Abstract
Background
Acetabular fracture diagnosis is traditionally made with AP and oblique pelvic plain radiographs. Obesity may impair diagnostic accuracy of plain radiographs. New CT reconstruction algorithms allow for simulated radiographs that may eliminate the adverse imaging effects of obesity.
Questions/purposes
In obese patients with acetabular fractures, we compared CT-generated and plain radiographs in terms of (1) ability to classify fracture type, (2) agreement in fracture classification, and (3) surgeon performance at different experience levels.
Methods
CT-generated and plain radiograph image sets were created for 16 obese (BMI > 35) patients with 17 acetabular fractures presenting from 2009 to 2011. Three orthopaedic trauma attending physicians, three senior residents, and three junior residents independently viewed these sets and recorded their diagnoses. These diagnoses were compared to the postoperative findings, which we defined as the gold standard for diagnosis. To assess intraobserver reliability, the same observers reviewed a rerandomized set 1 month later. We had 80% power to detect a 25% difference in the percentage of correctly classified fractures based on a post hoc sample size calculation and 80% power to detect a 0.10 difference in κ value based on both a priori and post hoc sample size calculations.
Results
With the numbers available (153 observations in each image set, 51 for each of the three observer groups), we found no differences between CT-generated and plain radiographs, respectively, in terms of percentage of correct diagnoses for the observer groups (all observers: 54% versus 49%, p = 0.48; attendings: 61% versus 59%, p = 0.83; senior residents: 51% versus 53%, p = 0.84; and junior residents: 49% versus 35%, p = 0.16). Furthermore, agreement between CT-generated and plain radiographic fracture classifications was substantial (κ = 0.67). Nonetheless, the attending and senior resident groups performed better in correctly classifying the fracture than the junior residents when using plain radiographs (p = 0.01 and p = 0.049, respectively). Performance was not different when comparing the attendings to the senior resident and junior groups or comparing the senior residents to the junior residents using CT-generated radiographs (p = 0.32, p = 0.22, and p = 0.83, respectively).
Conclusions
CT-generated radiographs are as good as plain radiographs for experienced surgeons for classifying acetabular fractures in obese patients. CT-generated imaging may be valuable in both teaching and clinical settings, and it may spare the patient additional radiation exposure and discomfort.
Level of Evidence
Level II, diagnostic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
Fractures of the acetabulum constitute approximately 10% of pelvic fractures [4]. They occur most commonly in young adults secondary to motor vehicle collisions or other high-energy trauma with a reported incidence of approximately three per 100,000 person years [8]. Accurate diagnosis is imperative, as it will dictate treatment, weightbearing status, and long-term clinical hip function of the patient [10]. Typically, two oblique Judet views (the obturator oblique and iliac oblique) are combined with the standard AP pelvic view to classify the fracture pattern [6, 10]. The Letournel classification system, adopted by the AO and the Orthopaedic Trauma Association, utilizes the information from these three views to classify acetabular fractures into 10 distinct patterns [10, 12]. This method has been shown to be reliable for acetabular fracture classification [1].
However, plain radiographs are subject to factors such as obesity that can impair diagnostic accuracy [2, 13, 17, 19]. Obesity is a worsening epidemic in the United States, affecting 35.7% of the population [3]. The WHO classifies obesity in three classes by BMI [22]: A BMI of greater than 30 but less than 35 is Obesity Class I; a BMI of 35 and greater but less than 40 is Obesity Class II; and a BMI of 40 or greater is Obesity Class III. Class II and III obesity are commonly referred to as morbid obesity [21]. In addition, patient positioning for radiographic imaging can become challenging, often resulting in multiple attempts as the technologist tries to correctly center the image on the pelvis [19]. Furthermore, obesity is associated with increased soft tissue apposition that may obscure subtle fracture lines making fracture classification more difficult [17].
Recent CT advancements allow the creation of two-dimensional images that approximate AP and Judet plain radiograph views, using the CT data obtained as part of the standard trauma evaluation [7, 13]. These CT-generated radiographs may obviate the need for plain radiograph Judet views, allow for more accurate and timely diagnosis and preoperative planning, and decrease the radiation burden to the patient [2, 15, 16]. We wondered whether they would help improve diagnostic accuracy compared to plain radiographs in a population of patients with obesity who present with acetabulum fractures.
