Abstract
Context
National efforts to measure hospital performance for cardiac arrest have focused on case survival, with the hope of improving survival after cardiac arrest. However, it is plausible that hospitals with high case-survival rates do a poor job of preventing cardiac arrests in the first place.
Objective
To describe the association between inpatient cardiac arrest incidence and survival rates.
Design, Setting, and Patients
Within a large, national registry, we identified hospitals with at least 50 adult in-hospital cardiac arrest cases between January 1, 2000 and November 30, 2009. We used multivariable hierarchical regression to evaluate the correlation between a hospital’s cardiac arrest incidence rate and its case-survival rate after adjusting for patient and hospital characteristics.
Main Outcome Measure
The correlation between a hospital’s incidence rate and case-survival rate for cardiac arrest.
Results
Of 102,153 cases at 358 hospitals, the median hospital cardiac arrest incidence rate was 4.02 per 1000 admissions (IQR: 2.95 to 5.65 per 1000 admissions), and the median hospital case-survival rate was 18.8% (IQR: 14.5% to 22.6%). In crude analyses, hospitals with higher case-survival rates also had lower cardiac arrest incidence (correlation of -0.16; P=0.003). This relationship persisted after adjusting for patient characteristics (correlation of -0.15; P=0.004). After adjusting for potential mediators of this relationship (i.e., hospital characteristics), the relationship between incidence and case-survival was attenuated (correlation of -0.07; P=0.18). The one modifiable hospital factor that most attenuated this relationship was a hospital’s nurse-to-bed ratio (correlation of -0.12; P=0.03).
Conclusions
Hospitals with exceptional rates of survival for in-hospital cardiac arrest are also better at preventing cardiac arrests, even after adjusting for patient case-mix. This relationship is partially mediated by measured hospital attributes. Performance measures focused on case-survival rates appear to be an appropriate first step in quality measurement for in-hospital cardiac arrest.
Introduction
Approximately 200,000 adults have hospitalizations complicated by a cardiac arrest annually in the U.S.1 Since fewer than 20% survive to hospital discharge,2 most prior studies have focused on identifying factors associated with improved in-hospital survival.3-9 However, this emphasis may not accurately reflect a hospital’s overall performance in resuscitation outcomes, as it ignores the hospital’s cardiac arrest incidence rate.10
It is possible that hospitals with high case-survival rates (“high performers”) do a poor job of preventing cardiac arrests, and therefore only appear to have better resuscitation outcomes because more “lower-risk” patients have an arrest and are able to survive resuscitation efforts.10 If this was the case, it would raise questions about current efforts by organizations such as The Joint Commission to disseminate performance measures for in-hospital resuscitation that focus only on case-survival rates. Alternatively, high-performing hospitals may excel at both preventing and treating in-hospital cardiac arrest (i.e., low incidence and high case-survival rates), or there may be no association between incidence and case-survival rates.
To assess whether or not case-survival rates are effective at identifying high performing hospitals, we examined the relationship between a hospital’s cardiac arrest incidence rate and its case-survival rate, using data from a large, national in-hospital cardiac arrest registry. In addition, we examined hospital factors that may mediate any relationship found between incidence and case-survival rates for cardiac arrest.
Methods
Data Sources
We conducted our study within Get with the Guidelines (GWTG) – Resuscitation, formerly known as the National Registry of Cardiopulmonary Resuscitation (NRCPR). GWTG-Resuscitation is a large, prospective national registry of patients with in-hospital cardiac arrest, and its design has been previously described.11 To summarize briefly, the registry enrolls patients with a pulseless cardiac arrest, which is defined as the absence of a palpable central pulse; apnea; and unresponsiveness in patients without do-not-resuscitate (DNR) orders. Using standardized Utstein-style definitions,12,13 quality improvement personnel at participating hospitals collect information on clinical characteristics and outcomes for consecutive patients with in-hospital cardiac arrest. Data accuracy is enhanced through training of research staff, quality assurance activities such as routine data re-abstraction, and standard software that flags outlier values and incomplete data. GWTG-Resuscitation also provides information on hospital characteristics and cardiac arrest incidence, as the registry data has been linked with data from the American Hospital Association.
Study Population
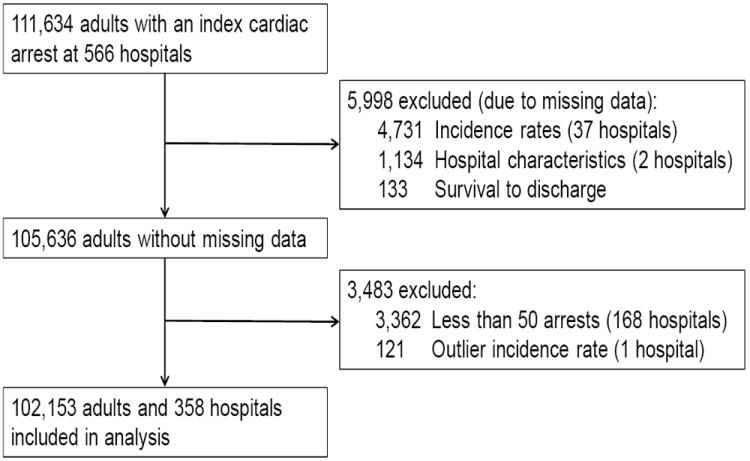
Between January 1, 2000 and November 30, 2009, we identified 111,634 patients 18 years of age or older at 566 hospitals with an index in-hospital cardiac arrest (Figure 1). Since we were interested in looking at the relationship between a hospital’s cardiac arrest incidence rate and case-survival rate, we excluded 4,731 patients from 37 hospitals with missing information on cardiac arrest incidence and 133 patients with missing data on survival to discharge. We also excluded two hospitals with 1,134 patients during the entire study period, because these hospitals lacked data on hospital characteristics. To ensure that each hospital had sufficient case volume, we restricted our analyses to those hospitals with at least 50 cardiac arrest cases during the study period (3,362 patients from 168 hospitals excluded). Finally, we excluded 121 patients from 1 hospital with an extreme outlier cardiac arrest incidence rate (17 times the standard deviation). Our final study sample comprised 102,153 adults with an in-hospital cardiac arrest at 358 hospitals.
Figure 1. Study cohort.
