Abstract
Background
It is commonly assumed that globally CVD risk factors are associated with affluence and Westernization. We investigated the associations of body mass index (BMI), fasting plasma glucose (FPG), systolic blood pressure (SBP), and serum total cholesterol (TC) with national income, Western diet, and (for BMI) urbanization in 1980 and 2008.
Methods and Results
Country-level risk factor estimates for 199 countries between 1980 and 2008 were from a previous systematic analysis of population-based data. We analyzed the associations between risk factors and natural logarithm of per-capita GDP [Ln(GDP)], a measure of Western diet, and (for BMI) percent population living in urban areas. In 1980, there was a positive association between national income and population mean BMI, SBP, and TC. By 2008, the slope of the association between Ln(GDP) and SBP became negative for women and zero for men. TC was associated with national income and Western diet throughout the period. In 1980, BMI rose with per-capita GDP and then flattened at about Int$7000; by 2008, the relationship resembled an inverted-U for women, peaking at middle income levels. BMI had a positive relationship with percent urban population in both 1980 and 2008. FPG had weaker associations with these country macro characteristics, but was positively associated with BMI.
Conclusions
The changing associations of metabolic risk factors with macroeconomic variables indicate that there will be a global pandemic of hyperglycemia and diabetes, together with high blood pressure in low income countries, unless effective lifestyle, and pharmacological interventions are implemented.
Keywords: obesity, hypertension, hypercholesterolemia, diabetes mellitus, epidemiology
Introduction
Cardiovascular diseases (CVD) are the leading cause of death and disease burden worldwide. Population aging leads to increase in CVD deaths because CVD mortality rises with age. In addition to aging, age-specific mortality rates may increase or decline over time. Age-specific CVD death rates are themselves affected by exposure to risk factors such as such as excess weight, smoking, and high blood pressure, cholesterol, and glucose, and by treatment availability and quality.
Access to treatment tends to rise with income1. While the association between CVD risk factors and socioeconomic status has been studied within countries, few studies have assessed the cross-country association of CVD risk factors with national macroeconomic variables2–4. Some studies have postulated that CVD risk factors may rise with national income or urbanization, due to a ’Westernized’ diet and lifestyle5, 6, referred to as the so-called ‘diseases of affluence’ or ’Western diseases’ paradigm; others have concluded that higher income and urban infrastructure may help reduce CVD risk factors through healthier lifestyle or better access to preventive interventions and primary care7. Even less is known about how these associations have changed over time with the availability of new public health and clinical programs, and with globalization of medicines and foods8, 9. Understanding the relationship between socioeconomic factors and CVD risk factors at the population level is essential to understand the role of risk factors in the epidemiological transition and to inform national and global policies and priorities. Individual-level studies that provide evidence on causal effects do not deal with changes in whole populations.
We investigated the population-level associations of major metabolic risk factors – body mass index (BMI), fasting plasma glucose (FPG), systolic blood pressure (SBP), and serum total fasting cholesterol (TC) – with national income, Western diet, and (for BMI only) urbanization in 1980 and 2008. While some of the associations reported here may be causal, they should not be generally interpreted as such because factors like national income and urbanization may themselves be correlated, making inferences about causal effects neither feasible nor possibly relevant. Rather, population-level analysis demonstrates how risk factors, whose causal effects on CVD are established in individual-level epidemiological studies, are distributed across countries in relation to the degree of social and economic development, and how these patterns have changed over time.
Methods
Risk factor levels by sex, country, and year
Mean BMI, FPG, SBP, and TC were from a systematic analysis of population-based data, by sex, for 199 countries and territories, as described in detail in previous publications10–13. In brief, we reviewed and accessed published and unpublished health examination surveys and population-based epidemiological studies to collate comprehensive data on these four risk factors between 1980 and 2008. There were 960 data sources across countries and years for BMI, 786 for SBP, 321 for TC, and 370 for FPG. Data in some sources were gathered in a single year while others covered more than one year. Counting each source as one country-year, these numbers are equivalent to 17% of all 5,771 country-years for which estimates were made for BMI, 14% for SBP, 5.5% for TC, and 6.5% for FPG. These figures should be compared with a recommended survey frequency of about one in five years, i.e. 20% of all country-years;14 to our knowledge only Japan has an annual health examination survey. The number of countries with no data ranged from 30 (i.e. 15%) for BMI to over 100 (i.e. over 50%) for TC.
For each risk factor, we developed and applied a Bayesian statistical model to impute missing data. The model incorporated the hierarchical nature of the data, non-linear time trends and age associations, and national vs. subnational and community representativeness of data. Using these data and methods, we estimated risk factor levels and their uncertainties by age and sex for each country-year. The uncertainties are larger for risk factors, countries, and years without data or with data that were not from a nationally representative survey (see Supplemental Materials for statistical details on how uncertainty due to missing data was incorporated in all analyses). We estimated age-standardized means using the WHO standard population to account for the fact that the age composition varies across countries and over time.
National income, urbanization, and Western diet
National income was measured as per-capita gross domestic product (GDP) converted to international dollars and adjusted for inflation with a base year of 2005.15 Urbanization was measured as proportion of a country’s population who live in urban areas using data from the Population Division of the Department of Economic and Social Affairs of the United Nations.
We used data on availability of multiple food types for human consumption from the food balance sheets (FBS) of the Food and Agriculture Organization of the United Nations. The FBS report the availability of 24 food types in kcal/capita/day. We used 22 out of 24 food types because one (“Sugar crops”) was missing in over 70% of country-years and another (“Miscellaneous”) may not be defined consistently across countries. For the remaining 22 food types, missing values were imputed using Imputation by Chained Equations (Stata 10.1 software command ice). The average of 100 imputed values was used. We defined outlier values for a single country-year as values that were larger or smaller than both the previous and the subsequent year’s values by 3 SD or 300% and set these outlier values to the average of the three previous and subsequent years. There was an abrupt change in the reported values for all food types in the Occupied Palestinian Territory around 1993 and in the values of one food type in one year in Mongolia, Maldives, Cyprus, and the Netherlands. These discontinuities were likely due to changes in reporting. We adjusted the earlier estimates by the difference between pre- and post-discontinuity values, resulting in a smooth trend.
