, p = <0.0001).
Publication bias
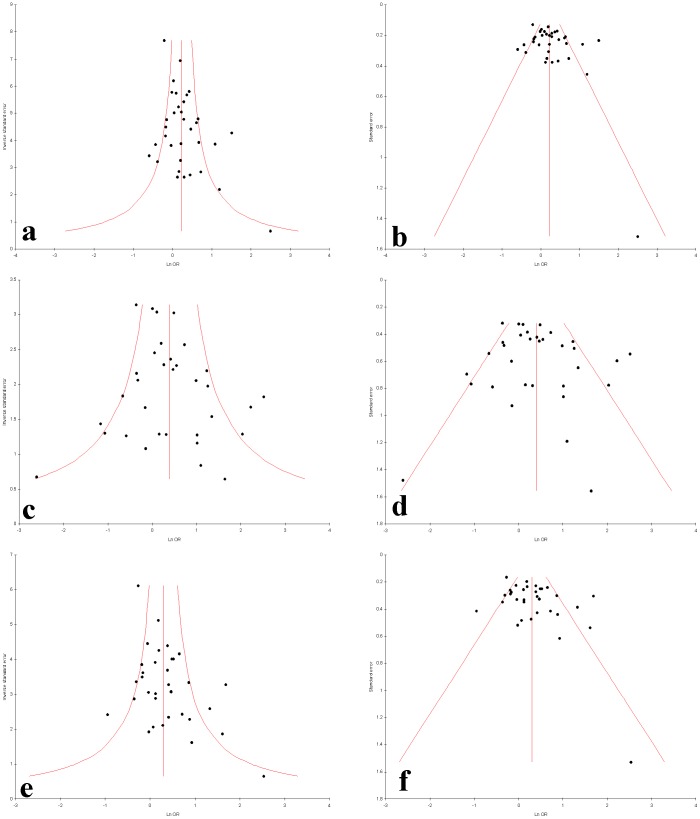
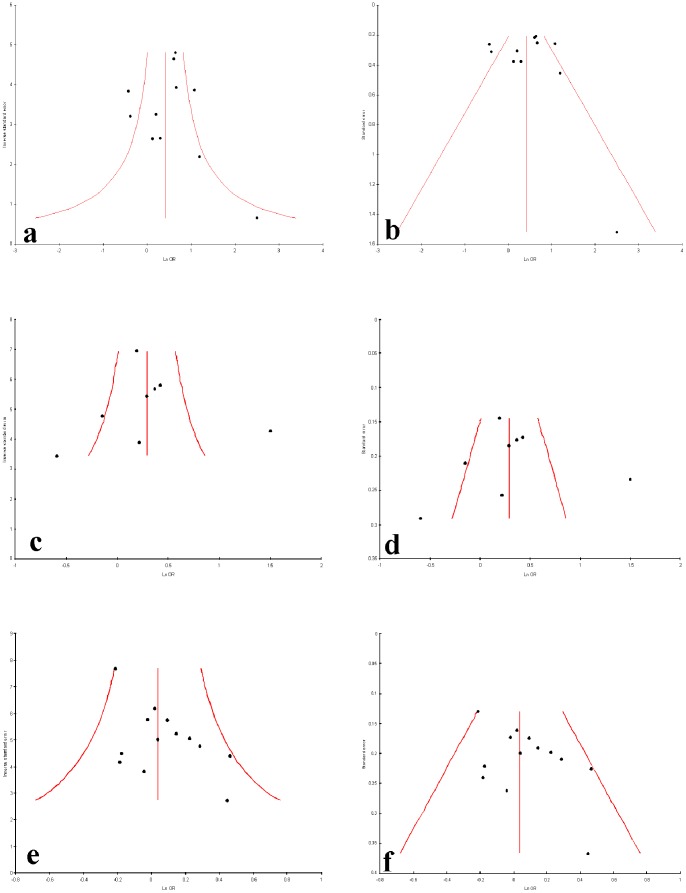
Publication bias was not observed in allele contrast, homozygote, dominant and recessive models (Begg’s p = 0.28, Egger’s p = 0.14 for T vs. C; Begg’s p = 0.38, Egger’s p = 0.56 for TT vs. CC; Begg’s p = 0.13, Egger’s p = 0.05 for TT+CT vs. CC and Begg’s p = 0.19, Egger’s p = 0.0.05 for TT vs. CC+CT) but publication bias was observed in co-dominant model (Begg’s p = 0.04, Egger’s p = 0.02 for CT vs. CC) of overall by using Begg’s and Egger’s test (Table 3). Funnel plots were showed in Figures 8 and 9.
