Abstract
Context
Sexually experienced women are at risk of cervical cancer, one of the most common female reproductive cancers. Nearly 20% of U.S. women aged 18–64 have a disability, and disability is associated with health care access; however, the relationship between disability and Pap smear receipt remains underexplored.
Methods
Data on 20,907 women aged 21–64 from the 2000 and 2005 National Health Interview Surveys were used to investigate the relationship between disability and cervical cancer screening. Logistic regression analyses were conducted to assess the association between disability and both women's receipt of a Pap smear and their receipt of a doctor's recommendation for a Pap smear in the past year.
Results
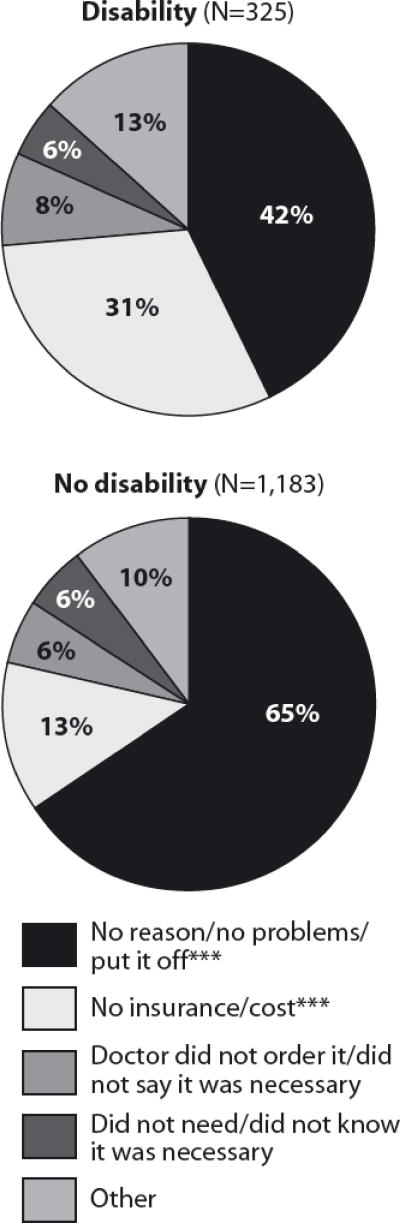
Having a disability was negatively associated with Pap smear receipt (odds ratio, 0.6). Compared with women with no disabilities, those with mobility limitations and those with other types of limitations had reduced odds of having received a Pap smear (0.5–0.7). Disability was positively associated with having received a recommendation for a Pap smear (1.2); however, among women who had received a recommendation, those with disabilities had reduced odds of having received a Pap smear (0.5). Among women who had not received a Pap smear, 31% of those with disabilities and 13% of others cited cost or lack of insurance as the primary reason.
Conclusions
The negative relationship between Pap smear receipt and multiple types of disability suggests barriers beyond the human-made physical features of the environment. Efforts to reduce inequalities in reproductive health care access should consider the needs of women with disabilities.
Cervical cancer is one of the most common cancers of the female reproductive system.1 Most cases are associated with the sexually transmitted infection of strains of the human papillomavirus (HPV),2 making sexual activity the primary risk factor for developing cervical cancer. According to the Centers for Disease Control and Prevention (CDC), an estimated 27% of U.S. women aged 14–59, or 24.9 million women, are infected with HPV.3
In addition to being one of the most common reproductive cancers, cervical cancer is one of the most preventable. Preventive screening is most widely done with the Pap smear,4,5 which has been credited with reducing the cervical cancer mortality rate by an estimated 70% over the past 40 years.6 Despite this decline, as of 2002, cervical cancer remained the 10th leading cause of cancer-related deaths among women, and the fifth leading cause of cancer-related deaths among women younger than 50.4
Most women who develop cervical cancer have not received screening as recommended by medical guidelines.4 Thus, identifying barriers to cervical cancer screening is critical to promoting the reproductive health of U.S. women. In this article, we focus on one potential barrier—having a disabling condition—and investigate the relationship between disability and Pap smear receipt.
Approximately 20% of U.S. females aged 18–64 live with at least one disabling condition.7 Although preventive care is important for all, access to preventive services may be especially important for individuals with disabilities. Some researchers argue that because individuals with disabilities experience a “thinner margin of health,” they are more vulnerable than individuals without disabilities to significant medical problems.8,9 As research has highlighted that people with disabilities may have reduced access to health care, particularly preventive care,8,10 disability has emerged as an important dimension of inequality in discussions of health disparities. Indeed, in 2005, the surgeon general issued a call to “break down barriers to health and wellness for people with disabilities.”11 This article seeks to broaden our understanding of the connection between disability and U.S. women's receipt of Pap smears.
Background
For many years, sexually active women and those 18 or older in the United States had been advised to receive annual Pap smear screenings. In 2002, the American Cancer Society issued new guidelines, and in 2003, the American College of Obstetricians and Gynecologists (ACOG) and the U.S. Preventive Services Task Force did likewise.4,12,13 The guidelines differed slightly, but each continued to recommend annual Pap smears for women younger than 30; however, the recommended screening frequency was changed to 2–3 years for women aged 30–69 who have had three consecutive negative tests and are not at high risk (e.g., those who are not immune-compromised or do not have a history of cervical neoplasia).14
The revised guidelines have been controversial, with some medical professionals calling for the continuation of one-year intervals for all women, because of the relatively high rate of false negatives.6 Preliminary evidence suggests that adherence to the new guidelines has been low, and that some medical professionals prefer for their patients to continue receiving annual screenings.15 Indeed, during the period in which this article was under review, guidelines for cervical cancer screening were again under debate and were revised further.14,16 Nonetheless, the recommendation that women receive regular screenings is firmly established.