Study Outcomes
Our outcome of interest was the correlation between a hospital’s incidence rate and case-survival rate for cardiac arrest. The hospital’s case-survival rate was determined by dividing the number of patients with in-hospital cardiac arrest who survived to hospital discharge by the number of patients with an arrest. The incidence rate for cardiac arrest at each hospital was determined by dividing the number of arrest cases by the number of total hospital admissions (expressed as cases per 1000 admissions) during the hospital’s period of participation in the registry. This latter variable was obtained by linking hospitals within GWTG-Resuscitation with data from the American Hospital Association, which provides the total number of admissions annually at each hospital. If a hospital participated for only part of the year (e.g., enrollment year), the total number of admissions was prorated by the hospital’s length of participation within GWTG-Resuscitation for that year.
Study Variables
A number of patient- and hospital-level factors were collected for this study. Patient factors within GWTG-Resuscitation included age; race (white, black, other); sex; initial cardiac arrest rhythm (asystole, pulseless electrical activity, ventricular fibrillation, pulseless ventricular tachycardia); year of admission; location of arrest (intensive care unit, monitored unit, non-monitored unit, emergency department, other); and time of arrest (night vs. day; weekend vs. weekday).8 In addition, the registry collected information on the presence or absence of the following conditions within 24 hours of the cardiac arrest: heart failure; myocardial infarction or ischemia; arrhythmia; hypotension; renal, hepatic or respiratory insufficiency; diabetes mellitus; metabolic or electrolyte abnormality; acute central nervous system event (stroke or other); pneumonia; septicemia; major trauma; and malignancy.
Information on several hospital factors were also obtained from the American Hospital Association. These included a hospital’s teaching status (major, minor, non-teaching), ownership (non-profit, public, private), location (urban vs. rural), geographic region (North and Mid-Atlantic, South and Atlantic, North Central, South Central, Mountain/Pacific), certification status as a trauma center, and number of beds (<200, 200-349, 350-499, 500+), as well as the ratio of full-time-equivalent registered nurses to beds at the hospital. Finally we also obtained information on a hospital’s case mix index - a composite measure of patients’ illness severity for all Medicare discharges (not simply those with an inpatient cardiac arrest) - from the Centers for Medicare and Medicaid Services (CMS).14
Statistical Analyses
To describe patient and hospital characteristics, we categorized the study sample by hospital quintiles of cardiac arrest incidence. Trends across hospital quintiles for continuous variables were examined using the linear trend test, and for categorical variables using the Mantel-Haenszel trend test.
We then examined the correlation between a hospital’s incidence rate and case-survival rate for cardiac arrest with sequential multivariable models. First, the correlation between a hospital’s unadjusted incidence rate and its unadjusted case-survival rate was examined using ordinary linear models.
Next, we examined the correlation between a hospital’s risk-adjusted incidence rate and risk-adjusted case-survival rate, after adjusting for patient factors only. This analysis is the main analysis for this study. To complete this analysis, both hospital rates were risk-adjusted for differences in patient case-mix across hospitals. To determine risk-adjusted incidence rates, we first estimated predicted incidence rates using a random effects logistic model for incidence rates. In this model, we adjusted for a hospital’s CMS case mix index, allowing us to control for differences in illness severity for all admitted patients among hospitals. For each hospital, we then calculated risk-adjusted incidence rates as follows: ([predicted incidence rate at the hospital /expected incidence rate for the same hospital)*average unadjusted incidence rate for our entire hospital sample. This approach is the same as that taken to calculate risk-adjusted case-survival rates (see below), leading to shrinkage of incidence rate estimates toward the global mean for hospitals with fewer patients.
Risk-adjusted cardiac arrest case-survival rates at hospitals were estimated using multivariable hierarchical logistic regression models, with survival to discharge as the dependent variable. We employed 2-level hierarchical models to adjust for clustering of outcomes within hospitals, with individual hospitals modeled as random effects and patient characteristics (collected by GWTG-Resuscitation and described in the Study Variables section) modeled as fixed effects within each hospital.15 From the multivariable model, we used hospital-specific random slope coefficients to calculate risk-adjusted case-survival rates as follows: (predicted case-survival rate at a hospital/expected case-survival rate at the same hospital)*average case-survival rate at all hospitals in our sample. This model is similar to one that has been used by others to calculate risk-standardized mortality rates for other conditions.16
If a significant correlation was found between a hospital’s cardiac arrest incidence rate and case-survival rate even after adjusting for patient case-mix, we determined a priori to conduct a mediation analysis to assess whether certain hospital factors accounted for this relationship. This was evaluated by examining the correlation between a hospital’s incidence rate and case-survival rate after additionally adjusting for hospital factors (described in the Study Variables section) in our regression models for hospital incidence and case-survival rates. We then systematically adjusted for all patient factors and each hospital factor individually in our final models to assess whether any single hospital factor accounted for a substantial proportion of the correlation between these 2 hospital rates (i.e., led to a significant attenuation of any observed correlations).
Overall, missing data rates were low. At least one covariate was missing for 8.1% of the patients, and two covariates were missing for 0.2% of patients. The most common variables with missing data were race (6.9%) and nighttime arrest (1.2%). These data were assumed to be missing at random and were imputed using IVEware software.17 Five imputed data sets were generated and were pooled for the imputed results. Results with and without imputation were not meaningfully different, so only the former are presented. Finally, we repeated the correlation analyses above using restricted cubic splines and found no evidence for a non-linear relationship in our models (p-value of 0.55 in the model adjusted for patient factors, and 0.90 in the model adjusted for patient and hospital factors).
All statistical analyses were conducted using SAS Version 9.1.3 (SAS Institute, Cary, NC), IVEware (University of Michigan, MI), and R Version 2.6.0 (Free Software Foundation, Boston, MA). All tests for statistical significance were 2-tailed and were evaluated at a significance level of 0.05. The Institutional Review Board at the Mid-America Heart Institute waived the requirement for informed consent, as the study used de-identified data.
Outcome Sciences, Inc. serves as the data collection (through their Patient Management Tool – PMT) and coordination center for GWTG-Resuscitation. The University of Pennsylvania serves as the data analytic center and prepared the data for research purposes. All analyses for this study were performed at the Mid-America Heart Institute.
Results
Among 102,153 patients with an in-hospital cardiac arrest, the overall case-survival rate was 19.2%. At the patient level, the overall cardiac arrest incidence rate was 4.54 per 1000 admissions.
Across the 358 hospitals, the median cardiac arrest incidence rate across the hospitals was 4.02 per 1000 admissions (interquartile range [IQR]: 2.95 to 5.65 per 1000 admissions; range, 0.90 to 18.4 per 1000 admissions) (Figure 2A). Patient and event characteristics differed across hospital quintiles of incidence rates (Tables 1A and 1B). Compared with patients at hospitals with the highest cardiac arrest incidence rates, patients at hospitals with lower incidence rates were more likely to be white, and have an initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia. Moreover, patients at hospitals with lower incidence rates were less likely to have certain conditions, such as renal insufficiency, hepatic insufficiency, and respiratory insufficiency. Table 1C describes the characteristics of hospitals, stratified by hospital quintile of incidence rates. Compared with hospitals in the lowest quintile of cardiac arrest incidence, hospitals in the highest quintile were more likely to be non-profit, have higher nurse-to-bed ratios, and possess a larger number of beds.
