Abstract
Purpose
To report the clinical features, and anatomic and visual outcomes of pediatric retinal detachment (RD) surgery at a tertiary referral center in Southern Iran.
Methods
In this retrospective, non-comparative, interventional case series, we reviewed the records of 77 patients less than 18 years of age who had undergone primary RD surgery at Khalili Hospital, Shiraz, Iran from 2005 to 2010. All patients had follow-up duration more than 12 months.
Results
Seventy-seven eyes of 77 patients with mean age of 12.5±5 (range, 2-18) years including 56 (73%) male subjects were included. The most common etiologies of RD included trauma (90%) and myopia (6%). Different types of breaks and proliferative viteroretinopathy were present in 75% and 13% of eyes, respectively. The most common primary surgery was deep viterectomy (78%) followed by scleral buckling (19.5%). Single-operation reattachment was accomplished in 55% of cases. At final follow up, functional visual loss [best corrected visual acuity (BCVA) <5/200] occurred in 66.7%, while the rate of anatomical success was 62.3%. Significant predictors of better final BCVA were higher initial BCVA (P=0.015), absence of relative afferent pupillary defect (P=0.002), less extensive RD (P=0.031), and primary RD surgery (P=0.056). Anatomical success was associated with a lower number of procedures (P<0.001) and marginally with phakic lens status (P=0.079).
Conclusions
Trauma was the most prevalent predisposing factor for pediatric RD in our study. The high rates of functional visual loss and low anatomical success may be due to a large proportion of trauma and the complex nature of RD.
Keywords: Pediatric, Retinal Detachment, Clinical Characteristics, Visual Outcome, Anatomical Success
INTRODUCTION
The prevalence of retinal detachment (RD) in children is much lower than adults and this age group comprises only 3.2-6.6% of all cases of RD.1 Pediatric RD is a severe threat to vision due to delayed diagnosis, complicating conditions, and an immature visual system.2,3 Furthermore, these eyes probably have a lifelong risk of recurrent RD, glaucoma and cataract.4
The etiology, anatomical characteristics and prognosis of RD are different in pediatric patients as compared to adults, and there is a high incidence of predisposing factors, especially trauma.5 Consequently, guidelines for management of adult cases may be inappropriate to apply in Children.6 Different etiologic factors and clinical features in pediatric RD pose a challenge to ophthalmologists.3 In this study, we evaluate the demographic features, etiology, surgical management, and anatomical and visual outcomes of RD in pediatric patients.
METHODS
We reviewed hospital records of patients younger than 18 years of age who had undergone primary surgery for RD (rhegmatogenous, tractional or combined rhegmatogenous and tractional) at Khalili Hospital, Shiraz, Iran, between 2005 and 2010. The study was approved by the Ethics Committee of Shiraz University of Medical Sciences. Postoperative follow-up was required to be at least 12 months for inclusion into the study.
The following data were collected: sex, age at presentation, laterality, etiology, local and systemic underlying diseases, type of breaks, initial lens status, chronicity, presence of proliferative vitreoretinopathy (PVR) grade C, presenting and postoperative best-corrected visual acuity (BCVA), relative afferent pupillary defect (RAPD), type and number of operations, functional and anatomical success, and complications.
Visual acuity was measured using a Snellen chart (when possible) except in uncooperative/preverbal children, in whom it was estimated according to the ability to fixate, follow, and maintain a target. For statistical analysis, visual acuities were categorized into ≥20/200, counting fingers, hand motions, light perception, and no light perception. For preverbal children, visual acuities were excluded from the statistical analysis.
Anatomic success was defined as persistent retinal reattachment at last follow-up (regardless of presence or absence of silicone oil tamponade). Eyes with best corrected visual acuity (BCVA) <5/200 at final follow-up were considered to have functional visual loss.
Data related to surgical management included the type of surgery (pneumatic retinopexy, scleral banding, encircling scleral buckling and vitrectomy), type of internal tamponade (such as silicone oil) and number of procedures. Surgical approaches were based on surgeons’ preference, guided mainly by presence of PVR and the size of the break(s). Eyes with PVR, retinal break(s) greater than 90 degrees, multiple retinal breaks, and total RD underwent primary vitrectomy.
