Abstract
Purpose
To determine the prevalence of refractive errors among high school students.
Methods
In a cross-sectional study, we applied stratified cluster sampling on high school students of Aligoudarz, Western Iran. Examinations included visual acuity, non-cycloplegic refraction by autorefraction and fine tuning with retinoscopy. Myopia and hyperopia were defined as spherical equivalent of -0.5/+0.5 diopter (D) or worse, respectively; astigmatism was defined as cylindrical error >0.5 D and anisometropia as an interocular difference in spherical equivalent exceeding 1 D.
Results
Of 451 selected students, 438 participated in the study (response rate, 97.0%). Data from 434 subjects with mean age of 16±1.3 (range, 14 to 21) years including 212 (48.8%) male subjects was analyzed. The prevalence of myopia, hyperopia and astigmatism was 29.3% [95% confidence interval (CI), 25-33.6%], 21.7% (95%CI, 17.8-25.5%), and 20.7% (95%CI, 16.9-24.6%), respectively. The prevalence of myopia increased significantly with age [odds ratio (OR)=1.30, P=0.003] and was higher among boys (OR=3.10, P<0.001). The prevalence of hyperopia was significantly higher in girls (OR=0.49, P=0.003). The prevalence of astigmatism was 25.9% in boys and 15.8% in girls (OR=2.13, P=0.002). The overall prevalence of high myopia and high hyperopia were 0.5% and 1.2%, respectively. The prevalence of with-the-rule, against-the-rule, and oblique astigmatism was 14.5%, 4.8% and 1.4%, respectively. Overall, 4.6% (95%CI, 2.6-6.6%) of subjects were anisometropic.
Conclusion
More than half of high school students in Aligoudarz had at least one type of refractive error. Compared to similar studies, the prevalence of refractive errors was high in this age group.
Keywords: Myopia, Hyperopia, Astigmatism, High School Children, Prevalence, Cross-Sectional Study
INTRODUCTION
Refractive errors are the most prevalent visual disorder among children with more than 20% of children having refractive errors. Although refractive errors are easily correctable, they are the main cause of visual impairment in children.1,2
In recent decades, many studies have focused on the prevalence of refractive errors throughout the world.1-19 It is well known that myopia is more prevalent in Eastern Asian countries while European and American nations are mostly affected by hyperopia. Although racial and ethnic differences are the most important reason for differences in the prevalence of refractive errors, differences in lifestyle such as the amount of near vision tasks has also increased the global variation in the prevalence of refractive errors.20,21 In addition to creating personal issues, the treatment and correction of refractive errors imposes high costs on the community in different countries.22
In 2000, the protocol of the Refractive Error Study in Children (RESC) was presented. This protocol was designed to standardize the methodology used to obtain prevalence data on childhood refractive errors. It emphasizes the importance of evaluating refractive errors using cycloplegic refraction.23 Since then, refractive errors in the 5-15 year age range have been studied in many populations around the world.6-8,10,24-32 In Iran, a number of studies have described refractive errors in students in this age range using cycloplegic refraction.6-8,33 Although we have abundant information regarding refractive errors in the 5 to 15 year old students in Iran, there is no comprehensive information regarding those older than 15 years. According to the education system in Iran, most high school students are over 14 years; these students are in the preparatory stages for university, and visual problems and refractive errors are very important for them.
There are few studies that have exclusively reported refractive errors in high school students,12,31,34 some of which have limitations such as studying male subjects only.34 In light of the importance of refractive errors in high school students and the paucity of information in this age group in Iran, this study was performed to determine the prevalence of refractive errors among high school students in Aligoudarz, a city in the West of Iran.
METHODS
This cross-sectional study was conducted on high school students in Aligoudarz, a city in Lorestan province in the West of Iran. We used stratified cluster sampling to select samples from Aligoudarz high schools, using classes and education years as clusters. The target sample size for this study was 400. Two educational institutions (one of the 3 boys’ centers, and one of the two girls’ centers which accommodated at least 200 rural and urban students) were randomly selected. Then, two classes were randomly selected from each grade in each school. All students enrolled in these classes were invited. If a certain class was not able to participate, for any reason, another class of the same grade was selected instead. Educational grade was implied in the sampling design to satisfy equal age categories among participants. A total of 16 classes were targeted as the sampling clusters.