Figure 8. Funnel plots a−f. a.
Precision by log odds ratio for additive model; b. standard error by log odds ratio for additive model; c. precision by log odds ratio for co-dominant model; d. standard error by log odds ratio for co-dominant model; e. precision by log odds ratio for dominant model; f. standard error by log odds ratio for Dominant model.
Figure 9. Funnel plots a−f. a.
Precision by log odds ratio for additive model; b. standard error by log odds ratio for additive model for Asian studies; c. precision by log odds ratio for additive model; d. standard error by log odds ratio for additive model for American studies; e. precision by log odds ratio for additive model; f. standard error by log odds ratio for additive model for European studies.
Discussion
In 1999, James et al [3] reported that genetic polymorphism of folate and homocysteine pathway enzymes predispose a woman to abnormal chromosome segregation, which act as risk factor for DS pregnancy. In subsequent years, several in vivo studies in humans suggested that chronic folate deficiency has been associated with abnormal DNA methylation [11], [53], [54], and aberrant chromosome segregation [6], . Population-based studies have shown that folic acid intake during fetal development has a protective effect, resulting in a significant reduction in the occurrence of developmental defects, like neural tube defects (NTD), congenital heart defects, limb defects, and orofacial clefts [60].
Meta-analysis is a powerful tool for analyzing cumulative data with small and low power studies. Several meta-analyses were published accessing MTHFR as risk factor to various diseases/disorders like- neural tube defects [61], [62], cleft lip and palate [63], stroke [64], psychiatric disorders [65]. During literature search, we identified four meta-analyses [66]–[69] published between 2007 and 2013. They examined the effect of maternal MTHFR C677T as DS risk, but no consistent conclusion was achieved. Zintzaras [66] performed a meta-analysis based on eleven studies and did not find any significant association between the maternal MTHFR polymorphisms and DS risk. Medica et al. [67] aggregated sixteen studies and reported significant relationship between the maternal mutant genotypes (TT+CT vs CC) and risk of DS child. Recently, Wu et al. [68] published a meta-analysis (included twenty eight studies with 2806 cases/4597 controls), and found statistical association with dominant model (OR = 1.305, 95% CI = 1.125–1.514, p = 0, p = 0.003). Yang et al. [69] performed a meta-analysis which was based on twenty six studies (2458 cases/3144 controls) and found statistically significant association in allele contrast model (OR = 1.28; 95% CI: 1.11–1.47) (Table 4). Several newly published studies were not included in the previous published meta-analyses. So authors conducted a comprehensive meta-analysis with the largest number of studies (34 studies). In the present meta-analysis significant association was found between maternal C677T polymorphism and DS risk in total 34 studies using all five genetic models. Whereas in stratified analysis, except allele contrast model in American population, no significant association was observed in European and American population but significant higher risk was found in Asian population. Such phenomenon probably could be ascribed to the folate metabolism profile and dietary structure of different regions.
