Abstract
Background
Treatment of chondroblastoma in the femoral head is challenging owing to the particular location and its aggressive nature. There is little published information to guide the surgeon regarding the appropriate approach to treating a chondroblastoma in this location. We developed a modified trapdoor procedure to address this issue. The primary modification is that the window surface of the femoral head is covered by the ligamentum teres rather than cartilage as in the traditional procedure.
Questions/purposes
We assessed (1) the clinical presentation of chondroblastoma of the femoral head and treatment results with the modified trapdoor procedure in terms of (2) the frequency of local recurrence, (3) complications, and (4) functional outcomes using the Musculoskeletal Tumor Society (MSTS) score.
Methods
Between 1999 and 2010, we treated 14 patients for chondroblastoma of the femoral head. All patients received the modified trapdoor procedure. Of those, 13 were available for followup at a minimum of 36 months (mean, 66 months; range, 36–117 months) and one patient was lost to followup. There were nine males and four females, with a mean age of 18 years (range, 9–29 years). Clinical features were ascertained by chart and radiographic review, and recurrence, complications, and functional outcomes (MSTS score) were recorded from chart review. Patterns of bone destruction were evaluated using the Lodwick classification, which ranges from IA (geographic appearance with sclerotic rim) to III (permeative appearance).
Results
The symptoms at diagnosis were pain in nine patients and discomfort in four. The mean duration of symptom was 11 months (range, 1–36 months). The physis was open in two patients, closing in one, and closed in 10. The patterns of bone destruction were evaluated as Lodwick Class IA in six patients, Lodwick Class IB in five, and Lodwick Class IC in two. At latest followup, no local recurrence was observed. Two patients had postoperative complications. One had avascular necrosis of the femoral head and was treated with prosthesis replacement. The other had asymptomatic heterotopic ossification in the surgical field. The mean MSTS score was 29.6 (range, 28–30).
Conclusions
Based on this small series, we believe our modified trapdoor procedure is a safe, effective means of treating a chondroblastoma in the femoral head, but additional clinical evaluation with more patients is necessary to confirm our findings.
Level of Evidence
Level IV, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
A chondroblastoma is a rare, benign cartilaginous lesion, accounting for approximately 1% to 2% of all benign bone tumors [3]. It occurs mostly during the second decade of life with a male-to-female ratio of nearly 2:1 [4, 10]. On radiographs, a chondroblastoma typically appears in the epiphysis or apophysis of long bones of the extremities. The most common reported sites include the proximal tibia, proximal femur, distal femur, and proximal humerus [16, 19, 24].
Lesions in the proximal femur arise from the trochanteric area or the femoral head. Those arising from the trochanteric area are relatively easy to access via an extraarticular approach. However, those arising from the epiphysis of the femoral head are difficult to treat owing to the intrinsic challenges of anatomy and exposure. There are three options for the surgical approach as described by Strong et al. [22]. The first is via a bone tunnel through the femoral neck, which potentially could damage the growth plate of the femoral head. Another is via an open window of the femoral neck, which is designed to avoid damaging the growth plate and the articular surface of the femoral head as well, but observation of the whole tumor field is difficult with this approach which is a significant disadvantage. The third is via a direct approach through the surface of the femoral head, which also is known as a trapdoor procedure.
The trapdoor procedure originally was developed by Mont et al. [13] to treat late-stage osteonecrosis of the femoral head. In 2008, Iwai et al. [9] introduced this same procedure to treat one case of chondroblastoma in the femoral head. In 1999, we developed a modified trapdoor procedure to treat chondroblastoma of the femoral head. The primary difference between the modified procedure and the traditional one is how the window surface of the femoral head is covered. The traditional procedure uses the cartilage lid while the modified approach uses the native ligamentum teres. To our knowledge, apart from the initial description of the procedure, no results in patients with femoral head chondroblastoma have been reported using the approach of Iwai et al. [9].
We therefore assessed (1) the clinical presentation of chondroblastoma of the femoral head and treatment results with the modified trapdoor procedure in terms of (2) the frequency of recurrence, (3) complications, and (4) functional outcomes using the Musculoskeletal Tumor Society (MSTS) score.
