Abstract
Background
Compelled by the psychosocial implications of short stature, patients with short stature are increasingly undergoing distraction osteogenesis for cosmetic limb lengthening. To the degree that this is true, evaluation of the risks and benefits of this treatment are very important, but to date, there are few studies reporting on using distraction osteogenesis for this indication.
Questions/purposes
We reviewed a group of patients undergoing cosmetic lower-extremity lengthening in terms of (1) soft tissue challenges, (2) bone-related complications, and (3) functional and subjective clinical outcomes.
Methods
The study was retrospective by reviewing data from medical records and radiographs. Between 1983 and 2006, we treated 138 somatically normal patients with bilateral lower-limb distraction osteogenesis for cosmetic purposes at our center using an Ilizarov external fixator, of whom 131 (95%; 65 males, 66 females) had complete clinical and radiographic data a minimum of 1 year after treatment (mean, 6 years; range, 1–14 years) and were reviewed for this report. The mean age of these patients was 25 years (range, 14–68 years) and their mean preoperative height was 159 cm (range, 130–174 cm). One hundred twenty-four (95%) patients had lengthening of the tibia alone, of which 66 (53%) were monofocal and 58 (47%) were bifocal. Six patients (4.58%) had crossed contralateral lengthening of the femur and tibia and one patient (0.76%) had bilateral lengthening of the femur. The mean height gained was 6.9 cm (range, 2–13 cm), 7.3 cm (range, 3.5–13 cm) in males and 6.5 cm (range, 2–13 cm) in females. The mean lengthening, maturation, and external fixator indexes were 12 days/cm (range, 4.3–24 days/cm), 19 days/cm (range, 5.2–63 days/cm), and 31 days/cm (range, 12–78 days/cm), respectively.
Results
Forty-eight patients (37%) had 59 complications related to treatment. Thirty-seven were soft tissue related (28%), of which 17 (46%) needed reinterventions, and 22 were bone related (17%), of which 16 (73%) needed reinterventions. At final followup, the outcome was excellent for 72 patients (55%), good for 52 (40%), satisfactory for six (4.58%), and poor for one (0.77%). One hundred thirty of 131 patients subjectively felt satisfied and had improved self-esteem.
Conclusions
Distraction osteogenesis using the Ilizarov external fixator is an option for carefully selected motivated patients with awareness of this technique. Soft tissue and bone-related complications including those that necessitate reinterventions should be expected during the course of treatment, although most can be managed without permanent sequelae or disability. Future studies with more robust methods will need to determine whether the risks and benefits of this procedure are well balanced. Preoperative counseling, considering the ethical questions this procedure can raise, is of paramount importance for the patient to weigh the risk versus anticipated benefits. Studies from other centers will be important as we move forward.
Level of Evidence
Level IV, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
Distraction osteogenesis using the circular external fixator of Ilizarov [13–16] is an accepted and time-tested modality of limb lengthening in patients with limb length discrepancy [3, 5, 7, 9], short stature, particularly achondroplasia [2, 8, 17] and bone defects [1]. The same technique is being used to increase the height of somatically normal persons who report negative feelings regarding their short stature [2, 6, 11, 20] deriving from cosmetic, social, and occupational concerns.
Short stature can have serious psychologic and social implications [22] and the number of patients undergoing cosmetic limb lengthening has increased [23]. However, this technique is not without concerns and controversies [12, 23], particularly in, only one study has been published regarding benefits and safety of cosmetic limb lengthening [6].
We therefore reviewed a group of patients undergoing cosmetic lower extremity lengthening in terms of (1) soft tissue challenges, (2) bone-related complications, and (3) functional and subjective clinical outcomes.
