Abstract
Objective
Sensory over-responsivity (SOR) refers to an exaggerated, intense, or prolonged behavioral response to ordinary sensory stimuli. The relationship of SOR to psychiatric disorders remains poorly understood. The current study examined the SOR construct within typically developing children with clinically significant anxiety, including the prevalence and course of SOR symptoms and relationship between SOR symptoms, demographic factors, and psychopathology.
Method
Children presenting at an anxiety specialty clinic (n = 88) completed a psychiatric diagnostic assessment, which included parent-report measures of SOR, anxiety, obsessive-compulsive disorder (OCD), and global behavior and child-report measures of anxiety, depression, and OCD.
Results
SOR symptoms were very common: 93.2% were bothered by at least one tactile or auditory sensation, and the mean number of bothersome sensations was 9.2 (SD = 7.4). SOR symptoms were reported to be “moderately bothersome” on average and to onset at an early age. Sensory Over-Responsivity Inventory (SensOR) scores did not differ by psychiatric disorder diagnosis, but SensOR scores significantly correlated with measures of obsessive compulsive disorder (OCD) and depression. Higher SensOR scores were associated with greater global impairment.
Conclusion
A high rate of SOR symptom occurrence was observed in this sample of children seeking anxiety treatment, suggesting that SOR may not be entirely independent of anxiety and may be closely associated with OCD. Future research on the validity and nosology of SOR using psychiatric samples is warranted.
Keywords: sensory, anxiety, obsessive compulsive disorder, depression, psychopathology
Sensory over-responsivity (SOR) refers to an exaggerated, intense, or prolonged behavioral response to ordinary sensory stimuli.1 Although many terms have been used to label this phenomenon (e.g., sensory intolerance, hypersensitivity, hyper-responsiveness, sensory defensiveness, sensory-processing sensitivity), all share a core symptom description of a heightened and atypical reaction to sensory stimulation to a degree that impacts daily functioning. SOR is most commonly reported in association with tactile and auditory stimuli, such as clothing textures, sticky substances, and alarms or sirens.2 Developmental research suggests that elevated SOR symptoms are early-emerging, chronic, and associated with child and family impairment and increased risk for social and emotional problems.3,4
SOR symptoms have long been recognized in the field of occupational therapy,5 but the relation of SOR to psychopathology has only begun to be studied in recent years. Existing data suggest that SOR occurs both concurrently and independently of psychiatric disorders, leading to debate about the proper nosological classification and diagnostic validity of SOR.6,7 SOR is not currently recognized in the International and Statistical Classification of Diseases and Related Health Problems8 and is included in the recent revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)9 only as a symptom of autism spectrum disorders (despite evidence that SOR is not specific to autism).10 The Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood-Revised (DC:0–3R)11 includes the provisional diagnostic category, “Regulation Disorder of Sensory Processing,” of which “hypersensitive” is a subtype (along with other provisional symptom clusters such as hyposensitive and sensory stimulation-seeking). Although this is the most commonly used DC:0–3R category, diagnostic reliability is poor among experts and existing criteria lack empirical backing.11,12
Therefore, there is no universally agreed upon operational definition of SOR, nor are there established criteria upon which to identify clinically significant SOR symptoms or to differentiate SOR from other symptoms or disorders. Controversy over how to properly conceptualize and classify SOR is largely due to limited data concerning the construct’s clinical significance, etiology, and relationship to existing psychiatric diagnoses in terms of distinct clinical characteristics and rates of co-occurrence.
Recent research indicates that SOR does occur independently of existing DSM diagnoses. Two large scale studies examined rates of SOR and co-occurring DSM-IV13 diagnoses in well-characterized, population-based samples of typically developing children (i.e., children without cognitive disabilities or autism spectrum disorders).3,14,15 Both samples were school-aged children (7–10 years old;3 7 years old15) whose parents completed a structured diagnostic interview (Diagnostic Interview Schedule for Children)16 and the Sensory Over-Responsivity Inventory (SensOR),17 a parent-report measure of SOR in the tactile and auditory domains. SOR status was based on the SensOR but criteria differed in each study, such that children were classified has having SOR if parents endorsed ≥ 4 items in the Carter et al. study and ≥ 6 tactile or ≥ 4 auditory items in the Van Hulle et al. study. Across both studies, SOR was found to occur in isolation in approximately 8–15% of children. SOR co-occurred with DSM-IV disorders in about 5–12% of children, such that about 25–60% of children with SOR also met criteria for a psychiatric disorder.
Rates of co-occurrence between SOR and specific DSM diagnoses remain unclear. Most research to date has focused on SOR among those with autism spectrum disorders (ASD), and estimates of SOR and ASD co-occurrence range from 23%18 to 56%.19 While some have viewed this high rate of co-occurrence as evidence that SOR is specific to ASD (as DSM 5 criteria imply), other evidence indicates that these results may be better attributable to a general maturational delay. For example, Baranek et al.10 found that mental age was an equally strong predictor of hyperresponsiveness across groups of children with autism, developmental delays, and typical development, such that increased mental age was associated with decreased hyperresponsivity across all three groups. The authors concluded that SOR may reflect an important developmental, transdiagnostic process rather than a specific ASD symptom or distinct syndrome.
Among typically developing children, there are speculations in the literature that SOR is more common in those with anxiety disorders, attention-deficit hyperactivity disorder (ADHD), and oppositional defiant disorder (ODD). However, this information is largely based on anecdotal case reports,20,21 studies using a broader definition of sensory problems14 (e.g., including both over- and under-responsiveness), and research using unsystematically diagnosed or poorly characterized samples. In the Carter et al.3 and Van Hulle et al.15 studies, rates of specific psychiatric disorders were not reported, but the rate of diagnoses within the broad domains of internalizing disorders among those with SOR ranged from 10.0%3 to 70.4%15 and externalizing disorders from 18.5%3 to 50.4%.15
In order to better understand the relationship of SOR to psychopathology, quantitative research examining the construct within well-characterized clinical samples is needed. One particular clinical sample that warrants further examination in this regard is children with anxiety disorders. Anxiety is one of the most frequently implicated internalizing problems among children with both SOR and psychopathology.22 In studies examining infant and preschooler temperament, SOR in the auditory and tactile domains has been found to be positively correlated with anxiety22,23 and fearfulness.24 Among toddlers with ASD, SOR was found to emerge before anxiety and predict later development of anxiety.18 While these studies suggest a relationship between SOR and anxiety broadly defined, some have argued that SOR may be more specific to certain anxiety disorders, such as obsessive-compulsive disorder (OCD).21,25 However, research on the relationship between anxiety and SOR is extremely limited, making it difficult to evaluate the possible ways in which these constructs may be distinct or overlap.
