Abstract
We investigated three potential predictors (educational attainment, pre-pregnancy smoking rate, and delay discounting [DD]) of spontaneous quitting among pregnant smokers. These predictors were examined alone and in combination with other potential predictors using study-intake assessments from controlled clinical trials examining the efficacy of financial incentives for smoking cessation and relapse prevention. Data from 349 pregnant women (231 continuing smokers and 118 spontaneous quitters) recruited from the greater Burlington, Vermont area contributed to this secondary analysis, including psychiatric/sociodemographic characteristics, smoking characteristics, and performance on a computerized DD task. Educational attainment, smoking rate, and DD values were each significant predictors of spontaneous quitting in univariate analyses. A model examining those three predictors together retained educational attainment as a main effect and revealed a significant interaction of DD and smoking rate (i.e., DD was a significant predictor at lower but not higher smoking rates). A final model considering all potential predictors included education, the interaction of DD and smoking rate, and five additional predictors (i.e., stress ratings, the belief that smoking during pregnancy will “greatly harm my baby,” age of smoking initiation, marital status, and prior quit attempts during pregnancy. The present study contributes new knowledge on predictors of spontaneous quitting among pregnant smokers with substantive practical implications for reducing smoking during pregnancy.
Keywords: delay discounting, pregnancy, cigarette smoking, health disparities, spontaneous quitting
Introduction
Smoking during pregnancy is the leading preventable cause of poor pregnancy outcomes in the U.S. and other developed countries, increasing risk for infertility, catastrophic pregnancy complications, intrauterine growth restriction, birth defects, infant death, and latter-in-life metabolic diseases (Cohen et al., 2010; Dietz et al., 2010; Guerrero-Preston et al., 2010; Hackshaw et al., 2011; Rogers, 2009). Thus, understanding factors underpinning the choices that women make around smoking during pregnancy is clearly important to improving maternal and infant health.
Approximately 20% of women who are smokers when they learn of their pregnancy have already quit smoking by their first prenatal care visit, referred to as spontaneous quitting in the smoking and pregnancy literature (Solomon & Quinn, 2004). Unfortunately, the majority of women will continue smoking through the pregnancy barring a formal smoking-cessation intervention. Lower educational attainment is highly associated with smoking during pregnancy (Higgins et al., 2009; Kandel et al., 2009). Among U.S. women in general, for example, prevalence of current smoking is 26.4%, 25.3%, 23.8%, and 12.1% among those with less than a high school education, a high school education, some college, and college graduates, respectively (Garrett et al., 2011). That relationship is exacerbated during pregnancy. For example, a comparison of the prevalence of smoking during pregnancy divided by prevalence of smoking among non-pregnant smokers by educational attainment in a nationally representative sample of U.S. women revealed ratios of .85, .68, .45, and .20 among those with less than a high school education, a high school education, some college, and college graduates, respectively (Kandel et al., 2009). Heavy smoking during pregnancy is also inversely associated with educational attainment, with 13.6% of pregnant women with less than a high school education reporting smoking a pack or more of cigarettes/day compared to only 0.3% among college graduates (Kandel et al., 2009).
The purpose of the present study was to follow-up on an earlier study we reported on predictors of spontaneous quitting (Higgins et al., 2009). In that study, women with more than 12 years of education were 27 times more likely than those with less than a high school education to have quit smoking prior to the start of prenatal care, but with relatively wide ranging confidence intervals (95% CI: 8-92). We wanted to further examine the influence of educational attainment in a larger sample with the goal of refining the precision of our estimate. Importantly, educational attainment was not the only significant predictor of spontaneous quitting in that study. Pre-pregnancy smoking rate (i.e., number of cigarettes smoked per day) was a strong predictor of spontaneous quitting, with the odds of quitting decreasing by 71% (95% CI: .60-.80) for every additional five cigarettes smoked per day. Smoking rate is well known to be an especially strong predictor of smoking cessation among pregnant and non-pregnant women (e.g., Graham & Der, 1999). Thus we were also interested in assessing the reliability of our estimate of that important predictor in this larger sample. Other significant predictors in the prior study were nicotine withdrawal symptoms, whether smoking was allowed in the home, number of quit attempts pre-pregnancy, and self-reported stress.
A new predictor of interest in the present study is delay discounting (DD), also referred to as temporal discounting (see Bickel & Marsch, 2001). DD measures reductions in the subjective value of rewards as a function of temporal delays to their delivery, with changes occurring relatively rapidly at smaller delays, and then to a lesser extent as delays become longer. This behavioral-economic concept is considered by many to measure a type of impulsivity that is relevant to health-related decision-making (Bickel, et al., 2012; Loewenstein et al., 2007). Like educational attainment, DD is associated with vulnerability to a wide range of health-related risk behaviors and associated problems, including smoking and other substance abuse, pathological gambling, eating disorders, bipolar disorder, and adherence with disease prevention regimens (Bickel, et al., 2012; Bickel & Marsch, 2001; Bradford, 2010; Davis et al., 2010; MacKillop, et al., 2011; Rogers, et al., 2010). Another type of discounting (i.e., social discounting) has been reported to be a significant independent predictor of spontaneous quitting in what is to our knowledge the only prior study examining discounting and spontaneous quitting (Bradstreet et al., 2012). Social discounting is a behavioral-economic concept wherein the amount of reward that one is willing to forgo in order to share with others decreases as a hyperbolic function of the perceived degree of social distance or separation between donor and recipient (Jones & Rachlin, 2006). Bradstreet et al. (2012) reported that spontaneous quitters compared to smokers showed a significantly more gradual decline in sharing as a function of degree of separation (i.e., greater generosity). Bradstreet et al. also examined DD and it was not a significant predictor of spontaneous quitting. However, the sample size was relatively small (91 smokers and 27 spontaneous quitters) as it was restricted to only the subsample of women who completed the social discounting task. Thus we wanted to examine further whether individual differences in DD may predict spontaneous quitting in a larger sample (which includes all participants from Bradstreet et al. (2012)) when examined alone and in combination with the other predictors discussed above, especially educational attainment and pre-pregnancy smoking rate.
