Abstract
The Ministry of Health and Family Welfare and its public health institutes are collaborating with Asia Australia Mental Health on an innovative community mental health development project designed to enhance initiatives under the District Mental Health Program and increase accessibility of essential community mental health services. The project is an exciting opportunity to create positive change in meeting the challenges of community mental health care in India. It recognizes that no one single model of care can be applied to all the community in the country and that locally appropriate models working in close partnership with local communities is required. Targeted and skill-based training programs are useful to build local leadership capacity in implementing quality and culturally appropriate community mental health services.
Keywords: Community, mental health, partnerships
INTRODUCTION
The community mental health development in India is facing numerous challenges. The World Health Survey[1] indicated that in India the prevalence of psychosis was between 0.7% and 3.6%, while the treatment rates were only 36-85%. In addition to the high mental health burden and large treatment gap of mental disorders there are significant limitations in the availability and integration of mental health services in the public health sector. Hence, the Ministry of Health and Family Welfare (MoHFW) India and its public health institutes are collaborating to develop local solutions to build and strengthen the national community mental health system. There is an urgent need for developing appropriate community mental health models in India that can be replicated and scaled up to increase access to appropriate care for people with mental illness.
DISTRICT MENTAL HEALTH PROGRAM
The District Mental Health Program (DMHP) is a community-based mental health service delivery program initiated in 1996 under the National Mental Health Plan and were now active in 123 of the 652 districts of India.[2,3] The program aspires to increase access to comprehensive mental health care service by developing partnerships between the district mental health team, the primary health care (PHC) teams, community-based organizations, nongovernmental organizations (NGOs), service users, family groups and various government departments.[4]
In the beginning, the project focused on early diagnosis and treatment, training of PHC staff, and information, education and communication activities with the core clinical team. Mental health promotional activities such as life skills education and counseling in schools, counseling services in colleges, workplace stress management, suicide prevention services, as well as a managerial team for implementing various DMHP activities have been added. The major achievements of the program have been the development of community mental health services in the most underserved areas. To decentralize mental health care in the community using the public health infrastructure and other resources,[5] mental health training, awareness and services are provided in collaboration with various community-based partners.
In terms of challenges, the training needs for PHC staff are enormous due to the large numbers of PHC workers in India. A shortage of qualified mental health human resources, as well as little involvement of other primary care health workers in the mental health services has meant difficulty in recruiting the district mental health teams.[2] Lack of coordination between Health and Medical Education Departments has resulted in conflict in program implementation. Stigmas attached to mental illness remain widely prevalent, and still pose formidable barriers between the mentally ill and community mental health services.[6] Mental health remains a comparatively neglected area, given the lowest priority in social and development planning. There is still much to be done to integrate mental health into the mainstream public and general health.[7]
THE COMMUNITY MENTAL HEALTH DEVELOPMENT PROJECT
As a strategy to build the DMHP and increase accessibility of essential community mental health services, MoHFW and its public health institutes have collaborated with Asia Australia Mental Health (AAMH) on innovative community mental health development project. The project began in 2011 and aims to develop locally sustainable best practice community mental health models to inform policy and practice at local district, state and national level. Four pilot sites were identified, and project activities are focused on developing local capacity to prevent, treat and rehabilitate people with mental disorders through integrating mental health care into public health. The project collaborates with international partners under a formal agreement with technical expertise provided by The University of Melbourne (AAMH). A bilateral Community Mental Health Advisory Committee chaired by the Director General of Health Services (DGHS), MoHFW provides the oversight of the overall project.
Development of the project
Four different pilot sites with a capacity to provide leadership for a national program and to develop best practice models were selected. These reflect the diverse conditions and needs across India including models for urban setting (Chandigarh), rural tribal setting (Gumla), mixed urban setting (Ramanathapuram) and low-health resource settings (Panchmahal).
Each of the four sites is linked to local tertiary care mental health institute for technical and managerial support. The pilot projects involved relevant public sectors and community stakeholders (such as state departments, health institutes, PHC providers, community agencies and NGO's) in the development and implementation of the program.
