Abstract
OBJECTIVE
To analyze the evolution of catastrophic health expenditure and the inequalities in such expenses, according to the socioeconomic characteristics of Brazilian families.
METHODS
Data from the National Household Budget 2002-2003 (48,470 households) and 2008-2009 (55,970 households) were analyzed. Catastrophic health expenditure was defined as excess expenditure, considering different methods of calculation: 10.0% and 20.0% of total consumption and 40.0% of the family’s capacity to pay. The National Economic Indicator and schooling were considered as socioeconomic characteristics. Inequality measures utilized were the relative difference between rates, the rates ratio, and concentration index.
RESULTS
The catastrophic health expenditure varied between 0.7% and 21.0%, depending on the calculation method. The lowest prevalences were noted in relation to the capacity to pay, while the highest, in relation to total consumption. The prevalence of catastrophic health expenditure increased by 25.0% from 2002-2003 to 2008-2009 when the cutoff point of 20.0% relating to the total consumption was considered and by 100% when 40.0% or more of the capacity to pay was applied as the cut-off point. Socioeconomic inequalities in the catastrophic health expenditure in Brazil between 2002-2003 and 2008-2009 increased significantly, becoming 5.20 times higher among the poorest and 4.17 times higher among the least educated.
CONCLUSIONS
There was an increase in catastrophic health expenditure among Brazilian families, principally among the poorest and those headed by the least-educated individuals, contributing to an increase in social inequality.
Keywords: Income, Health Expenditure, Health Inequality, Social Inequity, Health Economics
Abstract
OBJETIVO
Analisar a evolução dos gastos catastróficos em saúde e as desigualdades nesses gastos, segundo características socioeconômicas das famílias brasileiras.
MÉTODOS
Foram analisados dados da Pesquisa de Orçamentos Familiares de 2002-2003 (48.470 domicílios) e 2008-2009 (55.970 domicílios). Gasto catastrófico em saúde foi definido como despesas em excesso, considerando diferentes métodos de cálculo: 10,0% e 20,0% do consumo total e 40,0% da capacidade de pagamento da família. Consideraram-se indicadores socioeconômicos o Indicador Econômico Nacional e a escolaridade. As medidas de desigualdade utilizadas foram a diferença relativa entre taxas, razão das taxas e índice de concentração.
RESULTADOS
Os gastos catastróficos variaram entre 0,7% e 21,0%, a depender do método de cálculo. As menores prevalências foram observadas em relação à capacidade de pagamento, enquanto as maiores, em relação ao total do consumo. Houve aumento na prevalência de gastos catastróficos em saúde de 25,0%, entre 2002-2003 e 2008-2009, quando utilizado o ponto de corte de 20,0% em relação ao total de consumo, e de 100% quando aplicado o ponto de corte de 40,0% da capacidade de pagamento. Houve expressiva e crescente desigualdade socioeconômica na prevalência de gasto catastrófico em saúde no Brasil entre 2002-2003 e 2008-2009, chegando a ser 5,2 vezes maior o gasto catastrófico entre os mais pobres e 4,2 vezes maior nos menos escolarizados.
CONCLUSÕES
Houve crescimento da prevalência do gasto catastrófico entre as famílias brasileiras, principalmente entre aquelas mais pobres e chefiadas por indivíduos menos escolarizados, contribuindo para o aumento das desigualdades socioeconômicas.
INTRODUCTION
Catastrophic health expenditure (CHE) is defined as the spending on health that exceeds a pre-defined percentage of a household’s total costs and its capacity to pay. 19 , 21 The literature indicates different forms of calculations and cutoff points for estimating CHE, 1 , 6 , 13 , 19 , 21 although there is no consensus over the most adequate form to be used in studies regarding this subject.
However, regardless of the method selected for its calculation, CHE has great repercussions on people’s lives, discouraging them at times from using health services and resulting in their non-adherence to medicinal therapies and postponement of physical examinations, consultations, and necessary procedures. a In addition, this may result in a reduction in consumption of the goods and services essential to people’s daily lives, thus exposing families to social risk and quite often to economic ruin. 18
Family health expenditure in Brazil is especially concerning. Between 1995 and 2010, an increase in public health expenditure was observed; however, this was accompanied by greater expenditure by families and organizations with health plans and in direct costs. 8 , 9 Although the country possesses a public health system boasting universality, integrity and equality, it is one of the few in the world where the private health expenditure surpasses government expenditure. a
Multicentric research conducted by Xu et al 21 analyzed data from 59 countries and classified Brazil as second in terms of percentage of population with catastrophic expenditure (10.3%). However, other studies analyzing CHE exclusively in Brazil used different forms of calculations for obtaining the indicator and reported lower figures compared with those reported by Xu et al. 21 According to the data from the 1998 National Household Sample Survey (PNAD), the prevalence of catastrophic expenditure is 3.7%. 6 Analysis of the Pesquisa de Orçamentos Familiares (POF – Family Budget Research) from 2002 to 2003 also presented different cutoff points and identified a prevalence that varied from 2.0% to 16.0% of families with CHE in the country. 1 , b
The socioeconomic level of families is intimately linked with the risk of CHE and family impoverishment. Those families belonging to the lowest quintiles of income present a greater risk of incurring CHE and impoverishment resulting from such expenditure is more common than that in families belonging to the higher income quintiles. c Disparities in social, economic, and environmental conditions in different regions may play an important role in the risk of incurring CHE. 2 , 17
To analyze data regarding catastrophic expenditure in the country, its evolution throughout the years, and its distribution according to socioeconomic strata of society is of fundamental importance, both for the development and evaluation of health policies as well as for the efficient management of programs intended to reduce the magnitude and inequality occurring from such a phenomenon.
