Abstract
Background:
Medication nonadherence remains a significant public health problem, and efforts to improve adherence have shown only limited impact. The tailoring of messages has become a popular method of developing communication to influence specific health-related behaviors but the development and impact of tailored text messages on medication use is poorly understood.
Objectives:
The aim of this paper is to describe an approach to developing theory-based tailored messages for delivery via mobile phone to improve medication adherence among patients with diabetes.
Methods:
Kreuter’s five-step tailoring process was followed to create tailored messages for mobile phone delivery. Two focus group sessions, using input from 11 people, and expert review of message content were used to adapt the survey instrument on which the messages were tailored and edit the developed messages for the target population.
Results and conclusions:
Following established tailoring methods a library of 168 theory-driven and 128 medication-specific tailored messages were developed and formatted for automated delivery to mobile phones. Concepts from the Health Belief Model and Self-Determination Theory were used to craft the messages and an algorithm was applied to determine the order and timing of messages with the aim of progressively influencing disease and treatment-related beliefs driving adherence to diabetes medication. The process described may be applied to future investigations aiming to improve medication adherence in patients with diabetes and the effectiveness of the current messages will be tested in a planned analysis.
Keywords: Tailoring, Adherence, Mobile health, Text messaging, Behavioral theory
Background
A variety of interventions have been developed using communication theory to promote health behavior change. Many of these interventions have used targeted messaging whereby a particular patient population (defined by their age, disease, etc.) received the same type of message aimed at eliciting a particular behavior based on that group’s shared characteristics.1 Over time, methods have become more focused, narrowing the emphasis from population-level factors to tailoring according to characteristics that reffect more proximate determinants of health behaviors, such as beliefs about the risks and benefits of treatment. By tailoring, behavioral interventions may highlight condition and treatment-specific influences that are most personally relevant to each subject with a clear, personalized goal in mind.
The general approach to tailoring health communication is to create messages that are individualized for each recipient based on information collected about that user via survey. This information can be used to create original messages or can be added to pre-existing material. Common survey elements used to tailor health communication include the participant’s name, age, gender, race, family structure, and details related to the outcome of interest (e.g. potential consequences of inadequate disease management and the benefits of adhering to self-management plans). These characteristics are strategically placed into a message with the aim of influencing behavior by creating a piece of communication that appears to be relevant only to the recipient.
The foundation for tailoring messages rests on information processing theory, which suggests that people are more likely to process information thoughtfully when they perceive that information to be personally relevant.2 A prominent example of such a theory, the Elaboration Likelihood Model (ELM) posits that separate routes of information processing (peripheral and central) influence how information is managed and is based on the individual’s need for cognition and motivation.2 The benefits of more elaborated processing include longer message retention and an increased likelihood of permanent attitude change.3 Therefore, applying ELM, the benefit of tailoring health communication is the improved odds of capturing users’ attention through individualization that will increase the likelihood of thoughtful consideration of message content and ultimately a greater impact on health behavior.
Message tailoring has shown promise as a mechanism for effectively promoting individual health behavior change. Reviews of tailored health interventions have concluded that tailoring is useful in a variety of areas including smoking cessation, physical activity, dietary change, and preventative screening.4–16 Tailoring has also been applied successfully to the problem of medication nonadherence: the inability to take medications as prescribed by a health care provider, which may be either intentional (due to motivational or perceived issues) or unintentional (forgetfulness). Positive applications of tailoring to medication adherence have been observed among patients with hypertension, schizophrenia, hyperlipidemia, and asthma.17–23 However, the vast majority of these studies were conducted using either print or computer-based materials, limiting their reach and effectiveness. Adherence problems are also common among people with diabetes, resulting in inadequate physiological control and a higher risk of complications.24–26 Unfortunately, interventions focused on improving diabetes medication adherence have had only limited success.27 effective interventions for diabetes medication adherence support likely require an individualized approach addressing each patient’s array of health beliefs and other limitations – a problem for which tailored health communication may be ideally suited.
Recently, mobile phone messaging has been increasingly used in tailoring studies. Mobile phones are nearly ubiquitous and could be an effective channel for improving self-management support between face-to-face interactions with clinicians.28 Most studies focused on improving medication adherence using mobile phones have been limited to improving unintentional nonadherence through reminder messages, and results of these investigations have been mixed in terms of the effect on medication use.29–34 However, a limited number of studies have incorporated the tailoring of health messages into interventions focused on medication nonadherence. Petrie and colleagues (2012) showed improved medication adherence to controller inhalers among adult patients with asthma by text messaging subjects from 1 to 3 times daily over 18 weeks.35 Several recent studies have combined mobile phone adherence reminders and tailored messages addressing patients’ beliefs associated with intentional nonadherence. For example, using an intervention called “Sweet Talk”—a tailored text messaging support system for patients with type 1 diabetes—Franklin and colleagues (2006) observed improvements in self-reported adherence to diabetes medications after 12 months.36 Such results suggest that tailored text communication could improve diabetes-related adherence, but additional testing is necessary to confirm and expand on our understanding of how this messaging channel may be most effectively applied. The aim of this paper is to describe an approach to developing theory-based tailored messages that can be delivered by mobile phone to improve medication adherence among patients with diabetes.
