Abstract
Objectives
Many service members do not seek care for mental health and addiction problems, often with serious consequences for them, their families, and their communities. This study tested the effectiveness of a brief, telephone-based, cognitive-behavioral intervention designed to improve treatment engagement among returning service members who screened positive for PTSD.
Method
OEF/OIF service members who screened positive for PTSD but had not engaged in PTSD treatment were recruited (N=300), randomly assigned to either control or intervention conditions, and administered the baseline interview. Intervention participants received the brief CBT intervention; control condition participants had access to usual services. All participants received follow-up phones calls at months 1, 3 and 6 to assess symptoms and service utilization.
Results
Participants in both conditions had comparable rates of treatment engagement and PTSD symptom reduction over the course of the six-month trial, but receiving the telephone-based intervention accelerated service utilization (treatment engagement and number of sessions) and PTSD symptom reduction.
Conclusions
A one-time brief telephone intervention can engage service members in PTSD treatment earlier than conventional methods and can lead to immediate symptom reduction. There were no differences at longer-term follow-up, suggesting the need for additional intervention to build upon initial gains.
Research has consistently shown that serving in the wars in Iraq and Afghanistan increases risk for PTSD, regardless of sample, measurement tool, combat exposure, or being physically wounded. (1) The prevalence rate of PTSD among this population is approximately 8%. (2, 10, 31) Research has also documented poor recovery trajectories for those suffering from symptoms of PTSD, (3,4) who may suffer from symptoms as long as 20 years after their war experiences. (3)
Among service members who acknowledge mental health symptoms, only about one quarter seek treatment. (5–7, 8) This low rate of treatment seeking remains true despite extensive outreach by the Department of Defense, the Veterans Administration, the National Institutes of Health, and the Department of Health and Human Services. More disturbing is information suggesting that service members seeking services are unlikely to stay in treatment. (9)
Numerous trials have been conducted to determine the barriers to treatment among returning OEF/OIF Veterans. (5, 11, 8, 12–15) The emerging pattern indicates that returning service members do not wish to be perceived as weak, (5, 8, 15) and they worry about the consequences for their military position. (5, 8, 15) Individuals most in need of treatment are also those who report the most substantial barriers to seeking treatment. (11,14) Research consistently reveal a pattern of attitudinal or cognitive barriers as well as system-level barriers that impact meaningful treatment utilization. (16)
The unfolding story suggests that the prevalence of PTSD among returning service members is high, treatment utilization is low, and those who do seek treatment are unlikely to stay in treatment. While it would be reassuring to know that those who make it to treatment and stay in treatment get good treatment, research suggests that they are unlikely to get minimally adequate treatment. (17,18) Without adequate treatment, returning service members will likely continue to suffer from symptoms of PTSD throughout their lives.
The purpose of this randomized controlled trial was to test the effectiveness of a brief, cognitive-behavioral intervention, delivered by telephone, that was designed to modify beliefs about treatment seeking in order to improve PTSD treatment utilization. We hypothesized that, compared to participants in the control group, participants receiving the brief intervention: 1) would be more likely to initiate PTSD treatment; 2) would attend more PTSD treatment sessions over the course of six months; and 3) would have greater reductions in their symptoms of PTSD.
Method
Participants
Participants were recruited through visits to armories and through social media advertisements. Service members who screened positive for PTSD after deployment to Iraq and/or Afghanistan and who had not initiated PTSD treatment were eligible to participate in this study. Initial screenings for PTSD were conducted with the Mini-International Neuropsychiatric Interview-PTSD subscale (MINI) (19). Participants who screened positive for PTSD and were interested in participating were informed fully of the study’s procedures and provided informed consent. This study was reviewed and approved by the Committee for the Protection of Human Subjects at Dartmouth College. This study lasted from November 2009 through August 2012.
