Abstract
OBJECTIVE
To analyze the factors associated with the use of pacifiers and/or bottle feeding in infants aged under one year.
METHODS
This is a cross-sectional study with 34,366 children and using data from the database of the 2nd Nationwide Survey of Breastfeeding Prevalence performed in the Brazilian capitals and Federal District in 2008. Cluster sampling was used. The questionnaire included questions about the use of artificial nipples in the last 24 hours. The analysis considered three outcomes: exclusive use of pacifier, exclusive use of bottle feeding, and use of artificial nipples (pacifier and bottle feeding). Prevalence ratios were obtained using Poisson regression with robust variance following a hierarchical model.
RESULTS
The following factors were associated with exclusive use of the pacifier: mother working outside the home, primiparity, child was not breastfed within the first hour, and child had consumed tea on the first day at home. The following factors were associated with exclusive use of bottle feeding: mother working outside the home, primiparity, low birth weight, child not breastfed within the first hour, and child had consumed milk formula and tea on the first day at home. The following factors were associated with use of artificial nipples (pacifier and bottle feeding): mother working outside the home, primiparity, cesarean delivery, the male gender, low birth weight, born in a hospital not accredited as “baby friendly”, required health baby monitoring in the Primary Health Care Unit (PR = 0.91), and child had consumed milk formula, water, or tea on the first day at home.
CONCLUSIONS
This study identified profiles of exclusive users of pacifiers, bottle feeding, and both. The provided information can guide preventive practices for child health.
Keywords: Bottle Feeding; Pacifiers, utilization; Maternal and Child Health; Cross-Sectional Studies
RESUMO Abstract
OBJETIVO
Analisar os fatores associados ao uso de chupeta e/ou mamadeira em lactentes menores de um ano.
MÉTODOS
Estudo transversal realizado com dados de 34.366 crianças obtidos da II Pesquisa Nacional de Prevalência de Aleitamento Materno, realizada em 2008, nas capitais brasileiras e Distrito Federal. Foi utilizada amostragem por conglomerados e o questionário incluiu perguntas sobre o uso de bicos artificiais nas últimas 24h. Três desfechos foram considerados para a análise: uso exclusivo de chupeta, uso exclusivo de mamadeira e uso de bicos artificiais (chupeta e mamadeira). As razões de prevalência foram obtidas por regressão de Poisson com variância robusta seguindo modelo hierárquico.
RESULTADOS
Associaram-se ao uso exclusivo de chupeta: mãe trabalhar fora, primiparidade, não ter sido amamentado na primeira hora e uso do chá no primeiro dia em casa. Para uso exclusivo da mamadeira, foram identificados: mãe trabalhar fora, primiparidade, baixo peso ao nascer, não amamentado na primeira hora de vida, uso de fórmula e chá no primeiro dia em casa. O uso de bicos artificiais (chupeta e mamadeira) foi associado com trabalho materno fora do lar, primiparidade, parto cesárea, bebês do sexo masculino, baixo peso ao nascer, nascimento em um hospital não credenciado como “Amigo da Criança”, realizar o acompanhamento de saúde da criança em unidade básica de saúde (RP = 0,91), uso de fórmula, água e chá no primeiro dia em casa.
CONCLUSÕES
Este estudo encontrou perfis de usuários exclusivos de chupetas, mamadeiras e de ambos. Essas informações podem orientar as práticas preventivas para a saúde da criança.
INTRODUCTION
It is estimated that two-thirds of newborns will receive bottle feeding and pacifiers during the first year of life. 24 However, the use of these tools can affect breastfeeding 14 and induce alteration in the children’s health. 9 , 19 , 23 In the history of mankind, the use of artificial nipples has assumed different roles and sociocultural representations. 12 , 16 , 23
Among the pacifier users, those who use it more frequently include firstborn children, 19 , 24 males, 18 , 23 , 24 children with low birth weight, 23 children aged under 6 months, 19 children not breastfed in the maternity ward, 23 and children breastfed at prearranged times. 22 In addition, mothers who were younger, 1 , 6 , 23 were primiparous, 6 , 23 had a low socioeconomic status, 9 had a smoking history, 9 , 24 and were less educated 1 , 9 , 18 were more likely to resort to the use of pacifiers. Qualitative studies have indicated that the use of pacifiers is correlated with cultural issues, maternal uncertainty about her ability to breastfeed, and crying and behavior of baby. 3 , 16 , 23 , 24 Previous studies have indicated that infant-related factors that favor the use of bottle feeding include decreased weight gain, excessive crying, 12 the use of pacifiers, 6 and the consumption of processed milk, tea, and water. 6 Maternal-related factors that favor the use of bottle feeding include teenage mothers, 6 maternal uncertainty about her ability to breastfeed and difficulty in breastfeeding, 6 , 12 , 23 nervousness and impatience, 12 convenience, 12 working outside the home, 12 , 13 and coexistence with the maternal grandmother. 6 In addition, parents and health professionals indicate that the use of bottle feeding facilitates feeding and brings confidence during infant feeding.
However, these results cannot be generalized because the aforementioned studies were conducted in distinct periods, with distinct methodologies and population groups. Till date, no study has investigated the determinants of the use of artificial nipples using a representative sample of children in Brazil. Therefore, the present study aimed to identify the factors associated with the use of pacifiers and/or bottle feeding in children aged under one year.
