Abstract
Background
Improving asthma patients’ quality of life is an important clinical outcome. This study evaluated the efficacy of mindfulness-based stress reduction (MBSR) in improving quality of life and lung function in patients with asthma.
Methods
A randomized controlled trial compared an 8 week MBSR group-based program (n = 42) to an educational control program (n = 41) in adults with mild, moderate or severe persistent asthma recruited at a university hospital outpatient primary care and pulmonary care clinic. Primary outcomes were quality of life assessed by the Asthma Quality of Life Questionnaire (AQOL), and lung function assessed by change from baseline in two-week average morning peak expiratory flow (PEF). Secondary outcomes were asthma control assessed by 2007 NIH/NHLBI guidelines, and stress assessed by Perceived Stress Scale. Follow-up assessments were conducted at 10 weeks, 6 and 12 months.
Results
At 12 months MBSR resulted in clinically significant improvements in quality of life (intervention effect 0.55 (95% CI 0.21, 0.89, p=0.001)) and perceived stress (intervention effect −4.5 (95% CI −7.1, −1.9; p= 0.001)). No significant effect was found on lung function (morning PEF, PEF variability, and FEV1). At 12 months the percentage of patients in MBSR with well-controlled asthma showed a non-statistically significant increase (7.3% at baseline to 19.4%) compared to the control condition (7.5% and 7.9%, respectively) (p=0.30).
Conclusions
MBSR produced lasting clinically significant improvements in asthma-related quality of life and stress in patients with persistent asthma, even in the absence of improvements in lung function.
Keywords: Asthma, Complementary Medicine, Perception of Asthma/Breathlessness
INTRODUCTION
Asthma places considerable demands on patients, and interventions to facilitate adjustment to the disease may be important in asthma management and in reducing hospitalizations even when lung function does not improve as a result. [1]
Psychosocial factors also appear to be implicated in asthma. The elevated perceived stress prevalent among asthma patients negatively affects their quality of life (QOL) and is strongly associated with worse asthma control and reduced medication adherence. [2] Psychosocial distress is also associated with over-perceiving dyspnea and self-reported respiratory symptoms not accompanied by objective measures. [3] This is important since to respond appropriately and prevent symptom exacerbations, patients need to be able to discriminate between their asthma symptoms and the affect-related sensations and cognitions related to these. [4]
Despite the importance of coping and the capacity for discrimination, self-management programs typically focus on education about external triggers and medication usage, and no clear benefit has been shown for psychological interventions. [5] Similarly, the complementary and alternative approaches (including biofeedback, relaxation, breathing exercises and yoga) used by 40% of asthma patients have not shown a clear benefit. [6]
Mindfulness training involves learning to recognize and discriminate accurately between the components of experience, such as thoughts, feelings, and sensations, and development of a non-reactive awareness of these. Mindfulness-Based Stress Reduction (MBSR) is a widely-available group-based mindfulness training program that reduces perceived stress, disease-related distress and reported medical symptoms in a range of stress-related disorders and chronic diseases, [7] but it has not been studied for its effect on asthma QOL and management.
We hypothesized that participation in MBSR would result in greater improvements in QOL and lung function at one year follow-up, compared to a condition that controlled for attention, time, and group support.
METHODS
Study Sample
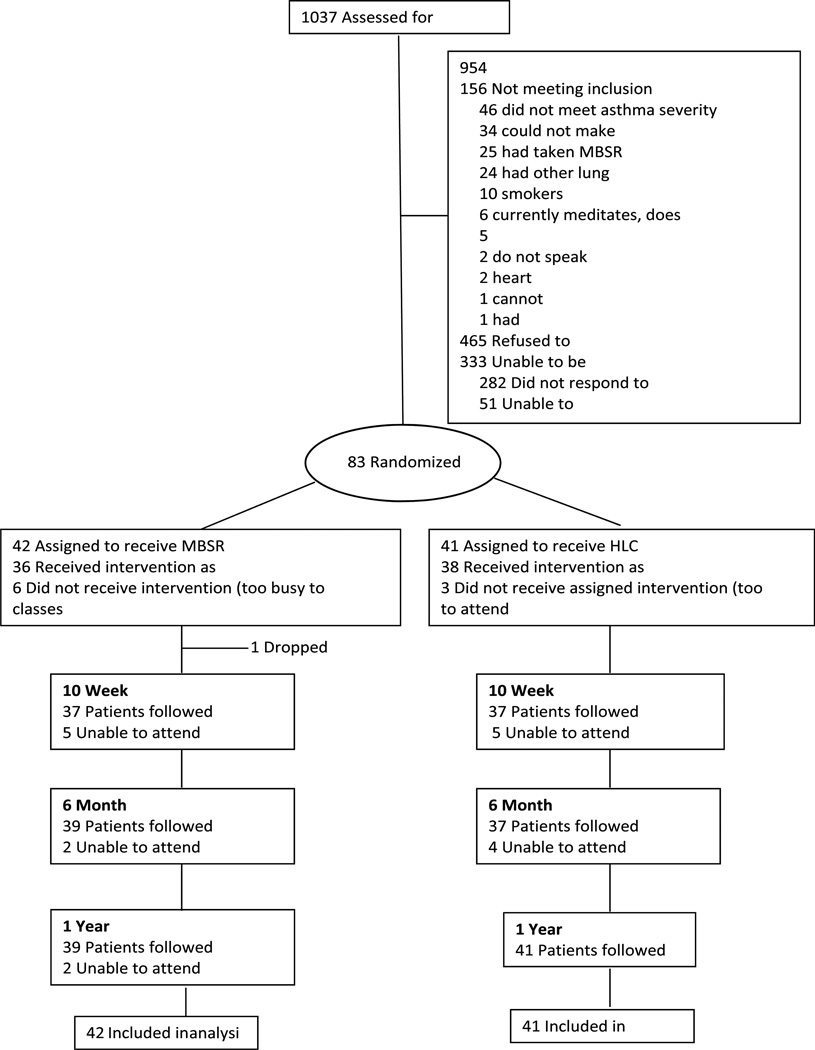
Participants were 83 adult patients with mild, moderate, or severe persistent asthma recruited between October 2006 and December 2007 from outpatient primary care and pulmonary care specialty clinics at UMass Memorial Health Care (UMMHC) in Worcester, Massachusetts. Figure 1 shows 1037 patients were assessed for eligibility: 156 did not meet inclusion criteria; 333 were unable to be contacted; and 465 declined to participate. Forty two were randomly assigned to MBSR; 41 to the Healthy Living Course control. Group assignment was determined by a computer-generated random allocation scheme. Follow-up occurred between April 2007 and February 2008. University of Massachusetts Medical School (UMMS) Institutional Review Board approved the protocol. Participants gave written informed consent, and continued to be medically managed by their own physician.