Procedure
Upon enrollment in the study, participants were randomly assigned to either the intervention or control conditions using a randomization chart. Trained research staff administered the baseline assessment by telephone to all participants to assess demographic information, beliefs about PTSD treatment, and symptom severity. Intervention participants scheduled a time for the intervention session, and they received an additional phone call for this session. Participants in the control condition did not receive this intervention session. All participants received follow-up calls to assess service utilization, beliefs about PTSD treatment, and symptoms at months 1, 3, and 6 following the baseline assessment.
Measures
The Perceptions about Services Scale (PASS) assessed beliefs about PTSD treatment. The PASS is a 45-item self-report measure with items conforming to the Theory of Planned Behavior (20). Responses are rated on a 7-point Likert-type scale with higher numbers reflecting more positive beliefs about treatment (e.g., “1 = strongly disagree” to “7 = strongly agree”). Examples of items on the scale include: “Treatment will reduce symptoms”; “Some of my experiences would be too difficult to talk about in treatment”; and “Going to treatment means I can’t handle my problems.” Some items are reverse-coded for scoring. The PASS has adequate test-retest reliability and high internal consistency (8).
We used the PTSD Checklist-Military Version (21), which is a reliable and valid 17-item assessment of PTSD symptoms (22), and the Physicians Health Questionnaire, PHQ-9, which is a reliable and valid 10-item measure of depressive symptoms (23). In both cases, the total score represents overall symptom severity, with higher scores indicating greater severity.
To assess treatment utilization, all participants received follow-up phone calls at months 1, 3, and 6 after the baseline assessment. Participants were asked whether they had initiated treatment (by both scheduling and attending the appointment), and the number of treatment sessions attended. Information regarding the treatment session was also gathered (e.g., whether the appointment was at the VA or a non-VA setting and whether the appointment was with a psychiatrist, psychologist, or other). We also assessed the type of treatment received (e.g., CBT, medications, or exposure therapy).
Intervention sessions
Participants in the intervention group received one intervention session within a week of the baseline assessment. The session was administered by telephone and lasted approximately 45–60 minutes. The sessions were based on the principles of cognitive-behavioral theory (CBT), which posits that thoughts, feelings, and behaviors interact with each other in predictable ways (12). Since thoughts are modifiable, changing thoughts about situations may change behavior in those situations. For example, the thought, “I don’t need treatment” might become “I might need treatment considering how hard it is to sleep and the impact it is having on my relationships and job” or “I am drinking a lot to avoid thinking so maybe treatment could help me deal with my memories better.” Participants identified individual beliefs about treatment during the intervention session. The intervention session addressed a maximum of three beliefs with each participant.
Statistical analyses
Means and frequencies described the characteristics of the sample, and t-tests and chi-square tests examined differences between the two groups at baseline. Logistic regression was used to compare the two groups for differences in treatment initiation at each follow-up point, which provides the same result as a chi-square test but also provides the regression coefficient. Because treatment utilization, that is, the number of treatment sessions attended, was a count variable that is positively skewed, the negative binomial model assessed group differences in the cumulative number of treatment visits at each follow-up point. Generalized estimating equation models with the normal distribution and the identity link were used for longitudinal analysis of PTSD and depression symptom severity. All statistical analyses were conducted with SAS v. 9.3. A p-value of .05 was used throughout to indicate statistical significance.
Results
Four hundred and seventy five individuals completed the PTSD screening assessment; three hundred eligible individuals provided informed consent and were enrolled in the trial. Of the 175 individuals who did not meet eligibility criteria, 63 were already in treatment, 76 did not screen positively for PTSD, and 36 were not eligible for other reasons (e.g., not an OEF/OIF veteran). Of the 300 enrolled participants, 143 were randomly assigned to the intervention condition, and 157 were assigned to the control condition. Twenty-six participants (20 in the intervention condition and 6 in the control condition) withdrew or were withdrawn from the study after baseline assessment, leaving a total of 274 participants. Thirty-six participants were lost to follow-up (14 in the intervention arm and 22 in the control arm). We removed participants who withdrew from the study from the analytic dataset leaving a total of 123 intervention participants and 151 control participants.