To date, no studies have examined SOR within a sample of children with clinically significant anxiety who do not have developmental delays or disabilities. Therefore, we sought to examine the SOR construct within a sample of children presenting for outpatient treatment with primary complaints of anxiety. The current study was exploratory in nature and sought to examine the phenomenology of SOR in this sample of youth who all demonstrated clinically significant psychiatric symptoms. The SOR construct was examined broadly using the SensOR, a parent-report checklist of bothersome sensory experiences. Study aims were to: 1) examine the frequency and course of SOR symptoms in this sample, 2) compare prevalence rates of SOR to those reported in population-based samples, 3) explore whether SOR symptom frequency differs across categorical demographic variables and psychiatric disorder diagnoses, and 4) examine the relationship between SOR symptoms and continuous measures of psychopathology.
Method
Participants
Participants were children (ages 4–17 years) presenting for a diagnostic evaluation at the Bradley-Hasbro Pediatric Anxiety Research Clinic (PARC), a specialty psychology/psychiatry clinic located in a major medical center. Participants were clinical referrals from the community interested in diagnostic evaluations and/or treatment. PARC utilizes a multi-step intake procedure. First, parents complete a telephone screen with a research assistant. During the timeframe considered for this study (May 2011–November 2012), 351 phone screens were completed. Children who had symptoms of a possible anxiety disorder, who did not have previous diagnoses of developmental disabilities (including autism spectrum disorders), and who did not qualify for other research studies at PARC (n = 17 for a study recruiting normal controls; n = 20 for a study recruiting for 9–17 year olds with OCD; n = 2 for a study recruiting 5–8 year olds with OCD) were invited for in-person assessments (n = 141).
Of these children, 100 (which represents 71% of those eligible), completed the in-person assessment. Assessments were conducted by advanced clinical psychology trainees (residents, postdoctoral fellows) under the supervision of licensed clinical psychologists. Clinicians were first required to observe and then be observed by an experienced clinician before conducting intake assessments independently. Psychiatric diagnoses were conferred within one week of the assessment following consultation with the supervising psychologist.
Children whose parents completed the Sensory Over-Responsivity Inventory (SensOR, described below) with ≤ 20% of data missing were included in the current analyses, resulting in a sample of 88 children. The data included in the current study were obtained under approval of the Rhode Island Hospital IRB. Informed consent was obtained from parents. Verbal assent was provided by all children, and those who were 8 years of age or older provided written assent.
Measures
Clinician Measures
Diagnosis was based on the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID),26 a brief structured diagnostic interview that screens for 24 DSM-IV-TR psychiatric disorders, including major Axis I domains and pervasive developmental disorder. The MINI-KID has demonstrated excellent diagnostic sensitivity and specificity, as well as substantial concordance with other structured diagnostic interviews. DSM-IV-TR global assessment of functioning (GAF) scores were recorded by the clinician in a diagnostic summary sheet.
Parent-Report Measures.a
Sensory Over-Responsivity Inventory (SensOR).17
The SensOR is an inventory of 76 items that describe sensations that may be bothersome to the child. The current study included 52 items describing sensations in the tactile (30 items) and auditory (22 items) modalities. These were the scales available from the authors for analysis and are the same scales used in population-based research.3,15 Parents indicate whether or not the child is bothered by each stimulus item (“To help us understand your child’s sensory experiences, please circle “Yes” or “No” to indicate whether or not each item has bothered your child in the past month”), and items are summed to yield a total score. In the current sample, psychometric properties were similar to those reported by Van Hulle et al.15 Internal consistency was good between all items, α = 0.90, and separate subscales of tactile, α = 0.86, and auditory items, α = 0.85. The scores from the auditory and tactile scales were moderately correlated, r = .45, p <.001.
Additional questions added to SensOR form
For each item endorsed as bothersome, parents were asked to “Circle the number that best describes HOW MUCH your child is bothered by this experience. This includes how bothered your child feels during the experience (e.g., while hearing an alarm) and/or how bothered your child feels when anticipating this experience (e.g., while expecting an alarm to sound).” Responses were rated on a Likert-type scale with the following anchors: 0 = “not at all”, 1 = “a little”, 2 = “moderately,” 3 = “a lot”, and 4 = “extremely.” A mean distress score was calculated for each child.
Questions about the course of the child’s symptoms were added at the end of the SensOR. Parents endorsing any SensOR items were asked to write an open response to the question, “How long has your child been bothered by these sensory experiences?” Answers were classified into three categories of symptom onset: 1) before age 3 (e.g., responses such as “whole life,” “since birth”), 2) preschool age (3–5 years old), and 3) school age (after age 5). Next, parents were asked, “Do your child’s difficulties with these sensory experiences change over time?” and circled “yes” or “no.” Finally, parents who answered “yes” were asked the follow-up question, “In the past month, have these difficulties been (circle one): better than usual, worse than usual, about the same as they usually are.”
Child Behavior Checklist-Parent Report Form (CBCL).27
The CBCL is a widely used, psychometrically sound scale that assesses an array of behavioral problems in children ages 6–18 years. T-scores allow for normative comparisons across three broadband scales (Internalizing, Externalizing, and Total Problems; mean = 50, SD = 10). Scores between 60–65 are interpreted to be in the borderline clinical range, and the clinical range is scores >65. CBCL scores were analyzed only for participants ages 6 years and older.
Obsessive Compulsive Inventory- Parent Version (OCI-PV)
The OCI-PV is a 42-item measure of obsessive compulsive symptom severity in children over the past month. The adult version of the measure,28 which as demonstrated adequate reliability and validity, was adapted for parent use in this study. Items are rated on two 5-point Likert-type scales measuring the frequency and distress of symptoms, and total scores range from 0–336.
Screen for Child Anxiety Related Emotional Disorders –Revised, Parent Version (SCARED-R).30
The SCARED-R is a 66-item parent-report questionnaire that assesses a broad range of DSM-defined anxiety disorder symptoms. Items are rated based on symptom frequency (0 = almost never, 1 = sometimes true, 2 = often). The SCARED-R has demonstrated satisfactory psychometrics (adequate internal consistency of >.80, and good convergent and discriminant validity)30 and yields a total score (range = 0–132) and the following subscales: separation anxiety disorder, generalized anxiety disorder, panic disorder, social phobia, specific phobia, obsessive-compulsive disorder, and post-traumatic stress disorder.
Demographics questionnaire
Parents provided information about basic child and family demographic characteristics, including child developmental history, treatment history, and family psychiatric history.
Child-Report Measures were only administered to children who were 8 years of age or older (n = 51).
Multidimensional Anxiety Scale for Children (MASC).31
The MASC is a 39-item measure of anxiety symptoms yielding a total score and four empirically derived factor score, reported as T-scores (60–65 = borderline clinical range, >65 = clinical range): Social Anxiety, Separation/Panic, Harm Avoidance, and Physical Symptoms. The scale has been shown to have acceptable psychometric properties, including construct validity through confirmatory factor analysis, internal consistency (>.80), and convergent and discriminant validity. 31 It is appropriate for children ages 7–17.