Patients and Methods
We retrospectively reviewed a consecutive series of 138 somatically normal patients with a negative feeling of short stature who underwent bilateral symmetric lower limb lengthening between January 1983 and December 2006. The indications for surgery were (1) the presence of a clear reason to undergo limb lengthening, (2) strong motivation, and (3) consented to undergo the procedure after complete awareness of the nature of surgery, possible complications, and the rehabilitation program. The contraindications to surgery were (1) the presence of psychologic disorders like dysmorphophobia, (2) associated endocrine disorders like hypothyroidism, (3) the presence of systemic illnesses related to growth and development like renal insufficiency, and (4) the presence of dysplastic syndromes like multiple epiphyseal dysplasia. After approval of our institutional review board, all patients who had a minimum followup of 1 year (mean, 6 years; range, 1–14 years) after removal of the fixator were included in the study. Seven patients were excluded as they did not have the required followup. Thus medical records, radiographs, and clinical photographs were available for 131 patients (95%; 65 males, 66 females).
The mean age of the patients at presentation was 25 years (range, 14–68 years), 28 years (range, 14–68 years) for males and 23 years (range, 14–45 years) for females (Table 1). The mean preoperative height was 159 cm (range, 130–174 cm), 162 cm (range, 143–174 cm) in males and 156 cm (range, 130–174 cm) in females. The reasons for limb lengthening were variable: students unable to keep up with their peers, requirements of individual sports such as volleyball, water polo, basketball, and tennis, vocation requirements, and issues with interpersonal relationships. Nine patients (six males, three females) had a mild varus deformity (5°–7°) of the proximal tibia that needed simultaneous correction. One hundred twenty-four of the 131 patients (95%) had tibial lengthening alone, 66 (53%) had monofocal lengthening and 58 (47%) had bifocal lengthening. Ninety-two patients (74%) preferred bilateral surgery on the same day; 32 (26%) had the surgeries performed with a gap of 4 weeks. One patient (0.76%) preferred simultaneous bilateral lengthening of the femur. In the other six patients (4.58%), crossed contralateral lengthening of the femur and tibia was done with a gap of 4 weeks. All six patients who had crossed tibial and femoral lengthening had more than 10 cm lengthening. They were concerned about the thigh leg proportion and therefore this option was selected. One patient had bilateral distal femur lengthening per his preference since he had disproportionate lower limbs with a longer leg segment and shorter thigh segment.
Table 1.
Age distribution of the patient cohort
| Age group | Number of patients |
|---|---|
| Younger than 20 years | 32 |
| 20–29 years | 70 |
| 30–39 years | 21 |
| 40–49 years | 7 |
| 50 years or older | 1 |
| Total | 131 |
We ascertained the height and trunk-limb proportions through standard anthropometric measurements. AP and lateral views of both lower limbs and a standing scanogram from the pelvis to the heel were done to assess length, deformity, limb length discrepancy, and any focal bone disorder. Consent for treatment was obtained after complete psychologic assessment by a psychologist and comprehensive counseling regarding the treatment and rehabilitation. Particular attention was given to rule out systemic illnesses, hormonal imbalances, dystrophic syndromes, and psychologic issues such as dysmorphophobia [21]. The patient and family were counseled on more than one occasion, and motivation to proceed with treatment was ensured.
We believe that optimum lengthening of the lower limb can be done only up to 5 to 7 cm, beyond which outcome may be suboptimal in view of cosmesis (trunk-limb proportions) [4, 19], altered biomechanics, and soft tissue function [10]. Therefore, most lengthenings were planned only for the tibial segment, bilaterally simultaneously, either monofocally (< 5 cm) or bifocally (> 5 cm to reduce the duration of fixator [18]). However, for patients who wanted more lengthening, we planned additional lengthening of the femoral segment. For the tibia, we used the standard three-ring construct for monofocal and bifocal lengthenings, with more wires for bifocal lengthening. The tibial corticotomy was below the tibial tuberosity for monofocal lengthening and also at the supramalleolar level for bifocal lengthening. A fibular osteotomy was done at the junction of the middle and distal thirds. Bifocal tibial corticotomies were accompanied by two level fibular osteotomies during the 1980s and 1990s. Later the proximal fibular osteotomy was avoided as it was found to be unnecessary and posed the possibility of injury to the common peroneal nerve. The femur was lengthened at the supracondylar level using an assembly consisting of two rings and a single arch with wires distally and half pins proximally.
