Abstract
Purpose
Biomarkers for the early detection of pancreatic cancer are urgently needed. The primary objective of this study was to evaluate whether increased levels of serum CA19-9, CA125, CEACAM1 and REG3A are present prior to clinical presentation of pancreatic cancer and to assess the performance of combined markers for early detection and prognosis.
Experimental Design
This nested case control study within UKCTOCS included 118 single- and 143 serial-serum samples from 154 post-menopausal women who were subsequently diagnosed with pancreatic cancer and 304 matched non-cancer controls. Samples were split randomly into independent training and test sets. CA19-9, CA125, CEACAM1 and REG3A were measured using ELISA and/or CLIA. Performance of markers to detect cancers at different times prior to diagnosis and for prognosis was evaluated.
Results
At 95% specificity, CA19-9 (>37 U/mL) had a sensitivity of 68% up to 1 year, and 53% up to 2 yrs before diagnosis. Combining CA19-9 and CA125 improved sensitivity as CA125 was elevated (>30 U/mL) in ~20% of CA19-9-negative cases. CEACAM1 and REG3A were late markers adding little in combined models. Average lead times of 20–23 months were estimated for test-positive cases. Pre-diagnostic levels of CA19-9 and CA125 were associated with poor overall survival (HR 2.69 and 3.15, respectively).
Conclusions
CA19-9 and CA125 have encouraging sensitivity for detecting pre-clinical pancreatic cancer and both markers can be used as prognostic tools. This work challenges the prevailing view that CA19-9 is up-regulated late in the course of pancreatic cancer development.
Keywords: pancreatic cancer, preclinical serum biomarkers, UKCTOCS, CA19-9, CA125, CEACAM1, REG3A
INTRODUCTION
Pancreatic ductal adenocarcinoma (PDAC) is a leading cause of cancer death and has the lowest survival rate for any solid cancer (~2%) (1, 2). Surgical resection is the only chance of cure, but due to advanced stage at presentation only 20% of patients have resectable tumours (3). Of these, only 15% will have early-stage cancers (4, 5). When resection is possible followed by adjuvant therapy, the 5-year survival is better at 20–30% (6). It is clear that early detection of smaller tumors is necessary to improve resectability rates and survival. Indeed it was shown that if tumor size at detection can be reduced from 3 to 2 cm, then there is an increase in resectability from 7% to 83% with increased median survival from 7.6 to 17.2 months (7).
The serum marker CA19-9 (8–10) is the only biomarker used routinely in the management of PDAC. It has a 79–81% sensitivity and 82–90% specificity for diagnosis (11), with false-positive results observed in benign pancreatico-biliary diseases such as pancreatitis, cholangitis and obstructive jaundice (12–14). Furthermore, CA19-9 is not expressed in 8–10% of the Caucasian population with the Lewis a-b- genotype, as the CA19-9 epitope is the sialylated Lewis A blood group antigen (14, 15). Despite this, CA19-9 has proved useful for disease management, where increased post-therapy levels indicate poor prognosis and poor therapy response (16, 17). Moreover, the levels of CA19-9 in the months and years prior to PDAC diagnosis have not previously been examined, leaving its capacity to contribute to early diagnosis untested. Other reported non-invasive diagnostic and/or prognostic markers of pancreatic cancer that have been tested alone or in combination, include CA125 (18–21), CEA (22), CEACAM1 (23), MUC1 (24), OPN/SPP1 (25), MIC1/GDF15 (26), REG3A/PAP1 (27, 28) and PKM2 (29). As yet, the clinical utility of these markers remains to be determined and most require further multi-centre validation.
A major shortcoming of cancer biomarker studies aiming to address early detection is a lack of appropriate samples. Biomarkers tested in samples taken from patients diagnosed with cancer and benign or healthy controls only address potential use for differential diagnosis. Samples collected prior to diagnosis are preferential, enabling early changes to be detected, with consistently rising levels in the lead up to diagnosis adding confidence to the discovery. The serum samples used in this study come from a repository collected as part of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS); a randomized controlled trial of ovarian cancer assessing impact of screening on mortality using transvaginal ultrasound and serum CA125 interpreted using the Risk of Ovarian Cancer Algorithm (ROCA). Preclinical samples from participating women who subsequently developed PDAC were available for evaluating CA19-9, CA125, CEACAM1 and REG3A for early diagnosis.
MATERIALS AND METHODS
Serum samples
This nested case control study was approved by the Joint UCL/UCLH Research Ethics Committee A (Ref. 05/Q0505/57). Written informed consent was obtained from donors and no data allowing identification of patients was provided. The study set comprised serum from women recruited to UKCTOCS between 2001 and 2005 and collected according to a SOP (30, 31). Trial participants at enrolment were post-menopausal women aged 50–74 who had no family history of ovarian cancer. All participants were ‘flagged’ with the national agencies for cancer registrations and deaths using their NHS number. Women subsequently diagnosed with pancreatic cancer (cases) were identified by cross-referencing with the Health and Social Care Information Centre cancer registry codes and death codes (ICD10 C25.0/1/2/3/9). Initially, 171 cases were identified (with 304 associated samples) that had not been registered as having any other cancer since randomization. Matched non-cancer controls (i.e. with no cancer registry code) from individual women (1 per case sample; n=304) were selected based on collection date and center to minimize variation due to handling. For the 171 cases, confirmation of diagnosis was sought from GPs and consultants through questionnaire and from the Hospitals Episode Statistics database. As a result, 17 cases were excluded that did not have a confirmed diagnosis of pancreatic ductal adenocarcinoma. The resulting study set was 261 serum samples from 154 women subsequently diagnosed with pancreatic ductal adenocarcinoma up to 6.5 years later and 304 matched control sera from 304 women. 119 cases provided single samples and 35 provided 2 or more serial samples. Table 1 shows clinical, lifestyle and sample data for the study set. Samples were distributed randomly into discovery and validation sets and grouped by time to diagnosis as indicated in Table 2.
Table 1.
Clinical, lifestyle and sample characteristics data for whole study set.
| Variable | Cases | Controls | P value |
|---|---|---|---|
|
| |||
| No. individuals | 154 | 304 | |
|
| |||
| No. samples | 261 | 304 | |
|
| |||
| Tumor site | 8 | na | |
| tail | |||
| body | 10 | na | |
| head | 65 | na | |
| unspecified | 71 | na | |
|
| |||
| Mean time to spin (hrs) (range) | 21.8 (0.5–47) | 22.0 (6.9–47) | 0.62 |
|
| |||
| Mean age at sample draw (yrs) (range) | 65.3 (51.2–74.9) | 62.5 (50.4–77.5) | <0.0001 |
|
| |||
| Mean BMI (kg/m2) (range) | 27.6 (17.8–43.7) | 26.6 (17.9–44.4) | 0.041 |
|
| |||
| Mean time from sample collection to diagnosis (months) (range) | 25.5 (0–79) | na | |
|
| |||
| HRT use (at randomisation) | |||
| yes | 16 | 58 | 0.022 |
| no | 138 | 246 | (OR 2.03) |
|
| |||
| OCP use (ever) | |||
| yes | 79 | 163 | 0.69 |
| no | 75 | 141 | |
|
| |||
| Smoker | |||
| yes | 15 | 75 | 1.00 |
| no | 28 | 136 | |
| no response | 111 | 93 | |
|
| |||
| Alcohol | |||
| yes | 25 | 182 | 0.01 |
| no | 20 | 58 | (OR 2.5) |
| no response | 109 | 64 | |
|
| |||
| Deaths as of 03/2013 (%) | 95.45% | 1.32% | |
|
| |||
| Median time from diagnosis to death (months) (range) | 4.04 (1–45) | na | |
P values determined using Mann Whitney or Fisher’s Exact test. BMI = body mass index at recruitment; HRT = hormone replacement therapy; OCP = oral contraceptive pill; na = not applicable.