Revision of literature published in 2012 identified few studies on CHE in Brazil, 1 , 2 , 6 , 10 , c among which none analyzed the evolution of inequalities resulting from the conclusions contemplating the 2002-2003 and 2008-2009 periods, the two most recent POF and the only ones based on a sample representing the entire nation.
The objective of this study was to analyze the evolution of CHE and the inequalities in these expenses according to the socioeconomic characteristics of Brazilian families.
METHODS
Data from POF conducted in Brazil during 2002-2003 and 2008-2009 were analyzed. The POF has national scope; it is conducted by the Brazilian Institute of Geography and Statistics (IBGE) since the 1970s, and its main objective is to obtain information about the budget structure of families and Brazilians. d , e
In the research conducted in the two biennia cited above, a sample plan was adopted by conglomerates, where 48,470 households were interviewed in the POF of 2002-2003 and 55,970 households in the POF of 2008-2009. Detailed information on the methodology may be found in the IBGE publications. d , e
The collection of data regarding expenditure included all monetary and non-monetary expenses of families during different recording periods, varying between seven days, 30 days, 90 days and 12 months. The monetary expenses are those carried out through means of payment, on demand or over a period of time, in cash or by check or credit card. The non-monetary expenses do not involve monetary payment, corresponding to acquisitions by means of donations, taken from the business, own production, fishing, hunting or gathering. The income data corresponded to a 12 month period. The health expenditure varied from 30 to 90 days. All figures were annualized and subject to deflation. The index figures used for deflation as well as the reference dates are available in IBGE publications. d , e
The outcome of the current study was the catastrophic expenditure on health. Due to a lack of consensus in domestic and international literature concerning the best methodology for calculating such expenditure, three different forms of calculations, widespread in literature, were employed: methodology proposed by Xu et al 21 (2003), used by Wagstaff & Van Doorslaer 19 (2003), and a variation of the Wagstaff & Van Doorslaer methodology. 7 , 12 Thus, a more deep understanding of the phenomenon in the country is possible as well as better comparison of results with findings from other countries.
The methodology used by Xu et al 21 (2003) employs the concept of the capacity to pay, defined as the subtraction of subsistence (se) expenses of each household from their total costs. When the figures derived from this operation were negative, the expenditure in subsistence was substituted by the expenditure on food in the equation. The subsistence expenditure, in turn, was equal to the average expenditure with food for the households among the 45 and 55 percentiles in expenditure with food (lp) multiplied by the number of residents in each household (size) to the power of beta (β), i.e., if se = lp * size β. 21 The figure for β was obtained for each biennium of the POF by regression of fixed effects, where the outcome was the logarithm of household expenditure on food as a function of the logarithm of the household size. CHE was considered to exist when the coefficient of the division of total health expenditure by the capacity of payment was equal to or greater than 20.0% and 40.0%.
In the methodology used by Wagstaff & Van Doorslaer 19 (2003), the CHE was calculated by dividing global health expenditure by the total household expenditure, discounting in the denominator the amount spent on food (χ 100). The cutoff points used to define CHE were ≥ 10.0% and ≥ 20.0%.
Finally, using the variation of the Wagstaff & Van Doorslaer 19 methodology, CHE was calculated considering the total health expenditure as the numerator and total household expenditure as the denominator (χ 100) with cutoff points of ≥ 10.0% and ≥ 20.0% to define the outcome. 7 , 12
The socioeconomic variables used were the academic level of the head of family and the domestic economic index (DEI). 3 The academic level was obtained in the completed years of study and categorized from zero to four, five to eight, nine to eleven and twelve years or more. The DEI was calculated according to a proposal by Barros & Victoria 3 (2005), considering for analysis 12 assets available in the household and the academic level of the head of family. Thereafter, the variable was categorized in quintiles, with Q1 being the quintile with a worse socioeconomic situation and Q5 the one with the best socioeconomic situation.
The prevalence of outcomes according to each methodology employed was described for all categories of socioeconomic variables in the study. The estimates were generated for both biennia of the POF as a means of comparison. The linear tendency test was used to test the difference between the prevalence of CHE among categories of socioeconomic variables.
In analyzing the socioeconomic inequalities in catastrophic expenditure prevalence, the following measures of inequality were used: (i) relative difference between rates, calculated as the difference in proportions of outcomes among the extreme socioeconomic groups; (ii) ratio of rates, division among proportions of outcomes of the worst socioeconomic level by the proportion of the best level; and (iii) concentration index, calculated for the DEI by means of the relative and accumulated frequency of catastrophic expenditure in the population by applying Brown’s formula (G = 1- ∑k-1 1- (Yi+1+ Yi) (Xi+1- Xi)), where y is the population’s accumulated frequency, and x is the accumulated frequency of the population’s CHE, sorted by socioeconomic variables. 15
The graphic representation of the outcomes distribution was also performed according to their concentration curves. They represent the cumulative distribution of each outcome according to the population’s cumulative proportion. 20
The data was analyzed resorting to the statistics program Stata 9, considering the effect of delineation of the study and sample weightings.