To identify major dietary patterns using all 22 food types, we used principal component analysis, an approach commonly used in dietary pattern studies to objectively aggregate food items based on the correlation structure within the dataset16. We used the first principal component in our analysis. This component explained over 28% of the variance of data10 and had relatively large positive coefficients for alcoholic beverages, animal fats and animal products, eggs, meat, milk, offals, stimulants, sugar and sweeteners, and total calories ; and negative coefficients for pulses and cereals (Table 1). Consistent with studies of dietary patterns in individuals, we considered this pattern as representing a “Western diet” (labeled as WD). Because a principal component does not have a directly interpretable scale, we used percentiles for presentation. Percentiles were calculated using the distribution of data pooled over all 29 years of analysis. Therefore, Westernization of diet over time in the same country increases its percentile.
Table 1.
Coefficients of 22 food types in the first principal component (with varimax rotation to improve interpretability), which represent a Western dietary pattern. Food types are ordered in descending order of coefficients. Food types with large coefficients are the ones that are common in the dietary pattern and those with small coefficients are uncommon.
| Food type | Principal component coefficients |
|---|---|
| Animal products | 0.39 |
| Meat | 0.36 |
| Animal fats | 0.34 |
| Milk, excluding butter | 0.34 |
| Offals | 0.30 |
| Alcoholic beverages | 0.29 |
| Sugar and sweeteners | 0.25 |
| Eggs | 0.24 |
| Stimulants | 0.23 |
| Total calories | 0.20 |
| Vegetable oils | 0.08 |
| Fish and seafood | 0.05 |
| Vegetables | 0.03 |
| Tree nuts | 0.02 |
| Fruits, excluding wine | −0.05 |
| Other aquatic products | −0.06 |
| Spices | −0.07 |
| Vegetal products | −0.09 |
| Oil crops | −0.10 |
| Starchy roots | −0.10 |
| Cereals (excluding beer) | −0.16 |
| Pulses | −0.19 |
Statistical methods
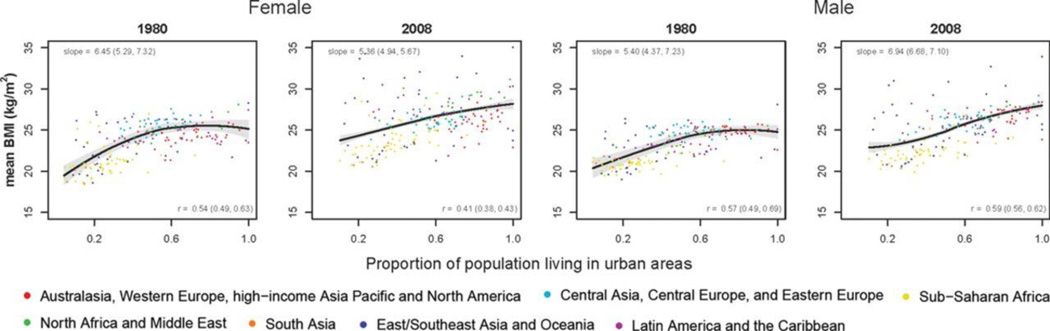
We investigated the univariate associations of age-standardized mean risk factor levels with national income, Western diet and urbanization (for BMI only) with countries as the units of observation. We did not weight country population as our aim was to investigate across countries as opposed to in the global population. We present the scatter plots and the estimated Pearson correlation coefficient and its 95% confidence interval for 1980 and 2008 (Figures 1–3). In each graph, we fitted a nonparametric (Loess) regression to visualize the association. We also fitted univariate regression models to each pair of variables in Figures 1–3 separately by year (1980 and 2008) and report the slopes in these Figures. We also analyzed the associations of mean FPG, SBP, and TC with mean BMI (Figure 4) because BMI causally affects the other three metabolic indicators, which also have other determinants, e.g. dietary salt and saturated fats and medication use.
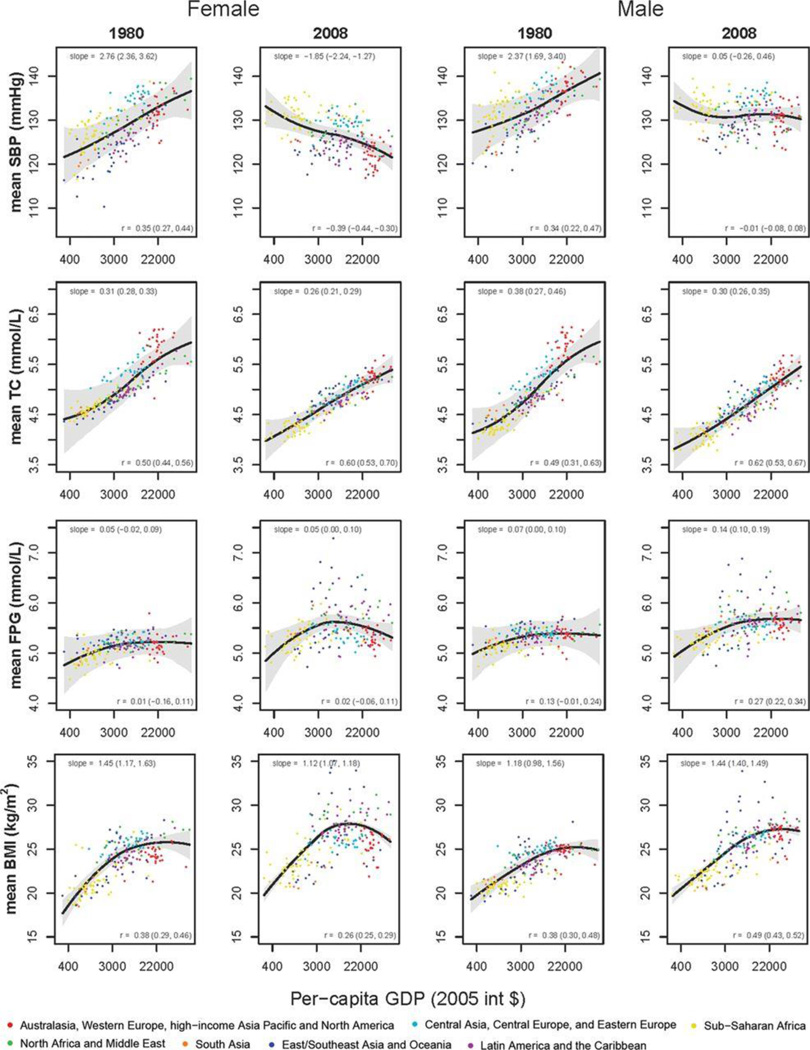
Figure 1.
