Abstract
Background
Acetabular fractures are rare injuries in heterogeneous patient groups, making it difficult to develop adequately powered prospective single-center clinical trials in the USA or Europe. Chinese trauma centers treat a high volume of these injuries, and if the patient population and injury patterns are comparable to those in the USA, this might support development of multicenter studies in Level I trauma centers in the two countries.
Questions/purposes
We determined whether the following parameters were similar between operative acetabular fractures treated at Chinese and US trauma centers: (1) epidemiology of injured patients, (2) mechanism of injuries and fracture types, and (3) hospital stay parameters, including symptomatic postoperative deep vein thrombosis (DVT) rate.
Methods
We extracted data from trauma databases for patients admitted with acetabular fractures managed surgically from 2005 to 2012 for one Chinese center and from 2008 to 2012 for one US center. Sex, age, mechanism of injury, fracture classification, Injury Severity Score (ISS), time from injury to surgery, length of hospital stay, and symptomatic DVT rate were analyzed. We included 661 Chinese patients (539 men, 122 women) and 212 US patients (163 men, 49 women).
Results
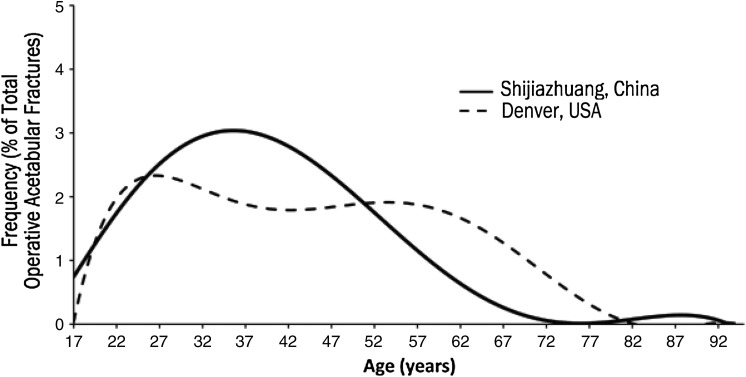
Mean age at time of injury was different between China and the USA, at 40 years with a unimodal distribution and 44 years with a bimodal distribution (p < 0.001), respectively. Incidence of surgically treated acetabular fractures has been increasing in China but decreasing in the USA. Mean ISSs were comparable. Although the distribution of mechanisms of injury was different (p = 0.004), high-energy injuries (motor vehicle accidents, falls > 10 feet) still accounted for most fractures in both centers. Fracture classifications (per Letournel) were comparable, with posterior wall fractures most common. Mean time from injury to surgery and mean hospital stay were longer in China than in the USA (9 versus 3 days [p < 0.001] and 26 versus 11 days [p < 0.001], respectively). Symptomatic DVT rates were comparable.
Conclusions
Although we identified differences between the two centers, we also noted important similarities. Multicenter clinical studies involving these locations should be performed with caution and focus on similar end points, taking into account the populations’ baseline differences. Because of the potential for such differences, this kind of validation study should be performed before embarking on resource-intensive multicenter trials.
Level of Evidence
Level III, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
The incidence of acetabular fractures in the USA and Western Europe has been relatively stable over the years, with 37 pelvic fractures per 100,000 annually and only 10% of these involving the acetabulum [10]. The epidemiology of these fractures in the USA and Europe has been well established, showing comparable bimodal age distributions (ie, the frequency of fractures occurs in two age peaks: the first peak representing young patients sustaining high-energy fractures and the second peak older patients sustaining low-energy osteoporotic/fragility fractures), mechanisms of injury, fracture types, functional outcomes, and conversion rates to THA [4, 11–13]. However, the rate of these fractures is declining in developed countries, leading to a small number of patients with heterogeneous injuries available, which makes it difficult to study these injuries in adequately powered prospective trials.
China is a rapidly growing developing country with a high volume of injuries treated at centralized trauma centers. The care at these centers can vary substantially, and to our knowledge, there are no data comparing these trauma centers to Western industrialized nations. Chinese trauma centers have a high volume of patients, making them ideal candidates to become research partners in the clinical evaluation of treatment strategies and efficacy. However, to engage in large-scale, prospective, multinational clinical trials, proof is needed that the populations, injuries, and treatments are similar enough to be included in multicenter trials.
We therefore determined whether, despite the many differences between the countries and their populations, acetabular fractures encountered in a Level I trauma center in the USA were comparable to those in a similar trauma center in China according to the following parameters: (1) epidemiology of injured patients, (2) mechanisms of injury and fracture types, and (3) hospital stay parameters, including the rate of symptomatic postoperative deep vein thrombosis (DVT).