Methods
Participants
Participants in this study were 349 pregnant women who were regular smokers at the time they learned of their most recent pregnancy, with 118 of them having quit smoking prior to initiating prenatal care (i.e., spontaneous quitters) and 231 who were still smoking at the start of prenatal care. The spontaneous quitters were enrolled in one of two sequential controlled clinical trials examining the efficacy of financial incentives for relapse prevention; the smokers were recruited simultaneously from the same population and were enrolled in one of three sequential controlled trials examining the efficacy of financial incentives for smoking cessation (see Higgins et al., 2012; Higgins et al., 2014). These five trials were all conducted in the same university research clinic. For all participants, smoking status was biochemically verified using urine cotinine testing. To be eligible for the relapse prevention trials, women had to report being smokers at the time of learning of the current pregnancy, to have quit smoking (i.e., no smoking in the past 7 days), and the self-report had to be confirmed with a cotinine-negative urine toxicology test result (≤ 80 ng/mg, enzyme immunoassay test, Microgenics Corp, Fremont, CA, run on a Roache Cobas Mira analyzer); to be eligible for the smoking cessation trials, women had to report smoking in the prior seven days confirmed by a cotinine-positive urine toxicology test result (> 80 ng/mg). The University of Vermont College of Medicine's Institutional Review Board approved these studies, and all participants provided written informed consent.
Participants in these trials were recruited from obstetrical care providers and the office of the Women, Infants, and Children (WIC) nutritional program in the greater Burlington, Vermont area. Women were eligible for inclusion for all trials if they resided in the county in which the research clinic is located, had no plans to leave the area within six months of giving birth, and were able to speak English. Exclusion criteria for all trials were incarceration, being a previous participant in the trial or living with a trial participant, living in a group residence, currently receiving opioid substitution therapy or using psychotropic medications (except for antidepressants), and being greater than 25 weeks gestation at the time of the intake assessment. Gestational age was derived from self-report and later verified via medical records. Patient flow is summarized in Figure 1.
Figure 1.
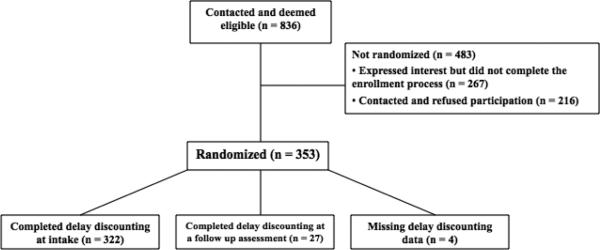
The flow of participants through the study Not randomized n = 483 (did not enroll n = 267; refused n = 216); randomized n = 353. Participants were pregnant smokers/quitters in greater Burlington, VT, studied April, 2002 – June, 2012.
Study Intake Assessment
All participants completed a study-intake assessment regarding sociodemographics, smoking characteristics, and psychiatric status. Educational attainment and pre-pregnancy smoking rate were included as part of this assessment. They also completed a DD task, which has been described previously (Johnson & Bickel, 2002). Briefly, participants were seated in front of the computer screen, which displayed the following message:
Imagine that you have a choice between waiting [length of time] and then receiving $1,000 and receiving a smaller amount of money right away. Please choose between the two options.
Seven delays were given (1 day, 1 week, 1 month, 6 months, 1 year, 5 years, or 25 years); participants always chose between $1,000 at one of these seven delays and a smaller amount available immediately. The program presented different values of the immediate reward until an indifference point was found, in which the value of the immediate amount was subjectively equivalent to the delayed $1,000 reward (Johnson & Bickel, 2002). This process was repeated for all time delays. The baseline DD assessment was not available for 27 women (9% of the overall sample); for these women, their DD data from the next available follow-up visit was used instead. A subset of these women (n = 118) also completed a social discounting task as reported in the Bradstreet et al. (2012), but results from that task were not considered in the present study.
Statistical Methods
Participant characteristics at the intake assessment were compared across the two smoking status groups using t tests for continuous variables and chi-square tests of homogeneity for dichotomous variables. Pearson correlation coefficients were used to examine associations between the estimated discounting parameter and participant characteristics. For the DD task, Mazur's (1987) hyperbolic equation, V = A/(1+kD), was used. This formula takes each subject's indifference points (V) for each of the seven delays (D; 1 day, 1 week, 1 month, 6 months, 1 year, 5 years, and 25 years), and fixes the value of the full-size reward A to $1000, to generate best-fit k values for each subject using nonlinear regression (SAS PROC NLIN). Each subject's derived discounting parameter (k) was used as the predictor variable for subsequent analyses. Because the distribution of estimated ks was skewed, analyses were performed using a logarithmic transformation of k, as is often used in the DD literature (e.g. Yoon, et al., 2007). Although the derived parameter estimates were lognormal, the distribution of indifference points at each delay was subject to outliers; thus, medians and associated standard errors are used to describe these data. The values of k generated by this equation may be conceived as the inverse of the number of years until a delayed reward of $1000 becomes functionally equivalent to an immediate reward of $500 (Yoon & Higgins, 2008). The k values represent a quantitative estimate of the degree to which an individual discounts the value of monetary and perhaps other types of rewards that are delayed in time, or said differently the loss that an individual is willing to absorb in order to have a reward now rather than in the future.