Statistical Analysis
Statistical analysis was performed using SPSS software (Version 18, SPSS Inc., Chicago, IL, USA). For descriptive purposes, qualitative variables were reported using percentage, odds ratio (OR) and 95% confidence interval (CI). Quantitative data were denoted by means and standard deviations. Logistic regression analysis was used to evaluate factors associated with poor visual or anatomical outcomes.
RESULTS
Seventy-seven eyes of 77 children with mean age of 12.5±5 (range, 2-18) years including 56 (73%) male subjects with RD were included for the purpose of the study. Clinical features of pediatric RD at presentation are detailed in Table 1. Most cases were pure rhegmatogenous RD (n=72, 93.5%) with flap tears (75%) being the most prevalent type of retinal break. PVR grade C was present in 13% of eyes (n=10). Most eyes were phakic (n=64, 84%). Trauma was the most prevalent (90%) cause of RD. Forty-one (53%) patients had previous intraocular surgery due to trauma, spherophakia, and congenital glaucoma.
Table 1.
Characteristics of subjects with pediatric retinal detachment
| Type | |
| Number (%) | Rhegmatogenous, 72 (93.5) |
| Tractional, 4 (5.3) | |
| Combined, 1 (1.2) | |
| Extent | |
| N (%) | ≤50%, 25 (32.5) |
| >50%, 52 (67.5) | |
| Location* | |
| N (%) | Superior, 9 (33) |
| Inferior, 13 (52) | |
| Temporal, 2 (11) | |
| Nasal, 1 (4) | |
| Break | |
| N (%) | Dialysis, 3 (4) |
| Flap tear, 54 (74) | |
| Giant tear, 10 (12) | |
| Hole†, 4 (5) | |
| Undetermined, 2 (5) | |
| Duration | |
| N (%) | ≤1 day, 16 (20) |
| >1-7 days, 14 (18) | |
| 8-30 days, 21 (27) | |
| 1-12 months, 22 (30) | |
| >1 year, 3 (4) | |
| Undetermined, 1 (1) | |
| Proliferative vitreoretinopathy | |
| N (%) | Absent, 66 (86) |
| Present, 11 (14) | |
| Lens status | |
| N (%) | Phakic, 64 (84) |
| Normal, 24 | |
| Cataract, 39 | |
| Microspherophakia, 1 | |
| Aphakic, 9 (11) | |
| Pseudophakic, 4 (5) | |
| Etiology | |
| N (%) | Trauma, 69 (90) |
| Myopia > 4 diopters, 6 (6) | |
| Other‡, 4 (4) | |
| Previous intraocular surgery | None, 36 (47) ≥1 surgery, 41§ (53) |
| N (%) | |
| None, 36 (47) | |
| ≥1 surgery, 41§ (53) |
Identified for retinal detachments with extension ≤50%
Three of the 4 patients with retinal holes had macular holes
Comprised of retinopathy of prematurity (1), posterior uveitis (1), previous lensectomy due to spherophakia (1), and previous trabeculotomy for congenital glaucoma (1)
Due to trauma (39), spherophakia (1), and congenital glaucoma (1)
Table 2 shows details of surgical procedures. The most common primary surgery was pars plana vitrectomy (n=60, 78%), and in this group, the associated tamponade were silicone oil (n=46) and gas (n=5). Scleral buckling and pneumatic retinopexy were other primary surgical procedures performed in 15 (19.5%) and 2 (2.5%) patients respectively. Forty-two patients (55%) were treated with only one surgical procedure, while 35 patients (45%) underwent more than one operation.
Table 2.