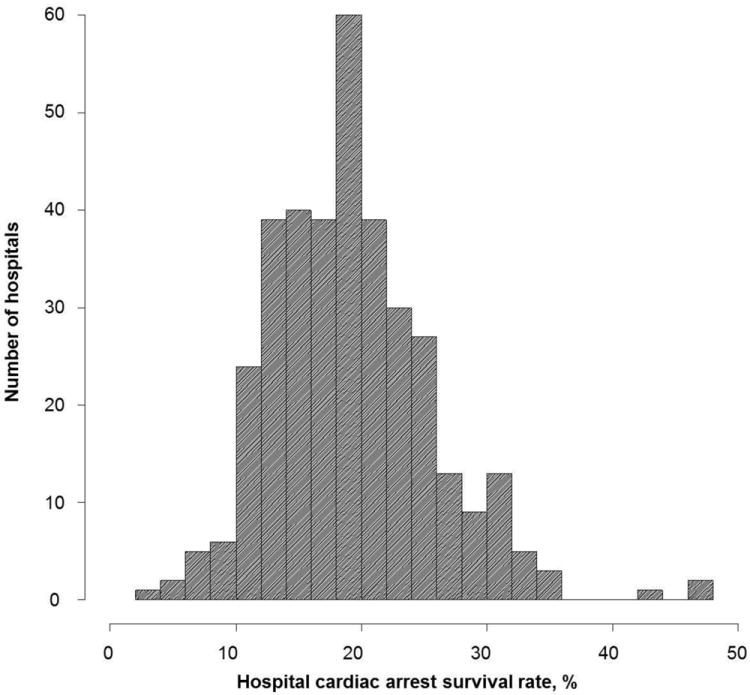
Figure 2.
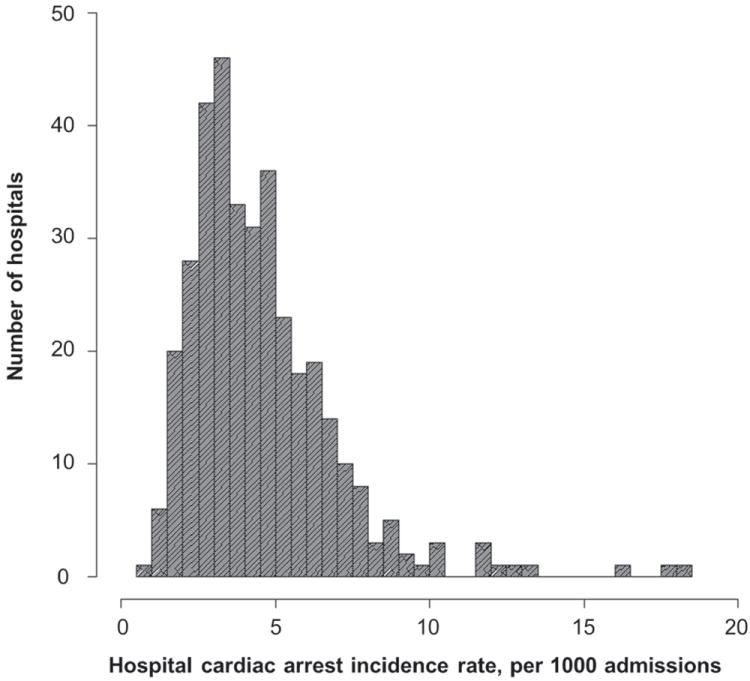
A. Distribution of unadjusted hospital rates of cardiac arrest incidence
B. Distribution of unadjusted hospital rates of in-hospital case-survival
Table 1.
A. Patient characteristics, stratified by quintiles of hospital cardiac arrest incidence rates
| Quintiles of Cardiac Arrest Incidence Rates
|
||||||
|---|---|---|---|---|---|---|
| Very Low | Low | Average | High | Very High | ||
| (n = 10702) | (n = 17321) | (n = 19686) | (n = 22833) | (n = 31611) | P-Value* | |
| (N = 71) | (N = 72) | (N = 71) | (N = 72) | (N = 72) | ||
|
| ||||||
| Cardiac Arrest Incidence Rates, % | 0.9 to <2.8 | 2.8 to <3.5 | 3.5 to <4.6 | 4.6 to <6.1 | 6.1 to 18.4 | |
| Patient Characteristics | ||||||
| Demographics | ||||||
| Age | 0.07 | |||||
| Mean ± SD | 66.0 ± 16.0 | 66.4 ± 15.7 | 66.3 ± 16.2 | 66.7 ± 15.5 | 65.5 ± 15.9 | |
| Median (IQR) | 68.0 (56.0, 78.0) | 69.0 (56.0, 79.0) | 69.0 (56.0, 79.0) | 69.0 (57.0, 78.0) | 67.0 (55.0, 78.0) | |
| Sex | 0.053 | |||||
| Male | 6340 (59.2) | 9953 (57.5) | 11378 (57.8) | 12971 (56.8) | 18812 (59.5) | |
| Female | 4361 (40.8) | 7368 (42.5) | 8308 (42.2) | 9862 (43.2) | 12799 (40.5) | |
| Race | < 0.001 | |||||
| White | 7398 (80.9) | 12138 (78.0) | 15023 (80.6) | 16833 (77.4) | 19728 (65.7) | |
| Black | 1221 (13.4) | 2616 (16.8) | 2866 (15.4) | 4413 (20.3) | 8979 (29.9) | |
| Other | 527 (5.8) | 817 (5.2) | 747 (4.0) | 494 (2.3) | 1302 (4.3) | |
| Pre-Existing Conditions | ||||||
| Heart failure this admission | 1704 (15.9) | 2757 (15.9) | 3308 (16.8) | 4872 (21.3) | 5980 (18.9) | < 0.001 |
| Heart failure prior to admission | 2264 (21.2) | 3448 (19.9) | 4110 (20.9) | 5429 (23.8) | 6611 (20.9) | 0.002 |
| MI/ischemia this admission | 1657 (15.5) | 3103 (17.9) | 3698 (18.8) | 4738 (20.8) | 5751 (18.2) | < 0.001 |
| MI/ischemia prior to admission | 1730 (16.2) | 2779 (16.0) | 3753 (19.1) | 4442 (19.5) | 4987 (15.8) | 0.90 |
| Arrhythmia | 3409 (31.9) | 5693 (32.9) | 6635 (33.7) | 8087 (35.4) | 10669 (33.8) | < 0.001 |
| Hypotension/hypoperfusion | 3029 (28.3) | 4533 (26.2) | 5632 (28.6) | 6701 (29.3) | 9200 (29.1) | < 0.001 |
| Respiratory insufficiency | 4068 (38.0) | 6818 (39.4) | 8541 (43.4) | 9501 (41.6) | 14060 (44.5) | < 0.001 |
| Renal insufficiency | 3275 (30.6) | 5555 (32.1) | 6256 (31.8) | 7669 (33.6) | 11051 (35.0) | < 0.001 |
| Hepatic insufficiency | 750 (7.0) | 1187 (6.9) | 1538 (7.8) | 1615 (7.1) | 2617 (8.3) | < 0.001 |
| Metabolic/electrolyte abnormality | 1653 (15.4) | 2892 (16.7) | 3639 (18.5) | 4207 (18.4) | 5376 (17.0) | 0.001 |
| Diabetes mellitus | 2973 (27.8) | 5134 (29.6) | 5623 (28.6) | 7280 (31.9) | 9772 (30.9) | < 0.001 |
| Baseline depression in CNS function | 1267 (11.8) | 1817 (10.5) | 2559 (13.0) | 3069 (13.4) | 4501 (14.2) | < 0.001 |
| Acute stroke | 403 (3.8) | 600 (3.5) | 855 (4.3) | 884 (3.9) | 1353 (4.3) | < 0.001 |
| Acute CNS non-stroke event | 873 (8.2) | 1141 (6.6) | 1443 (7.3) | 2151 (9.4) | 2702 (8.5) | < 0.001 |
| Pneumonia | 1245 (11.6) | 2180 (12.6) | 2351 (11.9) | 3257 (14.3) | 4613 (14.6) | < 0.001 |
| Septicemia | 1464 (13.7) | 2534 (14.6) | 3138 (15.9) | 3403 (14.9) | 5413 (17.1) | < 0.001 |
| Major trauma | 453 (4.2) | 500 (2.9) | 891 (4.5) | 730 (3.2) | 1511 (4.8) | < 0.001 |
| Metastatic/hematologic malignancy | 1316 (12.3) | 2141 (12.4) | 2539 (12.9) | 2550 (11.2) | 4005 (12.7) | 0.84 |
| Interventions in Place† | ||||||
| Assisted/mechanical ventilation | 2700 (25.2) | 4735 (27.3) | 6249 (31.7) | 6761 (29.6) | 10399 (32.9) | < 0.001 |
| Invasive airway | 2755 (25.8) | 4560 (26.3) | 6089 (30.9) | 6440 (28.2) | 10637 (33.7) | < 0.001 |
| Pacemaker | 679 (6.3) | 1161 (6.7) | 1357 (6.9) | 1694 (7.4) | 2152 (6.8) | 0.050 |