The aim and design of the study were explained to the subjects and those whose guardians consented to participation completed a form, had an interview, and their demographics were recorded.
Examinations
First, a skilled technician determined non-cycloplegic refraction using the Topcon RM8800 autorefractometer (Topcon Corporation, Tokyo, Japan), and the results were refined by retinoscopy using the Heine Beta 200 (Heine Optotechnic, Germany) and MSD trial frame (MSD, Meniscus Trial Lenses, Italy). Then, if the student had spectacles, visual acuity was first tested with the current glasses using a Snellen E-chart at 6 meters distance. If not, uncorrected visual acuity was measured.
Myopia was defined as a spherical equivalent refractive error of -0.5 diopter (D) or worse and hyperopia was defined as a spherical equivalent of +0.5 D or worse. Anisometropia was defined as an interocular difference exceeding 1.0 D in spherical equivalent. High, moderate, and low myopia were defined as spherical equivalent of worse than -6.0 D, between -3.1 and -6.0 D, and between -0.5 and -3.0 D, respectively. High, moderate, and mild hyperopia was defined as a spherical equivalent of worse than 4.0 D, between 2.1 and 4.0 D, and between 0.5 and 2.0 D, respectively.
Astigmatism was defined as a cylindrical error exceeding 0.5 D. Astigmatism was classified as with-the-rule (WTR) if the axis was 0±30º, against-the-rule (ATR) if the axis was 90±30º, and oblique with other axes.
Statistical Analysis
Prevalence and 95% confidence intervals (CIs) of refractive errors were calculated. A simple logistic regression model was used to examine correlations between myopia, hyperopia, astigmatism, and anisometropia on one hand, and age, sex and region of residence on the other hand. Age, sex and residence were then separately included into multivariate logistic regression models for myopia, hyperopia, astigmatism and anisometropia to test their role in these conditions and to eliminate the effects of confounding variables.
Ethical Issues
Informed consent was obtained from parents of children who participated in our study. The protocol of this study was approved by the Review Board of Noor Ophthalmology Research Center.
RESULTS
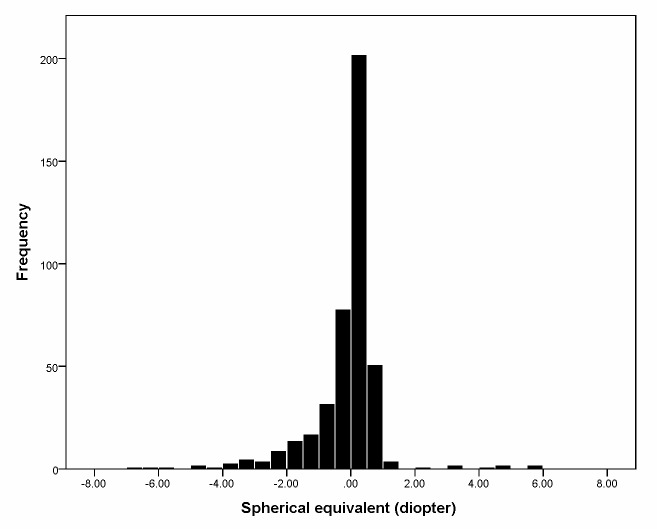
Of 451 selected students, 438 persons participated in the study (response rate, 97.0%). Due to missing refraction data for 4 participants, data from 434 people were analyzed. Mean age of the students was 16±1.3 (range, 14-21) years including 212 (48.8%) male subjects. Figure 1 illustrates the distribution of spherical equivalent in the study population. Mean spherical equivalent was -0.23±1.2 (range, -6.6 to 5.7) D overall; -0.4±1.5 D in boys and -0.1±1.1 D in girls (P=0.014). The overall prevalence of myopia was 29.3% (95% CI, 25-33.6%). Table 1 shows the prevalence of myopia based on sex and age. Table 2 summarizes the correlation among different types of refractive errors and the studied variables using simple and multiple logistic regression models.
Figure 1.
Distribution of spherical equivalent refractive error in high school children of Aligoudarz.
Table 1.