RESULTS
In 2002-2003, 78.0% of the researched households were concentrated in urban areas, 26.1% were families led by women, 40.2% had children, 24.0% were senior citizens, and 60.2% of the heads of family were over the age of 40. In 2008-2009, there was an increase in the number of households led by women (30.5%) and by people over the age of 40 (64.1%). Simultaneously, there was an increase in the proportion of households with senior citizens (27.1%) and little change in those with children (40.7%) and located in urban areas (76.7%).
Regarding CHE, an increase between 2002-2003 and 2008-2009 was observed. The prevalence of CHE according to the different calculation methods varied from 0.7% to 21.1% in 2002-2003 and from 1.4% to 25.0% in 2008-2009. The smallest prevalence was observed in relation to the capacity to pay, whereas the greatest was in relation to total expenditure net of food. When CHE was calculated in relation to total consumption, the increase was of 25.0% at the cutoff point of 10.0%, reaching up to 62.0% when the cutoff point was considered to be 20.0%. When CHE was calculated by subtracting food costs from total expenditure, the variance was 18.5% and 37.0% at the cutoff points of 10.0% and 20.0%, respectively. Finally, when the capacity to pay was included in the calculation, the increase in the proportion of households that incurred CHE was equal to 42.0%, using a cutoff point of 20.0%, and it was 100% when the cutoff point was 40.0% (Table 1).
Table 1. Proportion of households that spent 10.0% and 20.0% or more of their total consumption with catastrophic health expenditures and 40.0% or more in relation to their capacity to pay. Brazil, 2002-2003 and 2008-2009.
| Variable | 2002-2003 | 2008-2009 | ||
|---|---|---|---|---|
|
| ||||
| Catastrophic health expenditure | % | 95%CI | % | 95%CI |
| Total consumption | ||||
| ≥ 10.0% | 14.6 | 14.1;15.2 | 18.2 | 17.7;18.7 |
| ≥ 20.0% | 3.6 | 3.4;3.9 | 5.8 | 5.5;6.1 |
| Total consumption net of food | ||||
| ≥ 10.0% | 21.1 | 20.6;21.9 | 25.0 | 24.4;25.6 |
| ≥ 20.0% | 6.5 | 6.2;6.9 | 8.9 | 8.5;9.2 |
| Capacity to pay | ||||
| ≥ 20.0% | 5.9 | 5.6;6.3 | 8.3 | 8.0;8.7 |
| ≥ 40.0% | 0.7 | 0.6;0.8 | 1.4 | 1.3;1.5 |
When analyzing CHE according to socioeconomic conditions, it was verified that the expenditure was greater among the poorest, except at the cutoff point of 10.0% for the two outcomes in which it was used and among those with less schooling except at the cutoff point of 10.0% for the year of 2002-2003 (Tables 2 and 3).
Analysis of the DEI clearly indicated a socioeconomic gradient, varying from lesser prevalence in the most-favored quintile (Q5) to greater prevalence in the poorest (Q1) (Table 2). In addition, the positive variation in outcomes between the investigated biennia was greater in the poorest strata of society.
Table 2. Proportion of households with catastrophic health expenditures of 10.0% and 20.0% or more of their total health consumption and 40.0% or more in relation to their capacity to pay, according to socioeconomic index. Brazil, 2002-2003 and 2008-2009.
| Variable | 2002-2003 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Catastrophic Health expenditure | Q1a | Q2 | Q3 | Q4 | Q5 | pb | |||||
|
| |||||||||||
| % | 95%CI | % | 95%CI | % | 95%CI | % | 95%CI | % | 95%CI | ||
| Total consumption | |||||||||||
| ≥ 10.0% | 12.9 | 12.2;13.7 | 14.3 | 13.1;15.6 | 14.2 | 13.0;15.5 | 16.8 | 15.3;18.4 | 16.3 | 14.4;18.2 | < 0.001 |
| ≥ 20.0% | 4.0 | 3.6;4.5 | 3.9 | 3.2;4.6 | 3.7 | 3.0;4.4 | 3.1 | 2.5;3.8 | 2.6 | 2.0;3.3 | 0.141 |
| Total consumption net of food | |||||||||||
| ≥ 10.0% | 20.9 | 20.0;21.8 | 20.8 | 19.4;22.2 | 21.1 | 19.6;22.6 | 22.3 | 20.5;24.0 | 20.9 | 18.8;22.9 | 0.42 |