Table 4. A comparative analysis of details of Odds Ratio, 95% CI, genetic models reported in total 5 (including present) meta-analysis published so far analyzing case-control studies of MTHFR C677T polymorphism and Down syndrome.
| Study | Number of Studies | Cases | Controls | I2 (%) | Heterogeneity p-value (Q test) | OR (95% CI), p-value | Model | Subgroup analysis |
| Zintaras, 2007 | 11 | 1129 | 1489 | 49 | 0.03 | 1.20 (1.06–1.35) | Allelic contrast | Not reported |
| Medica et al., 2009 | 16 | 1545 | 2052 | – | – | 1.40 (1.16–1.70), 0.0006 | Dominant model | Not reported |
| Yang et al., 2013 | 26 | 2458 | 3144 | 58.2 | <0.01 | 1.28 (1.11–1.47) | Allelic contrast | Reported |
| Wu et al., 2013 | 28 | 2806 | 4597 | 48.0 | 0.0 | 1.224 (1.085–1.38), 0.001 | Dominant model | Reported |
| Present Study, 2014 | 34 | 3048 | 4852 | 69.42 | <0.0001 | 1.26 (1.09–1.46), 0.001 | Allelic contrast | Reported |
There are few limitations of the present meta-analysis like- i) we used crude ORs in the pooled analysis without adjustment; ii) the relatively small sample size in some of the included studies, especially those from Asia; iii) we considered only one gene polymorphism (MTHFR C677T) of folate pathway. Present meta-analysis had several advantages/strength to the previous published meta-analyses like- (i) the publication bias was not detected in present meta-analysis, (ii) pooled number of cases and controls from different studies significantly increased the statistical power of the analysis, (iii) largest number of studies (34 studies) with largest sample size (3,098 cases and 4,852 controls) was included in the present meta-analysis, (iv) controls included in the present meta-analysis was mothers of healthy child, (v) distribution of genotypes in control mothers except two studies was in Hardy-Weinberg equilibrium, (vi) significant association was found between maternal MTHFR C677T polymorphism and DS risk in allelic contrast, homozygote, co-dominant and dominant genetic models and (vii) in addition we did sub-group analysis according to geographical regions.
In conclusion, results of present meta-analysis suggest that the maternal MTHFR 677T allele is a risk factor for development of DS pregnancy. However the results of present meta-analysis were based on single gene polymorphism and significant heterogeneity was also observed; hence results should be interpreted with caution.
Supporting Information
PRISMA checklist.
(DOC)
Funding Statement
The authors have no support or funding to report.
References
- 1. Rai AK, Singh S, Mehta S, Kumar A, Pandey LK, et al. (2006) MTHFR C677T and A1298C polymorphisms are risk factors for Down’s syndrome in Indian mothers. J Hum Genet 51: 278–283. [DOI] [PubMed] [Google Scholar]
- 2. Tayeb MT (2012) The methylenetetrahydrofolate reductase gene variant (C677T) in risk mothers with Down syndrome among Saudi population. Egyptian J Med Hum Genet 13(3): 263–268. [Google Scholar]
- 3. James SJ, Pogribna M, Pogribny IP, Melnyk S, Hine RJ, et al. (1999) Abnormal folate metabolism and mutation in the methylenetetrahydrofolate reductase gene may be maternal risk factors for Down syndrome. Am J Clin Nutr 70: 495–50. [DOI] [PubMed] [Google Scholar]
- 4. Wang SS, Qiao F, Feng L, Juan-Juan LV (2008) Polymorphisms in genes involved in folate metabolism as maternal risk factors for Down syndrome in China. J Zhejiang Univ Sci B 9(2): 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kaur A, Kaur A (2013) Prevalence of methylenetetrahydrofolate reductase 677 C-T polymorphism among mothers of Down syndrome children. Indian J Hum Genet 19(4): 412–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hobbs CA, Sherman SI, Yi P, Torfs CP, Hine RJ, et al. (2000) Polymorphism in genes involved in folate metabolism as maternal risk factors for Down syndrome. Am J Hum Genet 67: 623–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Scala I, Granese B, Sellitto M, Salome S, Sammartino A, et al. (2006) Analysis of seven maternal polymorphisms of genes involved in homocysteine/folate metabolism and risk of Down syndrome offspring. Genet Med 8: 409–416. [DOI] [PubMed] [Google Scholar]