METHODS
This cross-sectional study analyzed data from the Second National Survey on the Prevalence of Breastfeeding (II NSPB), conducted in Brazil in 2008. a
The II NSPB is a national survey on the status of breastfeeding and complementary feeding involving children aged ≤ 12 months who participated in the second phase of the national campaign of multivaccination. 21
The survey was conducted with cluster samples, lots were cast in two stages, and the probabilities were proportional to the cluster size. In the first stage, lots were cast on the vaccination sites, and in the second stage, lots were cast on the children vaccinated at each site. The sample size considered the prevalence of exclusive breastfeeding in 1999, in the 26 state capitals and in the Federal District (FD), with an added rate of 2.0%-10.0% to account for the increase in prevalence. To compensate for the potential loss of precision, the design effect was added to the sample by multiplying the initial estimate by 1.5 and incorporating a nonresponse rate, which ranged between 5.0% and 10.0%. The sample size required to estimate the prevalence of breastfeeding in children aged < 6 months was multiplied by two. Therefore, the minimum sample size varied between each capital but was reached in all capitals, ensuring sample representativeness. In total, 34,366 children aged under one year, who participated in the second phase of the multivaccination campaign conducted in all Brazilian capitals and FD in 2008, were analyzed. Detailed data of each sample population by capital have been reported previously. 21 , 22
For proper implementation of the process of casting lots on the children participating in the vaccination program, the interviewers were provided instructions with regard to the importance of randomness in data collection and systematic random sampling. 21
The data collection instrument was also applied to the child’s parents or guardians. The questionnaire included closed questions related to the children and mother profile, infant feeding, health care services used by families, and use of pacifiers and bottle feeding in the last 24 hours.
Three outcomes were defined: the exclusive use of pacifiers (i.e., nonusers of bottle feeding), exclusive use of bottle feeding (i.e., nonusers of pacifiers), and use of artificial nipples (users of both pacifiers and bottle feeding). Each of the three outcomes were classified on the basis of the affirmative responses to the outcome in relation to the lack of use of artificial nipples during the study period, similar to the methodology used in studies on disease-associated factors (sick versus healthy patients). The three children subsamples with a positive outcome were compared with the subsample comprising the nonusers of artificial nipples. We chose this analysis strategy to attenuate potential confounders.
Data entry was performed by team members in each state capital using a web application specially developed for the typing of this information. 21 The II NSPB database was exported to Stata software version 9.2 for data analysis. Sample complexity in all the study phases was considered.
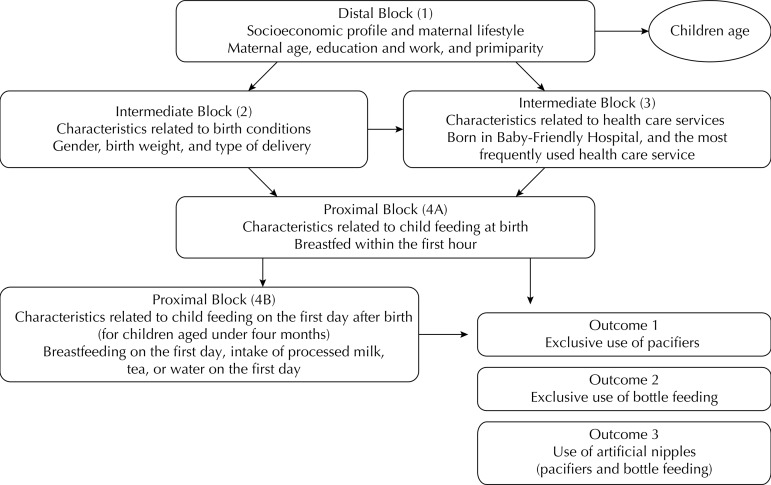
After descriptive analysis, age-adjusted Poisson regression analysis with robust variance 4 was used to estimate the prevalence ratio (PR) and confidence intervals (95%CI). A linear trend test was used for the variables having a theoretical assumption of a dose-response relation. To estimate the individual influence of the outcome-associated variables, we used a multiple hierarchical model. For this purpose, the variables were grouped into blocks and ordered according to the influence that they would have on each outcome. The theoretical model that guided the analysis and the variables are presented in Figure. Notably, the variables related to infant feeding during the first day after hospital discharge were only collected for children aged under four months (subsample) to any avoid possible memory bias.
Figure. Hierarchical theoretical model to determine the factors associated with use of artificial nipples. State capitals and Federal District, Brazil, 2008.
Considering that this study has three different outcomes, the steps for data analysis were separately reproduced for each outcome. Initially, PR was calculated for each variable and outcome (step 1). Variables with p < 0.20 were entered into multiple internal analysis of each block (step 2). Following this, variables with p < 0.20 in internal analysis of each block were used as control variables in step 3 as follows.
The variables of the more distal block (1), “Socioeconomic profile and maternal lifestyle”, were the first variables to be included in the model and served as adjustment factors for the hierarchically inferior variables. Similarly, the variables of the intermediate blocks (2 and 3), “Characteristics related to birth conditions and the health care services used”, which met the inclusion criteria of the multivariate model after adjusting for the distal block, became the control variables of the subsequent block. An analogous procedure was adopted for analyzing the proximal blocks (4A and 4B), “Characteristics of infant feeding within the first hour after birth and on the first day after hospital discharge”. The selected variables were maintained in the model despite having lost statistical significance after including the inferior blocks. After adjusting for the factors of the same block and superior blocks, the correlation between variables and outcomes was considered significant by adopting a significance level of 5%.
The research protocol was approved by the Research Ethics Committee of the Faculdade de Saúde Pública of the Universidade de São Paulo (Protocol 2,192, from 3/18/2011).
RESULTS
The study included 34,366 children aged ≤ 12 months. We observed a predominance of children aged under six months (54.5%) and of the male gender. Low birth weight was observed in 9.0% of the children. Most mothers were aged between 20 and 35 years (72.2%), had < 12 years of education (85.6%), and did not work outside the home (66.2%). Approximately 50.0% of the mothers were primiparous, and approximately 50.0% deliveries were cesarean. One-third of the deliveries occurred in a Baby-Friendly Hospital initiative (BFH), and 58.7% of the children had routine follow-up in public health care units (basic health care units or family health strategy (FHS) units). Approximately 70.0% of the children were breastfed within the first hour after birth. With regard to the outcomes, information on the use of pacifiers and/or bottle feeding was available for 33,776 children (98.3%). Of these, 2,901 (9.1%) exclusively used pacifiers, 8,757 (24.8%) exclusively used bottle feeding, and 10,451 (33.5%) used artificial nipples. Approximately one-third (n = 11,667, 32.6%) of the children used no artificial nipples.