Child Depression Inventory (CDI).32
The CDI is a 27-item measure of depressive symptomatology over the preceding two weeks in youth ages 8–17. T-scores for total symptom score and five subscales can be derived from the CDI (60–65 = borderline clinical range, >65 = clinical range): Negative Mood, Interpersonal Problems, Ineffectiveness, Anhedonia, and Negative Self-Esteem. The CDI has shown adequate internal consistency (>.80), good test-retest reliability (>.80), and concurrent validity.32
Obsessive Compulsive Inventory- Child Version (OCI-CV).29
The OCI-CV is a 21-item measure of obsessive compulsive symptoms over the past month in youth ages 7–17 years. Items are rated on a Likert-type scale based on frequency (0 = never, 1 = sometimes, 2 = always). The OCI-CV has satisfactory psychometrics29 and yields a total score (range = 0–42; the mean total score reported in a clinical sample of youth with OCD was 17) and six factorially derived subscales: doubting/checking, obsessions, hoarding, washing, ordering, and neutralizing).
Analytic Plan
Data were examined using descriptive analyses. Possible differences in SensOR total scores across categorical variables (gender, developmental history, family history, treatment history, and DSM-IV-TR diagnostic status) were examined using independent samples t-tests. Pearson’s correlations were used to examine the relationship between SensOR total and SensOR distress scores and continuous variables (e.g., age, GAF score, scores on parent- and child-report measures). Although the current study was exploratory in nature, an alpha level of p = .01 was used to determine statistical significance because of the number of analyses conducted.
Results
Sample Characteristics
Participants had a mean age of 8.9 years (SD = 3.2, range = 4–17) and 52.7% (n = 29) were male. The sample was predominately Caucasian (80.7%, n = 71; missing = 7, 8%) and not Hispanic or Latino (84.1%, n = 74; missing = 8, 9.1%). The majority of the sample was living in two-parent households (84.1%, n = 74, of which 67 parents were biological mother and father) with one sibling (58.0%, n = 51; 2 or more siblings = 27, 30.1%; no siblings = 10, 11.4%). Modal parental education level was college graduate for mothers (n = 37, 42.0%) and fathers (n = 29, 33%), and modal annual household income was “more than $100,000” (n = 24, 27.3%). At the time of the evaluation, 37 (42.0%) children were being treated with psychotropic medication and 42 (46.7%) had received previous psychotherapy.
Eighty-three (94.3%) children met full DSM-IV criteria for at least one anxiety disorder, including generalized anxiety disorder (GAD; n = 41, 42.7%), separation anxiety disorder (n = 24, 25.0%), obsessive compulsive disorder (OCD; n = 20, 20.8%), specific phobia (n = 14, 14.6%), social phobia (n = 12, 12.5%), anxiety disorder not otherwise specified (n = 9, 9.4%), and panic disorder (n = 2, 2.1%). Of the remaining five children in the sample, one had a “provisional” anxiety disorder diagnosis, two had mood disorder not otherwise specified and oppositional defiant disorder (ODD), and one had an adjustment disorder. These children were included in analyses given that they all had clinically significant psychiatric symptoms that included some complaints of anxiety (i.e., all reported difficulty with anxiety even though all did not meet full DSM criteria for anxiety disorder diagnoses). Current GAF scores, available for 82 children, indicated an overall moderate level of global impairment (m = 59.1, SD = 7.6, range = 35–75).
Frequency of SOR Symptoms
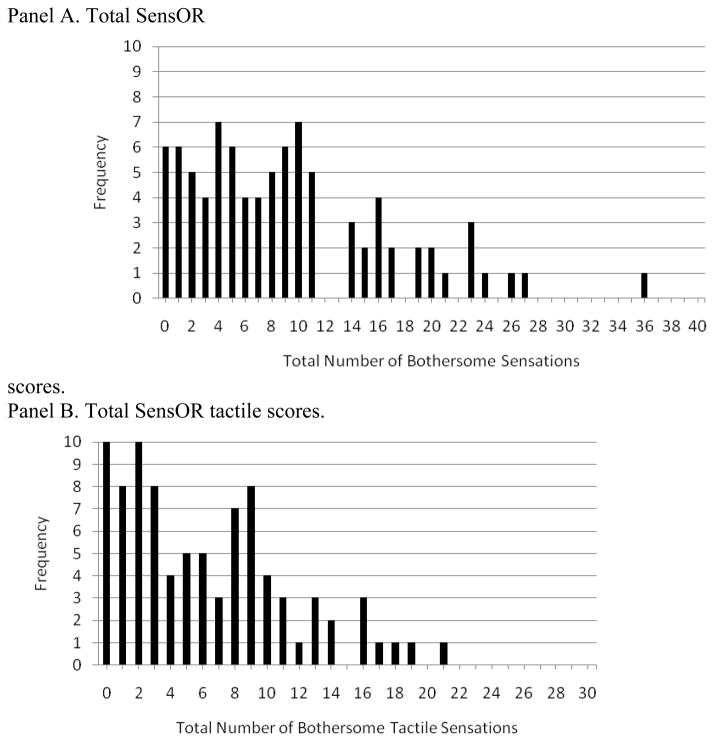
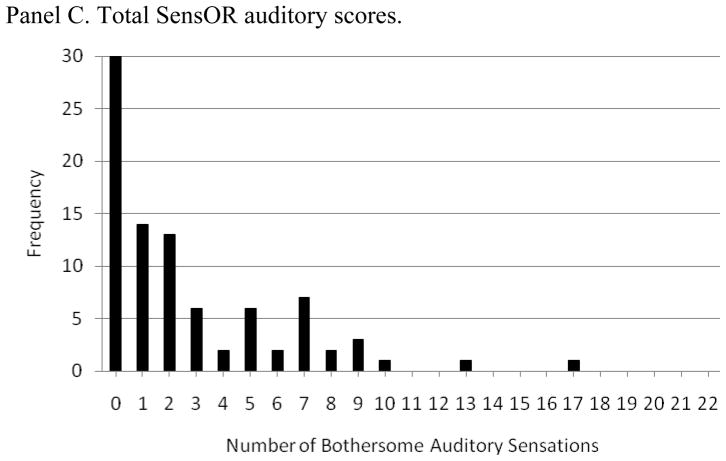
The mean SensOR total score (i.e., number of bothersome sensations endorsed) was 9.2 (SD = 7.4, range = 0–36, median = 8.0, mode = 4). A mean of 6.2 (SD = 5.1, range = 0–21) tactile items and a mean of 2.7 (SD = 3.4, range = 0–17) auditory items were endorsed. Almost all children had at least one bothersome sensation endorsed on the SensOR (93.2%, n = 82). Seventy-eight (88.6%) children experienced at least one bothersome tactile sensation and 58 (65.9%) experienced at least one bothersome auditory sensation. Distribution of the SensOR total, tactile, and auditory scores are presented in Figure 1. Table 1 presents the frequency of endorsement for each SensOR symptom.
Figure 1.
Distribution of SensOR scores (i.e., number of bothersome sensations endorsed) in a sample of children presenting with primary anxiety complaints.