Mean age-standardized levels of metabolic risk factors in relation to per-capita gross domestic product (GDP). GDP is in international dollar, which accounts for differences in purchasing power across countries, and is adjusted for inflation. The thick line shows the mean association and the gray area the 95% uncertainty interval of this relationship, calculated using a non-parametric (Loess) regression as described in Methods and Supplemental Material. Individual data points show country means. See Table S1 for country data.
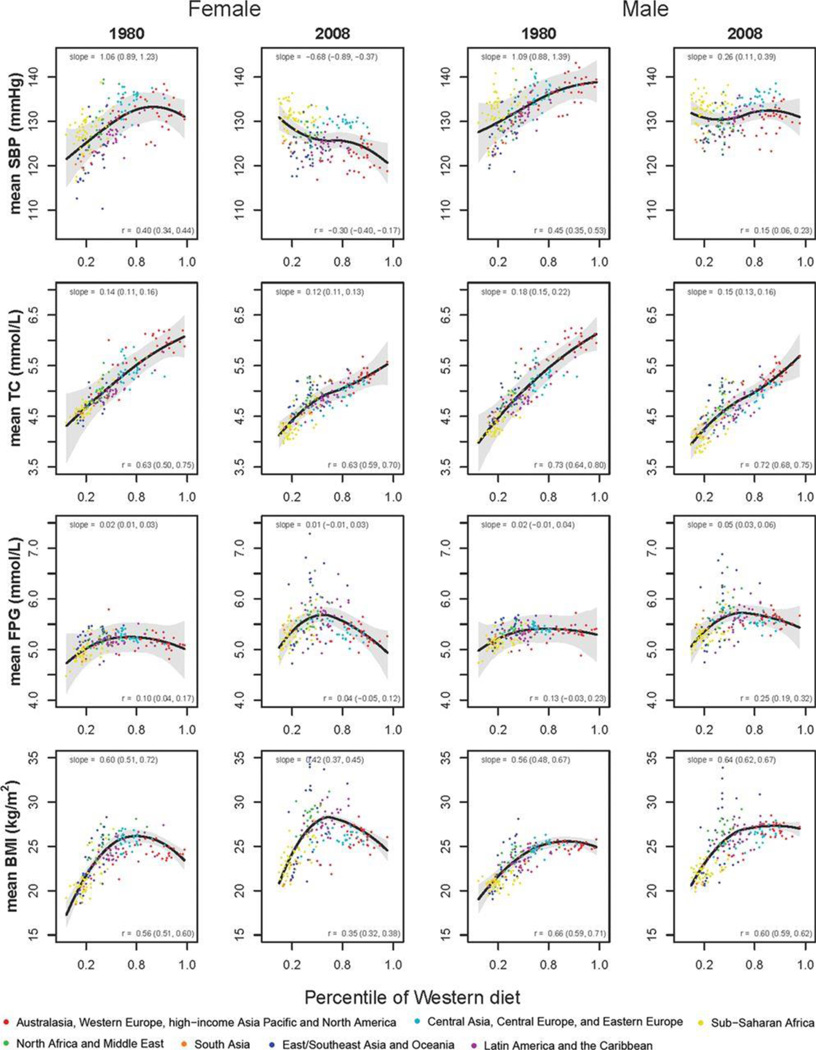
Figure 3.
Mean age-standardized levels of metabolic risk factors in relation to Western diet (WD). See Methods for how percentiles were calculated. See Table S1 for country data.
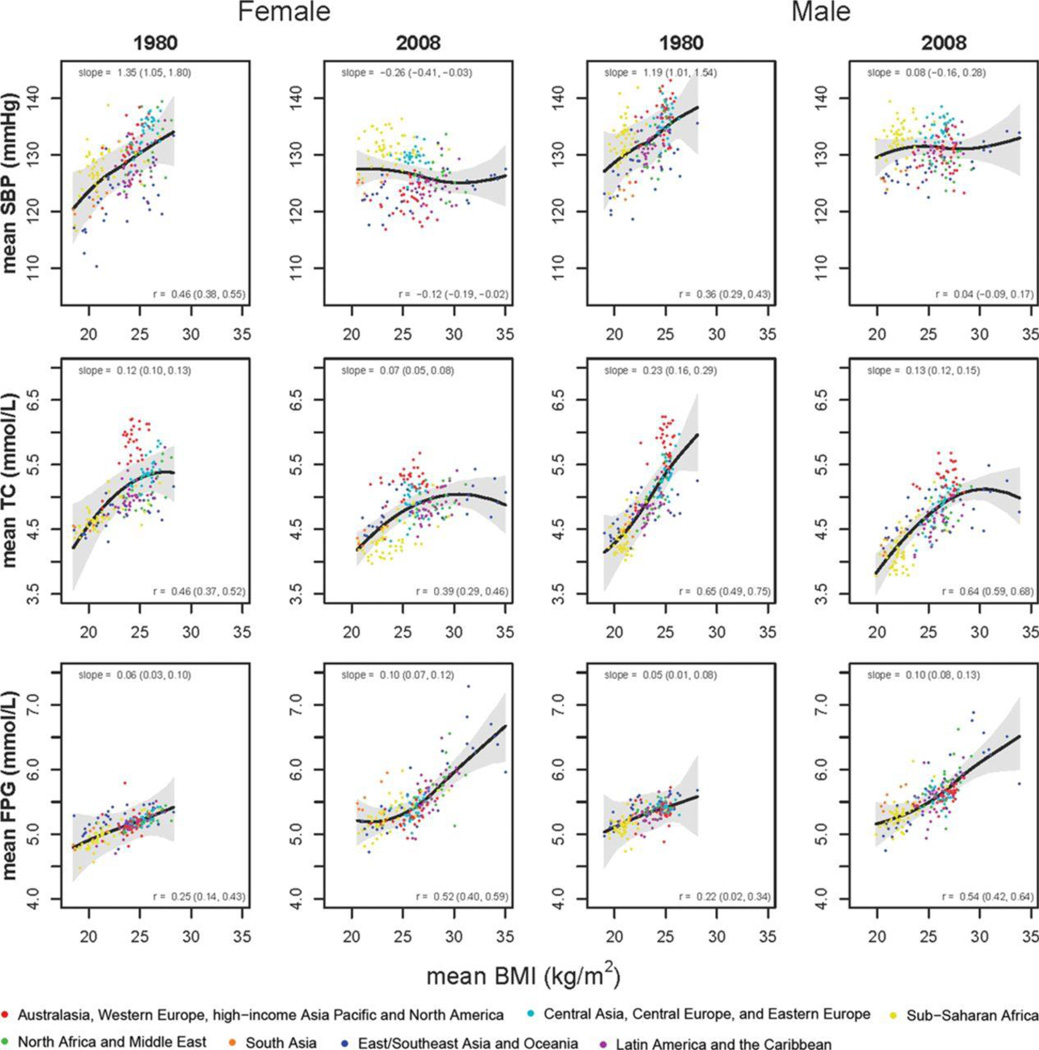
Figure 4.
