Abstract
Purpose
To determine the frequency of complement factor H (Y402H) and age related macular degeneration susceptibility gene 2 (A69S) single nucleotide polymorphisms in patients with age-related macular degeneration (AMD) and in matched non-AMD controls in an Iranian population.
Methods
Seventy patients with AMD and 86 age- and sex-matched controls were recruited and examined. Peripheral blood sample was obtained from all subjects for DNA extraction and direct sequencing of Y402H and A69S genes. Odds ratios (ORs) with 95% confidence intervals (CIs) for the association of Y402H and A69S polymorphisms with AMD were determined.
Results
The frequencies of both homozygous and heterozygous genotypes were significantly higher in cases than controls for both Y402H and A69S polymorphisms. In comparison to the wild genotypes, OR for AMD associated with Y402H and A69S polymorphisms were 1.9 (95% CI, 1.1-3.2) and 2.2 (95%CI, 1.6-3.1), respectively. Joint risk analysis considering both genes revealed a higher risk of AMD when polymorphisms were present for both genes.
Conclusion
Y402H and A69S polymorphisms were strongly associated with AMD in this Iranian population.
Keywords: Age-related Macular Degeneration, Gene, Complement Factor Polymorphism
INTRODUCTION
Age-related macular degeneration (AMD) is the leading cause of irreversible blindness in the elderly population worldwide.1,2 It is a late-onset, chronic and progressive degeneration of the retinal pigment epithelium (RPE) and photoreceptors at the macula. Early AMD is characterized by pigmentary alterations at the level of RPE and accumulation of cellular debris called drusen between RPE and Bruch’s membrane. Visual function is usually not disturbed at this stage. As the disease progresses, vision declines due to either loss of the RPE and atrophy of the overlying retina, or loss of RPE/Bruch’s membrane integrity and development of subretinal neovascularization.3 The latter usually presents with accelerated visual loss due to subretinal hemorrhage, subretinal and intraretinal fluid accumulation, and fibrosis and degeneration of photoreceptors. Anti-vascular endothelial growth factor (VEGF) agents have been able to slow down or abort this process.
AMD is a multifactorial disease. Age related oxidative stress in a genetically and environmentally predisposed person is believed to play the main role in its pathogenesis.1,4 Of these, the contribution of genetic factors in the development and progression of AMD has become clearer in recent years.5-7 Multiple family-based genome-wide and candidate region linkage studies have found two major linkage regions on chromosomes 1q31 and 10q26 as primary genetic loci associated with an increased risk of AMD.5-10 A single nucleotide polymorphism (SNP) in exon 9 on the complement factor H (CFH) gene on chromosome 1q31 resulting in a T to C change at the nucleotide position 1277 of the CFH gene was associated with a 2.1- to 7.4-fold increase in the risk of AMD in different populations worldwide.5-7 This SNP causes tyrosine to histidine substitution of the amino acid 402 (encoded by the allele C of rs1961170 SNP) of CFH. The second locus implicated to contribute to the risk of AMD is located on chromosome 10q26 and is called age related macular degeneration susceptibility gene 2 (ARMS2). A69S polymorphism in LOC387715 locus (rs10490924 variant) of this gene has been found to be associated with AMD.11
The functional consequence of the Y402H variant is attributed to its position within the binding sites of CFH for heparin and C-reactive protein (CRP). Heparin and CRP normally augment CFH’s affinity to the complement protein C3b increasing its ability to down regulate complement activity. The Y402H variant alters the ability of CFH to suppress complement resulting in increased local inflammation.7 The role of CFH in the pathogenesis of AMD has been supported by the observation of rich CFH transcripts in the RPE and choroid, and strong CFH immunofluorescence and staining around choroidal blood vessels and in drusen.12 ARMS2 gene is in close linkage disequilibrium with its closely located high temperature requirement-1 (HTRA-1) gene. HTRA-1 that encodes a serine protease associated with cellular stress9 is expressed in the retina and fibroblasts with aging and in drusen.13 However, the exact mechanism of action of the LOC387715 gene product is not fully elucidated.