Prevalence and 95% confidence intervals (CI) for myopia, hyperopia, astigmatism and anisometropia in high school children of Aligoudarz
| Myopia | Hyperopia | Astigmatism | Anisometropia | |
|---|---|---|---|---|
| % (95%CI) | % (95%CI) | % (95%CI) | % (95%CI) | |
| Age (yr) | ||||
| 14 | 21.8 (10.6-33.1) | 29.1 (16.7-41.5) | 7.3 (0.2 -14.4) | 5.5 (0.5-11.7) |
| 15 | 26.2 (18.4-34.0) | 19.8 (12.8-26.9) | 20.6 (13.5-27.8) | 6.3 (2.0-10.7) |
| 16 | 28.0 (19.0-37.0) | 22.0 (13.7-30.3) | 19.0 (11.2-26.8) | 4.0 (0.1-7.9) |
| 17 | 34.1 (24.1-44.0) | 18.7 (10.5-26.8) | 26.4 (17.1-35.6) | 3.3 (0.3-7.1) |
| 18> | 37.1 (24.7-49.5) | 22.6 (11.9-33.3) | 27.4 (16.0-38.8) | 3.2 (1.3-7.7) |
| Sex | ||||
| Female | 19.4 (14.1-24.6) | 27.5 (21.6 -33.4) | 15.8 (10.9-20.6) | 4.5 (1.8-7.3) |
| Male | 39.6 (33.0-46.3) | 15.6 (10.6-20.5) | 25.9 (20.0-31.9) | 4.7 (1.8-7.6) |
| Total | 29.3 (25.0-33.6) | 21.7 (17.8-25.5) | 20.7 (16.9-24.6) | 4.6 (2.6-6.6) |
Table 2.
Association between refractive errors and different variables based on simple and multiple logistic regression analysis
| Simple logistic regression | Multiple logistic regression | |||
|---|---|---|---|---|
| OR (95%CI) | P-value | OR (95%CI) | P-value | |
| Myopia | ||||
| Age (years) | 1.2 (1.02 -1.42) | 0.029 | 1.3 (1.1 -1.55) | 0.003 |
| sex (male/female) | 2.73 (1.77 -4.21) | <0.001 | 3.1 (1.98 -4.84) | <0.001 |
| Residence (urban/rural) | 1.62 (1.08 -2.42) | 0.019 | * | NS |
| Hyperopia | ||||
| Age (years) | 0.94 (0.78 -1.13) | 0.489 | * | NS |
| sex (male/female) | 0.49 (0.3 -0.78) | 0.003 | * | NS |
| Residence (urban/rural) | 0.58 (0.37 -0.9) | 0.016 | * | NS |
| Astigmatism | ||||
| Age (years) | 1.29 (1.07 -1.55) | 0.008 | 1.35 (1.12 -1.64) | 0.002 |
| sex (male/female) | 1.87 (1.17 -3.01) | 0.010 | 2.13 (1.31 -3.48) | 0.002 |
| Residence (urban/rural) | 1.82 (1.15 -2.87) | 0.010 | * | NS |
| Anisometropia | ||||
| Age (years) | 0.82 (0.56 -1.18) | 0.278 | * | NS |
| sex (male/female) | 1.05 (0.43 -2.59) | 0.907 | * | NS |
| Residence (urban/rural) | 1.44 (0.61 -3.42) | 0.408 | * | NS |
OR, odds ratio; CI, confidence interval; NS: not significant
These factors did not remain in the multiple logistic regression models
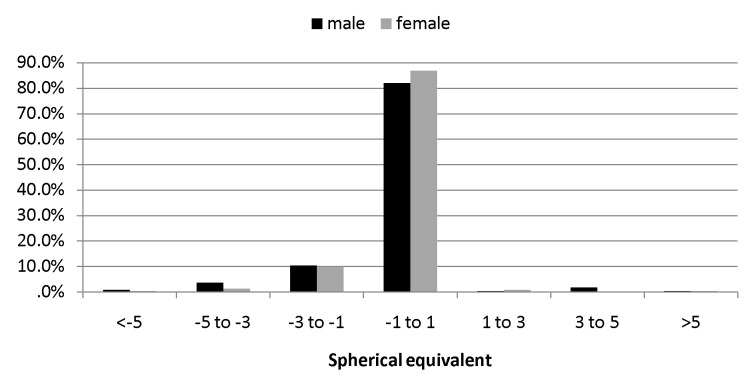
In simple logistic regression model, the prevalence of myopia was significantly higher in boys (P<0.001). Also as shown in Table 1, the prevalence of myopia significantly increased with age; 21.8% in 14 year-old subjects versus 37.1% in 18 year-old students (P=0.029). The prevalence of mild, moderate, and severe myopia was 25.6%, 3.2%, and 0.5%, respectively. Figure 2 illustrates the distribution of spherical equivalent based on the severity of refractive errors in boys and girls. The prevalence of myopia was 23.0% (95%CI, 16.8-29.3%) in rural students and 33.5% (95%CI, 27.5-39.4%) among urban students (P=0.019) (Table 2). Based on multiple logistic regression model, only older age (P=0.003) and male sex (P<0.001) were significantly correlated with myopia.