We therefore compared CT-generated and plain radiographs in a population of obese patients with acetabular fractures in terms of (1) the ability to classify fracture type, (2) the agreement in fracture classification, and (3) surgeon performance at different experience levels.
Patients and Methods
After obtaining institutional review board approval, we retrospectively reviewed a database of all patients with trauma presenting to our Level 1 trauma center from June 2009 to July 2011. There were 21 patients with a diagnosis of acetabular fracture and identified as having a BMI of greater than 35. Five patients were excluded for not having the required surgical intervention, leaving 16 patients with 17 total fractures. The mean age at presentation was 41 years (range, 21–66 years). Twelve patients were women, and four were men.
Images obtained on presentation to the emergency department were used for this study. All CT scans were obtained as part of the patients’ routine trauma evaluation using a Siemens Somatom® 40 detector CT (Siemens AG, Berlin, Germany) with 1- to 3-mm section cuts. For this study, two image sets were created for each patient: AP and two Judet oblique plain radiographs (Image Set A, Fig. 1) and AP and two Judet oblique CT-generated radiographs (Image Set B, Fig. 2). The CT-generated radiographs were created by radiology technicians using a standardized computer workstation and software (Syngo MMWP; Siemens AG). A total of 34 image sets were created for evaluation. All images had the patient identifiers removed. These 34 image sets were randomized using a computerized random number generator (Microsoft® Office Excel® 2003; Microsoft Corp, Redmond, WA, USA). The image sets were then randomly arranged in an alternating plain radiograph and CT-generated radiograph order. The images were transferred from Synapse® picture archiving and communication system (FUJIFILM Medical Systems USA, Inc, Stamford, CT, USA) and presented to the study group as a Microsoft® PowerPoint® (Microsoft Corp) presentation.
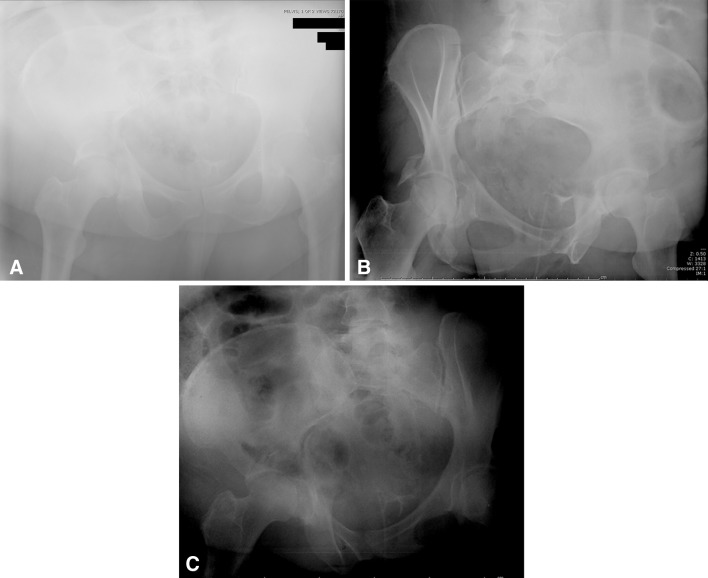
Fig. 1A–C.
Plain radiographic (A) AP, (B) obturator oblique, and (C) iliac oblique views show an acetabular fracture in a patient with Class II obesity.
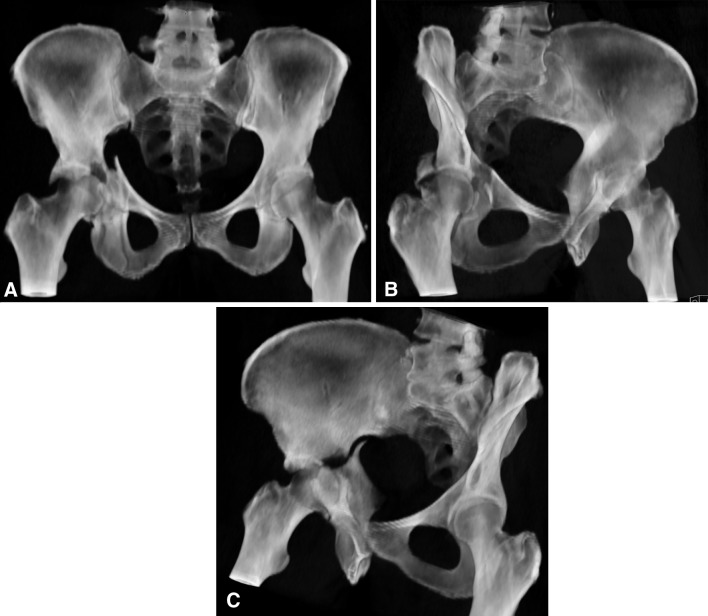
Fig. 2A–C.