A series of logistic regression analyses were performed in order to examine the three predictors of primary interest (educational attainment, pre-pregnancy smoking rate, and DD) and their interactions as predictors of spontaneous quitting. Initially, simple logistic regression was run on each of the three predictors. Subsequently, logistic regression with backward elimination was conducted starting with the saturated model for the three predictors. Variables were removed one at a time until only significant predictors remained in the model. In order to preserve the model hierarchy, main effects of variables included in an interaction effect could not be removed from the model as long as the interaction remained in the model. This procedure was repeated starting with the saturated model for the three predictors of interest but also including baseline characteristics that differed significantly between spontaneous quitters and smokers in the present study or were significant predictors in our prior study (Higgins et al., 2009). Tjur's coefficient of discrimination (D) was used as a measure of fit for the logistic regression models (Tjur, 2009). Tjur's D measures the difference in the average of the event (spontaneous quitting) probabilities under the model for the group of observed events versus the group of observed nonevents and ranges from 0 to 1, with larger values indicating a better fit. Finally, as a check that our results were not unduly influenced by DD data obtained from subjects who did not understand or otherwise were unable to follow instructions on how to complete the DD task, we compared results including and excluding selected DD data based on an algorithm reported by Johnson & Bickel (2008) in which cases are excluded from analysis if any indifference point is greater than its predecessor by a magnitude exceeding 20% of the larger, later value (in this case, $200 out of a larger, later value of $1000), or if the indifference point at the final time point is not lower than the first time point by at least 10% of the larger, later value (i.e. $100 out of $1000). Univariate analysis of the relationship between DD and quitting was re-run with this reduced data set as a check on the possibility that “noisy” data influenced the study outcome. Analyses were performed with SAS Version 9.1 statistical software (SAS Institute, Cary, NC, USA). Statistical significance was defined as p < .05.
Results
As expected, spontaneous quitters differed from smokers on many SES, smoking, and psychiatric characteristics assessed at intake (Table 1). They were more likely to have greater than a high school education, be married, work outside the home, have private health insurance, and report that the current pregnancy was their first. They reported smoking at a pre-pregnancy rate that was approximately half that of smokers (9.7 vs. 18.8 cigarettes per day), initiated smoking at an older age, reported more quit attempts since finding out they were pregnant, and reported fewer nicotine withdrawal symptoms on average. They were also more likely to have few or no close friends who smoked, to live in a home where smoking was not permitted, and endorse that smoking during pregnancy will “greatly harm the health of my baby.” Spontaneous quitters generally reported fewer psychiatric symptoms than smokers, including lower average stress levels and rates of prior depression (Table 1).
Table 1.
Participant characteristics (N = 349).
| Characteristic | Overall (N = 349) | Quitters (n = 118) | Smokers (n = 231) | p value | Correlation w/ baseline discounting |
|---|---|---|---|---|---|
| Demographics: | |||||
| Age (years) | 25.0 ± 5.2 | 26.2 ± 5.4 | 24.4 ± 5.0 | <.01 | .021 |
| Education | <.001 | −.185* | |||
| % <12 years | 21 | 12 | 26 | ||
| % 12 years | 49 | 39 | 54 | ||
| % >12 years | 30 | 49 | 20 | ||
| % Caucasian | 95 | 97 | 93 | .09 | −.006 |
| % Married | 25 | 41 | 17 | <.001 | −.044 |
| % Private insurance | 31 | 48 | 22 | <.001 | −.031 |
| % Employed outside of home | 58 | 75 | 50 | <.001 | −.177* |
| % 1st pregnancy | 61 | 72 | 56 | <.01 | −.161* |
| Weeks pregnant at intake | 10.2± 4.2 | 10.7 ± 4.6 | 9.9± 4.0 | .13 | .040 |
| Smoking Characteristics: | |||||
| Cigs/day prepregnancy | 15.7± 8.7 | 9.7 ± 5.9 | 18.8 ± 8.2 | <.001 | .078 |
| Age started smoking (years) | 15.4 ± 3.2 | 16.7 ± 3.4 | 14.7 ± 2.9 | <.001 | −.078 |
| % Living with other smoker(s) | 77 | 72 | 79 | .13 | .100 |
| % With no smoking allowed in home | 58 | 75 | 49 | <.001 | −.178* |
| % With none or few friends/family who smoke | 29 | 44 | 21 | <.001 | −.021 |
| % Attempted to quit pre-pregnancy | 71 | 76 | 68 | .11 | −.085 |
| Number of quit attempts during pregnancy | 0.9 ± 1.8 | 1.3 ± 0.9 | 0.8 ± 2.0 | <.01 | −.088 |
| Nicotine withdrawal questionnaire total score | 1.5 ± 0.8 | 1.3 ± 0.7 | 1.6 ± 0.9 | <.01 | .013 |
| Attitude Item: | |||||
| % Endorsing that smoking will greatly harm baby | 91 | 99 | 86 | <.001 | −.059 |
| Psychiatric Symptoms | |||||
| Stress rating | 5.2 ± 2.6 | 4.7 ± 2.5 | 5.5 ± 2.7 | <.01 | .007 |
| BDI-II | 10.0 ± 6.8 | 9.0 ± 6.3 | 10.5 ± 7.0 | 0.06 | .091 |
| % Ever having depressive symptoms for 2+ weeks | 32 | 23 | 36 | .01 | .048 |
Note: M ± SD or %.