Prior research on the relationship between disability status and cervical cancer screening using nationally representative data is limited. Two review studies on correlates of preventive cancer screenings suggest a negative relationship between disability status and Pap smear receipt.9,17 Disability, however, is not a central focus in either study, and both assess disability only in terms of mobility impairment, neglecting a range of other impairments that might interfere with health care receipt.
Studies focusing on disability have tended to rely on specialized samples. According to an analysis of data from the 2001 California Health Interview Study, among women aged 18 or older, those with disabilities were less likely than their peers with no disabilities to have received a Pap smear in the three years preceding the survey or a doctor's recommendation for a Pap smear in the previous year.18 Findings from a study among women with mobility impairment recruited from independent living centers also suggest a negative association between physical disability and cervical cancer screening.19 And according to a national study of 1994 data that focused on disability, the likelihood of Pap smear receipt was reduced among women with major lower extremity mobility difficulties;9 although the study did not focus on cervical cancer specifically, it provides the best evidence to date that some types of disability are connected to Pap smear receipt in the United States.
Another limitation of previous research is that most studies included only bivariate associations20 or regression analyses that considered disability status at the time of data collection and receipt of a Pap smear in the three years prior to data collection, making it possible that disability onset followed Pap smear receipt.7,17,18,21
Our research extends previous work on disability and cervical cancer screening in several ways. First, we use nationally representative National Health Interview Survey (NHIS) data from 2000 and 2005 to examine disability and Pap smear receipt. Second, we consider this relationship in a regression context and measure disability in a way to ensure that disability onset occurred prior to Pap smear receipt. In addition, we empirically explore two potential barriers to health care receipt—the built environment (human-made physical features of the environment) and clinical treatment. Finally, we investigate women's self-reported reasons for nonreceipt of a Pap smear, and whether those reasons differ by disability status.
Conceptualizing Disability
Most conceptualizations of disability recognize that a chronic illness or impairment becomes disabling when it prevents an individual from fulfilling social roles (such as student, worker, parent, woman and citizen) in the built, political, economic, social and cultural environments.7 This conceptualization is represented by the World Health Organization's (WHO) International Classification of Functioning, Disability and Health, which breaks disability into three domains: impairments (deviations from the population norm or losses in body structures or functions because of some underlying pathology), activities (an individual's ability to perform a task) and participation (“involvement in life situations”).22
Although WHO recognizes that disablement is partially caused by contextual factors, the standard measurement of disability in surveys—including the NHIS—relies on reported functional limitations, without further detail on contextual contributions to these limitations. For our study, we used all functional limitation measures available in the NHIS, but did not capture variations in the everyday meaning of limitations in individual lives. We did capture, however, broad categories of limitation that are relevant to understanding differences in Pap smear use in a way that is consistent with the WHO conceptual framework.
Barriers to Screening
The built environment and clinical factors have been identified as particularly salient for understanding the barriers to accessing health care experienced by women with disabilities.9,18 The built environment can affect cervical cancer screening receipt among women with disabilities insofar as it impedes their physical access to, into or within buildings in which screening is conducted. For example, buildings that lack elevators or ramps, or that have halls or doors that are too narrow to permit easy passage, may limit physical access. In addition, medical equipment and technologies—especially examination tables and diagnostic tools—that do not fit or measure “nonstandard” bodies can limit access. Finally, lack of accessible and convenient transportation to and from medical offices may also constitute a barrier related to the built environment.8
Although previous research has presented arguments about the importance of the built environment, most of this research has focused solely on women with mobility limitations,9,16,21,22 or has operationalized “disability” as the sum of mostly physical limitations.17,21 We considered disability more broadly. In particular, we explored simultaneously whether mobility and other types of limitations are associated with Pap smear receipt. Finding that mobility impairments are negatively associated with Pap smear receipt would be consistent with explanations pointing to effects of the built environment; finding that multiple forms of disability are negatively associated with Pap smear receipt would suggest that factors beyond the built environment are relevant.
Explanations for observed disparities that center on clinical factors,18 or “process barriers,”23 emphasize the knowledge, attitudes and practices of providers, and how they may affect the likelihood that women receive a Pap smear. Medical providers may lack knowledge about the sexual functioning and the reproductive health needs of women with disabilities.21,24,25 In addition, they may make erroneous assumptions about the desire or ability of women with disabilities to have sex or bear children, or may hold negative attitudes about the appropriateness of such sexual activity or childbearing.24,26–29 Finally, medical personnel may provide care to women with disabilities that is too “disability-focused”: care that views disabling conditions, rather than other health concerns, as the object of treatment.8,10 Such care likely diminishes individuals with disabilities' odds of receiving preventive services unrelated to their disabling condition. All of these factors lead us to expect that women with disabilities are less likely than others to receive a recommendation for a Pap smear.