Table 2.
Sample sets and case controls used in study.
| Time group (yrs) | Total case samples | Total control samples | Discovery case samples | Discovery control samples | Validation case samples (all) | Validation case samples (limited) | Validation control samples |
|---|---|---|---|---|---|---|---|
|
| |||||||
| 0–0.5 | 43 | 47 | 17 | 20 | 26 | 12 | 27 |
| 0.5–1 | 42 | 48 | 18 | 22 | 24 | 18 | 26 |
| 1–2 | 57 | 64 | 17 | 22 | 40 | 34 | 42 |
| 2–3 | 46 | 54 | 13 | 17 | 33 | 32 | 37 |
| 3–4 | 30 | 41 | 12 | 18 | 18 | 18 | 23 |
| 4+ | 43 | 50 | 16 | 21 | 27 | 24 | 29 |
|
| |||||||
| 0–1 | 85 | 95 | 35 | 42 | 50 | 30 | 53 |
| 0–2 | 142 | 159 | 52 | 64 | 90 | 64 | 95 |
| 0–3 | 188 | 213 | 65 | 81 | 123 | 96 | 132 |
| 0–4+ | 261 | 304 | 93 | 120 | 168 | 138 | 184 |
| 1–3 | 103 | 118 | 30 | 39 | 73 | 66 | 79 |
| 3+ | 73 | 91 | 28 | 39 | 45 | 42 | 52 |
|
| |||||||
| Total samples | 261 | 304 | 93 | 120 | 168 | 138 | 184 |
|
| |||||||
| Total cases | 154 | 53 | 101 | 101 | |||
In the ‘restricted’ validation set, serial samples from the same woman falling in the same time group were removed at random to leave a single representative sample. There were no such samples in the discovery set.
Serum measurements
All serum tests were executed and interpreted by trained and experienced staff. Samples were randomized for testing and blinded to the experimenters prior to interpretation. CA19-9 was measured in discovery set samples using the Mucin PC/CA19-9 ELISA kit (Alpha Diagnostic International) according to the manufacturer, using a 1:4 serum dilution. Values lower than the assay’s limit of detection were given a ‘low’ value of 0.6 U/mL. Duplicate measurements gave an average CV of 6.9% (R2=0.998). CA19-9 was measured in validation set samples using the Cobas CA19-9 CLIA with a CA19-9 Calibrator Set (Roche and Fujirebio Diagnostics), run on a Cobas E411 analyzer with PreciControl Tumour Marker to monitor assay imprecision. The average CV from 31 replicate measurements of serum standard run at the same time was 3.2%.
CA125 was measured using the Cobas CA125 II CLIA with a CA125 II Calibrator Set (Roche and Fujirebio Diagnostics) on a Cobas E411 analyzer with PreciControl Tumour Marker, as above. Assays were performed originally on 320 fresh study samples in UKCTOCS and on discovery set samples (after two freeze thaw cycles) where original values were missing. Assays were repeated on all validation set samples. For matched duplicate readings, average CV was 8.5 % (R2=0.997). The average CV from 31 replicate measurements of serum standard was 4.1%.
For CEACAM1, a sandwich ELISA was established using the human CEACAM1/CD66a DuoSet kit (R&D Systems), as described in Supplementary Data. Replicate readings gave an average CV of 10.3%; (R2=0.81). Serum REG3A/PAP was measured using the PANCREPAP ELISA kit (DynaBio) according to the manufacturer, using a 1:100 serum dilution. Replicate readings gave an average CV of 21.9 % (R2=0.46).
Statistical Analysis
GraphPad Prism and MedCalc software were used for statistical analyses. For normally distributed data, the Student t test was used to assess significance of differences, otherwise the Mann-Whitney U-test was used. Fisher’s exact test was used to assess significance of associations for non-continuous variables. Correlation analysis used Spearman’s rank test. All P values <0.05 were considered significant. Receiver operating characteristic (ROC) curves were constructed for each marker and combinations to assess diagnostic accuracy. Kaplan-Meier analysis was used to examine biomarker levels in relation to survival using time from sample collection to death.
RESULTS
Study set characteristics
There was no significant difference in time to centrifugation between case control samples, whilst there was a difference in mean age (2.8 years; P<0.0001) and BMI (1 kg/m2; P=0.041) between cases and controls (Table 1). Hormone replacement therapy (HRT) use at randomization was associated with lowered risk of pancreatic cancer (OR=0.49; 95%CI 0.27–0.88; P=0.022), whilst oral contraceptive pill use had no association. Smoking was not associated with pancreatic cancer, whilst alcohol consumption was negatively associated (OR=0.4; P=0.01). Notably, response rate for reporting smoking and alcohol consumption was poor, particularly from those volunteers who developed cancer. The death rate was 95.5% for cases with a median time from diagnosis to death of 4 months.
Serum CA19-9, CA125, CEACAM1 and REG3A in discovery set
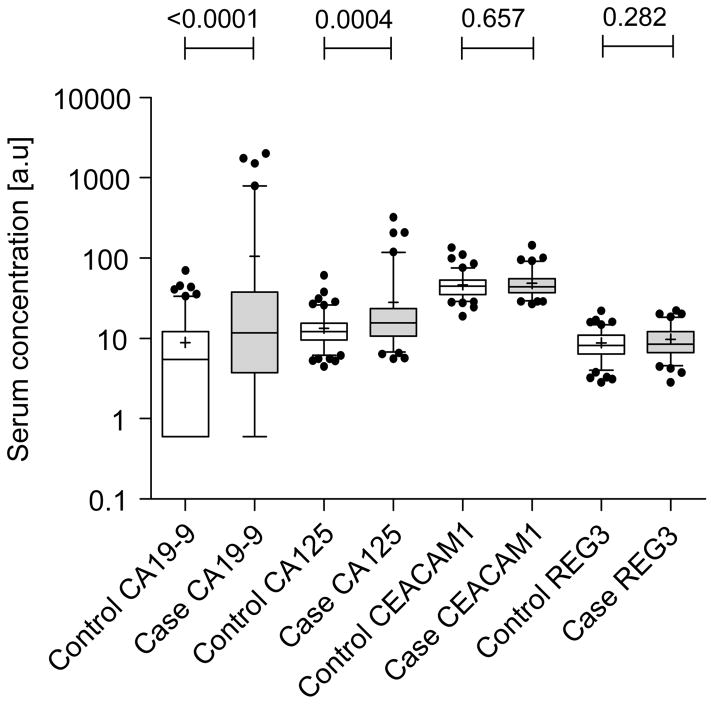
CA19-9, CEACAM1 and REG3A were measured in all discovery samples using commercial ELISA kits, whilst CA125 was measured using a robust CLIA assay. There was a significant increase in level between all case and control samples for CA19-9 (P<0.0001) and CA125 (P=0.0004), but not for CEACAM1 or REG3A (Figure 1). Time to diagnosis plots showed increasing CA19-9 and CA125 for cases in the lead up to diagnosis, whereas CEACAM1 and REG3A showed no such trend (Supplementary Data; Figure S1). For serial samples from the same women, CA19-9 and CA125 increased towards diagnosis in the majority of cases (Supplementary Data; Figure S2), whereas none showed increasing CEACAM1 or REG3A.