Figure 1.
Consort Diagram
Inclusion criteria were: (1) physician-documented asthma diagnosis with either an objective indicator of bronchial hyper-responsiveness (positive methacholine challenge test, ≥ 12% improvement in FEV1 or FVC in response to bronchodilator, or 20% variability in diurnal PEF variation) or ≥ 12% improvement in FEV1 in response to inhaled bronchodilator on spirometry conducted at study entry; and (2) met 2007 NIH/NHLBI [8] criteria for mild, moderate, or severe persistent asthma.
Patients were excluded if they: had intermittent asthma (symptoms less than once/week, brief exacerbations, nocturnal symptoms not more than twice/month, and normal lung function between episodes); were current smokers (smoked in past year); had lung diseases besides asthma (e.g., pulmonary hypertension, cystic fibrosis, COPD-emphysema, bronchiectasis, chronic bronchitis); had cancer, except non-melanoma skin cancer; were receiving treatment for symptomatic cardiovascular disease (including congestive heart failure, unstable angina, myocardial infarction in past 6 months); ever had a positive TB test; had psychiatric hospitalization in last 2 years; had participated in MBSR and/or were practicing meditation or yoga on a regular basis.
Intervention Groups
MBSR consisted of eight weekly 2½ hour sessions, and an all-day (six hour) session in the 6th week. [9] To enhance generalizability, participants were integrated into the MBSR groups held regularly at UMMHC, and which included non-study participants. Classes consisted of approximately 2 study and 28 non-study participants. Mindfulness training was through: (a) a body scan in which attention is systematically moved through the body to bring awareness to bodily sensations; (b) sitting meditation focusing on awareness of breathing, thoughts, and emotions; and (c) gentle stretching exercises to develop mindful awareness during movement. The interactive classes provided opportunity for mutual support, and emphasized integration of mindfulness into everyday life to support coping with symptoms and stress. Two CDs containing guided instruction in the mindfulness exercises were provided to be practiced for 30 minutes, 6 days/week.
For this trial we developed a Healthy Living Course (HLC) that matched MBSR for time, instructor attention, and format. Classes consisted of lectures and discussion of topics related to self-care: healthy nutrition; physical activity/fitness; coping with stress (not including mindfulness); how to get a good night’s sleep; balancing work and personal life; and living a drug-free life (smoking, alcohol and other drugs). Behavioral homework was assigned consistent in time with MBSR. To match the mix of participants in the MBSR program, the HLC was offered to community members in addition to study participants. Classes consisted of approximately 7 study participants and 18 non-study participants. Classes for each condition were held during the same time frame to control for seasonal variation.
Outcome Measures
Assessments occurred at study entry (baseline), 10-weeks (post-intervention), 6- and 12-month post-baseline follow up, and conducted by evaluators blinded to patients’ treatment assignment.
Primary outcomes were QOL and lung function. Quality of life was measured by the Asthma Quality of Life Questionnaire (AQOL), a 32-item survey assessing the degree to which important activities have been limited by asthma during the last two weeks in four domains: activity limitations, asthma symptoms, emotional function and environmental exposure. An overall QOL score is computed by averaging the four domains. The AQOL is valid, reliable and sensitive to changes in asthma symptoms.
Lung function was assessed by change from baseline in two-week average morning peak expiratory flow (PEF) (liters/minute). It was selected based on a review of asthma treatment studies conducted by National Heart, Lung, and Blood Institute’s (NHLBI) Asthma Clinical Research Network (ClinicalTrials.gov). While the correlation with FEV1 from spirometry is not always ideal, PEF can easily be performed at home and is often used as an indicator of lung function in asthma. Participants were provided a PEF meter, written instructions on how to use it correctly, had the procedure demonstrated by research staff, and then practiced until they were able to perform the maneuver appropriately. Participants were asked to document PEF first thing in the morning and last thing at night for two weeks following each assessment.
Two additional lung function measures were collected; PEF variability, and spirometry. PEF variability was calculated by comparing the minimum morning pre-bronchodilator PEF to the recent best (day’s highest minus lowest/mean), providing an amplitude percent mean. [10] Spirometry assessed forced expiratory in one second (FEV1) and forced vital capacity (FVC) and were performed in the UMMHC Pulmonary Diagnostic Laboratory according to American Thoracic Society guidelines. [11]
Secondary outcomes included asthma control and perceived stress. Control classifications were based on the 2007 NIH/NHLBI criteria. [8] Those in a less well-controlled category for any component were classified at the higher category. The 10-item Perceived Stress Scale (PSS) [12] assessed the degree to which the person appraised their coping resources as being insufficient to meet the demands of events in the past month.
At each assessment, participants also recorded asthma rescue medication use (frequency of short-acting bronchodilators) over a 14 day period, and days of work or school missed due to asthma. Asthma exacerbations were assessed by self-reported initiation of prednisone in the last 30 days.
Analysis
Analyses were carried out using Stata 10.1. (Stata Corporation). The pilot study was powered for a mean difference in AQOL between groups of 0.4, and a difference in mean percent change in PEF of 9%. With α=0.1, there was 80% power with n=35/group. A 15% dropout was predicted so recruitment goals were n=42/group. Patients were randomized using a block design (blocks of 4 and 6).
Baseline means were compared using t-tests, or Wilcoxon rank sum tests. Fisher’s Exact tests were used to compare categorical variables. Distributional assumptions were examined for all outcomes. A cubic transformation of AQOL scores was used to meet assumptions for the linear model and corresponding tests. Estimated differences and confidence intervals for AQOL were generated by transforming to original units (nlcom in Stata 10.1).