Patients and Methods
Between 1999 and 2010, we treated 14 patients for chondroblastoma of the femoral head. All patients received treatment using the modified trapdoor procedure. Thirteen of these 14 patients were available for followup at a minimum of 36 months, and represented the study cohort in this retrospective study. One patient lost to followup was excluded.
There were nine male and four female patients. Their mean age at the time of diagnosis was 18 years (range, 9–29 years). No patient had received prior surgical treatment. Diagnosis was histologically confirmed as chondroblastoma in each patient by a pathologist (YD), experienced in musculoskeletal tumors. Patients who had lesions arising from areas other than the femoral head (eg, trochanteric area, femoral neck) were excluded regardless of femoral head involvement. The minimum followup was 36 months (mean, 66 months; range, 36–117 months). This study was approved by the institutional review board of our institution.
Medical records were reviewed for each patient. The interval between the first symptom and the time of diagnosis was identified. Images including plain radiographs, CT scans, and MR images were reviewed for each patient, when available. The developmental status of the epiphysis of the femoral head was identified as open, closing, or closed [24]. Patterns of bone destruction were graded according to the Lodwick classification, as reported by Lehner et al. [11], which ranges from IA (geographic appearance with sclerotic rim) to III (permeative appearance).
The surgical procedure was similar to the technique described by Mont et al. [13] and Iwai et al. [9], but slightly modified. The patient was placed in the supine position with a cushion placed underneath the buttock of the affected limb so that the operative field was elevated. The surgery was performed via an anterior approach to the hip (Smith-Petersen approach). The hip was dislocated anteriorly with the ligamentum teres transected deep in the cotyloid fossa (Fig. 1A). The femoral head was exposed gently with an external rotation force applied to the hip (Fig. 1A). To help preserve the vascular support of the femoral head, the incision size in the anterior capsule should be no larger than is necessary for dislocation of the femoral head. Additionally by avoiding excessive traction and disruptive incisional trauma to the capsule, preservation of the vascular retinacular leash should help to minimize disruption of blood supply. To facilitate localization of the disease process, the anatomic relationship between the ligamentum teres and lesion was identified using preoperative images. Once the head was exposed, a cartilage window was opened near the ligamentum teres, with care to avoid involving the weightbearing region of the head (Fig. 1B). The window was large enough, usually 1 to 1.5 cm in diameter and pointing up, to facilitate full access to the entire tumor and for visual inspection of the defect. With this window, any lesion of the chondroblastoma in the femoral head is fully accessible regardless of the anterior or posterior aspect in the femoral head. Aggressive curettage was done to remove gross visible tumor. Additional mechanical and chemical adjuvants were used. Use of a high-speed burr followed by pulse irrigation and adjuvant phenol was applied to the cavity. The cavity then was filled with bone graft (autograft, allograft, or bone substitute). Autograft harvested from the ilium was used in seven patients, allograft alone in one, and a mixture of allograft and bone substitute in five. Instead of a cartilage trapdoor [9], closure of the defect involved using the native ligamentum teres sutured together to the rim of the residual articular cartilage (Fig. 1C).
Fig. 1A–C.