In the subsample of children aged under four months (n = 12,704), 95.9% were breastfed on the first day after hospital discharge. In contrast, processed milk, tea, and water were consumed on the first day after birth by 12.0%, 8.4%, and 5.0% of the children, respectively. To determine the similarity between the subsample of children aged under four months and the rest of the population, these two groups were compared in relation to maternal education (considered in this study as a proxy for the socioeconomic status), infant gender, birth weight, and type of delivery. No significant differences were found among these groups.
The sample strata used for analysis of the exclusive use of pacifiers comprised exclusive users of pacifiers (n = 2,901) and nonusers of artificial nipples (n = 11,667). The frequency of use of pacifiers gradually decreased as infant age increased, indicating a strong inverse correlation (p < 0.001) (data not shown).
Table 1 shows the prevalence of children who used exclusively pacifiers among those born from primiparous women, those born by cesarean delivery, and male infants. The use of pacifiers gradually increased among children born from mothers who worked outside the home. It was observed that the consumption of tea on the first day after hospital discharge and the inability to breastfeed within the first hour after birth were associated with the increased use of pacifiers.
Table 1. Poisson analysis of the exclusive use of pacifiers in children aged under one year and age-adjusted prevalence ratio. State capitals and Federal District, Brazil, 2008.
| Variable | Total Na | Exclusive use of pacifier (%) | PRadjusted | 95%CI | p |
|---|---|---|---|---|---|
| Distal block (1) | |||||
| Maternal age (years) | 0.122b | ||||
| 20 to 35 | 9,017 | 21.3 | 1 | ||
| < 20 | 3,044 | 23.0 | 1.09 | 0.97;1.24 | 0.119 |
| > 35 | 1,372 | 21.9 | 1.03 | 0.88;1.21 | 0.685 |
| Maternal education (years) | 0.161b | ||||
| > 12 | 1,795 | 24.8 | 1 | ||
| 9 to 12 | 6,363 | 21.7 | 0.90 | 0.77;1.03 | 0.139 |
| 0 to 8 | 5,189 | 20.9 | 0.90 | 0.76;1.02 | 0.093 |
| Maternal work | 0.016b | ||||
| Not working outside the home | 9,025 | 20.6 | 1 | ||
| On maternity leave | 1,964 | 26.9 | 1.13 | 0.99;1.29 | 0.076 |
| Working outside the home | 1,678 | 23.1 | 1.16 | 1.00;1.35 | 0.045 |
| Primiparity | |||||
| No | 7,079 | 19.3 | 1 | ||
| Yes | 6,114 | 24.8 | 1.28 | 1.16;1.41 | < 0.001 |
|
Intermediate block (2 to 3) | |||||
| Type of delivery | |||||
| Normal/Forceps | 7,582 | 20.7 | 1 | ||
| Cesarean | 6,862 | 23.0 | 1.10 | 1.00;1.21 | 0.049 |
| Infant gender | |||||
| Female | 7,395 | 20.8 | 1 | ||
| Male | 7,173 | 22.8 | 1.10 | 1.00;1.21 | 0.041 |
| Low birth weight ( < 2,500 g) | |||||
| No | 13,182 | 22.1 | 1 | ||
| Yes | 1,069 | 20.4 | 0.90 | 0.74;1.10 | 0.297 |
| Born in Baby-Friendly Hospital | |||||
| Yes | 5,092 | 21.5 | 1 | ||
| No | 8,385 | 22.1 | 1.02 | 0.92;1.13 | 0.611 |
| Routine health care services | |||||
| Family Health Strategy | 3,715 | 23.4 | 1 | ||
| Basic health care unit | 4,514 | 20.7 | 0.89 | 0.79;1.01 | 0.088 |
| Private health care services | 4,747 | 23.4 | 1.00 | 0.89;1.13 | 0.923 |
|
Proximal block (4A) | |||||
| Breastfed within first hour of birth | |||||
| Yes | 9,976 | 20.3 | 1 | ||
| No | 3,886 | 24.8 | 1.19 | 1.08;1.32 | 0.001 |
|
Proximal block (4B) | |||||
| Breastfed on the first day after hospital discharge | |||||
| Yes | 7,310 | 25.6 | 1 | ||
| No | 168 | 23.8 | 0.94 | 0.66;1.33 | 0.744 |
| Consumed processed milk on the first day after hospital discharge | |||||
| No | 7,021 | 25.3 | 1 | ||
| Yes | 384 | 28.9 | 1.16 | 0.91;1.48 | 0.219 |
| Consumed water on the first day after hospital discharge | |||||
| No | 7,219 | 25.6 | 1 | ||
| Yes | 186 | 23.3 | 0.96 | 0.62;1.48 | 0.873 |
| Consumed tea on the first day after hospital discharge | |||||
| No | 7,052 | 25.2 | 1 | ||
| Yes | 337 | 32.0 | 1.30 | 1.01;1.67 | 0.040 |
a This analysis included exclusively users of pacifiers and nonusers of artificial nipples.
b Linear trend test.
Table 2 shows that the factors associated with the exclusive use of pacifiers in multivariate analysis were primiparity, mother working outside the home, inability to breastfeed within the first hour after birth, and consumption of tea on the first day after hospital discharge.
Table 2. Multiple hierarchical model to identify the factors associated with the exclusive use of pacifiers in children aged under one year. State capitals and Federal District, Brazil, 2008.
| Variable | PRadjusted | 95%CI | p |
|---|---|---|---|
| Model 1a | |||
| Maternal work | 0.017d | ||
| Not working outside the home | 1 | ||
| On maternity leave | 1.11 | 0.96;1.27 | 0.139 |
| Working outside the home | 1.18 | 1.01;1.37 | 0.034 |
| Primiparity | |||
| No | 1 | ||
| Yes | 1.28 | 1.15;1.42 | < 0.001 |
|
Model 3b | |||
| Breastfed within the first hour after birth | |||
| Yes | 1 | ||
| No | 1.15 | 1.03;1.29 | 0.014 |
|
Model 4c | |||
| Ingested tea on the first day after birth | |||
| No | 1 | ||
| Yes | 1.37 | 1.05;1.79 | 0.020 |
a Model 1: work, primiparity, and infant age.