Table 1.
Frequency of endorsement for each item on the SensOR.
| SensOR Item | n |
|---|---|
| Tags in clothing | 48 (54.5%) |
| Alarms | 36 (40.9%) |
| Wet clothes | 36 (40.9%) |
| Cutting toenails | 33 (37.5%) |
| Socks | 32 (36.4%) |
| Seams in clothing | 31 (35.2%) |
| Cutting fingernails | 30 (34.1%) |
| Hair brushing or combing | 30 (34.1%) |
| People standing too close | 25 (28.4%) |
| Sirens | 23 (26.1%) |
| Brushing teeth | 22 (25.0%) |
| Getting dirty | 22 (25.0%) |
| Kissing or hugging | 22 (25.0%) |
| Concerts | 21 (23.9%) |
| Accessories | 20 (22.7%) |
| Haircut | 19 (21.6%) |
| Sounds at a large gathering | 18 (20.5%) |
| Taking a shower | 18 (20.5%) |
| Washing face | 17 (19.3%) |
| Sound of people talking | 17 (19.3%) |
| Sound of appliances | 17 (19.3%) |
| Hair washing or drying | 17 (19.3%) |
| Getting dressed | 16 (18.2%) |
| Dog barking | 15 (17.0%) |
| Changing from long to short pants | 14 (15.9%) |
| Lotion on skin | 14 (15.9%) |
| Food on hands | 13 (14.8%) |
| Sounds at crowded supermarket | 12 (13.6%) |
| Sounds at restaurant | 12 (13.6%) |
| Light stroking touch | 12 (13.6%) |
| Dirty floors | 11 (12.5%) |
| Mud | 11 (12.5%) |
| Sound of toilet flushing | 11 (12.5%) |
| Sound of utensils against each other | 10 (11.4%) |
| Sounds at cafeterias | 10 (11.4%) |
| Sounds at gymnasium | 9 (10.2%) |
| Sound of ticking clock | 7 (8.0%) |
| Sound of construction equipment | 7 (8.0%) |
| Sound of lawn mower | 7 (8.0%) |
| Sounds at malls | 7 (8.0%) |
| Dirt | 7 (8.0%) |
| Glue | 7 (8.0%) |
| Door bell ringing | 6 (6.8%) |
| Fuzzy textures | 5 (5.7%) |
| Finger paint | 5 (5.7%) |
| Sound of florescent lights | 5 (5.7%) |
| Grass | 4 (4.5%) |
| Clothing that makes a noise | 4 (4.5%) |
| Radio playing in background | 4 (4.5%) |
| Coarse carpet | 3 (3.4%) |
| Play dough | 3 (3.4%) |
| Sound of water running or dripping | 3 (3.4%) |
To compare the prevalence of SOR in this sample to those reported in population-based samples,3,15 we identified the number of children in this sample that met criteria for SOR as specified in these studies. Sixty-seven (76.1%) met the Carter et al.3 SOR criteria of four or more items endorsed on the SensOR, and 50 (56.8%) met the Van Hulle et al.15 SOR criteria of six or more tactile or four or more auditory items endorsed on the SensOR.
Comparisons of SensOR total scores across categorical variables are presented in Table 2. SensOR scores did not differ in terms of gender or any specific psychiatric disorder diagnosis. SensOR scores were significantly higher among those rated as being “temperamentally difficult as an infant” (t = 2.7, p = .01). SensOR scores were not significantly different across other developmental and family history categorical variables. There were no group differences in terms of treatment history.
Table 2.
Frequency of SOR symptoms across dichotomous classifications of demographic characteristics, developmental history, family history, and DSM-IV-TR diagnostic status.
| Yes | No | |||||
|---|---|---|---|---|---|---|
| N | SensOR, m(SD) | N | SensOR, m(SD) | t | p | |
| Demographic Characteristics | ||||||
| Male gender | 48 | 8.1 (7.3) | 40 | 10.5 (7.5) | 1.49 | .13 |
| Developmental History | ||||||
| Birth complications | 38 | 10.7 (8.3) | 48 | 8.3 (6.5) | 1.53 | .13 |
| Speech delay | 13 | 10.2 (8.1) | 74 | 8.8 (7.2) | 0.65 | .52 |
| Motor Delay, Gross | 8 | 8.4 (6.3) | 80 | 9.3 (7.6) | 0.32 | .75 |
| Motor Delay, Fine | 5 | 9.8 (7.8) | 62 | 9.1 (7.2) | 0.20 | .83 |
| Rigid, difficulty with change | 7 | 11.8 (7.2) | 74 | 9.1 (7.4) | 0.94 | .35 |
| Temperamentally difficult as infant | 22 | 13.5 (9.1) | 64 | 7.9 (6.2) | 2.70 | .01** |
| Family History | ||||||
| Anxiety | 70 | 9.4 (7.3) | 18 | 8.1 (1.9) | 0.65 | .52 |
| OCD | 58 | 9.1 (7.2) | 30 | 9.2 (7.9) | 0.07 | .94 |
| Depression | 42 | 10.5 (8.2) | 46 | 7.9 (6.6) | 1.69 | .09 |
| Inattention/Hyperactivity | 28 | 11.8 (7.2) | 60 | 7.9 (7.3) | 2.26 | .03* |
| Treatment History | ||||||
| Previous psychotherapy | 42 | 10.4 (7.6) | 45 | 8.2 (7.2) | 1.37 | .17 |
| Current Medication | 37 | 10.8 (8.4) | 47 | 7.5 (6.2) | 2.02 | .04* |
| DSM-IV-TR Diagnostic Status+ | ||||||
| OCD | 20 | 8.7 (7.4) | 62 | 8.9 (7.3) | 0.12 | .90 |
| GAD | 41 | 8.3 (6.5) | 40 | 9.0 (6.5) | 0.45 | .65 |
| Social Anxiety Disorder | 12 | 12.3 (8.1) | 75 | 8.8 (7.3) | 1.54 | .12 |
| Separation Anxiety | 24 | 10.8 (6.8) | 61 | 9.1 (7.8) | 0.54 | .58 |
| Specific Phobia | 14 | 10.4 (7.7) | 72 | 8.9 (7.3) | 0.66 | .50 |
| Anxiety NOS | 9 | 8.7 (6.4) | 79 | 9.2 (7.6) | .22 | .82 |
| ADHD | 7 | 11.8 (6.5) | 78 | 8.8 (7.6) | 1.00 | .32 |
| Chronic Tics/Tourette Syndrome | 12 | 8.3 (5.2) | 76 | 9.3 (7.7) | 0.42 | .67 |
| ODD | 10 | 12.9 (5.7) | 78 | 8.7 (7.5) | 1.69 | .09 |
significant at .05 level;
significant at .01 level.