Patients and Methods
We performed a retrospective review of data obtained from Chinese and US urban Level I trauma centers. Institutional review board and ethics committee approval were obtained for both institutions involved in the study.
Shijiazhuang, China, has a population of 2.24 million and has four similar urban trauma centers with available expertise to manage acetabular fractures. The Third Hospital of Hebei Medical University (HBMU), which participated in our study, is one of these centers. Founded in 1958, HBMU is a major urban trauma center serving a population base of 9.27 million and is a tertiary, university-affiliated teaching hospital located in the southern part of the Hebei province (province population of 71 million). HBMU has 1800 beds, with 180 beds dedicated to orthopaedic trauma. The orthopaedic department consists of 20 surgeons, including 12 fellowship-trained orthopaedic traumatologists (Table 1). The regional trauma referral system in China is managed by a government-run emergency medical system. Similar to the USA, the referrals in China involve stabilization of patients at their local hospitals followed by a transfer to a Level III trauma center (which is equivalent to a Level I trauma center in the USA) for management of complex injuries. Trauma patients are usually divided into three main categories, similar to the US healthcare system: commercially insured, government insured, and self-pay.
Table 1.
Hospital and population comparison between Denver, CO, USA, and Shijiazhuang, China
| Variable | Denver Health Medical Center, USA | Third Hospital of Hebei Medical University, China |
|---|---|---|
| City population | 0.64 million | 2.24 million |
| State population | 5.22 million | 72.41 million |
| Number of trauma centers in the city | 3 (Level I)* | 4 (Level III)* |
| Number of patient beds in hospital | 500 | 1800 |
| Number of orthopaedic trauma patient beds | 40 | 180 |
| Number of orthopaedic traumatologists (fellowship trained) | 4 | 12 |
* The trauma center designation of Level I in the USA is equivalent to Level III in China.
Denver, Colorado, USA, has a population of 640,000 and has three Level I trauma centers. Denver Health Medical Center (DHMC), where our study was performed, is one of these centers. Founded in 1860, DHMC is the busiest trauma center in the state of Colorado. It houses the Rocky Mountain Regional Level I Trauma Center, which serves Colorado and several other neighboring states with a population base of about 6 million. DHMC is a 500-bed, university-affiliated, tertiary referral center and one of the primary teaching hospitals in Denver. The department is staffed with four fellowship-trained orthopaedic traumatologists, three of whom manage acetabular fractures (Table 1).
Data from patients admitted to HBMU and DHMC from January 2005 to December 2012 from and January 2008 to December 2012, respectively, were extracted by querying AO/OTA classifications codes (AO 6.2A, B, and C). Before 2008, the AO/OTA classification was not routinely recorded in the DHMC’s fracture database; therefore, we chose January 2008 as the starting point for our data collection at this center.
We included all adult patients with a diagnosis of acetabular fracture requiring surgical intervention. Patients younger than 18 years and those with nonsurgically treated acetabular fractures were excluded from the study. Two blinded observers (JH, YZ, both orthopaedic traumatologists) verified the AO and Letournel classifications [7, 9] of the fractures coded by the surgeon at the time of the surgery; this was based on AP pelvic radiographs, Judet views, and pelvic CT scans. Our preference for the Letournel classification was driven by its improved reliability, clinical utility, and simplicity when compared to the AO/OTA system [2]. This classification system was used to identify both patterns of injuries and changes in trends during the study period.
We reviewed the medical charts of patients and documented their sex, age, mechanism of injury, Injury Severity Score (ISS), AO and Letournel classifications, time from the injury to definitive management, presence of symptomatic DVT, and their last followup date.
We included 661 patients (539 men, 122 women; in an 8-year period) from China and 212 patients (163 men, 49 women; in a 5-year period) from the USA with acetabular fractures requiring surgery in our analyses. For the purpose of our analysis, all patient charts were considered complete at both institutions.
For our data analysis, we used the chi-square test for categorical data and the unpaired Student’s t-test for parametric data. SPSS® for Windows® (Version 12.0; SPSS, Inc, Chicago, IL, USA) was used for all statistical analyses. We regarded p values of less than 0.05 as significant.