| IV/IO antiarrhythmics | 611 (5.7) | 1013 (5.8) | 1358 (6.9) | 1222 (5.4) | 1750 (5.5) | 0.01 |
| IV/IO vasoactive agents | 2583 (24.2) | 4494 (25.9) | 5583 (28.4) | 5928 (26.0) | 9021 (28.5) | < 0.001 |
| Dialysis/extracorporeal filtration | 354 (3.3) | 603 (3.5) | 885 (4.5) | 683 (3.0) | 1406 (4.4) | < 0.001 |
|
B. Event characteristics, stratified by quintiles of hospital cardiac arrest incidence rates
| ||||||
| Event Characteristics | ||||||
| Admission year | < 0.001 | |||||
| 2000 | 147 (1.4) | 150 (0.9) | 316 (1.6) | 470 (2.1) | 751 (2.4) | |
| 2001 | 629 (5.9) | 885 (5.1) | 1226 (6.2) | 1361 (6.0) | 1157 (3.7) | |
| 2002 | 1015 (9.5) | 1561 (9.0) | 1836 (9.3) | 2220 (9.7) | 2165 (6.9) | |
| 2003 | 1272 (11.9) | 2267 (13.1) | 2185 (11.1) | 2777 (12.2) | 3317 (10.5) | |
| 2004 | 1374 (12.9) | 2209 (12.8) | 2347 (11.9) | 2911 (12.8) | 3883 (12.3) | |
| 2005 | 1294 (12.1) | 2229 (12.9) | 2760 (14.0) | 2887 (12.6) | 4137 (13.1) | |
| 2006 | 1488 (13.9) | 2350 (13.6) | 2444 (12.4) | 2614 (11.5) | 4119 (13.0) | |
| 2007 | 1367 (12.8) | 1766 (10.2) | 2478 (12.6) | 2842 (12.5) | 4512 (14.3) | |
| 2008 | 1334 (12.5) | 2181 (12.6) | 2604 (13.2) | 2841 (12.4) | 4491 (14.2) | |
| 2009 | 763 (7.1) | 1709 (9.9) | 1465 (7.5) | 1900 (8.3) | 3070 (9.7) | |
| Night | 3421 (32.5) | 5735 (33.5) | 6352 (32.6) | 7251 (32.2) | 10006 (32.0) | 0.01 |
| Location | < 0.001 | |||||
| ICU | 4873 (45.6) | 8164 (47.2) | 9640 (49.0) | 10074 (44.1) | 15001 (47.5) | |
| Monitored unit | 1576 (14.7) | 2974 (17.2) | 2851 (14.5) | 3642 (16.0) | 4489 (14.2) | |
| Non-monitored unit | 2288 (21.4) | 3184 (18.4) | 3549 (18.1) | 4393 (19.2) | 5632 (17.8) | |
| Emergency | 1057 (9.9) | 1597 (9.2) | 1833 (9.3) | 2583 (11.3) | 3813 (12.1) | |
| Others | 902 (8.4) | 1395 (8.1) | 1789 (9.1) | 2137 (9.4) | 2659 (8.4) | |
| Weekend | 3297 (30.8) | 5398 (31.2) | 6092 (30.9) | 7005 (30.7) | 9757 (30.9) | 0.65 |
| Hospital-wide response activated | 8773 (82.0) | 14171 (81.8) | 15743 (80.0) | 17751 (77.7) | 23429 (74.1) | < 0.001 |
| Compressions | 10345 (96.7) | 16807 (97.0) | 19200 (97.5) | 22154 (97.0) | 30668 (97.0) | 0.55 |
| Automated External Defibrillator applied | < 0.001 | |||||
| Yes | 1466 (13.7) | 1835 (10.6) | 1696 (8.6) | 2712 (11.9) | 3986 (12.6) | |
| No/none | 9236 (86.3) | 15486 (89.4) | 17987 (91.4) | 20121 (88.1) | 27625 (87.4) | |
| Initial Rhythm | < 0.001 | |||||
| Asystole | 3762 (35.2) | 6053 (34.9) | 7264 (36.9) | 8027 (35.2) | 11829 (37.4) | |
| PEA | 4215 (39.4) | 7115 (41.1) | 8045 (40.9) | 9704 (42.5) | 13239 (41.9) | |
| VF | 1816 (17.0) | 2638 (15.2) | 2800 (14.2) | 3269 (14.3) | 4202 (13.3) | |
| PVT | 909 (8.5) | 1515 (8.7) | 1577 (8.0) | 1833 (8.0) | 2341 (7.4) | |
| Defibrillation/shock provided | 4322 (91.6) | 6922 (92.2) | 7664 (94.0) | 8855 (94.1) | 11909 (93.0) | < 0.001 |
| Cerebral Perfusion Category† | < 0.001 | |||||
| 1 | 5381 (57.1) | 8572 (57.1) | 7710 (47.9) | 10636 (51.3) | 12509 (48.4) | |
| 2 | 2443 (25.9) | 3895 (26.0) | 5172 (32.1) | 5987 (28.9) | 7381 (28.5) | |
| 3 | 1111 (11.8) | 1668 (11.1) | 2153 (13.4) | 2725 (13.1) | 3925 (15.2) | |
| 4 | 488 (5.2) | 869 (5.8) | 1062 (6.6) | 1393 (6.7) | 2038 (7.9) | |
|
C. Hospital characteristics, stratified by quintiles of hospital cardiac arrest incidence rates
| ||||||
| Hospital Characteristics | ||||||
| Teaching status | 0.98 | |||||
| Major teaching | 18 (25.4) | 16 (22.2) | 16 (22.5) | 12 (16.7) | 21 (29.2) | |
| Minor teaching | 21 (29.6) | 25 (34.7) | 22 (31.0) | 21 (29.2) | 22 (30.6) | |
| Non-teaching | 32 (45.1) | 31 (43.1) | 33 (46.5) | 39 (54.2) | 29 (40.3) | |
| Member of Council of Teaching Hospitals | 18 (25.4) | 16 (22.2) | 16 (22.5) | 12 (16.7) | 21 (29.2) | 0.89 |
| Trauma center | 0.36 | |||||
| No | 31 (43.7) | 27 (37.5) | 27 (38.0) | 36 (50.0) | 27 (37.5) | |