Trends over time in AQOL, PSS, PEF variability, morning PEF, and FEV1 were analyzed using linear mixed models with random intercepts and slopes, with participant as the random effect. Differences in trends over time between MBSR and HLC were estimated using the interaction term of group and time. A likelihood ratio test was used for hypotheses involving multiple coefficients.
Dichotomous outcomes (well-controlled asthma, prednisone use in past 30 days) were analyzed using Generalized Estimating Equation (GEE) logistic regression. Times/week using short-term rescue medication was modeled GEE negative binomial regression. Interactions were tested using a Wald statistic. Estimates of odds ratios, incident rate ratios, and confidence intervals were derived from the models.
Differences in improvement in AQOL (by 1 or 1.5 points) at 12 months was tested using Fisher’s exact test. Class attendance was compared using the Wilcoxon rank-sum test. Prednisone use differed between randomized groups at baseline and was included in final models if it was associated with time trends and altered estimates of study arm effects. Intervention effects were estimated as the difference in change from baseline between the two study conditions.
For the peak flow/medication form, there were 18 to 22 missing data points at each time point. In the case of short-term rescue medication use missing values were extrapolated using the slope of the two closest non-missing values; single non-missing values were carried forward to all subsequent time points. Results presented are from these imputed models.
RESULTS
Baseline Characteristics of Study Sample
The only significant difference in demographic and clinical characteristics between the arms (see Table 1) was in prednisone/Medrol use in the past 30 days (24.4% in MBSR vs. 4.9% in the HLC control, p=0.026). The two conditions did not differ on any other measures of asthma control. The sample of 56 women and 27 men had a mean age of 52.8 years. The majority were white (93.8%), non-Latino (92.3%), married or living with a partner (73.17%), and had either some college or a college or advanced degree (68.8%). The percent with well-controlled asthma at baseline was very low (7.4%), consistent with the exclusion criterion of intermittent or well-controlled asthma. The number of years taking medication for asthma was 13.3. Mean baseline AQOL (5.20 overall; 5.46 men 5.08 women) was similar to a cross-sectional study of U.S. adult asthmatics (5.55 men, 5.02 women). [13] The sample’s mean perceived stress (16.6) placed them 0.5 standard deviations above a U.S. normative mean. [14]
Table 1.
Baseline Sociodemographic and Clinical Characteristics of Participants
| No. (%) | |||
|---|---|---|---|
| Characteristic | MBSR Intervention Group (n=42) |
HLC Control Group (n=41) |
P Value |
| Age, mean (SD), y | 51.93(13.6) | 53.61(13.7) | 0.575 |
| Female Sex | 27 (64.3%) | 29 (70.7%) | 0.641 |
| Race | 0.233 | ||
| White | 36 (90.0%) | 40 (97.6%) | |
| Black | 1 (2.5%) | 0 (0.0%) | |
| Other | 3 (7.5%) | 1 (2.4%) | |
| Latino | 5 (12.8%) | 1 (2.6%) | 0.200 |
| Education | 0.649 | ||
| High school degree or GED | 6 (14.6%) | 7 (17.5%) | |
| College 1–3 yrs | 13 (31.7%) | 16 (40.0%) | |
| College degree | 14 (34.1%) | 13 (32.5%) | |
| MA or Doctoral | 8 (19.5%) | 4 (10.0%) | |
| Marital Status | 0.880 | ||
| Married or living w/partner | 29 (70.7%) | 31 (75.6%) | |
| Never married | 5 (12.2%) | 4 (9.8%) | |
| Divorced or widowed | 7 (17.0%) | 6 (14.7%) | |
| Asthma Control* | 0.941 | ||
| Well controlled | 3 (7.3%) | 3 (7.5%) | |
| Not well controlled | 20 (48.8%) | 21 (52.5%) | |
| Very poorly controlled | 18 (43.9%) | 16 (40.0%) | |
| Asthma Severity | 0.586 | ||
| Mild | 6 (14.3%) | 5 (12.2%) | |
| Moderate | 18 (42.9%) | 22 (53.7%) | |
| Severe | 18 (42.9%) | 14 (34.1%) | |
| FEV1, L, mean (SD) | 2.57 (0.6) | 2.54 (0.7) | 0.842 |
| FEV1 percent predicted, mean (SD) | 91.7(16.6) | 94.6(18.9) | 0.453 |
| Morning Peak Flow (PEF), L/min, mean (SD) |
448.3(145.8) | 395.1(135.7) | 0.100 |
| Short-term Bronchodilator/Rescue Medication Use |
2.92 (5.4) | 2.22 (4.2) | 0.623** |
| Long-term Controller Medication | 31 (75.6%) | 29 (74.4%) | 1.000 |
| Prednisone/Medrol past 30 days | 10 (24.4%) | 2 (4.9%) | 0.026 |
| Asthma Quality of Life (AQOL), mean (SD) |
5.07 (1.2) | 5.33 (1.0) | 0.417** |
| Perceived Stress (PSS), mean (SD) | 17.41 (6.3) | 15.75 (7.8) | 0.294 |
| Other Medical Conditions | |||
| Allergic rhinitis | 15 (36.6%) | 14 (34.1%) | 1.000 |
| Heart disease | 3 (7.3%) | 4 (9.8%) | 1.000 |
| Gastro-esophageal reflux disease | 25 (61.0%) | 19 (47.5%) | 0.268 |
| No. of Days Missed School or Work due to Asthma, mean (SD) |
0.61 (1.6) | 0.10 (0.4) | 0.094** |
Asthma control was assessed based on the National Heart Lung and Blood Institute (NHLBI)8 criteria. Presented are percent classified as well-controlled (vs. not well controlled or very poorly controlled).