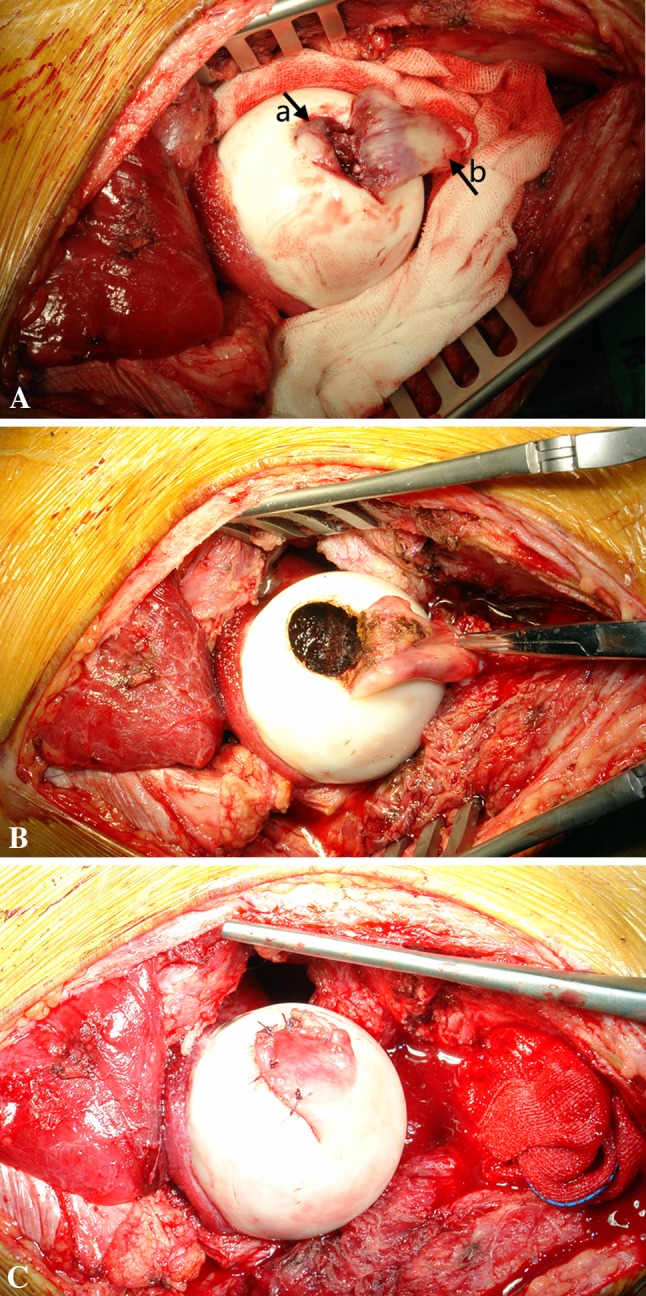
(A) The femoral head is exposed after dislocation. Arrow a indicates where the articular cartilage is breached, which can help locate the tumor but makes coverage with the affected cartilage (trapdoor) impossible. Arrow b indicates the acetabulum end of the ligamentum teres. (B) One window is open near the ligamentum teres, and the entire tumor can be curetted via this window. (C) After bone grafting, the ligamentum teres is sutured together with the cartilage rim of the window cartilage.
Patient activity was encouraged, with early rehabilitation training and continuous passive motion starting on the second postoperative day. Patients were restricted to nonweightbearing activity initially and then allowed partial weightbearing 3 months postoperatively when radiographic evidence (radiographs and CT scans) of graft incorporation was detected. Full weightbearing was allowed usually at 4 to 5 months postoperatively when radiographs indicated full incorporation of the bone graft.
Patients were followed with clinical examination and plain radiographs at 3-month intervals for the first year and then 6-month intervals until 5 years. Functional outcomes were evaluated using the MSTS scoring system [5].
Results
The presenting symptoms were pain in nine patients and discomfort in the hip without other symptoms in four. The mean interval between the onset of symptoms and the time of diagnosis was 11.2 months (range, 1–36 months). Review of radiographs and/or CT scans revealed that the physis was open in two patients, closing in one, and closed in 10 at the time of first diagnosis. There were 10 lesions located in the left femoral head and three involving the right femoral head. The aggressiveness of the lesion was classified as Lodwick Class IA in six patients, IB in five, and IC in two. No pathologic fracture was observed in this group.
At latest followup, no patient had evidence of recurrent disease.
Two patients had postoperative complications. Avascular necrosis of the femoral head was detected 4 months after the index surgery in one patient (Fig. 2). The patient underwent a THA as revision surgery at 7 months after the index surgery because of hip pain. The resected femoral head was histologically confirmed to be recurrence free. The second associated complication was in a patient who had heterotopic ossification develop in the anterior area of the hip (field of surgery) 3 months after surgery. It was considered Class III according to the classification of Brooker et al. for heterotopic ossification [2], defined as the space between the pelvis and the end of the femur as less than 1 cm. The patient was asymptomatic and hip movement was not compromised. No additional surgical intervention was done.
Fig. 2A–C.