Model 2: Model 1 + infant gender and type of delivery.
b Model 3: Model 2 + breastfeeding within the first hour.
c Model 4: Model 3 + consumption of tea on the first day after hospital discharge.
d Linear trend test.
The sample strata used for analysis of the exclusive use of bottle feeding comprised exclusive users of bottle feeding (n = 8,757) and nonusers of artificial nipples (n = 11,667).
It was observed that as the children age progressed, the exclusive use of bottle feeding increased. Trend analysis indicated the existence of a dose-response relationship (p < 0.001) (data not shown).
Table 3 shows that the frequency of use of bottle feeding gradually increased among working mothers; however, no significant difference was observed between mothers on maternity leave and those who did not work outside the home. Low birth weight and inability to breastfeed within the first hour after birth were associated with the increased use of bottle feeding. As expected, the consumption of commercial milk, tea, or water on the first day after hospital discharge stimulated the exclusive use of bottle feeding.
Table 3. Poisson analysis of the exclusive use of bottle feeding in children aged under one year and age-adjusted prevalence ratio. State capitals and Federal District, Brazil, 2008.
| Variable | Total Na | Exclusive use of baby bottles (%) | PRadjusted | 95%CI | p |
|---|---|---|---|---|---|
| Distal block (1) | |||||
| Maternal age (years) | 0.274b | ||||
| 20 to 35 | 12,127 | 40.6 | 1 | ||
| < 20 | 4,243 | 42.0 | 1.02 | 0.96;1.08 | 0.433 |
| > 35 | 1,897 | 44.5 | 1.07 | 0.98;1.15 | 0.090 |
| Maternal education (years) | 0.008b | ||||
| > 12 | 2,419 | 44.7 | 1 | ||
| 9 to 12 | 8,725 | 41.4 | 0.93 | 0.87;1.00 | 0.073 |
| 0 to 8 | 7,036 | 40.3 | 0.90 | 0.83;0.96 | 0.006 |
| Maternal work | < 0.001b | ||||
| Not working outside the home | 12,171 | 39.0 | 1 | ||
| On maternity leave | 1,985 | 26.6 | 0.99 | 0.88;1.12 | 0.953 |
| Working outside the home | 3,089 | 60.3 | 1.40 | 1.33;1.48 | < 0.001 |
| Primiparity | |||||
| No | 9,424 | 38.7 | 1 | ||
| Yes | 8,501 | 44.3 | 1.13 | 1.07;1.19 | < 0.001 |
|
Intermediate block (2 to 3) | |||||
| Type of delivery | |||||
| Normal/Forceps | 10,526 | 41.6 | 1 | ||
| Cesarean | 9,698 | 45.0 | 1.08 | 1.03;1.13 | 0.001 |
| Child gender | |||||
| Female | 10,287 | 42.3 | 1 | ||
| Male | 10,137 | 44.2 | 1.01 | 0.97;1.06 | 0.488 |
| Low birth weight (< 2,500 g) | |||||
| No | 18,188 | 42.4 | 1 | ||
| Yes | 1,711 | 49.6 | 1.18 | 1.09;1.27 | < 0.001 |
| Born in Baby-Friendly Hospital | |||||
| Yes | 6,993 | 41.9 | 1 | ||
| No | 11,881 | 44.2 | 1.05 | 1.00;1.10 | 0.050 |
| Routine health care services | |||||
| Family Health Strategy | 5,129 | 42.1 | 1 | ||
| Basic health care unit | 6,371 | 41.6 | 0.96 | 0.90;1.02 | 0.252 |
| Private health care services | 6,854 | 47.3 | 1.08 | 1.02;1.14 | 0.008 |
|
Proximal block (4A) | |||||
| Breastfed within the first hour after birth | |||||
| Yes | 13,793 | 24.9 | 1 | ||
| No | 5,485 | 38.7 | 1.55 | 1.15;2.09 | 0.003 |
|
Proximal block (4B) | |||||
| Breastfed on the first day after hospital discharge | |||||
| Yes | 7,467 | 24.9 | 1 | ||
| No | 197 | 38.7 | 1.50 | 1.12;2.03 | 0.007 |
| Consumed processed milk on the first day after hospital discharge | |||||
| No | 7,007 | 22.8 | 1 | ||
| Yes | 580 | 51.4 | 2.20 | 1.91;2.52 | < 0.001 |
| Consumed water on the first day after hospital discharge | |||||
| No | 7,318 | 24.6 | 1 | ||
| Yes | 266 | 41.3 | 1.54 | 1.21;1.94 | < 0.001 |
| Consumed tea on the first day after hospital discharge | |||||
| No | 7,079 | 23.3 | 1 | ||
| Yes | 493 | 52.2 | 2.15 | 1.86;2.49 | < 0.001 |
a This analysis included exclusively users of baby bottles and nonusers of artificial nipples.
b Linear trend test.
Table 4 indicates that the factors associated with the exclusive use of bottle feeding in multivariate analysis were primiparity, mother working outside the home, low birth weight, inability to breastfeed within the first hour after birth, and the consumption of processed milk or tea on the first day after hospital discharge.
Table 4. Multiple hierarchical model to identify the factors associated with the exclusive use of bottles in children aged under one year. State capitals and Federal District, Brazil, 2008.
| Variable | PRadjusted | 95%CI | p |
|---|---|---|---|
| Model 1a | |||
| Maternal work | < 0.001e | ||
| Not working outside the home | 1 | ||
| On maternity leave | 0.97 | 0.86;1.10 | 0.708 |
| Working outside the home | 1.39 | 1.32;1.47 | < 0.001 |
| Primiparity | |||
| No | 1 | ||
| Yes | 1.06;1.17 | < 0.001 | |
|
Model 2b | |||
| Low birth weight | |||
| No | 1 | ||
| Yes | 1.21 | 1.11;1.31 | < 0.001 |
|
Model 3c | |||
| Breastfed within the first hour after birth | |||
| Yes | 1 | ||
| No | 1.08 | 1.02;1.15 | 0.004 |
|
Model 4d | |||
| Consumed processed milk on the first day after hospital discharge | |||
| No | 1 | ||
| Yes | 1.82 | 1.52;2.19 | < 0.001 |
| Consumed tea on the first day after hospital discharge | |||
| No | 1 | ||
| Yes | 1.96 | 1.63;2.36 | < 0.001 |
a Model 1: maternal work, primiparity, infant age.
b Model 2: Model 1 + low birth weight.
c Model 3: Model 2 + breastfeeding within the first hour.
d Model 4: Model 3 + intake of processed milk or tea on the first day.
e Linear trend test.