Methods
Data
Data for this study come from the 2000 and 2005 NHIS focal adult samples. The NHIS—a series of annual household surveys administered in person by interviewers trained by the U.S. Census Bureau—is one of the best sources of information about the health and well-being of the American people. It collects a core set of data on each member of each household sampled. In addition, one adult and one child per household (the “focal adult” and “focal child”) are randomly selected to complete a more in-depth questionnaire about health and health care utilization.*
The NHIS, which had a focal adult response rate of 72% in 2000 and 69% in 2005, is particularly well suited for our research, because it includes information on health, health care access and utilization, and social and demographic characteristics.30,31 We used the 2000 and 2005 rounds because a cancer control module was administered to all women completing the in-depth questionnaire in these years. In this module, women were asked about Pap smear recommendation and receipt; if women had not received a Pap smear within the past three years, they were asked the primary reason for nonreceipt.30,31 We combined data from the person, focal adult and sample adult cancer control supplement questionnaires to create a data file with an unusually rich set of measures on disability and Pap smear screening.
Our sample was limited to women aged 21–64 who had not received a diagnosis of a genitourinary cancer (cervical, uterine or ovarian) or reported having a genitourinary problem or a hysterectomy, for a sample of 20,907 women. For our analyses of Pap smear recommendation, we limited the sample to data from 2005, the year in which all women were asked about recommendations. More than 95% of women from the 2005 sample who were eligible for analysis had data about recommendations; our final sample consisted of 9,661 women.*
Measures
We included two outcome measures. Pap smear receipt was a dichotomous variable measuring whether a woman had had a Pap smear in the year prior to the survey. Receipt of a Pap smear recommendation was also a dichotomous variable, which measured whether a woman had been recommended to receive a Pap smear by a health care provider in the previous year.
To measure disability, we used all functional limitation measures available in the NHIS. The NHIS employs a three-part question structure to measure disability. Interviewers first ask respondents whether they are limited in their ability or require help to perform a range of functions or to participate in activities. Those who report a limitation are next asked to identify the type of health condition that causes the limitation and when this health condition first occurred. We incorporated all 31 of the functional limitation variables available on the Person and Focal Adult files, which include Activities of Daily Living limitations and Instrumental Activities of Daily Living limitations.* We used the follow-up question about time of disability onset to identify respondents who had had disabilities for at least one year. Using these measures, we distinguished among four categories of functional limitations: mobility limitations; sensory, mental, cognitive or social limitations; a combination of these two types; and physical limitations unrelated to mobility.*
In addition, we included factors traditionally linked to reproductive health care receipt: age, race and ethnicity, marital status, education, household income, having had at least one birth, geographic region, number of visits to a doctor or other health care professional in the past year, type of health insurance and usual source of care. In our measurement of age, we took into account recommendations that women older than 29 receive less frequent screening if they are at low risk of cervical cancer. Accordingly, women 21–29 were grouped separately from older women.* Type of health insurance distinguished between the uninsured, those with public insurance and those with private insurance. Usual source of care was a dichotomous measure of whether a respondent reported having a place to go other than a hospital emergency room or outpatient department when sick or in need of health advice.
Analyses
We first calculated age-standardized percentage distributions of women by disability status, according to social, demographic and health care characteristics; differences by disability were evaluated with two-tailed t-tests. Next, we conducted a series of logistic regressions: Among the full sample, we investigated the relationship between disability status and Pap smear receipt, and among the 2005 sample, we looked at disability's relationship with receipt of a recommendation for a Pap smear and with Pap smear receipt after receiving a recommendation. In each case, we fitted a regression model using a binary disability indicator representing all those with one or more functional limitations and then fitted a model using a categorical disability indicator distinguishing among the four types of disability. All models were population-weighted and adjusted for the complex survey design of the NHIS.
We assessed missing data on independent variables and found it to be trivial—less than 1% for any individual characteristic, except income, for which it was 21%. We explored multiple approaches to handling the missing income data. Specifically, we compared unweighted and weighted models using complete case analysis, single imputation using mean values on income, multiple imputation using the Markov Chain Monte Carlo method and multiple imputation using chained equations.32,33 Results were robust across all of these strategies, and we present results based on multiple imputation of income using chained equations. We judged this method to be the best in that it allowed us to adjust estimates for complex survey design, as recommended by the National Center for Health Statistics.31 Cases with missing information on independent variables other than income were dropped.
Because women were asked their primary reason for nonreceipt only if they had not received a Pap smear in the past three years, we defined disability to include only women who had had functional limitations for at least three years. This ensured that women classified as having disabilities experienced disability for the full three-year period covered by the reason for nonreceipt. Estimates were age-adjusted, and differences by disability status were assessed with two-tailed t tests.
Results
Sample Characteristics
Overall, 18% of women had disabilities. Among women with disabilities, mobility limitations were the most common type (Table 1): Thirty-seven percent reported having only mobility limitations, and an additional 37% reported a mobility limitation in combination with a sensory, mental, cognitive or social impairment. Some 14% of women with disabilities reported having only sensory, mental, cognitive or social limitations and 11% reported a physical disability that did not limit their mobility.