| ≥ 20.0% | 7.6 | 7.0;8.2 | 7.0 | 6.2;7.9 | 6.4 | 5.5;7.3 | 5.6 | 4.6;6.5 | 3.9 | 3.1;4.7 | < 0.001 |
| Capacity to pay | |||||||||||
| ≥ 20.0% | 7.2 | 6.6;6.8 | 6.5 | 5.6;7.3 | 5.7 | 4.8;6.6 | 4.7 | 3.8;5.5 | 3.4 | 2.6;4.1 | < 0.001 |
| ≥ 40.0% | 1.0 | 0.8;1.2 | 0.9 | 0.6;1.2 | 0.6 | 0.4;0.8 | 0.3 | 0.1;0.4 | 0.3 | 0.08;0.6 | < 0.001 |
|
| |||||||||||
| 2008-2009 | |||||||||||
|
| |||||||||||
| Total consumption | |||||||||||
| ≥ 10.0% | 18.4 | 17.5;19.4 | 18.3 | 17.2;19.3 | 18.3 | 17.2;19.4 | 18.4 | 17.2;19.7 | 17.7 | 16.4;19.0 | 0.122 |
| ≥ 20.0% | 7.3 | 6.6;7.9 | 6.2 | 5.5;6.8 | 6.2 | 5.5;7.0 | 5.5 | 4.7;6.2 | 3.7 | 3.2;4.3 | < 0.001 |
| Total consumption net of food | |||||||||||
| ≥ 10.0% | 28.0 | 26.9;29.0 | 25.6 | 24.5;26.8 | 24.8 | 23.6;26.0 | 23.9 | 22.6;25.3 | 22.7 | 21.2;24.2 | < 0.001 |
| ≥ 20.0% | 12.0 | 11.2;12.8 | 9.8 | 9.0;10.5 | 9.3 | 8.5;10.1 | 7.9 | 7.0;8.7 | 5.5 | 4.7;6.2 | < 0.001 |
| Capacity to pay | |||||||||||
| ≥ 20.0% | 11.4 | 10.6;12.2 | 9.2 | 8.4;10.0 | 8.7 | 7.9;9.5 | 7.2 | 6.4;8.0 | 5.0 | 4.2;5.6 | < 0.001 |
| ≥ 40.0% | 2.6 | 2.2;2.9 | 1.6 | 1.3;1.9 | 1.4 | 1.0;1.7 | 0.9 | 0.6;1.2 | 0.5 | 0.3;0.7 | < 0.001 |
a Domestic economic index (DEI) in quintiles, in which Q1 corresponds to the poorest and Q5 to the richest.
b Linear tendency test.
A similar phenomenon was observed when schooling was used as a socioeconomic factor. Approximately one in three households in which the head of family had up to four years of education incurred CHE in 2008-2009, when the cutoff point was 10.0% in the calculation where the denominator was the total expenditure net of food. That amount was 35.0% greater than that observed in the previous biennium for the same socioeconomic group and 43.0% greater than that identified for the same period among those with higher schooling (Table 3).
Table 3. Proportion of households with catastrophic health expenditures of 10.0% and 20.0% or more of total health consumption and 40.0% or more in relation to their capacity to pay, according to academic level. Brazil, 2002-2003 and 2008-2009.
| Variable | 2002-2003 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Catastrophic health expenditure | E1a | E2 | E3 | E4 | pb | ||||
|
| |||||||||
| % | 95%CI | % | 95%CI | % | 95%CI | % | 95%CI | ||
| Total consumption | |||||||||
| ≥ 10.0% | 16.1 | 15.3;16.9 | 12.9 | 11.7;14.1 | 12.4 | 11.2;13.5 | 15.4 | 13.6;17.3 | 0.003 |
| ≥ 20.0% | 4.6 | 4.2;5.0 | 2.6 | 2.0;3.1 | 2.6 | 2.0;3.1 | 3.3 | 2.4;4.3 | < 0.001 |
| Total consumption net of food | |||||||||
| ≥ 10.0% | 23.8 | 22.9;24.6 | 19.0 | 17.7;20.4 | 18.4 | 17.0;19.8 | 19.3 | 17.3;21.4 | < 0.001 |
| ≥ 20.0% | 8.7 | 8.1;9.2 | 4.6 | 3.9;5.2 | 4.5 | 3.8;5.2 | 4.2 | 3.3;5.2 | < 0.001 |
| Capacity to pay | |||||||||
| ≥ 20.0% | 8.0 | 7.4;8.5 | 4.2 | 3.5;4.8 | 3.8 | 3.2;4.4 | 3.8 | 2.8;4.7 | < 0.001 |
| ≥ 40.0% | 1.2 | 1.0;1.3 | 0.4 | 0.2;0.5 | 0.4 | 0.2;0.5 | 0.2 | 0.0;0.5 | < 0.001 |
|
| |||||||||
| 2008-2009 | |||||||||
|
| |||||||||
| Total consumption | |||||||||
| ≥ 10.0% | 23.5 | 22.7;24.3 | 16.2 | 14.3;18.0 | 11.1 | 10.1;12.1 | 17.5 | 16.1;19.0 | < 0.001 |
| ≥ 20.0% | 8.7 | 8.2;9.2 | 4.6 | 3.5;5.6 | 3.2 | 2.6;3.8 | 4.5 | 3.8;5.2 | < 0.001 |
| Total consumption net of food | |||||||||
| ≥ 10.0% | 32.1 | 31.2;33.0 | 23.7 | 21.6;25.8 | 16.7 | 15.5;17.9 | 22.4 | 20.8;23.9 | < 0.001 |
| ≥ 20.0% | 13.5 | 12.8;14.1 | 6.8 | 5.6;8.0 | 5.0 | 4.3;5.7 | 6.3 | 5.4;7.2 | < 0.001 |
| Capacity to pay | |||||||||
| ≥ 20.0% | 12.7 | 12.1;13.3 | 6.4 | 5.2;7.6 | 4.7 | 4.0;5.4 | 5.6 | 4.8;6.4 | < 0.001 |
| ≥ 40.0% | 2.5 | 2.2;2.8 | 1.0 | 0.6;1.4 | 0.7 | 0.4;1.0 | 0.6 | 0.4;0.9 | < 0.001 |
a E1 = 0 to 4 years of study; E2 = 5 to 8; E3 = 9 to 11 and E4 = 12 or more.
b Linear tendency test.