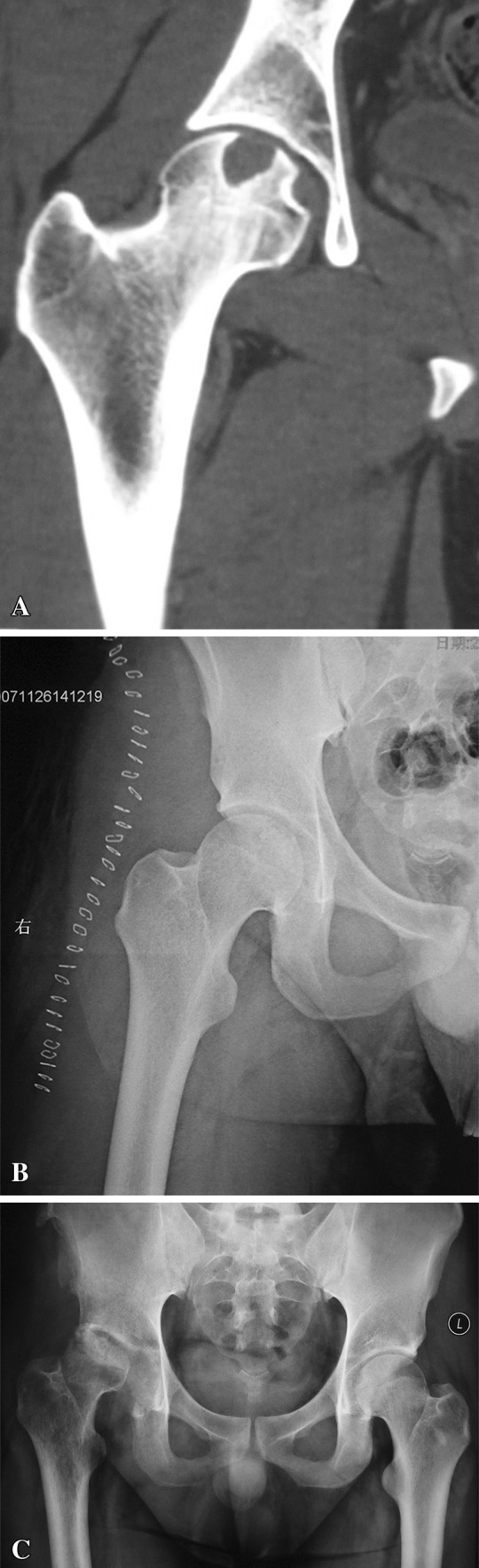
A 20-year-old man had a chondroblastoma of the femoral head treated with our modified trapdoor technique. (A) His coronal CT scan shows a round osteolytic lesion with a thick sclerotic rim. (B) A postoperative radiograph shows the bone defect after curettage is well grafted. (C) The 7-month postoperative radiograph shows the typical appearance of femoral head collapse with signs of osteoarthritic change.
All 13 of the patients recovered fully from the index surgery. No limb-length discrepancy was documented in the two skeletally immature patients. The mean MSTS score was 29.6 (range, 28–30). Ten patients had the highest possible score (30), reflecting the absence of pain or disability.
Discussion
A chondroblastoma is a rare benign, locally aggressive, primary cartilage bone tumor. Those arising from the femoral head are extremely uncommon. Various techniques have been reported for treatment of femoral head chondroblastomas [8, 9, 14, 17, 18, 20–22]. However, to the best of our knowledge, no study with more than five patients treated with one technique has been reported and apart from the initial description of the procedure, no results in patients with femoral head chondroblastoma have been reported using the approach of Iwai et al. since its initial description [9]. We therefore sought to assess (1) the clinical presentation of chondroblastoma of the femoral head and treatment results with the modified trapdoor procedure in terms of (2) the frequency of recurrence, (3) complications, and (4) functional outcomes using the MSTS score.
Our study as several limitations. First, it was a relatively small series of patients with insufficient power to fully assess potentially serious complications such as osteonecrosis, an occurrence that we observed in our small series. Second, as a retrospective study, we have no comparison group to assess how our results might compare with different described approaches. There are other approaches to the femoral head that respect the blood supply to the hip, such as anterior dislocation with a posterior approach proposed by Ganz et al. [7]. This technique was not compared or randomized in our patient population for comparison purposes. Furthermore, this approach can be used in patients only when the lesion is accessible through the fovea. It may not be applicable to all chondroblastomas of the femoral head with extension into the femoral neck. Finally, the small sample size does not allow for definitive comment on potential growth disturbance since most of our patients were close to the end of skeletal growth. The functional assessment we used for this study has not been validated.