Table 1. Percentage distribution of women aged 21–64, by selected characteristics, according to disability status, National Health Interview Surveys, 2000 and 2005.
| Characteristic | Disability (N=3,709) | No disability (N=17,198) |
|---|---|---|
| Disability type | ||
| Mobility only | 37.3 | na |
| Sensory/social/mental/cognitive only | 14.4 | na |
| Both | 37.0 | na |
| Other† | 11.3 | na |
| Pap smear receipt in past year | ||
| Yes*** | 68.3 | 75.3 |
| No | 31.7 | 24.7 |
| Age | ||
| 21–29*** | 12.1 | 27.0 |
| 30–39*** | 18.5 | 29.5 |
| 40–64*** | 69.4 | 43.5 |
| Race/ethnicity | ||
| White | 70.2 | 70.8 |
| Black*** | 14.4 | 11.4 |
| Hispanic** | 10.9 | 12.7 |
| Other | 4.4 | 5.0 |
| Education | ||
| <high school graduate*** | 19.2 | 11.0 |
| High school graduate*** | 31.6 | 26.5 |
| Some college | 30.9 | 30.4 |
| college graduate*** | 18.3 | 32.1 |
| Income as % of poverty line | ||
| <100*** | 16.9 | 6.8 |
| 100–299*** | 32.0 | 24.3 |
| 300*** | 33.5 | 48.0 |
| Missing** | 17.6 | 20.9 |
| Marital status | ||
| Married/cohabiting*** | 60.3 | 71.1 |
| Divorced/widowed/separated*** | 19.7 | 14.0 |
| Never-married*** | 20.0 | 15.0 |
| Has had 1 birth | ||
| Yes | 73.7 | 74.5 |
| No | 26.3 | 25.5 |
| Region | ||
| Northeast** | 17.6 | 20.7 |
| Midwest* | 27.8 | 24.8 |
| South | 34.1 | 34.8 |
| West | 20.6 | 19.7 |
| Health insurance | ||
| Public*** | 25.8 | 5.6 |
| Private*** | 55.5 | 78.4 |
| None** | 18.7 | 16.0 |
| Has a usual source of care | ||
| Yes | 86.8 | 86.0 |
| No | 13.2 | 14.0 |
| No. of doctor visits in past year | ||
| 0*** | 7.6 | 14.9 |
| 1–2*** | 29.3 | 49.7 |
| 3*** | 63.1 | 35.4 |
| Survey year | ||
| 2000* | 46.3 | 49.0 |
| 2005* | 53.7 | 51.0 |
| Total | 100.0 | 100.0 |
p<.05.
p<.01.
p<.001.
Includes physical disabilities not involving mobility limitations.
Notes: na=not applicable. All percentages are population-weighted and age-adjusted using U.S. Census 2000 population estimates, except for age and disability type; Ns are unweighted. Percentages may not add to 100% because of rounding.
Sixty-eight percent of women with disabilities had received a Pap smear in the previous year, compared with 75% of women without disabilities. Greater proportions of women with disabilities than those without were aged 40–64, were black, had a high school education or less, had an income of 299% of the federal poverty line or less and were not married or cohabiting. Roughly three-quarters of women, irrespective of disability status, reported having had at least one birth. Twenty-six percent of women with disabilities had public health insurance, compared with 6% of women without disabilities. Sixty-three percent of women with disabilities had visited a doctor three or more times in the past year, compared with 35% of other women.
Multivariate Findings
In multivariate analyses using the binary measure of disability, women with disabilities had 41% lower odds than those without disabilities of having received a Pap smear in the year prior to the survey (odds ratio, 0.6—Table 2). When we conducted further analyses by type of disability, women with mobility limitations had 35% lower odds than those without disabilities of having had a Pap smear (0.7). Women with both mobility limitations and sensory, social, mental or cognitive impairment had even lower odds of Pap smear receipt (0.5); such women were also less likely than women with only mobility limitations to have received a Pap smear (not shown). Having only a sensory, social, mental or cognitive impairment was negatively associated with receipt of a Pap smear (0.5).
Table 2. Odds ratios from logistic regression analyses assessing women's likelihood of having received a Pap smear in the past year, by selected characteristics, according to disability measure.
| Characteristic | Binary | Categorical |
|---|---|---|
| Disability | ||
| None (ref) | 1.00 | 1.00 |
| Any | 0.59*** | na |
| Mobility only | na | 0.65*** |
| Sensory/social/mental/cognitive only | na | 0.54*** |
| Both | na | 0.47*** |
| Other† | na | 0.97 |
| Age | ||
| 21–29 (ref) | 1.00 | 1.00 |
| 30–39 | 0.76*** | 0.76*** |
| 40–64 | 0.50*** | 0.51*** |
| Race/ethnicity | ||
| White (ref) | 1.00 | 1.00 |
| Black | 1.68*** | 1.68*** |
| Hispanic | 1.23** | 1.21** |
| Other | 0.52*** | 0.52*** |
| Education | ||
| <high school graduate | 0.61*** | 0.61*** |
| High school graduate | 0.61*** | 0.61*** |
| Some college | 0.78*** | 0.78*** |
| college graduate (ref) | 1.00 | 1.00 |
| Income as % of poverty line‡ | ||
| <100 | 0.82* | 0.84* |
| 100–299 | 0.76*** | 0.77*** |
| 300 (ref) | 1.00 | 1.00 |
| Marital status | ||
| Married/cohabiting (ref) | 1.00 | 1.00 |
| Divorced/widowed/separated | 0.91 | 0.91 |
| Never-married | 0.59*** | 0.59*** |
| Has had 1 births | ||
| Yes | 1.33*** | 1.32*** |
| No (ref) | 1.00 | 1.00 |
| Region | ||
| Northeast | 1.01 | 1.01 |
| Midwest | 1.01 | 1.01 |
| South | 1.01 | 1.02 |
| West (ref) | 1.00 | 1.00 |
| Health insurance | ||
| Public | 0.85 | 0.91 |
| Private (ref) | 1.00 | 1.00 |
| None | 0.57*** | 0.58*** |
| Has a usual source of care | ||
| Yes | 1.61*** | 1.61*** |
| No (ref) | 1.00 | 1.00 |
| No. of doctor visits in past year | ||
| 0 (ref) | 1.00 | 1.00 |
| 1–2 | 5.67*** | 5.68*** |
| 3 | 8.76*** | 8.91*** |
| Survey year | ||
| 2000 (ref) | 1.00 | 1.00 |
| 2005 | 0.80*** | 0.80*** |
p<.05.
p<.01.
p<.001.