Comparisons for the following disorders were not made due to low rates: Major Depressive Disorder (n = 1), Panic Disorder (n = 2), Transient Tic Disorder (n = 3), Conduct Disorder (n = 0), Post Traumatic Stress Disorder (n = 0), Selective Mutism (n = 0), Pervasive Developmental Disorder (n = 0). “Rule out” diagnoses were coded for some diagnoses and are not included in this table: OCD (n = 6), GAD (n = 7), Social Anxiety Disorder (n = 1), Separation Anxiety Disorder (n = 3), Specific Phobia (n = 2), ADHD (n = 3)
SOR Symptom Distress
The mean parent rating of sensation distress (i.e., how bothersome endorsed sensations were to the child) was 1.74 (SD = 0.90), representing moderate distress. Individual mean scores ranged from 0–3.79.
Course of SOR Symptoms
The additional SensOR questions were completed by 64 parents. Onset of SOR occurred before age 3 years in 38.6% (n = 34) of children, at preschool age (3–5 years old) in 20.5% (n = 18) of children, and at school age for 13.6% (n = 12) of children. Forty-one parents (46.6%) indicated that their child’s sensory symptoms change over time, while 23 (26.1%) said that symptoms do not change. Among children whose symptoms do change, parents rated symptoms in the past month as follows: 39 described symptoms as “about the same as they usually are,” 11 described symptoms as “better than usual,” and 8 described symptoms as “worse than usual” (n = 6 missing).
SOR and Continuous Measures of Psychopathology
The relationships between SensOR total score, SensOR distress score, and continuous variables are presented in Table 3. SensOR total scores were significantly and negatively correlated with GAF scores (r = −.27, p = .01), suggesting that children with more sensory symptoms were rated as more globally impaired. In terms of parent-report measures, the SensOR total score was significantly and positively correlated with CBCL Total (r = .48, p = <.0001) and CBCL Internalizing (r = .31, p = .007) scales as well as the SCARED-R Total (r = .39, p <.0001), Specific Phobia (r = .45, p <.0001), and OCD Scores (r = .42, p <.0001). The SensOR was significantly and positively correlated with the total and all subscale scores on the OCI-PV. In terms of the child-report measures, SensOR scores were significantly and positively correlated with the CDI total (r = .38, p = .007) and subscales measuring interpersonal problems and anhedonia. The SensOR was not significantly related to age or any scores on the MASC and OCI-CV. The SensOR distress score demonstrated somewhat similar relationships to continuous measures as the SensOR total score, showing significant positive correlations with the CBCL Total (r = .39, p < .001) and CBCL Internalizing (r = .32, p = .005) scales; the SCARED-R Total (r = .36, p = .001), Specific Phobia (r = .32, p = .005), and OCD subscales (r = .39, p = .001); and OCI-PV Total (r = .47, p < .001) and most subscale scores (exceptions were nonsignificant correlations with the Obsessions and Neutralizing subscales). On the CDI, the SensOR distress score only demonstrated a significant positive correlation Anhedonia subscale (r = .39, p = .006), and on the OCI-PV it was only significantly correlated with the Ordering subscale (r = .33, p = .01).
Table 3.
Correlations between SensOR total score, SensOR distress score, age, and measures of psychiatric functioning.
| Measure mean (SD) | Correlation with SensOR total score | Correlation with SensOR distress score | |||
|---|---|---|---|---|---|
| r | p | r | p | ||
| Age (n = 88) | 8.9 (3.2) | .03 | .79 | −.12 | .24 |
| GAF score (n = 82) | 59.1 (7.6) | −.27 | .01* | −.24 | .02 |
| Parent-report measures | |||||
| CBCL scores (n = 74) | |||||
| CBCL Total | 60.6 (9.2) | .48 | <.0001* | .49 | <.0001* |
| CBCL Externalizing | 53.1 (12.8) | .21 | .07 | .27 | .02 |
| CBCL Internalizing | 65.9 (10.7) | .31 | .007* | .32 | .005* |
| SCARED-R scores (n = 75) | |||||
| Total | 42.9 (18.1) | .39 | <.0001* | .36 | .001* |
| Separation Anxiety Disorder | 9.9 (4.9) | .25 | .03 | .25 | .02 |
| Generalized Anxiety Disorder | 9.6 (4.5) | .17 | .15 | .27 | .02 |
| Panic Disorder | 5.3 (4.4) | .18 | .12 | .15 | .20 |
| Social Phobia | 4.4 (2.8) | .19 | .10 | .09 | .42 |
| Specific Phobia | 8.2 (5.3) | .45 | <.0001* | .32 | .005* |
| Obsessive-Compulsive Disorder | 3.7 (2.9) | .42 | <.0001* | .39 | .001* |
| Post-Traumatic Stress Disorder | 1.6 (1.9) | .12 | .35 | .15 | .24 |
| OCI-PV scores (n = 69) | |||||
| Total | 49.7 (52.6) | .51 | <.0001* | .47 | <.0001* |
| Doubting | 2.5 (5.4) | .38 | .001* | .36 | .001* |
| Checking | 6.8 (9.2) | .47 | <.0001* | .42 | .001* |
| Obsessions | 9.7 (11.3) | .42 | .001* | .24 | .05 |
| Hoarding | 5.2 (7.0) | .38 | <.0001* | .34 | .004* |
| Washing | 8.3 (15.9) | .34 | .006* | .32 | .008* |
| Ordering | 8.3 (11.1) | .49 | <.0001* | .48 | <.0001* |
| Neutralizing | 3.6 (6.8) | .32 | .007* | .28 | .02 |
| Child-report measures | |||||
| CDI scores (n = 52) | |||||
| Total | 49.6 (9.4) | .38 | .007* | .27 | .05 |
| Negative mood | 51.6 (12.5) | .22 | .12 | .17 | .34 |
| Interpersonal problems | 50.5 (12.0) | .35 | .01* | .30 | .03 |
| Ineffectiveness | 49.4 (11.8) | .33 | .02 | .17 | .24 |
| Anhedonia | 51.3 (9.3) | .38 | .007* | .39 | .006* |
| Negative self-esteem | 45.6 (9.4) | .30 | .03 | .13 | .38 |
| MASC scores (n = 53) | |||||
| Total | 58.9 (11.5) | .08 | .56 | .24 | .08 |
| Social anxiety | 56.4 (13.0) | .05 | .69 | .23 | .09 |
| Separation/panic | 66.4 (13.7) | .18 | .20 | .18 | .18 |
| Harm avoidance | 49.4 (10.2) | −.22 | .13 | −.02 | .88 |
| Physical symptoms | 52.1 (10.8) | .11 | .43 | .23 | .10 |
| OCI-CV scores (n = 56) | |||||
| Total | 12.3 (7.1) | .21 | .11 | .14 | .27 |
| Doubting | 1.8 (1.5) | .19 | .14 | .04 | .76 |
| Checking | 1.5 (1.3) | .00 | .98 | .05 | .73 |
| Obsessions | 2.9 (1.6) | −.09 | .51 | −.15 | .25 |
| Hoarding | 1.8 (1.8) | .20 | .14 | .15 | .25 |
| Washing | 1.1 (1.5) | .25 | .07 | .10 | .44 |
| Ordering | 2.1 (1.8) | .26 | .06 | .33 | .01* |
| Neutralizing | 1.0 (1.4) | .08 | .56 | .09 | .47 |
significant at p = .01 level.