Characteristics of procedures performed for pediatric retinal detachment (RD)
| Primary surgery | |
| N (%) | Scleral buckling, 15 (19.5) |
| Pneumatic retinopexy, 2 (2.5) | |
| Deep vitrectomy, 60 (78) | |
| Tamponade | |
| Silicone, 46 | |
| Gas, 5 | |
| Undetermined, 14 | |
| Total procedures for RD‡ | |
| N (%) | 1 surgery, 42 (55) |
| >1 surgery, 35 (45) |
mean (SD), 1.8 (1.0); range, 1-5
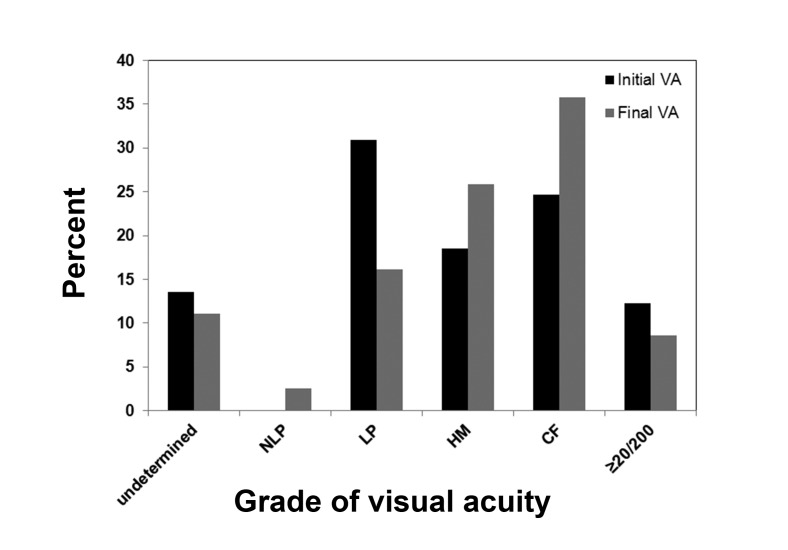
Initial and final BCVA is shown in Figure 1. Fifty-two percent (n=40) of the patients had negative RAPD on initial examination; RAPD could not be evaluated in 3 patients, and was positive in 34 patients (44.2%). Anatomical success rate was 62.3% (n=48). Final BCVA could not be assessed in 4 patients and the rate of functional visual loss at last examination was 48.6% (n=34 out of 70 eyes with available data). Of cases with trauma, 12 (17.1%) had sharp trauma while 58 (82.9%) had blunt trauma. The rates of anatomical failure were 66.7% and 34.5% (P=0.046), and the rates of functional visual loss were 66.7% and 44.4% (P=0.42) in cases with sharp and blunt trauma, respectively.
Figure 1.
Initial and final best corrected visual acuity (VA) in pediatric RD patients.
Table 3 shows the association between patient characteristics and visual or anatomical outcomes. Better initial BCVA, absence of RAPD, and retinal detachment involving less than 50% of the retina at presentation were associated with better visual outcome; however, the only independent factor was RAPD. The need for more than one RD surgery (compared to a single operation) and penetrating trauma (compared to other etiologies) were associated with anatomical failure; multiple regression analysis verified the independent association of both predictors.
Table 3.
Association between baseline characteristics and visual and anatomical outcomes
| Dependent outcome | Covariates | Logistic regression (P value)‡ | Multiple logistic regression§ |
||
|---|---|---|---|---|---|
| OR | CI (95%) | P value | |||
| Final BCVA* | Initial BCVA | 0.015 | 1.67 | 1.01-2.76 | 0.044 |
| RAPD | 0.002 | 0.47 | 0.28-0.78 | 0.004 | |
| Anatomical success | 0.053 | ||||
| Extent of RD | 0.031 | ||||
| Primary RD surgery | 0.056 | ||||
| Anatomical success† | Number of RD surgeries | <0.001 | 0.12 | 0.04-0.34 | <0.001 |
| Lens status | 0.079 | ||||
Defined as ≤HM vs. ≥CF
Defined as total retinal attachment
Covariates with P<0.1 in logistic regression analysis were entered to the multiple forward logistic regression model; only factors with P< 0.1 are shown here
OR is only provided for factors which showed statistical significance in the multiple logistic regression model
BCVA, best-corrected visual acuity; RAPD, relative afferent pupillary defect; RD, retinal detachment; OR, odds ratio; CI, confidence interval; HM, hand motion; CF, counting finger
Factors that were considered for anatomical success comprised of age, gender, extent of RD (>50% vs. ≤50%), location of subtotal RD (superior vs. inferior), PVR (present vs. absent), lens status (normal vs. abnormal [including cataract, aphakia, and pseudophakia]), etiology (trauma vs. myopia > diopters), type of beak (flap tear vs. giant break), duration of RD (≤1 month vs. >1 month), intraocular surgeries before RD (none vs. ≥1 surgery), type of primary RD surgery (scleral buckle vs. deep vitrectomy), type of tamponade (gas vs. silicone oil), number of surgeries for RD (1 vs. >1), RAPD (graded from 0 [absent] to 4+), initial visual acuity (graded as NLP, LP, HM, CF, and ≥20/200).