Figure 1.
Box and whisker plots showing serum levels of CA19-9, CA125, CEACAM1 and REG3A for all case and control discovery set samples. Whisker limits represent the 5th and 95th percentiles, the box limits represent interquartile range, the horizontal line the median and the cross the mean. Case and control groups were compared using the Mann-Whitney test; P values are shown above the plots.
Markers were analyzed according to time to diagnosis (grouped as 0–0.5 yrs, 0.5–1 yrs, 1–2 yrs, 2–3, yrs, 3+ yrs, 0–4+ yrs (all samples), 0–1 yrs and 1–4 yrs). In cases where serum was obtained <12 months before diagnosis, median CA19-9 was 43.2 U/mL (IQR 5.7–136.2 U/mL) compared to 3.1 U/mL (IQR 0.6–6.9 U/mL) in controls (P<0.0001; AUC=0.82) (Figure 2). For CA125, median values were 24.1 U/mL (IQR 12.9–47.9) for cases and 12.8 U/mL (IQR 9.3–14.5) for controls (P<0.0001; AUC=0.78). CEACAM1 (P=0.045; AUC=0.71) and REG3A (P=0.022; AUC=0.73) were only significantly elevated in the 6 months before diagnosis. CA19-9 and CA125 were also raised in the 0.5–1 year pre-diagnosis group (P=0.0016; AUC=0.80 and P=0.0167; AUC=0.73, respectively), but not >1 year. There were no significant associations for any of the markers with respect to time to centrifugation, age, BMI, smoking, alcohol consumption, HRT or OCP use, except REG3A, which correlated with age (ρ=0.31; P<0.001) in the controls.
Figure 2.
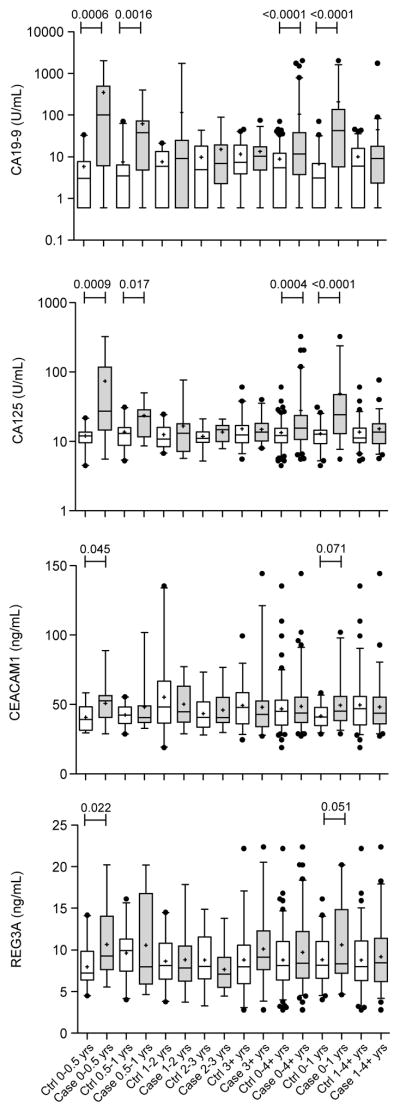
Box and whisker plots showing serum levels of CA19-9, CA125, CEACAM1 and REG3A for case control discovery samples grouped into different time to diagnosis groups. Whisker limits represent the 5th and 95th percentiles, the box limits represent interquartile range, the horizontal line the median and the cross the mean. Case and control groups were compared using the Mann-Whitney test; P values are shown above the plots.
Sensitivities for detection of PDAC were calculated using selected cut-offs (Table 3). CA19-9 (>25 U/mL) was the best performing marker, discriminating cases from controls with SN/SP of 70.6%/95.0% and 64.7/95.5% in the 0–0.5 yrs and 0.5–1 yrs prior to diagnosis (Table 3). The SN/SP for detection of PDAC with CA125 (>20 U/mL) in these time periods were somewhat poorer at 70.6%/90.0% and 52.9%/86.4%, respectively. CEACAM1 and REG3A were poor at detecting cancer compared to CA19-9 or CA125; for the 0–0.5 yrs group, the SN/SP for CEACAM1 was 53.3/83.3% (>50 ng/mL), whilst for REG3A it was 29.4/90% (>13 ng/mL). Combining markers showed the model ‘CA19-9>37 U/mL or CA125>30 U/mL’ provided the highest sensitivities at >90% specificity; 57.1% for the 0–1 year group (PPV 90.9%; OR=26.67, 95%CI 5.6–128.2) and 44.2% for the 0–2 year time group (PPV 92.0%; OR=24.59, 95%CI 5.4–111.4), but were only marginally better (and not significantly so) than using CA19-9 alone (Table 3). Adding CEACAM1 and/or REG3A into models decreased specificity with little improvement in sensitivity (data not shown). Logistic regression showed the best combined model (CA19-9, CA125 and CEACAM1) had an AUC of 0.88 (SE=0.042; 95%CI 0.79–0.95) for the 0–1 year group, but was not significantly higher than using CA19-9 alone (AUC=0.82). Together, these data indicate that CA19-9, and possibly CA125, may be useful in predicting PDAC up to 24 months in advance of diagnosis.
Table 3.
Performance of cut-off models for discovery set. Darker shading denotes higher values. See Supplementary Data; Table S1 for numbers of test positive cases and controls for using the CA19-9 >37 U/mL and CA125 >30 U/mL models.