- 8. Božović IB, Vraneković J, Cizmarević NS, Mahulja-Stamenković V, Prpić I, et al. (2011) MTHFR C677T and A1298C polymorphisms as a risk factor for congenital heart defects in Down syndrome. Pediatr Int 53(4): 546–550. [DOI] [PubMed] [Google Scholar]
- 9. James SJ, Melnyk S, Pogribna M, Pogribny IP, Caudill MA (2002) Elevation in S-adenosylhomocysteine and DNA hypomethylation: potential epigenetic mechanism for homocysteine-related pathology. J Nutr 132 8 Suppl: 2361S–2366S. [DOI] [PubMed] [Google Scholar]
- 10. Pogribny IP, James SJ, Jernigan S, Pogribna M (2004) Genomic hypomethylation is specific for preneoplastic liver in folate/methyl deficient rats and does not occur in non-target tissues. Mutat Res. 548(1–2): 53–59. [DOI] [PubMed] [Google Scholar]
- 11. Pogribna M, Melnyk S, Pogribny I, Chango A, Yi P, et al. (2001) Homocysteine metabolism in children with Down syndrome: in vitro modulation. Am J Hum Genet 69: 88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Parry EM, Parry JM, Corso C, Doherty A, Haddad F, et al. (2002) Detection and characterization of mechanisms of action of aneugenic chemicals. Mutagenesis. 17(6): 509–521. [DOI] [PubMed] [Google Scholar]
- 13. Pozzi E, Vergani P, Dalpra’ L, Combi R, Silvestri D, et al. (2009) Maternal polymorphisms for methyltetrahydrofolate reductase and methionine synthetase reductase and risk of children with Down syndrome. Am J Obstet Gynecol 63: e1–e6. [DOI] [PubMed] [Google Scholar]
- 14. Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, et al. (1995) A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 10: 111–113. [DOI] [PubMed] [Google Scholar]
- 15. Bagley PJ, Selhub J (1998) A common mutation in the methylenetetrahydrofolate reductase gene is associated with an accumulation of formylated tetrahydrofolates in red blood cells. Proc Natl Acad Sci USA 95(22): 13217–13220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brattström L, Wilcken DE, Ohrvik J, Brudin L (1998) Common methylenetetrahydrofolate reductase gene mutation leads to hyperhomocysteinemia but not to vascular disease: the result of a meta-analysis. Circulation 98(23): 2520–2526. [DOI] [PubMed] [Google Scholar]
- 17. van der Put NM, Eskes TK, Blom HJ (1997) Is the common 677CT mutation in the methylenetetrahydrofolate reductase gene a risk factor for neural tube defects? A meta-analysis. Q J Med 90: 111–115. [DOI] [PubMed] [Google Scholar]
- 18. Blanton SH, Henry RR, Yuan Q, Mulliken JB, Stal S, et al. (2011) Folate pathway and nonsyndromic cleft lip and palate. Birth Defects Res A Clin Mol Teratol 91: 50–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hua Y, Zhao H, Kong Y, Ye M (2011) Association between the MTHFR gene and Alzheimer’s disease: a meta-analysis. Int J Neurosci 121(8): 462–71. [DOI] [PubMed] [Google Scholar]
- 20. Benes P, Kankova K, Muzik J, Groch L, Benedik J, et al. (2001) Methylenetetrahydrofolate reductase polymorphism, typeII diabetes mellitus, coronary artery disease, and essential hypertension in the Czech population. Mol Genet Metab 73: 188–195. [DOI] [PubMed] [Google Scholar]
- 21. Jönsson EG, Larsson K, Vares M, Hansen T, Wang AG, et al. (2008) Two methylenetetrahydrofolate reductase gene (MTHFR) polymorphisms, schizophrenia and bipolar disorder: an association study. Am J Med Genet B Neuropsychiatr Genet 147B: 976–982. [DOI] [PubMed] [Google Scholar]