Mean age-standardized SBP, TC, and FPG in relation to mean age-standardized BMI. See Table S1 for country data.
All analyses were based on a Bayesian multiple imputation approach as described in Supplemental Material. We estimated the uncertainties of the correlation and regression coefficients as described in Supplemental Material. Analyses were carried out in R (v. 2.15.0) and Stata (10.1 StataCorp, College Station, Texas).
Results
In 1980, population mean BMI, SBP, and TC were positively associated with national income, with correlation coefficients ranging between 0.34 and 0.50 (Figure 1). The relationship between BMI and income flattened at a per-capita GDP of about Int$7000. The association between national income and FPG in 1980 was weaker than those of the other three risk factors, with correlation coefficients below 0.15 and regression slopes close to zero.
In 2008, the relationship between natural logarithm of GDP [Ln(GDP)] and BMI resembled an inverted-U for women, peaking at middle income levels. Middle- and upper-middle-income countries in Oceania, Middle East, and North Africa, had higher BMIs than countries with similar incomes in other regions, whereas women living in high-income countries in Asia-Pacific and Western Europe had lower BMIs than women in countries with similar incomes in other regions. The slope of BMI-Ln(GDP) association and the correlation coefficient in 2008 were about one third smaller than their 1980 levels for women.
The association between income and SBP reversed between 1980 and 2008, with the slopes becoming negative for women (from 2.76 (95% uncertainty interval (2.36, 3.62) mmHg per Ln(GDP) in 1980 to −1.85 (−2.24, −1.27) in 2008) and virtually zero for men. In 2008, TC was still strongly correlated with national income (correlation coefficients of 0.60 (0.53, 0.70) for women and 0.62 (0.53, 0.67) for men). Although the slope of TC-Ln(GDP) association declined slightly between 1980 and 2008, the declines were not statistically significant. The association between mean FPG and income remained weak in 2008.
The associations of risk factors with percent of population in urban areas, and how they changed between 1980 and 2008, mostly had the same patterns as associations with national income (detailed results available from the authors by request). The exception was the association between BMI and urbanization. The associations between mean BMI and urban population were positive and statistically significant in both 1980 and 2008, with slopes ranging between 0.54 and 0.7 kg/m2 per 10 percentage point increase in urbanization.
In 1980 BMI was associated with Western diet (WD), with some flattening for men and reversal of association at around the 80th percentile for women (Figure 3). In 2008, the BMI-WD curve for men maintained its linear-then-flat shape but was shifted upwards therefore showing higher BMI levels at the same value of WD. For women, the reversal occurred at around the 55th or 60th WD percentile. The association between SBP and WD shifted from positive to negative for women and was substantially weakened for men over the three decades of analysis. TC was positively and significantly associated with western diet in both 1980 and 2008 with slopes remaining positive and only slightly declining (Figure 3) and correlation coefficients > 0.6.
TC was positively associated with BMI in both 1980 and 2008, but there was more flattening of the curve in 2008 and the slope of the TC-BMI relationship declined in both men and women; The SBP-BMI association disappeared in both men and women over time (Figure 4). While mean FPG had weak associations with national income and Western diet, it was positively correlated with BMI, with correlation coefficients increasing from 0.22 (0.02, 0.34) and 0.25 (0.14, 0.43) in 1980 in men and women, respectively, to 0.54 (0.42, 0.64) and 0.52 (0.40, 0.59) in 2008. The FPG-BMI slope ranged between 0.06 and 0.10 mmol/L per kg/m2 over the analysis period for both men and women.
Discussion
Randomized and observational epidemiological studies have established elevated blood pressure and cholesterol, excess body weight, hyperglycemia, and smoking as some of the most important risk factors for CVD. Until now, little has been known about the associations of these risk factors with macroeconomic characteristics of countries, and how the associations have changed over time. Our analysis suggests that the associations of metabolic risk factors with affluence and Western diet are complex and dynamic. In 1980, three major metabolic risk factors for CVD – SBP, TC and BMI – were positively associated with national income and Western diet at the national level. By 2008, only TC retained a strong positive association with national income whereas the other associations changed qualitatively. Interestingly, BMI remained positively associated with urbanization over the nearly three decades of the analysis in both men and women, suggesting that urbanization may have effects on BMI apart from income and Western diet.