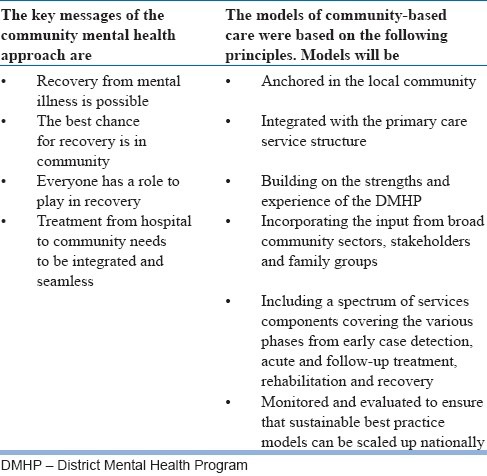
To more effectively measure and communicate project aims, processes, and potential outcomes, the advisory committee worked with the project team to establish common procedures for each site [Table 1] and key principles for developing best practice community mental health models [Table 2].
Table 1.
Common methodology for model development
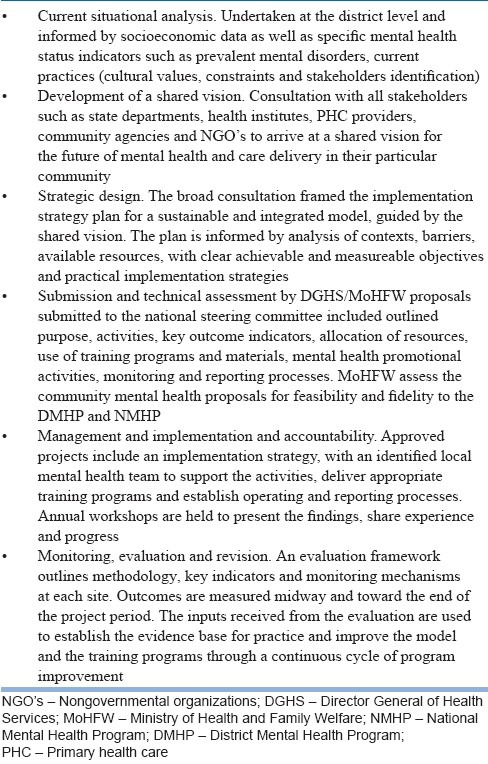
Table 2.
Key principles for developing community mental health model of care
Pilot project sites and partners
Gumla district, Ranchi Institute of Neuro Psychiatry and Allied Sciences (RINPAS) (Jharkhand - East region)
The RINPAS is situated in the tribal heartland of Jharkhand state embracing Santhal Pargana and Chotanagpur. District Gumla, almost 90 km away from capital city Ranchi, comprises of about 10.25 lakhs population. It is estimated that more than 75% of the population belonging to a tribal community, with unique cultural, religious, and social practices. As well as the district hospital, there is a district mental health center (DMHP with psychiatrist, clinical psychologist, psychiatrist social worker, and psychiatric nurse), 13 PHC centers, 11 community healthcare centers and 242 health sub centers
Some of the main areas of concern identified by the mental health services at the start of this project included a failure to understand the indigenous social and emotional context of the presenting problems, a high rate of unaddressed mental health needs which affect the physical health and overall socioeconomic development, as well as pervasive and harmful myths and misconceptions in the community surrounding mental illness. The project planned to cover two blocks with the goal of delivering proper treatment, follow-up and sociovocational rehabilitation that will benefit tribal people affected with mental illness and their caregivers
The planned approach aims to engage the local stakeholders (panchayat leaders, health workers, voluntary workers, faith healers, general practitioners) in a culturally appropriate way, encourage joint planning, and mobilize community mental health resources. The project aims to increase culturally appropriate mental health promotion, improve convergence with other health and administrative sectors and increase numbers of people identifying with the tribal backgrounds employed in health and education centers and training in mental health
Chandigarh district, Chandigarh Government Medical College (North region)
Chandigarh has an area of 1142 km and a population of 1.05 million, including an estimated 90% urban residents. As a joint capital of both Punjab and Haryana states, Chandigarh has 1 district hospital, 2 community health centers, 1 poly clinic, 30 civil dispensaries, 20 AYUSH dispensaries, and 17 sub centers
In the Chandigarh district, it has been identified that existing DMHP model may not have sustainable sources after funding after the 5 years current central government arrangement and the implementation of the DMHP has been in the nature of a parallel program rather than integrated, especially at the grassroots levels
The Department of Psychiatry, Government Medical College and Hospital has been working into the community for the last 14 years, providing community mental health services through community camps, community out-reach clinics in the periphery of Chandigarh, half way home, crisis intervention team, suicide prevention helpline and providing technical assistance to self-help groups
Through this work, it has been seen that there are insufficient social and vocational rehabilitation services for the persons with chronic and severe forms of mental disorders and one of the main goals of this pilot project is to explore initiatives for capacity building and empowerment of consumers and caregivers
As an overarching principle, this particular pilot site identified the importance of including prevention and positive mental health promotion into the mental health approach
Ramanathapuram district, Madurai Medical College (Tamil Nadu - South region)