The sample strata used for analysis of the use of artificial nipples comprised users of artificial nipples (pacifiers and bottle feeding) (n = 10,451) and nonusers of artificial nipples (n = 11,667).
Advancing child age was associated with the increased use of artificial nipples. Trend analysis indicated a significant correlation (p < 0.001), suggesting the existence of a dose-response relationship (data not shown).
Table 5 shows that younger women offered artificial nipples to their children more frequently than older women. Moreover, primiparous women offered artificial nipples to their children more frequently than nonprimiparous women. Cesarean delivery, low birth weight, and the male gender were factors associated with the increased use of artificial nipples. As expected, mothers who worked outside the home resorted to artificial nipples more frequently than those who did not work outside the home. However, births in BFH and breastfeeding within the first hour after birth favored the decreased use of artificial nipples. Children routinely attending basic health care units tended to use artificial nipples less frequently, whereas those attending private health care facilities tended to use artificial nipples more frequently.
Table 5. Poisson analysis of the use of artificial nipples in children aged under one year and age-adjusted prevalence ratio. State capitals and Federal District, Brazil, 2008.
| Variable | Total Na | Use of artificial nipples (%) | PRadjusted | 95%CI | p |
|---|---|---|---|---|---|
| Distal block (1) | |||||
| Maternal age (years) | 0.004b | ||||
| 20 to 35 | 12,809 | 46.8 | 1 | ||
| < 20 | 4,584 | 50.1 | 1.07 | 1.02;1.13 | 0.008 |
| > 35 | 2,018 | 50.6 | 1.06 | 0.99;1.14 | 0.072 |
| Maternal education (years) | < 0.001b | ||||
| > 12 | 2,783 | 55.7 | 1 | ||
| 9 to 12 | 9,056 | 47.1 | 0.86 | 0.81;0.91 | < 0.001 |
| 0 to 8 | 7,479 | 46.6 | 0.84 | 0.79;0.89 | < 0.001 |
| Maternal work | < 0.001b | ||||
| Not working outside the home | 12,550 | 43.8 | 1 | ||
| On maternity leave | 2,148 | 34.1 | 0.97 | 0.88;1.08 | 0.644 |
| Working outside the home | 3,562 | 69.1 | 1.45 | 1.39;1.52 | < 0.001 |
| Primiparity | |||||
| No | 9,680 | 43.2 | 1 | ||
| Yes | 9,349 | 52.9 | 1.21 | 1.16;1.26 | < 0.001 |
|
Intermediate block (2 to 3) | |||||
| Type of delivery | |||||
| Normal/Forceps | 11,132 | 48.4 | 1 | ||
| Cesarean | 10,718 | 52.7 | 1.09 | 1.04;1.13 | < 0.001 |
| Child gender | |||||
| Female | 11,021 | 49.4 | 1 | ||
| Male | 11,097 | 52.1 | 1.04 | 1.00;1.08 | 0.016 |
| Low birth weight (< 2,500 g) | |||||
| No | 19,657 | 49.9 | 1 | ||
| Yes | 1,866 | 55.2 | 1.11 | 1.05;1.19 | < 0.001 |
| Born in Baby-Friendly Hospital | |||||
| Yes | 7,496 | 45.5 | 1 | ||
| No | 12,812 | 53.0 | 1.15 | 1.10;1.20 | < 0.001 |
| Routine health care services | |||||
| Family Health Strategy | 5,521 | 49.6 | 1 | ||
| Basic health care unit | 6,528 | 46.7 | 0.93 | 0.88;0.98 | 0.011 |
| Private Health Care Service | 7,723 | 56.5 | 1.09 | 1.05;1.15 | < 0.001 |
|
Proximal block (4A) | |||||
| Breastfed within the first hour after birth | |||||
| Yes | 14,669 | 49.0 | 1 | ||
| No | 6,129 | 52.5 | 1.09 | 1.05;1.14 | < 0.001 |
|
Proximal block (4B) | |||||
| Breastfed on the first day after hospital discharge | |||||
| Yes | 8,082 | 33.5 | 1 | ||
| No | 399 | 72.4 | 2.11 | 1.91;2.33 | < 0.001 |
| Consumed processed milk on the first day after hospital discharge | |||||
| No | 7,493 | 30.6 | 1 | ||
| Yes | 910 | 70.5 | 2.25 | 2.08;2.44 | < 0.001 |
| Consumed water on the first day after hospital discharge | |||||
| No | 7,952 | 33.6 | 1 | ||
| Yes | 438 | 66.2 | 1.87 | 1.67;2.08 | < 0.001 |
| Consumed tea on the first day after hospital discharge | |||||
| No | 7,746 | 33.1 | 1 | ||
| Yes | 639 | 64.0 | 1.87 | 1.70;2.06 | < 0.001 |
a This analysis included exclusive user of artificial nipples (pacifiers and bottle feeding) and nonusers of artificial nipples.
b Linear trend test.
Table 6 presents the factors associated with the use of artificial nipples after adjusting for other variables: mother working outside the home, primiparity, cesarean delivery, the male gender, low birth weight, deliveries in hospitals not accredited by the BFH system, type of health care service (private/health insurance), inability to breastfeed within the first hour after birth, and consumption of processed milk, tea, or water on the first day after hospital discharge. Performing routine follow-up in primary health care units was a protective factor against the use of artificial nipples.