Figure 2.
Spherical equivalent refractive error by gender.
The overall prevalence of hyperopia was 21.7% (95%CI, 17.8-25.5%). As demonstrated in Table 2, the prevalence of hyperopia was significantly higher in girls (P=0.003) but was not significantly different among different age groups (P=0.489). The prevalence of mild, moderate, and severe hyperopia was 19.4%, 1.2%, and 1.2%, respectively. The prevalence of hyperopia was 27.5% (95%CI, 20.1-34.1%) in rural students and 17.9% (95%CI, 13.1-22.7%) in urban subjects (P=0.016). After entering age, sex and residence, only female gender was significantly correlated with hyperopia (Table 2).
Mean cylindrical power was 0.5±0.9 D. The overall prevalence of astigmatism was 20.7% (95%CI, 16.9-24.6%); 25.9% in boys and 15.8% in girls (P<0.001). Also, as demonstrated in Table 1, the prevalence of astigmatism had an increasing trend from 7.3% in 14 years old students to 27.4% in 18 year old subjects (P=0.008). The prevalence of WTR, ATR, and oblique astigmatism was 14.5%, 4.8%, and 1.4% overall; 17.5%, 6.1%, and 2.4% in boys; and 11.7%, 3.6% and 0.5% in girls, respectively. Inter-sex difference in terms of the type of astigmatism was statistically significant (p=0.043). The prevalence of astigmatism was significantly higher among rural students (24.5% in rural and 15.2% in urban students, P=0.010). The prevalence of WTR astigmatism was significantly lower in rural students than in urban students (P=0.020). The prevalence of WTR, ATR and oblique astigmatism was 28.3%, 42.9% and 16.7% in rural astigmatic students and 71.7%, 57.1% and 83.3% in urban astigmatic subjects. Based on multiple logistic regression model, the prevalence of astigmatism increased significantly with age and was significantly higher in boys (Table 2).
Anisometropia was detected in 4.6% (95%CI, 2.6-6.6%) of students and the differences between girls and boys (P=0.907), different age groups (P=0.278), and rural and urban students (P=0.408) were not significant. Overall, 55.3% of students were ametropic.
DISCUSSION
In this study, the prevalence of refractive errors was determined in a sample of high school students from Aligoudarz, Western Iran. Since different methods have been used to determine refractive errors in different studies, comparison of the results must be done with caution. More than half of the students in this study had at least one type of refractive error. This finding indicates the importance of refractive errors in this age group. Since uncorrected refractive errors are one of the most important causes of visual impairment in the world, refractive errors in this age range deserve special attention.2
Of students enrolled in this study, 29.3% were myopic; this prevalence is lower than that of East Asian countries such as Singapore,12 China,31 and Hong Kong35 but comparable to other parts of Iran.7,34 Nonetheless, compared to other refractive errors, myopia is more likely to go uncorrected and lead to visual impairment.36,37 Therefore, although its prevalence in this study was lower than other studies, its correction calls for attention.
The prevalence of hyperopia in this study was lower than myopia and astigmatism, however, since non-cycloplegic refraction in this age group has low sensitivity in detecting hyperopia,38 the observed prevalence is expected to be an underestimation. Still, the observed rate is significantly higher than that reported in previous studies.6-8,33 Use of different cut-off points can be one reason for such differences, but even when similar definitions are used, the prevalence of hyperopia in our study seems high. Based on previous studies, hyperopia is more common than myopia among Iranians.6-8,33
The prevalence of astigmatism is also relatively higher in this study as compared to previous studies in Iran.6-8 The prevalence of astigmatism was 18% in Dezful high school students and 10.5% in Varamin school boys.7,34 Using a similar definition, higher astigmatism prevalence rates have only been reported from East Asian countries, especially China (23.5%) and Singapore (58.7%).12,31 Astigmatism has already been reported to be affected by ethnicity and genetics.39,40 Our findings regarding astigmatism along with a high prevalence of hyperopia may also confirm the role of ethnicity for explaining the observed differences.