Table 1 shows that the majority of the participants were male (87%) and Caucasian (71%), with a mean age of 29 years. The only significant difference between groups was for age; the intervention group was younger than the control group (28.3 versus 30.2). Both groups reported moderate to moderately severe symptoms of PTSD and depression at baseline.
Table 1.
Characteristics of the intervention and control groups at baseline.
| INTERVENTION N = 123 |
CONTROL N = 151 |
Statistic | df | p-value | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Characteristic | N | % | N | % | |||
| Gender | .057 | ||||||
| Female | 21 | 40 | 14 | 60 | χ2 = 3.6 | 1 | |
| Male | 102 | 57 | 136 | 43 | |||
| Race | .774 | ||||||
| Caucasian | 87 | 46 | 103 | 54 | χ2 =.52 | 2 | |
| African American | 15 | 39 | 23 | 61 | |||
| Other | 18 | 45 | 22 | 55 | |||
| Age (M±SD) | 28.3±5.3 | 30.2±6.9 | t = −2.4 | 268 | .018 | ||
| Health Insurance | .898 | ||||||
| Yes | 96 | 79 | 109 | 73 | χ2 = 1.5 | 1 | |
| No | 25 | 21 | 40 | 27 | |||
| Travel to doctor | .330 | ||||||
| 0–30 miles | 85 | 69 | 99 | 66 | χ2 = −2.2 | 2 | |
| 31–60 miles | 8 | 7 | 16 | 11 | |||
| 61+miles | 2 | 2 | 5 | 3 | |||
| No doctor | 10 | 8 | 17 | 11 | |||
| PCL (M±SD) | 59.2±11.7 | 59.7±11.7 | t = .39 | 271 | .695 | ||
| PHQ9 (M±SD) | 16.3±4.7 | 16.4±4.8 | t = −.19 | 271 | .853 | ||
A clear pattern emerged regarding treatment engagement during the trial (see Table 2). Due to eligibility criteria, participants had no PTSD treatment engagement at baseline. At the one-month follow-up, the majority of participants continued to resist seeking PTSD treatment, although intervention participants were twice as likely to seek treatment as control participants (χ2 = 3.85, df = 1, p < .049, OR = 2.08). At the three-month follow-up, approximately one-third of both groups reported seeking treatment for PTSD (χ2 = 1.29, df = 1, p = .257, OR = 1.39.). At the six-month follow-up, rates of treatment initiation continued to rise for both groups, and did not differ significantly (χ2 = 3.45, df = 1, p = .063, OR = 1.62).
Table 2.
Rates of PTSD treatment initiation and mean number of treatment sessions attended for the two groups over time.
| Intervention | Control | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| PTSD Treatment Initiation | n | # initiated | % | n | # initiated | % |
| 1 mo.* | 103 | 22 | 21 | 121 | 14 | 12 |
| 3 mo. | 99 | 38 | 38 | 110 | 34 | 31 |
| 6 mo. | 111 | 65 | 59 | 131 | 61 | 47 |
| PTSD Treatment Attendance (number of sessions) | n | M±SD | n | M±SD |
|---|---|---|---|---|
| 1 mo. | 103 | .38±.89 | 121 | .20±.63 |
| 3 mo. | 99 | 1.08±2.17 | 110 | .67±1.47 |
| 6 mo.* | 111 | 4.06±11.45 | 131 | 2.47±4.54 |
p < .05
A similar pattern emerged for the number of PTSD treatment sessions attended (see Table 2. While the majority of participants attended no sessions of PTSD treatment in the first month of participation, those who did attend reported only one session, resulting in low overall rates of attendance and no difference between groups (χ2 = 2.81, df = 1, p = .094). At the three-month interview, the number of PTSD treatment sessions attended remained low and not significantly different between the two groups (χ2 = 2.77, df =1, p = .096). At the six-month follow-up, intervention participants reported attending a significantly greater number of treatment sessions than the control group participants (χ2 = 4.09, df = 1, p = .043).