CT-generated radiographic (A) AP, (B) obturator oblique, and (C) iliac oblique views show the acetabular fracture in the same patient as in Figure 1.
Three observer groups were created for comparison based on level of training, including an attending level (three fellowship-trained orthopaedic traumatologists), a senior resident level (three Postgraduate Year 4 and 5 residents), and a junior resident level (three Postgraduate Year 2 and 3 residents). The method for classifying the fractures was reviewed with each observer [11]. Each observer reviewed the 34 image sets and the diagnosis was recorded by each observer as one of the 10 types of acetabular fractures of the Letournel classification system: anterior wall, anterior column, posterior wall, posterior column, transverse, anterior column or wall plus posterior hemitransverse, posterior column plus posterior wall, transverse plus posterior wall, T-shaped, and both column [1, 10]. In this way, 51 total diagnoses (17 fractures × three observers) were produced per observer group (with 153 total observations) for each plain radiograph and CT-generated radiograph image set. These image sets were rerandomized and reviewed for a second time after a minimum 1-month washout period to assess intraobserver reliability. The first observer review of the image sets was used for all other statistical analyses. The gold standard diagnosis was determined by the treating surgeon, who was not a member of the study group and used all available imaging studies (including the two-dimensional CT data) and the findings at the time of surgical intervention (Table 1).
Table 1.
Gold standard* fracture type
| Fracture type | Number of fractures (n = 17) |
|---|---|
| Anterior wall | 0 |
| Anterior column | 0 |
| Posterior wall | 5 |
| Posterior column | 0 |
| Transverse | 1 |
| Anterior column or wall plus posterior hemitransverse | 4 |
| Posterior column plus posterior wall | 2 |
| Transverse plus posterior wall | 3 |
| T-shaped | 1 |
| Both column | 1 |
* As determined by the treating surgeon (see text).
Agreement between each of the two imaging methods and the gold standard diagnosis among observer groups and intraobserver agreements were evaluated with kappa statistics. The κ values were interpreted by using the guidelines of Landis and Koch [9], in which 0 to 0.20 indicates poor agreement, 0.21 to 0.40 fair agreement, 0.41 to 0.60 moderate agreement, 0.61 to 0.80 substantial agreement, and greater than 0.80 almost perfect agreement. Proportional probability statistics (Z-scores) were used to evaluate differences in observer performance using CT-generated and plain radiographs. Differences with a p value of less than 0.05 were considered significant. Analysis was performed on a commercially available statistical package (SPSS® Statistics for Windows®, Version 20.0; IBM Corp, Armonk, NY, USA).
Estimate for kappa (2c2) requires only two subjects to look at one method at a time (in this study, CT-generated radiographs or plain radiographs) and eight subjects to look at both methods [14]. An a priori analysis sample size calculation indicated that our planned 51 observations in each of three observer groups would produce sufficient power at 80% to detect a difference between plain and CT-generated radiographs in terms of interobserver agreement in diagnosis. A post hoc statistical power calculation was performed; with the data spread we observed, we had 80% power to detect a κ value difference of 0.10 [20]. Although somewhat study specific, a κ value difference of 0.10 is recommended as the smallest difference to be tested [20]. In addition, a post hoc sample size calculation indicated we had 80% power to detect a 25% difference in the percentage of correctly classified fractures, with alpha set at 0.05 [5].