| Yes | 33 (46.5) | 42 (58.3) | 41 (57.7) | 29 (40.3) | 32 (44.4) | |
| Unknown | 7 (9.9) | 3 (4.2) | 3 (4.2) | 7 (9.7) | 13 (18.1) | |
| Ownership | 0.03 | |||||
| Non-Profit | 56 (78.9) | 54 (75.0) | 52 (73.2) | 52 (72.2) | 43 (59.7) | |
| Public | 10 (14.1) | 9 (12.5) | 7 (9.9) | 12 (16.7) | 17 (23.6) | |
| Private | 5 (7.0) | 9 (12.5) | 12 (16.9) | 8 (11.1) | 12 (16.7) | |
| Region | 0.93 | |||||
| North and Mid-Atlantic | 15 (21.1) | 11 (15.3) | 10 (14.1) | 6 (8.3) | 6 (8.3) | |
| South and Atlantic | 12 (16.9) | 20 (27.8) | 19 (26.8) | 23 (31.9) | 22 (30.6) | |
| North Central | 15 (21.1) | 17 (23.6) | 16 (22.5) | 21 (29.2) | 10 (13.9) | |
| South Central | 7 (9.9) | 13 (18.1) | 12 (16.9) | 13 (18.1) | 25 (34.7) | |
| Mountain/Pacific | 22 (31.0) | 11 (15.3) | 14 (19.7) | 9 (12.5) | 9 (12.5) | |
| Urban | 64 (90.1) | 69 (95.8) | 63 (88.7) | 61 (84.7) | 68 (94.4) | 0.82 |
| Full-time equivalent nurse ratio | 0.02 | |||||
| <1.5 | 22 (31.0) | 19 (26.4) | 28 (39.4) | 40 (55.6) | 31 (43.1) | |
| 1.5<2 | 26 (36.6) | 30 (41.7) | 18 (25.4) | 14 (19.4) | 23 (31.9) | |
| 2-<2.5 | 14 (19.7) | 17 (23.6) | 18 (25.4) | 13 (18.1) | 13 (18.1) | |
| 2.5+ | 9 (12.7) | 6 (8.3) | 7 (9.9) | 5 (6.9) | 5 (6.9) | |
| Number of beds | 0.03 | |||||
| <200 | 13 (18.3) | 13 (18.1) | 17 (23.9) | 15 (20.8) | 19 (26.4) | |
| 200-349 | 23 (32.4) | 24 (33.3) | 19 (26.8) | 35 (48.6) | 26 (36.1) | |
| 350-499 | 15 (21.1) | 18 (25.0) | 15 (21.1) | 11 (15.3) | 13 (18.1) | |
| 500+ | 20 (28.2) | 17 (23.6) | 20 (28.2) | 11 (15.3) | 14 (19.4) | |
| Case mix index | 0.15 | |||||
| Mean ± SD | 1.5 ± 0.2 | 1.5 ± 0.2 | 1.6 ± 0.2 | 1.5 ± 0.3 | 1.6 ± 0.2 | |
| Median (IQR) | 1.5 (1.3, 1.7) | 1.5 (1.4, 1.7) | 1.5 (1.4, 1.7) | 1.5 (1.3, 1.6) | 1.6 (1.4, 1.7) | |
Abbreviations: N is number of hospitals; n is number of patients; SD is standard deviation; IQR is interquartile range; MI is myocardial infarction; CNS is central nervous system; IV/IO is intravenous/intraosseous
Continuous variables compared using linear trend test. Categorical variables compared using Mantel-Haenszel trend test
Interventions in Place refers to interventions already in place when need for chest compressions and/or defibrillation first recognized
Abbreviations: N is number of hospitals; n is number of patients; SD is standard deviation; IQR is interquartile range; ICU is intensive care unit; PEA is pulseless electrical activity; VF is ventricular fibrillation; PVT is pulseless ventricular tachycardia; ROSC is return of spontaneous circulation
Cerebral perfusion category (on admission) definitions: 1 is good cerebral performance, 2 is moderate cerebral disability, 3 is severe cerebral disability, 4 is coma or vegetative state, and 5 is brain death
Abbreviations: N is number of hospitals; n is number of patients; SD is standard deviation; IQR is inter-quartile range
Association between Hospital Rates of Cardiac Arrest Incidence and Survival
The median cardiac arrest case-survival rate was 18.8% (IQR: 14.5% to 22.6%; range, 2.5% to 46.9%) (Figure 2B). In unadjusted analysis, there was a significant negative correlation between a hospital’s case-survival rate and incidence rate (correlation of -0.16, P=0.003) (Figure 3A). This suggests that hospitals with high case-survival rates for in-hospital cardiac arrest also had lower cardiac arrest incidence rates, and hospitals with low case-survival rates had higher cardiac arrest incidence rates. Notably, the negative correlation between these 2 rates was minimally changed after adjusting for differences in patient case-mix (correlation of -0.15, P=0.004) (Figure 3B). In sensitivity analyses excluding three outliers with a crude incidence rate of >15 per 1000 admissions, our results were similar (correlation of -0.15, P=0.005).
