Abstract
Background
Acetabular fractures and surgical interventions used to treat them can result in nerve injuries. To date, only small case studies have tried to explore the frequency of nerve injuries and their association with patient and treatment characteristics. High-quality data on the risk of traumatic and iatrogenic nerve lesions and their epidemiology in relation to different fracture types and surgical approaches are lacking.
Questions/purposes
The purpose of this study was to determine (1) the proportion of patients who develop nerve injuries after acetabular fracture; (2) which fracture type(s) are associated with increased nerve injury risk; and (3) which surgical approach was associated with the highest proportion of patients developing nerve injuries using data from the German Pelvic Trauma Registry. Two secondary aims were (4) to assess hospital volume–nerve-injury relationship; and (5) internal data validity.
Methods
Between March 2001 and June 2012, 2236 patients with acetabular fractures were entered into a prospectively maintained registry from 29 hospitals; of those, 2073 (92.7%) had complete records on the endpoints of interest in this retrospective study and were analyzed. The neurological status in these patients was captured at their admission and at the discharge. A total of 1395 of 2073 (67%) patients underwent surgery, and the proportions of intervention-related and other hospital-acquired nerve injuries were obtained. Overall proportions of patients developing nerve injuries, risk based on fracture type, and risk of surgical approach type were analyzed.
Results
The proportion of patients being diagnosed with nerve injuries at hospital admission was 4% (76 of 2073) and at discharge 7% (134 or 2073). Patients with fractures of the “posterior wall” (relative risk [RR], 2.0; 95% confidence interval [CI], 1.4–2.8; p = 0.001), “posterior column and posterior wall” (RR, 2.9; CI, 1.6–5.0; p = 0.002), and “transverse + posterior wall” fracture (RR, 2.1; CI, 1.3–3.5; p = 0.010) were more likely to have nerve injuries at hospital discharge. The proportion of patients with intervention-related nerve injuries and that of patients with other hospital-acquired nerve injuries was 2% (24 of 1395 and 46 of 2073, respectively). They both were associated with the Kocher-Langenbeck approach (RR, 3.0; CI, 1.4–6.2; p = 0.006; and RR, 2.4; CI, 1.4–4.3; p = 0.004, respectively).
Conclusions
Acetabular fractures with the involvement of posterior wall were most commonly accompanied with nerve injuries. The data suggest also that Kocher-Langenbeck approach to the pelvic ring is associated with a higher risk of perioperative nerve injuries. Trauma surgeons should be aware of common nerve injuries, particularly in posterior wall fractures. The results of the study should help provide patients with more exact information on the risk of perioperative nerve injuries in acetabular fractures.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Acetabular fractures frequently are associated with nerve injuries that arise from the lumbar plexus, including the sciatic nerve and its component branches. Common nerve injuries associated with acetabular fractures involve the obturator, femoral, and lateral femoral cutaneous nerves on the anterior and the sciatic nerve on the posterior aspect of the hip [10, 14]. These nerve injuries associated with acetabular fractures can be subdivided into traumatic and iatrogenic with complications arising from traction, retractor placement, instrumentation, or implant position. Also, late nerve injuries may result from a hematoma, capsular or muscular scarring, and heterotopic ossifications [11].
To our knowledge, only small case studies have been published exploring the association of peripheral nerve damage and acetabulum fractures [6, 7, 22] and the evidence from large cohorts is lacking [8, 9, 16]. The need for evidence across hospitals brought us to perform the following study.
Using data from a large registry, we aimed to (1) describe the proportion of patients who develop nerve injuries after acetabular fracture; (2) which fracture type(s) are associated with increased nerve injury risk; (3) which surgical approach was associated with the highest proportion of patients developing nerve injuries; and to assess (4) hospital volume–nerve-injury relationship; and (5) the internal validity of the data.
Patients and Methods
German Pelvic Trauma Registry
The study design was a retrospective analysis of data collected prospectively from the German Multicenter Pelvic Study Group. This group started with documentation and reporting of pelvic fractures in 1991 based on the data from university and major trauma hospitals. With several content modifications and a steady increase in the number of participating hospitals, the group has been active until now and has been converted into the German Pelvic Trauma Registry. Today the group includes a consortium of trauma departments from 29 university hospitals and level I trauma centers. The participation hospitals are required to register all their treated cases. The documentation is based on modern web technology [18, 19]. The registry collects data prospectively in a central database located at the Institute for Evaluative Research in Medicine at the University of Bern in Switzerland (www.memcenter.unibe.ch). During the online data entry, various data validation rules apply to ensure the meaningfulness and completeness of each individual data set.