The clinical and radiographic presentations of our patients were similar to those reported by Bloem and Mulder [1] and Dahlin and Ivins [4]. All of our patients presented with pain or discomfort and their radiographs showed a geographic bone destruction pattern. However, most of our patients presented with closed physes. Various series of chondroblastomas have reported local recurrences ranging from 8.3% to 32% [12, 16, 19, 23]. Some reports [16, 19] indicated the proximal femur displayed a relatively higher risk of recurrence. Difficulty observing and gaining access to the entire tumor in the femoral head contributes to high local recurrence. In our study, the open window in the femoral head provided a direct view of the tumor and allowed the surgical team unimpeded access to the tumor cavity. This then helped facilitate removal of the entire tumor and coverage of the defect only if it was in the radius of the ligamentum teres. With this technique, no recurrence was observed at a mean followup of 5 years, and we believe that the modified trapdoor technique played a key role in these outcomes. Iwai et al. [9] reported treating one patient with a femoral head chondroblastoma with a trapdoor procedure. The patient showed no recurrence and good hip function at 5 years followup. Givissis et al. [8] treated a patient with a technique similar to that used by Iwai et al. [9], but via a Hardinge approach. The defect was filled with allograft matched for size and shape, which was harvested from a freeze-dried femoral head allograft with round trephines. The patient was free of disease with good function at 2 years followup. Strong et al. [22] reported two different treatment methods in 10 patients. Five patients treated via a direct approach through the femoral neck had no recurrence and achieved full function. The other five patients treated via a canal through the femoral neck had two local recurrences. Riedel et al. [17] and Stilli et al. [21] each reported one patient treated via a similar canal but with fibula graft filling the defect. Sawyer et al. [20] reported one patient treated with fresh osteochondral allograft transplantation, which is suitable for lesions in which the overlying cartilage has been seriously damaged. Most of these studies showed favorable results, but the rarity of these lesions treated with one specific surgical intervention make it difficult to objectively evaluate the effectiveness of the treatment. Two patients reported by Petsas et al. [14] and one by Erickson et al. [6] underwent radiofrequency ablation. Its success proved radiofrequency ablation to be an alternative to surgery in selected patients. However, uncertainty of tumor residue [15] and the need for more than one treatment in many patients [18] necessitate further evaluation of this technique with more patients and long-term followup.
Avascular necrosis of the femoral head is a substantial concern when treating lesions in the femoral head, particularly with this surgical technique. In the current study, although one patient had avascular necrosis of the femoral head develop, potentially owing to premature weightbearing, overall a large incidence of postoperative avascular necrosis was avoided. Bone grafting is believed to help reduce the occurrence of avascular necrosis and related events. To fully access the lesion, dislocation of the femoral head is necessary. Ganz et al. [7] described a method of femoral head dislocation that involves an anterior dislocation of the hip from a posterior approach with a trochanteric flip osteotomy. They suggested this type of surgical dislocation might be safer than others from an avascular necrosis standpoint. However, this approach is not suitable for our patients because of the risk of tumor replantation associated with osteotomy of the greater trochanter plus the potential for increased operative time and blood loss. The anterior approach has been proven to be a safe technique even considering avascular necrosis [4]. One of our patients had heterotopic ossification develop although it was asymptomatic. According to Swiontkowski et al. [24], the anterior approach seems to be associated with a greater risk of heterotopic ossification than the posterior approach.
In some patients who have the traditional approach, the articular cartilage (trapdoor) is thin and disrupted because of compromise by the underlying tumor [8]. It is difficult and sometimes impossible to preserve this cartilage trapdoor. One of the advantages of our approach is that the ligamentum teres is reliable and can easily be sutured to the cartilage to facilitate maintaining a contained defect. The modified trapdoor procedure destroys the foveolar artery by cutting the blood supply from it; however, the femoral head’s vascular flow is supplied mostly from the retinacular vessels. The foveal artery does not contribute as substantially to the blood supply of the femoral head [26]. However it is important to pay attention to the following points when performing this procedure. First, the lateral circumflex femoral artery should be protected during the exposure, especially when opening the joint capsule. Second, the joint dislocation and reduction should be performed gently to avoid unnecessary disturbance of vascular flow and potential physical collapse of the femoral head. The joint capsule should be sutured loosely to reduce hip contracture and facilitate functional recovery.