- 22. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Controlled Clinical Trials. 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 23. Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22: 719–748. [PubMed] [Google Scholar]
- 24. Bax L, Yu LM, Ikeda N, Tsuruta H, Moons KG (2006) Development and validation of MIX: comprehensive free software for meta-analysis of causal research data. BMC Med Res Methodol. 2006 6: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Clark MF, Baudouin SV (2006) A systematic review of the quality of genetic association studies in human sepsis. Intensive Care Med 32(11): 1706–1712. [DOI] [PubMed] [Google Scholar]
- 26. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4): 1088–1101. [PubMed] [Google Scholar]
- 27. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Acácio GL, Barini R, Bertuzzo CS, Couto EC, Annichino-Bizzacchi JM, et al. (2005) Methylenetetrahydrofolate reductase gene polymorphisms and their association with trisomy 21. Prenat Diagn 25: 1196–1199. [DOI] [PubMed] [Google Scholar]
- 29. da Silva LRJ, Vergani N, Galdieri LC, Porto MPR, Longhitano SB, et al. (2005) Relationship between polymorphisms in genes involved in homocysteine metabolism and maternal risk for Down syndrome in Brazil. Am J Med Genet Part A 135A: 263–267. [DOI] [PubMed] [Google Scholar]
- 30. Biselli JM, Goloni-Bertollo EM, Zampieri BL, Haddad R, Eberlin MN, et al. (2008) Genetic polymorphisms involved in folate metabolism and elevated plasma concentrations of homocysteine: maternal risk factors for Down syndrome in Brazil. Genet Mol Res 7: 33–42. [DOI] [PubMed] [Google Scholar]
- 31. Santos-Reboucas CB, Corre∧a JC, Bonomo A, Fintelman-Rodrigues N, Moura KC, et al. (2008) The impact of folate pathway polymorphisms combined to nutritional deficiency as a maternal predisposition factor for Down syndrome. Dis Markers 25: 149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Brandalize AP, Bandinelli E, dos Santos PA, Roisenberg I, Schüler-Faccini L (2009) Evaluation of C677T and A1298C polymorphisms of the MTHFR gene as maternal risk factors for Down syndrome and Congenital heart defects. Am J Med Genet 149A (10): 2080–2087. [DOI] [PubMed] [Google Scholar]
- 33. Zampieri BL, Biselli JM, Goloni-Bertollo EM, Vannucchi H, Carvalho VM, et al. (2012) Maternal risk for Down syndrome is modulated by genes involved in folate metabolism. Dis Markers 32(2): 73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Liang X, Feng Z, Lan-Fang Z, Guo XX, Xiao GF, et al. (2005) Analysis of Down syndrome screening and antenatal diagnosis of 3195 cases in the middle period of pregnancy. China J Modern Medicine 20: 011. [Google Scholar]
- 35. Wang W, Xie W, Wang X (2007) The relationship between polymorphism of gene involved in folate metabolism, homocysteine level and risk of Down syndrome. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 24: 533–537. [PubMed] [Google Scholar]
- 36. Liao YP, Bao MS, Liu CQ, Liu H, Zhang D (2010) Folate gene polymorphism and the risk of Down syndrome pregnancies in young Chinese women. Yi Chuan 32(5): 461–466. [DOI] [PubMed] [Google Scholar]
- 37. Vranekovic’ J, Babic’ Bozovic’ I, Starcevic’ Cizmarevic’ N, Buretic’- Tomljanovic’ A, Ristic’ S, et al. (2010) Functional inference of methylenetetrahydrofolate reductase gene polymorphisms on enzyme stability as a potential risk factor for Down syndrome in Croatia. Dis Markers 28: 293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Meguid NA, Dardir AA, Khass M, Hossieny LE, Ezzat A, et al. (2008) MTHFR genetic polymorphism as a risk factor in Egyptian mothers with Down syndrome children. Dis Markers 24: 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Elsayed GM, Elsayed SM, Ezz-Elarab SS (2013) Maternal MTHFR C677T genotype and septal defects in offspring with Down syndrome: A pilot study. The Egyptian J Med Hum Genet 15(1): 39–44. [Google Scholar]