Includes physical disabilities not involving mobility limitations.
Adjusted for family size.
Notes: na=not applicable. ref= reference category.
All of the included characteristics except region were significantly associated with Pap smear receipt, and results were essentially identical in the two models. Women aged 30–39 and those 40–64 were less likely than 21–29-year-olds to have received a Pap smear (odds ratios, 0.8 and 0.5, respectively). Blacks and Hispanics had greater odds than whites of having received a Pap smear (1.7 and 1.2, respectively). Women without health insurance were less likely than those with private insurance to have received a Pap smear (0.6); women with public insurance did not differ from those with private insurance. Having visited the doctor in the past year was strongly and positively associated with Pap smear receipt (5.7 for women with 1–2 visits and 8.9 for women with three or more). Women in the 2005 sample were less likely than those surveyed in 2000 to have received a Pap smear (0.8).*
In analyses using the binary disability measure among women in the recommendation analytical sample, having a disability was positively associated with receipt of a recommendation for a Pap smear (odds ratio, 1.2—Table 3). By disability type, the only association found was for women with only mobility limitations (1.3), although we interpret the null results cautiously because of the small numbers of women in some categories. Having had at least one birth, living in the Northeast or Midwest, having a usual source of care and having visited the doctor in the past year were positively associated with receipt of a Pap smear recommendation (1.3–2.5), whereas being Hispanic and never-married were negatively associated with a recommendation (0.8 and 0.7, respectively).
Table 3. Odds ratios from logistic regression analyses assessing women's likelihood of having received a recommendation for a Pap smear in the past year and of having received a Pap smear after receiving a recommendation, by selected characteristics, according to disability measure.
| Characteristics | Recommendation (N=9,661) | Pap smear (N=5,698) | ||
|---|---|---|---|---|
|
| ||||
| Binary | Categorical | Binary | Categorical | |
| Disability | ||||
| None (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Any | 1.17* | na | 0.51*** | na |
| Mobility only | na | 1.25* | na | 0.52*** |
| Sensory/social/mental/cognitive only | na | 0.85 | na | 0.39*** |
| Both | na | 1.11 | na | 0.47*** |
| Other† | na | 1.27 | na | 0.79 |
| Age | ||||
| 21–29 (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 30–39 | 0.88 | 0.91 | 0.74 | 0.75 |
| 40–64 | 0.88 | 0.89 | 0.44*** | 0.45*** |
| Race/ethnicity | ||||
| White (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 0.94 | 0.92 | 1.94*** | 1.94*** |
| Hispanic | 0.84* | 0.81** | 1.38* | 1.36* |
| Other | 0.80 | 0.77 | 0.98 | 0.97 |
| Education | ||||
| <high school graduate | 0.85 | 0.88 | 0.71 | 0.71 |
| High school graduate | 0.88 | 0.87 | 0.72* | 0.72* |
| Some college | 0.88 | 0.88 | 0.87 | 0.87 |
| college graduate (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Income as % of poverty line‡ | ||||
| <100 | 1.04 | 1.04 | 0.97 | 0.97 |
| 100–299 | 1.03 | 1.01 | 0.79* | 0.79* |
| 300 (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Marital status | ||||
| Married/cohabiting (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Divorced/widowed/separated | 0.98 | 0.97 | 0.81 | 0.82 |
| Never-married | 0.64*** | 0.65*** | 0.61** | 0.62** |
| Has had 1 birth | ||||
| Yes | 1.42*** | 1.42*** | 1.01 | 1.01 |
| No (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Region | ||||
| Northeast | 1.47*** | 1.48*** | 0.82 | 0.82 |
| Midwest | 1.25** | 1.26** | 0.94 | 0.93 |
| South | 0.91 | 0.90 | 1.02 | 1.03 |
| West (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Health insurance | ||||
| Public | 0.85 | 0.88 | 0.70* | 0.74 |
| Private (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| None | 0.93 | 0.94 | 0.49*** | 0.49*** |
| Has a usual source of care | ||||
| Yes | 1.28** | 1.27** | 1.40* | 1.38* |
| No (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| No. of doctor visits in past year | ||||
| 0 (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 1–2 | 1.75*** | 1.77*** | 3.89*** | 3.92*** |
| 3 | 2.48*** | 2.54*** | 5.90*** | 6.01*** |
p<.05.
p<.01.
p<.001.
Includes physical disabilities not involving mobility limitations.
Adjusted for family size.
Notes: na=not applicable. ref=reference category.
Among women who had received a recommendation, disability was negatively associated with receipt of a Pap smear (odds ratio, 0.5). Notably, the reduced likelihood of having received a Pap smear was found among women with mobility limitations and among those with sensory, mental, cognitive or social limitations (0.4–0.5). In addition, Pap smear receipt after recommendation was positively associated with being black or Hispanic, having a usual source of care and having visited the doctor in the past year (1.4–6.0); it was negatively associated with being aged 40–64, having a high school education, being at 100–299% of the federal poverty line, never having been married and not having health insurance (0.5–0.8).