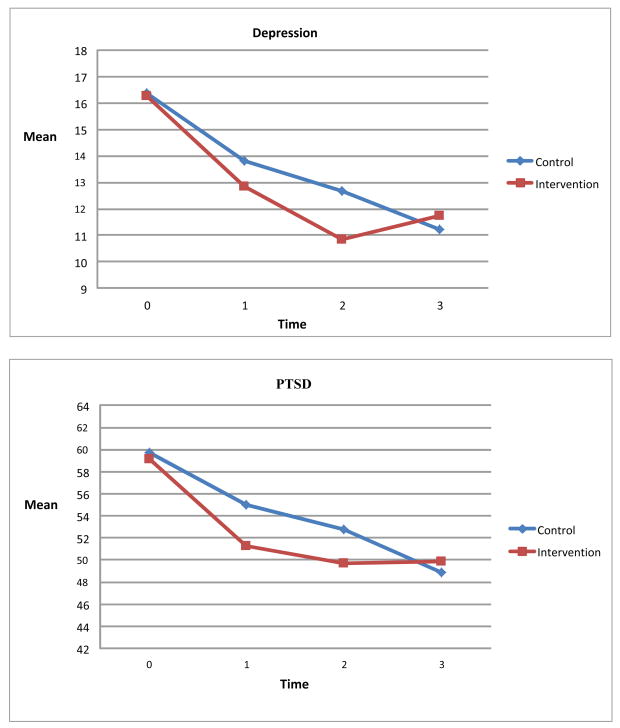
Participants in both groups reported significant reductions in symptoms of both PTSD and depression during the course of the six-month trial (see Table 3). Symptoms of PTSD reduced among intervention participants from a mean PCL of 59.2 at baseline to 49.8 at the 6-month follow-up. Participants in the control group reported comparable reductions in PTSD symptoms, with a mean PCL of 59.7 at baseline and a mean of 48.9 at 6-month follow-up. Due to the non-linear nature of the changes in symptoms over time, we conducted a piecewise regression analysis, where the first piece is from baseline to 3-month follow-up, and the second piece is from 3-month follow-up to 6-month follow-up. Longitudinal analysis indicated a non-significant group by time interaction for the first piece, although the intervention group showed more reduction in PTSD symptoms. A significant group by time interaction was found for the second piece, reflecting the crossover of the two groups between the 3-and 6-month follow-up (coefficient = 4.69, p = .004). Whereas both groups reported reductions in PTSD symptoms during the early course of the trial, intervention participants reported reductions earlier. Participants in the control group reported continued reductions from months 3 through 6, whereas intervention participants reported no further reductions.
Table 3.
Group mean PTSD and depression symptom severity scores over time.
| Intervention (N=123) | Control (N=151) | |
|---|---|---|
| PTSD Symptoms (M±SD) | ||
| Baseline | 59.2±11.8 | 59.7±11.7 |
| 1 mo. | 51.3±13.6 | 55.0±13.1 |
| 3 mo. | 49.7±15.2 | 52.8±14.2 |
| 6 mo. | 49.8±15.2 | 48.9±15.1 |
| Depression Symptoms (M±SD) | ||
| Baseline | 16.3±4.7 | 16.4±4.8 |
| 1 mo | 12.8±5.6 | 13.8±4.8 |
| 3 mo | 10.9±5.8 | 12.7±5.6 |
| 6 mo | 11.8±5.8 | 11.2±5.9 |
Possible scores range from 17 to 85, with higher scores indicating more severe PTSD
Possible scores range from 0 to 36, with higher scores indicating more severe depression
A similar pattern emerged for symptoms of depression (see Table 3 and Figure 1). Intervention participants changed from a mean PHQ9 score of 16.3 at baseline to 11.8 at the 6-month follow-up point. Control participants changed from a mean PHQ9 of 16.4 at baseline to 11.2 at 6-month follow-up. Piecewise longitudinal regression analysis revealed a significant group by time interaction effect for changes in symptoms of depression from baseline to 3-month follow-up (coefficient = −.856, p = .026) and a significant interaction from 3-month to 6-month follow-up (2.361, p = .0005). The pattern for depression symptoms is similar to the pattern as for symptoms of PTSD; the intervention group showed more change for the initial period, but less change for the latter period.