Results
Overall and within each experience level, with the numbers available, there was no difference in ability to correctly classify acetabular fracture type by CT-generated radiographs as compared to plain radiographs (all observers: 54% versus 49%, p = 0.48; attendings: 61% versus 59%, p = 0.83; senior residents: 51% versus 53%, p = 0.84; and junior residents: 49% versus 35%, p = 0.16) (Table 2). Furthermore, overall intraobserver reliability was substantial with both CT-generated radiographs (κ = 0.70; 95% CI: 0.58, 0.82) and plain radiographs (κ = 0.65; 95% CI: 0.41, 0.89) (Table 2). In addition, intraobserver reliability was substantial or better with both CT-generated and plain radiographs for the attending and senior resident groups (Table 2). For the junior resident group, intraobserver reliability was substantial with the CT-generated radiographs (κ = 0.69; 95% CI: 0.49, 0.89) but only moderate with plain radiographs (κ = 0.41; 95% CI: 0.17, 0.65).
Table 2.
Intraobserver agreements of two evaluating methods and their diagnostic accuracy before surgical interventions
| Experience level group | Agreement with gold standard (number of observations) | Intraobserver agreement (κ value) (95% CI) | |||
|---|---|---|---|---|---|
| CT-generated radiographs | Plain radiographs | p value | CT-generated radiographs | Plain radiographs | |
| All observers | 82/153 (54%) | 75/153 (49%) | 0.48 | 0.70 (0.58, 0.82) | 0.65 (0.41, 0.89) |
| Trauma attendings | 31/51 (61%) | 30/51 (59%) | 0.83 | 0.76 (0.62, 0.90) | 0.61 (0.39, 0.83) |
| Senior residents | 26/51 (51%) | 27/51 (53%) | 0.84 | 0.65 (0.44, 0.86) | 0.92 (0.81, 1.0) |
| Junior residents | 25/51 (49%) | 18/51 (35%) | 0.16 | 0.69 (0.49, 0.89) | 0.41 (0.17, 0.65) |
Agreement between CT-generated and plain radiographic fracture classifications was substantial overall (κ = 0.67; 95% CI: 0.55, 0.79) (Table 3). However, we found differences by experience level. Agreement between findings on CT-generated and plain radiographs was substantial among attendings (κ = 0.80; 95% CI: 0.63, 0.97) and senior residents (κ = 0.72; 95% CI: 0.53, 0.91) but only moderate among junior residents (κ = 0.48; 95% CI: 0.26, 0.72) (Table 3). Furthermore, the agreement between attending surgeons and residents increased when CT-generated radiographs were used (Table 3). Attending surgeons and senior residents demonstrated substantial agreement when CT-generated radiographs were used (κ = 0.65; 95% CI: 0.43, 0.87) but only moderate agreement for plain radiographs (κ = 0.56; 95% CI: 0.33, 0.79). Attendings and junior residents showed moderate agreement with CT-generated radiographs (κ = 0.53; 95% CI: 0.30, 0.76) but only fair agreement for plain radiographs (κ = 0.40; 95% CI: 0.18, 0.62). When comparing the resident groups, senior residents and junior residents showed substantial agreement when using CT-generated radiographs (κ = 0.73; 95% CI: 0.54, 0.92) but only fair agreement when using plain radiographs (κ = 0.35; 95% CI: 0.11, 0.59).
Table 3.
Agreement between CT-generated and plain radiographs according to experience level and experience level agreement with trauma attendings
| Experience level | Agreement between CT-generated and plain radiographs (κ value) (95% CI) | Agreement with trauma attending (κ value) (95% CI) | |
|---|---|---|---|
| CT-generated radiographs | Plain radiographs | ||
| All observers | 0.67 (0.55, 0.79) | ||
| Trauma attendings | 0.80 (0.63, 0.97) | ||
| Senior residents | 0.72 (0.53, 0.91) | 0.65 (0.43, 0.87) | 0.56 (0.33, 0.79) |
| Junior residents | 0.48 (0.26, 0.72) | 0.53 (0.30, 0.76) | 0.40 (0.18, 0.62) |
Attendings and senior residents performed better than junior residents when using plain radiographs, but performance was not different among the groups when using CT-generated images (Table 4). Although performance among experience levels when using plain or CT-generated radiographs, as compared to the gold standard, generally improved as the level of experience increased, performance improvement reached statistical significance only for the evaluation of the plain radiographs (Tables 2, 4). Attending physicians were better at reading plain radiographic views than junior residents (p = 0.01). Senior residents were also better at reading plain radiographs than junior residents (p = 0.049). There was no difference in performance among the experience levels when reading the CT-generated radiographs (Table 4).