Reasons for Nonreceipt of Pap Smear
Among women in the 2005 sample who had not received a Pap smear in the previous three years, the reasons for nonreceipt are similar for those with and without disabilities (Figure 1). The most common reason for not having a Pap smear was “no reason, not experiencing any problems, or putting it off,” which was given by 42% of women with disabilities and 65% of those without. Thirty-one percent of women with disabilities and 13% of women without cited cost or lack of insurance as their primary reason. Lack of knowledge about Pap smears may have contributed to the large number of women who gave no reason for nonreceipt,34 although we could not evaluate the possibility with these data.
Figure 1. Percentage distribution of women who had not received a Pap smear in the past three years, by primary reason for not having obtained a Pap smear, according to disability status, 2005.
***Difference by disability status significant at p<.001. Note:All percentages are population-weighted and age-adjusted using U.S. Census 2000 population estimates.
Discussion
According to our results, women with disabilities—both mobility limitations and others—are less likely than women without disabilities to receive Pap smears. This result is consistent with the argument that the built environment is an important barrier to health care delivery, but suggests that other barriers may be relevant as well. We found little support for the argument that disabled women are less likely than others to receive a recommendation for a Pap smear; however, among women who receive a recommendation, those with disabilities are less likely than others to receive a Pap smear.
Women with disabilities were almost as likely as others to be insured; nonetheless, they were substantially more likely to cite cost or lack of insurance as their primary reason for not receiving a Pap smear. The observation that insurance coverage alone is not sufficient to ensure use of health services is consistent with findings reported elsewhere. According to a review of the organization and financing of health care for individuals with disabilities, Medicaid offers better coverage for health services needs than either Medicare or private insurers, but necessary preventive care tends to fall by the wayside for people with disabilities, regardless of insurer type.8 Similarly, individuals with disabilities may become frustrated with organizational features of health care financing that leave them financially drained after major disability-related care, which suggests that they may forgo preventive care as a cost-saving strategy.10 In addition, delay in seeking needed medical care may be growing for the U.S. population as a whole;35 the uninsured and insured, many of whom experience higher than average deductibles and copayments, delay care because of cost as well as logistic barriers, such as trouble getting through to a doctor's office on the telephone or scheduling timely appointments. Our findings, when considered in the context of previous research, suggest that future work examine health systems barriers beyond insurance to understand underutilization of cervical cancer screening and other preventive reproductive health services for women with and without disabilities.
Limitations
This study has several limitations. First, although our measure of disability is more inclusive than those that rely solely on activities of daily living, the measures available in the NHIS (and in health surveys to date) limit our ability to fully capture the complexity of disability, especially in how an individual's environment may exacerbate or ameliorate barriers to health care access. We do not have reason to believe, however, that measurement error is nonrandom.
A second limitation is that we were unable to incorporate direct measures of social and community contexts that might shape access to Pap smears, such as distance to care or eligibility for state and local programs that subsidize such testing. Thus, our results do not distinguish between access to Pap smears and receipt of Pap smears.
Finally, we used retrospective data, which introduces the possibility of recall bias. Respondents reported on the onset of disability and timing of Pap smear receipt prior to the survey. Chronic conditions could have arisen over time, making onset difficult to report precisely. Further, recollections of Pap smear receipt may have been imprecise. If women with disabilities were more likely than others to fail to report Pap smears, the negative relationship between disability and Pap smear receipt could be overstated. Given the magnitude of the associations we report, however, we think it unlikely that differential recall bias could account fully for the basic patterns we observe.
Conclusions
In a 2009 study asking more than 80 international experts on disabilities to rank research priorities for the health and well-being of people with disabilities, the identification of barriers to health care was named as the number-one priority.36 The results presented here are consistent with arguments that such barriers need to be addressed to improve the reproductive health care of women with disabilities. The holistic approach taken by ACOG is one promising route. ACOG has developed an interactive site for clinicians providing care to women with disabilities that covers topics ranging from menstruation and fertility to STDs and pregnancy.37 However, the finding that women with disabilities are significantly more likely than others to forgo a Pap smear because of cost concerns suggests that despite the existence of government programs that promote and pay for breast and cervical cancer screening for uninsured and low-income women (such as the CDC's National Breast and Cervical Cancer Early Detection Program),38,39 there may be a need for programs specifically targeted at reducing barriers to reproductive health care for women with disabilities.
Although we have focused on disability and receipt of Pap smear, our analysis can inform understanding of a broader conceptualization of access to reproductive health care—that is, individuals' capacity to obtain appropriate, high-quality medical care from competent health care providers in a timely and efficient manner. One of the primary reasons the Pap smear has been credited with such a dramatic decline in cervical cancer incidence is that it is relatively inexpensive and easy to administer, and can be obtained in a variety of locations, from a general practitioner, an obstetrician-gynecologist or a nurse practitioner.6 Additionally, widely accepted guidelines recommend cervical cancer screening at regular intervals for all women aged 21–64 who have not undergone a hysterectomy. Thus, a better understanding of the factors that result in underutilization could inform discussion about health care access more generally.
Women most at risk for developing cervical cancer are those who do not receive recommended screenings; it is therefore imperative to identify underserved groups. Although recent years have brought the possibility of alternative prevention in the form of an HPV vaccine, according to the CDC, about 30% of cervical cancers will not be prevented by the current vaccine, and all vaccinated women should thus receive regular Pap smears.40 Financial costs of screening with a Pap smear are low, and the real or perceived costs women experience need to be addressed so as to protect all women from unnecessary risk.
Acknowledgments
During the preparation of this article, the first author was supported by National Institute of Child Health & Human Development training grant T32-HD07338 to the Population Studies and Training Center at Brown University
Footnotes
The sampling of individuals with disabilities for national research is likely biased despite the use of proxy respondents (source: Meyers AR and Andresen E, Enabling our instruments: accommodation, universal design, and access to participation in research, Archives of Physical Medicine and Rehabilitation, 2000, 81(12, P.2):S5–S9). Given current interview protocols, individuals with significant communication or cognitive disabling conditions are likely underrepresented. Uncertainty about the exact representation of adults with disabilities is common to research using nationally representative surveys.
The percentage of women missing data on recommendations did not differ by disability, and substantive results were not changed by exclusion of such cases.
Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) limitations refer to the most common sets of items used to measure functional disability, particularly among elderly persons. ADLs cover personal care limitations, such as in bathing or dressing oneself, and IADLs cover household management limitations, such as in cooking meals or managing money (source: Verbrugge, LM and Jette AM, The disablement process, Social Science and Medicine, 1994, 38(1):1–14.).
A mobility disability is a condition necessitating help with personal care needs (bathing, feeding or dressing) or making it difficult to walk, stand, sit, stoop, bend, kneel or reach overhead. A sensory limitation is a condition that creates substantial visual or hearing impairment, including blindness or deafness. A mental or cognitive disability is a condition that creates memory problems or functional limitations (mental retardation, depression, substance abuse or another mental or emotional condition). A social disability is a problem working, engaging in social or leisure activities (e.g., visiting friends, relaxing at home), performing household chores or shopping, because of a physical, mental or emotional condition. Physical limitations unrelated to mobility included limitations in grasping, carrying or pushing.
We tested for an interaction between age and year of survey, but found none.
We tested whether women with disabilities in 2005 were more or less likely than women with disabilities in 2000 to receive a Pap smear, but found no difference.
Contributor Information
Julia A. Rivera Drew, University of Minnesota Population Center, Minneapolis, MN.
Susan E. Short, Department of Sociology and Population Studies and Training Center, Brown University, Providence.
References
- 1.U.S. Cancer Statistics Working Group. United States Cancer Statistics: 2002 Incidence and Mortality. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (CDC) and National Cancer Prevention Institute; 2005. [Google Scholar]
- 2. [accessed Jan. 26, 2010];Mayo Clinic Staff, Cervical cancer. < www.mayoclinic.com/health/cervical-cancer/DS00167>.
- 3.Dunne EF, et al. Prevalence of HPV infection among females in the United States. Journal of the American Medical Association. 2007;297(8):813–819. doi: 10.1001/jama.297.8.813. [DOI] [PubMed] [Google Scholar]
- 4.Berg AO. Screening for cervical cancer: recommendations and rationale: United States Preventive Services Task Force. [accessed: Sept. 11, 2010];2004 < http://www.ispub.com/journal/the_internet_journal_of_oncology/volume_2_number_1_43/article/screening_for_cervical_cancer_recommendations_and_rationale_united_states_preventive_services_task_force.html>.
- 5.Duberstein LD, et al. Provision of contraceptive and related services by publicly funded family planning clinics, 2003. Perspectives on Sexual and Reproductive Health. 2006;38(3):139–147. doi: 10.1363/psrh.38.139.06. [DOI] [PubMed] [Google Scholar]
- 6.Kuo DY, Goldberg GL. Screening of cervical cancer: Where do we go from here? Cancer Investigation. 2003;21(1):157–161. doi: 10.1081/cnv-120016410. [DOI] [PubMed] [Google Scholar]
- 7.Altman B, Bernstein A. Disability and Health in the United States, 2001–2005. Hyattsville, MD: National Center for Health Statistics (NCHS); 2008. [Google Scholar]
- 8.DeJong G, et al. The organization and financing of health services for persons with disabilities. Milbank Quarterly. 2002;80(2):261–301. doi: 10.1111/1468-0009.t01-1-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iezzoni LI, et al. Mobility impairments and use of screening and preventive services. American Journal of Public Health. 2000;90(6):955–961. doi: 10.2105/ajph.90.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Albrecht GL. Rationing health care to disabled people. Sociology of Health and Illness. 2001;23(5):654–677. [Google Scholar]
- 11.Carmona RH, Cabe J. Improving the health and wellness of persons with disabilities: a call to action. American Journal of Public Health. 2005;95(11):1883. doi: 10.2105/ajph.95.11.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American College of Obstetricians and Gynecologists (ACOG) Guidelines for Women's Health Care. second. Washington, DC: ACOG; 2002. pp. 121–134.pp. 140–141. [Google Scholar]
- 13.Smith RA, et al. American Cancer Society guidelines for the early detection of cervical neoplasia and cancer. CA: A Cancer Journal for Clinicians. 2002;52(1):8–22. doi: 10.3322/canjclin.52.1.8. [DOI] [PubMed] [Google Scholar]
- 14.Sawaya GF. Cervical-cancer screening—new guidelines and the balance between benefits and harms. New England Journal of Medicine. 2009;361(26):2303–2505. doi: 10.1056/NEJMp0911380. [DOI] [PubMed] [Google Scholar]
- 15.Saint M, Gildengorin G, Sawaya GF. Current cervical neoplasia screening practices of obstetrician/gynecologists in the US. American Journal of Obstetrics & Gynecology. 2005;192(2):414–421. doi: 10.1016/j.ajog.2004.09.026. [DOI] [PubMed] [Google Scholar]
- 16.Grady D. Guidelines push back age for cervical cancer tests. [accessed Feb 2, 2010];New York Times. 2009 Nov 20; < www.nytimes.com/2009/11/20/health/20pap.html>.