Rank-Sum Test
Primary Outcomes
Asthma-related Quality of Life
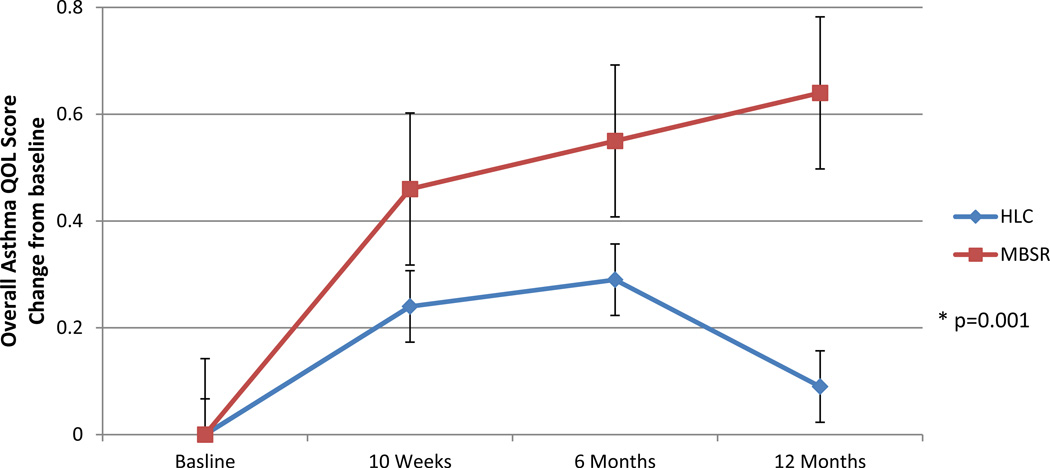
At 12-month follow-up, asthma-related quality of life (AQOL) had significantly improved in MBSR in both overall QOL (intervention effect 0.55, p=0.001), and three of the four components: activity limitations (0.57, p=0.005), symptoms (0.46, p=0.009), emotional function (0.63, p=0.002) (see Table 2). Only the environmental stimuli component did not demonstrate an effect (p=0.057). The greatest improvement was in emotional function (5.54 to 6.27). The MBSR overall AQOL improvement of 0.63 from baseline (5.34) to 12 months (5.97) was greater than the 0.50 considered clinically significant (see Figure 2), and more MBSR patients achieved moderate (≥ 1 point) (34% vs. 12%, p=0.031) and large improvements in AQOL (≥ 1.5 points) (18% vs. 5%, p=0.080).15
Table 2.
Change From Baseline in Asthma Quality of Life (AQOL)
| Mean (SE) | Mean (95% (CI) Change from baseline to |
|||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 10 Weeks | 6 Months | 12 Months | 10 Weeks | 6 Months | 12 Months | P Val* | |
| AQOL Overall Score | n=82 | n=74 | n=76 | n=80 | ||||
| MBSR | 5.34(0.15) | 5.80(0.13) | 5.89(0.13) | 5.97(0.12) | 0.46(0.23,0.69) | 0.55(0.34,0.76) | 0.64(0.40,0.87) | 0.015++ |
| HLC Control | 5.50(0.14) | 5.74(0.14) | 5.79(0.14) | 5.58(0.14) | 0.24(0.02,0.47) | 0.29(0.09,0.50) | 0.09(−0.15,0.33) | |
| Intervention Effect | 0.22(−0.10,0.54) | 0.26(−0.04,0.55) | 0.55(0.21,0.89) † | |||||
| P Value | 0.191 | 0.092 | 0.001 | |||||
|
Four AQOL Domains: | ||||||||
| Activity Limitations | n=82 | n=74 | n=76 | n=80 | ||||
| MBSR | 5.29(0.17) | 5.66(0.15) | 5.86(0.15) | 5.97(0.13) | 0.37(0.10,0.65) | 0.57(0.29,0.85) | 0.68(0.38,0.98) | 0.028++ |
| HLC Control | 5.45(0.16) | 5.71(0.15) | 5.83(0.15) | 5.56(0.15) | 0.26(−0.01,0.52) | 0.38(0.11,0.66) | 0.11(−0.19,0.41) | |
| Intervention Effect | 0.12(−0.26,0.50) | 0.19(−0.20,0.58) | 0.57(0.15,1.00)† | |||||
| P Value | 0.581 | 0.371 | 0.005 | |||||
| Symptoms | n=82 | n=73 | n=76 | n=80 | ||||
| MBSR | 5.37(0.15) | 5.87(0.14) | 5.91(0.14) | 5.96(0.13) | 0.50(0.25,0.50) | 0.54(0.33,0.50) | 0.59(0.34,0.84) | 0.055++ |
| HLC Control | 5.48(0.15) | 5.76(0.15) | 5.76(0.15) | 5.61(0.15) | 0.29(0.03,0.54) | 0.29(0.08,0.50) | 0.14(−0.12,0.39) | |
| Intervention Effect | 0.22(−0.14,0.57) | 0.25(−0.04,0.55) | 0.46(0.10,0.81)† | |||||
| P Value | 0.239 | 0.093 | 0.009 | |||||
| Emotional Function | n=82 | n=74 | n=76 | n=80 | ||||
| MBSR | 5.54(0.18) | 6.03(0.15) | 6.09(0.13) | 6.27(0.13) | 0.50(0.22,0.78) | 0.56(0.31,0.81) | 0.74(0.44,1.04) | 0.019++ |
| HLC Control | 5.63(0.17) | 5.96(0.15) | 5.90(0.14) | 5.74(0.15) | 0.33(0.05,0.61) | 0.27(0.02,0.52) | 0.11(−0.20,0.43) | |
| Intervention Effect | 0.17(−0.23,0.56) | 0.29(−0.07,0.64) | 0.63(0.19,1.07)† | |||||
| P Value | 0.405 | 0.090 | 0.002 | |||||
|
Environmental Stimuli |
n=80 | n=73 | n=76 | n=79 | ||||
| MBSR | 5.59(0.17) | 5.97(0.15) | 5.86(0.15) | 5.89(0.15) | 0.38(0.11,0.65) | 0.27(0.02,0.53) | 0.30(0.02,0.38) | 0.235++ |
| HLC Control | 5.78(0.17) | 5.86(0.16) | 5.89(0.15) | 5.70(0.16) | 0.09(−0.17,0.35) | 0.11(−0.14,0.36) | −0.08(−0.36,0.20) | |
| Intervention Effect | 0.29(−0.08,0.67) | 0.16(−0.20,0.52) | 0.38(−0.01,0.78) | |||||
| P Value | 0.129 | 0.400 | 0.057 | |||||
The p-value results from the likelihood ratio test comparing models with and without the group-time interaction.