Discussion
The construct validity and proper classification of SOR remains a controversial topic in large part due to a paucity of research examining the relationship of SOR to existing psychiatric disorders. Given implications that SOR and anxiety frequently co-occur, the current study examined the phenomenology of SOR in a sample of typically developing children seeking treatment for anxiety.
Symptoms of parent-reported SOR were extremely common in this sample. Nearly all children experienced at least one bothersome sensation (93.2%), and the mean and modal number of bothersome sensations experienced (mean = 9.2, mode = 4) were much higher than the mean number of symptoms endorsed in population-based samples (e.g., 2.3633). Parent ratings of SOR-related distress indicated that endorsed sensations were, on average, “moderately” bothersome to children, but the full range of distress ratings was observed across the sample. When SOR criteria set by previous population-based research3,15 were used to identify SOR status, one-half to two-thirds of the sample met this SOR threshold (depending on the specific cutoff used). Rates of SOR symptoms did not seem to be unique or distinct to a particular diagnostic category, but dimensional measures support the idea that parent perceived SOR may be more closely associated with symptoms of parent perceived OCD than other anxiety disorders.
The high rate of SOR symptom occurrence in this anxiety treatment-seeking sample could be attributable to a number of factors. First, it is possible that SOR is not entirely independent from anxiety problems, especially in children, who are still developing cognitive and verbal abilities and may not yet experience symptoms that are common in adults, such as rumination and worry.33 As such, SOR may be a phenomenological characteristic of childhood anxiety that has yet to be fully described. The finding that SOR was more closely related to dimensional measures of OCD than to other specific anxiety problems is particularly interesting given the increased recognition of sensory phenomena in OCD, such as incompleteness, “not just right” experiences, sensory urges, and disgust.34 These phenomena are thought to be especially common among young children with OCD, who may engage in repetitive or ritualistic behavior to achieve a “just right” feeling, such as putting on socks over and over.21,35 Both childhood ritualism and hypersensitivity in the olfactory, gustatory, and tactile domains have been linked to increased risk of OCD symptoms later in life.25,36 The degree to which SOR symptoms are linked to OCD symptoms developmentally and among those with OCD at other ages warrants further investigation.
Second, it is possible that the high co-occurrence rate is attributable to overlapping or fuzzy construct boundaries between SOR and anxiety, especially since SOR slacks a precise operational definition. Existing descriptions of SOR encompass a wide array of symptom-triggering stimuli (i.e., any sensation) and behavioral or emotional responses (e.g., anxiety, fearfulness, avoidance, escape or withdrawal, aggression, rigidity, irritability, moodiness, compulsivity, social avoidance).1,37 This non-specificity makes it difficult to determine whether anxiety and SOR are best conceptualized as separate constructs. Presumably, the defining element of SOR is its “sensory” nature; however, precisely what is meant by the term “sensory” in the SOR literature and in existing assessment tools remains unclear. Current descriptions note that “sensory” refers not to “sensation” in its neurophysiologic sense, but rather to “a behavioral response to sensory input.”1 In other words, SOR is defined in terms of the antecedent stimuli that trigger a maladaptive response (i.e., child has a “sensory problem” if bothered by objects or activities that elicit sensory input/physiological arousal).
Current psychiatric nosology clusters together anxiety disorders based not upon the stimuli that trigger anxiety but on core features of responding. It is probable that SOR and anxiety share many of these response features, such as heightened sensitivity to contextual and explicit threat cues, elevated psychophysiological reactivity to aversive stimuli, slowed or disrupted habituation, attentional biases to threat-relevant stimuli, and threat-based appraisals of ambiguous stimuli.38 The self-report nature of the current study precludes us from drawing conclusions about these potential shared features. However, at a minimum, the high occurrence of SOR symptoms highlights the need for more empirical research to determine whether SOR is indeed a separate, distinct construct.
Third, findings of high co-occurrence may be influenced by Berkson’s bias,39 such that children with co-occurring problems are more likely to seek help for any condition they have when compared to a child with only one condition. Therefore, children with only anxiety or only SOR may be less likely to present for treatment, particularly at an anxiety specialty clinic. Future research examining the relationship between psychopathology and SOR across multiple specialty and general clinics and in children presenting with primary SOR complaints is needed.
Consistent with prior research, current data suggest early onset of SOR symptoms. Results may reflect a particular developmental trajectory of SOR, anxiety, and depression symptoms. Onset of SOR was reported to be at a very young age for the majority of the sample, with 59.1% of parents recalling SOR before the age of 5 years. SOR symptom frequency was also significantly higher among those children described by parents as “temperamentally difficult” infants. Although the temporal sequence of symptom onset was not assessed in the current study, the findings of early SOR onset and current significant relationships between SOR and dimensional measures of internalizing problems are consistent with prior research showing that sensory regulation difficulty, broadly defined, is a significant risk factor for anxiety and depression.23 Researchers have speculated that SOR is a prodromal phase of internalizing disorders or a risk factor for psychopathology.4 From a biological perspective, SOR may be an early indication of dysfunction neurobiological substrates or functional domains that cut across psychiatric problems and disorders (e.g., arousal, executive/inhibitory control). For example, cortico-basal ganglia-subcortical circuits have been implicated in SOR as well as in anxiety and obsessive-compulsive spectrum disorders.40 From a behavioral perspective, early onset SOR symptoms may limit a child’s social and academic participation. Parents may also accommodate symptoms by helping the child avoid distressing situations. This avoidance may diminish the child’s access to potential reinforcers and opportunities to learn self-regulation and coping strategies.4,41 Future research examining the developmental trajectory of SOR and its potential neurobiological and functional substrates (e.g., using NIMH’s Research Doman Criteria constructs) may help us to understand if SOR is a prodrome or early risk factor for anxiety. Such research could potentially identify opportunities for early intervention or prevention focused treatments.
The clinical significance of SOR has yet to be clearly established, but this study supports the idea that SOR may be linked to greater impairment. Correlational analyses of the SensOR distress score with dimensional measures suggested that greater SOR-related distress may be associated with greater anxiety, obsessive-compulsive, and mood difficulties. Given that the most common sensations endorsed as bothersome were tactile stimuli associated with dressing and grooming, SOR symptoms may most adversely impact a child’s ability to complete basic activities of daily living. For younger children who still rely on parental support in these activities (e.g., a child who may not yet dress themselves independently), SOR may impact a child’s ability to willingly cooperate in activities of daily living.