| Time group |
Mean time to Dx (months) |
Parameter | CA19-9 >25 |
CA125 >20 |
CEACAM1 >50 |
REG3A >13 |
CA125 or CA19-9 |
CA19-9 >30 |
CA125 >25 |
CA125 or CA19-9 |
CA19-9 >37 |
CA125 >30 |
CA125 or CA19-9 |
CA19-9 >40 |
CA125 >25 |
CA125 or CA19-9 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–0.5 yrs | 2.94 | Sensitivity | 70.6 | 70.6 | 53.3 | 29.4 | 88.2 | 58.8 | 52.9 | 64.7 | 52.9 | 47.1 | 58.8 | 52.9 | 52.9 | 58.8 |
| Specificity | 95.0 | 90.0 | 83.3 | 90.0 | 85.0 | 95.0 | 100.0 | 95.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | ||
| 0.5–1 yrs | 9.11 | Sensitivity | 64.7 | 52.9 | 23.5 | 37.5 | 77.8 | 64.7 | 35.3 | 66.7 | 58.8 | 17.6 | 55.6 | 47.1 | 35.3 | 50.0 |
| Specificity | 95.5 | 86.4 | 81.0 | 90.9 | 81.8 | 95.5 | 90.9 | 86.4 | 95.5 | 95.5 | 90.9 | 95.5 | 90.9 | 86.4 | ||
| 1–2 yrs | 18.24 | Sensitivity | 23.5 | 17.6 | 46.7 | 18.8 | 29.4 | 23.5 | 11.8 | 23.5 | 17.6 | 5.9 | 17.6 | 17.6 | 11.8 | 17.6 |
| Specificity | 100.0 | 86.4 | 55.0 | 90.5 | 86.4 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | ||
| 2–3 yrs | 28.76 | Sensitivity | 8.3 | 7.7 | 33.3 | 7.7 | 15.4 | 8.3 | 0.0 | 7.7 | 8.3 | 0.0 | 7.7 | 8.3 | 0.0 | 7.7 |
| Specificity | 88.2 | 94.1 | 68.8 | 94.1 | 82.4 | 88.2 | 100.0 | 88.2 | 94.1 | 100.0 | 94.1 | 94.1 | 100.0 | 94.1 | ||
| 3+ yrs | 52.54 | Sensitivity | 10.7 | 8.0 | 28.6 | 21.4 | 14.3 | 3.6 | 8.0 | 10.7 | 3.6 | 4.0 | 7.1 | 3.6 | 8.0 | 10.7 |
| Specificity | 89.7 | 87.2 | 55.6 | 81.6 | 79.5 | 89.7 | 89.7 | 82.1 | 94.9 | 94.9 | 92.3 | 94.9 | 89.7 | 87.2 | ||
|
| ||||||||||||||||
| 0–4+ (all) | 25.44 | Sensitivity | 34.1 | 30.3 | 35.6 | 23.3 | 43.0 | 29.7 | 21.3 | 33.3 | 26.4 | 14.6 | 28.0 | 24.2 | 21.3 | 28.0 |
| Specificity | 93.3 | 88.3 | 66.7 | 88.1 | 82.5 | 93.3 | 95.0 | 89.2 | 96.7 | 97.5 | 95.0 | 96.7 | 95.0 | 92.5 | ||
| 0–1 yrs | 6.11 | Sensitivity | 67.6 | 61.8 | 37.5 | 33.3 | 82.9 | 61.8 | 44.1 | 65.7 | 55.9 | 32.4 | 57.1 | 50.0 | 44.1 | 54.3 |
| Specificity | 95.2 | 88.1 | 82.1 | 90.5 | 83.3 | 95.2 | 95.2 | 90.5 | 97.6 | 97.6 | 95.2 | 97.6 | 95.2 | 92.9 | ||
| 0–2 yrs | 12.18 | Sensitivity | 52.9 | 47.1 | 40.4 | 28.6 | 65.4 | 49.0 | 33.3 | 51.9 | 43.1 | 23.5 |

|
39.2 | 33.3 | 42.3 |
| Specificity | 96.9 | 87.5 | 72.9 | 90.5 | 84.4 | 96.9 | 96.9 | 93.8 | 98.4 | 98.4 | 98.4 | 96.9 | 95.3 | |||
| 1–4+ yrs | 37.10 | Sensitivity | 14.0 | 10.9 | 34.5 | 17.5 | 19.0 | 10.5 | 7.3 | 13.8 | 8.8 | 3.6 | 10.3 | 8.8 | 7.3 | 12.1 |
| Specificity | 92.3 | 88.5 | 58.3 | 86.8 | 82.1 | 92.3 | 94.9 | 88.5 | 96.2 | 97.4 | 94.9 | 96.2 | 94.9 | 92.3 | ||
Validation of CA19-9 and CA125 as early detection biomarkers
CA19-9 and CA125 were further assessed in a validation set comprising 168 samples from 101 cases. This was subsequently restricted to 138 samples by removing all but one serial samples (at random) from the same case/woman that fell within the same time group (Table 2). In this restricted set, CA19-9 was significantly higher in cases than controls for the 0–0.5, 1–2, 2–3 and 3+ year time groups, though failed significance for the 0.5–1 year group (Supplementary Data Figure S3). CA125 was significant for the 0–0.5 and 3+ year time groups. The simple cut-off model ‘CA19-9>37 U/mL or CA125>30 U/mL’ applied to this dataset gave 56.7% sensitivity and 90.6% specificity for the 0–1 year group (PPV=77.3%; OR=12.55, 95%CI 3.89–40.48), compared to 50% sensitivity and 94.3% specificity using CA19-9 alone (PPV=83.3%; OR=16.67, 95%CI 4.25–65.43) (Table 4). For the 0–2 year group, sensitivity was 40.6% and specificity 90.5% (PPV=74.3%; OR=6.54, 95%CI 2.80–15.28). Logistic regression combining CA19-9 and CA125 gave AUCs of 0.90 and 0.76 for the 0–0.5 and 0–1 year groups, respectively, but was not significantly higher than using CA19-9 alone. Thus, CA125 adds little discriminatory power in combined models. Despite this, 13 out of 53 positive cases in the validation set were detected solely using CA125.
Table 4.
Performance of cut-off models for restricted validation set. Darker shading denotes higher values. See Supplementary Data; Table S1 for numbers of test positive cases and controls for using the CA19-9 >37 U/mL and CA125 >30 U/mL models.