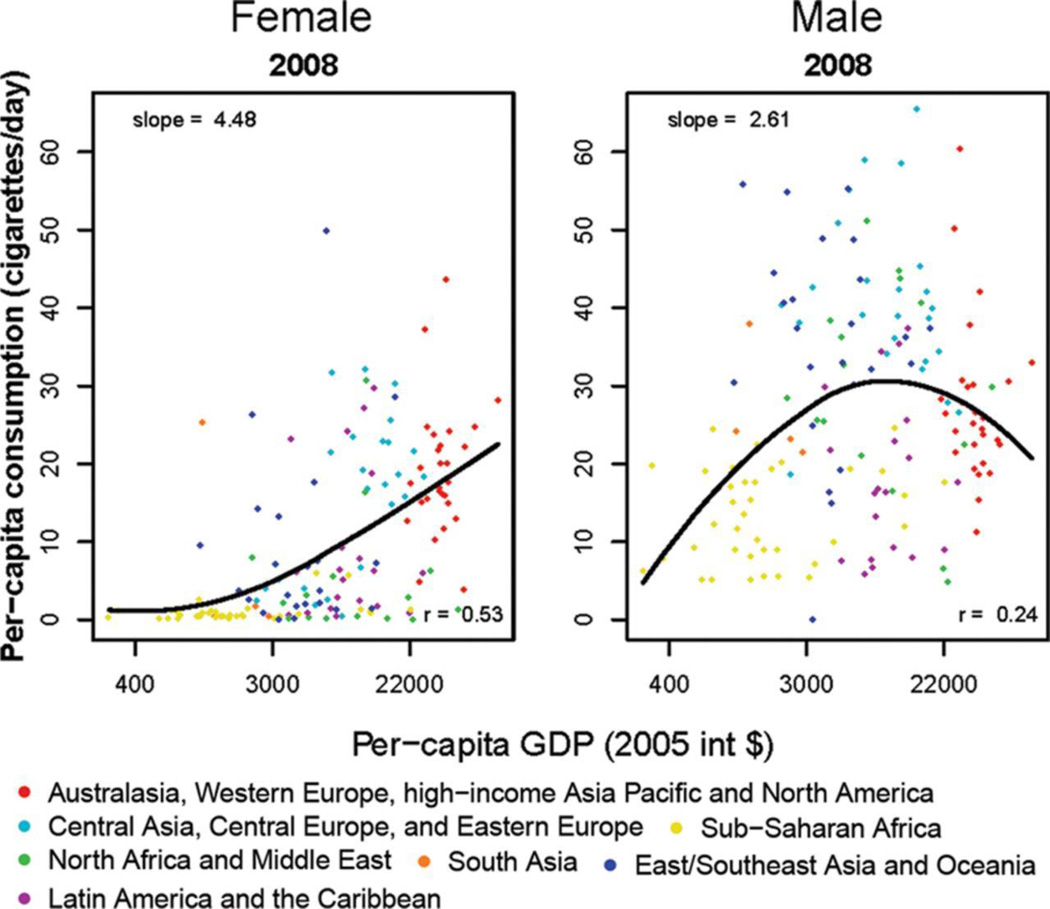
Comparable country data for smoking, the other key CVD risk factor, are available only for recent years and hence do not allow analysis between 1980 and 2008.14 Analysis using 2008 data, which were available, shows that correlation between adult per-capita number of cigarettes smoked per day and ln(GDP) was 0.24 in men and 0.53 in women (Figure 5). The absence of a simple direct association with income in men could be due to effective tobacco control in high-income countries and high smoking prevalence in middle-income countries in Eastern Europe and East and Southeast Asia.
Figure 5.
Age standardized prevalence of smoking in relation to per-capita gross domestic product (GDP) in 2008. Smoking data are from the WHO Global status report on noncommunicable diseases 201014.
The strengths and innovations of this study include analysis of associations with multiple macroeconomic variables in both 1980 and 2008; using a Bayesian hierarchical model for estimating risk factor levels that incorporated their important features such as non-linear trends and age associations; and systematic analysis of uncertainty. The main limitation of our study is that despite extensive data seeking, many country-years still lacked data, especially in the 1980s and for FPG and TC. As reported elsewhere, our model performed well in external predictive validity tests, i.e., in estimating risk factor levels in countries and years which had data but whose data were held back from the analysis to test the model’s predictions10–13. Further, in the current analysis, this shortage of data is reflected in larger uncertainty intervals in 1980 compared to 2008, and in larger uncertainty for the associations of FPG and TC compared with BMI. Our results were similar and our conclusions were unchanged in a sensitivity analysis using those countries with at least one data point over time.
There are several potential reasons for the changing associations of metabolic risk factors with affluence and Western diet. The VA Cooperative Studies and subsequent randomized trials demonstrated the benefits of lowering blood pressure at pre-hypertension levels and led to lower clinical thresholds for treatment with antihypertensives. This may have differentially advantaged high-income countries17. Lower salt intake and higher intake of fresh fruits and vegetables may also be responsible for lower blood pressure in some high-income countries17, 18. There is further evidence from within-country studies that the decline in blood pressure has been even larger in individuals with higher BMI19, 20, which is consistent with the decoupling the two causally-linked factors at the population level.
The large rise in BMI in middle-income and even lower-middle-income countries may be occurring because food cost has become (at least until recent rise in food prices) an increasingly smaller share of household expenditure in these countries. The fact that the association of BMI with Western diet has weakened indicates that the rise in BMI in developing countries may be as much due to increased caloric intake from traditional sources as from a shift to Western diet. In addition, the persistent positive association of BMI with urbanization, especially for men, is consistent with a role of physical inactivity in urban populations and in urbanizing countries. The differences in associations of BMI with macroeconomic variables between men and women is consistent with the faster rise in female BMI in low- and middle-income countries (LMICs) compared to male BMI13, 21. The continued positive association between serum TC and national income may be due to relatively high cost of animal products in low- and even middle-income countries. Nonetheless, TC declined in Western countries12, possibly due to changes in diet and wider use of statins22.
The changes in metabolic risk factors, especially in relation to national income, may help explain some of the trends in CVD mortality. Age-standardized cardiovascular disease mortality in high-income countries has declined substantially over the past few decades23, 24. Faster emergency response times; use of medicines such as anti-platelet agents, ACE inhibitors, beta blockers, and statins after heart attack or stroke; and medical advances such as angioplasty, defibrillation, and thrombolysis, have improved the survival of people with a cardiovascular event25. However, the contribution of post-event treatment to lower CVD mortality is estimated as less than 50%26. Rather the mortality decline is largely a result of lower disease incidence, itself due to preventive interventions, especially population-level improvements in blood pressure, cholesterol and reduction in smoking26 which have occurred despite rising BMI levels. There are less data on CVD trends in low- and middle-income countries. The available data nonetheless indicate that relatively soon after the decline in infectious diseases, CVD mortality also declines even in low- and middle-income countries27, 28; where this decline has been documented, it has accompanied a decline in blood pressure29.
Given this evidence, the dynamic global epidemiology of metabolic risk factors has important implications for CVD prevention worldwide. First, a key focus of global CVD prevention should be to reverse the shifting burden of SBP to low-income countries seen in Figure 1. Lowering salt intake through regulation and well-designed health education, improving access to fresh fruits and vegetables, and strengthening primary care to better detect and manage high blood pressure can help lower blood pressure worldwide, replicating the decline in high-income nations24, 30. Second, low- and middle-income countries could implement food policies that encourage the use of polyunsaturated fats instead of saturated fats22, avoiding the high cholesterol levels experienced in Western countries and the rise in Japan and China. Third, high- and middle-income countries can increase the coverage of statins for lowering serum cholesterol31. The cost of medicines and screening and follow-up tests may be too high for low-income countries. Availability of generic drugs and lower-cost tests will help make statins affordable even in low-income settings, but their implementation requires investment in an equitable and high-quality primary care system. Currently, high- and middle-income countries spend significant healthcare resources on treatment of CVD, diabetes, and their complications32–35. Redirecting some of these resources to primary prevention of high blood pressure and cholesterol may lead to a net cost saving36, 37. In low-income countries, additional strengthening and investment in primary care38 and regulatory infrastructures, e.g. establishing and enforcing limits on salt in more commonly used packaged foods and staples such as flour and bread, may be needed.