The prevalence of myopia increased with age and was higher in boys, while the prevalence of hyperopia was higher in girls. This observation is in agreement with most previous studies.6,7,11,30,41 Most changes in the prevalence of hyperopia have been observed in children before the age of 15; a myopic shift is expected to occur thereafter. Other studies have also shown this age group to coincide with the onset of myopia.42-44 Overall, it seems that both biometric and environmental factors may play a role in the increased prevalence of myopia in this age group.42,43,45-47 Possible causes of increased myopia in this age group are firstly the increase in axial length with age, and secondly an increase in near work in high school students.42-44
Since changes in refraction are mainly attributed to ocular biometric components, it seems that inter-sex differences in ocular biometrics is the main cause of the higher prevalence of myopia in boys and hyperopia in girls. We believe that axial length plays the most important role in explaining the inter-sex difference in refractive errors. In all age groups, axial length has been reported to be larger in male subjects as compared to females.48,49 According to our findings, the prevalence of astigmatism increased with age and was higher in boys. Although most studies agree that the prevalence of astigmatism increases with aging after the age of 40 years,50 there are contradictory results in this age group in this regard.51,52 Nonetheless, there are hardly any studies suggesting that astigmatism increases in this age group. Most studies indicate that the prevalence of astigmatism is high in infancy and follows a decreasing trend towards adolescence.40
In summary, based on the results of the present study, more than half of high school students had refractive errors. Compared to other studies on the 5-15 years age group, our results show that the prevalence of refractive errors in this age group is high. In light of the importance of perfect visual acuity in this age group, the health system should give priority to identifying affected students and correcting their refractive errors.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Hashemi H, Fotouhi A, Mohammad K. The age- and gender-specific prevalences of refractive errors in Tehran: the Tehran Eye Study. Ophthalmic Epidemiol. 2004;11:213–225. doi: 10.1080/09286580490514513. [DOI] [PubMed] [Google Scholar]
- 2.Wong TY, Foster PJ, Hee J, Ng TP, Tielsch JM, Chew SJ, et al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000;41:2486–2494. [PubMed] [Google Scholar]
- 3.Saw SM, Chan YH, Wong WL, Shankar A, Sandar M, Aung T, et al. Prevalence and risk factors for refractive errors in the Singapore Malay Eye Survey. Ophthalmology. 2008;115:1713–1719. doi: 10.1016/j.ophtha.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 4.Rosman M, Wong TY, Tay WT, Tong L, Saw SM. Prevalence and risk factors of undercorrected refractive errors among Singaporean Malay adults: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci. 2009;50:3621–3628. doi: 10.1167/iovs.08-2788. [DOI] [PubMed] [Google Scholar]
- 5.Brown SA, Weih LM, Fu CL, Dimitrov P, Taylor HR, McCarty CA. Prevalence of amblyopia and associated refractive errors in an adult population in Victoria, Australia. Ophthalmic Epidemiol. 2000;7:249–258. [PubMed] [Google Scholar]
- 6.Rezvan F, Khabazkhoob M, Fotouhi A, Hashemi H, Ostadimoghaddam H, Heravian J, et al. Prevalence of refractive errors among school children in Northeastern Iran. Ophthalmic Physiol Opt. 2012;32:25–30. doi: 10.1111/j.1475-1313.2011.00879.x. [DOI] [PubMed] [Google Scholar]