| Time group | Ave time to Dx (months) |
Parameter | CA19-9 >25 |
CA125 >20 |
CA19-9 or CA125 |
CA19-9 >30 |
CA125 >25 |
CA19-9 or CA125 |
CA19-9 >37 |
CA125 >30 |
CA19-9 or CA125 |
CA19-9 >40 |
CA125 >25 |
CA19-9 or CA125 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–0.5 yr | 3.42 | Sensitivity | 75.0 | 75.0 | 83.3 | 75.0 | 58.3 | 83.3 | 75.0 | 41.7 | 83.3 | 75.0 | 58.3 | 83.3 |
| Specificity | 77.8 | 77.8 | 63.0 | 85.2 | 92.6 | 85.2 | 92.6 | 96.3 | 88.9 | 100.0 | 92.6 | 92.6 | ||
| 0.5–1 yr | 9.27 | Sensitivity | 24.0 | 24.0 | 22.0 | 43.8 | 13.3 | 50.0 | 37.5 | 12.5 | 43.8 | 31.3 | 13.3 | 37.5 |
| Specificity | 50.0 | 20.0 | 62.5 | 96.2 | 96.2 | 92.3 | 96.2 | 96.2 | 92.3 | 96.2 | 96.2 | 92.3 | ||
| 1–2 yr | 18.68 | Sensitivity | 32.4 | 20.6 | 41.2 | 32.4 | 11.8 | 35.3 | 23.5 | 8.8 | 26.5 | 20.6 | 11.8 | 23.5 |
| Specificity | 85.7 | 78.6 | 69.0 | 92.9 | 97.6 | 90.5 | 92.9 | 97.6 | 90.5 | 95.2 | 97.6 | 92.9 | ||
| 2–3 yr | 29.24 | Sensitivity | 34.4 | 25.0 | 50.0 | 28.1 | 18.8 | 43.8 | 18.8 | 15.6 | 31.3 | 18.8 | 18.8 | 34.4 |
| Specificity | 94.4 | 80.6 | 77.8 | 94.4 | 97.2 | 91.7 | 97.2 | 97.2 | 94.4 | 97.2 | 97.2 | 94.4 | ||
| 3+ yr | 50.07 | Sensitivity | 23.8 | 35.7 | 45.2 | 14.3 | 14.3 | 26.2 | 9.5 | 7.1 | 14.3 | 9.5 | 14.3 | 21.4 |
| Specificity | 94.2 | 78.8 | 75.0 | 98.1 | 88.5 | 86.5 | 98.1 | 92.3 | 90.4 | 98.1 | 88.5 | 86.5 | ||
|
| ||||||||||||||
| 0–4+ (all) | 25.13 | Sensitivity | 35.5 | 30.4 | 50.0 | 30.4 | 18.1 | 39.9 | 23.9 | 13.0 | 30.4 | 22.5 | 18.1 | 31.9 |
| Specificity | 89.6 | 80.9 | 73.8 | 94.0 | 94.0 | 89.1 | 95.6 | 95.6 | 91.3 | 97.3 | 94.0 | 91.3 | ||
| 0–1 yr | 6.93 | Sensitivity | 56.7 | 40.0 | 66.7 | 53.3 | 30.0 | 60.0 | 50.0 | 23.3 |
|
46.7 | 30.0 | 53.3 |
| Specificity | 84.9 | 84.9 | 73.6 | 90.6 | 94.3 | 88.7 | 94.3 | 96.2 | 98.1 | 94.3 | 92.5 | |||
| 0–2 yr | 13.17 | Sensitivity | 43.8 | 29.7 | 53.1 | 42.2 | 20.3 | 46.9 | 35.9 | 15.6 | 40.6 | 32.8 | 20.3 | 37.5 |
| Specificity | 85.3 | 82.1 | 71.6 | 91.6 | 95.8 | 89.5 | 93.7 | 96.8 | 90.5 | 96.8 | 95.8 | 92.6 | ||
| 1–4+ yr | 34.02 | Sensitivity | 29.6 | 27.8 | 45.4 | 24.1 | 14.8 | 34.3 | 16.7 | 10.2 | 23.1 | 15.7 | 14.8 | 25.9 |
| Specificity | 91.5 | 79.2 | 73.8 | 95.4 | 93.8 | 89.2 | 96.2 | 95.4 | 91.5 | 96.9 | 93.8 | 90.8 | ||
Our intention was also to build algorithms based on available serial/longitudinal data. ROCA used in UKCTOCS (32, 33) could not be developed for CA19-9 due to lack of serial control samples. A Parametric Empirical Bayes algorithm (34) applied to the combined dataset gave sensitivities of 19% and 17% (at 95% specificity) for CA19-9 and CA125, respectively, and was thus poorer than the threshold models. This again is likely due to an insufficient longitudinal data for accurate model building.
Lead time estimation
In two cases with sufficient longitudinal samples, increasing CA19-9 was apparent as early as 3 years prior to diagnosis of PDAC (Supplementary Data; Figure S2; Cases 5 and 6). However, most marker ‘change-points’ occurred within 12 months of diagnosis. CA125 tended to rise later than CA19-9, but was diagnostic alone in ~20% of cases where CA19-9 was not elevated (Figure S2; Case 40). Taking the earliest point of detection for cases with longitudinal samples, the model ‘CA19-9>30 or CA125>25’ gave an average lead time of 22.9 months (median 18.5 months; IQR 8.0–32.8 months). Whilst estimated lead times were slightly higher for combined models versus CA19-9 alone, differences were not significant.
Prognosis
The four markers were investigated as prognostic factors using time from sample collection to death in cases where pancreatic cancer was cited as the primary or contributory cause of death. Firstly, poor and good prognosis case samples were respectively defined as falling below and above the median time from sample collection to death (30.5 months). Both CA19-9 and CA125 were significantly elevated in the poor prognosis group, whilst CEACAM1 and REG3A were not (data not shown). Kaplan-Meier analysis confirmed a significant difference in survival curves for CA19-9 (cut-off 40 U/mL; Log-rank test P<0.0001; HR=2.69, 95%CI 1.84–3.91) and CA125 (cutoff 25 U/mL; Log-rank test P<0.0001; HR= 3.15, 95%CI 2.11–4.69), confirming them as prognostic markers (Figure 3). Median survival times from collection were 14.5 versus 36.0 months for CA19-9 and 14.0 versus 35.0 months for CA125.
Figure 3.
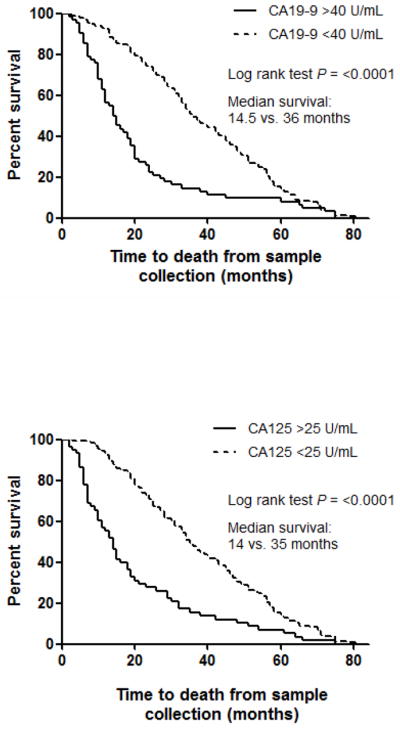
Survival curves for CA19-9 and CA125 using time from sample collection to death due to pancreatic cancer.
DISCUSSION
To our knowledge this is the first study to show serum CA19-9, CA125, CEACAM1 and REG3A are significantly elevated prior to PDAC diagnosis. To our surprise, in 16% of cases, CA19-9 was elevated (>37 U/mL) 2–3 years before diagnosis, with sensitivity increasing towards diagnosis. The PPV of CA19-9 was 90% up to 1 year before diagnosis and >80% up to 2 years, depending on the cut-off level used. CA125 also increased in pre-clinical disease and although combined models gave only modest increases in performance versus CA19-9 alone, CA125 detected 13% of CA19-9-negative cases; some of which are likely to be Lewis antigen negative. Notably, combined models gave average lead times up to 23 months. Together, our data support the notion that a panel of markers including CA19-9 may be beneficial for earlier detection of pancreatic cancer with potential use in screening.
Three studies have explored the utility of serum CA19-9 levels as a screening tool for pancreatic cancer (35–37). Kim et al assessed CA19-9 in 70,940 asymptomatic individuals identifying 4 cancers among 1,063 individuals with elevated CA19-9 (>37 U/mL; PPV= 0.9%; sensitivity 100%; specificity 98.5%). Notably, a higher proportion of women (2.5%) compared to men (0.5%) had elevated CA19-9. This did not increase with age in women, as was observed here. Given the low predictive value of CA19-9 and low prevalence of pancreatic cancer in the general population, it was concluded from these studies that CA19-9 testing alone has no utility as a screening tool. However, here CA19-9 elevations were noted up to 36 months prior to diagnosis, indicating its potential as a first line test for early detection that may increase the number of patients with resectable disease. These results need to be independently validated. Annual CA19-9 blood testing may also benefit high-risk populations such as those from kindred with familial pancreatic cancer. Guidelines for the surveillance of these family members are not established, although there are recent studies assessing outcomes of screening these high-risk populations (38, 39).