Methods
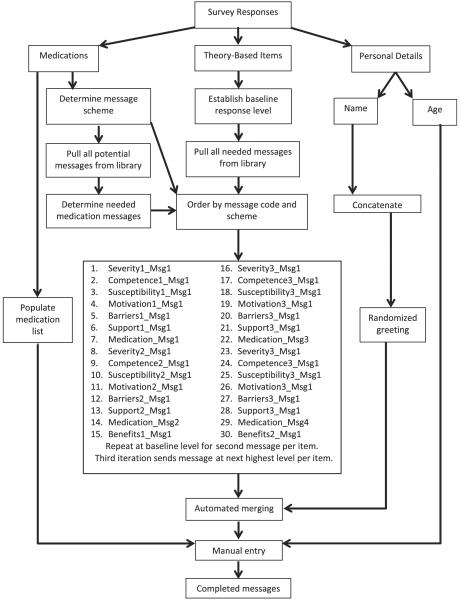
Kreuter’s five-step process of tailored message development was used to produce a library of messages addressing various contributing factors to nonadherence and an algorithm for individualizing each patient’s series of messages while customizing this approach for mobile text messaging delivery.5 This process included the following steps as suggested: problem identification, assessment tool creation, message creation, message storage, and tailoring algorithm development (Fig. 1).5 The following section describes the processes taken to fulfill these steps for developing the message library for a diabetes adherence support intervention. This study was approved by the Institutional Review Boards at both the University of Michigan and Mercy Health Partners (Muskegon, MI).
Fig. 1.
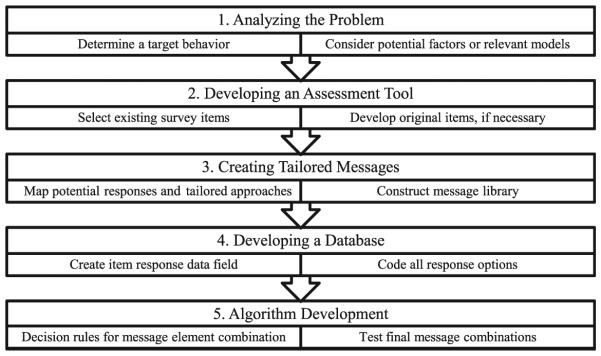
Kreuter’s five-step tailoring process. Adapted from process detailed in Kreuter (1999).5
Problem identification
Recognizing that diabetes medication nonadherence was an important contributor to poor outcomes, Lakeshore Health Network (“Network”), a physician hospital organization with over 300 primary care and specialty physicians, began exploring potential solutions in 2011, including a community-wide medication adherence awareness campaign focusing on consumer engagement. The network prioritized strategies using information technology in order to improve self-management support in a way that would be potentially cost-effective. Tailored health communication supporting adherence and delivered via text messages appealed to the community’s health leaders, who partnered with researchers at the University of Michigan to develop such an approach.
To clearly define the problem, it was critical to first understand the specific factors impacting diabetes patients’ adherence behavior. Two theories of health behavior were chosen to establish a framework for understanding the processes determining diabetes medication use. Self-Determination Theory (SDT) suggests that people are driven by 3 essential needs: competence, relatedness, and autonomy. The pursuit of these needs is reffected in a continuum of motivation, ranging from amotivation to intrinsic motivation, where the latter is completely selfdetermined.37 Evidence suggests that the likelihood of long-term maintenance of behavior change is increased if one is intrinsically motivated rather than influenced by external forces.38,39 For example, individuals may take medications initially because physicians tell them to do so. Over time, continuing to take medications is likely a decision based on internal motivation that includes an implicit balancing of benefits and costs to the user. Ultimately, medication taking may become habit; however, adoption of such a behavior may be a process for some and, as such, requires that messages encouraging the behavior guide the patient along the way rather than forcing change upon them. Applied to medication-taking, Self-Determination Theory concepts have been found to be related to this behavior: evidence suggests that autonomous self-regulation and perceived competence each play an important role in the ongoing taking of medication.40
The Health Belief Model (HBM) has been extensively applied to a variety of health behaviors including medication adherence. Using the model, studies of adherence have identified numerous barriers that contribute to inadequate medication use and several health beliefs (perceived susceptibility, severity, and benefits) have been predictive of this behavior.18,41,42 At its core, HBM posits that a health-related action will be taken if a person believes that a negative health condition can be avoided through that action, the behavior is likely to result in a positive outcome, and they can successfully execute the intended behavior.43 In the context of medication use, the likelihood of an individual taking their medication may then be increased if they believe that they are susceptible to a specific condition, believe that condition would have serious potential consequences, believe that taking the medication would reduce the probability or severity of the condition, and understand that these benefits outweigh any costs of or barriers to taking the medication. Additionally, the likelihood of taking the medication would be increased if the individual believed in their ability to take it as directed and may also be improved if triggers to taking the medication (such as symptoms or encouragement) are introduced. Multiple studies have observed the role that HBM constructs may play in the medication-taking process, suggesting that levels of each of the incorporated concepts may be predictive of resulting adherence or nonadherence.44–49 Applying this model allows the crafting of messages to be based on the particular constellation of beliefs for individual patients and the level of belief individuals have in each construct.
Assessment tool creation
Initial concepts and items in the assessment tool
The first step in message development is the selection of a proper survey to capture patient characteristics that can guide the tailoring process. In the current study, the tailoring process was guided by instruments incorporating Self-Determination Theory and the Health Beliefs Model (Fig. 2).
Fig. 2.
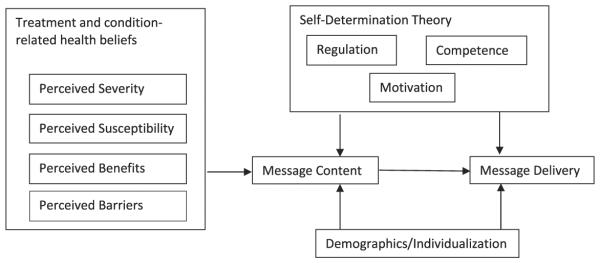
Framework for message development.