Distraction started on the seventh postoperative day. Monofocal lengthening was commenced at a rate of 0.75 to 1 mm/day over three to four fractions and gradually increased to 1 to 1.5 mm/day over four to six fractions as guided by clinicoradiographic assessment of new bone formation. We observed that the rate could be increased slightly more than 1 mm/day for teenagers and could be maintained only at less than 1 mm/day for patients in the older age categories. The rate for bifocal distraction was 1.25 to 1.5 mm/day per bone over three to four fractions, with distraction at one site being greater than at the other site in the beginning. Distraction gradually become equal, and then gradually reversed toward the end of distraction.
ROM exercises of the joints (as much as the fixator allowed) and weightbearing walking with use of axillary crutches were encouraged as much as tolerated from the second postoperative day. All patients were monitored as inpatients until removal of the fixator. Radiographs were taken every 2 weeks to assess the quality of regenerate, lengthening, and occurrence of any deformity. After gaining sufficient length by distraction, the fixators were left in place for the necessary time to allow consolidation of the regenerate. The decision to remove the fixator was based on a satisfactory stress test after removing the connecting rods and satisfactory consolidation observed on the radiographs as evidenced by complete bone bridging in at least two projections. After fixator removal, the patients wore a cast extending from the thigh to the supramalleolar region for 2 to 4 weeks as determined during stress testing at the time of fixator removal. We did not use a removable orthosis for any patient because of unavailability.
We looked for the incidence of pin tract and soft tissue infections, common peroneal neuropathy, and assessment of knee and ankle ROM during and after external fixation to assess for soft tissue complications. For bone-related complications we watched for the incidence of osteomyelitis during treatment, and did clinicoradiologic monitoring for knee and ankle congruity to rule out any subluxations, speed of regeneration, incidence of any deformity, or fracture of regenerate during and after external fixation. We recorded how each of these challenges was approached or treated and the final outcome. We also recorded all technical challenges and how they were managed.
The patients were followed up every 3 months for 1 year and then yearly thereafter. Assessment was for patient satisfaction, axial deviation, ROM of the joints, foot and ankle deformities, limb length discrepancy, infection, pain, and functional status. A physician-based outcome score developed by one of us (KIN) was used to assess outcome: excellent = planned increase in the length of limb segments achieved with good preservation of body proportions and function in the absence of deformity and joint stiffness; good = planned extension of the limbs achieved against trunk-limb proportions, or partial restriction of limb function, in the form of abnormal gait, 3° to 5° axial deviation, or 5° to 10° limitation of joint movement; satisfactory = lengthening of limbs achieved up to 75% of the planned value or presence of 5° to 10° axial deviation or 10° to 15° limitation of joint movement; and unsatisfactory = lengthening achieved to less than 75% of the planned value or presence of axial deviation greater than 10° or limitation of joint movement greater than 15°.
Patient-based outcomes were measured in terms of patient satisfaction and improvement of self-esteem. Patient-related outcome was measured by asking the patient at the completion of treatment whether they were satisfied (yes/no), whether the procedure led to improvement of their self-esteem (yes/no), whether they would undergo the procedure again (yes/no), and whether they would recommend it to someone with subjective feelings of short stature (yes/no).
All patients were available for followup at a minimum of 1 year (mean, 5.75 years; range, 1–14 years). The mean height gained was 6.9 cm (range, 2–13 cm); 7.3 cm (range, 3.5–13 cm) in males and 6.5 cm (range, 2–13 cm) in females. The associated bilateral proximal tibial varus in nine patients was corrected. The mean duration of distraction and maintenance phases were 79 days (range, 17–168 days) and 116 days (range, 31–301 days), respectively. The mean duration of fixator wear was 215 days (range, 71–390 days). The mean lengthening index was 12 days/cm (range, 4.3–24 days/cm), the mean maturation index was 19 days/cm (range, 5.2–63 days/cm), and the mean external fixator index was 31 days/cm (range, 12–78 days/cm).