In contrast to blood pressure, which has become increasingly disassociated from BMI at the population level, the persistent association between BMI and FPG and the rising BMI levels mean that unless effective interventions for weight control or improvements in diet and other lifestyle factors are designed and implemented to prevent diabetes, health systems worldwide will face an increasing burden of hyperglycemia and diabetes, and will have to develop mechanisms for better detection and management of diabetes. A costly global epidemic of hyperglycemia and diabetes, together with high blood pressure in low income countries, may be the most salient feature of the global cardiovascular risk transition in the coming decades.
Supplementary Material
Figure 2.
Mean age-standardized BMI in relation to the proportion of a country’s population that lived in urban areas. Associations of other risk factors with urbanization are available from the authors by request. See Table S1 for country data.
Acknowledgments
Funding Sources: Majid Ezzati is supported by a strategic award from the UK Medical Research Council (MRC) and by the National Institute for Health Research Comprehensive Biomedical Research Centre at Imperial College Healthcare NHS Trust. GMS is supported by a T32 Training Grant in Academic Nutrition (Grant Number DK007703) from the National Institute of Diabetes and Digestive and Kidney Diseases. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Global Burden of Metabolic Risk Factor of Chronic Diseases Collaborating Group
Writing and Global Analysis Group: Goodarz Danaei,* Gitanjali M Singh,* Christopher J Paciorek, Mariel M Finucane, John K Lin, Farshad Farzadfar, Gretchen A Stevens, Melanie J Cowan, Leanne M Riley, Yuan Lu, Mayuree Rao, Majid Ezzati
*Contributed equally to the research and manuscript and listed in alphabetical order
Country Data Group: Geir Aamodt; Ziad Abdeen; Nabila A Abdella; Hanan F Abdul Rahim; Juliet Addo; Wichai Aekplakorn; Mustafa M Afifi; Enrico Agabiti-Rosei; Carlos A Aguilar Salinas; Charles Agyemang; Mohamed M Ali; Mohannad Al-Nsour; Abdul R Al-Nuaim; Ramachandran Ambady; Pertti Aro; Fereidoun Azizi; Carlo M Barbagallo; Marco Antonio M Barbieri; Alberto Barceló; Sandhi M Barreto; Henrique Barros; Leonelo E Bautista; Athanase Benetos; Peter Bjerregaard; Cecilia Björkelund; Simona Bo; Martin Bobak; Enzo Bonora; Babu V Bontha; Manuel A Botana; Pascal Bovet; Juergen Breckenkamp; Monique M Breteler; Grazyna Broda; Ian J Brown; Michael Bursztyn; Antonio Cabrera de León; Hannia Campos; Francesco P Cappuccio; Vincenzo Capuano; Edoardo Casiglia; Maurizio Castellano; Katia Castetbon; Luis Cea; Chih-Jen Chang; Noureddine Chaouki; Somnath Chatterji; Chien-Jen Chen; Zhengming Chen; Chien-Jen Chen; Jin-Su Choi; Lily Chua; Renata Cífková; Linda J Cobiac; Richard S Cooper; Anna Maria Corsi; Michael C Costanza; Cora L Craig; Rachel S Dankner; Saeed Dastgiri; Elias Delgado; Gonul Dinc; Yasufumi Doi; Guang-Hui Dong; Eleonora Dorsi; Nico Dragano; Adam Drewnowski; Robert W Eggertsen; Paul Elliott; Anders Engeland; Cihangir Erem; Alireza Esteghamati; Caroline HD Fall; Jian-Gao Fan; Catterina Ferreccio; Leopold Fezeu; Josélia O Firmo; Hermes J Florez; Nélida S Fornés; F Gerry R Fowkes; Guido Franceschini; Fredrik Frisk; Flávio D Fuchs; Eva L Fuller; Linn Getz; Simona Giampaoli; Luis F Gómez; Juan M Gomez-Zumaquero; Sidsel Graff-Iversen; Janet F Grant; Ramiro Guerrero Carvajal; Martin C Gulliford; Rajeev Gupta; Prakash C Gupta; Oye Gureje; Tine W Hansen; Jun Hata; Jiang He; Noor Heim; Joachim Heinrich; Tomas Hemmingsson; Anselm Hennis; William H Herman; Victor M Herrera; Suzanne Ho; Michelle Holdsworth; Gunilla Hollman Frisman; Wilma M Hopman; Akhtar Hussain; Abdullatif Husseini; M Mohsen Ibrahim; Nayu Ikeda; Bjarne K Jacobsen; Hashem Y Jaddou; Tazeen H Jafar; Mohsen Janghorbani; Grazyna Jasienska; Michel R Joffres; Jost B Jonas; Othman A Kadiki; Ofra Kalter-Leibovici; Raoul M Kamadjeu; Ioannis Karalis; Mika J Kastarinen; Joanne Katz; Lital Keinan-Boker; Paul Kelly; Omid Khalilzadeh; Young-Ho Khang; Stefan Kiechl; Ki Woong Kim; Yutaka Kiyohara; Junji Kobayashi; Maressa P Krause; Růžena Kubínová; Pawel Kurjata; Yadlapalli S Kusuma; Tai H Lam; Arnulf Langhammer; Carlene MM Lawes; Cai Le; Jeannette Lee; Claire Lévy-Marchal; Yanping Li; Yuqiu Li; Stephen Lim; TO Lim; Xu Lin; Cheng-Chieh Lin; Xu Lin; Hsien-Ho Lin; Lars Lind; Lauren Lissner; Xiaoqing Liu; Patricio Lopez-Jaramillo; Roberto Lorbeer; Roberto Lorbeer; Guansheng Ma; Stefan Ma; Francesc Macià; David R MacLean; Stefania Maggi; Dianna J Magliano; Marcia Makdisse; Giuseppe Mancia; Toshifumi Mannami; Pedro Marques-Vidal; Jean Claude N Mbanya; Norma McFarlane-Anderson; Roberto Miccoli; Juhani Miettola; Hoang V Minh; Juan F Miquel; J Jaime Miranda; Mostafa K Mohamed; Mostafa K Mohamed; Mostafa K Mohamed; V Mohan; Salim Mohanna; Ali Mokdad; Willem F Mollentze; Dante D Morales; Karen Morgan; Lorenza M Muiesan; Sergio Muntoni; Iraj Nabipour; Tomoko Nakagami; Vinay Nangia; Barbara Nemesure; Martin Neovius; Kjersti A Nerhus; Flavio Nervi; Hannelore Neuhauser; Minh Nguyen; Toshiharu Ninomiya; Marianna Noale; Sang W Oh; Takayoshi Ohkubo; Oliviero Olivieri; Ayse Emel Önal; Altan Onat; Myriam Oróstegui; Hermann Ouedraogo; Wen-Harn Pan; Demosthenes B Panagiotakos; Francesco Panza; Yongsoo Park; Valeria MA Passos; Mangesh S Pednekar; Marco A Peres; Cynthia