Ramanathapuram district is an administrative district of Tamil Nadu state in Southern India with a population of 1,337,560. There are 45 PHCs, seven Taluk hospitals and one district headquarters hospital in Ramnad district Tamil Nadu. This district also has 56 private hospitals, including the three Siddha, Homeopathy and Unanni Medicines Hospitals
The DMHP has been in operation in Ramnad district since, 2001. At this time, resources were put into training public health staff, but there have been no ongoing mental health education for the 300 medical doctors and 700 health workers working in the district
For this region, the Ramanathapuram DMHP is supported by the M. S. Chellamuthu Trust and Research Foundation, Madurai. This leading NGO has a wide range of activities, including treatment, psycho-social rehabilitation, vocational training and placements aiming to assist people with mental health problems to recover and reintegrate with the mainstream community through this work, facilities and infrastructure have been identified as inadequate for comprehensive care and universal coverage, particularly in rural areas. Travelling costs for treatment can be a barrier or lead to incomplete treatment. Myths and misconception about mental illness also contribute to poor access of existing services, including the lack awareness about the availability of, or the effectiveness of treatment
The Ramanathapuram district project highlighted the potential for services creating shared responsibility with village panchayats and primary health center teams created a better link for specialist mental health services and community services. The project also identified the capacity to actively engage religious persons, native healers and spiritual guides who can assist with providing support for people experiencing mental health problems and bring a wider expertise in mental health advocacy work
There is another innovative experiment in creating a teleconference facility by which we are linking the block level hospitals with district headquarters hospital and thereby we are increasing the accessibility, affordability and decreasing the stigma to a greater extend.
Panchmahal district, Ahmedabad Mental Hospital (Gujarat - West region)
Gujarat, with a population of 60,383,638 (census-2011) has a district hospital, 13 community health centers, 63 PHC centers, 400 sub centers, 21 Ayurveda centers, and 9 homeopathic centers
The DMHP has been extended to eight districts of Gujarat, linking district general/civil hospitals to adjoining hospitals for mental health or Department of Psychiatry of Medical Colleges. The Department of Health and Family Welfare, Government of Gujarat commissioned work which led to the 2004 mission report titled priorities for mental health sector development in Gujarat. This report provided a broad canvas of strategies which need to be pursued to address issues facing this sector in the context of Gujarat in 12 strategic directions including: Resource mobilization and allocation, strengthening the ethics of care, addressing stigma, and integration of mental health with health and other sectors[8]
Department of Health and Family Welfare, Government of Gujarat also released a 12th 5 year plan 2012-2017, which includes the commitment to strengthening the Mental Health Program to provide better medical services to the mentally ill patients, protect their right and rehabilitate them in the society
In line with these state strategies, the hospital for mental health, Ahmedabad focused the community project on utilizing available human resources at the village/taluka level for case identification and counseling and well-established referral linkages with both public and private agencies. The project sought to build on foundations of existing sources of rapport, influence and capacity to mobilize the community at the village level. Including these stakeholders and expertise in mainstream mental health delivery will help reduce the stigma as well as address crucial gaps in MH services. The project aims to increase mental health awareness, sensitization and use of local mental health services and its impact on the explanatory models used to understand mental illness.
Building human resource capacity
Appropriate and trained human resources are critical to developing collaborative arrangements for effective community based mental health services. A skilled workforce has been recognized as key to strong community participation, linkages with the voluntary sector and civil society initiatives, with academic institutions from inter-disciplinary backgrounds.[2]
The National Institute of Health and Family Welfare (NIHFW), DGHS, MoHFW and AAMH have jointly designed structured training for community mental health workforce. The training explores methods to develop human resources for community-based services, and importantly to develop a broad understanding of the role of the mental health professional. It incorporates the core principles of recovery-oriented practice including: supporting personal recovery and promoting well-being; delivering services informed by evidence and consistent with the social model of health; proactive and purposeful engagement to build trusting relationships. This ensures practice is sensitive to the needs of families, friends and careers; and working in partnership with key stakeholders.
Innovative training programs thus not only need to build on existing training resources but also develop new skill sets relevant to the principles and approach of the project. An example of the training delivered is the 5 days training program delivered in November 2013, which included 20 participants from the 4 pilot sites. Participants included medical officers and program managers who were responsible for the implementation of community mental health projects. The training started with topics that would set the context, by reflecting on global trends and best practice in Asia Pacific. The interactive workshops sought to broaden the perspectives of key stakeholders on the burden of mental illness in India and factors influencing progression of mental illness and rates of recovery, as well as efforts to respond to the challenges of mental illness and the mental health treatment gap.
An essential strategy was to develop a shared understanding and consistent approach to recovery - oriented and community-based mental health service delivery in India. Expertise on management strategies for mental illnesses complemented participants’ discussions and workshops on a multidisciplinary approach and local considerations. Material included establishment of rehabilitation services within communities as well as the roles of families, self-help groups, caregivers associations, and other specialized NGO's. The philosophy of recovery was also seen to positively influence stronger methods for measuring success. The training examined existing guidelines for monitoring and evaluation for each site with discussion on various aspects such as project indicators, data collection, data compilation, and report writing.
The training sessions also examined effective management of common mental disorders including treatment seeking behaviors and treatment compliance, common childhood and adolescent psychiatric problems, addiction, abuses of addictive substances, and aged mental health problems. The workshops were centered on clinicians creating positive futures for people suffering from mental illness. Expertise shared at the training incorporated information, education and communication strategies for mental health promotion.
DISCUSSION
With an enormous mental health burden and inadequate treatment access in India, innovative solutions in community mental health care based on local conditions are urgently needed. Local community resources are increasingly being recognized as a valuable part of the health system but are often neglected in the medical model of care. Solutions to address the high-burden need to acknowledge that culture and traditional care, family and community structures are important elements in mental health care. Further cultural aspects of the ways mental illnesses and disorders are viewed, presented and treated must be considered when applying an intervention model that is acceptable to the local community. As one model of care cannot be applied to all persons or for all parts of India the project thus has developed different models and trialed across four pilot sites, to help increase access to appropriate community mental health care.
India today has a framework for mental health care in the public, private and voluntary sectors[9] and the challenges for the future will be improving the interfaces between mental health services and the wider community. Thus, building partnerships with the local communities and partners like families and careers or traditional healers are not only essential for a comprehensive community mental health system but it can have important benefits to patients. Developing these partnerships, which is promoted in the project, needs to be based upon mutual trust, respect, good communication, accountability and collaborative work. Apart from the input of people with mental disorders and their families, care plans need to consider all relevant stakeholders, and through consultation employ their abilities and resources efficiently.
Just relying on increasing mental health hospitals or specialists workforce, though important to a certain extent in meeting the needs of those with acute and serious mental illness, is neither sustainable nor sufficient. If qualified mental health personnel are insufficient to meet the high demands, then short-term skill-based training for general and primary health staff can be conducted. They can be linked to specialist professionals either in the public or private sector for specialist referral services. Training the PHC team can be streamlined with standard training material and detailed operational guidelines. Integration of primary care mental health training with the district training program will avoid any potential conflict with training for other programs. These “task-shifting” training that incorporate recovery and community oriented approaches are being implemented within the project sites.
Challenges in expanding the DMHP to all districts in India remained and one strategic approach would be to develop regional training resource centers such as through the local tertiary care mental health institutes to support the program. It is critical to examine the role of the existing mental health professionals and administrators in facilitating such the change from a hospital-based service system to a community-oriented service. Through effective and unique training programs, clinicians can be better equipped to apply leadership skills and qualities to support better patient recovery outcomes. Further the integration of mental health into socioeconomic and health policies requires sensitization of relevant administrators and staff at various sectors including social welfare, health, education, employment, and other development agencies.
CONCLUSION
The community mental health project is an innovative and exciting opportunity to create positive change in meeting the challenges of community mental health care in India. It recognizes that no one single model of care can be applied all communities in the country and that locally appropriate models working in close partnership with local communities is required. Targeted and skill-based training programs are useful to build local leadership capacity in implementing quality and culturally appropriate community mental health services.
ACKNOWLEDGMENTS
The authors would like to acknowledge the following individuals/organizations for their contribution to this report: MoHFW (Dr. Prakash, Dr. Alok Mathur); NIHFW (Dr. M. Bhattacharya, Dr. T. Bir, Dr. Sanjay Gupta, Dr. J. P. Shivdasani, Ashwani Singh, G. S. Karol).
Footnotes
Source of Support: The activities of Asia-Australia Mental Health for this project were supported by the Australian Government Public Sector Linkages Program
Conflict of Interest: None declared
REFERENCES
- 1.Mumbai, New Delhi: WHO India, WR Office; 2006. World Health Survey, India, 2003. Health System Performance Assessment, International Institute for Population Sciences (IIPS) [Google Scholar]
- 2.Ministry of Health and Family Welfare. XIIth Plan District Mental Health Programme. MH Policy Wordpress: Ministry of Health and Family Welfare. 2012. [Last accessed on 2014 Jan 23]. Available from: http://www.mhpolicy.files.wordpress.com/2012/07/final-dmhp-design-xii-plan2.pdf .
- 3.Murthy RS. Mental health initiatives in India (1947-2010) Natl Med J India. 2011;24:98–107. [PubMed] [Google Scholar]
- 4.Agarwal SP, Goel DS, Ichhpujani RL, Salhan RN, Shrivastava S. New Delhi: Directorate General of Health Services Ministry of Health and Family Welfare; 2004. Mental Health: An Indian Perspective, 1946-2003. [Google Scholar]
- 5.Waraich BK, Raj L, Chavan BS, Badhan R, Panda S. Decentralisation of mental health services under DMHP. Indian J Psychiatry. 2003;45:161–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Shidhaye R, Kermode M. Stigma and discrimination as a barrier to mental health service utilization in India. Int Health. 2013;5:6–8. doi: 10.1093/inthealth/ihs011. [DOI] [PubMed] [Google Scholar]
- 7.Isaac M. National Mental Health Programme: Time for are. appraisal. In: Kulhara P, Avasthi A, Thirunavukarasu M, editors. Themes and Issues in Contemporary Indian Psychiatry. New Delhi: Indian Psychiatric Society; 2011. pp. 2–26. [Google Scholar]
- 8.Bhat R. Managing Mental Health Sector in Gujarat: An Overview of Strategic Priorities. Vikalpa (Indian Institute of Management) 2004;29:1–12. [Google Scholar]
- 9.Chavan BS, Nitin G, Sidana A, Arun P, Jadhav S. New Delhi: Jaypee Brothers Medical Publishers; 2012. Community Mental Health in India. [Google Scholar]