Results
There were 37 soft tissue complications (28%) of which 17 (46%) needed reinterventions. The soft tissue complications were significant pin tract infections (n = 5; 3.82%), common peroneal neuropathy (n = 6; 4.58%), equinus of the ankle (n = 12; 9.16%), and fixed flexion deformity of the knee (n = 14; 11%). Other than minor pin tract infections treated with dressings, antibiotics, and removal of wires without affecting fixator stability, major infection that needed changes of wires with the patient under anesthesia occurred in five patients (3.82%). The infections were controlled. Common peroneal neuropathy occurred in six patients (4.58%) while undergoing distraction and was treated by reducing the amount of distraction, physiotherapy, and pharmacologic supplementation (intramuscular injection of neurotropic medications such as prozerin or galantamine and vitamins B1, B6, and B12 for 10 to 14 days). All but one patient (despite exploration and neurolysis) achieved complete recovery. Twelve patients (9.16%) had equinus deformity while wearing the fixator. Ten of these patients had bilateral equinus deformities, and nine of these patients were treated by extending the frame to the foot and gradual stretching of the tendoachilles, with additional percutaneous lengthening in one patient. One patient had tendoachilles lengthening alone followed by bracing and physiotherapy. Two patients refused any surgery and underwent physiotherapy and prolonged bracing. Four patients had only 20° ankle dorsiflexion at final followup. Fourteen patients (11%) had a fixed flexion deformity of the knee between 10° to 40° at various stages of treatment. Physiotherapy, exercises, and splinting helped in all but two patients. One of these patients had successful correction with Ilizarov distraction and the other had a residual deformity of 15°.
There were 22 (17%) bone-related complications of which 16 (73%) needed reinterventions. These complications were technical issues (n = 2; 1.53%; one incomplete corticotomy of the tibia that needed osteoclasis, and premature fibular consolidation requiring reosteotomy with the patient under anesthesia), osteomyelitis (n = 3; 2.29%), delayed regeneration (n = 6; 4.58%), deformity of the regenerate while wearing the fixator (n = 5; 3.82%), deformity of the regenerate after removal of the fixator (n = 4; 3.05%), subluxation of the knee (n = 1; 0.76%), and late fracture through the regenerated bone (n = 1; 0.76%). Pin tract infection progressed to deep infection in three patients (2.29%) and needed exploration, débridement, removal of sequestrum, and exchange of wires. None of these infections progressed to a chronic infection. Poor regeneration occurred in six patients (4.58%), and two of these patients had crossed oblique olive wires applied through the regenerate to stimulate osteogenesis. Consolidation occurred in the other four by expectant management and continued rehabilitation. None of these patients experienced nonunion. Four patients had substantial deformities of the tibial regenerate develop while they were wearing the fixator (varus of the proximal tibia [n = 1], valgus-recurvatum of the proximal tibia [n = 1], varus of the distal tibia [n = 2]) that needed correction and realignment with the patients under anesthesia. Another patient had his femoral fixator realigned twice for deformity of the regenerate. Four patients had deformities develop after removal of the fixator (valgus-recurvatum of the proximal tibia [n = 3], varus of the proximal tibia [n = 1]), two of whom had a corrective cast applied and two had reapplication of the fixator. None of the patients had residual deformity greater than 5°. One patient had lateral subluxation of the knee during distraction, which was reduced by modifying the fixator. One patient had delayed posttraumatic fracture through the new bone region 1 year after fixator removal and was treated successfully with Ilizarov osteosynthesis.