A cubic transformation was used to meet the distributional assumptions of the model (providing appropriate p-values for testing). Estimates shown in the table were derived from the models and back transformed into the original units for ease of interpretation.
The p-value for the group-time interaction at the particular time-point ≤ 0.05.
Figure 2.
Overall Asthma Quality of Life (AQOL) Change from Baseline
Lung Function
The primary lung function measure (two-week average morning PEFs (liters/minute)) did not improve in MBSR compared to controls (p=0.705) (see Table 3). Similarly, PEF variability (p=0.966) and FEV1 (p=0.917) did not demonstrate effects. Adherence to PEF monitoring, defined as completing at least one full day of monitoring, was 78% at 10 weeks, 77% at 6 months, and 78% at 12 months.
Table 3.
Change From Baseline in Lung Function
| Mean (SE) | Mean (95% (CI) Change from baseline to |
|||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 10 Weeks | 6 Months | 12 Months | 10 Weeks | 6 Months | 12 Months | P Val* | |
|
2-week Average AM Peak Flow (PEF) (liters/min) |
n=78 | n=63 | n=63 | n=63 | ||||
| MBSR | 445.5(21.6) | 440.7(22.2) | 443.7(21.5) | 448.5(23.7) | −4.8(−31.5,21.8) | −1.9(−27.1,23.4) | 2.9(−26.5,32.4) | 0.974 |
| HLC Control | 394.5(22.2) | 398.7(22.8) | 400.9(22.1) | 405.7(24.6) | 4.2(−23.2,31.6) | 6.4(−19.7,32.5) | 11.3(−20.1,42.7) | |
| Intervention Effect | −9.0(−47.3,29.2) | −8.2(−44.6,28.1) | −8.3(−51.4,34.7) | |||||
| P Value | 0.644 | 0.656 | 0.705 | |||||
|
Peak Expiratory Flow (PEF) Variability (%) |
n=77 | n=64 | n=63 | n=62 | ||||
| MBSR | 8.86(0.78) | 7.26(0.70) | 9.20(0.76) | 8.17(0.90) | −1.60(−3.10,−0 .10) | 0.34(−1.49,2.17) | −0.69(−2.42,1.04) | 0.032 |
| HLC Control | 9.19(0.79) | 8.46(0.69) | 7.30(0.76) | 8.45(0.95) | −0.73(−2.23,0.77) | −1.89(−3.73,−0.05) | −0.75(−2.57,1.08) | |
| Intervention Effect | −0.87(−2.99,1.26) | 2.23(−0.37,4.83) | 0.06(−2.46,2.57) | |||||
| P Value | 0.424 | 0.092 | 0.966 | |||||
|
Spirometry (FEV1) (liters) |
n=83 | n=66 | n=63 | n=78 | ||||
| MBSR | 2.57(0.10) | 2.61(0.11) | 2.62(0.11) | 2.60(0.11) | 0.04(−0.03,0.11) | 0.05(−0.02,0.13) | 0.03(−0.05,0.11) | 0.408 |
| HLC Control | 2.54(0.10) | 2.65(0.11) | 2.61(0.11) | 2.56(0.11) | 0.11(0.04,0.11) | 0.07(−0.002,0.15) | 0.02(−0.06,0.11) | |
| Intervention Effect | −0.07(−0.18,0.03) | −0.02(−0.13,0.09) | 0.01(−0.11,0.13) | |||||
| P Value | 0.159 | 0.692 | 0.917 | |||||
The p-value results from the likelihood ratio test comparing models with and without the group-time interaction.
Secondary Outcomes
Asthma Control
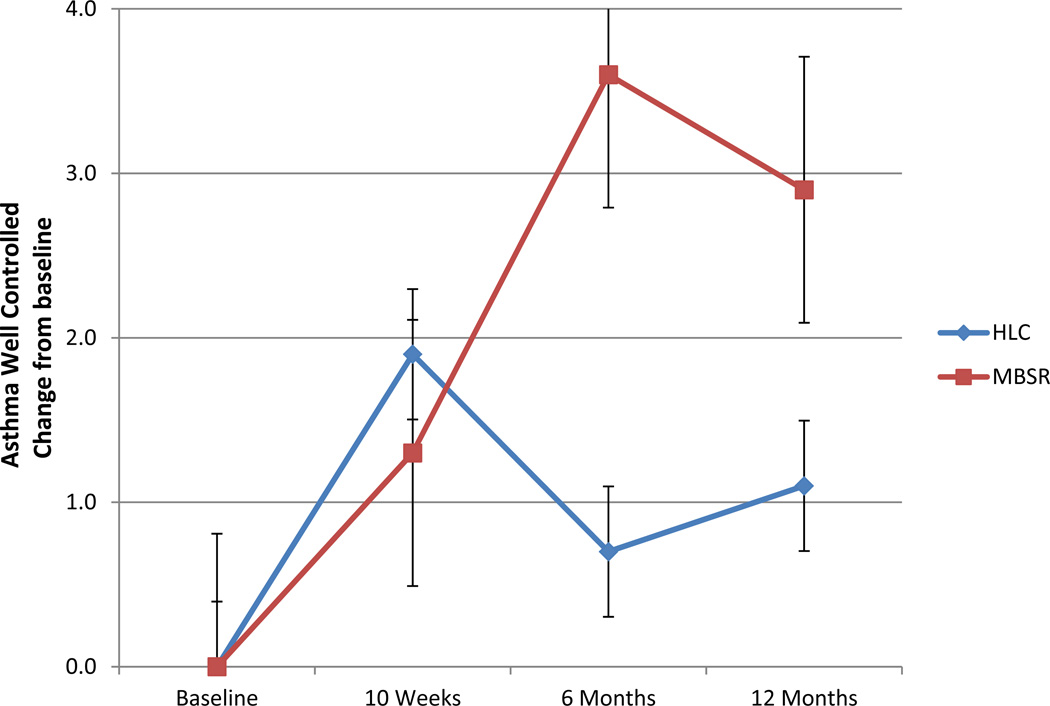
The percentage of MBSR patients with well-controlled asthma [8] was not significant over time compared to controls (p=0.132). However, the estimated percentage of MBSR patients classified as well-controlled went from 7.3% at baseline to 19.4% at 12 month follow up, compared to a change from 7.5% to 7.9% in controls (p=0.301) (see Figure 3).