The registry collects data on the type of acetabular fracture, injury patterns, and injury severity. Furthermore, patient age and sex, fracture location, time to treatment, and treatment type (nonsurgical or surgical management) are documented. Data from surgically treated patients include surgical approaches and the used implants. Fracture classifications with explanations are available for participants within the documentation portal to allow for a common language. Each participating hospital has a medical doctor responsible for documentation, who is typically experienced in correct coding based on the provided documentation guide, classification guidelines, and other definitions.
The registry documentation captures the neurological status of the patients at hospital admission and at discharge. Furthermore, the registry allows for distinction of secondary nerve injury as a result of surgery complication. Based on two clinical examinations and distinction of intervention-related complications, the following frequencies and subfrequencies of nerve injuries were assessed: (1) nerve injuries at hospital admission; (1a) nerve injuries that were seen at hospital admission and that persisted until discharge; (1b) nerve injuries that were seen at admission and resolved until discharge; (2) intervention-related nerve injuries; (2a) intervention-related nerve injuries that persisted until discharge; (2b) intervention-related nerve injuries that resolved until discharge; (3) other hospital-acquired nerve injuries; and (4) nerve injuries at hospital discharge.
These frequencies of nerve injuries were analyzed in relation to the AO/OTA fracture type (A, B, C) [1] and the Letournel classification [15], which both are part of the documentation in the registry. Type A in the AO/OTA classification describes stable pelvic ring fractures, type B - fractures with only rotational instability, and type C fractures with both rotational and translational instability [1]. The proportions of intervention-related nerve injuries and other hospital-acquired nerve injuries were also assessed in relation to surgical approach. Moreover, the relationship between the frequency of nerve injuries and the number of treated patients per hospital was analyzed. The latter analysis studied nerve injuries at hospital admission, at discharge, and the nerve injuries declared as surgery complications.
To assess the internal validity of the data, patient characteristics and outcomes were compared between the group of the four largest “reference” hospitals (one of which is the founding center of the registry and another one is the registry-coordinating center and a coinvestigator) against pooled data from all “other” participating hospitals.
Study Population
Between March 2001 and June 2012, 2236 patients with acetabular fractures were entered into a prospectively maintained registry from 29 hospitals; of those, 2073 (92.7%) had complete records on the endpoints of interest in this retrospective study and were analyzed. The remaining 7.3% of patients in the database were with the status “under completion” and were excluded from the analysis.
The mean ± SD age was 57 ± 21 years (range, 9–100 years). The female-to-male ratio was 1:3. As a result of severe general medical condition, multiple injuries, or only minimal dislocation or fractures not involving the main loading zone of the acetabulum, 678 fractures were treated nonoperatively. The remaining 1395 patients were treated surgically. The overall mean Injury Severity Score was 13 ± 8. Only 3% of the patients were polytraumatized and had a mean Injury Severity Score of 21 ± 11. Of the 2073 acetabular fractures, 2026 (98%) were classified according to the Letournel classification. The mean time from trauma to hospital admission for final treatment including interhospital transfers was 2 ± 5 days. The mean time between admission and surgery was 4.5 ± 4.1 days (median, 2 days). The mean length of hospital stay was 21 ± 17 days. As a result of a central acetabular protrusion component or unstable posterior dislocation, 277 patients were initially treated with distal femoral traction.
Statistical Analysis
Relative risk of each fracture type and surgical approach was assessed in comparison to all other fracture types and approaches, respectively. The association of nerve injuries with the number of treated patients per hospital was assessed using Pearson correlation statistics with Fisher’s z-transformation. Comparisons between the data from “reference” and “other” hospitals were performed using the chi square test for categorical data and Wilcoxon rank sum test for continuous data, as appropriate.
The alpha was set to 0.05 throughout the study. All statistical analyses were conducted using SAS® 9.4 (SAS Institute, Inc, Cary, NC, USA).
Results
The total prevalence of nerve injury at admission was 4% (76 of 2073) and at discharge 7% (134 of 2073). Of this 4% rate at admission, 0.5% (11 of 2073) of the injuries resolved during hospitalization and the remaining 3% (65 of 2073) had persistent nerve injury at discharge (Tables 1, 2; Fig. 1). In 2% (27 of 1395) of the surgically treated patients, an intervention-related nerve injury occurred and persisted until discharge in most of the patients (2% [24 of 1395]) (Table 1; Fig. 1). In 2% (46 of 2073) of all patients, other hospital-acquired nerve injuries were seen (Table 1).
Table 1.