Table 4 presents the absolute and relative difference among the extreme groups of academic backgrounds and DEI in 2002-2003 and 2008-2009. In 2008-2009, the prevalence of CHE, considering the capacity to pay, was five times greater in the first quintile of the DEI and four times greater in the group with lesser education, in comparison with the richer and more educated strata, respectively. On the other hand, when the cutoff point was of 20.0%, for the outcome that incorporated the total consumption net of food expenditure in the denominator, the differences reached 118.0% and 114.0% in 2002-2003 and 2008-2009, respectively. The worst condition was always for the families with the least favorable socioeconomic situation.
Table 4. Measures of inequality in catastrophic health expenditure, according to education and socioeconomic index. Brazil, 2002-2003 and 2008-2009.
| Variable | DEIa | |||
|---|---|---|---|---|
|
| ||||
| Catastrophic health expenditure | Difference between rates (Q1-Q5) | Ratio of rates (Q1/Q5) | ||
|
| ||||
| 2002-2003 | 2008-2009 | 2002-2003 | 2008-2009 | |
| Total consumption | ||||
| ≥ 10.0% | -3.4 | 0.7 | 0.8 | 1.0 |
| ≥ 20.0% | 1.4 | 3.6 | 1.5 | 2.0 |
| Total consumption net of food | ||||
| ≥ 10.0% | 0.0 | 5.3 | 1.0 | 1.2 |
| ≥ 20.0% | 3.7 | 6.5 | 2.0 | 2.2 |
| Capacity to pay | ||||
| ≥ 20.0% | 3.8 | 6.4 | 2.1 | 2.3 |
| ≥ 40.0% | 0.7 | 2.1 | 3.3 | 5.2 |
|
| ||||
| Schoolingb | ||||
|
| ||||
| Total consumption | ||||
| ≥ 10.0% | 0.7 | 6.0 | 1.0 | 1.3 |
| ≥ 20.0% | 1.3 | 4.2 | 1.4 | 1.9 |
| Total consumption net of food | ||||
| ≥ 10.0% | 4.5 | 9.7 | 1.2 | 1.4 |
| ≥ 20.0% | 4.5 | 7.2 | 2.1 | 2.1 |
| Capacity to pay | ||||
| ≥ 20.0% | 4.2 | 7.1 | 2.1 | 2.3 |
| ≥ 40.0% | 1.0 | 1.9 | 6.0 | 4.2 |
a Domestic economic index (DEI) in quintiles, in which Q1 corresponds to the poorest and Q5 to the richest. The comparisons were conducted from Q5 in relation to Q1.
b E1 = 0 to 4 years of schooling; E2 = 5 to 8; E3 = 9 to 11 and E4 = 12 or more. The comparisons were conducted from E5 in relation to E1.
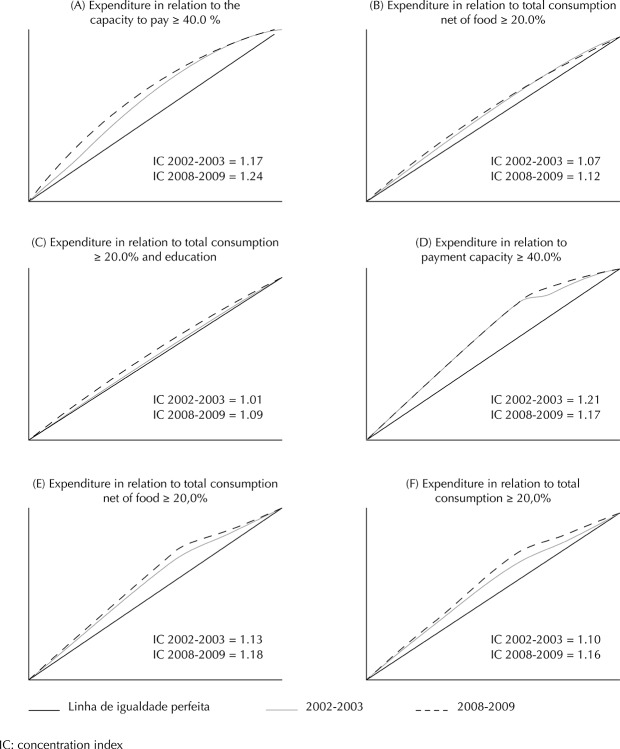
This was also verified in the concentration curves of the different outcomes (Figure). In every case, the distribution curve for 2008-2009 presented greater departure from the line of perfect equality. The greatest index of concentration was recorded in 2008-2009 when analyzing the DEI and CHE in relation to the capacity to pay ≥ 40.0% (Figure A). On the other hand, the smaller concentration was identified when the CHE in relation to total consumption ≥ 20.0% as an outcome (Figure C).