Table 6. Multiple hierarchical model to identify the factors associated with the use of artificial nipples in children aged under one year. State capitals and Federal District, Brazil, 2008.
| Variable | PRadjusted | 95%CI | p |
|---|---|---|---|
| Model 1a | |||
| Maternal work | < 0.001f | ||
| Not working outside the home | 1 | ||
| On maternity leave | 0.95 | 0.86;1.07 | 0.447 |
| Working outside the home | 1.43 | 1.37;1.51 | < 0.001 |
| Primiparity | |||
| No | 1 | ||
| Yes | 1.21 | 1.15;1.27 | < 0.001 |
|
Model 2b | |||
| Type of delivery | |||
| Normal/Forceps | 1 | ||
| Cesarean | 1.06 | 1.01;1.12 | 0.008 |
| Child gender | |||
| Female | 1 | ||
| Male | 1.07 | 1.02;1.12 | 0.003 |
| Low birth weight | |||
| No | 1 | ||
| Yes | 1.11 | 1.03;1.19 | 0.005 |
|
Model 3c | |||
| Born in Baby-Friendly Hospital | |||
| Yes | 1 | ||
| No | 1.12 | 1.06;1.18 | < 0.001 |
| Routine health care services | |||
| Family Health Strategy | 1 | ||
| Basic Health Care Unit | 0.91 | 0.86;0.97 | 0.005 |
| Private health care services | 1.02 | 0.96;1.09 | 0.397 |
|
Model 4d | |||
| Breastfed within the first hour after birth | |||
| Yes | 1 | ||
| No | 1.06 | 1.00;1.11 | 0.030 |
|
Model 5e | |||
| Consumed processed milk on the first day after hospital discharge | |||
| No | 1 | ||
| Yes | 2.06 | 1.83;2.31 | < 0.001 |
| Consumed water on the first day after hospital discharge | |||
| No | 1 | ||
| Yes | 1.18 | 1.01;1.37 | < 0.001 |
| Consumed tea on the first day after hospital discharge | |||
| No | 1 | ||
| Yes | 1.38 | 1.21;1.59 | < 0.001 |
a Model 1: maternal age, education and work, primiparity, and infant age.
b Model 2: Model 1 + child gender, low birth weight, and type of delivery.
c Model 3: Model 2 + BFH and health care services.
d Model 4: Model 3 + breastfeeding within the first hour.
e Model 5: Model 4 + intake of processed milk, tea, or water on the first day.
f Linear trend test.
DISCUSSION
This study is the first to investigate the determinants of the use of artificial nipples in a representative sample of children living in state capitals in Brazil. Importantly, the study classified the use of nipples into three outcomes (use of pacifiers, bottle feeding, or both), which allowed us to understand the use of these equipment, which can negatively interfere with breastfeeding and child health.
Maternal-related factors, including mother working outside the home and primiparity, were significantly correlated with the three outcomes, whereas infant-related factors, including low birth weight, cesarean delivery, and the male gender, were significantly correlated with only two outcomes (exclusive use of bottle feeding and use of artificial nipples). Child feeding on the first day after hospital discharge (through the consumption of baby formula, tea, or water) influenced the three outcomes but not the same components of each outcome, which suggests the existence of different motivations for the adoption of each feeding equipment. Birth in BFH and child follow-up in basic health care units were factors significantly correlated with the decreased use of artificial nipples.
Child age was significantly correlated with all the three outcomes. Previous studies indicated that child age may influence the use of artificial nipples. 1 , 9 , 18 , 19 , 23 , 24 Victora et al 23 and Aarts et al 1 observed that the use of pacifiers begins in early childhood and is a dynamic process until the age of three and four months. However, with advancing age, the use of this feeding equipment decreases. 1 , 9 , 23 Other authors indicated that bottle use is associated with water and tea intake and with the intake of processed milk, which increases the use of bottle feeding as child age progresses. 6 , 23 Considering the potential influence of this variable on the outcomes studied, infant age was considered an adjustment variable.
The male gender was significantly correlated with the use of artificial nipples but not with the isolated use of the two equipment. Previous studies on the use of pacifiers identified a correlation between its increased use and the male gender. 9 , 18 , 23 , 24 Another study reported a higher probability of interruption of breastfeeding in male infants. 20 In this respect, the authors suggest that mothers believe that male infants have higher nutritional requirements than female infants and they are therefore provided food supplements first. 11 Scott et al 15 indicated that the cultural construction of gender can influence this decision and can lead to the increased use of bottle feeding by male infants. However, till date, no study has indicated child gender as a determinant of the use of bottle feeding. The higher tendency of male infants to use artificial nipples than female infants warrants an explanation and should be further explored in qualitative studies. 15 , 18
Low birth weight was associated with the exclusive use of bottle feeding and artificial nipples. Weight gain is associated with child survival and is a condition that raises concerns among family members and health professionals. 3 This condition stimulates the early indication of food supplements, which are usually provided in bottle feeding, 6 , 23 thereby increasing its use among children with low birth weight. The associated use of bottle feeding and pacifiers has not been reported in previous studies. However, it is plausible to assume that these equipment will be used more frequently, considering the stressful conditions that the mother and infant are exposed to in hospital settings and during family adaptation. 3
The consumption of processed milk, tea, and water within the first day after hospital discharge was significantly correlated with the three outcomes. Previous studies have indicated that these liquids are usually provided by bottle feeding. 6 , 23 França et al 6 found that 21.3% and 46.9% infants used bottle feeding seven days and 30 days after birth, respectively, and tea and processed milk were the main ingredients offered at both instances. Bottle feeding is used as a vehicle for fluid delivery, whereas pacifiers are used to calm the infants, 16 , 18 and the latter function is also attributed to tea. 6 The symbolic and sociocultural role of calming the infant 16 , 18 , 23 corroborates the results of the present study. Although previous studies have indicated that the use of pacifiers increases the likelihood of using bottle feeding, 6 a causal relationship could not be established.
Primiparity was significantly correlated with the three outcomes, and it has been reported as a risk factor for early weaning and consequently for the use of artificial nipples. 18 , 19 , 24 Silva 17 reported that since child birth, mothers go through a learning process to understand their child’s language. Previous studies have found that parents are poorly oriented on how to manage child crying and behavior, 3 , 8 and when oriented, they feel more confident in comforting the child without resorting to artificial nipples. 8 Therefore, one can assume that less experienced mothers become more anxious when managing infant crying and behavior 16 , 19 and therefore resort to artificial nipples more frequently.