Serum CA125 has been evaluated as a marker for detecting malignant versus benign pancreatic tumours with a reported sensitivity of 60.8% and specificity of 83.3% (21). Combining CA19-9 and CA125 gave values of 87.8% and 77.8% respectively, with the authors concluding that test results should be interpreted in reference to imaging. A similar study reported a sensitivity of 56.9% and specificity of 77.6%, with CA125 providing a limited contribution in jaundiced patients (40). Herein, in the pre-diagnosis setting, we show that CA125 performed with higher specificity, providing additional sensitivity in combination with CA19-9.
CEACAM1 is expressed in pancreatic carcinoma in situ lesions, and thus has early stage marker potential (23). It was further shown in this previous study that serum CEACAM1 had superior accuracy to CA19-9 in clinical samples from PDAC patients. Whilst the function of CEACAM1 remains unclear, several studies have identified its aberrant expression in a variety of cancers often with conflicting reports (41–43). Herein, CEACAM1 appears to be up-regulated in pancreatic adenocarcinoma, although is elevated in serum closer to diagnosis as compared to CA19-9. CEACAM1 did not significantly improve classification in combined models and it was not a prognostic factor. We conclude that serum CEACAM1 is not an early marker of pancreatic cancer.
REG3A expression has been associated with pancreatic inflammation (44) and cancer (27, 28, 45). In the latter study, REG3A had 90% sensitivity and 82.8% specificity for discriminating PDAC cases from healthy controls and was not correlated with CA19-9 level or associated with concomitant pancreatitis or jaundice. In the present study, REG3A was discriminatory within 6 months of diagnosis, but was rarely elevated independently of CA19-9. In summary, REG3A is a poor early marker, adding little in combined models.
Our data also confirm CA19-9 as a prognostic marker since we show that pre-diagnosis cases with levels <40 U/mL had a prolonged median survival (from 14.5 to 36 months using time from blood draw), and is in agreement with published data (reviewed in (11)). CA125 was similar in predicting overall survival, and thus also appears to be a prognostic factor in pancreatic cancer. This is supported by the notion that CA125 plays a direct role in the progression and dissemination of pancreatic tumour cells (46).
Our study has several limitations. Firstly, only post-menopausal women were studied, and hence may not reflect the utility of pancreatic tumor markers in the general population. Secondly, there was insufficient information on grading, staging, tumor size and treatment to be able to examine correlations with the markers. Indeed, it is likely that many of the test-positive cases were at an advanced stage of disease when tested, in agreement with observed correlations between serum CA19-9 levels and pancreatic tumor burden (47); although this may not always hold true (48). Thirdly, the number of cases (and controls) with serial samples was insufficient to accurately build and assess longitudinal algorithms. Fourthly, there was a lack of data on benign morbidities in both the case and control groups for which CA19-9 may be elevated. Despite these limitations, the study is unique in that pre-clinical samples were investigated, allowing an objective assessment of how serological markers change during disease progression. Indeed, our findings suggest that raised CA19-9 can be detected early in the course of PDAC development when tumor size is likely to be smaller and when survival outcomes are improved (7). Importantly, although the majority of test positive cases in our study had elevated CA19-9 (and/or CA125) within 1 year of diagnosis, likely indicating advanced disease, these patients still went undiagnosed. This alludes to the non-specific nature of the symptoms of pancreatic cancer, but also raises the possibility of an earlier diagnosis that may improve outcome. Whilst one recent study has assessed pre-diagnostic PDAC samples (from the prospective EPIC cohort), reporting that autoantibodies against ezrin appear early in PDAC development, CA19-9 levels were unfortunately not reported in the 16 cases examined (49).
Our data also suggest that that HRT use at randomization was associated with lowered risk of pancreatic cancer. The apparent protective effect of HRT use is at odds with two large prospective cohort studies showing no association (50, 51). The reason for this discrepancy is unclear, but may be a chance association given the much lower number of controls used in the present study.
In conclusion, CA19-9 may have clinical utility in screening for pancreatic cancer as a first line test, particularly if used longitudinally in higher risk or symptomatic populations, whilst CA125 measurements may improve its performance and increase its prognostic value. It is unclear whether the use of other screening investigations (EUS, CT scan) would have allowed earlier diagnosis (i.e. at a still resectable state) when applied at the time of a CA19-9 or CA125 rise and this would need to be trialed in future studies.
Supplementary Material
TRANSLATIONAL RELEVANCE.
Pancreatic ductal adenocarcinoma is a leading cause of cancer death and has the lowest survival rate for any solid cancer. Biomarkers for the early detection of pancreatic cancer are urgently needed to improve survival, although studies assessing biomarkers for early detection rarely use samples from patients with pre-clinical disease. For the first time, serum markers CA19-9, CA125, CEACAM1 and REG3A have been assessed in samples taken up to 6 years prior to clinical presentation of pancreatic cancer. We show that CA19-9 and CA125 are elevated many months prior to clinical presentation of pancreatic cancer and when used in combination, CA125 improved upon the performance of CA19-9 alone through the detection of CA19-9 negative cases. Moreover, both markers can be used as prognostic tools in pancreatic cancer. These markers have the potential, when combined, for screening high-risk groups, particularly if used longitudinally.
Acknowledgments
Financial support: This research was funded by Cancer Research UK (grant A12790) and Pancreatic Cancer UK, and was supported by the US National Institutes of Health (P01 CA084203) and the National Institute for Health Research (NIHR) University College London Hospitals (UCLH) Biomedical Research Centre. UKCTOCS was core funded by the Medical Research Council, Cancer Research UK, and the Department of Health with additional support from the Eve Appeal, Special Trustees of Bart’s and the London, and Special Trustees of UCLH.
Footnotes
Conflicts of interest: IJ has a consultancy arrangement with Becton Dickinson in the field of tumor markers and ovarian cancer. Both IJ and UM has a financial interest through UCL Business and Abcodia Ltd in the third party exploitation of clinical trials biobanks which have been developed through research at UCL.