Concepts related to Self-Determination Theory were captured using the Treatment Self-Regulation Questionnaire (TSRQ) and the Perceived Competency Scale. The concepts of motivation and support as measured in the TSRQ have acceptable internal consistency (Cronbach’s α > 0.80) and validity has been verified in diabetes.50,51 Perceived competence was measured using items from the Perceived Competence Scale, allowing messages to be based on initial competence that can be adjusted over time. Cronbach’s a for this scale is 0.94 and support for its construct validity has been demonstrated.52
The extensive application of Health Belief Model (HBM) to health behaviors has produced validated survey instruments specific to conditions and modes of treatment. We used a diabetes-specific instrument developed by Given (1983), and then by Becker and Janz (1985), to capture diabetes and treatment-related health beliefs.41,53 The Cronbach’s α ranged from 0.70 to 0.89 depending on the domain of the scale and content validity was verified by a separate study.53,54 Using this instrument, 4 HBM concepts were assessed including perceived disease severity, susceptibility to negative outcomes, benefits of medication use, and barriers to medication use.
In addition to these theory-driven items, 2 other domains of questions were added to the instrument to more deeply tailor the messages. The subject’s name was used in every message and their age was used sporadically. In addition, we included details about the subject’s current diabetes medications, including the name of the medications (as written on the bottles), number of times taken each day, number of pills taken at each dose, and time of day the medication was to be taken. This information was used to time text message delivery and craft messages that would be specific to each subject’s treatment (benefits, safety, and mechanism of action). The name of medications was also included in some theory-driven messages.
Assessment tool adjustment
To incorporate specific perspectives from the target population in the message design, 2 focus groups were held on separate days including patients with diabetes from the Muskegon, MI area. These sessions were led by the study’s primary investigator and guided by questions focused on issues related to diabetes treatment adherence and mobile phone use. The goal of the focus groups was to uncover any medication-taking problems specific to this community and not already considered in our theories, as well as inform the study on how adults in the area use their mobile phones to text message and access health-related information. Recruitment was done with advertisements in area physician offices, pharmacies, and community health practices using flyers and word-of-mouth. The target population for these sessions was intended to represent the population of interest for the larger, proposed study: adults with diabetes currently under treatment for diabetes and who had an active mobile phone. Basic demographic information on the participants was collected by an anonymous survey given at the end of each session. Sessions were audio recorded, dictated by a research assistant, and lasted approximately an hour each. Transcriptions were analyzed by the principal investigator following each session. Emerging themes and concepts were noted and used to inform potential changes to the proposed assessment tool and the message development process.
Two sessions were held including 11 people with diabetes. All but 3 of the participants were female, most were Caucasian, and most had been diagnosed with type 2 diabetes (Table 1). Most participants reported that they have been treated for diabetes for 5 years or less. Participants’ ages ranged from 48 to 69 and the number of medications being taken for diabetes ranged from 0 to 4.
Table 1.
Focus group subject characteristics (n = 11)
| Characteristic | Frequency (n) |
|---|---|
| Gender | |
| Male | 3 |
| Female | 8 |
| Race | |
| Caucasian | 6 |
| African American | 4 |
| Hispanic | 1 |
| Diagnosis | |
| Type I diabetes | 4 |
| Type II diabetes | 7 |
| Treatment years | |
| <1 | 4 |
| 1–3 | 2 |
| 3–5 | 1 |
| 5–10 | 2 |
| >10 | 2 |
Several themes were identified from the focus groups. First, participants reported that their mobile phone use was relatively limited. Most indicated that they used their phone for basic functions, generally talking to family members or for emergencies, and if other functions were used it tended to be text messaging. When texting, many subjects indicated that it was mostly for communicating with family members, 1 person specifically mentioned that they “liked the texting because it is faster.” For those utilizing texting functions, estimates of the number of messages per day ranged from 1–2 to 9–10. However, not all participants viewed texting favorably: “I don’t like reading information on text messages. texting is for the younger people.” One subject specifically mentioned that the size of the text in the message made them too difficult to read. Members of both groups reported even more limited use of smartphone applications.
Several participants indicated that they already used their mobile phone to access health-related materials, mostly to gather information about symptoms and treatments. However, the majority of participants indicated that the computer remains their primary source of health-related information, “to see what’s wrong, you know symptoms that I have. I just Google it.” Patients who sought health information online did so with varying frequency, some as often as weekly and others less than once every few months. When asked how valuable they would view receiving personalized health-related information on their phone, participants reported mixed feelings. Generally, those already using their phones on a more regular basis reported more favorable interest; however, more consistent support was garnered for receipt of similar information if delivered by “snail mail… a couple times a month.”
Participants indicated that adherence to their prescribed diabetes treatment was generally good: “I don’t see a challenge, just follow the rules. They say just take it 2 times a day and that’s what I do.” When given explicit directions from their physician, these subjects indicated that they were better able to follow the protocol, knowing what the consequences of inaction would be. Moreover, if doses were missed, respondents indicated that these were only on occasion.
However, 1 point was raised by members of both focus groups. When beginning a new medication, participants said that they would have benefitted from learning more about potential side effects of new treatments. Multiple participants mentioned unexpected side effects that were brought on by new medications that were not mentioned by their providers. Specifically, the participants suggested that these details could have been better described to them by pharmacists: “As soon as they gave [it to] me I wish they had told me I would feel tired. It’s 3 o’clock in the evening and I’m trying to go do something and I was knocked out. They didn’t tell me that right away.”