Figure 1.
Mean changes to depression and PTSD over time.
Analysis of covariance assessed the impact of PTSD treatment utilization on symptoms of PTSD at endpoint, controlling for baseline PTSD symptom severity. It was hypothesized that participants who received treatment, regardless of experimental condition, would have fewer symptoms than those who did not receive treatment. Attending PTSD treatment during the six-month study was not associated with lower PTSD symptoms.
Discussion
Our brief, phone-based, cognitive-behavioral intervention accelerated treatment utilization and symptom reduction among OEF/OIF Veterans who screened positive for PTSD and had resisted treatment. Participants receiving the intervention were likely to get to treatment sooner than participants in the control condition. Likewise, participants receiving the intervention attended more PTSD treatment sessions than participants in the control condition during the 6-month study period. The intervention used in this study was low dose, only composed of one hour by phone with a psychologist. Adding follow-up sessions might improve the rate of treatment initiation and attendance beyond that found in this trial. Results of this trial are consistent with other literature assessing interventions to increase psychotherapy attendance (24).
This is one of very few studies that focus on military populations that are not currently enrolled in VHA or DoD mental health care. Much of the current work focuses on improving rates of mental health utilization among patients already being seen in primary care (25,26). In this trial, success was dependent on the individual attending PTSD treatment attendance, and also in being able to navigate enrollment into the VA system. Likewise, this is one of the only trials that focus on using cognitive-behavioral strategies with military populations to improve treatment utilization. Other trials have used motivational interviewing to improve treatment utilization among patients already enrolled in VA care. One potential benefit of using cognitive-behavioral methods is that with large enough samples, beliefs about treatment could be coded and tested to see if a change in belief predicted the behavior of initiating PTSD treatment. Testing models of belief change would provide evidence as to whether individual perceptions drive the decision of whether or not to seek treatment.
It was hypothesized that participants who received the intervention session would have greater reductions in symptoms over the course of the six-month study than participants in the control condition. Yet, both groups showed similar reductions in symptoms of PTSD and depression over the course of the study. Although PTSD treatment attendance was hypothesized to result in greater symptom reduction, the results indicated that treatment attendance was not associated differentially with symptom reduction. Further research is needed to help understand this PTSD treatment response.
Several factors have been associated with the decision to seek treatment within military populations. Many Veterans have identified an unwillingness to seek treatment because they do not want to be prescribed medications (27, 28). Stigma has also been identified in the literature as influential in the decision (29, 30); however, participants in this study only infrequently identified stigma as an issue during intervention sessions (28). The most influential cognitive predictors of treatment utilization may be perceived symptom severity and avoidance discussing the traumatic event (28).
This study was limited in that it only focused on the cognitive barriers to treatment seeking for PTSD. Other barriers, including distance to VA although it was not a significant covariate in our outcome analyses, may be involved in the decision to seek treatment. While these practical barriers are often cited as limiting treatment engagement, ultimately it may be individual’s perceptions of these barriers that drive the decision of whether or not to seek care. Further, substance use was not measured within this trial, and may have been involved in decisions to seek treatment.
This study was also limited as treatment utilization was assessed by self-report. Self-report measures of treatment utilization were the only practical method of attaining this information. Almost half of the sample reported that they never attended treatment, and many accessed treatment in non-VA settings. Having a self-report measure allowed us to gather data on individuals outside of the VA setting.
Twenty-six participants withdrew from the study (20 in the intervention condition and 6 in the control condition) after the baseline assessment. A higher level of withdrawal may have occurred in the intervention condition from participants who were avoiding an “intervention session”. Avoidance behavior is common among individuals suffering with symptoms of PTSD, and this avoidance may have been demonstrated through a higher withdrawal rate among participants in the intervention condition.