Figure. Concentration curve of catastrophic health expenditure with the domestic economic index: Brazil, 2002-2003 and 2008-2009.
DISCUSSION
The current study revealed an increase in the prevalence of CHE of Brazilian families between 2002-2003 and 2008-2009. In addition, an expressive and increasing socioeconomic inequality was identified in this prevalence, which was higher among the poorer households, which were led by less educated individuals. The prevalence of CHE found in the current study was similar to those verified in the country by Barros et al, 1 Diniz et al, b and Knaul et al 10 and differed from studies by Xu et al 21 and Bos & Waters. 6 The differences occurred, mainly, due to the use of different databases for estimating national expenditure. Xu et al, 21 who reported a CHE of 10.3%, employed the Research about Living Standards, which was conducted in 1996-1997 and included 4,800 households, without national representation. On the other hand, Bos & Waters 6 used data from the PNAD without considering non-monetary expenditure and reported the prevalence of CHE between 3.7% and 20.0%, depending on the definition and cutoff point of the outcome. The POF, besides considering non-monetary expenses, employs a level of detail in capturing expenses and incomes which is unparalleled in any other national research; therefore, it is the most indicated base for studies on expenditure and incomes of Brazilian families. d , e
As expected, the different forms of measuring CHE had a direct impact on the estimated outcomes. Diniz et al b also reported an expressive variation in the prevalence of catastrophic expenditure depending on the formula or cutoff point used. The smallest estimates of CHE were observed logically when the cutoff points were the greatest. Besides, the formulas which used total health expenditure in the numerator and payment capacity in the denominator were those which presented the greatest percentage of CHE. Each calculation method expresses different methods of observing the phenomenon, and there is no consensus over which is the most adequate or which estimates the outcome with greater precision. Meanwhile, the clarity in defining the concept is fundamental as well as the calculation method and data collection instrument to allow the use of this measure by monitoring studies of health expenditure, subsidizing, and evaluating public policies.
In the period under analysis, the average monthly expenditure in health increased by approximately 5.0% in the country, with medication and health plans as the main items, corresponding to 76.0% of private health expenditure in 2008-2009. 9 In addition, both presented an increase in Brazilian family expenditure between the analyzed biennia (9.0% in case of medication and 25.0% for health plans) 9 and were composed of items that substantially compromise their income. 5 , 16
Regarding medication, the difference may be explained by the aging of the population, the increase of the prevalence of chronic diseases, difficulties in accessing products in the scope of a Brazilian Unified Health System (SUS) and by the increase in their use due to the incorporation of new therapeutic products. The analysis conducted with data from the 2008 PNAD verified that only 45.3% of the SUS users, who received prescription medicine in the system, obtained all their medication free of charge. Among those who did not receive them via the UHS, 78.1% had to acquire them from the private sector. 4
The Popular Pharmacy Program (PPP) was created in 2004 f with the aim of broadening the population’s access to basic and essential medication, thereby reducing the impact of these items on the family budget. This program was structured in partnership with states and municipalities and in 2006 was amplified by means of agreements with private establishments.
Although the program’s target audience is the part of the population using the private sector and has financial difficulty in acquiring medication, it became an option both for the users of the private network as well as for the users of the public network who do not obtain their medication free of charge. 14 In a few states and regions of the country, approximately 70.0% of people assisting in the PPP belonged to the population of the public health network, which should have obtained their medication free of charge at the health unit where they were assisted. 14
As such, bearing in mind the aim of mitigating private expenditure on medication, this policy may be directing users from the public sector toward the private sector, with a potential impact on the prevalence of CHE. Therefore, there is a need for additional studies to evaluate such a possibility. Anyhow, the financing capacity of the public sector must be improved, resources must be used efficiently, and an adequate system of the supply of consumables must be structured. 23
Regarding health plans, between 2000 and 2012, there was a substantial increase in the covered population, varying from 18.1% to 25.1%. g In Brazil, the private market for health plans has been set up as a parallel system that competes with the SUS, when in fact is should simply be complementary to the SUS.
Although the monthly fee for these plans is an expense that is part of the household budget, the system of co-payment is ever more common in Brazil and, in some cases, may lead to costs that are greater than people’s capacity to pay. A study conducted with data from the POF 2002-2003 indicated that the coverage per health plan was not sufficient to safeguard families against CHE. 1
Finally, we can observe a growing prevalence of chronic diseases and the incorporation of new therapeutic technologies of elevated cost. Diseases that demand long-treatment times and resources of high technological density have become predominant, thus decisively compromising family budgets. Although the SUS contemplates universal and integral treatment, it is notorious that Brazil possesses a subfinancing of the public health sector when compared with other countries, 23 thus compromising the public system’s capacity to comply with quality and its principles. Consequently, a part of the population returns to the private health care sector in search of answers to their needs, increasing private expenditure, which proportionally in relation to their income may penalize the poorest. While France invested 11.9% of its GDP in 2009 on health, the United Kingdom used 9.8%, New Zealand 10.0%, and Canada 11.4%, Brazil only invested 8.8%, 23 where less than half of this amount was derived from the public sector. In Brazil, the proportion of public expenditure in relation to the total health expenditure (public plus private) was only 43.6%, whereas in Canada this figure was 70.6%, in France it was 77.9%, in New Zealand it was 83.0%, and in the United Kingdom it was 84.1%. 23
According to a study by Xu et al, 22 the incidence of financial catastrophe is inversely proportional to countries’ financing of their health systems, with a greater public financing an important measure in combating CHE.