Frequencies of nerve injuries by AO/OTA fracture type
| Fracture type | Fracture Type A (partial articular fractures) | Fracture Type B (partial articular, transverse fractures) | Fracture Type C (complete articular, both columns) | Unknown/not classifiable | Total |
|---|---|---|---|---|---|
| Number (%) | 990 (48) | 721 (35) | 321 (16) | 41 (2) | 2073 (100) |
| NI at admission (%) | 44 (4) | 23 (3) | 7 (2) | 2 (5) | 76 (4) |
| Persisted until discharge (%) | 39 (4)* | 19 (3) | 6 (2) | 1 (2) | 65 (3)* |
| Resolved until discharge (%) | 5 (0.5) | 4 (0.6) | 1 (0.3) | 1 (2) | 11 (0.5) |
| Intervention-related NI (%) | 10 (2) | 13 (2) | 4 (2) | – | 27 (2) |
| Persisted until discharge (%) | 10 (2)* | 11 (2) | 3 (1) | – | 24 (2)* |
| Resolved until discharge (%) | – | 2 (0.4) | 1 (0.4) | – | 3 (0.2) |
| Other hospital-acquired NI (%) | 13 (1) | 19 (3) | 13 (4) | 1 (2) | 46 (2) |
| NI at discharge (%) | 61 (6) | 49 (7) | 22 (7) | 2 (5) | 134 (7) |
The proportions of the intervention-related nerve injuries were calculated based on the number of surgically treated cases (n = 1395); *there was one patient who had both a nerve injury at admission and an intervention-related nerve injury; NI = nerve injury.
Table 2.
Proportions of patients with nerve injuries by Letournel fracture types
| Fracture type | Anterior column | Anterior wall | Posterior column | Posterior wall | Transverse | T-type | Transverse + posterior wall | Posterior column + posterior wall | Anterior column + posterior hemitransverse | Both columns | Unknown/not classifiable | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number (%) | 413 (20) | 112 (6) | 85 (4) | 314 (16) | 132 (7) | 111 (6) | 117 (6) | 63 (3) | 352 (17) | 327 (16) | 46 (2) | 2073 (100) |
| NI at admission (%) | 4 (1) | – | 6 (7) | 24 (8) | 5 (4) | 7 (6) | 7 (6) | 9 (14) | 4 (1) | 9 (3) | 1 (2) | 76 (4) |
| Persisted until discharge (%) | 3 (0.7) | – | 6 (7) | 22 (7) | 5 (4) | 4 (4) | 6 (5) | 8 (13)* | 4 (1) | 7 (2) | – | 65 (3)* |
| Resolved until discharge (%) | 1 (0.2) | – | – | 2 (0.6) | – | 3 (3) | 1 (0.9) | 1 (2) | – | 2 (0.6) | 1 (2) | 11 (0.5) |
| Intervention-related NI (%) | 1 (0.5) | 1 (6) | – | 6 (3) | 1 (2) | 3 (4) | 3 (3) | 2 (4) | 5 (2) | 5 (2) | – | 27 (2) |
| Persisted until discharge (%) | 1 (0.5) | 1 (6) | – | 6 (3) | 1 (2) | 3 (4) | 2 (2) | 2 (4)* | 4 (2) | 4 (2) | – | 24 (2)* |
| Resolved until discharge (%) | – | – | – | – | – | – | 1 (0.9) | – | 1 (0.3) | 1 (0.3) | – | 3 |
| Other hospital-acquired NI (%) | 2 (0.5) | 1 (0.9) | – | 7 (2) | 2 (2) | 3 (3) | 7 (6) | 2 (3) | 6 (2) | 12 (4) | 4 (9) | 46 (2) |
| NI at discharge (%) | 6 (2) | 2 (2) | 6 (7) | 35 (11) | 8 (6) | 10 (9) | 15 (13) | 11 (18) | 14 (4) | 23 (7) | 4 (9) | 134 (7) |
The proportions of the intervention-related nerve injuries were calculated based on the number of surgically treated cases (n = 1395); *there was one patient who had both a nerve injury at admission and an intervention-related nerve injury; NI = nerve injury.
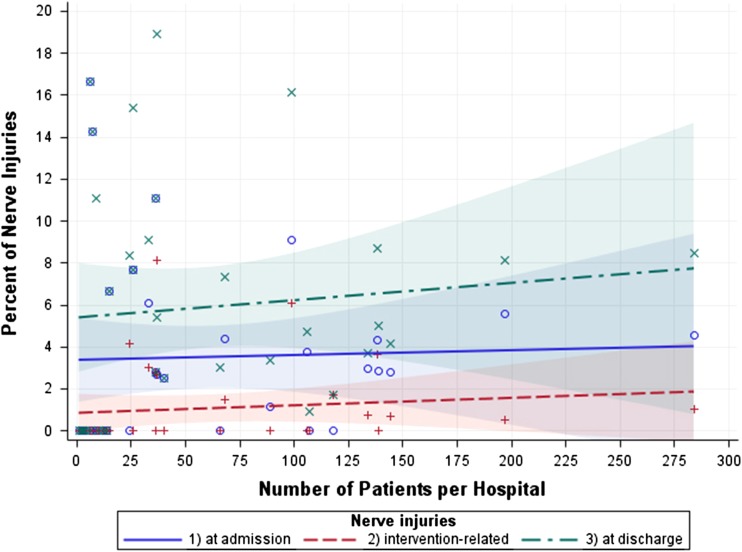
Fig. 1.
The figure displays relationships between the number of treated patients per hospital and the frequencies of nerve injuries at admission, at discharge, and intervention-related nerve injuries. Incidences of nerve injuries for each participating hospital are coded as o (on admission), + (intervention related), and X (at discharge).
Type C fractures were associated with the highest proportion of other hospital-acquired nerve injuries (risk ratio [RR] 2.2; 95% confidence interval [CI], 1.1–4.0; p = 0.022), and type A had the lowest proportion (RR, 0.4; CI, 0.2–0.8; p = 0.007) (Table 1); by fracture location, transverse + posterior wall fracture was associated with the highest (RR, 3.0; CI, 1.4–6.6; p = 0.013) and anterior column the lowest (RR, 0.2; CI, 0.04–0.8; p = 0.013) proportion of other hospital-acquired injuries (Table 2). Furthermore, anterior wall fractures were associated with the lowest proportion of nerve injuries at discharge (RR, 0.3; CI, 0.1–1.1; p = 0.045); anterior column fractures with the lowest proportion of nerve injuries at admission (RR, 0.2; CI, 0.1–0.6; p < 0.001), intervention-related (RR, 0.2; CI, 0.0–1.1; p = = 0.029) and at discharge (RR, 0.2; CI, 0.1–0.4; p < 0.001); anterior column + posterior hemitransverse with the lowest proportion of nerve injuries at admission (RR, 0.3; CI, 0.1–0.7; p = 0.003) and at discharge (RR, 0.6; CI, 0.3–1.0; p = 0.042); posterior wall fracture with the highest proportion of nerve injuries at admission (RR, 2.6; CI, 1.6–4.1; p < 0.001) and at discharge (RR, 2.0; CI, 1.4–2.8; p = 0.001); and posterior wall + posterior column fractures with the highest proportion of nerve injuries at admission (RR, 4.3; CI, 2.2–8.2; p < 0.001) and at discharge (RR, 2.9; CI, 1.6–5.0; p = 0.002) (Table 2). The majority of acetabular fractures were type A (48%) followed by type B (35%) and type C fractures (16%) (Table 1). The majority of acetabular fractures were found in the anterior column (20%) and in the anterior column plus posterior hemitransverse (17%) followed by both columns (16%) and posterior wall (16%) (Table 2). The proportions of other fracture locations were below 7% each (Table 2).
The Kocher-Langenbeck approach was associated with the highest proportion of intervention-related nerve injuries (RR, 3.0; CI, 1.4–6.2; p = 0.006) and the highest proportion of other hospital-acquired nerve injuries (RR, 2.4; CI, 1.4–4.3; p = 0.004). The relative risk of intervention-related nerve injuries for ilioinguinal approach was 2.2 (CI, 1–4.7; p = 0.053). The relative risk of intervention-related or other hospital-acquired nerve injuries in other surgical approaches had p values of 0.07 or above. The Kocher-Langenbeck and the ilioinguinal approaches were the two most popular (Table 3).
Table 3.
Frequencies of intervention-related and other hospital-acquired nerve injuries by surgical approach
| Surgical approach | Number (%) | Intervention-related NI (number [%]) | Other hospital-acquired NI (number [%]) |
|---|---|---|---|
| Kocher-Langenbeck | 495 (36) | 13 (3) | 20 (4) |
| Ilioinguinal | 616 (44) | 13 (2) | 14 (2) |
| Smith-Peterson/iliofemoral | 8 (0.6) | – | – |
| Extended iliofemoral | 2 (0.1) | – | – |
| Maryland | 12 (0.9) | – | – |
| Triradiate | 3 (0.2) | – | 1 (33) |
| Ventral + dorsal simultaneously | 7 (0.5) | – | – |
| Ventral + dorsal staged | 3 (0.2) | – | – |
| Limited | 14 (1) | 1 (7) | – |
| Stoppa | 25 (2) | – | – |
| Percutaneous | 74 (5) | – | 1 (1) |
| Other | 136 (10) | – | 6 (4) |
| Total | 1395 (100) | 27 (2) | 42 (3) |
NI = nerve injury.