significant correlation (p < .05)
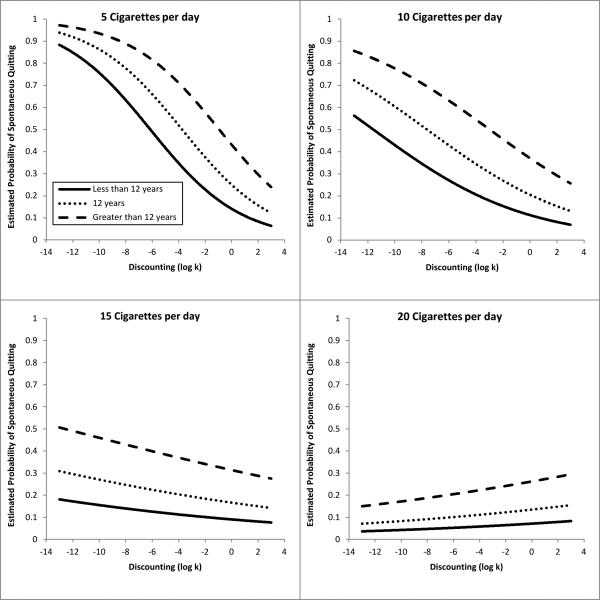
In univariate analyses, educational attainment, pre-pregnancy smoking rate, and discounting (log k) were each significantly associated with spontaneous quitting, with model fits of .09, .30, and .02, respectively (Table 2, Block 1). When these three predictors and all possible interactions were entered into a backward-elimination regression model, educational attainment remained a significant predictor and there was a significant two-way interaction of smoking rate and DD; this model had a fit of .39 (Table 2, Block 2). The final model involved examining the saturated model with the three predictors of interest as well as all other significant predictors from the Higgins et al (2009) study and those significant at the univariate level in the current data set (Figure 2). Educational attainment and the interaction of smoking rate and DD were retained in this model (Table 2, Block 3). In this final model, those with greater-than-high-school education had almost five times greater odds of spontaneous quitting than those with less-than-high-school education (OR = 4.62, 95% CI = 1.70 – 12.54, p < .01). With regard to the interaction of smoking rate and DD, the odds of spontaneously quitting smoking decreased as discounting increased, but only at lower rates (≤10 cigs/day) of cigarette smoking. As pre-pregnancy smoking rate increased (>10 cigs/day), the relationship between discounting and quitting diminished to statistically non-significant levels (OR and 95% CI at 5 cigs/day: 0.74 (0.61 – 0.90), at 10 cigs/day: 0.84 (0.73 – 0.96), at 15 cigs/day: 0.94 (0.83 – 1.07), at 20 cigs/day: 1.06 (0.89 – 1.25)). Five additional significant independent predictors entered the final model: stress ratings, the belief that smoking during pregnancy will “greatly harm my baby,” age of smoking initiation, marital status and quits during pregnancy. This model had a fit of .48.
Table 2.
Odds Ratios from Models Predicting Spontaneous Quitting with Educational Attainment, Prepregnancy Smoking Rate, and Delay Discounting (N = 349).
| Block 1. Univariate Models | ||
|---|---|---|
| OR (95% CI) | Tjur's D | |
| Discounting (log k)** | 0.87 (0.79, 0.96) | 0.02 |
| Smoking rate*** (per 5 cigarettes) | 0.37 (0.30, 0.47) | 0.30 |
| Education*** | 0.09 | |
| 12 vs. <12 | 1.56 (0.79, 3.07) | |
| >12 vs. <12 | 5.34 (2.65, 10.77) |
| Block 2. Model from Backward Elimination on Saturated Model | ||
|---|---|---|
| OR (95% CI) | Tjur's D | |
| Education*** | ||
| 12 vs. <12 | 2.55 (1.15, 5.68) | |
| >12 vs. <12 | 6.94 (2.93, 16.42) | |
| Log k × smoking rate*a | ||
| at 5 cigarettes | 0.78 (0.66, 0.93) | |
| at 10 cigarettes | 0.85 (0.75, 0.97) | |
| at 15 cigarettes | 0.93 (0.82, 1.04) | |
| at 20 cigarettes | 1.01 (0.86, 1.18) | 0.39 |
| Block 3. Model from Backward Elimination on Saturated Model and Baseline Characteristics | ||
|---|---|---|
| OR (95% CI) | Tjur's D | |
| Education** | ||
| 12 vs. <12 | 2.02 (0.85, 4.80) | |
| >12 vs. <12 | 4.62 (1.70, 12.54) | |
| Log k × smoking rate*a | ||
| at 5 cigarettes | 0.74 (0.61, 0.90) | |
| at 10 cigarettes | 0.84 (0.73, 0.96) | |
| at 15 cigarettes | 0.94 (0.83, 1.07) | |
| at 20 cigarettes | 1.06 (0.89, 1.25) | |
| Self-reported stress* | 0.86 (0.76, 0.97) | |
| Smoking will harm baby greatly* | 14.42 (1.77, 117.25) | |
| Age initiated smoking** | 1.15 (1.04, 1.28) | |
| Married* | 2.45 (1.17, 5.09) | |
| Number of quits during pregnancy* | 1.18 (1.01, 1.37) | 0.48 |
p < .05
p < .01
p < .001
The main effects of log k and smoking rate are included in the model, but only the odds ratios for log k at the given levels of smoking rate are presented in the table.