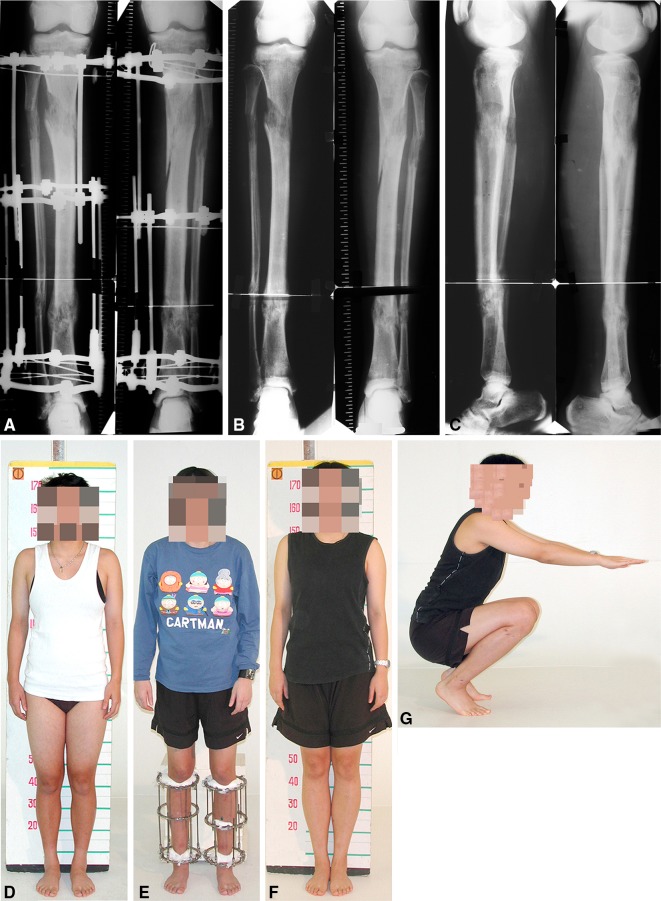
On the basis of the established criteria, treatment outcome was excellent in 72 patients (55%) (Fig. 1), good in 52 (40%), satisfactory in six (4.58%), and poor in one (0.77). One patient discontinued lengthening after achieving 2 cm because of her concerns regarding the prolonged duration of treatment. At completion of treatment, all but this last patient stated on our questionnaire that they were satisfied with the outcome of treatment, felt improvement of self-esteem, they would undergo the procedure again, and they would recommend it to another person having short stature.
Fig. 1A–G.
A 16-year-old patient had bilateral lower-limb lengthenings using the Ilizarov external fixator. (A) A radiograph shows the patient’s limbs while wearing the Ilizarov fixator for bifocal lengthening of the tibia by 6.5 cm. (B) AP and (C) lateral views show the patient’s limbs after removal of the fixator. Clinical photographs show the patient (D) before, (E) during, and (F) after lengthening. (G) Functional outcome after removal of the external fixator is shown.
Discussion
We performed this study to evaluate the risk and benefits of cosmetic limb lengthening in terms of soft tissue and bone complications and functional and subjective clinical outcomes. Forty-eight patients (37%) experienced 59 complications and seven patients (5.34%) had more than one complication. There were 37 (28%) soft tissue complications and 22 (17%) bone-related complications during treatment. Twenty-three patients (18%) needed reoperations and residual problems occurred in six patients (4.58%); four patients had limitation of ankle dorsiflexion, one had a flexion deformity of the knee, and one had common peroneal palsy (Table 2).
Table 2.