Associations between these genetic variants and the risk of AMD are not universal and uniform. For example, Y402H SNP is less common in the Chinese and absent in Japanese populations.14,15 A69S SNP at LOC387715 locus is highly associated with the risk of AMD in Caucasians but the association in other ethnicities has been reported to be moderate.16,17 There is no data from the Iranian population in this regard. AMD is a major cause of irreversible visual loss in the general population in Iran.18 As the population ages, the incidence and prevalence of AMD is expected to increase progressively. Determining high risk genotypes associated with AMD in Iranian population, and the significance of the risk associated with them may prove valuable in early detection, treatment, and risk modification.
Herein, we examine the frequency of two major genetic variations associated with the risk of AMD (CFH Y402H and LOC387715 A69S SNPs) in an Iranian population. This is the first report on the genetic risk factors of AMD in Iranians.
METHODS
This prospective case-control study was conducted on 70 patients with AMD in at least one eye and 86 non-AMD age- and sex-matched controls from non-blood-relatives of the AMD group attending the retina clinic at Rassoul Akram Hospital and two private retina clinics in Tehran, Iran. The participants were Iranian with no known familial relation with other ethnicities such as African, Indian, East Asian, or Caucasian. The study protocol was approved by the ethics committee of the Eye Research Center at Rassoul Akram Hospital and adhered to the tenets of the Declaration of Helsinki for research involving human subjects. Informed consent was obtained from all participants.
The participants were recruited by retina specialists experienced in the diagnosis of retinal degeneration and underwent a full ophthalmologic examination including assessment of best corrected visual acuity (BCVA) using a modified Snellen chart, slit lamp biomicroscopy, intraocular pressure measurement, and dilated fundus examination using 90 and 20 diopter noncontact lenses. The diagnosis of AMD was confirmed in all participants in the AMD group with fluorescein angiography (FA) and optical coherence tomography (OCT), with or without indocyanine green angiography (ICG). Inclusion criteria for the AMD group consisted of age ≥ 55 years and the presence of multiple soft drusen, pigment epithelial detachment, subretinal choroidal neovascular membrane, disciform scar, or geographic atrophy. Patients were subclassified based on the features in the worse eye to early AMD (presence of drusen and pigmentary changes) and advanced AMD (choroidal neovascularization, disciform scar, and geographic atrophy). Patients with other conditions known to cause geographic atrophy or choroidal neovascularization including high myopia, choroidal rupture, ocular histoplasmosis syndrome, and angioid streaks were excluded. Controls were selected from individuals aged ≥ 65 years without AMD pathologies. Higher inclusion age was considered for the control group to minimize the possibility of late development of AMD in controls.
Peripheral blood samples were collected in the clinic by trained personnel. Genomic DNA was extracted from the blood samples by a commercially available kit (FlexiGene DNA kit, Qiagen, Hilden, Germany) within 24 hours of collection. Polymorphic Y402H sites on the CFH gene and LOC 387715 A69S mutations (rs10490924 variant) on the ARMS2 gene were determined by polymerase chain reaction (PCR) fragment length polymorphism technique. The following primers were designed and checked for specificity with the National Center for Biotechnology Information (NCBI) primer BLAST tool. Forward 5'-TTTTTGGATGTTTATGCAATCTT-3' and reverse 5' CATTTTGCCACAATTAATATAGATGAG-3' primer pair was designed for amplification of T>C SNP at 1277 nucleotide located in exon 9 of the CFH gene producing a PCR product of 389 bp. A69S mutations were identified by the primers 5'-GTGGAGAAGGAGCCAGTGAC-3' (forward) and 5'-CAGTGTCAGGTGGTGCTGAG-3' (reverse) amplifying a PCR product of 158 bp. PCR amplicons were separated on 1.5% agarose gel containing 0.5% etidium bromide by electrophoresis and visualized by UV imaging system (BioRad, Germany) (Figure 1). Subsequently, the amplicons were subjected to direct gene sequencing (ABI 3730XL sequencer, Macrogen, Seoul, South Korea) of the mutated allele. PCR analysis and gene sequencing were performed by investigators who were unaware of the ocular condition of the participants.
Figure 1.
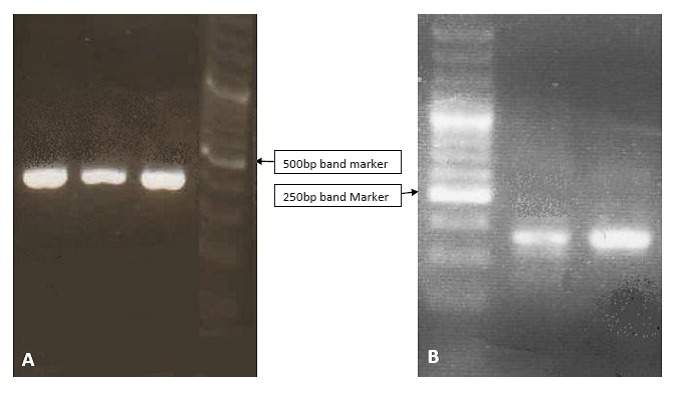
Gel electrophoresis demonstrates bands corresponding to exon 9 of the complement factor H Y402H gene (A) and the amplified regions of A69S mutation of age related macular degeneration susceptibility 2 gene (B).
Data was analyzed using SPSS software (Version 15, SPSS Inc. Chicago, IL, USA). Numerical data were compared by Student’s t-test. The allele and genotype frequencies of cases and control subjects were compared using Chi square test. Odds ratios (ORs) with 95% CIs for AMD associated with the Y402H and A69S polymorphisms were determined. Statistical significance was set at P≤0.05.
RESULTS
The AMD group consisted of 31 female (44.3%) and 39 male (55.7%) subjects with mean age of 70.8±8.8 years. Non-AMD individuals included 49 female (57%) and 37 male (43%) subjects with mean age of 71.6±5.7 years. Age and gender distribution was comparable between the two study groups (P=0.5 and P=0.8, respectively). Seventeen cases (24.3%) and 28 controls (32.6%) had history of systemic hypertension (P=0.3). Six cases (8.5%) and 25 controls (29.1%) had history of diabetes mellitus (P<0.002). There was no difference between the study groups in term of the frequency of smoking (18.5% in cases and 16.2% in controls, P=0.5). Fifty-five patients had advanced AMD (i.e. geographic atrophy, choroidal neovascularization or disciform scar) in the worse eye, while 10 patients had early AMD.
The genotype and allele frequency of Y402H and A69S mutations in cases and controls are presented in Table 1. The Y402H variant was more frequently detected in cases as compared to controls (57.9% vs 38.4%, P=0.002) with an OR of 1.9 (95% CI, 1.1- 3.2) for association with AMD. There was a significant difference in CFH genotype between AMD patients (TT 18.6%, TC 47.1%, and CC 34.3%) and non-AMD controls (TT 40.7%, TC 41.9%, and CC 17.4%, P=0.005). The presence of heterozygote Y402H gene (OR 1.7; 95% CI, 1.042-2.9) as well as homozygous genotype at Y402H (OR 2.2; 95% CI, 1.3-3.8) was significantly associated with an increased risk of AMD.
Table 1.
Allele and genotype frequency of complement H factor variant Y402H and ARMS2 variant A69S in age related macular degeneration (AMD) cases and non-AMD controls
| CFH Y402H | |||||||
|---|---|---|---|---|---|---|---|
| Allele | Genotype | ||||||
| Frequency | P value | Frequency | P value | ||||
| Case | control | Case | control | ||||
| T | 59 (42.1%) | 106 (61.6%) | 0.002 | TT | 13 (18.6%) | 35 (40.7%) | 0.005 |
| C | 81 (57.9%) | 66 (38.4%) | TC | 33 (47.1%) | 36 (41.9%) | ||
| CC | 24 (34.3%) | 15 (17.4%) | |||||
| LOC387715 A69S | |||||||
| Allele | Genotype | ||||||
| Frequency | P value | Frequency | P value | ||||
| Case | control | Case | control | ||||
| G | 58 (41.4%) | 142 (82.6%) | 0.002 | GG | 17 (24.3%) | 58 (67.4%) | <0.0001 |
| T | 82 (58.6%) | 30 (17.4%) | GT | 24 (34.3%) | 26 (30.3%) | ||
| TT | 29 (41.4%) | 2 (2.3%) | |||||
The odds ratio of having Y402H variant did not differ significantly in patients with early and advanced stages of the disease. In patients with advanced AMD the OR for the Y402H allele was 2.3 (95% CI, 1.2-4.3) as compared to normal controls. Individuals with heterozygous (TC) and homozygous (CC) genotype had an OR of 2.1 (95% CI, 1.1-4.01) and 2.6 (95% CI, 1.3-5.1) for advanced AMD. Based on multivariate analysis, the association between Y402H gene and AMD was still significant after considering other systemic conditions including systemic hypertension, family history of AMD and diabetes (P=0.002).
A69S SNP was observed in 58.6% of cases and in 17.4% of controls (P=0.002) with a 2.2 fold increase in the risk of AMD (95% CI, 1.6-3.1). There was a significant increase in the risk of AMD with heterozygous and homozygous genotypes for the mutation such that individuals with heterozygous mutations had an OR of 1.8 (95%CI, 1.2-2.9) and those with homozygous mutation had an OR of 18.9 (95%CI, 3.1-46) for AMD. The frequency of homozygote genotype for A69S mutation in patients with advanced AMD (45.5%) was not significantly different from those with early AMD (40%, P=0.2). Multivariate analysis considering systemic conditions such as hypertension, family history of AMD and diabetes showed that the association between A69S gene and AMD was significant (P=0.002). Joint risk analysis considering both mutations showed that individuals heterozygote for the CFH gene (Y402H) and homozygote for ARMS2 gene (A69S) had a 7.3 fold increased odds of association with AMD phenotype (Table 2).
Table 2.
Joint risk analysis for CFH Y402H and LOC387715 A69S genes for association with age related macular degeneration
| Number of risk alleles | Case (No.) | Control (No.) | P value | OR | 95% CI | |
|---|---|---|---|---|---|---|
| CFH -/- LOC -/- | 0 | 4 | 24 | <0.001 | 0.2 | 0.07-0.5 |
| CFH-/- LOC -/+ | 1 | 2 | 11 | 0.03 | 0.2 | 0.05-0.9 |
| CFH-/- LOC +/+ | 2 | 7 | 0 | 0.003 | 0.9 | 0.83-0.97 |
| CFH-/+ LOC -/- | 1 | 5 | 28 | <0.001 | 0.2 | 0.08-0.5 |
| CFH-/+ LOC -/+ | 2 | 16 | 6 | 0.006 | 3.2 | 1.3-7.9 |
| CFH-/+ LOC+/+ | 3 | 12 | 2 | 0.002 | 7.3 | 1.7-31.8 |
| CFH+/+ LOC -/- | 2 | 8 | 6 | 0.4 | 1.6 | 0.5-4.4 |
| CFH+/+ LOC -/+ | 3 | 6 | 9 | 0.7 | 0.8 | 0.2-3.1 |
| CFH+/+ LOC +/+ | 4 | 10 | 0 | <0.001 | 2.4 | 2.00-2.9 |
CFH, complement factor H
DISCUSSION
AMD is becoming a significant worldwide health problem. CFH Y402H and LOC387715 A69S mutations are two major SNPs linked to the increased risk of AMD in various populations. In the current study, we found that the Y402H variant of CFH gene is present in 57.9% of AMD patients but in 38.4% of non-AMD individuals in an Iranian population. Also, A69S SNP was detected in 58.6% of AMD patients but in 17.4% of non-AMD individuals in the same population. Y402H and A60S SNPs were associated with a 1.9- and 2.2-fold increase in the risk of AMD, respectively. The presence of both alleles in a patient conferred much higher risk for AMD.
The strong association of Y402H and A69S genes with the risk of AMD in our study is in agreement with similar studies on other ethnic populations. The Y402H variant has been associated with AMD in other studies including Caucasians, Asians, Turkish, and Israeli populations.5-7,14,17,19,20 In a recent study on a Turkish population, the frequency of Y402H and A69S alleles was significantly higher in AMD patients as compared to controls with an OR of 2.12 and 3 for Y402H and A69S alleles, respectively.17 In Israel, Y402H allele was associated with an increased risk of neovascular AMD with an OR of 1.9.19 On the other hand, in Koreans, Y402H polymorphism was only marginally associated with the risk of AMD.21 In a systematic review of studies on different populations, each CFH Y402H allele was associated with AMD with an average OR of 2.5.22 LOC387715 A69S mutations were also associated with a 7.6 fold increase in the risk of AMD.23,24 Seitsonen et al20 showed an increased risk of AMD in a Finnish population bearing both Y402H and A69S genes and suggested that a common causative pathway may exist for these genes in the pathogenesis of AMD. Joint risk analysis in our population confirms an increased risk of AMD in individuals having both Y402H and A69S genes.
The Y402H variant of CFH and the A69S variant of ARMS2 are linked with AMD progression rate and treatment response.25,26 Therefore, determining the presence of these genes may affect clinical decision making. A patient harboring CFH Y402H SNP may need more frequent follow up and lower threshold for treatment. In addition, it is proposed that individual responses to vitamins and micronutrient supplementation as suggested by the Age Related Disease Study (AREDS) may be related to CHF phenotype.27 Although an interaction has been observed between antioxidant and zinc supplementation and the CHF Y402 genotype, such interactions were not detected between supplementation and A69S SNP.27 Considering the frequency of AMD risk alleles in our population and their associations with a higher risk of AMD, we now have evidence to support that more aggressive screening and management is required in patients with these two risk alleles. We continue to follow these AMD patients for long-term evaluation of disease progression and outcome.
Although discoveries on the potential causal relation between SNPs in various genes and multifactorial diseases such as AMD have aroused great promise in personalized medicine and early risk diagnosis, these data should be interpreted with caution.28 Detection of risky mutations in target genes could help lifestyle changes and adjust screening protocols, but the weight of such genetic data in alteration of current clinical decision and treatment plans is arguable.28 Using statistical methods for evaluation of the role of Y402H, A69S, and C2 SNP variants on risk classification, Jakobsdottir and colleagues showed that only 30%, 12%, and 3% of high risk individuals harboring these genes are clinically affected.28 This is especially true for patients with intermediate disease phenotypes.
Our study suffers from some limitations including small sample size. Although the power of the study for this sample size with a=0.05 was 100% and 71% for A69S and Y402H mutations, respectively; further studies with larger sample size are needed to confirm our results. Additionally, the Iranian population consists of various minor ethnicities and there is no data on the variability of the genetic content of these ethnicities; therefore, we did not consider ethnic variations within the Iranian population in our analysis.
In summary, this is the first genetic analysis of two major genetic risk factors for AMD in an Iranian population showing an OR of 1.9 and 2.2 for association with AMD in individuals harboring CFH Y402H and LOC387715 A69S mutations, respectively. Homozygotes had a higher risk of association with AMD. The correlation follows the same pattern of risk as in other white populations. Testing for AMD risk SNPs may help in modifying environmental and medical risk factors of AMD and tailoring treatment and follow-up plans.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Klein R, Peto T, Bird A, Vannewkirk MR. The epidemiology of age-related macular degeneration. Am J Ophthalmol. 2004;137:486–495. doi: 10.1016/j.ajo.2003.11.069. [DOI] [PubMed] [Google Scholar]
- 2.Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–851. [PMC free article] [PubMed] [Google Scholar]
- 3.Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv Ophthalmol. 1995;39:367–374. doi: 10.1016/s0039-6257(05)80092-x. [DOI] [PubMed] [Google Scholar]
- 4.Yates JR, Moore AT. Genetic susceptibility to age related macular degeneration. J Med Genet. 2000;37:83–87. doi: 10.1136/jmg.37.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klein RJ, Zeiss C, Chew EY, Tsai JY, Sackler RS, Haynes C, et al. Complement factor H polymorphism in age-related macular degeneration. Science. 2005;308:385–389. doi: 10.1126/science.1109557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edwards AO, Ritter R, Abel KJ, Manning A, Panhuysen C, Farrer LA. Complement factor H polymorphism and age-related macular degeneration. Science. 2005;308:421–424. doi: 10.1126/science.1110189. [DOI] [PubMed] [Google Scholar]
- 7.Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P, et al. Complement factor H variant increases the risk of age-related macular degeneration. Science. 2005;308:419–421. doi: 10.1126/science.1110359. [DOI] [PubMed] [Google Scholar]
- 8.Fisher SA, Abecasis GR, Yashar BM, Zareparsi S, Swaroop A, Iyengar SK, et al. Meta-analysis of genome scans of age-related macular degeneration. Hum Mol Genet. 2005;14:2257–2264. doi: 10.1093/hmg/ddi230. [DOI] [PubMed] [Google Scholar]
- 9.Seddon JM, Francis PJ, George S, Schultz DW, Rosner B, Klein ML. Association of CFH Y402H and LOC387715 A69S with progression of age-related macular degeneration. JAMA. 2007;297:1793–1800. doi: 10.1001/jama.297.16.1793. [DOI] [PubMed] [Google Scholar]
- 10.Jakobsdottir J, Conley YP, Weeks DE, Mah TS, Ferrell RE, Gorin MB. Susceptibility genes for age-related maculopathy on chromosome 10q26. Am J Hum Genet. 2005;77:389–407. doi: 10.1086/444437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scholl HP, Fleckenstein M, Charbel Issa P, Keilhauer C, Holz FG, Weber BH. An update on the genetics of age-related macular degeneration. Mol Vis. 2007;13:196–205. [PMC free article] [PubMed] [Google Scholar]
- 12.Hageman GS, Luthert PJ, Victor Chong NH, Johnson LV, Anderson DH, Mullins RF. An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE-Bruch's membrane interface in aging and age-related macular degeneration. Prog Retin Eye Res. 2001;20:705–732. doi: 10.1016/s1350-9462(01)00010-6. [DOI] [PubMed] [Google Scholar]
- 13.Dewan A, Liu M, Hartman S, Zhang SS, Liu DT, Zhao C, et al. HTRA1 promoter polymorphism in wet age-related macular degeneration. Science. 2006;314:989–992. doi: 10.1126/science.1133807. [DOI] [PubMed] [Google Scholar]