Based on the information from the focus groups, changes to the assessment tool were deemed unnecessary, as other challenges to the medication use process in this population were not identified. However, 1 item from the original survey was removed as it was specific to changing eating habits rather than medication use; altering this item to fit the study’s aims was deemed inappropriate. The final assessment tool included 3 sections (a medication list, the theory-based items, and demographic details) and 34 items, 29 of which were used for tailoring (Appendix).
Message creation
Based on the items in the assessment tool, text message stems were drafted using each theoretical concept survey item, and the range of answer options for each item was used to develop different messages tailored to the specific response on that item. The assessment tool included Likert-type items with response options ranging from “strongly disagree” to “strongly agree” for HBM constructs and from 1 to 7, ranging from “not at all true” to “very true,” for SDT items. For Health Belief Model items, messages were written for responses deemed “high” or “low.” This was determined using a survey response to each item where responses of “agree” or “strongly agree” (“disagree” or “strongly disagree” for those reverse coded) indicated “high” and responses of “uncertain,” “disagree,” or “strongly disagree” would indicate “low” (“uncertain,” “agree,” or “strongly agree” for those reverse coded). For Self-Determination Theory items, messages were drafted for “low,” “medium,” and “high,” corresponding to 1 and 2, 3–5, and 6 and 7 responses, respectively, or the opposite if reverse coded. For example, a response of “2” to the first item related to competence, “I am confident that I can take care of my diabetes” would suggest that this subject had a low level of this construct and that the individual would then receive a “low” message.
Messages within each level were framed with the goal to improve or make more positive the concept/attitude, and the intention of the messages was to guide rather than force change from a less desirable to a more optimal level.38 Practically, this means that those starting at “low” or “medium” would receive messages intended to guide them toward a higher level of either “medium” or “high.” This approach may include recognizing the challenges of their treatment or condition, acknowledging the frustrations that may be introduced by external pressures, recognizing small victories, or valuing gradual progress. Conversely, subjects starting at “high” would only receive messages that reinforced this level of the intended concept. These messages were framed with maintenance and recognition in mind to keep subjects at the target level. Each message had a singular theme aligned with the corresponding survey item (Table 2). This eased the manner by which subjects may be guided toward more optimal levels of beliefs and self-determination. Two to 3 separate messages per item-level were drafted because of the number of messages required for the study. Consequently, 96 Health Belief Model messages (16 items and 2 levels) and 84 Self-Determination Theory messages (12 items and 3 levels) were created.
Table 2.
Message themes
| Concept | Themes | Example message stems |
|---|---|---|
| Severity |
|
|
| Susceptibility |
|
|
| Barriers |
|
|
| Benefits |
|
|
| Competence |
|
|
| Motivation |
|
|
| Regulation |
|
|
Drafts of the message stems were reviewed by an expert panel of health behavior researchers for readability (appropriate reading level), content (matching of the material to the concept), and tone (matching of the messages to the response level). Suggested revisions centered on appropriately structuring messages that included the subject’s age—to avoid inadvertent stereotyping—as well as simplifying the language to an 8th grade reading level. The study team recognized that the medication-specific messages detailed the benefits of each treatment, and the inclusion of medication tailoring in benefits-based messages was redundant. As a result, only 2 messages per item-level focusing on “perceived benefits” were included in the library. After this review, substantive changes were applied to 55 of the theory-based items. Following these changes, a total of 168 potential, theory-based messages were included in the final library.
Messages were also developed that included tailoring based on diabetes treatment with messages addressing medication efficacy, safety, mechanism of action, and reminders. These messages were crafted for 10 therapeutic classes of medications, including 5 combination products and 3 insulin categories, and did not vary for individual products available in each class; however, combination medications were handled by including information about both therapeutic classes. Separate messages were created for short, intermediate, and long-acting insulin. Based on feedback from focus groups, several messages were drafted that focused on communication with providers, specifically pharmacists, to encourage patients to ask for medication-specific information. Up to 3 messages per category were developed resulting in a total of 128 possible messages; a clinical pharmacist reviewed initial drafts for clarity and accuracy. Two of the 128 potential messages were revised and all messages were deemed appropriate for inclusion in the final library.
Finally, messages were edited to limit their length to approximately 160 characters to allow for the inclusion of the subject’s age, name, and medication names. Such limitations allowed the messages to be properly delivered by a single mobile phone text message.
Message storage
The final library was maintained in a Microsoft Excel spreadsheet, which served as the primary tailoring engine for the larger study. The file was programmed to automatically concatenate the subject’s name with the appropriate message stem after all stems (both medication and theory-based items) were pulled from the library.
Tailoring algorithm
The tailoring algorithm provides the logic to link the messages with survey responses and places them in a pre-determined way that is established by the investigator. Tailored messages for each subject were constructed in a step-wise fashion. First, raw survey information (name, medications, and item responses) was entered into coded worksheets. These responses created coded output that concatenated information based on survey item number and leveling. For instance, a response to the first item indicating “low” competence on the baseline survey would retrieve the appropriately leveled message stem from the library creating a list of the specific theory-based messages for this item (3 in total). This process is then repeated for each survey item until all theory-based messages are created using baseline measures and the message bank is populated for each user. Concurrently, medication codes retrieved all of the medication message stems from the library based on the subject’s reported treatment plan, and all message stems were automatically concatenated with the subject’s name and a randomly selected greeting (e.g. Hello, Hi, Good [morning, afternoon, evening], etc.) Finally, the subject’s age and/or medications were manually imputed to select, randomly determined messages. These additions increase the specificity of the message to the individual, creating a message that is tailored on upwards of 5 characteristics (name, timing, treatment, age, and beliefs). For instance, a subject (Jane) with a baseline competence level of “low” (response equaled “1” or “2”) would receive the following message related to competence: “Hello, Jane. Building confidence in being able to take care of your diabetes takes time. But you make progress every day by following your treatment plan.”