References
- 1.CRUK. Pancreatic cancer statistics. 2013 http://info.cancerresearchuk.org/cancerstats/types/pancreas/ [cited 2013 20/10/2013]; Available from: http://info.cancerresearchuk.org/cancerstats/types/pancreas/
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA: a cancer journal for clinicians. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 3.Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362:1605–17. doi: 10.1056/NEJMra0901557. [DOI] [PubMed] [Google Scholar]
- 4.Tascilar M, Skinner HG, Rosty C, Sohn T, Wilentz RE, Offerhaus GJ, et al. The SMAD4 protein and prognosis of pancreatic ductal adenocarcinoma. Clin Cancer Res. 2001;7:4115–21. [PubMed] [Google Scholar]
- 5.Yeo CJ, Cameron JL. Prognostic factors in ductal pancreatic cancer. Langenbecks Arch Surg. 1998;383:129–33. doi: 10.1007/s004230050104. [DOI] [PubMed] [Google Scholar]
- 6.Sultana A, Cox T, Ghaneh P, Neoptolemos JP. Adjuvant therapy for pancreatic cancer. Recent Results Cancer Res. 2012;196:65–88. doi: 10.1007/978-3-642-31629-6_5. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal B, Correa AM, Ho L. Survival in pancreatic carcinoma based on tumor size. Pancreas. 2008;36:e15–20. doi: 10.1097/mpa.0b013e31814de421. [DOI] [PubMed] [Google Scholar]
- 8.Baeckstrom D, Hansson GC, Nilsson O, Johansson C, Gendler SJ, Lindholm L. Purification and characterization of a membrane-bound and a secreted mucin-type glycoprotein carrying the carcinoma-associated sialyl-Lea epitope on distinct core proteins. J Biol Chem. 1991;266:21537–47. [PubMed] [Google Scholar]
- 9.Baeckstrom D, Nilsson O, Price MR, Lindholm L, Hansson GC. Discrimination of MUC1 mucins from other sialyl-Le(a)-carrying glycoproteins produced by colon carcinoma cells using a novel monoclonal antibody. Cancer Res. 1993;53:755–61. [PubMed] [Google Scholar]
- 10.Ho JJ, Siddiki B, Kim YS. Association of sialyl-Lewis(a) and sialyl-Lewis(x) with MUC-1 apomucin ina pancreatic cancer cell line. Cancer Res. 1995;55:3659–63. [PubMed] [Google Scholar]
- 11.Ballehaninna UK, Chamberlain RS. The clinical utility of serum CA 19-9 in the diagnosis, prognosis and management of pancreatic adenocarcinoma: An evidence based appraisal. Journal of gastrointestinal oncology. 2012;3:105–19. doi: 10.3978/j.issn.2078-6891.2011.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steinberg W. The clinical utility of the CA 19-9 tumor-associated antigen. Am J Gastroenterol. 1990;85:350–5. [PubMed] [Google Scholar]
- 13.Duffy MJ. Carcinoembryonic antigen as a marker for colorectal cancer: is it clinically useful? Clin Chem. 2001;47:624–30. [PubMed] [Google Scholar]
- 14.Lamerz R. Role of tumour markers, cytogenetics. Ann Oncol. 1999;10 (Suppl 4):145–9. [PubMed] [Google Scholar]
- 15.DiMagno EP, Reber HA, Tempero MA. AGA technical review on the epidemiology, diagnosis, and treatment of pancreatic ductal adenocarcinoma. American Gastroenterological Association. Gastroenterology. 1999;117:1464–84. doi: 10.1016/s0016-5085(99)70298-2. [DOI] [PubMed] [Google Scholar]
- 16.Ziske C, Schlie C, Gorschluter M, Glasmacher A, Mey U, Strehl J, et al. Prognostic value of CA 19-9 levels in patients with inoperable adenocarcinoma of the pancreas treated with gemcitabine. Br J Cancer. 2003;89:1413–7. doi: 10.1038/sj.bjc.6601263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Micke O, Bruns F, Kurowski R, Horst E, deVries AF, Hausler JW, et al. Predictive value of carbohydrate antigen 19-9 in pancreatic cancer treated with radiochemotherapy. Int J Radiat Oncol Biol Phys. 2003;57:90–7. doi: 10.1016/s0360-3016(03)00524-8. [DOI] [PubMed] [Google Scholar]
- 18.Haga Y, Sakamoto K, Egami H, Yoshimura R, Mori K, Akagi M. Clinical significance of serum CA125 values in patients with cancers of the digestive system. The American journal of the medical sciences. 1986;292:30–4. doi: 10.1097/00000441-198607000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Haglund C. Tumour marker antigen CA125 in pancreatic cancer: a comparison with CA19-9 and CEA. Br J Cancer. 1986;54:897–901. doi: 10.1038/bjc.1986.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sakamoto K, Haga Y, Yoshimura R, Egami H, Yokoyama Y, Akagi M. Comparative effectiveness of the tumour diagnostics, CA 19-9, CA 125 and carcinoembryonic antigen in patients with diseases of the digestive system. Gut. 1987;28:323–9. doi: 10.1136/gut.28.3.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cwik G, Wallner G, Skoczylas T, Ciechanski A, Zinkiewicz K. Cancer antigens 19-9 and 125 in the differential diagnosis of pancreatic mass lesions. Arch Surg. 2006;141:968–73. doi: 10.1001/archsurg.141.10.968. discussion 74. [DOI] [PubMed] [Google Scholar]
- 22.Yasue M, Sakamoto J, Teramukai S, Morimoto T, Yasui K, Kuno N, et al. Prognostic values of preoperative and postoperative CEA and CA19.9 levels in pancreatic cancer. Pancreas. 1994;9:735–40. doi: 10.1097/00006676-199411000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Simeone DM, Ji B, Banerjee M, Arumugam T, Li D, Anderson MA, et al. CEACAM1, a novel serum biomarker for pancreatic cancer. Pancreas. 2007;34:436–43. doi: 10.1097/MPA.0b013e3180333ae3. [DOI] [PubMed] [Google Scholar]
- 24.Gold DV, Modrak DE, Ying Z, Cardillo TM, Sharkey RM, Goldenberg DM. New MUC1 serum immunoassay differentiates pancreatic cancer from pancreatitis. J Clin Oncol. 2006;24:252–8. doi: 10.1200/JCO.2005.02.8282. [DOI] [PubMed] [Google Scholar]
- 25.Koopmann J, Fedarko NS, Jain A, Maitra A, Iacobuzio-Donahue C, Rahman A, et al. Evaluation of osteopontin as biomarker for pancreatic adenocarcinoma. Cancer Epidemiol Biomarkers Prev. 2004;13:487–91. [PubMed] [Google Scholar]
- 26.Koopmann J, Buckhaults P, Brown DA, Zahurak ML, Sato N, Fukushima N, et al. Serum macrophage inhibitory cytokine 1 as a marker of pancreatic and other periampullary cancers. Clin Cancer Res. 2004;10:2386–92. doi: 10.1158/1078-0432.ccr-03-0165. [DOI] [PubMed] [Google Scholar]
- 27.Rosty C, Christa L, Kuzdzal S, Baldwin WM, Zahurak ML, Carnot F, et al. Identification of hepatocarcinoma-intestine-pancreas/pancreatitis-associated protein I as a biomarker for pancreatic ductal adenocarcinoma by protein biochip technology. Cancer Res. 2002;62:1868–75. [PubMed] [Google Scholar]