Figure 2.
Curves represent estimated probability of smoking in the final model, as a function of discounting (x-axis) and educational attainment (lines) at different levels of smoking. The four panels represent pre-pregnancy smoking rates of 5, 10, 15, and 20 cigarettes per day. Fit computed at the mean level of stress rating, age of smoking initiation, and quits during pregnancy and at the modal level of belief that smoking during pregnancy will “greatly harm my baby,” and marital status.
Delay Discounting Data Check
Eliminating nonsystematic DD data did not substantively alter these relationships. The algorithm eliminated 14% (49/349) of cases; median indifference points were insensitive to exclusions based on rule use. That is, the relationship between log k and spontaneous quitting remained relatively unchanged independent of whether nonsystematic DD data were included using any or all of the exclusion criteria.
Discussion
Prior reports by our group and others have shown that educational attainment is strongly associated with an enormous range of life-course choices that women make, including those involving smoking while pregnant (Graham et al., 2007; Higgins et al., 2009; Jaroni et al., 2004; Kandel et al., 2009). Consistent with our previous studies (Bradstreet, et al., 2012; Higgins, et al., 2009), educational attainment was again a strong predictor of spontaneous quitting in the present study. Differences of >12 years versus <12 years of education consistently predict substantial differences in the odds of quitting, and that difference does not appear to interact with smoking rate, DD, or any of the other predictors examined. The larger sample size used in the present study allowed us to refine our earlier estimate that having >12 years of education increased the odds of quitting 27.2 times (8.0-92.8) over <12 years to a still large but more reasonable increase of 5.95 times (2.27-15.63).
Consistent with our earlier observations, pre-pregnancy smoking rate remained a strong predictor in the present study accounting for the greatest amount of variance in spontaneous quitting. The odds of quitting were quite consistent across our earlier and the present study, with the earlier estimate being an increase of 71% (60%-80%) in the odds of quitting for every five fewer cigarettes smoked to the current estimate of a 64% (54%-72%) increase. Also consistent with our earlier research and other studies reporting stress as a predictor of smoking among women, higher ratings of stress over the past 7 days were associated with a decreased likelihood of smoking in the present study (e.g., Berlin et al. 2003; Higgins et al., 2009).
DD was negatively correlated with spontaneous quitting, although only at lower pre-pregnancy smoking rates. That is, as preference for monetary rewards shifted from larger, delayed rewards to smaller, more immediate rewards across individual lighter-rate smokers, the probability of quitting smoking upon learning of a pregnancy decreased significantly. As discussed in the Introduction to this report, we previously reported that social, but not delay, discounting predicted spontaneous quitting (Bradstreet, et al., 2012), but we were concerned that the prior study may have underestimated the role of DD considering that the sample size was relatively small (91 smokers and 27 quitters) and the increasing number of reports of associations between DD and a wide range of other health-related risk behaviors and problems (e.g. Bickel, et al., 2012; Bradford, 2010; Davis et al., 2010; MacKillop, et al., 2011; Rogers, et al., 2010). The significant association between DD and spontaneous quitting in this larger sample lends support to that concern regarding the potential influence of low statistical power in the Bradstreet et al. estimates, and suggests a significant, although relatively modest, association with spontaneous quitting. DD did not interact with educational attainment, meaning that the association of educational attainment with the likelihood of quitting is evident across the varying levels of DD. However, DD did interact with smoking rate; that is, DD was associated with quitting among those who smoked ≤10 cigs/day, but was not a significant predictor among those smoking >10 cigs/day. Excluding cases based on nonsystematic data (Johnson & Bickel, 2008) had minimal effect on the relationships between DD and spontaneous quitting observed in the present study.
Three of the predictors that entered the final model in the Higgins et al (2009) report did not survive in the final model of this analysis. Those variables were nicotine withdrawal, number of pre-pregnancy quit attempts, and smoking banned in the home. Meanwhile, three other predictors that did not enter the model in the earlier paper did remain in the final model in this analysis: age of smoking initiation, quit attempts during pregnancy, and marital status. Additionally, one variable that we did not examine previously (belief that smoking will harm the baby “greatly”) entered the final model as well. The change of predictors from the prior report to the present study merits comment. Nicotine withdrawal is negatively correlated with age of smoking initiation and marital status in this data set; it is possible that these latter variables accounted for variance that was previously accounted for by the former. The replacement of pre-pregnancy quit attempts with quit attempts during pregnancy can also be attributed to common variance. Smoking banned in the home is correlated with DD at the baseline level in this study, so the inclusion of DD in the final model may have accounted for variance previously accounted for by smoking bans. As noted above, we had not previously examined the predictive utility of asking women whether they endorsed the position that smoking will greatly harm their babies, but it was a strong predictor in the present study with those who endorsed a strong belief being 14.42 (1.77 -117.25) times more likely to quit than those who did not endorse that item. The confidence intervals are clearly large on this item, but even at the lower end they indicate a substantial association between endorsing this belief and the likelihood of spontaneous quitting. The age of smoking initiation was also a significant predictor of spontaneous quitting in the present study, which was not the case in our prior report, but has been reported previously in studies on predictors of spontaneous quitting (e.g., Cnattingius, 1989).