Figure 3.
Asthma Control Change from Baseline
Perceived Stress
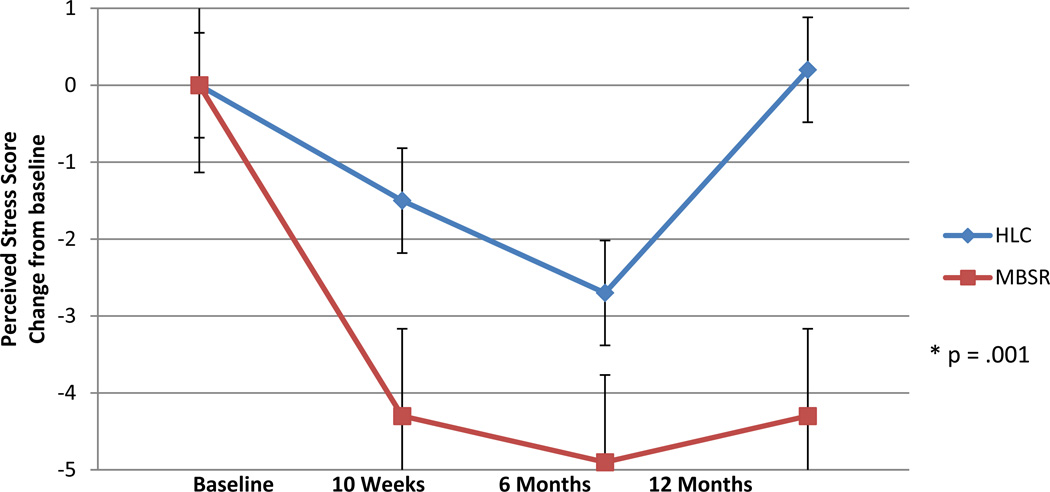
Perceived stress (PSS) had significantly reduced in MBSR compared to controls at 12-months (p=0.001) (see Table 4). At baseline the MBSR arm mean (17.3) placed them at the 75th percentile for a U.S. normative sample; [14] at 12 months the mean (13.0) had improved to the U.S. norm, while the controls remained relatively unchanged (15.8 to 16.0) (see Figure 4).
Table 4.
Change From Baseline in Asthma Control, Perceived Stress, Rescue Medication and Prednisone Use
| Percent (n/total) | OR (95% (CI) Change from baseline to |
|||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 10 Weeks | 6 Months | 12 Months | 10 Weeks | 6 Months | 12 Months | P Val+ | |
|
Percent Well- controlled Asthma |
n=81 | n=70 | n=75 | n=74 | ||||
| MBSR | 7.3(3/41) | 9.1(3/33) | 21.6(8/37) | 19.4(7/36) | 1.3(0.3,5.1) | 3.6(1.1,11.7) | 2.9(0.9,9.7) | 0.132‡ |
| HLC Control | 7.5(3/40) | 13.5(5/37) | 5.4(2/37) | 7.9(3/38) | 1.9(0.5,6.8) | 0.7(0.1,3.3) | 1.1(0.3,4.5) | |
| Intervention Effect | 0.7(0.1,4.4) | 5.4(0.8,38.7) | 2.6(0.4,16.4) | |||||
| P Value | 0.689 | 0.093 | 0.301 | |||||
| Mean (SE) | Mean (95% (CI)) Change from baseline to |
|||||||
| Baseline | 10 Weeks | 6 Months | 12 Months | 10 Weeks | 6 Months | 12 Months | P Val* | |
| Perceived Stress (PSS) | n=81 | n=73 | n=76 | n=77 | ||||
| MBSR | 17.3(1.1) | 13.0(1.0) | 12.4(1.0) | 13.0(1.0) | −4.3(−6.2,−2.3) | −4.9(−6.6,−3.1) | −4.3(−6.1,−2.4) | 0.012 |
| HLC Control | 15.8(1.1) | 14.3(1.0) | 13.1(1.0) | 16.0(1.0) | −1.5(−3.5,0.5) | −2.7(−4.5,0.9) | 0.2(−1.7,2.0) | |
| Intervention Effect | −2.8(−5.6,0.1) | −2.1(−4.6,0.4) | −4.5(−7.1,−1.9)† | |||||
| P Value | 0.055 | 0.097 | 0.001 | |||||
| Mean (SE) | IRR (95% (CI) Change from baseline to |
|||||||
| Baseline | 10 Weeks | 6 Months | 12 Months | 10 Weeks | 6 Months | 12 Months | P Val+ | |
| Times/Week Used | n=79 | n=81 | n=82 | n=82 | ||||
| Short-Term Rescue | ||||||||
| Medication | ||||||||
| MBSR | 2.92(0.85) | 3.21(1.15) | 2.97(1.02) | 2.39(0.89) | 0.71(0.53,0.96) | 0.81(0.60,1.08) | 0.48(0.36,0.65) | <0.001Δ |
| HLC Control | 2.22(0.69) | 2.15(0.61) | 1.83(0.55) | 2.49(0.74) | 1.00(0.77,1.30) | 0.83(0.63,1.08) | 1.04(0.80,1.36) | |
| Intervention Effect | 0.71(0.49,1.05) | 0.98(0.66,1.44) | 0.46(0.31,0.68)† | |||||
| P Value | 0.087 | 0.902 | <0.001 | |||||
| Percent(n/total) | OR (95% (CI) Change from baseline to |
|||||||
| Baseline | 10 Weeks | 6 Months | 12 Months | 10 Weeks | 6 Months | 12 Months | P Val+ | |
|
Prednisone Use % in last 30 days |
n=82 | n=73 | n=76 | n=78 | ||||
| MBSR | 24.4(10/41) | 13.9(5/36) | 12.8(5/39) | 17.9(7/39) | 0.5(0.2,1.5) | 0.5(0.2,1.4) | 0.7(0.3,1.9) | 0.119‡ |
| HLC Control | 4.9(2/41) | 18.9(7/37) | 5.4(2/37) | 15.4(6/39) | 4.6(1.0,21.1) | 1.1(0.2,7.0) | 3.5(0.8,16.1) | |
| Intervention Effect | 0.1(0.02,0.7)† | 0.4(0.05,3.4) | 0.2(0.03,1.2) | |||||
| P Value | 0.021 | 0.415 | 0.084 | |||||
The p-value results from the Wald Test of the group-time interaction.