- 40. Chadefaux-Vekemans B, Coude M, Muller F, Oury JF, Chabli A, et al. (2002) Methylenetetrahydrofolate reductase polymorphism in the etiology of Down syndrome. Pediatr Res 51: 766–767. [DOI] [PubMed] [Google Scholar]
- 41. Kohli U, Arora S, Kabra M, Ramakrishnan L, Gulati S, et al. (2008) Prevalence of MTHFR 677C>T polymorphism in north Indian mothers having babies with Trisomy 21 Down syndrome. Downs Syndr Res Pract 12: 133–137. [DOI] [PubMed] [Google Scholar]
- 42. Cyril C, Rai P, Chandra N, Gopinath PM, Satyamoorthy K (2009) MTHFR gene variants C677T A1298C and association with Down syndrome: a case–control study from South India. Indian J Hum Genet 15: 60–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pandey SK, Mohanty PK, Polipalli SK, Kapoor S (2013) Genetic polymorphisms of MTHFR (677T and 1298C) and homocysteine metabolism as maternal risk factor for Down’s syndrome patients in north indian population. Int J Pharm Bio Sci 4(2): (B)249–256. [Google Scholar]
- 44. O’Leary VB, Parle-McDermott A, Molloy AM, Kirke PN, Johnson Z, et al. (2002) MTRR and MTHFR polymorphism: link to Down syndrome? Am J Med Genet A 107: 151–155. [DOI] [PubMed] [Google Scholar]
- 45. Stuppia L, Gatta V, Gaspari AR, Antonucci I, Morizio E, et al. (2002) C677T mutation in the 5,10-MTHFR gene and risk of Down syndrome in Italy. Eur J Hum Genet 10: 388–390. [DOI] [PubMed] [Google Scholar]
- 46. Coppedè F, Marini G, Bargagna S, Stuppia L, Minichilli F, et al. (2006) Folate gene polymorphisms and the risk of Down syndrome pregnancies in young Italian women. Am J Med Genet A 140(10): 1083–1091. [DOI] [PubMed] [Google Scholar]
- 47. Coppede’ F, Migheli F, Bargagna S, Siciliano G, Antonucci I, et al. (2009) Association of maternal polymorphisms in folate metabolizing genes with chromosome damage and risk of Down syndrome offspring. Neurosci Lett 449: 15–19. [DOI] [PubMed] [Google Scholar]
- 48. Coppedè F, Grossi E, Migheli F, Migliore L (2010) Polymorphisms in folate-metabolizing genes, chromosome damage, and risk of Down syndrome in Italian women: identification of key factors using artificial neural networks. BMC Med Genomics 3: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sadiq MF, Al-Refai EA, Al-Nasser A, Khassawneh M, Al-Batayneh Q (2011) Methylenetetrahydrofolate reductase polymorphisms C677T and A1298C as maternal risk factors for Down syndrome in Jordan. Genet Test Mol Biomarker 15: 1–7. [DOI] [PubMed] [Google Scholar]
- 50. Kokotas H, Grigoriadou M, Mikkelsen M, Giannoulia-Karantana A, Petersen MB (2009) Investigating the impact of the Down syndrome related common MTHFR 677C[T polymorphism in the Danish population. Dis Markers 27: 279–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Martínez-Frías ML (2008) The biochemical structure and function of methylenetetrahydrofolate reductase provide the rationale to interpret the epidemiological results on the risk for infants with Down syndrome. Am J Med Genet A 146A(11): 1477–1482. [DOI] [PubMed] [Google Scholar]
- 52. Boduroğlu K, Alanay Y, Koldan B, Tunçbilek E (2004) Methylenetetrahydrofolate reductase enzyme polymorphisms as maternal risk for Down syndrome among Turkish women. Am J Med Genet 127A: 5–10. [DOI] [PubMed] [Google Scholar]
- 53. Balaghi M, Wagner C (1993) DNA methylation in folate deficiency: use of CpG methylase. Biochemical and Biophysical Research Communications 193: 1184–1190. [DOI] [PubMed] [Google Scholar]