There was no association between the hospital’s caseload and their proportions of nerve injuries at admission (r = 0.04; CI, −0.3 to 0.4; p = 0.84), at discharge (r = 0.1; CI, −0.2 to 0.4; p = 0.58), and their proportions of intervention-related nerve injuries (r = 0.1; CI, −0.2 to 0.4; p = 0.49).
Comparison of outcomes between the reference and other hospitals showed no differences (Table 4). The frequencies of nerve injury at hospital admission, as surgery complication and at hospital discharge, were even slightly, but not relevantly, higher in the pooled data of other hospitals. Comparison of patient characteristics showed differences in Injury Severity Score, length of hospital stay, fracture type, fracture location, proportion of surgically treated patients, and proportions of different surgical approaches (Table 4).
Table 4.
Patient, core injury, and treatment characteristics
| Patient characteristics | Four reference hospitals | Other hospitals | Comparison (p value) |
|---|---|---|---|
| Number (%) | 536 (26) | 1537 (74) | – |
| Mean age ± SD (years) | 58 ± 22 | 57± 21 | 0.16 |
| Females (%) | 113 (21) | 377 (25) | 0.11 |
| Polytraumatized patients (%) | 17 (3) | 34 (2) | 0.22 |
| ISS score ± SD | 11 ± 6 | 13 ± 8 | < 0.001 |
| Length of hospital stay | 18 ± 12 | 22 ± 18 | < 0.001 |
| Fracture type A (%) | 255 (48) | 735 (49) | 0.023 |
| Fracture type B (%) | 212 (40) | 509 (34) | |
| Fracture type C (%) | 69 (13) | 252 (17) | |
| Anterior column fracture (%) | 114 (21) | 299 (20) | 0.020 |
| Anterior wall fracture (%) | 28 (5) | 84 (6) | |
| Posterior column fracture (%) | 24 (5) | 61 (4) | |
| Posterior wall fracture (%) | 74 (14) | 240 (16) | |
| Transverse fracture (%) | 30 (6) | 102 (7) | |
| T-type fracture (%) | 27 (5) | 84 (6) | |
| Transverse + posterior wall fracture (%) | 23 (4) | 94 (6) | |
| Posterior column + posterior wall fracture (%) | 15 (3) | 48 (3) | |
| Anterior column + posterior hemitransverse fracture (%) | 117 (22) | 235 (15) | |
| Both columns fracture (%) | 68 (13) | 259 (17) | |
| Unknown/not classifiable fracture (%) | 16 (3) | 31 (2) | |
| Surgically treated patients (%) | 403 (75) | 992 (65) | < 0.001 |
| Kocher-Langenbeck approach (%) | 122 (30) | 373 (38) | < 0.001 |
| Ilioinguinal approach (%) | 193 (48) | 423 (43) | |
| Smith-Peterson/iliofemoral approach (%) | 4 (1) | 4 (0.4) | |
| Extended iliofemoral approach (%) | – | 2 (0.2) | |
| Maryland approach (%) | – | 12 (1) | |
| Triradiate approach (%) | 3 (0.7) | – | |
| Ventral + dorsal simultaneously approach (%) | – | 7 (0.7) | |
| Ventral + dorsal staged approach (%) | 1 (0.3) | 2 (0.2) | |
| Limited approach (%) | – | 14 (1) | |
| Stoppa approach (%) | 17 (4) | 8 (0.8) | |
| Percutaneous approach (%) | 24 (6) | 50 (5) | |
| Other approach (%) | 39 (10) | 97 (10) | |
| Outcomes | |||
| NI at admission (%) | 18 (3) | 58 (4) | 0.66 |
| Persisted until discharge | 17 (3) | 47 (3) | 0.90 |
| Resolved until discharge | 1 (0.2) | 10 (0.7) | 0.20 |
| Intervention-related NI (%) | 3 (0.6) | 24 (2) | 0.08 |
| Persisted until discharge | 3 (0.6) | 20 (1) | 0.16 |
| Resolved until discharge | – | 4 (0.3) | 0.31 |
| Other hospital-acquired NI (%) | 13 (2) | 33 (2) | 0.71 |
| NI at discharge (%) | 33 (6) | 101 (7) | 0.74 |
ISS = Injury Severity Score; NI = nerve injury.
Discussion
Nerve injuries can occur after acetabular fractures and from surgical interventions. To date, only small case studies have been published exploring the association of peripheral nerve damage and acetabulum fractures [6, 7, 22]. There is a paucity of detailed data on the frequency of traumatic nerve injuries and nerve injuries as surgery complications as well as their relationships with fracture types, fracture location, and surgical approaches. For this reason, the data from currently the largest observational cohort on pelvic trauma were analyzed to determine (1) the proportion of nerve injuries; (2) which fracture type(s) are associated with increased nerve injury risk; and (3) which surgical approach was associated with iatrogenic nerve injuries. Additionally, (4) the hospital volume–nerve-injury relationship as well as (5) internal validity of the data were assessed.