Owing to the local aggressive nature of chondroblastomas and the particular location of this tumor, the ideal treatment would be complete tumor removal without compromising the patients’ long-term function. Our patients achieved an average of 99% of that expected for normal function based on the observed MSTS functional evaluation score (28–30). No large series have been reported with functional outcomes of chondroblastomas after curettage. Our study is similar to those of Suneja et al. [23] and van der Geest et al. [25]. Although the numbers in this series were small, we believe this modified trapdoor procedure is a safe, effective means of treating chondroblastoma in the femoral head. Attention should be paid to dislocation of the femoral head and postoperative physical rehabilitation to avoid avascular necrosis of the femoral head. Future research will focus on the lesion that involves the femoral neck but extends into the femoral head, which is challenging using the current technique.
Acknowledgments
We thank Yi Ding MD from Department of Pathology, Beijing Ji Shui Tan Hospital, for the pathology review of this series, and YongKun Yang MD, Bin Li MD, Tao Jin MD, and Weifeng Liu MD from Department of Orthopedic Oncology Surgery, Beijing Ji Shui Tan Hospital, for their contributions to data collection.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Lee Moffitt Cancer Center & Research Institute (Tampa, FL, USA) and Beijing Ji Shui Tan Hospital (Beijing, China).
References
- 1.Bloem JL, Mulder JD. Chondroblastoma: a clinical and radiological study of 104 cases. Skeletal Radiol. 1985;14:1–9. doi: 10.1007/BF00361187. [DOI] [PubMed] [Google Scholar]
- 2.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 3.Campanacci M. Bone and Soft Tissue Tumors: Clinical Features, Imaging, Pathology, and Treatment. 2. New York, NY: Springer; 1999. pp. 247–264. [Google Scholar]
- 4.Dahlin DC, Ivins JC. Benign chondroblastoma: a study of 125 cases. Cancer. 1972;30:401–413. doi: 10.1002/1097-0142(197208)30:2<401::AID-CNCR2820300216>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 5.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246. [PubMed] [Google Scholar]
- 6.Erickson JK, Rosenthal DI, Zaleske DJ, Gebhardt MC, Cates JM. Primary treatment of chondroblastoma with percutaneous radio-frequency heat ablation: report of three cases. Radiology. 2001;221:463–468. doi: 10.1148/radiol.2212010262. [DOI] [PubMed] [Google Scholar]
- 7.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 8.Givissis P, Agathangelidis F, Christodoulou E, Christodoulou A. Chondroblastoma of the femoral head disrupting the articular cartilage: description of a novel surgical technique. Acta Orthop Belg. 2012;78:414–417. [PubMed] [Google Scholar]
- 9.Iwai T, Abe S, Miki Y, Tokizaki T, Matsuda K, Wakimoto N, Nakamura S, Imamura T, Matsushita T. A trapdoor procedure for chondroblastoma of the femoral head: a case report. Arch Orthop Trauma Surg. 2008;128:763–767. doi: 10.1007/s00402-007-0490-9. [DOI] [PubMed] [Google Scholar]
- 10.Kurt AM, Unni KK, Sim FH, McLeod RA. Chondroblastoma of bone. Hum Pathol. 1989;20:965–976. doi: 10.1016/0046-8177(89)90268-2. [DOI] [PubMed] [Google Scholar]
- 11.Lehner B, Witte D, Weiss S. Clinical and radiological long-term results after operative treatment of chondroblastoma. Arch Orthop Trauma Surg. 2011;131:45–52. doi: 10.1007/s00402-010-1099-y. [DOI] [PubMed] [Google Scholar]