Results
Epidemiology
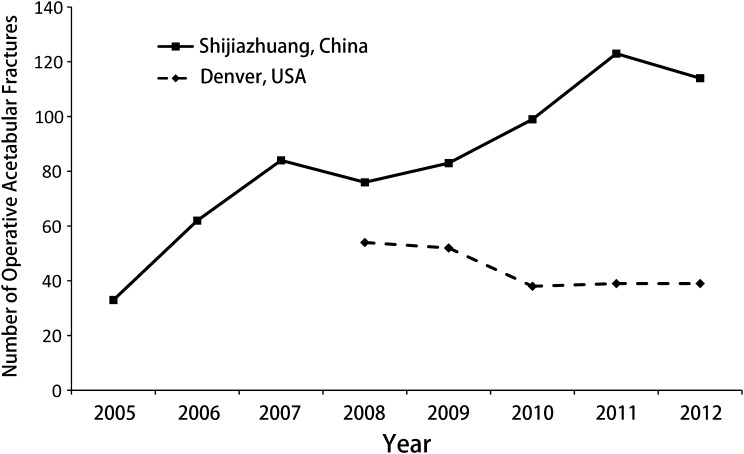
While the epidemiology of acetabular fractures between China and the USA was similar, some important differences were noted. The mean patient age in the Chinese center was 40 ± 13 years (range, 18–90 years), while the mean age in the USA center was 44 ± 16 years (range, 18–90 years) (p < 0.001). In addition, the age distribution curve (histogram/frequency curve) of Chinese patients followed a unimodal distribution, with most fractures occurring in younger patients, while a bimodal distribution was identified in the USA center (Fig. 2). The male-to-female ratio was 3:1 in both countries (Table 2). During the study period, an increase in the incidence of operative acetabular fractures was noted in China (33 fractures in 2005 to 114 fractures in 2012), with a decreasing and then stabilizing incidence in the USA (54 fractures in 2008 to 39 fractures in 2012) (Fig. 1).
Fig. 2.
A graph shows the incidence of operative acetabular fractures in Shijiazhuang, China, from 2005 to 2012 and Denver, CO, USA, from 2008 to 2012.
Table 2.
Comparison of patients with acetabular fractures between Denver, CO, USA, and Shijiazhuang, China
| Variable | Shijiazhuang, China | Denver, CO, USA | p value |
|---|---|---|---|
| Age (years)* | 40 ± 13 | 44 ± 16 | < 0.001 |
| Sex (%) | 0.92 | ||
| Male | 77 | 77 | |
| Female | 23 | 23 | |
| Injury Severity Score (points)* | 12 ± 7 | 12 ± 10 | 0.44 |
| Injury type (%) | 0.004 | ||
| Motor vehicle accident | 54 | 61 | |
| Fall > 10 feet | 20 | 3 | |
| Fall < 10 feet | 12 | 21 | |
| Other (biking, horse riding, skiing) | 14 | 15 | |
| Mean time from injury to surgery (days) | 9 | 3 | < 0.001 |
| Mean length of hospital stay (days) | 26 | 11 | < 0.001 |
| Symptomatic deep vein thrombosis (%) | 3 | 1 | 0.27 |
* Values are expressed as mean ± SD.
Fig. 1.
A line graph, derived from a histogram, shows the age distribution of operative acetabular fractures in Shijiazhuang, China, and Denver, CO, USA, during study period.
Mechanism of Injury and Fracture Types
The mechanisms of injury and fracture types were similar between the two countries, but some differences were highlighted (Table 2). In China, 74% of operative acetabular fractures were caused by high-energy mechanisms (which we defined as falls from a height > 10 feet [3 m] and high- to moderate-speed motor vehicle accidents), with the remaining 26% caused by low-energy mechanisms. Similarly, in the USA, 64% of the fractures were caused by high-energy mechanisms, while 36% were caused by low-energy mechanisms. However, the number of fractures caused by falls of greater than 10 feet was 20% in China compared to 3% in the USA, while fractures caused by falls of less than 10 feet were 12% and 31%, respectively.
The ISS was comparable between the two countries with a mean score of 12 (Table 2), although a trend for increasing mean scores was noted in China from 2005 to 2012 (11 in 2005 to 13 in 2012; p = 0.12). Finally, posterior wall acetabular fractures were the most common type of operative fractures seen in both countries, accounting for 30% in China and 32% in the USA, followed by both column fractures (21% and 17%, respectively) (Table 3). There was no change in the distribution by fracture type noted over the study period.
Table 3.