Pérez; Román Pérez-Fernández; Rafael Pichardo; Hwee Pin Phua; Francesco Pistelli; Pedro Plans; Maria Polakowska; Neil Poulter; Dorairaj Prabhakaran; Qing Qiao; Masoud Rafiei; Olli T Raitakari; Luiz R Ramos; Sanjay Rampal; Lekhraj Rampal; Finn Rasmussen; Kanala KR Reddy; Josep Redon; Luis Revilla; Victoria Reyes-García; Ragab B Roaeid; Fernando Rodriguez-Artalejo; Rosalba Rojas-Martinez; Kimmo Ronkainen; Luis Rosero-Bixby; Gregory A Roth; Harshpal S Sachdev; José R Sánchez; Selim Y Sanisoglu; Susana Sans; Nizal Sarraf-Zadegan; Marcia Scazufca; Beatriz D Schaan; Norberto Schapochnik; Hedi Schelleman; Ione JC Schneider; C Mary Schooling; Bernhard Schwarz; Cevad Sekuri; Martha S Sereday; Lluís Serra-Majem; Jonathan Shaw; Abdul S Shera; Zumin Shi; Rahman Shiri; Xiao Ou Shu; Diego Augusto Santos Silva; Eglé Silva; Leon A Simons; Margaret Smith; Stefan Söderberg; Suharko Soebardi; Vincenzo Solfrizzi; Emily Sonestedt; Ahmet Soysal; Pär Stattin; Aryeh D Stein; George S Stergiou; Jochanan Stessman; Akihiro Sudo; Machi Suka; Valter Sundh; Kristina Sundquist; Johan Sundström; Andrew B Swai; E Shyong Tai; Kristian Tambs; Fikru Tesfaye; George N Thomas; Margaret Thorogood; Reijo S Tilvis; Martin Tobias; Liv E Torheim; Peter Trenkwalder; Jaakko O Tuomilehto; Josep A Tur; Christophe Tzourio; Ana I Uhernik; Flora A Ukoli; Nigel Unwin; Stephen Vander Hoorn; Mark P Vanderpump; Jose Javier Varo; Marit B Veierød; Gustavo Velásquez-Meléndez; Monique Verschuren; Lucie Viet; Salvador Villalpando; Jesus Vioque; Peter Vollenweider; Stefano Volpato; Ningli Wang; Ya X Wang; Mark Ward; Sarwono Waspadji; Lennart X Welin; Lars Wilhelmsen; Johann Willeit; Mark Woodward; André J Xavier; Fei Xu; Liang Xu; Akira Yamamoto; Gonghuan Yang; Xiaoguang Yang; Li-Chia Yeh; Jin-Sang Yoon; Qisheng You; Zhijie Yu; Jian Zhang; Lei Zhang; Wei Zheng; Maigeng Zhou
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The author is a staff member of the World Health Organization. The author alone is responsible for the views expressed in this publication and they do not necessarily represent the decisions, policy or views of the World Health Organization.
Contributions
GD and ME developed the study concept and CJP developed the statistical approach for the analysis of associations. ME wrote the first draft of the paper and CJP wrote the first draft of the Statistical Methods. GMS, MMF, and JKL analyzed data. Other members of the Writing and Global Analysis Group contributed to study design, analysis, and writing of manuscript. The members of the Country Data Group analyzed health examination survey and epidemiologic study data. GD and GMS had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. ME oversaw the research and is the study guarantor.
Conflict of Interest Disclosures: CJP holds stock in Pfizer. Other authors do not have a conflict of interest.
References
- 1.DiCesare M, Khang YH, Asaria P, Blakely T, Cowan MJ, Farzadfar F, Guerrero R, Ikeda N, Kyobutungi C, Msyamboza KP, Oum S, Lynch JW, Marmot MG, Ezzati M. Inequalities in non-communicable diseases and effective responses. Lancet. 2013 Feb 16;381:585–597. doi: 10.1016/S0140-6736(12)61851-0. Epub 2013 Feb 12. [DOI] [PubMed] [Google Scholar]
- 2.Ezzati M, Vander Hoorn S, Lawes CM, Leach R, James WP, Lopez AD, Rodgers A, Murray CJ. Rethinking the "diseases of affluence" paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2005;2:e133. doi: 10.1371/journal.pmed.0020133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim D, Kawachi I, Hoorn SV, Ezzati M. Is inequality at the heart of it? Cross-country associations of income inequality with cardiovascular diseases and risk factors. Soc Sci Med. 2008;66:1719–1732. doi: 10.1016/j.socscimed.2007.12.030. [DOI] [PubMed] [Google Scholar]
- 4.Pelletier DL, Rahn M. Trends in body mass index in developing countries. Food and Nutrition Bulletin. 1998;19:223–239. [Google Scholar]
- 5.Popkin BM. The shift in stages of the nutrition transition in the developing world differs from past experiences. Public Health Nutr. 2002;5:205–214. doi: 10.1079/PHN2001295. [DOI] [PubMed] [Google Scholar]
- 6.Reddy KS. Cardiovascular disease in non-Western countries. N Engl J Med. 2004;350:2438–2440. doi: 10.1056/NEJMp048024. [DOI] [PubMed] [Google Scholar]
- 7.Anand SS, Yusuf S. Stemming the global tsunami of cardiovascular disease. Lancet. 2011;377:529–532. doi: 10.1016/S0140-6736(10)62346-X. [DOI] [PubMed] [Google Scholar]
- 8.Beaglehole R, Yach D. Globalisation and the prevention and control of non-communicable disease: the neglected chronic diseases of adults. Lancet. 2003;362:903–908. doi: 10.1016/S0140-6736(03)14335-8. [DOI] [PubMed] [Google Scholar]
- 9.Pang T, Guindon GE. Globalization and risks to health. EMBO Rep. 2004;5 doi: 10.1038/sj.embor.7400226. Spec No:S11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Danaei G, Finucane MM, Lin JK, Singh GM, Paciorek CJ, Cowan MJ, Farzadfar F, Stevens GA, Lim SS, Riley LM, Ezzati M. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5.4 million participants. Lancet. 2011;377:568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 11.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 12.Farzadfar F, Finucane MM, Danaei G, Pelizzari PM, Cowan MJ, Paciorek CJ, Singh GM, Lin JK, Stevens GA, Riley LM, Ezzati M. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3.0 million participants. Lancet. 2011;377:578–586. doi: 10.1016/S0140-6736(10)62038-7. [DOI] [PubMed] [Google Scholar]