- 12.Lin PP, Thenappan A, Deavers MT, Lewis VO, Yasko AW. Treatment and prognosis of chondroblastoma. Clin Orthop Relat Res. 2005;438:103–109. doi: 10.1097/01.blo.0000179591.72844.c3. [DOI] [PubMed] [Google Scholar]
- 13.Mont MA, Einhorn TA, Sponseller PD, Hungerford DS. The trapdoor procedure using autogenous cortical and cancellous bone grafts for osteonecrosis of the femoral head. J Bone Joint Surg Br. 1998;80:56–62. doi: 10.1302/0301-620X.80B1.7989. [DOI] [PubMed] [Google Scholar]
- 14.Petsas T, Megas P, Papathanassiou Z. Radiofrequency ablation of two femoral head chondroblastomas. Eur J Radiol. 2007;63:63–67. doi: 10.1016/j.ejrad.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 15.Rajalakshmi P, Srivastava DN, Rastogi S, Julka PK, Bhatnagar S, Gamanagatti S. Bipolar radiofrequency ablation of tibialchondroblastomas: a report of three cases. World J Radiol. 2012;4:335–340. doi: 10.4329/wjr.v4.i7.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramappa AJ, Lee FY, Tang P, Carlson JR, Gebhardt MC, Mankin HJ. Chondroblastoma of bone. J Bone Joint Surg Am. 2000;82:1140–1145. doi: 10.1302/0301-620X.82B8.10791. [DOI] [PubMed] [Google Scholar]
- 17.Riedel B, Franklin C, Seal A, Stevanovic M. Free vascularized fibula graft to treat chondroblastoma of the hip. Orthopedics. 2012;35:e259–e261. doi: 10.3928/01477447-20120123-20. [DOI] [PubMed] [Google Scholar]
- 18.Rybak LD, Rosenthal DI, Wittig JC. Chondroblastoma: radiofrequency ablation—alternative to surgical resection in selected cases. Radiology. 2009;251:599–604. doi: 10.1148/radiol.2512080500. [DOI] [PubMed] [Google Scholar]
- 19.Sailhan F, Chotel F, Parot R, SOFOP Chondroblastoma of bone in a pediatric population. J Bone Joint Surg Am. 2009;91:2159–2168. doi: 10.2106/JBJS.H.00657. [DOI] [PubMed] [Google Scholar]
- 20.Sawyer GA, Heard WM, Terek RM. Fresh osteochondral allograft transplantation for treatment of chondroblastoma of the femoral head: a case report. JBJS Case Connect. 2013;3:e13. doi: 10.2106/JBJS.CC.L.00122. [DOI] [PubMed] [Google Scholar]
- 21.Stilli S, Marchesini Reggiani L, Boriani L, Donzelli O. Osteochondral allograft in a femoral head chondroblastoma: a case report. Hip Int. 2010;20:280–283. doi: 10.1177/112070001002000224. [DOI] [PubMed] [Google Scholar]
- 22.Strong DP, Grimer RJ, Carter SR, Tillman RM, Abudu A. Chondroblastoma of the femoral head: management and outcome. Int Orthop. 2010;34:413–417. doi: 10.1007/s00264-009-0779-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suneja R, Grimer RJ, Belthur M, Jeys L, Carter SR, Tillman RM, Davies AM. Chondroblastoma of bone: long-term results and functional outcome after intralesional curettage. J Bone Joint Surg Br. 2005;87:974–978. doi: 10.1302/0301-620X.87B7.16009. [DOI] [PubMed] [Google Scholar]
- 24.Swiontkowski MF, Thorpe M, Seiler JG, Hansen ST. Operative management of displaced femoral head fractures: case-matched comparison of anterior versus posterior approaches for Pipkin I and Pipkin II fractures. J Orthop Trauma. 1992;6:437–442. doi: 10.1097/00005131-199212000-00008. [DOI] [PubMed] [Google Scholar]
- 25.van der Geest IC, van Noort MP, Schreuder HW, Pruszczynski M, de Rooy JW, Veth RP. The cryosurgical treatment of chondroblastoma of bone: long-term oncologic and functional results. J Surg Oncol. 2007;96:230–234. doi: 10.1002/jso.20804. [DOI] [PubMed] [Google Scholar]
- 26.Zlotorowicz M, Szczodry M, Czubak J, Ciszek B. Anatomy of the medial femoral circumflex artery with respect to the vascularity of the femoral head. J Bone Joint Surg Br. 2011;93:1471–1474. doi: 10.1302/0301-620X.93B11.26993. [DOI] [PubMed] [Google Scholar]