Besides the increase in CHE, we identified inequality in its distribution. Although the richest quintile spends about 10 times more on health than the poorest, 9 the prevalence of CHE was superior among the poorest quintiles. This result is in accordance with the literature, as observed in China, 11 Argentina, 21 Mexico, 21 and Burkina Faso. 17 The CHE was inversely proportional to the socioeconomic level of those countries, with an increase in expenditure among the richest, whereas the economic cost supported by that group is proportionally smaller. 11 Among the poorest, the need for use and consumption of health goods and services associated with an inadequate health system for their needs, leads to greater costs, and they are forced to access private services.
This perspective of high private expenditure has a great impact on the general population, leading to many not using the health services even when necessary and even to cut back on important expenses for their subsistence to maintain access to the service and to adhere to treatments. 18 , a
One of the limitations of the current study is the restrictive recording period of the collection of health expenditures. When only considering the last 30 days in the case of medication and 90 days for other health expenditure and the observed annual value, one can underestimate or overestimate expenditure estimates. Further, expenditure and income were self-referred, and reported values may have not been the real figures.
Besides the relevance of the SUS as a social policy in Brazil and the improvement of its management and the quality of its services since 1988, it is still insufficient to protect families from CHE. To reverse the regressive structure of health expenditure of families with the worst socioeconomic conditions, one must guarantee access to health goods and services, especially medication, which represents a large proportion of the expenditure of these groups, b by means of financing and efficient management of pharmaceutical services. The SUS user within this system should be guaranteed access to professionals, technologies, and necessary supplies for the promotion and recovery of their health as well as disease prevention. All actions promoting greater access and guaranteeing the integrity and capacity for resolution within the SUS have a strong potential of minimizing CHE because they limit the need for people to resort to the private sector. Access to the SUS has been communicated as a protection factor against catastrophic expenditure, whereas this is not directly observed in relation to health plans. 1 , 6
Footnotes
Organização Mundial de Saúde. Relatório Mundial da Saúde: o financiamento da cobertura Universal. Genebra; 2010.
Diniz BP, Servo LM, Piola SF, Eirado M. Gasto das Famílias com saúde no Brasil: evolução e debate sobre gasto catastrófico. In: Silveira FG, Servo LM, Menezes, Piola SF, organizadores. Gasto e consumo das famílias brasileiras contemporâneas. Brasília (DF): Instituto de Pesquisa Econômica Aplicada; 2007.
Diaz MDM, Sarti FM, Campino ACC, Lunes RF. Catastrophic health expenditure in Brazil: Regional differences, budget constraints and private health insurance. In: Knaul FM, Wong R, Arreola-Ornelas H, organizadores. Financing health in Latin America: household spending and impoverishment. vol. 1. Cambridge: Global Equity Initiative/Harvard University; 2012.
Instituto Brasileiro de Geografia e Estatística. Pesquisa de Orçamentos Familiares 2008-2009. Antropometria e estado nutricional de crianças, adolescentes e adultos no Brasil. Rio de Janeiro; 2010.
Instituto Brasileiro de Geografia e Estatística. Pesquisa de Orçamentos Familiares 2002-2003: primeiros resultados: Brasil e grandes regiões. Rio de Janeiro; 2004.
Brasil. Lei nº 10.836, de 9 de janeiro de 2004. Cria o Programa Bolsa Família e dá outras providências. Diario Oficial. 12 Jan. 2004:1.
Agência Nacional de Saúde. FOCO: Saúde Suplementar. Brasília (DF); 2012 [cited 2013 Jan 15]. Available from: http://www.ans.gov.br/images/stories/Materiais_para_pesquisa/Perfil_setor/Foco/20130124_foco_dezembro_web_2012.pdf
Article based on doctorate thesis by Boing AC, entitled: “Desigualdade socioeconômica nos gastos catastróficos em saúde no Brasil: análise da Pesquisa de Orçamentos Familiares 2002-3 e 2008-9”, presented to the Programa de Pós-Graduação em Saúde Coletiva of the Universidade Federal de Santa Catarina, in 2013.
The authors declare no conflict of interest.