Complications
| Complications | Number of occurrences | Residual deficits |
|---|---|---|
| Soft tissue | ||
| Pin tract infection needing intervention | 5 | None |
| Common peroneal neuropathy | 6 | Did not resolve in one patient |
| Ankle equinus | 12 | Four patients had restricted dorsiflexion |
| Flexion deformity of the knee | 14 | 15° deformity persisted in one patient |
| Bone-related | ||
| Technical issues | 2 | None |
| Osteomyelitis | 3 | None |
| Delayed consolidation of regenerate | 6 | None |
| Deformity of regenerate while on fixator | 5 | None |
| Deformity of regenerate after removal of fixator | 4 | None |
| Knee subluxation | 1 | None |
| Delayed fracture through regenerated bone | 1 | None |
This study has numerous limitations. First, this is a retrospective study of available medical records. We did not assess the patients directly. Seven patients were excluded owing to lack of required followup; this potentially could have biased the results. Some of these operations were performed before validated tools were used for outcome assessment. The physician-based and patient-based outcome scores that we used are unvalidated and because the surgeries were performed in the 1980s and 1990s, there was no way to use the outcome measures currently being used. The result also could have been influenced by bias of assessment as the surgeons documented the postoperative assessment of their own work, regardless whether it was physician-related or patient-related outcomes. All these factors could have exaggerated our results. There is a chance of selection bias as surgery was offered only to patients who were thought to be ideal candidates for this procedure. Proper patient selection is of paramount importance with this procedure which is a prolonged and arduous treatment modality. Despite proper patient selection, our experience with this technique, and the facilities for rigorous in-patient physiotherapy and rehabilitation, there were numerous challenges to overcome to ensure optimum results. We believe that extreme caution should be exercised in using this technique for cosmetic lengthening. Only studies from other institutes can clarify whether our results are replicable elsewhere. The patients came to us for various reasons (cosmetic, occupational, and social), and we do not have data regarding numerical gain in height translated as fulfilment of these objectives.
We recognize that performing surgery of this magnitude for cosmetic or avocational purposes (such as sport) is extremely controversial. Our institute has extensive experience with limb lengthening and many of our patients are from various parts of the world who come to us for cosmetic limb lengthening. These patients attend many counseling sessions with a psychologist and surgeon to determine whether they need this surgery. They are made fully aware of the nature of the treatment and the possible complications. Wherever possible nonsurgical solutions are offered and discussed. Many patients have changed their mind after these sessions and chose not to undergo the surgery. Some patients were rejected because of the psychologist’s recommendation as they showed features of dysmorphophobia or histrionic traits. Other patients persist, although their reasons may lack sense to us. Some patients, despite being rejected for surgery, have repeatedly requested we reconsider, and some to whom surgery was refused have gone to other centers with less experience with this technique and have returned to us for treatment of their complications. Therefore, in some cases, even when the patients were not rejected by the psychologists, we went beyond numerical values of height and the medical logic for cosmetic lengthening after ensuring motivation and compliance of the patients. Some patients have unrealistic expectations regarding the extent of lengthening and the counseling sessions have helped them to align their expectations with realistic levels. However, when the patients wanted to achieve the maximum possible lengthening, we obliged but with precautions and close monitoring to avoid complications. As an example, one of our patients was an intensely motivated 68-year-old man who could have 3.5 cm lengthening without significant complications despite concerns of bone regeneration owing to his age. The cost of this treatment is not covered by any medical insurance or public health system.
To our knowledge, the only published study of cosmetic bilateral lower limb lengthening was by Catagni et al. [6], who reviewed 54 patients with constitutional short stature in whom a mean length of 7 cm was gained. Twenty of their 54 (37%) patients had equinus of the ankle develop. Whereas we used extension of the Ilizarov apparatus to the ankle and gradual stretching with limited use of percutaneous tendoachilles lengthening, Catagni et al. performed tendoachilles lengthening in 19 of their patients (one patient refused surgery). Twenty-five of their 54 patients (46%) had pin tract infections that needed intervention. In our series, even though the incidence of pin tract infection requiring interventions was lower, we had deep infections requiring sequestrectomy, which was not seen by Catagni et al. This may be attributable to differences in pin tract care protocols.