The final model in the present study provides a reasonable fit for the data (Tjur's D = .49) on spontaneous quitting and thus raises the important question of what practical implications might be gleaned from it in terms of reducing smoking during pregnancy. Like a growing number of others, we advocate a broad approach to the goal of reducing smoking among girls and women through policies that encompass more distal risk factors in addition to the more proximal and conventional tobacco-control foci (see Graham et al., 2007; Graham, 2009; Higgins et al., 2009; Kandel et al., 2009). The association between educational attainment and smoking in women, generally and during pregnancy, may also be associated with a number of other significant factors relating to quality of life in women. Greater education is associated with increases in the likelihood of being married, having a spouse and friends who are nonsmokers, being employed in a work setting with low smoking prevalence, being more knowledgeable about health risks, and having enhanced decision-making and problem-solving skills (Cutler & Lleras-Muney, 2008; Jones et al., 2009; Wetter, Cofta-Gunn, Irvin, et al., 2005; Wetter, Cofta-Gunn, Fouladi, et al. 2005). The multifaceted potential to impact smoking vulnerability through furthering educational attainment among girls and young women could prove to be an important component in any comprehensive plan for reducing smoking risk and improving women's health. Of course, the strong influence of smoking rates in the present study underscores the importance of continuing to focus on proximal factors in tobacco control efforts among girls and women. Encouraging girls and women to avoid heavy smoking if they are going to smoke, delaying the onset of smoking, and helping all women understand the serious short- and longer-term risks that smoking holds for the fetus are steps that have the potential to substantially increase the likelihood that women can discontinue smoking should they become pregnant. Of course, even lighter smokers often have difficulty quitting smoking including during pregnancy, and the present results suggest that delay discounting may be a contributor to that difficulty. The present results also demonstrate that stress and being a single parent are associated with greater difficulty quitting smoking during pregnancy independent of smoking rate. Although there are no silver bullets for promoting smoking abstinence during pregnancy among women with one or more of these different risk factors, financial incentives is an evidence-based strategy that merits serious consideration based on evidence from at least seven controlled clinical trials supporting their efficacy in promoting smoking cessation among pregnant women (Higgins, Washio, et al., 2012; Higgins et al., 2014) as well as a larger track record of successfully promoting health-related behavior change in treatment recalcitrant and otherwise challenging populations (see Higgins, Silverman, et al., 2012). The application of financial incentives with pregnant smokers using Medicaid funds is currently being evaluated in two states within the U.S. (WI & OR), and has been used in routine care in Scotland and other areas within the U.K. for several years (Radley et al., 2013). This practice is also growing well beyond smoking cessation with pregnant women. The U.S. VA hospital system is also offering incentives (i.e., contingency management) as part of routine care within their intensive outpatient clinics with nationwide training and implementation ongoing at the time this article went to press (Petry et al., 2014). The U.K. has had a similar program underway for the past 5 years (e.g., Weaver et al., 2014). Dissemination of financial incentive programs into the private sector has grown considerably over the past decade. For example, a RAND report on the topic showed that more than half of all major employers in the U.S. offer employee wellness programs (Mattke et al, 2013). Almost 70% of those programs use financial incentives to promote wellness participation, meaning that 40 million or more U.S. workers are currently exposed to health-related incentive programs with many programs incentivizing smoking cessation in one form or another.
The present study has characteristics that may limit extending implications to other populations, including the use of a cohort selected from a small metropolitan area with an almost exclusively Caucasian population, and a sample comprised exclusively of women willing to participate in treatment-outcomes studies. Generalizing to broader populations should be done with those characteristics in mind. Additionally, the relationships characterized in the present study are correlational and thus cannot support causal inferences. As in any observational study there are potentially important other predictors of smoking during pregnancy that we were unable to control for in the present study that may have influenced the relationships of interest. For example, knowing whether a pregnancy was planned or unplanned, maternal use of illicit drugs, and pre-pregnancy daily versus less-than-daily smoking status could potential enhance or otherwise change the relationships of interest (e.g., Finer & Henshaw, 2006; Ford et al., 2002; Gaalema et al., 2012). These limitations notwithstanding, we believe the present study contributes new knowledge on predictors of smoking during pregnancy that has substantive implications for improving efforts to reduce smoking during pregnancy.
Acknowledgments
The authors appreciate the help of Evan Herrmann and Matthew Bradstreet during the early phases of this project.
This research was supported by National Institutes of Health Center of Biomedical Research Excellence award P20GM103644 from the National Institute of General Medical Sciences, Tobacco Centers of Regulatory Science award P50DA036114 from the National Institute on Drug Abuse and the U.S. Food and Drug Administration, research grants R01DA14028 and R01HD075669 from the National Institute on Drug Abuse and National Institute of Child Health and Human Development, respectively, and institutional training grant T32DA07242 from the National Institute on Drug Abuse. The funding sources had no other role in this project other than financial support.
Footnotes
All authors contributed in a significant way to this manuscript, and all authors read and approved the final manuscript. The authors have no conflict of interest to report.