The ordering and delivery of messages was based on several constraints. First, the associated intervention lasted 90 days with participants receiving 1 tailored message per day. This allowed for 78 theory-driven messages for each subject; 12 tailored, medication-specific messages were added in order to total 90 messages.
Second, the leveling of items had to be considered as the delivery of messages was intended to guide subjects from lower to higher levels of the concepts over the 90-day intervention. The system was designed so that subjects would receive 2 Self-Determination Theory messages from their baseline level and 1 message from the next higher level with both sets drawn randomly from the available messages in each level. As an example, a subject with a baseline level of “low” for a competence item would receive 2 messages from the “low” category and then their third message would be from the “medium” category. Subjects whose baseline response was high for any item would receive 3 messages from the “high” category in order to maintain their self-reported level. Messages for subjects beginning at “low” for Health Belief Model items—meaning baseline survey response indicated a limited understanding of or belief in their disease severity or susceptibility—would first receive 2 messages to encourage understanding of these concepts and then change to messages focusing on reinforcement as they progressed through the intervention. Following this approach, subjects who were low for any HBM construct would receive 2 messages from the “low” category and then 1 message from the “high” category. For instance, a subject deemed “high” for an item related to severity may receive a message with the following text: “You know how serious diabetes can be. Taking your medications as directed will help you control this condition and improve your health.”
Finally, as stated earlier, medication messages were incorporated into the algorithm to fill the gap created by the number of theory-driven messages and the 90-day study period. All subjects received the same number of medication-specific messages and these were received on defined days that were identical for each subject; however, the mix of the types of medication messages (efficacy, mechanism of action, and potential side effects) was dependent on the number of medications for each subject. All messages were timed for delivery based on the time of day at which the first dose of any medication was reported to be taken.
The order of messages was pre-determined to alternate between theories and their individual concepts, but an identical scheme for each subject for the order of messages was used (Fig. 3). The final algorithm specified that theory-driven messages alternated between those based on HBM and SDT until all messages were exhausted. Using the baseline level for each item, messages began with the first message for the baseline level of each corresponding item, cycling through the first message, then the second, and (if applicable) the third item.
Fig. 3.
Tailoring process and algorithm.
Once placed in chronological order, message stems were automatically combined with the subject’s name and a randomly assigned greeting. The addition of subject medication and age were completed manually prior to message delivery. Following these steps, the resulting combination of messages was stored in individual worksheets (1 per subject) and formatted to meet the needs for server-based delivery to each subject’s mobile phone.
Discussion
Tailored messaging has become an increasingly used means to encourage health-related behaviors, including medication adherence. Only recently has this approach been modified to communicate with patients by mobile phone text messaging. Building effective messages that are sufficiently tailored and formatted for mobile phone delivery poses unique challenges. A repository of theory-driven messages is vital to the success of mobile phone-based and tailored adherence support services. Applying the library of messages built by the methods described here will contribute both broadly, by adding available messages to the architecture of tailoring, and specifically, by demonstrating how tailored text messages may impact medication adherence.
The applied methods were similar to prior efforts although there were some important differences. Applying “Sweet Talk,” Franklin and colleagues targeted pediatric patients with type 1 diabetes using messages that were informed by Social Cognitive Theory but their approach had a more universal focus on self-management behaviors (e.g. exercise and glucose self-testing) rather than a specific targeting of medication use.36 Moreover, as an intervention targeting children, “Sweet Talk” involved the use of “texting jargon”—the shortening of particular wordsdthat likely improved the resonance of the messages with this younger population.
More recently, Petrie and colleagues focused on improving asthma treatment adherence in young adults.35 The basis for their messages was a validated Illness Perceptions Questionnaire.55 Messages were crafted around each illness perception item in order to change beliefs over the course of the intervention. This was accomplished using responses to the instrument’s 11-point scale; messages were tailored to match baseline patient beliefs for those higher or lower than the mean reported values. However, those within the standard deviation of the mean responses for a particular item did not receive a message tailored for that belief and it was unclear whether these messages were replaced with others. It was also not clear to what extent individual patient characteristics were used in message tailoring. In contrast, our message delivery was designed to reach all participants for all concepts of each theory, regardless of baseline values, so that all elements studied were tailored to and studied.