The p-value results from a logistic regression model.
The p-value results from the likelihood ratio test comparing models with and without the group-time interaction.
The p-value for the group-time interaction at the particular time-point ≤ 0.05.
The p-value results from a negative binomial regression model.
Figure 4.
Perceived Stress Change from Baseline
Asthma Rescue Medications, Exacerbations, Days of Work/School Missed
In an unadjusted model, there were no significant differences in change between the arms in use of short-term rescue medications (bronchodilators) (p=0.095), or use of prednisone for asthma exacerbations (p=0.084) (see Table 4). However, when adjustment was made for prednisone use in the 30 days before baseline assessment, MBSR showed a significant decrease in use of rescue medications at 12 months (p<0.001). There was no difference between arms in days of work or school missed (p=0.538).
Intervention and Control Sessions Attended
Of the 9 program sessions (8 weekly and one full day), the mean number attended was 5.64 in MBSR, and 4.54 in HLC (p=0.047).
DISCUSSION
Our findings indicate that participation in an MBSR program as an adjunct to medical asthma treatment resulted in enduring and clinically significant improvements in QOL in these patients with persistent asthma. [15] Although direct comparison cannot be made in the effect of medication on QOL, some clinical perspective is provided by noting that the improvements are comparable to those in trials of widely prescribed asthma medications including inhaled corticosteroids [16] and an anti-IgE antibody. [17] Further, other complementary and alternative medicine (CAM) programs have not shown similar definitive improvements in asthma quality of life, [6] suggesting that mindfulness training may have uniquely effective features. The independence of QOL improvements from lung function is consistent with a normative study which also found no correlation between AQOL and lung function. [13]
It was hypothesized that mindfulness training would affect QOL through decreases in stress from the increased coping resources represented by changes in appraisal and reduced reactivity to symptoms. [18] A number of findings support this model. First, the largest intervention effect in AQOL was in emotional function. Second, the environmental triggers domain did not change. Third, there was a substantial reduction in perceived stress in MBSR (intervention effect −4.5 (CI −7.1, −1.9), p=0.001) suggesting that coping resources increased in MBSR patients.
The finding of reduced stress has important clinical implications since higher stress levels are associated with increased asthma morbidity, poorer QOL and sub-optimal disease management. [2] The lack of accompanying improvements in lung function however has implications for the debate on the causal relation between stress and asthma. Increased airway resistance in asthma patients has been shown with laboratory induced stress [19] but longer term life stress is not associated with FEV1 [20] and relaxation therapies have not been found to improve lung function in asthmatics. [21] The present findings add support to the view that life stress, while affecting asthma patients QOL, may not contribute to impairment in lung function.
An interesting and encouraging feature of the findings is the pattern of change between the treatment conditions over 12 months. While there was a tendency for both conditions to show improvement in QOL, stress, and asthma control in the first six months, the smaller gains achieved by controls largely deteriorated to baseline levels at 12 months while MBSR maintained, or improved their gains without further intervention. It may be that the HLC educational program produced an initial placebo effect, a suggestion supported by a recent trial of bronchial thermoplasty that demonstrated some placebo effect on QOL can be expected from participation in an asthma trial. [22] A similar pattern was observed in a cognitive behavioral intervention for asthma patients with co-existing panic disorder that found AQOL gains made during the 8-week intervention were not sustained at 6 months. [23] It may be that more accurate discrimination between thoughts, feelings, and sensations, and the reduced urgency and distress resulting from non-reactive awareness associated with mindfulness training, is a lasting perceptual change. [18] To our knowledge this is the first randomized trial of MBSR using an active control that has followed participants for 12 months.
The present study also addresses the critiques of studies of mindfulness training [24] and CAM programs used by 40% of asthma patients [6] as being limited by lack of a credible active control, including only subjective end-points, and inadequately defined participant characteristics and treatment methods. In doing so it enhances confidence in the findings and moves mindfulness research forward. Additionally, by employing a widely available, standardized program as the intervention including non-asthmatics in the classes rather than an experimental program tailored to the needs of asthma patients, the study created conditions that were no more tightly monitored than ‘real world’ MBSR programs. As such, it addresses the more general criticism that behavioral trials create intervention conditions not generalizable, or translatable into the ‘real world’. Given these features, it is reasonable to expect that the findings are similar to what could be expected in the approximately 200 MBSR programs available at health care facilities across the U.S. Many of these are covered by third party payers, making this a realistic adjunctive treatment for many patients with asthma.
There were a number of study limitations. The modest sample size limited power to detect differences in a number of variables, including asthma control. Sample size also limited our ability to detect whether the intervention effect was specific to asthmatics of a particular severity, and whether it was related to changes in concomitant medications. And while structured to reflect ‘real world’ MBSR programs, the generalizability of the findings are limited by three factors: patients were from a pulmonary medicine and primary care population in an academic medical center; the refusal rate was high among eligible patients, raising concerns about the self-selected nature of the sample; and while MBSR has been shown to be acceptable to low-income and multi-ethnic samples, [25] the majority of patients were white, non-Latino, and of higher socioeconomic status.