- 17.Hewitt M, Devesa SS, Breen N. Cervical cancer screening among US women: analyses of the 2000 National Health Interview Survey. Preventive Medicine. 2004;39(2):270–278. doi: 10.1016/j.ypmed.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 18.Ramirez A, et al. Disability and preventive cancer screening: results from the 2001 California Health Interview Survey. American Journal of Public Health. 2005;95(11):2057–2064. doi: 10.2105/AJPH.2005.066118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nosek MA, Howland CA. Breast and cervical cancer screening among women with physical disabilities. Archives of Physical Medicine and Rehabilitation. 1997;78(12, Suppl. 5):S39–S44. doi: 10.1016/s0003-9993(97)90220-3. [DOI] [PubMed] [Google Scholar]
- 20.Swan J, et al. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97(6):1528–1540. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 21.Diab ME, Johnston MV. Relationships between level of disability and receipt of preventive health services. Archives of Physical Medicine and Rehabilitation. 2004;85(5):749–757. doi: 10.1016/j.apmr.2003.06.028. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization (WHO) International Classification of Functioning, Disability, and Health. Geneva: WHO; 2001. p. 10. [Google Scholar]
- 23.Kroll T, et al. Barriers and strategies affecting the utilization of primary preventive services for people with physical disabilities: a qualitative inquiry. Health and Social Care in the Community. 2006;14(4):284–293. doi: 10.1111/j.1365-2524.2006.00613.x. [DOI] [PubMed] [Google Scholar]
- 24.Nosek MA, et al. National Study of Women with Physical Disabilities: final report. Sexuality and Disability. 2001;13(1):5–40. [Google Scholar]
- 25.Smeltzer SC. Preventive health screening for breast and cervical cancer and osteoporosis in women with physical disabilities. Family and Community Health. 2006;29(Suppl. 1):35S–43S. doi: 10.1097/00003727-200601001-00007. [DOI] [PubMed] [Google Scholar]
- 26.Havercamp SM, Scandlin D, Roth M. Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in North Carolina. Public Health Reports. 2004;119(4):418–426. doi: 10.1016/j.phr.2004.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O'Toole CJ, Doe T. Sexuality and disabled parents with disabled children. Sexuality and Disability. 2002;20(1):89–101. [Google Scholar]
- 28.Milligan MS, Neufeldt AH. The myth of asexuality: a survey of social and empirical evidence. Sexuality and Disability. 2001;19(2):91–109. [Google Scholar]
- 29.Block P. Sexuality, fertility, and danger: twentieth-century images of women with cognitive disabilities. Sexuality and Disability. 2000;18(4):239–254. [Google Scholar]
- 30.NCHS. [accessed Sept. 23, 2010];Data File Documentation, National Health Interview Survey, 2000 (machine readable data file and documentation) 2002 < http://www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm>.
- 31.NCHS. [accessed Sept. 23, 2010];Data File Documentation, National Health Interview Survey, 2005 (machine readable data file and documentation) 2006 < http://www.cdc.gov/nchs/nhis/nhis_2005_data_release.htm>.
- 32.Horton NJ, Kleinman KP. Much ado about nothing: a comparison of missing data methods and software to fit incomplete data regression models. American Statistician. 2007;61(1):79–90. doi: 10.1198/000313007X172556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Royston P. Multiple imputation of missing values: update. Stata Journal. 2005;5(2):1–14. [Google Scholar]
- 34.Radecki C, Pearson Breitkopf HC, Breitkopf DM. Poor knowledge regarding the Pap test among low-income women undergoing routine screening. Perspectives on Sexual and Reproductive Health. 2005;37(2):78–84. doi: 10.1363/psrh.37.078.05. [DOI] [PubMed] [Google Scholar]
- 35.Maybe I'll get better on my own, editorial. [accessed Jan. 26, 2010];New York Times. 2008 Jun 30; < www.nytimes.com/2008/06/30/opinion/30mon2.html>.
- 36.Tomlinson M, et al. Research priorities for health of people with disabilities: an expert opinion exercise. Lancet. 2009;374(9704):1857–1862. doi: 10.1016/S0140-6736(09)61910-3. [DOI] [PubMed] [Google Scholar]
- 37.American Congress of Obstetricians and Gynecologists, Interactive site for clinicians serving women with disabilities. [accessed Jan. 26, 2010]; < www.acog.org/departments/dept_notice.cfm?recno=38&bulletin=4526>.
- 38.CDC. National breast and cervical cancer early detection program. [accessed Jan. 26, 2010.]; < www.cdc.gov/cancer/nbccedp/>.
- 39.National Women's Law Center and Henry J. Kaiser Family Foundation. Women's Access to Health Care: A State-Level Analysis of Key Health Policies. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2003. [Google Scholar]
- 40.CDC. [accessed Jan. 26, 2010];HPV Fact Sheet. < www.cdc.gov/vaccines/vpd-vac/hpv/default.htm>.