Comparison of acetabular fracture classification between Denver, CO, USA, and Shijizhuang, China
| Fracture classification | Percentage of patients | |
|---|---|---|
| Denver, CO, USA | Shijizhuang, China | |
| Posterior wall | 32 | 30 |
| Posterior column | 1 | 2 |
| Anterior wall | 1 | 1 |
| Anterior column | 8 | 6 |
| Transverse | 6 | 5 |
| T-shaped | 4 | 4 |
| Posterior column/posterior wall | 3 | 4 |
| Transverse posterior wall | 14 | 10 |
| Anterior column/posterior hemitransverse | 5 | 4 |
| Both columns | 17 | 21 |
| Not classified | 9 | 13 |
| Total | 100 | 100 |
Hospital Parameters
Our results highlighted several important differences between the two countries with regard to two of the hospital parameters analyzed (Table 2). The mean time from injury to surgery was longer in the Chinese center than in the US center (9 days versus 3 days, respectively; p < 0.001). Similarly, the mean inpatient stay was longer in the Chinese center than in the US center (26 days versus 12 days, respectively; p < 0.001). The rates of symptomatic DVT were similar in the two centers (3% in the Chinese center versus 0.9% in the US center; p = 0.27).
Discussion
Given that the number of acetabular fractures in developed/industrialized countries is low and possibly decreasing, large multicenter clinical trials will become necessary if prospective research is to be performed. For many reasons, international cooperation on musculoskeletal research is essential. In addition, China has a large population base and its referral trauma centers see large patient volumes, which makes establishing collaboration with a large Chinese trauma center (such as HBMU) the next logical step. However, before expending resources on prospective multicenter trials, it is important to characterize the different sites to establish in what ways they are comparable and in what ways they are different. Therefore, our aim was to characterize the epidemiology of acetabular fractures in two large metropolitan areas by comparing one large trauma center in the USA with a similar trauma center in China. To our knowledge, this is the first paper of its kind to both establish benchmark data for the characteristics of acetabular fractures treated surgically in China and compare these data with a similar trauma center in the USA.
Our study does have notable weaknesses, though, and these merit careful consideration. The choice to analyze two different study periods between the USA and China (5-year period versus 8-year period, respectively) was driven by the quality of data collection (or lack thereof) at each center before the chosen start dates. In 2005, HBMU adopted a new electronic medical record system that made retrospective review of data a feasible option, where prior studies only included patients from individual surgeons. Similarly at DHMC, before 2008, the AO/OTA fracture classification codes were not routinely recorded in our database, which is why we used 2008 as our starting point to avoid any additional selection bias (ie, only certain fracture types or surgeons cases being selected). We believe that the number of acetabular fractures analyzed over the study period is sufficient to be representative and comparable to the data from a set taken 5 years before. More concerning is the selection bias inherent to most epidemiologic study of this kind. First, we only included acetabular fractures that were treated surgically. Nonsurgically managed fractures are not recorded in either fracture database. Another concern is that surgical indications for acetabular fractures in China may have changed (toward a more aggressive approach) over the study period and created an apparent increase in the number of operative acetabular fracture cases. Furthermore, the decision to operate on one injury over the other may have been influenced by training, culture, and, at the time, insurance status in China. We realize that the above variables may more frequently influence the decision making in one center than the other and could represent a bias in our data analysis. However, both senior authors from the USA (CM, WS) have visited this Chinese trauma center (HBMU) on several occasions and have spent time in the clinic, in the operating room, and at fracture conferences and believe that the indications there are comparable to those used in US trauma centers, such as DHMC. More studies are needed focusing specifically on these poorly quantifiable factors to tease out how these nuances affect management. Likewise, the baseline populations differ between the two countries (ie, height, weight, activity level, BMI, etc), but since surgical and functional outcomes were outside the scope of our study, we did not include these data. Finally, the use of symptomatic DVT as an end point may represent another limitation of our work. Since the symptoms of a DVT can vary widely, its diagnosis may be subject to interpretation.
Our results suggest that the epidemiologic characteristics of the two countries are in many ways comparable, opening the door to a number of opportunities for international collaboration involving multicenter research studies on acetabular fracture. In fact, the male-to-female ratio, fracture types, ISSs, and most common mechanisms of injury were comparable between the two centers. However, some differences have been highlighted by our research, for example, mean patient age and its distribution curve, time from injury to surgery, length of hospital stay, and distribution of injury mechanisms.
The lower mean age of patients with operative acetabular fractures in China and their unimodal age distribution when compared to the higher mean age and bimodal age distribution of US patients may be related to a less active, nondriving generation of osteoporotic patients in China.
Of note, there was a noticeable increase in the incidence of surgically treated acetabular fractures during our study period (2005 to 2012) in China, while our data and most papers from Europe and the USA quote a constant incidence [1, 3, 8]. This change in China may be due to the growing number of cars per capita, a booming economy with a significant development of the construction industry, and a migration from the countryside to the cities. Additionally, it may be attributed to improved prehospital care and increased survival of severely injured patients [5]. China’s urbanization as described in TheNew York Times [6] (migration of > 250 million people from rural areas to towns and cities within the next decade) may have a significant impact on the epidemiology of trauma in the country.