ACKNOWLEDGEMENT
Study supported by grant R21 AT002938 (awarded to Drs. Pbert and Carmody) from the NIH National Center for Complementary & Alternative Medicine. The sponsor provided financial support only and had no role in the design, conduct; data collection, management, analysis, and interpretation of the study; or in the preparation, review, or approval of the manuscript. Drs. Pbert and Carmody had full access to all of the data and take responsibility for the integrity and the accuracy of the data and analysis.
We gratefully acknowledge the technicians in the UMMHC Pulmonary Diagnostic Laboratory for conducting the spirometry, and Dr. Sarah Reiff-Hekking for conducting the Healthy Living Course (compensated financially for their work on this study).
Footnotes
Clinical Trail Registration: Asthma and Mindfulness-Based Reduction (MBSR) Identifier: NCT00682669. clinicaltrials.gov
Contributor Information
Lori Pbert, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, USA
J. Mark Madison, Division of Pulmonary, Allergy and Critical Care Medicine. University of Massachusetts Medical School, Worcester, USA
Susan Druker, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, USA
Nicholas Olendzki, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, USA
Robert Magner, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, USA
George Reed, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, USA
James Carmody, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, USA
REFERENCES
- 1.Lemmens KM, Nieboer AP, Huijsman R. A systematic review of integrated use of disease-management interventions in asthma and COPD. Respir Med. 2009;103(5):670–691. doi: 10.1016/j.rmed.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 2.Wisnivesky JP, Lorenzo J, Feldman JM, et al. The relationship between perceived stress and morbidity among adult inner-city asthmatics. J Asthma. 2010;47:100–104. doi: 10.3109/02770900903426989. [DOI] [PubMed] [Google Scholar]
- 3.Janssens T, Verleden G, De Peuter S, et al. Inaccurate perception of asthma symptoms: a cognitive-affective framework and implications for asthma treatment. Clin Psychol Rev. 2009;29:317–327. doi: 10.1016/j.cpr.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Rietveld S. Symptom perception in asthma: a multidisciplinary review. J Asthma. 1998;35:137–146. doi: 10.3109/02770909809068201. [DOI] [PubMed] [Google Scholar]
- 5.Yorke J, Fleming SL, Shuldham C. Psychological interventions for adults with asthma: a systematic review. Respir Med. 2007;101:1–14. doi: 10.1016/j.rmed.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Markham AW, Wilkinson JM. Complementary and alternative medicines (CAM) in the management of asthma: an examination of the evidence. J Asthma. 2004;41:131–139. doi: 10.1081/jas-120028581. [DOI] [PubMed] [Google Scholar]
- 7.Shigaki CL, Glass B, Schopp LH. Mindfulness-based stress reduction in medical settings. J Clinl Psychol Med Settings. 2006;13:209–216. [Google Scholar]
- 8.National Heart Lung and Blood Institute (NHLBI) Expert Panel Report 3: Guidelines for the diagnosis and management of asthma. NIH Publication NO. 07-4051: U.S. Department of Health and Human Services. 2007 http://www.nhibi.nih.gov/guidelines/asthma/asthgdin.htm.
- 9.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness. New York: Delacorte; 1990. [Google Scholar]
- 10.Reddel HK, Taylor DR, Bateman ED, et al. An official American Thoracic Society/European Respiratory Society statement: Asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009;180:59–99. doi: 10.1164/rccm.200801-060ST. [DOI] [PubMed] [Google Scholar]
- 11.Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med. 1995;152:1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 12.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 13.Leidy NK, Coughlin C. Psychometric performance of the Asthma Quality of Life Questionnaire in a US sample. Qual Life Res. 1998;7:127–134. doi: 10.1023/a:1008853325724. [DOI] [PubMed] [Google Scholar]
- 14.Cohen S, Williamson C. Spacapan S, Oskamp S, editors. Perceived stress in a probability sample of the United States. The Social Psychology of Health: Sage. 1998:31–67. [Google Scholar]
- 15.Juniper EF, Guyatt GH, Willan A, et al. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol. 1994;47:81–87. doi: 10.1016/0895-4356(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 16.Boulet LP, Bateman ED, Voves R, et al. A randomized study comparing ciclesonide and fluticasone propionate in patients with moderate persistent asthma. Respir Med. 2007;101:1677–1686. doi: 10.1016/j.rmed.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 17.Holgate ST, Chuchalin AG, Hebert J, et al. Efficacy and safety of a recombinant anti-immunoglobulin E antibody (omalizumab) in severe allergic asthma. Clin Exp Allergy. 2004;34(4):632–638. doi: 10.1111/j.1365-2222.2004.1916.x. [DOI] [PubMed] [Google Scholar]
- 18.Carmody J. Evolving conceptions of mindfulness in clinical settings. J Cogn Psychother. 2009;23:270–280. [Google Scholar]
- 19.Ritz T, Kullowatz A. Effects of emotion and stress on lung function in health and asthma. Curr Respir Med Rev. 2005;1:209–218. [Google Scholar]
- 20.Kullowatz A, Rosenfield D, Dahme B, et al. Stress effects on lung function in asthma are mediated by changes in airway inflammation. Psychosom Med. 2008;70:468–475. doi: 10.1097/PSY.0b013e31816f9c2f. [DOI] [PubMed] [Google Scholar]
- 21.Huntley A, White AR, Ernst E. Relaxation therapies for asthma: a systematic review. Thorax. 2002;57:127–131. doi: 10.1136/thorax.57.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Castro M, Rubin AS, Laviolette M, et al. Effectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trial. Am J Respir Crit Care Med. 2010;181:116–124. doi: 10.1164/rccm.200903-0354OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ross CJ, Davis TM, MacDonald GF. Cognitive-behavioral treatment combined with asthma education for adults with asthma and coexisting panic disorder. Clin Nurs Res. 2005;14:131–157. doi: 10.1177/1054773804273863. [DOI] [PubMed] [Google Scholar]
- 24.Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300:1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- 25.Roth B, Robbins D. Mindfulness-Based Stress Reduction and Health-Related Quality of Life: Findings From a Bilingual Inner-City Patient Population. Psychosom Med. 2004;66:113–123. doi: 10.1097/01.psy.0000097337.00754.09. [DOI] [PubMed] [Google Scholar]