Two patients in the series of Catagni et al. had delayed consolidation of regenerate in which autologous bone graft was used. We did not need to use bone graft in any of our patients. In two of our patients with unsatisfactory progress of consolidation after 3 months of the maturation phase, we applied two crossed olive wires across the regenerate from proximal to distal connected to the apparatus through slotted, threaded rods in gentle traction which is thought to stimulate maturation. Catagni et al. also reported deformity of the regenerate after fixator removal in three patients and which they corrected with reapplication of the Ilizarov frame. We tried using plaster casts for correction and reapplied the fixator only if the correction was unsatisfactory. Catagni et al. reported one patient had a limb length discrepancy greater than 1 cm whereas none of our patients had a length discrepancy. They also reported minor complications with eight patients having axial deviation less than 5°, five patients with subtalar stiffness, and two patients with limited ankle dorsiflexion.
Catagni et al. reported that all their patients felt satisfaction, improvement in self-esteem, distress, shyness, and quality of life, although they also did not seem to have used any validated score. Their functional outcome score was based on patient satisfaction, axial deviation, ROM, pronation of the foot, leg length discrepancy, and scarring, and they reported an excellent outcome in 49 patients (91%) and good outcome in five (9%).
Distraction osteogenesis using the Ilizarov external fixator is an option for carefully selected patients with short stature motivated to have an increase of height. The patients must be made aware of the nature of the technique and all possible complications. Many soft tissue and bone-related complications including those that necessitate reinterventions should be expected during the course of treatment, and patients must be monitored and followed up carefully. Most of these challenges can be managed without much permanent sequelae and disability. Future studies with more robust methods and rigorous statistical analysis will need to determine whether the risks and benefits of this procedure are well balanced and establish safe limits of cosmetic lengthening. In all situations of cosmetic limb lengthening, the surgeon must counsel the patient - keeping in mind the ethical issues the surgery can raise - to critically examine whether it is worth taking such risks for the anticipated benefit. The surgeon must always keep the safety of the patient the main priority over the numerical values of height gained. Our center is dedicated to the Ilizarov technique, therefore studies from other centers will be important as we move forward with this technique.
Acknowledgments
We thank Irina A. Saranskih MA, International Department, Russian Ilizarov Scientific Centre for Restorative Traumatology and Orthopaedics, for facilitating the study by translating relevant information between Russian and English.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Russian Ilizarov Scientific Centre for “Restorative Traumatology and Orthopaedics,” Kurgan, Russia.
References
- 1.Abdel-Aal AM. Ilizarov bone transport for massive tibial bone defects. Orthopedics. 2006;29:70–74. doi: 10.3928/01477447-20060101-10. [DOI] [PubMed] [Google Scholar]
- 2.Aldegheri R. Dall’Oca C. Limb lengthening in short stature patients. J Pediatr Orthop B. 2001;10:238–247. [PubMed] [Google Scholar]
- 3.Aston WJ, Calder PR, Baker D, Hartley J, Hill RA. Lengthening of the congenital short femur using the Ilizarov technique: a single-surgeon series. J Bone Joint Surg Br. 2009;91:962–967. doi: 10.1302/0301-620X.91B7.21304. [DOI] [PubMed] [Google Scholar]
- 4.Bogin B, Varela-Silva MI. Leg length, body proportion and health: a review with a note on beauty. Int J Environ Res Public Health. 2010;7:1047–1075. doi: 10.3390/ijerph7031047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burnei G, Vlad C, Gavriliu S, Georgescu I, Hodorogea D, Pârvan A, Burnei C, El Nayef T, Drăghici I. Upper and lower limb length equalization: diagnosis, limb lengthening and curtailment, epiphysiodesis. Rom J Intern Med. 2012;50:43–59. [PubMed] [Google Scholar]