Based on our findings, we recommend that clinical trials involving China and the USA adjust their methodology to account for similarities and differences highlighted by our study. For clinical studies on acetabular fractures, exclusion of patients located in the late age peak of the bimodal curve (those older 60 years) should be considered. Based on the differences in the mechanisms of injury highlighted by our study, we would suggest focusing on high-energy acetabular fractures, bypassing the differences observed in the incidence of acetabular fractures in the older osteoporotic patients. Studies looking at outcomes may need to standardize the surgical indications between the two centers and acknowledge the significant differences between the time from injury to surgery and the duration of inpatient stay between the two countries. As the Chinese population ages and becomes more urbanized, we anticipate that the epidemiology of acetabular fractures will mirror the trends of the USA, including a reduction in the number of fractures caused by high-energy trauma, an increase in fractures caused by low-energy mechanisms, a bimodal age distribution, and an increase in the mean age of injured patients.
China is the most populous country in the world. The ongoing economic development in China has brought about a concomitant increase in pelvic and acetabular fractures associated with automobile use and industrialization. Declining trauma volumes in countries, such as the USA and those in Western Europe, present challenges in terms of prospectively evaluating the efficacy of orthopaedic trauma care. Our study on acetabular fractures highlighted many similarities and some key differences between the USA and China. We believe multicenter clinical trials involving centers in the USA and China will help us answer clinically relevant questions that underpowered single-center trials may not be able to elucidate. However, those should be performed with caution with a methodology that takes into account the key similarities and differences in epidemiology, injury types, and hospital parameters between the centers involved.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This study was carried out at Denver Health & Hospital Authority (Denver, CO, USA) and The Third Hospital of Hebei Medical University (Shijiazhuang, People’s Republic of China).
References
- 1.al-Qahtani S, O’Connor G. Acetabular fractures before and after the introduction of seatbelt legislation. Can J Surg. 1996;39:317–320. [PMC free article] [PubMed]
- 2.Beaule PE, Dorey FJ, Matta JM. Letournel classification for acetabular fractures: assessment of interobserver and intraobserver reliability. J Bone Joint Surg Am. 2003;85:1704–1709. [PubMed] [Google Scholar]
- 3.Davarinos N, Ellanti P, Morris S, Mc Elwain JP. Epidemiology of pelvic and acetabular trauma in a Dublin tertiary hospital: a 10-year experience. Ir J Med Sci. 2012;181:243–246. doi: 10.1007/s11845-011-0791-4. [DOI] [PubMed] [Google Scholar]
- 4.Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010;92:250–257. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 5.Gui L, Gu S, Lu F, Zhou B, Zhang L. Prehospital emergency care in Shanghai: present and future. J Emerg Med. 2012;43:1132–1137. doi: 10.1016/j.jemermed.2012.02.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson I. China embarking on vast program of urbanization. The New York Times. June 16, 2013.
- 7.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646. [PubMed] [Google Scholar]
- 8.Laird A, Keating JF. Acetabular fractures: a 16-year prospective epidemiological study. J Bone Joint Surg Br. 2005;87:969–973. doi: 10.1302/0301-620X.87B7.16017. [DOI] [PubMed] [Google Scholar]
- 9.Letournel E. Fractures of the acetabulum: a study of a series of 75 cases—Les fractures du cotyle, etude d’une serie de 75 cas. J de Chirurgie 82:47–87, 1961. (Translated and substantially abridged). J Orthop Trauma. 2006;20(1 suppl):S15–S19. [PubMed]
- 10.Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003;407:173–186. doi: 10.1097/00003086-200302000-00026. [DOI] [PubMed] [Google Scholar]
- 11.Ochs BG, Marintschev I, Hoyer H, Rolauffs B, Culemann U, Pohlemann T, Stuby FM. Changes in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU) Injury. 2010;41:839–851. doi: 10.1016/j.injury.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 12.O’Neill F, Leonard M, Lui D, McElwain J, Morris S. Pelvic and acetabular fractures. Ir Med J. 2012;105:306. [PubMed] [Google Scholar]
- 13.Tibbs BM, Kopar P, Dente CJ, Rozycki GS, Feliciano DV. Acetabular and isolated pelvic ring fractures: a comparison of initial assessment and outcome. Am Surg. 2008;74:538–541; discussion 541. [PubMed]