Table 4.
Performance comparison between experience levels using proportional probability
| Experience level group | Proportional probability (Z-score) | |
|---|---|---|
| CT-generated radiographs | Plain radiographs | |
| Trauma attendings versus senior residents | 1.00 (p = 0.32) | 0.55 (p = 0.58) |
| Trauma attendings versus junior residents | 1.22 (p = 0.22) | 2.55 (p = 0.01) |
| Senior versus junior residents | 0.22 (p = 0.83) | 1.95 (p = 0.049) |
Discussion
While the current standard recommendations in the care of acetabular fractures include the use of three plain radiograph views of the pelvis (AP, iliac oblique, and obturator oblique), there are a number of factors that can limit their effectiveness in the trauma setting [2]. These factors include overlying gas patterns, patient discomfort, associated injuries, and obesity [2, 13, 17, 19]. Since the initial description of this method of assessment, there have been advances in imaging techniques that may allow for accurate imagining without the above-mentioned limitations [2, 7, 19]. Two-dimensional CT of the pelvis is part of the routine trauma workup at trauma centers and permits quick imaging of the pelvis without placing the patient in oblique positions. CT reconstruction algorithms have been developed that can create simulated radiographs while subtracting bladder contrast material, gas patterns, and soft tissue [2, 7, 16]. However, to our knowledge, CT-generated radiographs have not been evaluated against plain radiographs to determine whether they improve the clinician’s ability to make a diagnosis in obese patients. We therefore compared CT-generated and plain radiographs in a population of obese patients with acetabular fractures in terms of (1) the ability to classify fracture type, (2) the agreement in fracture classification, and (3) surgeon performance at different experience levels.
There are a number of limitations to this study. First, the retrospective nature of our patient selection does not allow for prospective standardization of the radiographic methods. However, all of the radiology technicians at our institution see a high volume of patients with acetabular fractures and are well trained. Because of the clinical volume and the experience of these technicians, these images most likely also represent a best-case scenario of what can be obtained in an orthopaedic practice. Second, the CT images were subject to the pelvic CT protocol in place at the time that the patient was treated and vary from 1 to 3 mm in thickness. However, our study demonstrates that, despite not having a specific set protocol, radiographs generated from routinely acquired CTs functionally are not different from plain radiographs. In addition, the apparent overall low percentage of correct interpretations (Table 2) could be viewed as a study limitation. However, the performance of our attending traumatologists was similar to previously reported rates when plain radiographs are used in isolation from axial CTs [16]. Our accuracy rate of 59% was similar to the 52% reported by O’Toole et al. [16] using plain radiographs alone. Similarly, our accuracy rate of 61% was similar to the 68% reported by O’Toole et al. [16] using CT-generated radiographs. These radiographs were used in isolation from axial CT images and intraoperative findings that would no doubt aid the treating surgeon in correctly diagnosing the acetabular fracture pattern.
Another limitation is our sample size of 153 total observations for each image set divided among three observer groups. Both a priori and post hoc statistical analyses substantiated sufficient power for all level of agreement (κ) calculations. However, post hoc analysis revealed that our accuracy calculations required a 25% difference in the percentage of correctly classified fractures to produce 80% power with alpha set at 0.05. Therefore, this study is underpowered to detect relatively small observed differences. This limitation may not be material to interpreting the results, however, as we observed less variability in the raw percent correct data for CT-generated radiographs (range, 49%–61%) versus plain radiographs (range, 35%–59%). Furthermore, for the findings not attaining statistical significance, the raw numbers, if anything, point to better diagnostic accuracy using the CT-generated radiographs as compared to the plain radiographs. However, it is possible that the findings of no difference in diagnostic accuracy by experience level group represent a Type II statistical error, as the study was powered for the measurement of interobserver agreement rather than diagnostic accuracy. In addition, this study did not explore the association between fracture type and interobserver agreement or diagnostic accuracy. Observers were presented only 17 unique fractures, which does not allow thorough statistical analysis given that observers could have selected 10 different fracture types, of which seven were among those presented to the observers. If there is an association between fracture type and interobserver agreement or diagnostic accuracy, it is possible that a different mix of fracture types would have produced different results.