- 28.Faca VM, Song KS, Wang H, Zhang Q, Krasnoselsky AL, Newcomb LF, et al. A mouse to human search for plasma proteome changes associated with pancreatic tumor development. PLoS medicine. 2008;5:e123. doi: 10.1371/journal.pmed.0050123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cerwenka H, Aigner R, Bacher H, Werkgartner G, el-Shabrawi A, Quehenberger F, et al. TUM2-PK (pyruvate kinase type tumor M2), CA19-9 and CEA in patients with benign, malignant and metastasizing pancreatic lesions. Anticancer Res. 1999;19:849–51. [PubMed] [Google Scholar]
- 30.Menon U, Gentry-Maharaj A, Ryan A, Sharma A, Burnell M, Hallett R, et al. Recruitment to multicentre trials--lessons from UKCTOCS: descriptive study. BMJ (Clinical research ed. 2008;337:a2079. doi: 10.1136/bmj.a2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Menon U, Gentry-Maharaj A, Hallett R, Ryan A, Burnell M, Sharma A, et al. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) Lancet Oncol. 2009;10:327–40. doi: 10.1016/S1470-2045(09)70026-9. [DOI] [PubMed] [Google Scholar]
- 32.Skates SJ, Pauler DK, Jacobs IJ. Screening based on the risk of cancer calculation from Bayesian hierarchical changepoint and mixture models of longitudinal markers. J Am Stat Assoc. 2001;96:429–39. [Google Scholar]
- 33.Skates SJ, Jacobs IJ, Sjovall K, Einhorn N, Xu FJ, Yu YH, et al. High sensitivity and specificity of screening for ovarian cancer with the risk of ovarian cancer (ROC) algorithm based on rising CA125 levels. Journal of Clinical Oncology. 1996;14:2007. [Google Scholar]
- 34.McIntosh MW, Urban N. A parametric empirical Bayes method for cancer screening using longitudinal observations of a biomarker. Biostatistics. 2003;4:27–40. doi: 10.1093/biostatistics/4.1.27. [DOI] [PubMed] [Google Scholar]
- 35.Kim JE, Lee KT, Lee JK, Paik SW, Rhee JC, Choi KW. Clinical usefulness of carbohydrate antigen 19-9 as a screening test for pancreatic cancer in an asymptomatic population. Journal of gastroenterology and hepatology. 2004;19:182–6. doi: 10.1111/j.1440-1746.2004.03219.x. [DOI] [PubMed] [Google Scholar]
- 36.Satake K, Takeuchi T, Homma T, Ozaki H. CA19-9 as a screening and diagnostic tool in symptomatic patients: the Japanese experience. Pancreas. 1994;9:703–6. doi: 10.1097/00006676-199411000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Chang CY, Huang SP, Chiu HM, Lee YC, Chen MF, Lin JT. Low efficacy of serum levels of CA 19-9 in prediction of malignant diseases in asymptomatic population in Taiwan. Hepatogastroenterology. 2006;53:1–4. [PubMed] [Google Scholar]
- 38.Greenhalf W, Grocock C, Harcus M, Neoptolemos J. Screening of high-risk families for pancreatic cancer. Pancreatology. 2009;9:215–22. doi: 10.1159/000210262. [DOI] [PubMed] [Google Scholar]
- 39.Zubarik R, Gordon SR, Lidofsky SD, Anderson SR, Pipas JM, Badger G, et al. Screening for pancreatic cancer in a high-risk population with serum CA 19-9 and targeted EUS: a feasibility study. Gastrointest Endosc. 2011;74:87–95. doi: 10.1016/j.gie.2011.03.1235. [DOI] [PubMed] [Google Scholar]
- 40.Duraker N, Hot S, Polat Y, Hobek A, Gencler N, Urhan N. CEA, CA 19-9, and CA 125 in the differential diagnosis of benign and malignant pancreatic diseases with or without jaundice. Journal of surgical oncology. 2007;95:142–7. doi: 10.1002/jso.20604. [DOI] [PubMed] [Google Scholar]
- 41.Laack E, Nikbakht H, Peters A, Kugler C, Jasiewicz Y, Edler L, et al. Expression of CEACAM1 in adenocarcinoma of the lung: a factor of independent prognostic significance. J Clin Oncol. 2002;20:4279–84. doi: 10.1200/JCO.2002.08.067. [DOI] [PubMed] [Google Scholar]
- 42.Zhu J, Yang Y, Ma C, Zhang G, Wang K, Hu S. CEACAM1 cytoplastic expression is closely related to tumor angiogenesis and poorer relapse-free survival after curative resection of hepatocellular carcinoma. World J Surg. 2011;35:2259–65. doi: 10.1007/s00268-011-1119-2. [DOI] [PubMed] [Google Scholar]
- 43.Cruz PV, Wakai T, Shirai Y, Yokoyama N, Hatakeyama K. Loss of carcinoembryonic antigen-related cell adhesion molecule 1 expression is an adverse prognostic factor in hepatocellular carcinoma. Cancer. 2005;104:354–60. doi: 10.1002/cncr.21159. [DOI] [PubMed] [Google Scholar]
- 44.Orelle B, Keim V, Masciotra L, Dagorn JC, Iovanna JL. Human pancreatitis-associated protein. Messenger RNA cloning and expression in pancreatic diseases. J Clin Invest. 1992;90:2284–91. doi: 10.1172/JCI116115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cerwenka H, Aigner R, Bacher H, Werkgartner G, el-Shabrawi A, Quehenberger F, et al. Pancreatitis-associated protein (PAP) in patients with pancreatic cancer. Anticancer Res. 2001;21:1471–4. [PubMed] [Google Scholar]
- 46.Haridas D, Chakraborty S, Ponnusamy MP, Lakshmanan I, Rachagani S, Cruz E, et al. Pathobiological implications of MUC16 expression in pancreatic cancer. PLoS One. 2011;6:e26839. doi: 10.1371/journal.pone.0026839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hartwig W, Strobel O, Hinz U, Fritz S, Hackert T, Roth C, et al. CA19-9 in potentially resectable pancreatic cancer: perspective to adjust surgical and perioperative therapy. Ann Surg Oncol. 2013;20:2188–96. doi: 10.1245/s10434-012-2809-1. [DOI] [PubMed] [Google Scholar]
- 48.Katz MH, Varadhachary GR, Fleming JB, Wolff RA, Lee JE, Pisters PW, et al. Serum CA 19-9 as a marker of resectability and survival in patients with potentially resectable pancreatic cancer treated with neoadjuvant chemoradiation. Ann Surg Oncol. 2010;17:1794–801. doi: 10.1245/s10434-010-0943-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Capello M, Cappello P, Linty FC, Chiarle R, Sperduti I, Novarino A, et al. Autoantibodies to Ezrin are an early sign of pancreatic cancer in humans and in genetically engineered mouse models. Journal of hematology & oncology. 2013;6:67. doi: 10.1186/1756-8722-6-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Navarro Silvera SA, Miller AB, Rohan TE. Hormonal and reproductive factors and pancreatic cancer risk: a prospective cohort study. Pancreas. 2005;30:369–74. doi: 10.1097/01.mpa.0000160301.59319.ba. [DOI] [PubMed] [Google Scholar]
- 51.Duell EJ, Travier N, Lujan-Barroso L, Dossus L, Boutron-Ruault MC, Clavel-Chapelon F, et al. Menstrual and reproductive factors in women, genetic variation in CYP17A1, and pancreatic cancer risk in the European prospective investigation into cancer and nutrition (EPIC) cohort. Int J Cancer. 2013;132:2164–75. doi: 10.1002/ijc.27875. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.