References
- Berlin I, Singleton EG, Pedarriosse AM, Lancrenon S, Rames A, Aubin HJ, Niaura R. The Modified Reasons for Smoking Scale: factorial structure, gender effects and relationship with nicotine dependence and smoking cessation in French smokers. Addiction. 2003;98:1575–1583. doi: 10.1046/j.1360-0443.2003.00523.x. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Jarmolowicz DP, Mueller ET, Koffarnus MN, Gatchalian KM. Excessive discounting of delayed reinforcers as a trans-disease process contributing to addiction and other disease-related vulnerabilities: emerging evidence. Pharmacology & Therapeutics. 2012;134:287–297. doi: 10.1016/j.pharmthera.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA. Toward a behavioral economic understanding of drug dependence: Delay discounting processes. Addiction. 2001;96:73–86. doi: 10.1046/j.1360-0443.2001.961736.x. [DOI] [PubMed] [Google Scholar]
- Bradford WD. The association between individual time preferences and health maintenance habits. Medical Decision Making. 2010;30:99–112. doi: 10.1177/0272989X09342276. [DOI] [PubMed] [Google Scholar]
- Bradstreet MP, Higgins ST, Heil SH, Badger GJ, Skelly JM, Lynch ME, Trayah MC. Social discounting and cigarette smoking during pregnancy. Journal of Behavior & Decision Making. 2012;25:502–511. doi: 10.1002/bdm.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cnattingius S. Smoking habits in early pregnancy. Addictive Behaviors. 1989;14:453–457. doi: 10.1016/0306-4603(89)90033-6. [DOI] [PubMed] [Google Scholar]
- Cohen G, Jeffery H, Lagercrantz H, Katz-Salamon M. Long-term reprogramming of cardiovascular function in infants of active smokers. Hypertension. 2010;55:722–728. doi: 10.1161/HYPERTENSIONAHA.109.142695. [DOI] [PubMed] [Google Scholar]
- Cutler D, Lleras-Muney A. Education and health: evaluating theories and evidence. In: House J, Schoeni R, Kaplan G, Pollack H, editors. Making Americans healthier: social and economic policy as health policy. Russel Sage Foundation; New York, NY: 2008. pp. 29–60. [Google Scholar]
- Davis C, Patte K, Curtis C, Reid C. Immediate pleasures and future consequences. A neuropsychological study of binge eating and obesity. Appetite. 2010;54(1):208–213. doi: 10.1016/j.appet.2009.11.002. [DOI] [PubMed] [Google Scholar]
- Dietz PM, England LJ, Shapiro-Mendoza CK, Tong VT, Farr SL, Callaghan WM. Infant morbidity and mortality attributable to prenatal smoking in the US. American Journal of Preventive Medicine. 2010;39:45–52. doi: 10.1016/j.amepre.2010.03.009. [DOI] [PubMed] [Google Scholar]
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on Sexual and Reproductive Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- Ford DE, Vu HT, Anthony JC. Marijuana use and cessation of tobacco smoking in adults from a community sample. Drug & Alcohol Dependence. 2002;67:243–248. doi: 10.1016/s0376-8716(02)00066-2. [DOI] [PubMed] [Google Scholar]
- Gaalema DE, Higgins ST, Pepin CS, Heil SH, Bernstein IM. Illicit Drug Use Among Pregnant Women Enrolled in Treatment for Cigarette Smoking Cessation. Nicotine & Tobacco Research. 2013;15(5):987–991. doi: 10.1093/ntr/nts220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett BE, Dube SR, Trosclair A, Caraballo RS, Pechacek TF. MMWR Surveill Summ. 2011;Cigarette smoking - United States, 1965-2008.60(Suppl):109–113. [PubMed] [Google Scholar]
- Graham H, Der G. Patterns and predictors of smoking cessation among British women. Health Promotions International. 1999;14:231–239. [Google Scholar]
- Graham H, Inskip HM, Francis B, Harman J. Pathways of disadvantage and smoking careers: Evidence and policy implications. Journal of Epidemiology and Community Health. 2007;60(Suppl II):ii7–ii12. doi: 10.1136/jech.2005.045583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham H. Women and smoking: Understanding socioeconomic influences. Drug & Alcohol Dependence. 2009;104(Suppl. 1):S11. doi: 10.1016/j.drugalcdep.2009.02.009. [DOI] [PubMed] [Google Scholar]
- Guerrero-Preston R, Goldman LR, Brebi-Mieville P, Ili-Gangas C, LeBron C, Hernández-Arroyo M, Sidransky D. Global DNA hypomethylation is associated with in utero exposure to cotinine and perfluorinated alkyl compounds. Epigenetics. 2010;5:539. doi: 10.4161/epi.5.6.12378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackshaw A, Rodeck C, Boniface S. Maternal smoking in pregnancy and birth defects: A systematic review based on 173,687 malformed cases and 11.7 million controls. Human Reproduction Update. 2011;17:589–604. doi: 10.1093/humupd/dmr022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, Badger GJ, Skelly JM, Solomon LJ, Bernstein IM. Educational disadvantage and cigarette smoking during pregnancy. Drug & Alcohol Dependence. 2009;104(Suppl. 1):S100–S105. doi: 10.1016/j.drugalcdep.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Silverman K, Sigmon SC, Naito NA. Incentives and health: An introduction. Preventive Medicine. 2012;55(Suppl):S2–S6. doi: 10.1016/j.ypmed.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Washio Y, Heil SH, Solomon LJ, Gaalema DE, Higgins TM, Bernstein IM. Financial incentives for smoking cessation among pregnant and newly postpartum women. Preventive Medicine. 2012;55:S33–S40. doi: 10.1016/j.ypmed.2011.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Washio Y, Lopez AA, Heil SH, Solomon LJ, Lynch ME, Hanson JD, Higgins TM, Skelly JM, Redner R, Bernstein IM. Examining two different schedules of financial incentives for smoking cessation among pregnant women. Preventive Medicine. 2014 Apr 2; doi: 10.1016/j.ypmed.2014.03.024. Epub ahead of print 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaroni JL, Wright SM, Lerman C, Epstein LH. Relationship between education and delay discounting in smokers. Addictive Behaviors. 2004;29:1171–1175. doi: 10.1016/j.addbeh.2004.03.014. [DOI] [PubMed] [Google Scholar]