- 54. Fenech M (2001) The role of folic acid and Vitamin B12 in genomic stability of human cells. Mutat Res 475: 57–67. [DOI] [PubMed] [Google Scholar]
- 55. Libbus BL, Borman LS, Ventrone CH, Branda RF (1990) Nutritional folate deficiency in CHO cells: chromosomal abnormalities associated with perturbations in nucleic acid precursors. Cancer Genet Cytogenet 46: 231–242. [DOI] [PubMed] [Google Scholar]
- 56. Leyton BL, Mergudich D, del la Torre D, Sans J (1995) Impaired chromosome segregation in plant anaphase alter moderate hypomethylation of DNA. Cell Prolif 28: 481–496. [DOI] [PubMed] [Google Scholar]
- 57. Pogribny IP, Basnakian AG, Miller BJ, Lopatina NG, Poirier LA, et al. (1995) Breaks in genomic DNA and within the p53 gene are associated with hypomethylation in livers of folate/methyl-deficient rats. Cancer Res 55(9): 1894–1901. [PubMed] [Google Scholar]
- 58. Chen RZ, Pettersson U, Beared C, Jackson-Grusby I, Jaenisch R (1998) DNA hypomethylation leads to elevated mutation rates. Nature 395: 89–93. [DOI] [PubMed] [Google Scholar]
- 59. Titenko-Holland N, Jacob RA, Shang N, Balaraman A, Smith MT (1998) Micronuclei in lymphocytes and exfoliated buccal cells of postmenopausal women with dietary changes in folate. Mutat Res 417: 101–114. [DOI] [PubMed] [Google Scholar]
- 60. Botto LD, Yang Q (2000) 5, 10-methylenetetrahydrofolate reductase variants and congenital anomalies: A huge review. Am J Epidemiol 151: 862–877. [DOI] [PubMed] [Google Scholar]
- 61. Zhang T, Lou J, Zhong R, Wu J, Zou L, et al. (2013) Genetic Variants in the Folate Pathway and the Risk of Neural Tube Defects: A Meta-Analysis of the Published Literature. PLos One 8: e59570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yadav U, Kumar P, Yadav SK, Mishra OP, Rai V (2014) Polymorphisms in folate metabolism genes as maternal risk factor for Neural Tube Defects: an updated meta-analysis. Metab Brain Dis. [Ahead of Print; DOI: 10.1007/s11011–014–9575–7]. [DOI] [PubMed]
- 63. Zhao M, Ren Y, Shen L, Zhang Y, Zhou B (2014) Association between MTHFR C677T and A1298C Polymorphisms and NSCL/P Risk in Asians: A Meta-Analysis. Plos One 9(3): e88242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Yadav S, Hasan N, Marjot T, Khan MS, Prasad K, et al. (2013) Detailed Analysis of Gene Polymorphisms Associated with Ischemic Stroke in South Asians. PLos One 8: e57305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Peerbooms OL, van Os J, Drukker M, Kenis G, Hoogveld L, et al. (2011) Meta-analysis of MTHFR gene variants in schizophrenia, bipolar disorder and unipolar depressive disorder: evidence for a common genetic vulnerability? Brain Behav Immun 25(8): 1530–1543. [DOI] [PubMed] [Google Scholar]
- 66. Zintzaras E (2007) Maternal gene polymorphisms involved in folate metabolism and risk of Down syndrome offspring: a meta analysis. J Hum Genet 52: 943–953. [DOI] [PubMed] [Google Scholar]
- 67. Medica I, Maver A, Augusto GF, Peterlin B (2009) Polymorphisms in genes involved in folate metabolism as maternal risk factors for Down syndrome- meta-analysis. Cent Eur J Med 4: 395–408. [Google Scholar]
- 68. Wu X, Wang X, Chan Y, Jia S, Luo Y, et al. (2013) Folate metabolism gene polymorphisms MTHFR C677T and A1298C and risk for Down syndrome offspring: a meta-analysis. Eur J Obstet Gynecol Reprod Biol 167(2): 154–159. [DOI] [PubMed] [Google Scholar]
- 69. Yang M, Gong T, Lin X, Qi L, Guo Y, et al. (2013) Maternal gene polymorphisms involved in folate metabolism and the risk of having a Down syndrome offspring: a meta-analysis. Mutagenesis 28(6): 661–671. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOC)