Abstract
Background
Most patients receiving warfarin are man- aged in outpatient office settings or anticoagulation clinics that require frequent visits for monitoring.
Objective
To measure the amount and value of time required of patients for chronic anticoagulation therapy with warfarin.
Design/Participants
Prospective observation of a cohort of adult patients treated at a university-based anticoagulation program.
Measurements
Participants completed a questionnaire and a prospective diary of the time required for 1 visit to the anticoagulation clinic, including travel, waiting, and the clinic visit. The authors reviewed subjects’ medical records to obtain additional information, including the frequency of visits to the anti- coagulation clinic. They used the human capital method to estimate the value of time.
Results
Eighty-five subjects completed the study. The mean (median) total time per visit was 147 minutes (123). Subjects averaged 15 visits per year (14) and spent 39.0 hours (29.3) per year on their visits. Other anticoagulation-related activities, such as communication with providers, pharmacy trips, and extra time preparing food, added an average of 52.7 hours (19.0) per year. The mean annual value of patient time spent traveling, waiting, and attending anticoagulation visits was $707 (median $591). The mean annual value when also including other anticoagulation-related activities was $1799 (median $1132).
Conclusions
The time required of patients for anticoagulation visits was considerable, averaging approximately 2.5 hours per visit and almost 40 hours per year. Methods for reducing patient time requirements, such as home-based testing, could reduce costs for patients, employers, and companions.
Keywords: anticoagulation, warfarin, time, human capital method, health economics
Long-term anticoagulation therapy with warfarin is the mainstay of treatment for venous thrombosis, pulmonary embolism, atrial fibrillation and cardiac valve replacement, with close to 4 million patients taking warfarin in the United States.1 Due to warfarin's narrow therapeutic window and the potential for bleeding or thromboembolic complications, frequent monitoring of the international normalized ratio (INR) is required. Most patients receiving warfarin are managed in outpatient office settings or anticoagulation clinics that require frequent visits for INR monitoring. Thus, the time required of patients may be substantial.
Patient time costs are an important factor in comparing the cost-effectiveness of alternative approaches to warfarin therapy, such as self-monitoring at home and anticoagulation clinic-based management. In addition, they may be an important factor for deciding about whether to use anticoagulation therapy with warfarin v. other treatments (aspirin, no treatment, or low molecular weight heparin in some situations). The consensus Panel on Cost-Effectiveness in Health and Medicine recommends the incorporation of patient time costs in economic analyses.2-5 Measuring and valuing patient time and including it in cost- effectiveness models has been shown to have an important impact on cost-effectiveness results.6-8 Previously published models have either not included or not reported patient time or have used crude estimates of patient time.8-10
Although some studies have reported the amount of patient time related to a variety of other health care activities,3,5,11,12 we found none that have done so adequately for chronic anticoagulation therapy with warfarin. The aim of this study was to use prospective time diaries to measure the patient time requirements for visits (including travel and waiting) for chronic anticoagulation therapy with warfarin and to estimate the economic value of that time. In addition, we sought to measure and value the time patients spend on other anticoagulation-related activities, including communicating with the anticoagulation clinic, obtaining warfarin from the pharmacy, and spending extra time for diet and food preparation.
Methods
Subjects
We enrolled patients from a university-based anticoagulation program within our General Internal Medicine practice between April and November 2007. At that time, our anticoagulation program pro- vided care for 410 patients. The mean age of these patients was 61.4 years (range, 20–93), 59% were male, 62% were white, 30% were African American, and 88% were insured. Our clinic is part of a tertiary care center in a state with a large rural population. All INR testing was done by point-of-care fingerstick using the CoaguChek S meter in our clinic.
The study research assistant (RA) reviewed the daily schedule to identify potentially eligible patients, who were then approached in person. After verifying eligibility, the RA obtained informed consent and presented the study materials. Patients were eligible for inclusion if they were at least 18 years old, on chronic stable warfarin therapy for at least 3 months, and able to complete the study materials. We excluded patients with antiphospholipid antibody syndrome (APLA) due to different treatment (and time) requirements for care and patients who were unable to complete the study materials by themselves or with assistance from our RA or a family member. We also excluded non- English-speaking patients without a friend or family member who could translate for them.
The RA generally spent 2 out of 5 weekdays recruiting subjects. The days of the week spent recruiting varied from month to month. The RA attempted to recruit consecutive patients, but once he began enrolling one subject, he would not be able to approach other potential subjects because of the time required for enrollment and questions. Each day of the week had a similar contribution to our total sample.
Patients who completed the study received a $20 gift card. The study was approved by the University of North Carolina's Biomedical Institutional Review Board.
Measures
Participants were asked to complete a written questionnaire and keep a diary that recorded the time requirements for one visit to the anticoagulation clinic, including travel, waiting, and the clinic visit.
We used previous studies6,7,13-15 and the expertise of our team to develop our diary and questionnaire. We pretested the diary and questionnaire with 10 patients at the study site. The study RA asked patients to read and complete the questionnaires, explaining out loud how they would interpret and answer the questions. Changes were made to the diary and questionnaire based on this feedback.
Subjects enrolled in the study were asked to use a formatted time diary to note the time when 4 steps in the anticoagulation clinic visit process occurred (Appendix 1). Items recorded included when they departed home (or other location) to go to the clinic, arrived at the front desk of the clinic, checked out at the front desk, and arrived at home (or other destination) after the visit. Subjects were instructed to record whether or not they stopped for any reason (such as food or another appointment) between when they left home and arrived home. They were asked to provide the reasons and amounts of time spent for each stop so that this time would not be included. We did not collect data to separate waiting time from time spent receiving services while in the clinic, but such data from a patient flow analysis in our clinic have been published previously.16 Subjects were provided with the time diary at the time of enrollment (visit 1, the index anticoagulation clinic visit) and instructed to complete the diary prospectively during their next anticoagulation clinic visit (visit 2). They were called 2 days prior to the next visit (visit 2) to remind them to complete the diary. After completion, subjects returned the diary to the RA using a self-addressed, postage-paid envelope or in person when they returned to the clinic (visit 3).
The questionnaire was to be completed for the same anticoagulation clinic visit as the diary. It included questions about the overall visit experience, activities missed due to the visit, and time spent in activities related to anticoagulation (Appendix 2). To estimate the incremental time cost for warfarin management compared with other care, we asked patients how much time they spend for each of the following: communicating with the anticoagulation clinic by phone or e-mail, getting their warfarin from the pharmacy (for trips or phone calls), and extra time spent on diet and food preparation because of their anticoagulation. We also asked questions about the following themes: travel costs, the patient's companion, demographic information, occupational history, annual household income, and health (including self-rated overall health and past medical history).
We reviewed subjects’ medical records to obtain the following information: age, frequency of visits to the anticoagulation clinic over the year prior to the index visit, duration of warfarin therapy, warfarin dose, time in therapeutic range (how often their INR was at goal), and indication(s) for warfarin. Time in therapeutic range was calculated as the proportion of INRs within 0.2 of the target range. For example, for subjects with a target range of 2 to 3, values from 1.8 to 3.2 were considered in range.
We used the Rapid Estimate of Adult Literacy in Medicine (REALM) to measure literacy.17 The REALM is a reading cognition assessment tool designed to measure literacy by assessing a patient's recognition of health care terms. It takes approximately 3 minutes to complete.
Data Analysis
We described reported time requirements by means, medians, and ranges. We excluded subjects not returning the diary and questionnaire from our analyses. We examined differences in the time requirements for anticoagulation clinic visits (including travel and waiting) by age, sex, race, educational attainment, income, insurance, employment status, health literacy, travel distance, duration of warfarin therapy, reason for anticoagulation, and time in therapeutic range. We tested these bivariate comparisons using nonparametric statistics because the data were not normally distributed for the key outcome (time). We calculated medians and P values using Wilcoxon rank sum for variables with 2 categories and Kruskal-Wallis for variables with more than 2 categories. We calculated correlations with time for continuous variables using Spearman's correlation. We then conducted multivariate analyses using linear regression; models included all variables found to have significant (P < 0.05) associations with time in bivariate analyses.
We used the human capital method to estimate the value of patients’ time. The human capital method, recommended by the Panel on Cost-Effectiveness in Health and Medicine,2 is based on the following economic reasoning: if a person can choose how many hours to work for pay, he or she will choose to work until the gain from the last hour (the wage) equals the value he or she places on using that hour for unpaid activities.18 Thus, as an approximation, the wage rate indicates the value of the person's time at the margin (i.e., for small changes in activities). If the person chooses not to work, that indicates that he or she values unpaid activities more highly than the market wage he or she could command. Thus, we valued time by multiplying it by the wage rate. To represent a population perspective, we used $19.29 per hour, the national average wage from the June 2006 National Compensation Survey.19 Based on the above reasoning, the appropriate value of time for nonworking hours, or for those outside the workforce, is at least the market wage rate.2 As such, we also used the national average wage for nonworking hours, including participants who were homemakers, retired, or unemployed.
We conducted sensitivity analyses for the annual value of patient time required for anticoagulation clinic visits, including travel and waiting. Our reference case was based on the average population wage rate, our subjects’ actual travel times, our subjects’ actual number of visits, and no companion time. We conducted sensitivity analyses by altering several factors. First, we changed the wage rate, using our subjects’ personal hourly wages, to illustrate the value for our participants rather than the general population. Personal hourly wages were estimated by using the midpoint of the personal annual income range from the questionnaire ($97,500 was used for the $90,000 or greater category) and dividing by 2080 hours (assuming a 40-hour workweek for 52 weeks per year). Second, we used shorter one- way travel times reported in other cost-effectiveness models8-10 to illustrate the possible impact of the relatively long travel times of our subjects. Third, we varied the number of visits per year to those reported in other cost-effectiveness publications.8-10 Finally, we calculated the impact of including companion time for the participants who reported having a companion for their visit.
We also conducted sensitivity analyses for the time spent communicating with the anticoagulation clinic, getting warfarin from the pharmacy, and for diet and food preparation by removing responses for reported times that seemed excessively long. For diet and food preparation, we removed responses of greater than 10 minutes extra per day (16 subjects). For pharmacy trips, we removed those reporting an average of more than 1 trip per month (9 subjects) and those reporting over 2 hours per trip (8 subjects). For e-mails and phone calls communicating with anticoagulation providers, we removed those reporting more than 2 communications per month on average (1 subject reporting 8 per month).
Results
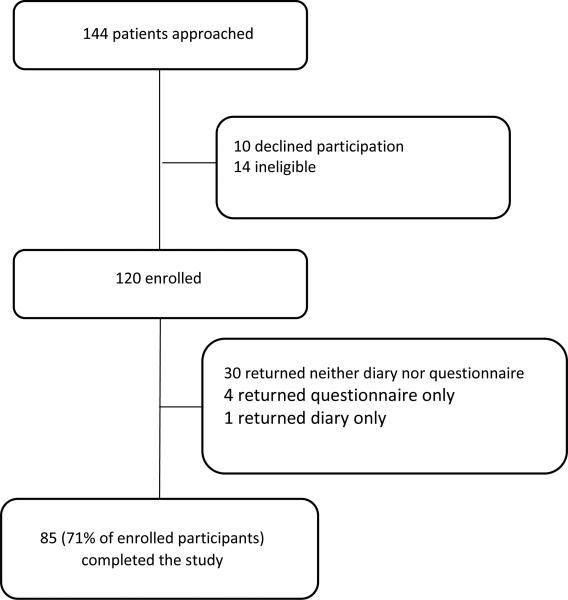
We contacted 144 patients through on-site recruiting. Of these, 120 were enrolled in the study. Thirty-five subjects did not return one or both of the survey materials (diary or questionnaire). Overall, 85 of the 120 enrolled subjects (71%) completed the study (Figure 1).
Figure 1.
Flow of study participants.
Participant characteristics are summarized in Table 1. The mean age of participants was 56.8 years (range, 20–89), 52% were male, 72% were white, 93% were insured, and 46% had annual household incomes under $30,000. The 35 subjects enrolled who did not complete the study were similar in age but were more likely to be male, be African American, and have atrial fibrillation as their indication for anticoagulation. Participants completing the study were similar to the overall anticoagulation clinic population in age, sex, and insurance status but were more likely to be white. Subjects averaged 15 visits per year (median 14) to the anticoagulation clinic.
Table 1.
Participant Characteristics (n=120)
| Percentagea | |||
|---|---|---|---|
| Characteristic | Completers (n=85) | Noncompleters (n=35)b | Overall Anticoagulation Clinic Population (n=410) |
| Mean age (SD) [range] | 56.8 (15.4) [20-89] | 58.5 [20-83] | 61.4 [20-93] |
| % Male | 52 | 63 | 59 |
| Race, % | |||
| White, non-Hispanic | 72 | 54 | 62 |
| Black/African American | 24 | 43 | 30 |
| Other | 4 | 3 | 8 |
| Primary reason for anticoagulation, % | |||
| Atrial fibrillation/flutter | 43 | 54 | 42 |
| Venous thromboembolism | 42 | 20 | 44 |
| Heart valve | 14 | 17 | 14 |
| % Insured | 93 | 66 | 88 |
| % Medicare | 41 | 40 | |
| % Medicaid | 16 | 11 | |
| % Other insurance | 69 | 50 | |
| One-way travel distance (miles), mean (SD) [range]c | 16.9 (18.7) [0-100] | 15.6 (12.3) [1-45] | |
| Warfarin dose, mg/d, mean (SD) [range] | 6.2 (3.5) [0.7-15] | 6.1 (3.3) [1.4-13.6] | |
| Time in therapeutic range, %, mean (SD) [range] | 58.6 (20.1) [0-100] | 59.1 (21.9) [10-94] | |
| Proportion of INRs >4 (or >4.5 for those with target 2.5-3.5), %, mean (SD) [range] | 6.2 (8.6) [0-33] | 8.5 (10.1) [0-33] | |
| Employment status, % | |||
| Employed | 28 | ||
| Unemployed | 5 | ||
| Housewife/husband | 5 | ||
| Retired | 28 | ||
| Disabled | 26 | ||
| Student | 6 | ||
| Other | 5 | ||
| Annual household income range, % | |||
| 0 to $14,999 | 33 | ||
| $15,000 to $29,999 | 13 | ||
| $30,000 to $44,999 | 11 | ||
| $45,000 to $59,999 | 12 | ||
| $60,000 to $74,999 | 0 | ||
| $75,000 to $89,999 | 5 | ||
| $90,000 or greater | 26 | ||
| Education level completed, % | |||
| 7th grade or lower | 1 | ||
| 8th to 11th grade | 9 | ||
| High school graduate or GED | 21 | ||
| Some college or vocational school | 20 | ||
| 2-year college degree | 6 | ||
| 4-year college degree | 20 | ||
| Professional or graduate degree | 23 | ||
| General health (self-rated), % | |||
| Excellent | 8 | ||
| Very good | 21 | ||
| Good | 34 | ||
| Fair | 29 | ||
| Poor | 8 | ||
INR, international normalized ratio.
Percents were rounded to the nearest whole number and may not total 100 due to rounding.
Limited characteristics available for noncompleters because most information was obtained from the self-administered questionnaire that they did not return.
One-way travel distance was based on self-report for those returning the questionnaire. For noncompleters, we calculated one-way travel distance using MapQuest to determine the distance between our clinic and each patient's address of record.
The amount and value of patient time spent on anticoagulation clinic visits and other anticoagulation-related activities are shown in Table 2. The mean time required for 1 visit, including travel and waiting, was 147 minutes. This time was divided among travel to the clinic (mean 46.6 minutes), time in the clinic for waiting and consultation (mean 56.5 minutes), and travel back home (mean 43.7 minutes). Given the average of 15 visits per year, we calculated that subjects spent an average of 39 hours for visits, travel, and waiting. Subjects spent an average of 52.7 hours on other anticoagulation-related activities annually (16.4 hours in sensitivity analyses when excluding excessively long responses). From the human capital method, the mean annual value of patient time spent traveling, waiting, and attending anticoagulation visits was $707 (median $591). The mean annual value of total patient time for traveling, waiting, attending visits, and other anticoagulation-related activities was $1799 (median $1132).
Table 2.
Amount and Value of Patient Time Spent on Anticoagulation Care
| Anticoagulation Clinic Visits | Mean Time (Median) | $ Mean (Median) Valuea | |
|---|---|---|---|
| One visit | Travel to the clinic | 46.6 minutes | |
| Time in clinic (including waiting) | 56.5 minutes (50) | ||
| Travel back home | 43.7 minutes | ||
| Total for travel and time in clinic | 147 minutes (123) | ||
| Annual total for all visits (mean 15 visits) | Visits, travel, and waiting | 39 hoursb (29) | $707 ($591) |
| Other Anticoagulation-Related Activities | Mean Time Per Year (Median, Range) | $ Mean (Median) Valuea | Sensitivity Analyses, Mean Time per Yearc | |
|---|---|---|---|---|
| Diet and food preparation | 40.9 hours (0, 0-274) | 9.5 hours | ||
| Pharmacy trips | 9.4 hours (6, 0-66) | 5.5 hours | ||
| E-mails and phone calls communicating with anticoagulation providers | 1.4 hours (0, 0-32) | 1.1 hours | ||
| Annual total for other anticoagulation-related activities | 52.7 hours (19) | 16.4 hours | ||
| Overall annual total for anticoagulation clinic visits (including travel and waiting) and other anticoagulation-related activitiesd | 93.9 hours (58.7) | $1799 ($1132) | ||
Value of time calculated using the human capital method with an hourly rate of $19.29.
When also including companion time for subjects who had someone accompany them for the visit (26% of subjects), the mean annual time for visits (including travel and waiting) increased from 39 to 48 hours of person time per year.
Data for the times for “other anticoagulation-related activities” were obtained from self-report from the questionnaire (see Web Appendix 2 at http://mdm.sagepub.com/supplemental) rather than prospectively, thus introducing potential recall bias. Results for some of these times revealed mean values that were considerably greater than the median values. Thus, we conducted sensitivity analyses removing unlikely responses. For diet and food preparation, we removed responses of greater than 10 minutes extra per day (16 subjects). For pharmacy trips, we removed those reporting more than an average of 1 trip per month (9 subjects) and those reporting over 2 hours per trip (8 subjects). For e-mails and phone calls communicating with anticoagulation providers, we removed 1 subject reporting an average of 8 communications per month. All other subjects reported between 0 and 2 communications per month for 0 to 60 minutes each, on average.
When also including companion time, the mean annual total increased to 100.5 hours, and the mean value increased to $1939.
The time required for 1 anticoagulation clinic visit (including travel and waiting) was sensitive to the following categorical variables: sex, health literacy, employment status, household income, educational attainment, and whether the patient missed work (Table 3). Time required for anticoagulation clinic visits was correlated with the following continuous variables: age, REALM score (health literacy), time in therapeutic range (TTR), and travel distance. Time requirements decreased with increasing age (correlation −0.29, P = 0.008), with increasing REALM score (− 0.32, P = 0.003), and with increasing TTR (− 0.30, P = 0.006). Increasing travel distance was correlated with increasing time requirements (0.45, P < 0.001). In multivariate linear regression, only travel distance and TTR remained significantly associated with time requirements.
Table 3.
Bivariate Associations between Patient Characteristics and Time Required for One Anticoagulation Clinic Visit, Including Travel and Waiting
| Characteristica | n | Medianb | Pb |
|---|---|---|---|
| Male | 45 | 105 | 0.029 |
| Female | 40 | 140 | |
| REALM categoryc | |||
| 3rd grade and below (0-18) | 0 | 0.024 | |
| 4th to 6th grade (19-44) | 5 | 190 | |
| 7th to 8th grade (45-60) | 9 | 150 | |
| High School (61-66) | 71 | 115 | |
| Medicare | |||
| Yes | 36 | 109.5 | 0.03 |
| No | 50 | 133.5 | |
| Medicaid | |||
| Yes | 14 | 140 | 0.038 |
| No | 72 | 115 | |
| Other insurance | 59 | 112 | 0.014 |
| No other insurance | 27 | 140 | |
| Current employment status | |||
| Employed | 23 | 105 | 0.002 |
| Unemployed | 4 | 142.5 | |
| Housewife/husband | 3 | 100 | |
| Retired | 24 | 94 | |
| Disabled | 21 | 180 | |
| Student | 5 | 115 | |
| Other | 4 | 122.5 | |
| Annual household income range | |||
| 0 to $14,999 | 26 | 150 | 0.029 |
| $15,000 to $29,999 | 11 | 160 | |
| $30,000 to $44,999 | 9 | 100 | |
| $45,000 to $59,999 | 10 | 131.5 | |
| $60,000 to $74,999 | 0 | ||
| $75,000 to $89,999 | 4 | 117.5 | |
| $90,000 or greater | 19 | 112 | |
| Education | |||
| 7th grade or lower | 1 | 150 | 0.011 |
| 8th to 11th grade | 8 | 190 | |
| High school graduate or GED | 18 | 150 | |
| Some college or vocational school | 16 | 119.5 | |
| 2-year college degree | 5 | 125 | |
| 4-year college degree | 16 | 101 | |
| Professional or graduate degree | 19 | 100 | |
| Missed work | 25 | 105 | 0.018 |
| Did not miss work | 60 | 133.5 | |
Bivariate associations are only shown for those factors with statistically significant associations with time (P < 0.05). Race, target international normalized ratio range, primary reason for anticoagulation, duration of warfarin therapy, who accompanied the patient, self-rated general health, insurance status, and satisfaction with the clinic were not significantly associated (P > 0.05).
Medians and P values calculated using Wilcoxon rank-sum tests for variables with 2 categories and Kruskal-Wallis tests for variables with more than 2 categories. For variables with more than 2 categories, the P values reported are those for the entire variable group.
REALM scores range from 0 to 66 and are divided into 4 categories: (1) 3rd grade and below, scores of 0 to 18, subject will not be able to read most low literacy materials and will need repeated oral instructions and materials composed primarily of illustrations or audio- or videotapes; (2) 4th to 6th grade, scores of 19 to 44, will need low literacy materials and may not be able to read prescription labels; (3) 7th to 8th grade, scores of 45 to 60, will struggle with most patient education materials; (4) high school, scores of 61 to 66, will be able to read most patient education materials.
Results of our sensitivity analyses for the annual value of patient time required for anticoagulation clinic visits are shown in Table 4. Our first sensitivity analysis, using our subjects’ personal hourly wages, which averaged $16.89, decreased the mean (median) annual value of patient time required for anticoagulation clinic visits from $707 ($591) to about $504 ($370). In our next sensitivity analysis, we adjusted the one-way travel time to 20, 30, and 40 minutes. This decreased the mean annual value of patient time to $465 ($434), $562 ($530), and $658 ($627), respectively. Adjusting the number of visits per year to 18 and 24 resulted in an increase in mean annual value to $849 ($709) and $1132 ($945), respectively. Last, we included companion time for the 26% of subjects who were accompanied for their visit. This resulted in an increase in mean annual value up to $921 ($644) of person time.
Table 4.
Sensitivity Analyses for the Annual Value of Patient Time Required for Anticoagulation Clinic Visits, Including Travel and Waiting
| Mean (Median) Annual Hours | Mean (Median) Annual Value | |
|---|---|---|
| Reference case | ||
| Mean US population wage rate of $19.29 | ||
| One-way travel time of our subjects (mean, 57 minutes) | 39 (29) | $707 (591) |
| Our subjects’ actual number of visits per year (mean, 15) | ||
| No companion time | ||
| Sensitivity analyses | ||
| Using our subjects’ personal hourly wages (mean, $16.89; median, $10.82) | Same as reference case | $504 (370) |
| One-way travel time | ||
| 20 minutes | $465 (434) | |
| 30 minutes | 24 (23) | $562 (530) |
| 40 minutes | 29 (28) | $658 (627) |
| Visits per year | 34 (33) | |
| 18 | 44 (37) | $849 (709) |
| 24 | 59 (49) | $1132 (945) |
| Including companion time for the 26% of subjects who reported having a companion for the anticoagulation clinic visit | 48 (33) | $921 (644) |
Discussion
In this study, the time required of patients for anticoagulation visits (including travel and waiting) was considerable, averaging approximately 2.5 hours per visit and almost 40 hours per year. Travel time accounted for almost two thirds of the time related to clinic visits. When including the time invested by patients’ companions, the total person time required for anticoagulation visits was about 50 hours per year.
In addition to time spent on visits, patients reported spending a substantial amount of time on other anticoagulation-related activities, including about 40 hours per year of extra time for diet and food preparation beyond the amount they would spend if they were not on warfarin. Our results for the time spent on other anticoagulation-related activities may seem greater than expected. Our sensitivity analyses (removing responses that seemed excessively long) found considerably shorter times for diet and food preparation and pharmacy trips, suggesting that the responses of a small percentage of subjects may have resulted in overestimates or that a small percentage of subjects spend a much larger than expected amount of time on some activities. Notably, even if the time spent on other anticoagulation activities is not considered, patients treated with warfarin still spent a considerable amount of time on visits, travel, and waiting.
Management strategies for patients on chronic warfarin therapy include home self-monitoring (either self-testing with self-management or self-testing with clinician management), anticoagulation clinic management, and primary care physician management. Differences in the time required of patients for these different management strategies can affect their relative cost-effectiveness.8,9 In addition, the time required for treatment is important information for patients with atrial fibrillation and their providers to make informed decisions about whether to begin chronic anticoagulation therapy with warfarin v. aspirin or no treatment.
Although self-monitoring has been reported to be more effective than standard monitoring (i.e., by anticoagulation clinics or personal physicians), with improvement in both the benefits and harms related to anticoagulation and a reduction in death from all causes, cost-effectiveness analyses have reached mixed conclusions about the value of self-monitoring.8,10,20-30 Some analyses have found self-monitoring to be cost- saving, whereas others have reported a relatively high cost per quality-adjusted life year (QALY) gained.9 One potential reason for these differences is how these analyses accounted for patient time. Just 2 out of 7 cost-effectiveness analyses comparing self-monitoring to other models of managing long-term oral anticoagulation included patient time costs.8,10,27-30 One of these compared anticoagulation clinic care with patient self-testing.8 The model included 20 minutes of patient time for the anticoagulation clinic visit and 52 minutes of travel time per patient. When the time and travel costs were included, the incremental cost- effectiveness ratio for patient self-testing changed from $153,000 per QALY to being cost-saving.
Several previously published studies have focused on measuring the time that patients spend in health- related activities.6,7,13,31-46 Some measured visit time or clinic time but ignored travel time, waiting time, or other time invested.40,45 Others have measured time away from work.36 We tried to measure all the relevant time intervals invested in the anticoagulation clinic visit process from a patient perspective. In addition, a strength of our study is the prospective design, with real-time patient experiences recorded in time diaries, thus reducing the potential for measurement bias and recall bias. Most previous studies measured patient time using clinic schedules or retrospective surveys.13,14,32,35,36,42,45-48 Few used prospective patient time diaries,6,7 which may be a better way to obtain reliable data on time allocation.49
One study with 20 patients measured and reported a component of the time patients spend monitoring warfarin.31 The study was designed to compare the cost-effectiveness of monitoring INR using venipuncture v. fingerstick testing (for practice-based anticoagulation). It aimed to measure only the time and costs for the testing itself rather than all time related to a visit that included clinical care. It measured patient waiting time for a nurse, patient/nurse encounter time, and INR testing time. Patients spent an average of 20 minutes for venipuncture testing and 16.2 minutes for fingerstick testing. The difference between these times and those measured in our study (mean 56.5 minutes, not including travel) can be explained by differences in the time intervals that were measured and in the services provided.
A study using data from the American Time Use Survey (ATUS), a telephone survey conducted by the Census Bureau for the Bureau of Labor Statistics, determined the average time costs of outpatient visits (not specific to anticoagulation clinic visits).43 Respondents were asked how they spent the 24 hours beginning at 4 a.m. the day before the call. During the first 4 years of the survey (2003-2006), 1621 out of over 60,000 respondents reported spending an average of 121 minutes on outpatient care.43
The Panel on Cost-Effectiveness in Health and Medicine recommends the incorporation of patient time costs in economic analyses.2 In addition, it supports the use of the human capital method, which is dependent on accurate measures of time, to value time.2 Although time diaries have been considered the gold standard for measuring time,43,49 it is not clear when other measures, such as retrospective questionnaires, are sufficient. Whether prospective studies using real-time diaries, which may be time and resource intensive, are necessary or if information from published retrospective studies or the ATUS should be used may differ depending on the situation. The ATUS showed that the average total time spent on an outpatient visit was 121 minutes compared with the mean of 147 minutes (median 123) in our study. But is that difference likely to have enough impact on cost-effectiveness results to make it worthwhile to do a separate study?
Measuring time prospectively with real-time diaries as we have done is likely the most accurate method of measuring time because it minimizes the potential for measurement bias (from recall bias). However, prospective time diaries and 24-hour recall have not been compared head-to-head for common settings and situations to determine the magnitude of difference between the 2 methods. Nevertheless, we hypothesize that there are some circumstances where it is worthwhile for analysts to make the effort to measure patient time prospectively and others where they could use numbers from other sources.
For cost-effectiveness analyses conducted from the societal perspective, for common health conditions, it seems reasonable to use published data from retrospective surveys such as the ATUS for time spent on travel, waiting, and visits. The ATUS has the advantage of representing subjects from all over the United States, rather than one location as most other studies of patient time have been. Conversely, surveys such as the ATUS that measure time in general without obtaining any information about health conditions or the type of provider seen make it difficult to determine what to attribute the time costs to. If analysts need to accurately determine patient time costs for a specific condition rather than for visits in general, then it may be necessary to conduct a separate study. Otherwise, they may be overestimating time costs by attributing them to just one condition, when the time may be related to care for several conditions.
The frequency and number of relevant events should be considered in determining whether a separate study is indicated. For example, treatments that require a large number of visits, such as radiation oncology treatments for some cancers, may necessitate more accurate measurement of patient time. This is also the case for anticoagulation therapy with warfarin, where small errors in the measurement of time spent per visit would be multiplied many times when calculating annual time costs. An error of just 10 minutes per visit would lead to an error of 150 minutes per year (assuming 15 visits per year), worth $48.23 per patient per year. With close to 4 million patients taking warfarin in the United States, the error in societal time costs resulting from inaccurate measurement would be substantially large.1
Another important consideration in determining whether a separate study is necessary is whether there are potential interventions that can do any- thing to improve (often by reducing) patient time costs. For instance, quality improvement efforts to decrease patient time spent in care or to improve efficiency, such as to decrease patient waiting times, should rely on local prospective data rather than previously published literature.
Cost-effectiveness analyses that focus on patients from rural locations may underestimate travel times if they use data from previously published studies. In our study, for example, travel times were longer than societal averages (mean approximately 90 minutes in our study compared with 35 minutes from the ATUS)43 because our clinic is a tertiary care center located in a relatively rural state. Thus, if one was attempting to determine the cost-effectiveness of home monitoring compared with anticoagulation clinic care, results may differ if the analysis considers only rural locations as opposed to urban locations or an “average” location. For locations where patients have longer travel times, home monitoring would be more cost-effective than locations where patients have shorter travel times.
Perhaps most important, prior to using their own time and resources, analysts should consider the potential impact of patient time on the incremental cost-effectiveness ratio. In situations where patient, companion, or caregiver time invested will be roughly equal among the options being considered, it is likely not necessary to conduct separate studies to determine time costs. On the other hand, if large differences in time between the options being considered are hypothesized, separate studies may be necessary.
Our study has several limitations. First, 29% of subjects did not complete the study, which may have affected our results. Analyses of the noncompleters do not suggest a clear direction of this bias. Noncompleters were less likely to be female and less likely to be insured, which would suggest their time requirements would be greater, according to our bivariate analyses. However, they were less likely to be white, which would suggest their time requirements would be less than completers. Next, our study is based on one site with a structured anticoagulation program that uses fingerstick INR testing. Our anticoagulation clinic providers and staff have conducted multiple quality improvement activities designed to improve clinic efficiency. For example, one quality improvement intervention in our clinic decreased mean visit time (from 84 to 59 minutes) and waiting time between check-in and INR testing (from 28 to 4 minutes).16 In addition, travel times may be longer than other sites due to our role as a tertiary care center in a rural state.
Another potential limitation is that our measure may have slightly overestimated travel time. Although we explicitly asked subjects to record any stops between the time they left home and arrived home so this time would not be included, we did not explicitly ask them to include travel time related to the stops. Some of these stops may have been on the route home and not added additional travel time; others may have required additional travel time. About one third (29/85, 34%) of subjects reported stopping for any reason between when they left home and arrived home. Finally, although the time for travel, waiting, and visits was measured prospectively in ‘real time,” the time for other anticoagulation-related activities was based on patient recall of time spent recently and extrapolated to annual values, introducing possible measurement bias.
In conclusion, the time required of patients for chronic oral anticoagulation is considerable. Methods for reducing patient time requirements, such as home-based testing or self-monitoring, could reduce costs for patients, employers, and companions. Analysts should contemplate their specific context of interest to determine whether it is essential to mea- sure time prospectively with real-time experiences or if retrospective surveys or general estimates from other sources will suffice.
Supplementary Material
Footnotes
Some of these data were presented as an oral presentation at the meeting of the Society for General Internal Medicine, 9–12 April 2008, Pittsburgh, Pennsylvania.
References
- 1.AHRQ announces guide to help patients on Coumadin1/warfarin therapy. Available from: http://www.ahrq.gov/research/jul08/0708RA1.htm.
- 2.Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost- Effectiveness in Health and Medicine. Oxford University Press; New York: 1996. [Google Scholar]
- 3.Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1172–7. [PubMed] [Google Scholar]
- 4.Siegel JE, Weinstein MC, Russell LB, Gold MR. Recommendations for reporting cost-effectiveness analyses. Panel on Cost- Effectiveness in Health and Medicine. JAMA. 1996;276:1339–41. doi: 10.1001/jama.276.16.1339. [DOI] [PubMed] [Google Scholar]
- 5.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1253–8. [PubMed] [Google Scholar]
- 6.Jonas DE, Russell LB, Sandler RS, Chou J, Pignone M. Patient time requirements for screening colonoscopy. Am J Gastroenterol. 2007;102:2401–10. doi: 10.1111/j.1572-0241.2007.01387.x. [DOI] [PubMed] [Google Scholar]
- 7.Jonas DE, Russell LB, Sandler RS, Chou J, Pignone M. Value of patient time invested in the colonoscopy screening process: time requirements for colonoscopy study. Med Decis Making. 2008;28:56–65. doi: 10.1177/0272989X07309643. [DOI] [PubMed] [Google Scholar]
- 8.Lafata JE, Martin SA, Kaatz S, Ward RE. The cost-effectiveness of different management strategies for patients on chronic warfarin therapy. J Gen Intern Med. 2000;15:31–7. doi: 10.1046/j.1525-1497.2000.01239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Connock M, Stevens C, Fry-Smith A, et al. Clinical effective- ness and cost-effectiveness of different models of managing long- term oral anticoagulation therapy: a systematic review and economic modelling. Health Technol Assess. 2007;11:iii–iv. ix–66. doi: 10.3310/hta11380. [DOI] [PubMed] [Google Scholar]
- 10.Jowett S, Bryan S, Murray E, et al. Patient self-management of anticoagulation therapy: a trial-based cost-effectiveness analysis. Br J Haematol. 2006;134:632–9. doi: 10.1111/j.1365-2141.2006.06243.x. [DOI] [PubMed] [Google Scholar]
- 11.Pignone M, Levin B. Recent developments in colorectal cancer screening and prevention. Am Fam Physician. 2002;66:297–302. [PubMed] [Google Scholar]
- 12.Frew E, Wolstenholme JL, Whynes DK. Willingness-to-pay for colorectal cancer screening. Eur J Cancer. 2001;37:1746–51. doi: 10.1016/s0959-8049(01)00200-3. [DOI] [PubMed] [Google Scholar]
- 13.Frew E, Wolstenholme JL, Atkin W, Whynes DK. Estimating time and travel costs incurred in clinic based screening: flexible sigmoidoscopy screening for colorectal cancer. J Med Screen. 1999;6:119–23. doi: 10.1136/jms.6.3.119. [DOI] [PubMed] [Google Scholar]
- 14.Safford MM, Russell L, Suh DC, Roman S, Pogach L. How much time do patients with diabetes spend on self-care? J Am Board Fam Pract. 2005;18:262–70. doi: 10.3122/jabfm.18.4.262. [DOI] [PubMed] [Google Scholar]
- 15.Whynes DK, Frew E, Wolstenholme JL. A comparison of two methods for eliciting contingent valuations of colorectal cancer screening. J Health Econ. 2003;22:555–74. doi: 10.1016/S0167-6296(03)00006-7. [DOI] [PubMed] [Google Scholar]
- 16.Potisek NM, Malone RM, Shilliday BB, et al. Use of patient flow analysis to improve patient visit efficiency by decreasing wait time in a primary care-based disease management programs for anticoagulation and chronic pain: a quality improvement study. BMC Health Serv Res. 2007;7:8. doi: 10.1186/1472-6963-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–5. [PubMed] [Google Scholar]
- 18.Phelps CE. Health Economics. 3rd ed. Addison Wes- ley; Boston: 2003. [Google Scholar]
- 19.Bureau of Labor Statistics National Compensation Survey. 2006 Jun; Available from: http://www.bls.gov/ncs/ncspubs_2006.htm.
- 20.Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133(suppl):160S–198S. doi: 10.1378/chest.08-0670. [DOI] [PubMed] [Google Scholar]
- 21.Hirsh J, Fuster V, Ansell J, Halperin JL. American Heart Association/American College of Cardiology Foundation guide to warfarin therapy. Circulation. 2003;107:1692–711. doi: 10.1161/01.CIR.0000063575.17904.4E. [DOI] [PubMed] [Google Scholar]
- 22.Agency for Healthcare Research and Quality . Your Guide to Coumadin1/Warfarin Therapy. AHRQ Pub. No. 08-0028-A. Agency for Healthcare Research and Quality; Rockville, MD: 2008. Available from: http://www.ahrq.gov/consumer/coumadin.htm. [Google Scholar]
- 23.The Role of Vitamin K and COUMADIN Use [brochure] Bristol-Myers Squibb Company; New York: 2008. Available from: http://www.coumadin.com/pdf/293US08WA03002_v9_Vitamin KBro_8.5x11.pdf. [Google Scholar]
- 24.Selden CR, Zorn M, Ratzan SC, Parker RM, editors. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. National Institutes of Health, US Department of Health and Human Services; Bethesda, MD: 2000. Pub. No. CBM 2000-1. Available from: http://www.nlm.nih.gov/archive//20061214/pubs/cbm/hliteracy.html. [Google Scholar]
- 25.CMS Manual System National Coverage Determinations Publication 100-3, Transmittal 90. 2008 Available from: http://www.cms.hhs.gov/Transmittals/Downloads/R90NCD.pdf.
- 26.Heneghan C, Alonso-Coello P, Garcia-Alamino JM, et al. Self- monitoring of oral anticoagulation: a systematic review and meta-analysis. Lancet. 2006;367:404–11. doi: 10.1016/S0140-6736(06)68139-7. [DOI] [PubMed] [Google Scholar]
- 27.Taborski U, Wittstamm FJ, Bernardo A. Cost-effectiveness of self-managed anticoagulant therapy in Germany. Semin Thromb Hemost. 1999;25:103–7. doi: 10.1055/s-2007-996432. [DOI] [PubMed] [Google Scholar]
- 28.Muller E, Bergemann R, GELIA Study Group Economic anal- ysis of bleeding and thromboembolic sequelae after heart valve replacement (GELIA 7). Eur Heart J Suppl. 2001;3:Q65–9. [Google Scholar]
- 29.de Sola-Morales Serra O, Elorza Ricart JM. Portable coagulometers: a systematic review of the evidence on self-management of oral anticoagulant treatment [in Spanish]. Med Clin (Barc) 2005;124:321–5. doi: 10.1157/13072418. [DOI] [PubMed] [Google Scholar]
- 30.Regier DA, Sunderji R, Lynd LD, Gin K, Marra CA. Cost- effectiveness of self-managed versus physician-managed oral anticoagulation therapy. CMAJ. 2006;174:1847–52. doi: 10.1503/cmaj.051104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ansell JE, Hamke AK, Holden A, Knapic N. Cost effectiveness of monitoring warfarin therapy using standard versus capillary prothrombin times. Am J Clin Pathol. 1989;91:587–9. doi: 10.1093/ajcp/91.5.587. [DOI] [PubMed] [Google Scholar]
- 32.Cantor SB, Levy LB, Cardenas-Turanzas M, et al. Collecting direct non-health care and time cost data: application to screening and diagnosis of cervical cancer. Med Decis Making. 2006;26:265–72. doi: 10.1177/027298906288679. [DOI] [PubMed] [Google Scholar]
- 33.Mandelblatt JS, Lawrence WF, Womack SM, et al. Benefits and costs of using HPV testing to screen for cervical cancer. JAMA. 2002;287:2372–81. doi: 10.1001/jama.287.18.2372. [DOI] [PubMed] [Google Scholar]
- 34.Shireman TI, Tsevat J, Goldie SJ. Time costs associated with cervical cancer screening. Int J Technol Assess Health Care. 2001;17:146–52. doi: 10.1017/s0266462301104137. [DOI] [PubMed] [Google Scholar]
- 35.Bech M, Gyrd-Hansen D. Cost implications of routine mammography screening of women 50–69 years in the county of Funen, Denmark. Health Pol. 2000;54:125–41. doi: 10.1016/s0168-8510(00)00104-4. [DOI] [PubMed] [Google Scholar]
- 36.Secker-Walker RH, Vacek PM, Hooper GJ, Plante DA, Detsky AS. Screening for breast cancer: time, travel, and out-of-pocket expenses. J Natl Cancer Inst. 1999;91:702–8. doi: 10.1093/jnci/91.8.702. [DOI] [PubMed] [Google Scholar]
- 37.Bryan S, Buxton M, McKenna M, Ashton H, Scott A. Private costs associated with abdominal aortic aneurysm screening: the importance of private travel and time costs. J Med Screen. 1995;2:62–6. doi: 10.1177/096914139500200202. [DOI] [PubMed] [Google Scholar]
- 38.Lawrence WF, Peshkin BN, Liang W, et al. Cost of genetic counseling and testing for BRCA1 and BRCA2 breast cancer susceptibility mutations. Cancer Epidemiol Biomarkers Prev. 2001;10:475–81. [PubMed] [Google Scholar]
- 39.Stringer M. Personal costs associated with high-risk prenatal care attendance. J Health Care Poor Underserved. 1998;9:222–35. doi: 10.1353/hpu.2010.0248. [DOI] [PubMed] [Google Scholar]
- 40.Attard NJ, Zarb GA, Laporte A. Long-term treatment costs associated with implant-supported mandibular prostheses in edentulous patients. Int J Prosthodont. 2005;18:117–23. [PubMed] [Google Scholar]
- 41.Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research. JAMA. 1997;278:1759–66. [PubMed] [Google Scholar]
- 42.Robbins JM, Tilford JM, Gillaspy SR, et al. Parental emotional and time costs predict compliance with respiratory syncytial virus prophylaxis. Ambul Pediatr. 2002;2:444–8. doi: 10.1367/1539-4409(2002)002<0444:peatcp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 43.Russell LB, Ibuka Y, Carr D. How much time do patients spend on outpatient visits? The American Time Use Survey. Patient. 2008;1:211–222. doi: 10.2165/1312067-200801030-00008. [DOI] [PubMed] [Google Scholar]
- 44.Salome HJ, French MT, Miller M, McLellan AT. Estimating the client costs of addiction treatment: first findings from the client drug abuse treatment cost analysis program (Client DATCAP). Drug Alcohol Depend. 2003;71:195–206. doi: 10.1016/s0376-8716(03)00133-9. [DOI] [PubMed] [Google Scholar]
- 45.Sculpher M, Palmer MK, Heyes A. Costs incurred by patients undergoing advanced colorectal cancer therapy: a comparison of raltitrexed and fluorouracil plus folinic acid. Pharmacoeconomics. 2000;17:361–70. doi: 10.2165/00019053-200017040-00006. [DOI] [PubMed] [Google Scholar]
- 46.Yabroff KR, Warren JL, Knopf K, Davis WW, Brown ML. Estimating patient time costs associated with colorectal cancer care. Med Care. 2005;43:640–8. doi: 10.1097/01.mlr.0000167177.45020.4a. [DOI] [PubMed] [Google Scholar]
- 47.Stringer M, Ratcliffe SJ, Evans EC, Brown LP. The cost of pre- natal care attendance and pregnancy outcomes in low-income working women. J Obstet Gynecol Neonatal Nurs. 2005;34:551–60. doi: 10.1177/0884217505280276. [DOI] [PubMed] [Google Scholar]
- 48.Whitney CW, Milgrom P, Conrad D, Fiset L, O’Hara D. The relationship between price of services, quality of care, and patient time costs for general dental practice. Health Serv Res. 1997;31:773–790. [PMC free article] [PubMed] [Google Scholar]
- 49.Juster FT, Stafford FP. The allocation of time: empirical findings, behavioral models, and problems of measurement. J Econ Lit. 1991;29:471–522. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.