- 7.Fotouhi A, Hashemi H, Khabazkhoob M, Mohammad K. The prevalence of refractive errors among schoolchildren in Dezful, Iran. Br J Ophthalmol. 2007;91:287–292. doi: 10.1136/bjo.2006.099937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yekta A, Fotouhi A, Hashemi H, Dehghani C, Ostadimoghaddam H, Heravian J, et al. Prevalence of refractive errors among schoolchildren in Shiraz, Iran. Clin Experiment Ophthalmol. 2010;38:242–248. doi: 10.1111/j.1442-9071.2010.02247.x. [DOI] [PubMed] [Google Scholar]
- 9.Raju P, Ramesh SV, Arvind H, George R, Baskaran M, Paul PG, et al. Prevalence of refractive errors in a rural South Indian population. Invest Ophthalmol Vis Sci. 2004;45:4268–4272. doi: 10.1167/iovs.04-0221. [DOI] [PubMed] [Google Scholar]
- 10.Anera RG, Soler M, de la Cruz Cardona J, Salas C, Ortiz C. Prevalence of refractive errors in school-age children in Morocco. Clin Experiment Ophthalmol. 2009;37:191–196. doi: 10.1111/j.1442-9071.2009.02001.x. [DOI] [PubMed] [Google Scholar]
- 11.Czepita D, Mojsa A, Ustianowska M, Czepita M, Lachowicz E. Prevalence of refractive errors in schoolchildren ranging from 6 to 18 years of age. Ann Acad Med Stetin. 2007;53:53–56. [PubMed] [Google Scholar]
- 12.Quek TP, Chua CG, Chong CS, Chong JH, Hey HW, Lee J, et al. Prevalence of refractive errors in teenage high school students in Singapore. Ophthalmic Physiol Opt. 2004;24:47–55. doi: 10.1046/j.1475-1313.2003.00166.x. [DOI] [PubMed] [Google Scholar]
- 13.Midelfart A, Kinge B, Midelfart S, Lydersen S. Prevalence of refractive errors in young and middle-aged adults in Norway. Acta Ophthalmol Scand. 2002;80:501–505. doi: 10.1034/j.1600-0420.2002.800508.x. [DOI] [PubMed] [Google Scholar]
- 14.Ostadimoghaddam H, Fotouhi A, Hashemi H, Yekta A, Heravian J, Rezvan F, et al. Prevalence of the refractive errors by age and gender: the Mashhad eye study of Iran. Clin Experiment Ophthalmol. 2011;39:743–751. doi: 10.1111/j.1442-9071.2011.02584.x. [DOI] [PubMed] [Google Scholar]
- 15.Wu SY, Nemesure B, Leske MC. Refractive errors in a black adult population: the Barbados Eye Study. Invest Ophthalmol Vis Sci. 1999;40:2179–2184. [PubMed] [Google Scholar]
- 16.Liang YB, Wong TY, Sun LP, Tao QS, Wang JJ, Yang XH, et al. Refractive errors in a rural Chinese adult population the Handan eye study. Ophthalmology. 2009;116:2119–2127. doi: 10.1016/j.ophtha.2009.04.040. [DOI] [PubMed] [Google Scholar]
- 17.Sawada A, Tomidokoro A, Araie M, Iwase A, Yamamoto T. Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology. 2008;115:363–370. doi: 10.1016/j.ophtha.2007.03.075. [DOI] [PubMed] [Google Scholar]
- 18.Attebo K, Ivers RQ, Mitchell P. Refractive errors in an older population: the Blue Mountains Eye Study. Ophthalmology. 1999;106:1066–1072. doi: 10.1016/S0161-6420(99)90251-8. [DOI] [PubMed] [Google Scholar]
- 19.Dandona R, Dandona L, Naduvilath TJ, Srinivas M, McCarty CA, Rao GN. Refractive errors in an urban population in Southern India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci. 1999;40:2810–2818. [PubMed] [Google Scholar]
- 20.Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ, et al. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008;49:2903–2910. doi: 10.1167/iovs.07-0804. [DOI] [PubMed] [Google Scholar]
- 21.Low W, Dirani M, Gazzard G, Chan YH, Zhou HJ, Selvaraj P, et al. Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br J Ophthalmol. 2010;94:1012–1016. doi: 10.1136/bjo.2009.173187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fricke TR, Holden BA, Wilson DA, Schlenther G, Naidoo KS, Resnikoff S, et al. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ. 2012;90:728–738. doi: 10.2471/BLT.12.104034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Negrel AD, Maul E, Pokharel GP, Zhao J, Ellwein LB. Refractive Error Study in Children: sampling and measurement methods for a multi-country survey. Am J Ophthalmol. 2000;129:421–426. doi: 10.1016/s0002-9394(99)00455-9. [DOI] [PubMed] [Google Scholar]