Figure 3.
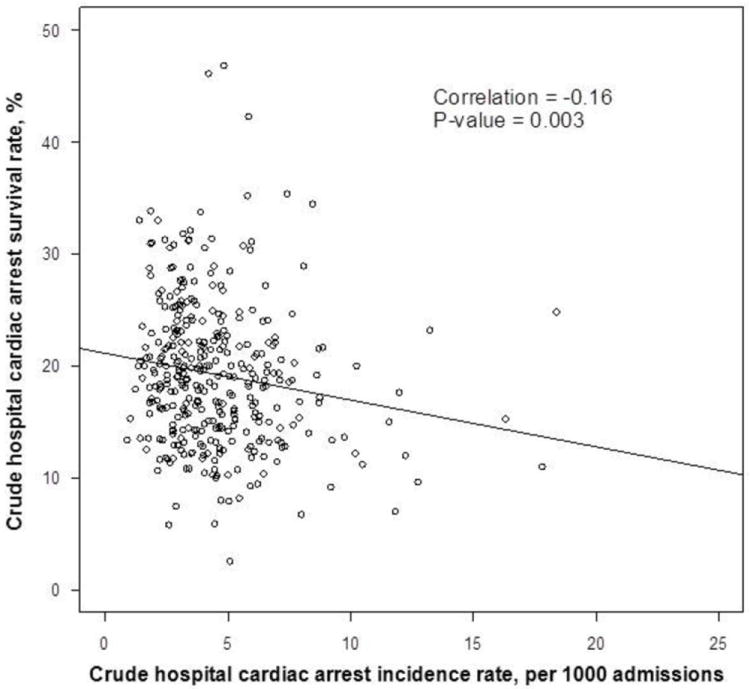
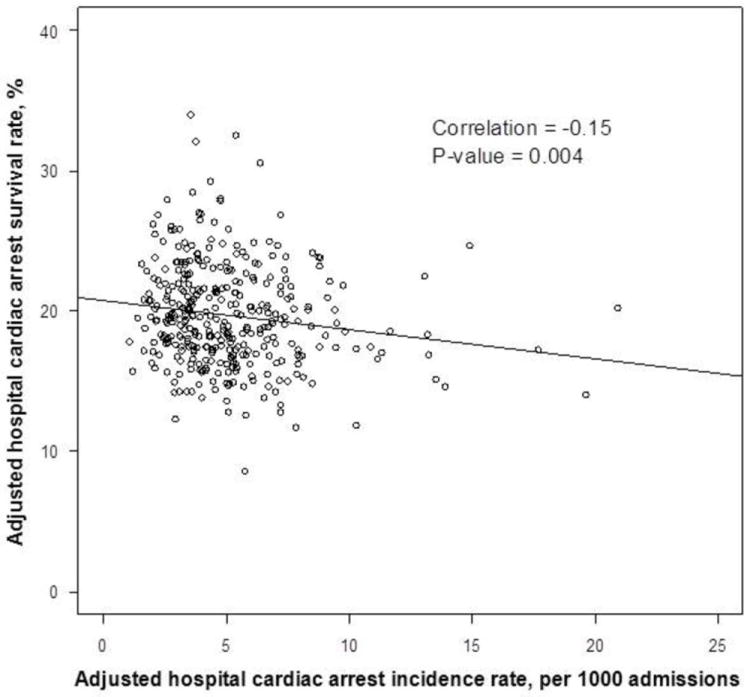
A. Correlation between unadjusted hospital rates of cardiac arrest incidence and case-survival
B. Correlation between hospital rates of cardiac arrest incidence and case-survival, adjusted for patient factors only
Incidence is adjusted for the CMS case mix index for hospital admissions, and case-survival is adjusted for patient factors (i.e., age, gender, race/ethnicity, pre-existing conditions), including event characteristics (i.e., initial arrest rhythm, year of admission, night vs. day, weekend vs. weekday).
Finally, we examined whether hospital factors mediated the relationship between a hospital’s cardiac arrest incidence and case-survival rate. Adjustment for hospital and patient characteristics led to a significant attenuation of the relationship between these two rates (correlation of -0.07, P=0.18) (Figure 4). This suggests that the correlation between cardiac arrest incidence and case-survival was partly attributable to the hospital factors in the model. In sensitivity analyses excluding three outliers with a crude incidence rate of >15 per 1000 admissions, our results were similar (correlation of -0.08, P=0.13). In further exploratory analyses, each hospital factor led to some attenuation of the relationship between a hospital’s cardiac arrest case-survival and incidence rates (Table 2). The largest attenuation (i.e., the greatest shift in the correlation estimate from a negative to a positive direction) occurred after adjusting solely for geographical region or a hospital’s nurse-to-bed ratio.
Figure 4. Mediation analysis of hospital factors which may account for the correlation between hospital rates of cardiac arrest incidence and case-survival.