- Jones B, Rachlin H. Social discounting. Psychological Science. 2006;17:283–286. doi: 10.1111/j.1467-9280.2006.01699.x. [DOI] [PubMed] [Google Scholar]
- Jones BA, Landes RD, Yi R, Bickel WK. Temporal horizon: modulation by smoking status and gender. Drug and Alcohol Dependence. 2009;104(Suppl 1):S87–S93. doi: 10.1016/j.drugalcdep.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. Within-subject comparison of real and hypothetical money rewards in delay discounting. Journal of the Experimental Analysis of Behavior. 2002;77:129–146. doi: 10.1901/jeab.2002.77-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. An algorithm for identifying nonsystematic delay-discounting data. Experimental & Clinical Psychopharmacology. 2008;16:264. doi: 10.1037/1064-1297.16.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel DB, Griesler PC, Schaffran C. Educational attainment and smoking among women: risk factors and consequences for offspring. Drug and Alcohol Dependence. 2009;104(Suppl. 1):S24–33. doi: 10.1016/j.drugalcdep.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298:2415–2417. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafò MR. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology. 2011;216:305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattke S, Liu H, Caloyeras JP, Huang CY, Van Busum KR, Khodyakov D, Shier V. Workplace wellness programs study: Final report. RAND Corporation; Santa Monica, CA: 2013. [PMC free article] [PubMed] [Google Scholar]
- Mazur JE. An adjustment procedure for studying delayed reinforcement. In: Commons ML, Nevin JA, editors. The effect of delay and of intervening events on reinforcement value. Lawrence Erlbaum Associates, Inc.; Hillsdale, NJ: 1987. pp. 55–73. [Google Scholar]
- Petry NM, DePhillippis D, Rash CJ, Drapkin M, McKay JR. Nationwide dissemination of contingency management: the Veterans Administration initiative. American Journal of Addictions. 2014;23:205–210. doi: 10.1111/j.1521-0391.2014.12092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radley A, Ballard P, Eadie D, MacAskill S, Donnelly L, Tappin D. Give it Up for Baby: outcomes and factors influencing uptake of a pilot smoking cessation incentive scheme for pregnant women. BMC Public Health. 2013;13:343–355. doi: 10.1186/1471-2458-13-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers JM. Tobacco and pregnancy. Reproductive Toxicology. 2009;28:152–160. doi: 10.1016/j.reprotox.2009.03.012. [DOI] [PubMed] [Google Scholar]
- Rogers RD, Moeller FG, Swann AC, Clark L. Recent research on impulsivity in individuals with drug use and mental health disorders: Implications for alcoholism. Alcoholism: Clinical & Experimental Research. 2010;34:1319–1333. doi: 10.1111/j.1530-0277.2010.01216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon LJ, Quinn VP. Spontaneous quitting: Self-initiated smoking cessation in early pregnancy. Nicotine & Tobacco Research. 2004;6(Suppl 2):S203–S216. doi: 10.1080/14622200410001669132. [DOI] [PubMed] [Google Scholar]
- Tjur T. Coefficients of determination in logistic regression models—A new proposal: The coefficient of discrimination. The American Statistician. 2009;63:366–372. [Google Scholar]
- Wetter DW, Cofta-Gunn L, Fouladi RT, Irvin JE, Daza P, Mazas C, Wright K, Cinciripini PM, Gritz ER. Understanding the association among education, employment characteristics, and smoking. Addictive Behaviors. 2005;30:905–914. doi: 10.1016/j.addbeh.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Weaver T, Metrebian N, Hellier J, Pilling S, Charles V, Little N, Poovendran D, Mitcheson L, Ryan F, Bowden-Jones O, Dunn J, Glasper A, Finch E, Strang J. Use of contingency management incentives to improve completion of hepatitis B vaccination in people undergoing treatment of heroin dependence: a cluster randomized trial. Lancet. 2014 Apr 8; doi: 10.1016/S0140-6736(14)60196-3. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Cofta-Gunn L, Irvin JE, Fouladi RT, Wright K, Daza P, Mazas C, Cinciripini PM, Gritz ER. What accounts for the association of education and smoking cessation? Preventive Medicine. 2005;40:452–460. doi: 10.1016/j.ypmed.2004.07.001. [DOI] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST. Turning k on its head: Comments on use of an ED50 in delay discounting research. Drug & Alcohol Dependence. 2008;95:169–172. doi: 10.1016/j.drugalcdep.2007.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, Thomas CS, Badger GJ. Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Experimental and clinical psychopharmacology. 2007;15:176. doi: 10.1037/1064-1297.15.2.186. [DOI] [PubMed] [Google Scholar]