- 14.Quan YL, Zhou AY, Feng ZH. Association between complementary factor H Y402H polymorphisms and age-related macular degeneration in Chinese: Systematic review and meta-analysis. Int J Ophthalmol. 2012;5:242–246. doi: 10.3980/j.issn.2222-3959.2012.02.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fuse N, Miyazawa A, Mengkegale M, Yoshida M, Wakusawa R, Abe T, et al. Polymorphisms in complement factor H and Hemicentin-1 Genes in a Japanese population with dry-type age-related macular degeneration. Am J Ophthalmol. 2006;142:1074–1076. doi: 10.1016/j.ajo.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 16.Hughes AE, Orr N, Patterson C, Esfandiary H, Hogg R, McConnell V, et al. Neovascular age-related macular degeneration risk based on CFH, LOC387715/HTRA1, and smoking. PLoS Med. 2007;4:e355. doi: 10.1371/journal.pmed.0040355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soysal Y, Inan U, Küsbeci T, Imirzalioğlu N. Age-related macular degeneration and association of CFH Y402H and LOC387715 A69S polymorphisms in a Turkish population. DNA Cell Biol. 2012;31:323–330. doi: 10.1089/dna.2011.1214. [DOI] [PubMed] [Google Scholar]
- 18.Fotouhi A, Hashemi H, Mohammad K, Jalali KH, Tehran Eye Study The prevalence and causes of visual impairment in Tehran: the Tehran Eye Study. Br J Ophthalmol. 2004;88:740–745. doi: 10.1136/bjo.2003.031153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chowers I, Cohen Y, Goldenberg-Cohen N, Vicuna-Kojchen J, Lichtinger A, Weinstein O, et al. Association of complement factor H Y402H polymorphism with phenotype of neovascular age related macular degeneration in Israel. Mol Vis. 2008;14:1829–1834. [PMC free article] [PubMed] [Google Scholar]
- 20.Seitsonen SP, Onkamo P, Peng G, Xiong M, Tommila PV, Ranta PH, et al. Multifactor effects and evidence of potential interaction between complement factor H Y402H and LOC387715 A69S in age-related macular degeneration. PLoS One. 2008;3:e3833. doi: 10.1371/journal.pone.0003833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim NR, Kang JH, Kwon OW, Lee SJ, Oh JH, Chin HS. Association between complement factor H gene polymorphisms and neovascular age-related macular degeneration in Koreans. Invest Ophthalmol Vis Sci. 2008;49:2071–2076. doi: 10.1167/iovs.07-1195. [DOI] [PubMed] [Google Scholar]
- 22.Thakkinstian A, Han P, McEvoy M, Smith W, Hoh J, Magnusson K, et al. Systematic review and meta-analysis of the association between complementary factor H Y402H polymorphisms and age-related macular degeneration. Human Molecular Genetics. 2006;15:2784–2790. doi: 10.1093/hmg/ddl220. [DOI] [PubMed] [Google Scholar]
- 23.Rivera A, Fisher SA, Fritsche LG, Keilhauer CN, Lichtner P, Meitinger T, et al. Hypothetical LOC387715 is a second major susceptibility gene for age-related macular degeneration, contributing independently of complement factor H to disease risk. Hum Mol Genet. 2005;14:3227–3236. doi: 10.1093/hmg/ddi353. [DOI] [PubMed] [Google Scholar]
- 24.Shastry BS. Further support for the common variants in complement factor H (Y402H) and LOC387715 (A69S) genes as major risk factors for the exudative age-related macular degeneration. Ophthalmologica. 2006;220:291–295. doi: 10.1159/000094617. [DOI] [PubMed] [Google Scholar]
- 25.Yu Y, Reynolds R, Rosner B, Daly MJ, Seddon JM. Prospective assessment of genetic effects on progression to different stages of age-related macular degeneration using multistate Markov models. Invest Ophthalmol Vis Sci. 2012;53:1548–1556. doi: 10.1167/iovs.11-8657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nischler C, Oberkofler H, Ortner C, Paikl D, Riha W, Lang N, et al. Complement factor H Y402H gene polymorphism and response to intravitreal bevacizumab in exudative age-related macular degeneration. Acta Ophthalmol. 2011;89:e344–349. doi: 10.1111/j.1755-3768.2010.02080.x. [DOI] [PubMed] [Google Scholar]
- 27.Klein ML, Francis PJ, Rosner B, Reynolds R, Hamon SC, Schultz DW, et al. CFH and LOC387715/ARMS2 genotypes and treatment with antioxidants and zinc for age-related macular degeneration. Ophthalmology. 2008;115:1019–1025. doi: 10.1016/j.ophtha.2008.01.036. [DOI] [PubMed] [Google Scholar]
- 28.Jakobsdottir J, Gorin MB, Conley YP, Ferrell RE, Weeks DE. Interpretation of genetic association studies: markers with replicated highly significant odds ratios may be poor classifiers. PLoS Genet. 2009;5:e1000337. doi: 10.1371/journal.pgen.1000337. [DOI] [PMC free article] [PubMed] [Google Scholar]