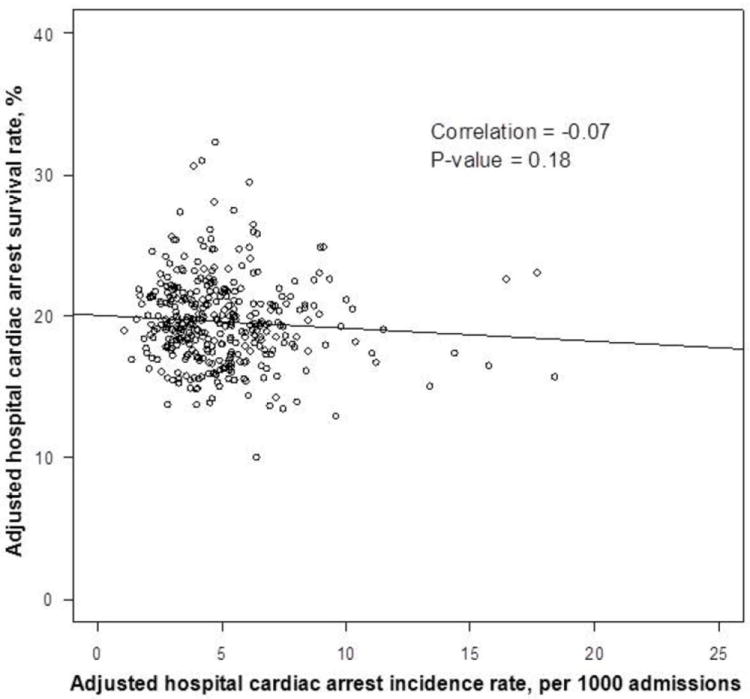
Regression models were adjusted for both patient and hospital factors to determine if certain hospital factors may, in part, mediate this relationship. Incidence is adjusted for the CMS case mix index for hospital admissions and hospital factors (i.e., teaching status, ownership, geographical region, urban vs. rural, full-time equivalent nurse ratio, number of beds, certification as a trauma center). Case-survival is adjusted for case mix index, patient factors, and the hospital factors described above.
Table 2.
Mediation analysis of hospital factors which may account for the correlation between hospital rates of cardiac arrest incidence and case-survival
| Adjusted Models | Correlation | P-value |
|---|---|---|
| No Adjustment Factors | -0.16 | 0.003 |
| Patient Case-Mix | -0.15 | 0.004 |
|
| ||
| Mediation Analysis | Correlation | P-value |
|
| ||
| Patient Case-Mix and All Hospital Factors Together | -0.07 | 0.18 |
| Patient Case-Mix and All Hospital Factors One-by-One | ||
| Urban vs. rural | -0.15 | 0.004 |
| Teaching status | -0.15 | 0.004 |
| Hospital beds | -0.15 | 0.004 |
| Trauma center | -0.14 | 0.01 |
| Ownership | -0.13 | 0.01 |
| Nurse-to-bed ratio | -0.12 | 0.02 |
| Region | -0.12 | 0.03 |
Comment
As the country works to increase its ability to measure and distinguish hospitals on the basis of quality, cardiac arrest survival has emerged as a potential performance measure. However, it is important to ensure that this measure does not “reward” hospitals that do a poorer job of preventing cardiac arrests, thus artificially appearing to have higher survival rates. In a large national registry of in-hospital cardiac arrest, we found substantial variation in rates of cardiac arrest incidence and case-survival across hospitals. There was a sizable negative correlation between a hospital’s incidence and case-survival rates for cardiac arrest, suggesting that hospitals that have higher survival rates after cardiac arrest also have lower cardiac arrest incidence rates. This correlation persisted after adjustment for patient factors. These findings suggest that cardiac arrest case-survival rates are not confounded by incidence rates, as a positive correlation between the two was not observed; therefore, a focus on comparing case-survival rates across similar hospitals would be a useful hospital quality performance measure. Furthermore, we found that additional adjustment for certain hospital factors significantly attenuated the negative correlation between incidence and case-survival, thereby suggesting that these hospital factors may, in part, mediate (and explain) why some hospitals are better at both preventing and treating in-hospital cardiac arrest.
Most prior studies of in-hospital cardiac arrest have examined case-survival and incidence rates independently of one another. For instance, prior work has found that case-survival rates differ by time of arrest (i.e., nights or weekends),8 arrest location, initial cardiac arrest rhythm,9,18 time to defibrillation,4 and processes of care during acute resuscitation (e.g., delays in medication administration).7,19 Others have reported that hospitals with urban locations, a higher proportion of black patients, and fewer hospital beds have higher rates of cardiac arrest incidence.20
Together, the hospital factors we examined appeared, in part, to mediate the relationship between a hospital’s incidence and case-survival rate for cardiac arrest. For example, the correlation between incidence and case-survival decreased by one-quarter when comparing hospitals with similar nurse staffing. This suggests that care in certain types of hospitals (e.g. hospitals with higher nurse staffing) may be associated with both decreased cardiac arrest incidence and improved survival to discharge. In fact, prior studies have demonstrated an association between registered nurse staffing and lower rates of mortality and adverse events.21 Additional studies are needed to understand whether or not a causal relationship exists between nurse staffing and cardiac arrest outcomes, and to identify other modifiable factors that may mediate the relationship between hospital rates of case-survival and cardiac arrest incidence.
It is important to acknowledge that the overarching goal of many clinicians and policymakers is to reduce the mortality rate from in-hospital cardiac arrest for all hospital admissions – a goal that can be achieved either by lowering the incidence rate, increasing case survival, or both. However, given limited resources for measurement development and collection, as well as inherent difficulties in capturing the true case mix for all hospital admissions (the denominator for cardiac arrest incidence), we believe our results support the pragmatic approach already taken by others to focus on case-survival as an initial measure of hospital performance for in-hospital cardiac arrest. Future efforts to identify factors that distinguish high-performing hospitals from low-performing hospitals would benefit from examining the relationship of hospital factors to both cardiac arrest incidence and case-survival.
Our study had several potential limitations. First, although we were able to adjust for a number of patient and hospital factors, the possibility of unmeasured confounding in our use of registry data exists. Second, our sample was restricted to hospitals that participated in GWTG-Resuscitation; therefore, our findings may not be generalizable to all hospitals. Third, we were able to examine only a handful of hospital factors, and we did not have specific information on nurse and physician staff experience and training, nor on quality improvement resuscitation programs implemented by a hospital (e.g., mock codes, debriefing after codes, rapid response teams, increased use of telemetry, and remote intensive care unit monitoring, etc.). Finally, our data lacked information about variation in hospital practices concerning end-of-life care. In particular, some hospitals may be more aggressive about obtaining DNR orders for patients with a poor prognosis. These hospitals may have lower incidence rates and higher case-survival rates than their peers. Furthermore, while we excluded patients with DNR orders from the numerator for cardiac arrest incidence rate, we did not have data to exclude all patients with DNR orders from the denominator for our incidence rate. Thus, we may have overestimated the correlation between unadjusted incidence and case-survival.