The factor mother working outside the home was significantly correlated with the three outcomes studied. Maternal work was expressed in categories of increased frequency of the use of nipples. Therefore, maternity leave was considered an intermediate condition with respect to the others. 10 , 12 , 13 Rea & Cukier 12 observed that mother working outside the home has become a primary reason for bottle feeding and weaning. Previous studies have shown that reconciling the roles of a worker and mother is increasingly common and that employee benefits alone are not sufficient for mothers to continue breastfeeding and not resort to artificial nipples. 12 , 13 In Brazil, women working in the formal sector are entitled to 120 days of maternity leave. However, their return to work is filled with anxiety and uncertainty related to children feeding and comfort in times of maternal absence. 12 Therefore, maternal work outside the home and the return to work after maternity leave are situations of great vulnerability that favor the interruption of exclusive breastfeeding and the consequent introduction of pacifiers and bottle feeding. 10
A significant correlation was observed between cesarean delivery and the use of artificial nipples. Victora et al 23 found that women who had cesarean delivery breastfed for a shorter period and resorted to pacifiers more frequently. Other authors found that women having cesarean deliveries showed a significant delay in the initiation of breastfeeding, which could lead to decreased frequency of breastfeeding and increased use of artificial nipples. 2
Breastfeeding in the first hour after birth was a protective factor and was strongly correlated with the three outcomes. In this sense, no previous studies that correlated the use of artificial nipples with breastfeeding in the first hour were found. However, some studies have correlated breastfeeding in the first hour with the increased prevalence of breastfeeding and the establishment of stronger bonds between the mother and child, 2 which are important factors involved in the decision to use artificial nipples.
BFH follow the “Ten Steps to Successful Breast-feeding”. 5 , 18 , 22 Step 9 establishes the nonuse of pacifiers and bottle feeding in hospitals for breastfed children. 5 In this study, child birth in hospitals without BFH accreditation was associated with the increased use of artificial nipples. Corroborating these findings, Coutinho et al 5 observed that the use of pacifiers and bottle feeding decreased after an BFH training program in two maternity wards. Moreover, Venancio et al 22 found a correlation between birth in BFH and the decreased use of pacifiers. Therefore, these studies highlight the need for effective support and guidance interventions during child follow-up in health care units and in the community. 5 , 22
Child follow-up is performed through primary health care services in public health care facilities, which comprise basic health care units and FHS units. In basic health care units, follow-up is performed by a pediatrician, whereas in FHS units, it is performed by a multidisciplinary team. Follow-up in public health care facilities, particularly in basic health care units, was considered a protective factor against the use of artificial nipples. The noninfluence of FHS in the results can be attributed to its low application in the Brazilian capitals (53.1% of the Brazilian territory in 2011). b
With regard to the surveys conducted during the vaccination campaigns, Venancio et al 22 reported that they are widely used in Brazil and can collect data in a short period, at a low cost. The adopted sample design and the high sample coverage (> 80.0%) in the second stage of the vaccination campaign in 2008 ensured sample representativeness. Furthermore, maternal educational levels were similar to those reported in the Live Births Information System in the same year. 21
One limitation of the present study is the noninclusion of subjects living in rural areas, and this aspect deserves attention in relation to the generalization of results. The other limitation is that the cross-sectional design of the study did not allow an assessment of the temporality of facts. However, the present study helped to identify situations that may serve as “markers” of the analyzed outcomes and to generate hypotheses for the development of longitudinal studies. 7
This is the first study to identify the factors associated with the exclusive use of bottle feeding and pacifiers and the use of artificial nipples (bottle feeding and pacifiers) in children aged under one year, in a representative sample of children. These results can be generalized to populations living in middle-income urban areas in countries such as Brazil and contribute to the planning of preventive actions in maternal and child health.
Footnotes
Ministério da Saúde. Prevalência de aleitamento materno nas capitais brasileiras e no Distrito Federal. Brasília (DF); 2001.
Ministério da Saúde. Secretária de Atenção a Saúde. Departamento de Atenção Básica. Números da Saúde da Família. Brasília (DF); 2012 [cited 2014 Jun 12]. Available from: http://dab.saude.gov.br/abnumeros.php
Article based on the master’s dissertation of Buccini GS, titled: “Determinantes do uso de chupeta e mamadeira em crianças menores de um ano nas Capitais Brasileiras e Distrito Federal”, presented to the Programa de Pós-Graduação em Nutrição em Saúde Pública of the Faculdade de Saúde Pública of the Universidade de São Paulo, in 2012.
The authors declare no conflict of interest.