REFERENCES
- 1.Barros AJ, Bastos JL, Dâmaso AH. Catastrophic spending on health care in Brazil: private health insurance does not seem to be the solution. 10.1590/S0102-311X2011001400012Cad Saude Publica. 2011;27(Suppl 2):254–262. doi: 10.1590/s0102-311x2011001400012. [DOI] [PubMed] [Google Scholar]
- 2.Barros AJ, Bertoldi AD. Out-of-pocket health expenditure in a population covered by the Family Health Program in Brazil. 10.1093/ije/dyn063Int J Epidemiol. 2008;37(4):758–765. doi: 10.1093/ije/dyn063. [DOI] [PubMed] [Google Scholar]
- 3.Barros AJD, Victora CG. Indicador econômico para o Brasil baseado no censo demográfico de 2000. 10.1590/S0034-89102005000400002Rev Saude Publica. 2005;39(4):523–529. doi: 10.1590/s0034-89102005000400002. [DOI] [PubMed] [Google Scholar]
- 4.Boing AC, Bertoldi AD, Boing AF, Bastos JL, Peres KG. Acesso a medicamentos no setor público: análise de usuários do Sistema Único de Saúde no Brasil. 10.1590/S0102-311X2013000800007Cad Saude Publica. 2013;29(4):691–701. [PubMed] [Google Scholar]
- 5.Boing AC, Bertoldi AD, Peres KG. Desigualdades socioeconômicas nos gastos e comprometimento da renda com medicamentos no Sul do Brasil. 10.1590/S0034-89102011005000054Rev Saude Publica. 2011;45(5):897–905. [Google Scholar]
- 6.Bos AM, Waters HR. The impact of the public health system and private insurance on catastrophic health expenditures. CEPAL Rev. 2008;95:125–139. [Google Scholar]
- 7.Bredenkamp C, Mendola M, Gragnolati M. Catastrophic and impoverishing effects of health expenditure: new evidence from the Western Balkans. 10.1093/heapol/czq070Health Policy Plan. 2011;26(4):349–356. doi: 10.1093/heapol/czq070. [DOI] [PubMed] [Google Scholar]
- 8.Couttolenc B, Dmytraczenko T. Brazil’s primary care strategy. Vol. 2. Washington (DC): World Bank; 2013. (Universal Health Coverage Studies Series (UNICO)). [Google Scholar]
- 9.Garcia LP, Sant’ana AC, Magalhães LCG, Aurea AP. Gastos com saúde das famílias brasileiras residentes em regiões metropolitanas: composição e evolução no período 1995-2009. 10.1590/S1413-81232013000100013Cienc Saude Coletiva. 2013;18(1):115–128. doi: 10.1590/s1413-81232013000100013. [DOI] [PubMed] [Google Scholar]
- 10.Knaul FM, Wong R, Arreola-Ornelas H, Méndez O, Network on Health Financing and Social Protection in Latin America and the Caribbean (LANET) Household catastrophic health expenditures: a comparative analysis of twelve Latin American and Caribbean Countries. 10.1590/S0036-36342011000800005Salud Publica Mex. 2011;53(Suppl 2):85–95. [PubMed] [Google Scholar]
- 11.Li Y, Wu Q, Xu L, Legge D, Hao Y, Gao L, et al. Factors affecting catastrophic health expenditure and impoverishment from medical expenses in China: policy implications of universal health insurance. 10.2471/BLT.12.102178Bull World Health Organ. 2012;90(9):664–671. doi: 10.2471/BLT.12.102178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mataria A, Raad F, Abu-Zaineh M, Donaldson C. Catastrophic healthcare payments and impoverishment in the occupied Palestinian territory. 10.2165/11318200-000000000-00000Appl Health Econ Health Policy. 2010;8(6):393–405. doi: 10.2165/11318200-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.O’Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation. Washington (DC): World Bank; 2008. [Google Scholar]
- 14.Santos-Pinto CB, Costa NR, Osorio-de-Castro CGS. Quem acessa o Programa Farmácia Popular do Brasil? Aspectos do fornecimento público de medicamentos. 10.1590/S1413-81232011000600034Cienc Saude Coletiva. 2011;16(6):2963–2973. doi: 10.1590/s1413-81232011000600034. [DOI] [PubMed] [Google Scholar]
- 15.Schneider MC, Castillo-Salgado C, Bacallao J, Loyola E, Mujica OJ, Vidaurre M, et al. Métodos de mensuração das desigualdades em saúde. 10.1590/S1020-49892002001200006Rev Panan Salud Publica. 2002;12(6):1–17. [Google Scholar]
- 16.Silveira FG, Osório RG, Piola SF. Os gastos das famílias com saúde. 10.1590/S1413-81232002000400009Cienc Saude Coletiva. 2002;7(4):719–731. [Google Scholar]
- 17.Su TT, Kouyaté B, Flessa S. Catastrophic household expenditure for health care in a low income society: a study from Nouna district, Burkina Faso. 10.2471/BLT.05.023739Bull World Health Organ. 2006;84(1):21–27. doi: 10.2471/blt.05.023739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Doorslaer E, O’Donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Garg CC, et al. Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. 10.1016/S0140-6736(06)69560-3Lancet. 2006;368(9544):1357–1364. doi: 10.1016/S0140-6736(06)69560-3. [DOI] [PubMed] [Google Scholar]
- 19.Wagstaff A, Van Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993-1998. 10.1002/hec.776Health Econ. 2003;12(11):921–934. doi: 10.1002/hec.776. [DOI] [PubMed] [Google Scholar]
- 20.Wagstaff A, Bilger M, Sajaia Z, Lokshin M. Health equity and financial protection. Washington (DC): World Bank; 2011. [Google Scholar]
- 21.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. 10.1016/S0140-6736(03)13861-5Lancet. 2003;362(9378):111–117. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 22.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Health Aff. 4. Vol. 26. Millwood: 2007. Protecting households from catastrophic health spending; pp. 972–983. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization WHO Global Health Expenditure Atlas. Geneva: 2012. [Google Scholar]