The current study has several limitations. First, and critically, findings may be influenced by our ability to accurately assess SOR with available measures. There is currently no gold standard assessment tool for measuring SOR, which is likely a direct consequence of the absence of an operational definition of SOR. Although the SOR measure used in the current study, the SensOR, is meant to measure a more narrow set of symptoms than other “sensory processing” measures (e.g., Sensory Profile42), the measure is essentially only a list of stimuli. The way that parents interpreted “bother” in the instructions is unclear, as cognitive testing of measure instructions for the SensOR has never been conducted. Items could be rated as bothersome for a multitude of reasons, some of which could be anxiety-related (e.g., “getting dirty” could be endorsed for a child with contamination-related OCD, “dog barking” could be endorsed in association with a specific phobia of dogs). Item contamination is a recognized problem with other broad measures of sensory responsiveness,43 leading some researchers to exclude particular items on sensory scales that seem better indicators of temperamental characteristics or behavior problem symptoms.23 The extent to which findings are comparable across SOR studies that use different measures of SOR is unclear, as each measure used implies a particular operational definition of SOR.
Another limitation of the SensOR is that it is only a parent-report measure. Including multi-informant ratings of SOR symptoms and psychopathology may help further elucidate the relationship between these constructs. Perspectives that will be important to include in future research include child, teacher, and occupational therapist ratings. An additional limitation is the “yes/no” dichotomous response format of the SensOR. We added a rating scale to assess the degree to which endorsed symptoms are bothersome, but these anchors have not been tested elsewhere. It is unclear how parents interpreted these anchors and whether these ratings are accurate representations of SOR specific distress and functional impairment (i.e., it may be difficult for parents to distinguish SOR-related distress from anxiety or mood-related distress).
The format of the SensOR and the availability of only tactile and auditory scales provided no information about symptom frequency, duration, threshold of stimulation that elicits distress, intensity of behavioral response, and symptoms in other sensory domains (e.g., olfactory, gustatory). It may be the case that sensitivity in uncommon modalities or at a particular threshold of intensity or interference is more predictive of anxiety problems. Future research is needed to develop psychometrically sound, multimodal measures of SOR symptoms, a need that has been repeatedly acknowledged in the literature.3 Further research isolating particular SOR characteristics that are most predictive of anxiety is also necessary.
Other notable limitations include the homogenous nature of the sample in terms of race, ethnicity, and SES. There were some discrepancies between parent and child reporting of anxiety and OCD symptoms, an issue that is common in child anxiety research.44 Of note, statistically significant correlations were not found between the SensOR and child-rated anxiety (MASC) and OCD symptoms (OCI-CV). The reasons for this discrepancy could be attributable to a host of factors (e.g., child age, cognitive ability, parent anxiety, quality of parent-child relationship43) that should be explored further using multi-informant research methods. Finally, although OCD was not the most common diagnosis in this sample, it is worth noting that our clinic has a reputation for treating pediatric OCD, which may have influenced sample composition.
In terms of clinical practice, results highlight the importance of routinely assessing for distress and functional impairment related to bothersome tactile and auditory stimuli in children presenting with anxiety complaints. Although the construct validity and nosology of SOR continues to be debated, converging evidence across the literature suggests that this symptom cluster may be functionally impairing in some cases. Acknowledgement of these symptoms may be validating to struggling children and families and help pave the way for much needed intervention research, given that there is currently no empirically supported treatment for SOR.7
How to conceptualize and operationally define SOR remain important questions that require empirically-based answers. The paucity of methodologically rigorous data on the topic of SOR was highlighted by the DSM-5, which declined to classify SOR and other sensory symptom clusters as independent psychiatric diagnoses on the grounds of limited research demonstrating diagnostic independence. Although not without limitations, the current study is the first to examine SOR symptoms in a well-characterized anxiety sample. Future research focused on SOR and its relation to existing psychiatric diagnoses is likely to contribute to our overall understanding of this construct, which will hopefully lead to advancements in the care of children struggling with SOR symptoms.
Acknowledgments
Sources of Support: Funding for this study was provided by a grant from the National Institute of Mental Health (F32MH095274; PI: Conelea).
Footnotes
A correlation matrix of parent and child-report measures is available upon request from the authors.
References
- 1.Miller LJ, Anzalone ME, Lane SJ, et al. Concept evolution in sensory integration: a proposed nosology for diagnosis. Am J Occup Ther. 2007;61:135–140. doi: 10.5014/ajot.61.2.135. [DOI] [PubMed] [Google Scholar]
- 2.Baranek GT, Foster LG, Berkson G. Tactile defensiveness and stereotyped behaviors. Am J Occup Ther. 1997;51:91–95. doi: 10.5014/ajot.51.2.91. [DOI] [PubMed] [Google Scholar]
- 3.Carter AS, Ben-Sasson A, Briggs-Gowan MJ. Sensory over-responsivity, psychopathology, and family impairment in school-aged children. J Am Acad Child Adolesc Psychiatry. 2011;50:1210–1219. doi: 10.1016/j.jaac.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ben-Sasson A, Carter AS, Briggs-Gowan MJ. The development of sensory over-responsivity from infancy to elementary school. J Abnorm Child Psychol. 2010;38:1193–1202. doi: 10.1007/s10802-010-9435-9. [DOI] [PubMed] [Google Scholar]
- 5.Ayres AJ. Tactile Functions. Their relation to hyperactive and perceptual motor behavior. Am J Occup Ther. 1964 Jan-Feb;18:6–11. [PubMed] [Google Scholar]
- 6.Rogers C, Luby J. Sensory over-responsivity: a diagnosis whose time has come? J Am Acad Child Adolesc Psychiatry. 2011;50:1205–1207. doi: 10.1016/j.jaac.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 7.Section On Complementary and Integrative Medicine, Council on Children with Disabilities, American Academy of Pediatrics. Sensory integration therapies for children with developmental and behavioral disorders. Pediatrics. 2012;129:1186–1189. doi: 10.1542/peds.2012-0876. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. International Classification of Diseases (ICD-10) Geneva: World Health Organization; 1991. [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 10.Baranek GT, Boyd BA, Poe MD, et al. Hyperresponsive sensory patterns in young children with autism, developmental delay, and typical development. Am J Ment Retard. 2007;112:233–245. doi: 10.1352/0895-8017(2007)112[233:HSPIYC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Zero to Three. Diagnostic Classification: 0–3R: Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood. Washington, DC: Zero To Three Press; 2005. Rev ed. [Google Scholar]