REFERENCES
- 1.Aarts C, Hörnell A, Kylberg E, Hofvander Y, Gebre-Medhin M. Breastfeeding patterns in relation to thumb sucking and pacifier use. Pediatrics. 1999;104(4): doi: 10.1542/peds.104.4.e50. [DOI] [PubMed] [Google Scholar]
- 2.Araújo MFM, Schmitz BAS. Doze anos de evolução da iniciativa Hospital Amigo da Criança no Brasil. Rev Panam Salud Publica. 2007;22(2):91–99. doi: 10.1590/S1020-49892007000700003. [DOI] [PubMed] [Google Scholar]
- 3.Buccini GS, Sanches MTC, Nogueira-Martins MCF, Bonamigo AW. Acompanhamento de recém-nascidos de baixo peso pela atenção básica na perspectiva das equipes de Saúde da Família. Rev Bras Saude Matern Infant. 2011;11(3):239–247. doi: 10.1590/S1519-38292011000300004. [DOI] [Google Scholar]
- 4.Coutinho LMS, Scazufca M, Menezes PR. Métodos para estimar razão de prevalência em estudos de corte transversal. Rev Saude Publica. 2008;42(6):992–998. doi: 10.1590/S0034-89102008000600003. [DOI] [PubMed] [Google Scholar]
- 5.Coutinho SB, Lima MC, Ashworth A, Lira PIC. Impacto de treinamento baseado na Iniciativa Hospital Amigo da Criança sobre práticas relacionadas à amamentação no interior do Nordeste. J Pediatr (Rio J). 2005;81(6):471–477. doi: 10.2223/JPED.1422. [DOI] [PubMed] [Google Scholar]
- 6.França MCT, Giugliani ERJ, Oliveira LD, Weigert EML, Espirito Santo LC, Köhler CV, et al. Uso de mamadeira no primeiro mês de vida: determinantes e influência na técnica de amamentação. Rev Saude Publica. 2008;42(4):607–614. doi: 10.1590/S0034-89102008005000028. [DOI] [PubMed] [Google Scholar]
- 7.Habicht JP, Victora CG, Vaughan JP. Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. Int J Epidemiol. 1999;28(1):10–18. doi: 10.1093/ije/28.1.10. [DOI] [PubMed] [Google Scholar]
- 8.Kramer MS, Barr RG, Dagenais S, Yang H, Jones P, Ciofani L, et al. Pacifier use, early weaning, and cry/fuss behavior: a randomized controlled. JAMA. 2001;286(3):322–326. doi: 10.1001/jama.286.3.322. [DOI] [PubMed] [Google Scholar]
- 9.North K, Fleming P, Golding J, ALSPAC study team Pacifier use and morbidity in the first six months of life. Pediatrics. 1999;103(3): doi: 10.1542/peds.103.3.e34. [DOI] [PubMed] [Google Scholar]
- 10.Osis MJD, Duarte GA, Pádua KS, Hardy E, Sandoval LM, Bento SF. Aleitamento materno exclusivo entre trabalhadoras com creche no local de trabalho. Rev Saude Publica. 2004;38(2):172–179. doi: 10.1590/S0034-89102004000200004. [DOI] [PubMed] [Google Scholar]
- 11.Pérez-Escamilla R, Lutter C, Segall AM, Rivera A, Treviño-Siller S, Sanghvi T. Exclusive breast-feeding duration is associated with attitudinal, socieconomic and biocultural determinants in three Latin American countries. J Nutr. 1995;125(12):2972–2984. doi: 10.1093/jn/125.12.2972. [DOI] [PubMed] [Google Scholar]
- 12.Rea MF, Cukier R. Razões de desmame e de introdução da mamadeira: uma abordagem alternativa para seu estudo. Rev Saude Publica. 1988;22(3):184–191. doi: 10.1590/S0034-89101988000300004. [DOI] [PubMed] [Google Scholar]
- 13.Rea MF, Venancio SI, Batista LE, Santos RG, Greiner T. Possibilidades e limitações da amamentação entre mulheres trabalhadoras formais. Rev Saude Publica. 1997;31(2):149–156. doi: 10.1590/S0034-89101997000200008. [DOI] [PubMed] [Google Scholar]
- 14.Righard L. Are breastfeeding problems related to incorrect breastfeeding technique and the use of pacifier and bottles? Birth. 1998;25(1):40–44. doi: 10.1046/j.1523-536x.1998.00040.x. [DOI] [PubMed] [Google Scholar]
- 15.Scott JA, Aitkin I, Binns CW, Aroni RA. Factors associated with the duration of breastfeeding amongst women in Perth, Australia. Acta Paediatr. 1999;88(4):416–421. doi: 10.1111/j.1651-2227.1999.tb01133.x. [DOI] [PubMed] [Google Scholar]
- 16.Sertório SCM, Silva IA. As faces simbólica e utilitária da chupeta na visão das mães. Rev Saude Publica. 2005;39(2):156–162. doi: 10.1590/S0034-89102005000200003. [DOI] [PubMed] [Google Scholar]
- 17.Silva IA. Reflexões sobre a prática do aleitamento materno. Rev Esc Enferm USP. 1998;30(1):58–72. [PubMed] [Google Scholar]
- 18.Soares MEM, Giugliani ERJ, Braun ML, Salgado ACN, Oliveira AP, Aguiar PR. Uso de chupeta e sua relação com o desmame precoce em população de crianças nascidas em Hospital Amigo da Criança. J Pediatr (Rio J). 2003;79(4):309–316. doi: 10.1590/S0021-75572003000400008. [DOI] [PubMed] [Google Scholar]
- 19.Tomasi E, Victora CG, Olinto MTA. Padrões e determinantes do uso de chupeta em crianças. J Pediatr (Rio J). 1994;70(3):167–171. doi: 10.2223/JPED.766. [DOI] [PubMed] [Google Scholar]
- 20.Venancio SI, Escuder MML, Kitoko P, Rea MF, Monteiro CA. Freqüência e determinantes do aleitamento materno em municípios do Estado de São Paulo. Rev Saude Publica. 2002;36(3):313–318. doi: 10.1590/S0034-89102002000300009. [DOI] [PubMed] [Google Scholar]
- 21.Venancio SI, Escuder MML, Saldiva SRDM, Giugliani ERJ. A prática do aleitamento materno nas capitais brasileiras e Distrito Federal: situação atual e avanços. J Pediatr (Rio J). 2010;86(4):317–324. doi: 10.1590/S0021-75572010000400012. [DOI] [Google Scholar]
- 22.Venancio SI, Saldiva SRDM, Escuder MML, Giugliani ERJ. The Baby-Friendly Hospital Initiative shows positive effects on breastfeeding indicators in Brazil. J Epidemiol Community Health. 2012;66(10):914–918. doi: 10.1136/jech-2011-200332.. [DOI] [PubMed] [Google Scholar]
- 23.Victora CG, Behague DP, Barros FC, Olinto MTA, Weiderpass E. Pacifier use and short breastfeeding duration: cause, consequence, or coincidence? Pediatrics. 1997;99(3):445–453. doi: 10.1542/peds.99.3.445. [DOI] [PubMed] [Google Scholar]
- 24.Vogel AM, Hutchison BL, Mitchell EA. The impact of pacifier use on breastfeeding: a prospective cohort study. J Paediatr Child Health. 2001;37(1):58–63. doi: 10.1046/j.1440-1754.2001.00581.x. [DOI] [PubMed] [Google Scholar]