In conclusion, a one-time brief telephone intervention can engage service members in PTSD treatment earlier than conventional methods and can lead to immediate symptom reduction. There were no differences at longer-term follow-up, suggesting the need for additional intervention to build upon initial gains. This could take place in the form of additional booster sessions occurring at 2 weeks or 1 month subsequent to the initial intervention session. This additional session could booster the intention to receive PTSD treatment, to stay in PTSD treatment, allow for continued use of coping skills, or even allow service members to continue to explore the meaning of the trauma experienced.
Contributor Information
Tracy Stecker, Email: tracy.stecker@dartmouth.edu, Dartmouth Medical School, Family Medicine, 2 Whipple Place Suite 202, Lebanon, New Hampshire 03766.
Gregory McHugo, Dartmouth College, Dartmouth Psychiatric Research Center, Rivermill Commercial Center.
Haiyi Xie, NH-Dartmouth Psychiatric Research Center, 2 Whipple Place, Suite 202, Lebanon, New Hampshire 03766
Katrina Whyman, Dartmouth.
Meissa Jones, Dartmouth.
References
- 1.Ramchand R, Karney BR, Osilla KC, et al. Prevalence of PTSD, depression, and TBI among returning service members. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. 2008:35–84. [Google Scholar]
- 2.Schnurr PP, Kaloupek D, Sayer N, et al. Introduction to Special Section: Understanding the impact of the wars in Iraq and Afghanistan. Journal of Traumatic Stress. 2010;23(1):3–4. doi: 10.1002/jts.20502. [DOI] [PubMed] [Google Scholar]
- 3.Solomon Z, Mikulincer M. Trajectories of PTSD: a 20-year longitudinal study. American Journal of Psychiatry. 2006;163(4):659. doi: 10.1176/ajp.2006.163.4.659. [DOI] [PubMed] [Google Scholar]
- 4.Kulka RA, Schlenger WE, Fairbank JA, et al. Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment Study. New York: 1990. [Google Scholar]
- 5.Hoge CW, Castro CA, Messer SC, et al. Combat Duty in Iraq and Afghanistan, Mental Health Problems, and Barriers to Care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 6.Milliken CS, Auchterlonie MS, Hoge CW. Longitudinal Assessment of Mental Health Problems Among Active and Reserve Component Soldiers Returning from the Iraq War. Journal of the American Medical Association. 2007;298(18):2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- 7.Tanielian TL. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Vol. 720. Rand Corp; 2008. [Google Scholar]
- 8.Stecker T, Fortney J, Hamilton F, et al. Engagement in mental health treatment among veterans returning from Iraq. Patient Preferences and Adherence. 2010;4:45–49. doi: 10.2147/ppa.s7368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenheck RA, Fontana AF. Recent trends in VA treatment of post-traumatic stress disorder and other mental disorders. Health Affairs. 2007;26(6):1720. doi: 10.1377/hlthaff.26.6.1720. [DOI] [PubMed] [Google Scholar]
- 10.Stecker T, Fortney J, Owen R, et al. Co-Occurring Medical, Psychiatric, and Alcohol-Related Disorders Among Veterans Returning From Iraq and Afghanistan. Psychosomatics. 2010;51(6):503. doi: 10.1176/appi.psy.51.6.503. [DOI] [PubMed] [Google Scholar]
- 11.Kim PY, Britt TW, Klocko R, et al. Stigma, Negative Attitudes About Treatment, and Utilization of Mental Health Care Among Soldiers. Military Psychology. 2011;23(1):65–81. [Google Scholar]
- 12.Britt TW, Bennett EA, Crabtree M, et al. The Theory of Planned Behavior and Reserve Component Veteran Treatment Seeking. Military Psychology. 2011;23(1):82–96. [Google Scholar]
- 13.Rae Olmsted KL, Brown JM, Peeler JR, et al. Mental health and substance abuse treatment stigma among soldiers. Military Psychology. 2011;23(1):52–64. [Google Scholar]