DISCUSSION
The current study was performed to delineate the clinical characteristics and surgical outcomes of pediatric RD. Predisposing factors or underlying retinal conditions were present in 100% of the patients; trauma was the most important etiologic factor (90%) followed by myopia (6%). Previous lensectomy for spherophakia and previous trabeculotomy for congenital glaucoma were present in 3% of cases. Trauma has been the most prevalent cause in previous studies as well ranging from 36 to 45%;6,7 however the prevalence of trauma as the etiologic factor was much higher in our study (90%). In contrast we observed a lower rate of myopia (6%) than other studies on pediatric RD (11.5-43.3%)4,8 possibly because refractive status was not known or recorded for many patients. In our series the most prevalent form of pediatric RD developed after trauma (90%). Five patients had high myopia, some of these cases probably had vitreohyaloidopathies such as stickler syndrome, but unfortunately there was no documentation on patient records. We also found a strong male predominance (73%) similar to previous series.6 Although the higher incidence of trauma among male children may explain this finding, prior studies, even after excluding perforating trauma found that 75% to 80% of pediatric patients with rhegmatogenous RD were boys.9,10 In the current series about 95% of retinal detachments were rhegmatogenous.
Most of our patients required vitrectomy as the initial surgical procedure (n=60, 78%), as opposed to scleral buckling alone (n=15, 19%) which was due to the complexity of retinal detachment and presence of PVR, giant tears, multiple retinal breaks and total RD. Silicone oil was needed for intraocular tamponade in most patients (57.1%). Final anatomical success rate was 62.3% in our series, while other studies have reported higher success rates ranging from 74.9 to 84.5%.3,5,11,12 This may be explained by the type of primary surgery performed in our study. Vitrectomy in pediatric subjects is more difficult and challenging due to strong viteroretinal adhesions and few areas with posterior vitreous detachment.11 Hence an external approach is preferred by many surgeons.3,5,11 External approaches such as scleral buckling are believed to entail less surgical trauma and morbidity than vitrectomy; furthermore, silicone oil tamponade may also lead to a low rate of sustained retinal detachment, poor visual rehabilitation, and a high complication rate.11
The rate of functional visual loss in our study was very high (48.6%) which may be due to the high incidence of trauma as the cause of RD in our series (90%); morphologic and functional outcomes of traumatic RD surgery are not favorable due to longer duration of RD, frequent macular involvement, and high rate of PVR.13 RD involving more than 50% of the retina was present in about two third of our patients and less than one fourth had PVR. RD was detected in the first 7 days in only 30% of patients and diagnosis was delayed by more than 1 month in 38% of subjects. Most cases of trauma were blunt (82.9%). Rates of anatomical failure and functional visual loss were much higher in cases with sharp trauma as compared to blunt trauma.
We evaluated the association between final BCVA and anatomical success with other factors. Better final BCVA was associated with better initial BCVA, absence of RAPD, and retinal detachment involving less than 50% of the retina; however, the only independent factor was RAPD. The need for more than one RD surgery (compared to a single operation) and penetrating trauma (compared with other etiologies) were independently associated with anatomical failure. The mismatch between anatomical and functional success rates may be due to the high risk of amblyopia in children; however, other factors such as corneal irregularity due to corneal laceration, simultaneous traumatic optic neuropathy or choroidal detachment and/or Berlin edema, and the presence of PVR may also have a role in functional visual loss.