Our findings indicate that, in a study population of obese patients, plain radiographs offer no advantage over CT-generated radiographs for fracture classification. This is similar to previous work by O’Toole et al. [16], which evaluated the utility of CT-generated radiographs for acetabular fracture diagnosis and demonstrated that Judet view plain radiographs had a lower agreement (52%) and κ value (0.512) than CT-generated radiographs (68% and 0.659, respectively). However, that study did not specifically look at an obese patient population and included only patients who already had a three-dimensional CT reconstruction available, thereby introducing the possibility of selection bias. In addition, their study was limited by using consensus opinion as the gold standard. Therefore, in the current study, we sought to determine the applicability of CT-generated radiographs in obese patients and used all these patients who presented to a Level 1 trauma center. Furthermore, we believe that a more appropriate gold standard diagnosis is that determined by the treating surgeon, using all available imaging studies and the intraoperative findings by which the presumed fracture can be validated during the operative procedure. We believe that this method offers greater potential accuracy in obtaining the true classification. Using this method in a general population of patients with acetabular fractures, Borelli et al. [2] had findings similar to ours (CT-generated radiographs: κ = 0.73; plain radiographs: κ = 0.78).
The analysis of the frequency of diagnosis agreement between CT-generated and plain radiographs demonstrated substantial overall agreement (κ = 0.67). However, for the less experienced junior surgeons, it was found that the agreement was merely moderate (κ = 0.48), indicating that less experienced surgeons have more difficulty in delineating the same fracture pattern. In addition, surgeons with greater experience performed better than junior residents when looking specifically at plain radiographs. These findings are consistent with those of Beaule et al. [1]. They found that their most experienced observers (a group consisting of three orthopaedic surgeons who had studied under Letournel and had 15 to 18 years of experience treating acetabular fractures) did better than the less experienced observers (three general orthopaedic trauma surgeons who had treated fewer than 50 fractures over the previous 5- to 10-year period) [1]. However, for CT-generated radiographs, we did not observe a difference by experience level. This would suggest that CT-generated radiographs are valuable not simply for clinical applications but also for teaching less experienced residents. As one’s experience increased, the accuracy of plain radiographs improved to eventually be no different from that with CT-generated radiographs.
Electing to forego plain radiographs in favor of generated images has a number of potential benefits. Returning the patient to the radiology suite to obtain Judet views or repeat imaging due to inadequate films would be eliminated. Furthermore, CT-generated radiographs may be rotated and manipulated without subjecting the patient to possible pain and discomfort from transport to the radiology suite and positioning for the oblique radiographs. In patients who have associated injuries that may preclude the positional manipulation required for plain radiographic Judet views, CT-generated radiographs offer the ability to stabilize the patient but still obtain all necessary information. In addition, for surgeons less experienced with viewing Judet plain radiographs, CT-generated radiographs facilitate improved understanding of the fracture morphology and communication among all members of the orthopaedic trauma team. However, it should be noted that, due to the contained supine patient position during the CT procedure, CT-generated radiographs may underestimate fracture instability that may be more apparent under the oblique positioning required for plain radiographic Judet views [18].
Our findings echo those of previous studies [2, 16] in unselected patient populations but extend those findings and confirm them in a population of patients with obesity. Based on our findings, we believe that, for obese patients, once an acetabular fracture is suspected, there is no need to obtain plain radiographic Judet views. The data obtained from the routine pelvic CT with 3-mm or less slice thickness can be used to create simulated AP and Judet plain radiographic views. In conjunction with the standard two-dimensional axial CT images, these CT-generated radiographs should be sufficient for diagnosis and preoperative planning. Furthermore, we believe that CT-generated radiographs are an important imaging development and consideration should be given for their general use as an alternative to repeat imaging when initial plain radiographs prove to be inadequate. In this way, additional radiation exposure and patient discomfort can be avoided.
Based on our findings, we no longer see the need to put obese patients through the discomfort and additional cost and radiation exposure associated with plain radiographs if they are getting a CT scan as part of their evaluation.