- 24.Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB. Refractive Error Study in Children: results from La Florida, Chile. Am J Ophthalmol. 2000;129:445–454. doi: 10.1016/s0002-9394(99)00454-7. [DOI] [PubMed] [Google Scholar]
- 25.Pokharel GP, Negrel AD, Munoz SR, Ellwein LB. Refractive Error Study in Children: results from Mechi Zone, Nepal. Am J Ophthalmol. 2000;129:436–444. doi: 10.1016/s0002-9394(99)00453-5. [DOI] [PubMed] [Google Scholar]
- 26.Zhao J, Pan X, Sui R, Munoz SR, Sperduto RD, Ellwein LB. Refractive Error Study in Children: results from Shunyi District, China. Am J Ophthalmol. 2000;129:427–435. doi: 10.1016/s0002-9394(99)00452-3. [DOI] [PubMed] [Google Scholar]
- 27.Dandona R, Dandona L, Srinivas M, Sahare P, Narsaiah S, Munoz SR, et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43:615–622. [PubMed] [Google Scholar]
- 28.Murthy GV, Gupta SK, Ellwein LB, Munoz SR, Pokharel GP, Sanga L, et al. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci. 2002;43:623–631. [PubMed] [Google Scholar]
- 29.Naidoo KS, Raghunandan A, Mashige KP, Govender P, Holden BA, Pokharel GP, et al. Refractive error and visual impairment in African children in South Africa. Invest Ophthalmol Vis Sci. 2003;44:3764–3770. doi: 10.1167/iovs.03-0283. [DOI] [PubMed] [Google Scholar]
- 30.Goh PP, Abqariyah Y, Pokharel GP, Ellwein LB. Refractive error and visual impairment in school-age children in Gombak District, Malaysia. Ophthalmology. 2005;112:678–685. doi: 10.1016/j.ophtha.2004.10.048. [DOI] [PubMed] [Google Scholar]
- 31.He M, Huang W, Zheng Y, Huang L, Ellwein LB. Refractive error and visual impairment in school children in rural southern China. Ophthalmology. 2007;114:374–382. doi: 10.1016/j.ophtha.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 32.Zhang M, Li L, Chen L, Lee J, Wu J, Yang A, et al. Population density and refractive error among Chinese children. Invest Ophthalmol Vis Sci. 2010;51:4969–4976. doi: 10.1167/iovs.10-5424. [DOI] [PubMed] [Google Scholar]
- 33.Ostadi-Moghaddam H, Fotouhi A, Khabazkhoob M, Heravian J, Yekta AA. Prevalence and risk factors of refractive errors among schoolchildren in Mashhad, 2006-2007. Iranian Journal of Ophthalmology. 2008;20:3–9. [Google Scholar]
- 34.Faghihi M, Ostadimoghaddam H, Fatemi A, Heravian J, Yekta A. The Prevalence of refractive errors, strabismus and amblyopia in schoolboys of Varamin, Iran, in 2010. Iranian Journal of Ophthalmology. 2012;24:33–39. [Google Scholar]
- 35.Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY, et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci. 2004;45:1071–1075. doi: 10.1167/iovs.03-1151. [DOI] [PubMed] [Google Scholar]
- 36.Padhye AS, Khandekar R, Dharmadhikari S, Dole K, Gogate P, Deshpande M. Prevalence of uncorrected refractive error and other eye problems among urban and rural school children. Middle East Afr J Ophthalmol. 2009;16:69–74. doi: 10.4103/0974-9233.53864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lamoureux EL, Saw SM, Thumboo J, Wee HL, Aung T, Mitchell P, et al. The impact of corrected and uncorrected refractive error on visual functioning: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci. 2009;50:2614–2620. doi: 10.1167/iovs.08-2164. [DOI] [PubMed] [Google Scholar]