The current study is limited by its retrospective nature, and incomplete records in some cases regarding visual acuity, refractive status and fellow eye conditions. The other shortcoming is that our data are from a tertiary eye center and may differ from those of a primary care center.
In summary, pediatric RD is commonly associated with an underlying condition. Although children often present with chronic RD and PVR, the anatomical outcomes with surgical intervention are favorable in most cases. A higher number of RD procedures and abnormal lens status are associated with worse anatomical outcomes. This single center study over a 5-year period may provide a basis for information on pediatric RD in Iran and serve as a reference to compare visual and anatomical outcomes of different surgical approaches for RD in children.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Meier P. Retinal detachment in children: differential diagnosis and current therapy. Klin Monbl Augenheilkd . 2008;225:779–790. doi: 10.1055/s-2008-1027515. [DOI] [PubMed] [Google Scholar]
- 2.Bier C, Kampik A, Gandorfer A, Ehrt O, Rudolph G. Retinal detachment in pediatrics: Etiology and risk factors. Ophthalmologe. 2010;107:165–174. doi: 10.1007/s00347-009-1996-z. [DOI] [PubMed] [Google Scholar]
- 3.Chang PY, Yang CM, Yang CH, Huang JS, Ho TC, Lin CP, et al. Clinical characteristics and surgical outcomes of pediatric rhegmatogenous retinal detachment in Taiwan. Am J Ophthalmol . 2005;139:1067–1072. doi: 10.1016/j.ajo.2005.01.027. [DOI] [PubMed] [Google Scholar]
- 4.Tassman W. Retinal detachment in children. Trans Am Acad Ophthalmol Otolaryngol. 1967;71:455–460. [PubMed] [Google Scholar]
- 5.Weinberg DV, Lyon AT, Greenwald MJ, Mets MB. Rhegmatogenous retinal detachments in children: risk factors and surgical outcomes. Ophthalmology . 2003;110:1708–1713. doi: 10.1016/S0161-6420(03)00569-4. [DOI] [PubMed] [Google Scholar]
- 6.Cheema RA, Al-Khars W, Al-Askar E, Amin YM. Pediatric retinal detachment in the Eastern Province of Saudi Arabia: experience of a tertiary care hospital. Ann Saudi Med. 2009;29:361–364. doi: 10.4103/0256-4947.55165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gangwar DN, Dogra MR, Jain IS, Grewal SP. Study of juvenile retinal detachment. Indian J Ophthalmol. 1983;31:892–894. [PubMed] [Google Scholar]
- 8.Hudson JR. The role of trauma in juvenile retinal detachment. Modern Problems Ophthalmol. 1969;8:235–241. [PubMed] [Google Scholar]
- 9.Chen SN, Jiunn-Feng H, Te-Cheng Y. Pediatric rhegmatogenous retinal detachment in Taiwan. Retina. 2006;26:410–414. doi: 10.1097/01.iae.0000238546.51756.cd. [DOI] [PubMed] [Google Scholar]
- 10.Fivgas GD, Capone A. Pediatric rhegmatogenous retinal detachment. Retina. 2001;21:101–106. doi: 10.1097/00006982-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Wang NK, Tsai CH, Chen YP, Yeung L, Wu WC, Chen TL, et al. Pediatric rhegmatogenous retinal detachment in East Asians. Ophthalmology. 2005;112:1890–1895. doi: 10.1016/j.ophtha.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 12.Soheilian M, Ramazani A, Malihi M, Yaseri M, Ahmadieh H, Dehghan MH, et al. Clinical features and surgical outcomes of pediatric rhegmatogenous retinal detachment. Retina. 2009;29:545–551. doi: 10.1097/IAE.0b013e318194fd1a. [DOI] [PubMed] [Google Scholar]
- 13.Shukla M, Ahuja OP, Jamal N. Traumatic retinal detachment. Indian J Ophthalmol. 1986;34:29–32. [PubMed] [Google Scholar]