Some limitations of the study deserve mention. Although the documentation in the registry is prospective and participating hospitals are required to document all their cases, no on-site audits validating the accuracy and completeness of the data of this multicenter observational registry are currently performed. One can imagine that such audits in such a large study setting would require enormous personal and financial resources. The goal of the registry is to improve patient safety, effectiveness of treatments, and patient outcome. There is no financial support for documentation or participation of hospitals. Participation in the registry is voluntary and includes, to the opinion of the authors, dedicated and motivated pioneers only. The documentation takes place through an online web-based portal, which applies data validation rules ensuring certain generic accuracy and completeness of the data. For example, the order and correctness of accident, admission, treatment, and discharge dates is ensured. If acetabulum fracture is endorsed, then acetabulum-specific fracture classifications, treatment, and complications are mandatory. This ensures meaningfulness of the collected data. Only complete records can be submitted and, thus, locked for analyses and internal reports. The proportion of incomplete records is constantly assessed and consequently efforts are made to keep this proportion to a minimum. Each participating hospital has a medical doctor responsible for documentation, who is typically experienced in correct coding based on the provided documentation guide, classification guidelines, and other definitions. The responsible colleagues are meeting twice annually to discuss the documentation load, methodological questions, scientific analyses, etc. Monitoring of documentation by participating center and internal data validation are taking place at these meetings. As a result of inability to perform on-site audits, the registry group has just decided to start collecting documentation coverage rates based on the number of treated and registered cases in each center and to introduce a hospital certification. To assess potential selection bias and their influence on the outcomes, the four largest reference hospitals including the registry-founding center and the registry coordination center (which is also a coinvestigator of the study) were selected and their data were compared against the pooled data of other 25 participating hospitals. The analysis showed some slight but significant differences in patient characteristics, which may be anticipated in multicenter settings. However, importantly, no significant differences were seen regarding the studied frequencies of nerve injuries. The frequencies of nerve injury at hospital admission, as surgery complication, and at hospital discharge were slightly, but not relevantly, higher in the pooled data of other hospitals, which points to rather trustworthy documentation, at least of nerve injuries in the registry. Nevertheless and although there is no reason to doubt the accuracy of the data, potential selection bias may not completely be excluded in these unmonitored settings. The study represents a univariate descriptive analysis. In the next step in a further growing cohort, it would be desirable to perform multivariate-adjusted analyses for detection of quantitative relationships and assessment of the influence of potential confounding variables. Moreover, analysis of the injuries of specific nerves was not possible in this article, because these data were not part of the documentation. A detailed documentation of the injuries of specific nerves is desired in future studies. One should be aware of other factors with a potential influence on nerve injury risk, for example, such as the level of experience of the surgeon [5] or the country. For example, in Germany, the most experienced surgeon is often the primary operating surgeon, whereas in other countries, the experienced surgeon may be helping a fellow or senior resident to perform the surgery. The study may represent the results of rather experienced surgeons. The factor country and healthcare system is also important for interpretation of length of hospital stay, which has strong variation in different countries and which depends for example on the extent of rehabilitative measures applied in the hospital. Our analyses showed that nerve injuries were not uncommon in acetabular fractures. Others have reported between 3% and 23% of patients experience nerve injuries, but different study designs and definitions of a nerve injury make them hard to compare across studies [5–7, 15, 17]. The frequency of nerve injuries changed during the hospital stay. Some of the nerve injuries including also some intervention-related nerve injuries resolved until hospital discharge. On the other hand, there were no intervention-related nerve injuries that were also not diagnosed at hospital admission, which were categorized as “other hospital-acquired nerve injuries” and which could have occurred at any time point before discharge. Poor or limited initial physical examination may well be the explanation for them. Furthermore, space-occupying hemorrhages that pinch nerves may be a further explanation, at least to some extent.
Fractures of the posterior acetabulum were most frequently associated with nerve injuries in our study. These results are consistent with previous reports that indicated an increased risk for nerve injury in cases of posterior wall and transverse fractures [3, 9]. In the anterior part of the acetabulum, the obturator nerve and the femoral nerve can be affected during trauma [22]. In our study, only 2% (six of 413 and two of 112, respectively) of patients with anterior column and anterior wall fractures had lesions of these nerves, respectively. According to our own clinical experience, intraoperative entrapment of the obturator nerve in the quadrilateral space is frequently seen, particularly in anterior column fractures involving the anterior portion of the quadrilateral surface.