- 12.Egger HL, Emde RN. Developmentally sensitive diagnostic criteria for mental health disorders in early childhood: the diagnostic and statistical manual of mental disorders-IV, the research diagnostic criteria-preschool age, and the diagnostic classification of mental health and developmental disorders of infancy and early childhood-revised. Am Psychol. 2011;66:95–106. doi: 10.1037/a0021026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, D.C: American Psychiatric Publishing; 2000. Text Revision. [Google Scholar]
- 14.Gouze KR, Hopkins J, LeBailly SA, et al. Re-examining the epidemiology of sensory regulation dysfunction and comorbid psychopathology. J Abnorm Child Psychol. 2009;37:1077–1087. doi: 10.1007/s10802-009-9333-1. [DOI] [PubMed] [Google Scholar]
- 15.Van Hulle CA, Schmidt NL, Goldsmith HH. Is sensory over-responsivity distinguishable from childhood behavior problems? a phenotypic and genetic analysis. J Child Psychol Psychiatry. 2012;53:64–72. doi: 10.1111/j.1469-7610.2011.02432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaffer D, Fisher P, Lucas CP, et al. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Schoen SA, Miller LJ, Green KE. Pilot study of the Sensory Over-Responsivity Scales: assessment and inventory. Am J Occup Ther. 2008;62:393–406. doi: 10.5014/ajot.62.4.393. [DOI] [PubMed] [Google Scholar]
- 18.Green SA, Ben-Sasson A, Soto TW, et al. Anxiety and sensory over-responsivity in toddlers with autism spectrum disorders: bidirectional effects across time. J Autism Dev Disord. 2012;42:1112–1119. doi: 10.1007/s10803-011-1361-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baranek GT, David FJ, Poe MD, et al. Sensory Experiences Questionnaire: discriminating sensory features in young children with autism, developmental delays, and typical development. J Child Psychol Psychiatry. 2006;47:591–601. doi: 10.1111/j.1469-7610.2005.01546.x. [DOI] [PubMed] [Google Scholar]
- 20.Reynolds S, Lane SJ. Diagnostic validity of sensory over-responsivity: a review of the literature and case reports. J Autism Dev Disord. 2008;38:516–529. doi: 10.1007/s10803-007-0418-9. [DOI] [PubMed] [Google Scholar]
- 21.Hazen EP, Reichert EL, Piacentini JC, et al. Case series: sensory intolerance as a primary symptom of pediatric OCD. Ann Clin Psychiatry. 2008;20:199–203. doi: 10.1080/10401230802437365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldsmith HH, Van Hulle CA, et al. A population-based twin study of parentally reported tactile and auditory defensiveness in young children. J Abnorm Child Psychol. 2006;34:393–407. doi: 10.1007/s10802-006-9024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hopkins J, Lavigne JV, Gouze KR, et al. Multi-domain models of risk factors for depression and anxiety symptoms in preschoolers: evidence for common and specific factors. J Abnorm Child Psychol. 2013;41:705–722. doi: 10.1007/s10802-013-9723-2. [DOI] [PubMed] [Google Scholar]
- 24.Keuler MM, Schmidt NL, Van Hulle CA, et al. Sensory overresponsivity: prenatal risk factors and temperamental contributions. J Dev Behav Pediatr. 2011;32:533–541. doi: 10.1097/DBP.0b013e3182245c05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dar R, Kahn DT, Carmeli R. The relationship between sensory processing, childhood rituals and obsessive-compulsive symptoms. J Behav Ther Exp Psychiatry. 2012;43:679–684. doi: 10.1016/j.jbtep.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 26.Sheehan DV, Sheehan KH, Shytle RD, et al. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) J Clin Psychiatry. 2010;71:313–326. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- 27.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington: University of Vermont Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 28.Foa EB, Kozak MJ, Salkovskis PM, et al. The validation of a new obsessive-compulsive disorder scale: The obsessive compulsive inventory. Psych Assessment. 1998;10:206–214. [Google Scholar]
- 29.Foa EB, Coles M, Huppert JD, et al. Development and validation of a child version of the obsessive compulsive inventory. Behav Ther. 2010;41:121–132. doi: 10.1016/j.beth.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 30.Muris P, Dreessen L, Bogels S, et al. A questionnaire for screening a broad range of DSM-defined anxiety disorder symptoms in clinically referred children and adolescents. J Child Psychol Psychiatry. 2004;45:813–820. doi: 10.1111/j.1469-7610.2004.00274.x. [DOI] [PubMed] [Google Scholar]
- 31.March J. Multidimensional Anxiety Scale for Children. North Tonawanda, NY: Multi-Health Systems Inc; 1997. [Google Scholar]
- 32.Kovacs M. Children’s Depression Inventory Manual. North Tonawanda, NY: Multi-Health Systems, Inc; 1992. [Google Scholar]
- 33.Ben-Sasson A, Carter AS, Briggs-Gowan MJ. Sensory over-responsivity in elementary school: prevalence and social-emotional correlates. J Abnorm Child Psychol. 2009;37:705–716. doi: 10.1007/s10802-008-9295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garcia AM, Freeman JB, Himle MB, et al. Phenomenology of early childhood onset obsessive compulsive disorder. J Psychopathol Behav Assess. 2009;31:104–111. doi: 10.1007/s10862-008-9094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pietrefesa AS, Coles ME. Moving beyond an exclusive focus on harm avoidance in obsessive-compulsive disorder: behavioral validation for the separability of harm avoidance and incompleteness. Behav Ther. 2009;40:251–259. doi: 10.1016/j.beth.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 36.Bolton D, Rijsdijk F, Eley TC, et al. Normative childhood repetitive routines and obsessive compulsive symptomatology in 6-year-old twins. J Child Psychol Psychiatry. 2009;50:1139–1146. doi: 10.1111/j.1469-7610.2009.02094.x. [DOI] [PubMed] [Google Scholar]
- 37.Miller LJ. Sensational Kids: Hope and Help for Children with Sensory Processing Disorder. New York, NY: Penguin Group Inc; 2006. [Google Scholar]
- 38.Craske MG, Rauch SL, Ursano R, et al. What is an anxiety disorder? Depress Anxiety. 2009;26:1066–1085. doi: 10.1002/da.20633. [DOI] [PubMed] [Google Scholar]
- 39.Berkson J. Limitations of the application of fourfold table analysis to hospital data. Biometrics. 1946;2:47–53. [PubMed] [Google Scholar]
- 40.Koziol LF, Budding DE, Chidekel D. Sensory integration, sensory processing, and sensory modulation disorders: putative functional neuroanatomic underpinnings. Cerebellum. 2011;10:770–792. doi: 10.1007/s12311-011-0288-8. [DOI] [PubMed] [Google Scholar]
- 41.Dawson G, Ashman SB, Carver LJ. The role of early experience in shaping behavioral and brain development and its implications for social policy. De Psychopathol. 2000;12:695–712. doi: 10.1017/s0954579400004089. [DOI] [PubMed] [Google Scholar]
- 42.Dunn W. Sensory Profile: User’s Manual. San Antonio, TX: Pearson, Inc; 1999. [Google Scholar]
- 43.Lengua LJ, West SG, Sandler IN. Temperament as a predictor of symptomatology in children: addressing contamination of measures. Child Dev. 1998;69:164–181. [PubMed] [Google Scholar]
- 44.Foley D, Rutter M, Pickles A, et al. Informant disagreement for separation anxiety disorder. J Am Acad Child Adoesc Psychiatry. 2004:452–460. doi: 10.1097/00004583-200404000-00011. [DOI] [PubMed] [Google Scholar]