The current methods have limitations. Both the type and number of messages were limited to 2 health behavior theories and daily delivery, respectively. While evidence suggests that such a “dose” of messages is acceptable to subjects, a truly individualized approach would incorporate patient preferences for the number of messages into the design.35 Moreover, a host of health communication and behavior theories (e.g. Theory of Planned Behavior, Trans-theoretical Model, Regulatory Focus Theory) could apply to the message creation process, particularly expanding on the role of need for cognition as defined by the Elaboration Likelihood Model. Additionally, messages did not consider the effect of present versus future oriented subjects when framing messages from either a loss or gain perspective – a previous study highlighted the impact that this type of framing may have on medication adherence.56 Similarly, messages were drafted without specific subject input to the process and content; future studies should incorporate this step into the message-creation process to improve the specificity and content of each message as well as to increase the use of patient preferences. Also, while the theories applied to the current messages supplied sufficient concepts for tailoring, they may not be comprehensive in addressing all factors that influence medication use. Specifically, the cost of medications was not addressed and the concern for side effects, while acknowledged by our medication-specific messages, was not applied extensively in this study. As previous research has suggested the role that these concerns may play in motivating adherence to medication, future studies involving theory-driven messaging should consider including these issues in the message development process.57
The process described by Kreuter and demonstrated herein is a practical approach to tailoring messages aimed at changing a specific behavior. This study’s methodology applied such an algorithm with the goal of delivering tailored messages by mobile phone – one of the first studies to do so. The result of this integration is a process that similar studies may duplicate so that further theory-driven tailoring of text messages may be applied to improving medication adherence and other health-related behaviors. The current library of messages will be tested in a future study among patients with poorly controlled diabetes. Specifically, this will quantify the impact of tailored text messages on patients’ beliefs regarding diabetes treatment and their disease as well as the impact of the intervention on users’ acceptance of mobile technology and medication adherence.
Acknowledgments
This research was sponsored by an award from the University of Michigan Rackham Graduate School and by grant number HS021976 from AHRQ and the contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of AHRQ. John Piette is a VA Senior Research Career Scientist and received additional support from grants number P30DK092926 and 1-R18-DK-088294-01-A1 from the National Institute of Diabetes and Digestive and Kidney Diseases. The authors wish to thank Benjamin Korman (University of Michigan College of Pharmacy) and Jason Barnum, Pharm.D. (Mercy Health Partners) for their assistance with the focus groups.
Appendix
Tailoring survey instrument items
| Section | Category | Item |
|---|---|---|
| Medication usea | Diabetic regimen | Name of medication |
| Number of pills | ||
| Times taken per day | ||
| Time(s) of day taken | ||
| Health beliefsb | Severity | My diabetes is well controlled. |
| My diabetes would be worse if I did nothing about it. | ||
| I believe that my medications will help prevent complications related to diabetes. |
||
| Diabetes can be a serious disease if you don’t control it. | ||
| Susceptibility | My diabetes is no problem to me as long as I feel alright. | |
| My diabetes will have a bad effect on my future health. | ||
| My diabetes will cause me to be sick a lot. | ||
| I believe I will always need my diabetes medications. | ||
| Benefits | I believe I can control my diabetes. | |
| I believe that my medications will control my diabetes. | ||
| My medicine makes me feel better. | ||
| Barriers | I would have to change too many habits to follow my medications. |
|
| It has been difficult following the medications prescribed for me. |
||
| I cannot understand what the doctor told me about my medications. |
||
| Taking my medications interferes with my normal daily activities. |
||
| Self-determinationc | Competence | I am confident that I can take care of my diabetes. |
| I can handle my diabetes now. | ||
| I can do my own routine diabetes care now. | ||
| I can meet the challenge of controlling my diabetes. | ||
| Motivation | Taking my diabetes medication is very important for being as healthy as possible. |
|
| I personally believe that taking my diabetes medications is the best thing for my health. |
||
| I feel that I want to take responsibility for my own health. | ||
| I have carefully thought about it and believe taking my medications is very important for many aspects of my life. |
||
| Regulation | I feel pressure from others to take my diabetes medications. | |
| Others would be upset with me if I didn’t take my diabetes medications. |
||
| I want others to see that I can take my diabetes medications. | ||
| I want others to approve of me. | ||
| Demographics | Aged | Subject age |
| Gendere | Subject gender | |
| Marital statuse | What best describes your current marital status? | |
| Racee | What race best describes you? | |
| Incomee | Total household income? | |
| Inhabitantsd | With how many people do you currently live? |
Responses were written in by the subjects in the space provided; time of day was indicated among given options.
5-item Likert scale responses, ranging from “Strongly Disagree” to “Strongly Agree.”
7-item Likert scale responses, ranging from “1 (Not at all true)” to “7 (Very true).”
Open-ended response.
Categorical options given.