Intervention-related nerve injuries and other hospital-acquired nerve injuries were associated with the Kocher-Langenbeck approach only, which was the second most popular approach after the ilioinguinal one. In the literature, the Kocher-Langenbeck approach is used in approximately 60% of fractures followed by the ilioinguinal approach in approximately 30%. Other approaches were not associated with a significantly higher risk for nerve injuries. Letournel was able to decrease his initially reported rate of 18% of iatrogenic nerve injuries to 9% by using transcondylar traction in combination with knee flexion [15, 17]. Vrahas et al. have suggested that the remaining proportion of injuries is most probably caused by compression resulting from poorly placed retractors [21]. In addition to gentle hook insertion, it may be helpful to allow for more effective retraction of the posterior flap to partially release the distal insertion of the gluteus maximus tendon onto the posterior aspect of the femoral shaft [11]. It is the sciatic nerve that is typically injured in posterior approaches. However, in a series of 726 acetabular fractures treated using the Kocher-Langenbeck approach, Gruson and Moed reported an iatrogenic injury of the femoral nerve in 0.3% of cases [8, 20]. This is despite that the femoral nerve should rather be at risk in anterior approaches. Also, the extended iliofemoral approach is considered to be most frequently associated with nerve injuries [9]. According to the registry data, this approach is not popular in German hospitals with only 0.1% of all approaches. Regardless of which approach is used, particular attention should be paid to retraction [9] as well as to avoid trapping of the nerve during reduction of fracture fragments [2, 4, 12, 13, 16, 20].
The analysis of relationships between hospital caseload and frequency of nerve injuries at hospital admission, discharge, and intervention-related nerve injuries showed no significant correlations. However, only bivariate relationships were assessed. The relationships may be much more complex in reality, eg, depending on other factors such as proportions of complex fractures and complex surgery, patient age and sex, etc. Future adjusted analyses of the growing registry cohort are desired.
In conclusion, in patients with acetabular fractures, nerve injuries were observed in 4% at hospital admission and in 7% at hospital discharge, whereas the proportion of nerve injuries as surgical complications was 2%. Some nerve injuries are transient and resolve during the hospital stay. Posterior wall fractures of the pelvic ring were more frequently associated with the nerve injuries at discharge. Furthermore, the posterior Kocher-Langenbeck approach was associated with both intervention-related and other hospital-acquired nerve injuries. Trauma surgeons should be aware of the common nerve injuries in acetabular fractures. The results of this large multicenter study help to provide patients with more exact information on the risk of perioperative nerve injuries in acetabular fractures.
Acknowledgments
We thank all members of the Pelvic Trauma Working Group of the German Trauma Association. Without their efforts, the German Pelvic Trauma Registry and this study would not have been possible. Institutions contributing to the German Pelvic Trauma Registry include: AZ Groeninge Hospital, Kortrijk, Belgium; BG Trauma Hospital, Halle, Germany; BG Trauma Hospital, Tübingen, Germany; BG Trauma Hospital, Ludwigshafen, Germany; BG Trauma Hospital, Murnau, Germany; German Army Hospital, Ulm, Germany; Charité Virchow Campus, Berlin, Germany; Friederikenstift Hospital, Hannover, Germany; University Hospital, Regensburg, Germany; General Hospital, Ludwigsburg, Germany; Hospital of the Technical University, Munich, Germany; General Hospital, Augsburg, Germany; General Hospital, Dortmund, Germany; General Hospital, Biberach, Germany; Medical University, Hannover, Germany; University Hospital Aachen, Aachen, Germany; SKM Hospital, Koblenz, Germany; Municipal Hospital, Braunschweig, Germany; Municipal Hospital, Karlsruhe, Germany; University Hospital, Magdeburg, Germany; University Hospital, Kiel, Germany; University Hospital, Mainz, Germany; University Hospital, Halle, Germany; University Hospital, Freiburg, Germany; University Hospital, Jena, Germany; University Hospital, Münster, Germany; University Hospital, Homburg, Germany; University Hospital, Leipzig, Germany; University Hospital, Hamburg, Germany; University Hospital, Ulm, Germany; and Westpfalz Hospital, Kaiserslautern, Germany.
Footnotes
W. Lehmann and M. Hoffmann contributed equally and therefore share first authorship.
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at University Medical Center Hamburg-Eppendorf, Hamburg, Germany.
References
- 1.AO/OTA. Pelvis. J Orthop Trauma. 2007;21(Suppl 10):S59–S67.