- 13.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F, Riley LM, Ezzati M. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO. Global status report on non-communicable diseases 2010. Geneva: WHO; 2011. [Google Scholar]
- 15.James SL, Gubbins P, Murray CJ, Gakidou E. Developing a comprehensive time series of GDP per capita for 210 countries from 1950 to 2015. Population health metrics. 2012;10:12. doi: 10.1186/1478-7954-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Current opinion in lipidology. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Ikeda N, Gakidou E, Hasegawa T, Murray CJ. Understanding the decline of mean systolic blood pressure in Japan: an analysis of pooled data from the National Nutrition Survey, 1986–2002. Bull World Health Organ. 2008;86:978–988. doi: 10.2471/BLT.07.050195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009;23:363–384. doi: 10.1038/jhh.2008.144. [DOI] [PubMed] [Google Scholar]
- 19.Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, Narayan KM, Williamson DF. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;20:293, 1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 20.Danon-Hersch N, Chiolero A, Shamlaye C, Paccaud F, Bovet P. Decreasing association between body mass index and blood pressure over time. Epidemiology. 2007;18:493–500. doi: 10.1097/EDE.0b013e318063eebf. [DOI] [PubMed] [Google Scholar]
- 21.Pampel FC, Denney JT, Krueger PM. Obesity, SES, and economic development: a test of the reversal hypothesis. Soc Sci Med. 2012;74:1073–1081. doi: 10.1016/j.socscimed.2011.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pietinen P, Vartiainen E, Seppanen R, Aro A, Puska P. Changes in diet in Finland from 1972 to 1992: impact on coronary heart disease risk. Preventive medicine. 1996;25:243–250. doi: 10.1006/pmed.1996.0053. [DOI] [PubMed] [Google Scholar]
- 23.Levi F, Lucchini F, Negri E, La VC. Trends in mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world. Heart. 2002;88:119–124. doi: 10.1136/heart.88.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ezzati M, Riboli E. Can noncommunicable diseases be prevented? Lessons from studies of populations and individuals. Science. 2012;337:1482–1487. doi: 10.1126/science.1227001. [DOI] [PubMed] [Google Scholar]
- 25.Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med. 2012;366:54–63. doi: 10.1056/NEJMra1112570. [DOI] [PubMed] [Google Scholar]
- 26.Ford ES, Capewell S. Proportion of the decline in cardiovascular mortality disease due to prevention versus treatment: public health versus clinical care. Annual review of public health. 2011;32:5–22. doi: 10.1146/annurev-publhealth-031210-101211. [DOI] [PubMed] [Google Scholar]
- 27.Stringhini S, Sinon F, Didon J, Gedeon J, Paccaud F, Bovet P. Declining stroke and myocardial infarction mortality between 1989 and 2010 in a country of the african region. Stroke. 2012;43:2283–2288. doi: 10.1161/STROKEAHA.112.658468. [DOI] [PubMed] [Google Scholar]
- 28.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 29.Bovet P, Romain S, Shamlaye C, Mendis S, Darioli R, Riesen W, Tappy L, Paccaud F. Divergent fifteen-year trends in traditional and cardiometabolic risk factors of cardiovascular diseases in the Seychelles. Cardiovascular diabetology. 2009;8:34. doi: 10.1186/1475-2840-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370:2044–2053. doi: 10.1016/S0140-6736(07)61698-5. [DOI] [PubMed] [Google Scholar]
- 31.Roth GA, Fihn SD, Mokdad AH, Aekplakorn W, Hasegawa T, Lim SS. High total serum cholesterol, medication coverage and therapeutic control: an analysis of national health examination survey data from eight countries. Bull World Health Organ. 2011;89:92–101. doi: 10.2471/BLT.10.079947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370:1929–1938. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 33.Barcelo A, Aedo C, Rajpathak S, Robles S. The cost of diabetes in Latin America and the Caribbean. Bull World Health Organ. 2003;81:19–27. [PMC free article] [PubMed] [Google Scholar]
- 34.Leeder S, Raymond S, Greenberg H, Liu H, Esson K. A Race Against Time: The Challenge of Cardiovascular Disease in Developing Economies. New York: 2004. [Google Scholar]
- 35.Nugent RA, Fathima SF, Feigl AB, Chyung D. The Burden of Chronic Kidney Disease on Developing Nations: A 21st Century Challenge in Global Health. Nephron Clin Pract. 2011;118:c269–c277. doi: 10.1159/000321382. [DOI] [PubMed] [Google Scholar]
- 36.Cohen JT, Neumann PJ, Weinstein MC. Does preventive care save money? Health economics and the presidential candidates. N Engl J Med. 2008;358:661–663. doi: 10.1056/NEJMp0708558. [DOI] [PubMed] [Google Scholar]
- 37.Vos T, Carter R, Barendregt J, Mihalopoulos C, Veerman JL, Magnus A, Cobiac L, Bertram MY, Wallace AL APT. Assessing Cost-Effectiveness in Prevention (ACE-Prevention): Final Report. Melbourne: University of Queensland, Brisbane and Deakin University; 2010. 2010. [Google Scholar]
- 38.Farzadfar F, Murray CJ, Gakidou E, Bossert T, Namdaritabar H, Alikhani S, Moradi G, Delavari A, Jamshidi H, Ezzati M. Effectiveness of diabetes and hypertension management by rural primary health-care workers (Behvarz workers) in Iran: a nationally representative observational study. Lancet. 2011;379:47–54. doi: 10.1016/S0140-6736(11)61349-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.