References
- 1.Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27:S227–S232. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- 2.Petty RE, Cacioppo JT. Epilog: a general framework for understanding attitude change processes. In: Petty, Cacioppo, editors. Attitudes and Persuasion: Classic and Contemporary Approaches. William C. Brown Company; Dubuque, IA: 1981. pp. 255–269. [Google Scholar]
- 3.Petty RE, Cacioppo JT, Strathman AJ, Priester JR. To think or not to think. Exploring two routes to persuasion. In: Shavitt S, Brock TC, editors. Persuasion. Psychological Insights and Perspectives. Allyn and Bacon; Boston: 1994. pp. 113–147. [Google Scholar]
- 4.Strecher VJ. Computer-tailored smoking cessation materials: a review and discussion. Patient Educ Couns. 1999;36:107–117. doi: 10.1016/s0738-3991(98)00128-1. [DOI] [PubMed] [Google Scholar]
- 5.Kreuter MW, Strecher VJ, Glassman B. One size does not fit all: the case for tailoring print materials. Ann Behav Med. 1999;2:276–283. doi: 10.1007/BF02895958. [DOI] [PubMed] [Google Scholar]
- 6.Velicer WF, Prochaska JO, Redding CA. Tailored communications for smoking cessation: past successes and future directions. Drug Alcohol Rev. 2006;25:49–57. doi: 10.1080/09595230500459511. [DOI] [PubMed] [Google Scholar]
- 7.Strecher VJ, Kreuter M, Den Boer D, et al. The effects of computer tailored smoking cessation messages in family practice settings. J Fam Pract. 1994;39:262–270. [PubMed] [Google Scholar]
- 8.Prochaska JO, DiClemente CC, Velicer WF, Rossi JS. Standardized, individualized, interactive, and personalized self-help programs for smoking cessation. Health Psychol. 1993;12:399–405. doi: 10.1037//0278-6133.12.5.399. [DOI] [PubMed] [Google Scholar]
- 9.Bull FC, Kreuter MW, Scharff DP. effects of tailored, personalized, and general materials physical activity. Patient Educ Couns. 1999;36:181–192. doi: 10.1016/s0738-3991(98)00134-7. [DOI] [PubMed] [Google Scholar]
- 10.Kreuter MW, Strecher VJ. Do tailored behavior change messages enhance the effectiveness of health risk appraisal? Results from a randomized trial. Health Educ Res. 1996;1:97–105. doi: 10.1093/her/11.1.97. [DOI] [PubMed] [Google Scholar]
- 11.Prochaska JO, Velicer WF, Redding C, et al. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive mammograms. Prev Med. 2005;41:406–416. doi: 10.1016/j.ypmed.2004.09.050. [DOI] [PubMed] [Google Scholar]
- 12.Brug J, Glanz K, Van Assema P, Kok G, Van Breukelen GJP. The impact of computer-tailored feedback and iterative feedback on fat, fruit, and vegetable consumption. Health Educ Behav. 1998;25:517–531. doi: 10.1177/109019819802500409. [DOI] [PubMed] [Google Scholar]
- 13.Kreuter MW, Skinner CS, Holt CL, et al. Cultural tailoring for mammography and fruit and vegetable intake among low-income African American women in urban public health centers. Prev Med. 2005;41:53–62. doi: 10.1016/j.ypmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Saywell RM, Champion VL, Skinner CS, Menon U, Daggy J. A cost-effectiveness comparison of three tailored interventions to increase mammography screening. J Womens Health. 2004;13:909–918. doi: 10.1089/jwh.2004.13.909. [DOI] [PubMed] [Google Scholar]
- 15.Paul CL, Redman S, Sanson-Fisher RW. A cost-effective approach to the development of printed materials: a randomized controlled trial of three strategies. Health Educ Res. 2004;19:698–706. doi: 10.1093/her/cyg090. [DOI] [PubMed] [Google Scholar]
- 16.Skinner CS, Strecher VJ, Hospers H. Physicians’ recommendations for mammography: do tailored messages make a difference? Am J Public Health. 1994;84:43–49. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization . Adherence to Long-term Therapies: Evidence for Action. Geneva: Switzerland: 2003. [Google Scholar]
- 18.Krueger KP, Berger BA, Felkey B. Medication adherence and persistence: a comprehensive review. Adv Ther. 2005;22:313–356. doi: 10.1007/BF02850081. [DOI] [PubMed] [Google Scholar]
- 19.National Council on Patient Information and Education . Enhancing Prescription Medicine Adherence: A National Action Plan. Bethesda, MD: Aug, 2007. [Google Scholar]
- 20.Bosworth HB, Olsen MK, Neary A, et al. Take Control of Your Blood pressure (TCYB) study: a multifactorial tailored behavioral and educational intervention for achieving blood pressure control. Patient Educ Couns. 2008;70:338–347. doi: 10.1016/j.pec.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hudson TJ, Owen RR, Thrush CR, Armitage TL, Thapa P. Guideline implementation and patient-tailoring strategies to improve medication adherence for schizophrenia. J Clin Psychiatry. 2008;69:74–80. doi: 10.4088/jcp.v69n0110. [DOI] [PubMed] [Google Scholar]
- 22.Johnson SS, Driskell MM, Johnson JL, et al. Transtheoretical model intervention for adherence to lipid-lowering drugs. Dis Manag. 2006;9:102–114. doi: 10.1089/dis.2006.9.102. [DOI] [PubMed] [Google Scholar]
- 23.Janson SL, McGrath KW, Covington JK, Cheng SC, Boushey HA. Individualized asthma self-management improves medication adherence and markers of asthma control. J Allergy Clin Immunol. 2009;123:840–846. doi: 10.1016/j.jaci.2009.01.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lau DT, Nau DP. Oral antihyperglycemic medication nonadherence and subsequent hospitalization among individuals with type 2 diabetes. Diabetes Care. 2004;27:2149–2153. doi: 10.2337/diacare.27.9.2149. [DOI] [PubMed] [Google Scholar]
- 25.Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Lafata JE. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27:2800–2805. doi: 10.2337/diacare.27.12.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 27.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD000011.pub3. CD000011. http://dx.doi.org/10.1002/14651858.CD000011.pub3. [DOI] [PubMed]
- 28.Pew Research Center Americans and Their Cell Phones. 2011 Aug 15; Available at: http://www.pewinternet.org/Reports/2011/Cell-Phones/Key-Findings.aspx.