- 38.Fotouhi A, Morgan IG, Iribarren R, Khabazkhoob M, Hashemi H. Validity of noncycloplegic refraction in the assessment of refractive errors: the Tehran Eye Study. Acta Ophthalmol. 2012;90:380–386. doi: 10.1111/j.1755-3768.2010.01983.x. [DOI] [PubMed] [Google Scholar]
- 39.Dirani M, Islam A, Shekar SN, Baird PN. Dominant genetic effects on corneal astigmatism: the genes in myopia (GEM) twin study. Invest Ophthalmol Vis Sci. 2008;49:1339–1344. doi: 10.1167/iovs.07-1011. [DOI] [PubMed] [Google Scholar]
- 40.Read SA, Collins MJ, Carney LG. A review of astigmatism and its possible genesis. Clin Exp Optom. 2007;90:5–19. doi: 10.1111/j.1444-0938.2007.00112.x. [DOI] [PubMed] [Google Scholar]
- 41.Pokharel A, Pokharel PK, Das H, Adhikari S. The patterns of refractive errors among the school children of rural and urban settings in Nepal. Nepal J Ophthalmol. 2010;2:114–120. doi: 10.3126/nepjoph.v2i2.3717. [DOI] [PubMed] [Google Scholar]
- 42.Zadnik K, Manny RE, Yu JA, Mitchell GL, Cotter SA, Quiralte JC, et al. Ocular component data in schoolchildren as a function of age and gender. Optom Vis Sci. 2003;80:226–236. doi: 10.1097/00006324-200303000-00012. [DOI] [PubMed] [Google Scholar]
- 43.Garner LF, Yap MK, Kinnear RF, Frith MJ. Ocular dimensions and refraction in Tibetan children. Optom Vis Sci. 1995;72:266–271. doi: 10.1097/00006324-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Gonzalez Blanco F, Sanz Fernandez JC, Munoz Sanz MA. Axial length, corneal radius, and age of myopia onset. Optom Vis Sci. 2008;85:89–96. doi: 10.1097/OPX.0b013e3181622602. [DOI] [PubMed] [Google Scholar]
- 45.Wu HM, Gupta A, Newland HS, Selva D, Aung T, Casson RJ. Association between stature, ocular biometry and refraction in an adult population in rural Myanmar: the Meiktila eye study. Clin Experiment Ophthalmol. 2007;35:834–839. doi: 10.1111/j.1442-9071.2007.01638.x. [DOI] [PubMed] [Google Scholar]
- 46.Warrier S, Wu HM, Newland HS, Muecke J, Selva D, Aung T, et al. Ocular biometry and determinants of refractive error in rural Myanmar: the Meiktila Eye Study. Br J Ophthalmol. 2008;92:1591–1594. doi: 10.1136/bjo.2008.144477. [DOI] [PubMed] [Google Scholar]
- 47.Wickremasinghe S, Foster PJ, Uranchimeg D, Lee PS, Devereux JG, Alsbirk PH, et al. Ocular biometry and refraction in Mongolian adults. Invest Ophthalmol Vis Sci. 2004;45:776–783. doi: 10.1167/iovs.03-0456. [DOI] [PubMed] [Google Scholar]
- 48.Mallen EA, Gammoh Y, Al-Bdour M, Sayegh FN. Refractive error and ocular biometry in Jordanian adults. Ophthalmic Physiol Opt. 2005;25:302–309. doi: 10.1111/j.1475-1313.2005.00306.x. [DOI] [PubMed] [Google Scholar]
- 49.Ip JM, Huynh SC, Robaei D, Kifley A, Rose KA, Morgan IG, et al. Ethnic differences in refraction and ocular biometry in a population-based sample of 11-15-year-old Australian children. Eye (Lond) 2008;22:649–656. doi: 10.1038/sj.eye.6702701. [DOI] [PubMed] [Google Scholar]
- 50.Gudmundsdottir E, Jonasson F, Jonsson V, Stefansson E, Sasaki H, Sasaki K. "With the rule" astigmatism is not the rule in the elderly. Reykjavik Eye Study: a population based study of refraction and visual acuity in citizens of Reykjavik 50 years and older. Iceland-Japan Co-Working Study Groups. Acta Ophthalmol Scand. 2000;78:642–646. doi: 10.1034/j.1600-0420.2000.078006642.x. [DOI] [PubMed] [Google Scholar]
- 51.Fotouhi A, Hashemi H, Yekta AA, Mohammad K, Khoob MK. Characteristics of astigmatism in a population of schoolchildren, Dezful, Iran. Optom Vis Sci. 2011;88:1054–1059. doi: 10.1097/OPX.0b013e318221727d. [DOI] [PubMed] [Google Scholar]
- 52.Tong L, Saw SM, Lin Y, Chia KS, Koh D, Tan D. Incidence and progression of astigmatism in Singaporean children. Invest Ophthalmol Vis Sci. 2004;45:3914–3918. doi: 10.1167/iovs.04-0492. [DOI] [PubMed] [Google Scholar]