Acknowledgments
We thank Todd Gebke BSRT for his assistance in obtaining the CT-generated images and Heidi Israel PhD and Eric S. Armbrecht PhD for their help with the statistical analyses.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Beaule PE, Dorey FJ, Matta JM. Letournel classification for acetabular fractures: assessment of interobserver and intraobserver reliability. J Bone Joint Surg Am. 2003;85:1704–1709. [PubMed] [Google Scholar]
- 2.Borrelli J, Jr, Peelle M, McFarland E, Evanoff B, Ricci WM. Computer-generated radiographs are as good as plain radiographs for assessment of acetabular fractures. Am J Orthop. 2008;37:455–4603. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Overweight and obesity. Available at: http://www.cdc.gov/obesity/data/adult.html. Accessed November 28, 2013.
- 4.Court-Brown CM, Aitken SA, Forward D, O’Toole RV., 3rd . The epidemiology of fractures. In: Bucholz RW, Heckman JD, Court-Brown CM, Tornetta P 3rd, editors. Rockwood and Green’s Fractures in Adults. 7. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. pp. 1463–1523. [Google Scholar]
- 5.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 6.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. J Bone Joint Surg Am. 1964;46:1615–1638. [PubMed] [Google Scholar]
- 7.Kuszyk BS, Heath DG, Bliss DF, Fishman EK. Skeletal 3-D CT: advantages of volume rendering over surface rendering. Skeletal Radiol. 1996;25:207–214. doi: 10.1007/s002560050066. [DOI] [PubMed] [Google Scholar]
- 8.Laird A, Keating JF. Acetabular fractures: a 16 year prospective epidemiological study. J Bone Joint Surg Br. 2005;87:969–973. doi: 10.1302/0301-620X.87B7.16017. [DOI] [PubMed] [Google Scholar]
- 9.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 10.Letournel E, Judet R. Fractures of the Acetabulum. 2. New York, NY: Springer; 1993. [Google Scholar]
- 11.Ly TV, Stover MD, Sims SH, Reilly MC. The use of an algorithm for classifying acetabular fractures. Clin Orthop Relat Res. 2011;469:2371–2376. doi: 10.1007/s11999-011-1925-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, De Coster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(suppl 10):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 13.Martinez CR, Di Pasquale TG, Helfet DL, Graham AW, Sanders RW, Ray LD. Evaluation of acetabular fractures with two- and three-dimensional CT. Radiographics. 1992;12:227–242. doi: 10.1148/radiographics.12.2.1561413. [DOI] [PubMed] [Google Scholar]
- 14.Norman GR, Streiner DL. Biostatistics: The Bare Essentials. 2. London, UK: BC Decker, Inc; 2000. [Google Scholar]
- 15.Ohashi K, El-Khoury GY, Abu-Zahra KW, Berbaum KS. Interobserver agreement for Letournel acetabular fracture classification with multidetector CT: are standard Judet radiographs necessary? Radiology. 2006;241:386–391. doi: 10.1148/radiol.2412050960. [DOI] [PubMed] [Google Scholar]
- 16.O’Toole RV, Cox G, Shanmuganathan K, Castillo RC, Turen CH, Sciadini MF, Nascone JW. Evaluation of computed tomography for determining the diagnosis of acetabular fracture. J Orthop Trauma. 2010;24:284–290. doi: 10.1097/BOT.0b013e3181c83bc0. [DOI] [PubMed] [Google Scholar]
- 17.Porter SE, Russell GV, Dews RC, Qin Z, Woodall J, Jr, Graves M. Complications of acetabular fracture surgery in morbidly obese patients. J Orthop Trauma. 2008;22:589–594. doi: 10.1097/BOT.0b013e318188d6c3. [DOI] [PubMed] [Google Scholar]
- 18.Routt ML, Jr, Agarwal A. Acetabular fractures: definitive treatment and expected outcomes. In: Teague D, Schmidt A, editors. Orthopaedic Knowledge Update: Trauma 4. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010. pp. 323–335. [Google Scholar]
- 19.Scott WW, Fishman EK, Magid D. Acetabular fractures: optimal imaging. Radiology. 1987;165:537–539. doi: 10.1148/radiology.165.2.3659379. [DOI] [PubMed] [Google Scholar]
- 20.Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005;85:257–268. [PubMed] [Google Scholar]
- 21.Sturm R. Increases in morbid obesity in the USA: 2000–2005. Public Health. 2007;121:492–496. doi: 10.1016/j.puhe.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. BMI classification. Available at: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed November 28, 2013.