- 6.Catagni MA, Lovisetti L, Guerreschi F, Combi A, Ottaviani Cosmetic bilateral leg lengthening: experience of 54 cases. J Bone Joint Surg Br. 2005;87:1402–1405. doi: 10.1302/0301-620X.87B10.16468. [DOI] [PubMed] [Google Scholar]
- 7.Catagni MA, Radwan M, Lovisetti L, Guerreschi F, Elmoghazy NA. Limb lengthening and deformity correction by the Ilizarov technique in type III fibular hemimelia: an alternative to amputation. Clin Orthop Relat Res. 2011;469:1175–1180. doi: 10.1007/s11999-010-1635-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cattaneo R, Villa A, Catagni MA, Tentori L. Limb lengthening in achondroplasia by Ilizarov’s method. Int Orthop. 1988;12:173–179. doi: 10.1007/BF00547160. [DOI] [PubMed] [Google Scholar]
- 9.Courvoisier A, Sailhan F, Thevenin-Lemoine C, Vialle R, Damsin J. Congenital tibial deficiencies: treatment using the Ilizarov’s external fixator. Orthop Traumatol Surg Res. 2009;95:431–436. doi: 10.1016/j.otsr.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 10.Emara KM, Diab RA, El Ghazali S, Farouk A, El Kersh MA. Foot and ankle function after tibial overlengthening. J Foot Ankle Surg. 2014;53:12–15. doi: 10.1053/j.jfas.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Emara K, Farouk A, Diab R. Ilizarov technique of lengthening and then nailing for height increase. J Orthop Surg (Hong Kong). 2011;19:204–208. doi: 10.1177/230949901101900215. [DOI] [PubMed] [Google Scholar]
- 12.Gross RH. Limb lengthening for stature: another view. J Pediatr Orthop. 2005;25:128–129. doi: 10.1097/00004694-200501000-00027. [DOI] [PubMed] [Google Scholar]
- 13.Gubin AV, Borzunov DY, Malkova TA. The Ilizarov paradigm: thirty years with the Ilizarov method, current concerns and future research. Int Orthop. 2013;37:1533–1539. doi: 10.1007/s00264-013-1935-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238:249–281. [PubMed] [Google Scholar]
- 15.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;239:263–285. [PubMed] [Google Scholar]
- 16.Ilizarov GA. The tension stress effect on the genesis and growth of tissues. The influence of blood supply and loading upon the shape-forming processes in bone and joints. In: Green SA, ed. The Transosseous Osteosynthesis: Theoretical and Clinical Aspects of the Regeneration and Growth of Tissue. Berlin, Germany: Springer; 1992.137–257.
- 17.Kim SJ, Balce GC, Agashe MV, Song SH, Song HR. Is bilateral lower limb lengthening appropriate for achondroplasia? Midterm analysis of the complications and quality of life. Clin Orthop Relat Res. 2012;470:616–621. doi: 10.1007/s11999-011-1983-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maffulli N, Lombari C, Matarazzo L, Nele U, Pagnotta G, Fixsen JA. A review of 240 patients undergoing distraction osteogenesis for congenital post-traumatic or post-infective lower limb length discrepancy. J Am Coll Surg. 1996;182:394–402. [PubMed] [Google Scholar]
- 19.Motoc A, Motoc M, Bolintineanu S, Musori C, Munteanu M. The construction of body: from model to reality. Rom J Morphol Embryol. 2005;46:63–66. [PubMed] [Google Scholar]
- 20.Park HW, Yang KH, Lee KS, Joo SY, Kwak YH, Kim HW. Tibial lengthening over an intramedullary nail with use of the Ilizarov external fixator for idiopathic short stature. J Bone Joint Surg Am. 2008;90:1970–1978. doi: 10.2106/JBJS.G.00897. [DOI] [PubMed] [Google Scholar]
- 21.Phillips KA. Body dysmorphic disorder and depression: theoretical considerations and treatment strategies. Psychiatr Q. 1999;70:313–331. doi: 10.1023/A:1022090200057. [DOI] [PubMed] [Google Scholar]
- 22.Sandberg DE. Short stature: psychosocial interventions. Horm Res Paediatr. 2011;76(suppl 3):29–32. doi: 10.1159/000330151. [DOI] [PubMed] [Google Scholar]
- 23.Stanitski CL. Limb lengthening for stature. J Pediatr Orthop. 2004;24:593–594. doi: 10.1097/01241398-200409000-00024. [DOI] [PubMed] [Google Scholar]