- 2.Archdeacon MT, Kazemi N, Guy P, Sagi HC. The modified Stoppa approach for acetabular fracture. J Am Acad Orthop Surg. 2011;19:170–175. doi: 10.5435/00124635-201103000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Bradshaw C, McCrory P, Bell S, Brukner P. Obturator nerve entrapment. A cause of groin pain in athletes. Am J Sports Med. 1997;25:402–408. doi: 10.1177/036354659702500322. [DOI] [PubMed] [Google Scholar]
- 4.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305:112–123. doi: 10.1097/00003086-199408000-00015. [DOI] [PubMed] [Google Scholar]
- 5.de Ridder VA, de Lange S, Kingma L, Hogervorst M. Results of 75 consecutive patients with an acetabular fracture. Clin Orthop Relat Res. 1994;305:53–57. doi: 10.1097/00003086-199408000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Dunbar RP, Jr, Gardner MJ, Cunningham B, Routt ML., Jr Sciatic nerve entrapment in associated both-column acetabular fractures: a report of 2 cases and review of the literature. J Orthop Trauma. 2009;23:80–83. doi: 10.1097/BOT.0b013e318190cfa0. [DOI] [PubMed] [Google Scholar]
- 7.Fassler PR, Swiontkowski MF, Kilroy AW, Routt ML., Jr Injury of the sciatic nerve associated with acetabular fracture. J Bone Joint Surg Am. 1993;75:1157–1166. doi: 10.2106/00004623-199308000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Gruson KI, Moed BR. Injury of the femoral nerve associated with acetabular fracture. J Bone Joint Surg Am. 2003;85:428–431. doi: 10.2106/00004623-200303000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Haidukewych GJ, Scaduto J, Herscovici D, Jr, Sanders RW, DiPasquale T. Iatrogenic nerve injury in acetabular fracture surgery: a comparison of monitored and unmonitored procedures. J Orthop Trauma. 2002;16:297–301. doi: 10.1097/00005131-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Hospodar PP, Ashman ES, Traub JA. Anatomic study of the lateral femoral cutaneous nerve with respect to the ilioinguinal surgical dissection. J Orthop Trauma. 1999;13:17–19. doi: 10.1097/00005131-199901000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Issack PS, Helfet DL. Sciatic nerve injury associated with acetabular fractures. HSS J. 2009;5:12–18. doi: 10.1007/s11420-008-9099-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keel MJ, Bastian JD, Buchler L, Siebenrock KA. Anterior approaches to the acetabulum [in German] Der Unfallchirurg. 2013;116:213–220. doi: 10.1007/s00113-012-2332-7. [DOI] [PubMed] [Google Scholar]
- 13.Keel MJ, Ecker TM, Cullmann JL, Bergmann M, Bonel HM, Buchler L, Siebenrock KA, Bastian JD. The Pararectus approach for anterior intrapelvic management of acetabular fractures: an anatomical study and clinical evaluation. J Bone Joint Surg Br. 2012;94:405–411. doi: 10.1302/0301-620X.94B3.27801. [DOI] [PubMed] [Google Scholar]
- 14.Kloen P, Siebenrock KA, Ganz R. Modification of the ilioinguinal approach. J Orthop Trauma. 2002;16:586–593. doi: 10.1097/00005131-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;151:81–106. [PubMed] [Google Scholar]
- 16.Matta JM. Operative treatment of acetabular fractures through the ilioinguinal approach: a 10-year perspective. J Orthop Trauma. 2006;20:S20–S29. [PubMed] [Google Scholar]
- 17.Middlebrooks ES, Sims SH, Kellam JF, Bosse MJ. Incidence of sciatic nerve injury in operatively treated acetabular fractures without somatosensory evoked potential monitoring. J Orthop Trauma. 1997;11:327–329. doi: 10.1097/00005131-199707000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Ochs BG, Marintschev I, Hoyer H, Rolauffs B, Culemann U, Pohlemann T, Stuby FM. Changes in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU) Injury. 2010;41:839–851. doi: 10.1016/j.injury.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 19.Pohlemann T, Tosounidis G, Bircher M, Giannoudis P, Culemann U. The German Multicentre Pelvis Registry: a template for an European Expert Network? Injury. 2007;38:416–423. doi: 10.1016/j.injury.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 20.Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified Rives-Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24:263–270. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 21.Vrahas M, Gordon RG, Mears DC, Krieger D, Sclabassi RJ. Intraoperative somatosensory evoked potential monitoring of pelvic and acetabular fractures. J Orthop Trauma. 1992;6:50–58. [PubMed] [Google Scholar]
- 22.Yang KH, Han DY, Park HW, Park SJ. Intraarticular entrapment of the obturator nerve in acetabular fracture. J Orthop Trauma. 2001;15:361–363. doi: 10.1097/00005131-200106000-00010. [DOI] [PubMed] [Google Scholar]