- 29.Marquez-Contreras E, Figuera von Wichmann M, Guillen V, Figueras M, Balana M, Naval J. effectiveness of an intervention to provide information to patients with hypertension as short text messages of reminders sent to their mobile phone. Aten Primaria. 2004;34:399–405. doi: 10.1016/S0212-6567(04)78922-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cocosila M, Archer N, Haynes RB, Yuan Y. Can wireless text messaging improve adherence to preventive activities? Results of a randomized controlled trial. Int J Med Inform. 2009;78:230–238. doi: 10.1016/j.ijmedinf.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 31.Hou MY, Hurwitz S, Kavanagh E, Fortin J, Goldberg AB. Using daily text-message reminders to improve adherence with oral contraceptives, a randomized controlled trial. Obstet Gynecol. 2010;116:633–640. doi: 10.1097/AOG.0b013e3181eb6b0f. [DOI] [PubMed] [Google Scholar]
- 32.Strandbygaard U, Thomsen SF, Backer V. A daily SMS reminder increases adherence to asthma treatment: a three-month follow-up study. Respir Med. 2010;104:166–171. doi: 10.1016/j.rmed.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 33.Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25:825–834. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vervloet M, van Dijk L, Santen-Reestman J, et al. SMS reminders improve adherence to oral medication in type 2 diabetes patients who are real time electronically monitored. Int J Med Inform. 2012;81:594–604. doi: 10.1016/j.ijmedinf.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 35.Petrie KJ, Perry K, Broadbent E, Weinman J. A text message programme designed to modify patients’ illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psychol. 2012;17:74–84. doi: 10.1111/j.2044-8287.2011.02033.x. [DOI] [PubMed] [Google Scholar]
- 36.Franklin VL, Waller A, Pagliarit C, Greene SA. A randomized controlled trial of sweet talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23:1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 37.Deci EL, Ryan RM. The “what” and “why” of goal pursuits: human needs and self-determination of behaviour. Psychol Inq. 2000;11:227–268. [Google Scholar]
- 38.Deci EL, Ryan RM. Self-Determination Theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 39.Deci EL, Ryan RM. Facilitating optimal motivation and well-being across life’s domains. Can Psychol. 2008;49:14–23. [Google Scholar]
- 40.Williams GC, Patrick H, Niemiec CP, et al. Reducing the health risks of diabetes: how self-determination theory may help improve medication adherence and quality of life. Diabetes Educ. 2009;35:484–492. doi: 10.1177/0145721709333856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Becker MH, Janz NK. The Health Belief Model applied to understanding diabetes regimen compliance. Diabetes Educ. 1985;11:41–47. [Google Scholar]
- 42.Horne R, Weinman J, Hankins M. The beliefs about medications questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14:1–24. [Google Scholar]
- 43.Champion VL, Skinner CS. The Health Belief Model. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4th Jossey-Bass; San Francisco: 2008. [Google Scholar]
- 44.Becker MH, Radius SM, Rosenstock IM, Drachman RH, Schuberth KC, Teets KC. Compliance with a medical regimen for asthma: a test of the Health Belief Model. Public Health Rep. 1978;93:268–277. [PMC free article] [PubMed] [Google Scholar]
- 45.Cerkoney KAB, Hart LK. The relationship between the Health Belief Model and compliance of persons with diabetes mellitus. Diabetes Care. 1980;3:594–598. doi: 10.2337/diacare.3.5.594. [DOI] [PubMed] [Google Scholar]
- 46.Harris R, Skyler JS, Linn MW, Pollack L, Tewksbury D. Relationship between the health belief model and compliance as a basis for intervention in diabetes mellitus. Pediatr Adolesc Endocrinol. 1982;10:123–132. [Google Scholar]
- 47.Ried LD, Christensen DB. A psychosocial perspective in the explanation of patients’ drug-taking behavior. Soc Sci Med. 1988;27(3):277–285. doi: 10.1016/0277-9536(88)90132-3. [DOI] [PubMed] [Google Scholar]
- 48.Morris LS, Schulz RM. Patient compliancedan overview. J Clin Pharm Ther. 1992;17:283–295. doi: 10.1111/j.1365-2710.1992.tb01306.x. [DOI] [PubMed] [Google Scholar]
- 49.DiMatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence. Med Care. 2007;45:521–528. doi: 10.1097/MLR.0b013e318032937e. [DOI] [PubMed] [Google Scholar]
- 50.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21:1644–1651. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 51.Williams GC, Freedman Z, Deci EL. Promoting motivation for diabetics’ self-regulation of HbA1c. Diabetes. 1996;45:13A. [Google Scholar]
- 52.Williams GC, Lynch M, Glasgow RE. Computer-assisted intervention improves patient-centered diabetes care by increasing autonomy support. Health Psychol. 2007;26:728–734. doi: 10.1037/0278-6133.26.6.728. [DOI] [PubMed] [Google Scholar]
- 53.Given CW, Given BA, Gallin RS, Condon JW. Development of scales to measure beliefs of diabetic patients. Res Nurs Health. 1983;6:127–141. doi: 10.1002/nur.4770060306. [DOI] [PubMed] [Google Scholar]
- 54.Hurley AC. The Health Belief Model: evaluation of a diabetes scale. Diabetes Educ. 1990;16:44–48. doi: 10.1177/014572179001600111. [DOI] [PubMed] [Google Scholar]
- 55.Broadbent E, Petrie KJ, Main J, Weinman J. The Brief Illness Perception Questionnaire. J Psychosom Res. 2006;60:631–637. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 56.Zhao X, Villagran MM, Kreps GL, McHorney C. Gain versus loss framing in adherence-promoting communication targeting patients with chronic diseases: the moderating effect of individual time perspective. Health Commun. 2012;27:75–85. doi: 10.1080/10410236.2011.569002. [DOI] [PubMed] [Google Scholar]
- 57.Kreps GL, Villagran MM, Zhao X, et al. Development and validation of motivational messages to improve prescription medication adherence for patients with chronic health problems. Patient Educ Couns. 2011;83:375–381. doi: 10.1016/j.pec.2011.04.029. [DOI] [PubMed] [Google Scholar]