- 14.Pietrzak RH, Johnson DC, Goldstein MB, et al. Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatric Services. 2009;60(8):1118. doi: 10.1176/ps.2009.60.8.1118. [DOI] [PubMed] [Google Scholar]
- 15.Schell TL, Marshall GN. Survey of individuals previously deployed for OEF/OIF. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. 2008:87–115. [Google Scholar]
- 16.Vogt D. Mental Health-Related Beliefs as a Barrier to Service Use for Military Personnel and Veterans: A Review. Psychiatric Services. 2010;62(2):135. doi: 10.1176/ps.62.2.pss6202_0135. [DOI] [PubMed] [Google Scholar]
- 17.Lu MW, Duckart JP, O’Malley JP, et al. Correlates of Utilization of PTSD Specialty Treatment Among Recently Diagnosed Veterans at the VA. Psychiatric Services. 2011;62(8):943. doi: 10.1176/ps.62.8.pss6208_0943. [DOI] [PubMed] [Google Scholar]
- 18.Harpaz-Rotem I, Rosenheck RA. Serving Those Who Served: Retention of Newly Returning Veterans From Iraq and Afghanistan in Mental Health Treatment. Psychiatric Services. 2011;62(1):22. doi: 10.1176/ps.62.1.pss6201_0022. [DOI] [PubMed] [Google Scholar]
- 19.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59 (Suppl 20):22–33. [PubMed] [Google Scholar]
- 20.Ajzen I. The Theory of Planned Behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- 21.Weathers FW, Litz BT, Herman DS, et al. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility in Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- 22.Blanchard E, Jones-Alexander J, Buckley T, et al. Psychometric properties of the PTSD Checklist (PCL) Behavior Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Journal of the American Medical Association. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 24.Oldham M, Kellett S, Miles E, et al. Interventions to increase attendance at psychotherapy: a meta-analysis of randomized controlled trials. Journal of Consulting and Clinical Psychology. 2012;80(5):928–939. doi: 10.1037/a0029630. [DOI] [PubMed] [Google Scholar]
- 25.Seal KH, Abadjian L, McCamish N, et al. A randomized controlled trail of telephone motivational interviewing to enhance mental health treatment engagement in Iraq and Afghanistan veterans. General Hospital Psychiatry. 2012 doi: 10.1016/j.genhosppsych.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 26.Seal KH, Cohen G, Bertenthal D, et al. Reducing barriers to mental health and social services for Iraq and Afghanistan veterans: Outcomes of an integrated primary care clinic. Journal of General Internal Medicine. 2011;26(10):1160–1167. doi: 10.1007/s11606-011-1746-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reger GM, Durham TL, Tarantino KA, et al. Deployed soldiers reactions to exposure and medication treatments for PTSD. Psychological Trauma: Theory, Research, Practice and Policy. 2012:1–8. [Google Scholar]
- 28.Stecker T, Shiner B, Watts B, et al. Barriers to Treatment Seeking Among Veterans of the Wars in Iraq and Afghanistan Who Screen Positive For Posttraumatic Stress Disorder. Psychiatric Services. 2013;64(3):280–283. doi: 10.1176/appi.ps.001372012. [DOI] [PubMed] [Google Scholar]
- 29.GAO Report. Number of Veterans receiving care, barriers faced and efforts to increase access. 2011. VA mental health. [Google Scholar]
- 30.Brown MC, Creel AH, Engel CC, et al. Factors associated with interest in receiving help for mental health problems in combat veterans returning from deployment to Iraq. Journal of Nervous Mental Disorders. 2011;199:797–801. doi: 10.1097/NMD.0b013e31822fc9bf. [DOI] [PubMed] [Google Scholar]
- 31.Sundin J, Fear N, Iverson A, et al. PTSD after deployment to Iraq: conflicting rates, conflicting claims. Psychological Medicine. 2010;40(3):367–82. doi: 10.1017/S0033291709990791. [DOI] [PubMed] [Google Scholar]