In summary, we found that a significant negative correlation exists between a hospital’s incidence and case-survival rates for in-hospital cardiac arrest. Hospitals that excelled at preventing cardiac arrests also had higher survival rates for cardiac arrest cases, and this correlation persisted after adjustment of patient case mix. We found evidence that certain hospital factors, in part, mediated this relationship, but only one of the factors we examined —a hospital’s nurse-to-bed ratio — is potentially quickly modifiable. Future studies are needed to determine which hospital factors are surrogate markers of a hospital’s resuscitation performance and which may lead to improvements in cardiac arrest incidence and case-survival.
Supplementary Material
Appendix Figure 1. Correlation between hospital rates of cardiac arrest incidence and case-survival, adjusted for patient factors only, after excluding three outliers
Incidence is adjusted for the CMS case mix index for hospital admissions, and case-survival is adjusted for patient factors (i.e., age, gender, race/ethnicity, pre-existing conditions), including event characteristics (i.e., initial arrest rhythm, year of admission, night vs. day, weekend vs. weekday).
Appendix Figure 2. Mediation analysis of hospital factors which may account for the correlation between hospital rates of cardiac arrest incidence and case-survival, after excluding three outliers
Regression models were adjusted for both patient and hospital factors to determine if certain hospital factors may, in part, mediate this relationship. Incidence is adjusted for the CMS case mix index for hospital admissions and hospital factors (i.e., teaching status, ownership, geographical region, urban vs. rural, full-time equivalent nurse ratio, number of beds, certification as a trauma center). Case-survival is adjusted for case mix index, patient factors, and the hospital factors described above.
Acknowledgments
We thank Mary Jane Giesey, BA, for the research assistance she provided. She was compensated for her work.
Study concept and design: Chen, Chan
Acquisition of data: Chen, Chan
Drafting of the manuscript: Chen, Chan
Revision of the manuscript for important intellectual content: Chen, Nallamothu, Spertus, Li, Chan
Statistical analysis: Chen, Li, Chan
Obtained funding: N/A
Administrative, technical or material support: N/A
Study supervision: Chan
Funding/support: Dr. Chan is supported by a Career Development Grant Award (K23HL102224) from the National Heart Lung and Blood Institute. Dr. Chen is supported by a Career Development Grant Award (K08HS020671) from the Agency for Healthcare Research and Quality. GWTG-Resuscitation is sponsored by the American Heart Association, which had no role in the study design, data analysis or manuscript preparation and revision. This material is the result of work supported with resources of the VA Health Services Research and Development Center for Clinical Management Research, VA Ann Arbor Healthcare System.
Footnotes
Author contributions: Dr. Chen had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial disclosures: I need to consult my co-authors about potential conflicts of interest and will provide details on the journal’s financial disclosure form or in an attachment to the form.
References
- 1.Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011 Jun 23; doi: 10.1097/CCM.0b013e3182257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009 Jul 2;361(1):22–31. doi: 10.1056/NEJMoa0810245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brady WJ, Gurka KK, Mehring B, Peberdy MA, O’Connor RE. American Heart Association’s Get with the Guidelines I. In-hospital cardiac arrest: impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge. Resuscitation. 2011 Jul;82(7):845–852. doi: 10.1016/j.resuscitation.2011.02.028. [DOI] [PubMed] [Google Scholar]
- 4.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008 Jan 3;358(1):9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 5.Chan PS, Krumholz HM, Spertus JA, et al. Automated external defibrillators and survival after in-hospital cardiac arrest. JAMA. 2010;304(19):2129–2136. doi: 10.1001/jama.2010.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jain R, Nallamothu BK, Chan PS. Body mass index and survival after in-hospital cardiac arrest. Circ Cardiovasc Qual Outcomes. 2010 Aug 10; doi: 10.1161/CIRCOUTCOMES.109.912501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ornato JP, Peberdy MA, Reid RD, Feeser VR, Dhindsa HS, Investigators N. Impact of resuscitation system errors on survival from in-hospital cardiac arrest. Resuscitation. 2012 Jan;83(1):63–69. doi: 10.1016/j.resuscitation.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008 Feb 20;299(7):785–792. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 9.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006 Jan 4;295(1):50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 10.Chan PS, Nallamothu BK. Improving outcomes following in-hospital cardiac arrest: life after death. JAMA. 2012 May 9;307(18):1917–1918. doi: 10.1001/jama.2012.3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003 Sep;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 12.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital “Utstein style”. American Heart Association. Ann Emerg Med. 1997 May;29(5):650–679. doi: 10.1016/s0196-0644(97)70256-7. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004 Nov 23;110(21):3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 14.Medicare Impact Files. [February 15, 2012]; http://www.cms.gov/AcuteInpatientPPS/HIF/list.asp#TopOfPage.
- 15.Goldstein H. Multilevel Statistical Models. London and New York: Edward Arnold; Wiley; 1995. [Google Scholar]
- 16.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006 Apr 4;113(13):1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 17.Raghunathan TE, Solenberger PW, Van Hoewyk J. IVEware: Imputation and Variance Estimation Software - User Guide. Michigan: Survey Research Center, Institute for Social Research; University of Michigan: 2002. [Google Scholar]
- 18.Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010 Jan;38(1):101–108. doi: 10.1097/CCM.0b013e3181b43282. [DOI] [PubMed] [Google Scholar]
- 19.Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007 Feb;33(2):237–245. doi: 10.1007/s00134-006-0326-z. [DOI] [PubMed] [Google Scholar]
- 20.Merchant RM, Yang L, Becker LB, et al. Variability in case-mix adjusted in-hospital cardiac arrest rates. Med Care. 2012 Feb;50(2):124–130. doi: 10.1097/MLR.0b013e31822d5d17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care. 2007 Dec;45(12):1195–1204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Figure 1. Correlation between hospital rates of cardiac arrest incidence and case-survival, adjusted for patient factors only, after excluding three outliers
Incidence is adjusted for the CMS case mix index for hospital admissions, and case-survival is adjusted for patient factors (i.e., age, gender, race/ethnicity, pre-existing conditions), including event characteristics (i.e., initial arrest rhythm, year of admission, night vs. day, weekend vs. weekday).
Appendix Figure 2. Mediation analysis of hospital factors which may account for the correlation between hospital rates of cardiac arrest incidence and case-survival, after excluding three outliers
Regression models were adjusted for both patient and hospital factors to determine if certain hospital factors may, in part, mediate this relationship. Incidence is adjusted for the CMS case mix index for hospital admissions and hospital factors (i.e., teaching status, ownership, geographical region, urban vs. rural, full-time equivalent nurse ratio, number of beds, certification as a trauma center). Case-survival is adjusted for case mix index, patient factors, and the hospital factors described above.


