Abstract
Background
In the clinic, variations in circadian rhythm are evident in patients with cardiovascular disease, and the risk of cardiovascular events increases when rhythms are disrupted. In this study, we focused on the role of the circadian gene period2 (per2) in mobilization and function of endothelial progenitor cells (EPCs) in vitro and in vivo after myocardial infarction (MI) in mice.
Methods and Results
MI was produced by surgical ligation of the left anterior descending coronary artery in mice with and without per2 deficiency. Trans-thoracic echocardiography was used to evaluate cardiac function in mice. Per2−/− mice with MI showed decreased cardiac function and increased infarct size. The number of CD34+ cells and capillary density were decreased in the myocardium of per2−/− mice on immunohistochemistry. Flow cytometry revealed decreased number of circulating EPCs in per2−/− mice after MI. In vitro, per2−/− EPCs showed decreased migration and tube formation capacity under hypoxia. Western blot analysis revealed inhibited activation of extracellular signal-regulated kinase and Akt signaling in the bone marrow of per2−/− mice and inhibited PI3K/Akt expression in per2−/− EPCs under hypoxia.
Conclusions
Per2 modulates EPC mobilization and function after MI, which is important to recovery after MI in mice.
Introduction
For most of the past 2 decades, the role of the microvasculature in recovery from myocardial infarction (MI) has been considered important. Studies of humans and animals have shown that a subpopulation of mononuclear cells with enhanced potential for differentiation into endothelial cells are mobilized endogenously from the bone marrow in response to MI and become incorporated into sites of new vessel growth in the ischemic tissue [1]–[4]. These cells are known as endothelial progenitor cells (EPCs). Circulating EPC level and function are predictive of prognosis following acute MI and are associated with cumulative cardiovascular risk, cardiovascular mortality and atherosclerosis progression in patients with coronary artery disease [5]–[11]. Mobilization of CD34+ cells by drugs or transplantation of ex vivo-expanded EPCs could improve cardiac function after myocardial ischemia [12], [13], [35].
Variations in circadian rhythm are evident in patients with cardiovascular diseases, and the risk of cardiovascular events increases when rhythms are disrupted [14]–[17]. Epidemiologic studies have demonstrated circadian patterns associated with the incidence of cardiovascular disease. For example, the onset of MI is markedly increased between 6:00 AM and 12:00 PM [18]. However, the specific relationship between a circadian gene and mobilization of bone-marrow EPCs associated with early MI has not been determined.
Period2 (per2) regulating EPC function under hypoxia has not been determined. Given that circadian rhythms control the cell cycle and tumor growth [19], per2 may be able to alter the response of bone marrow and EPC function to ischemic injury. Therefore, we investigated the effect of per2 deletion on the response of bone-marrow EPC mobilization and function in mice with MI and in vitro.
Methods
Mouse Model of MI
C57BL/6 wild-type (WT) mice (n = 30, 8–12 weeks old) weighing 25–30 g were obtained from VITAL RIVER (Beijing). Per2−/− mice (n = 25) were obtained from the Model Animal Research Center, Nanjing University (Nanjing, China), and backcrossed for more than 10 generations onto a C57BL/6 inbred background. All animal studies were carried out at the Animal Care Center of the Key Laboratory of Cardiovascular Remodeling and Function Research, Shandong University (Shandong, China). The experiment followed the Animal Management Rule of the Ministry of Public Health, People's Republic of China (document no. 55, 2001), and the experimental protocol was approved by the Animal Care Committee of Shandong University.
Mice were acclimatized in the same room with a 12-h/12-h light–dark cycle for at least 2 weeks before experiments. MI was induced by surgical ligation of the left anterior descending (LAD) coronary artery as described [20]. Mice were anesthetized with sodium pentobarbital (50 mg/kg), then the chest was opened at the left fourth intercostal space and the LAD was ligated with a 7–0 silk suture. Successful ligation was verified by color change in the artery.
Assessment of Cardiac Function
Four weeks after MI, trans-thoracic echocardiography (Visual Sonics Vevo 770, Canada) was used to evaluate cardiac function in mice. We measured the left-ventricular (LV) internal dimension diastolic, LV internal dimension systolic, systolic ejection fraction and percent LV fractional shortening (FS). An observer blinded to the experiment performed the measurements for at least 3 consecutive pulsation cycles.
Histology
Briefly, mice were euthanized with sodium pentobarbital (50 mg/kg). The chest was opened and the heart was arrested in diastole by intraventricular injection of KCL (10%). The myocardial vasculature was perfused with 4% formalin for 10 min. Hearts were harvested and fixed in 4% formalin for 48 hr. Cardiac fibrosis was assessed by Masson's trichrome staining. The infarct size and fibrosis areas were expressed as the sum of the epicardial and endocardial scar length divided by the sum of the LV epicardial and endocardial circumferences [21]. CD34 (1∶200, Abcam, USA) immunohistochemistry was used to assess EPCs in the infarcted myocardium. Capillary density in the peri-infarct area was determined 28 days after infarction. Paraffinized LV 5-µm sections were immunohistochemically stained with anti-CD31 monoclonal antibody (PECAM-1, 1∶50, R&D, Germany). Briefly, sections were deparaffinized, pretreated with 0.3% H2O2 for 20 min to inhibit endogenous peroxidase activity, then blocked with 2% goat serum for 30 min and incubated with primary antibody overnight at 4°C. Visualization involved the avidinbiotin-complex technique and high-sensitivity diaminobenzidine (DAB+) chromogenic substrate system (Dako Denmark), then counterstaining with hematoxylin. We counted 6 randomly selected 400×fields, and mean CD34+ or CD31+ cells per field was obtained for statistical analysis.
Evaluation of Circulating EPCs
Circulating EPCs were quantified 3 days after the onset of MI. Circulating EPCs were defined as CD34+ (FITC-conjugated anti-mouse CD34 antibody, eBioscience) and positive for endothelial-specific antigen KDR (APC-conjugated anti-mouse KDR antibody, eBioscience) [22]–[24]. FITC- or APC-conjugated isotype IgG antibody (eBioscience) was used as a control. Cells were analyzed by use of a fluorescence-activated cell sorter (FACS caliber, BD Biosciences) and CD34+ and KDR+ EPCs were expressed as proportion of mononuclear cells.
Bone-marrow Cell Isolation and EPC Culture
Hollow bones of mouse legs were extracted by standard surgical procedures, and whole bone marrow was harvested by flushing the marrow out with 500 µl phosphate buffered solution (PBS) by use of a syringe with a 20-gauge needle. Some bone marrow extracts were shock-frozen before analysis.
EPC isolation, ex vivo expansion and culture of EPCs was performed as previously described [25]. In brief, bone-marrow mononuclear cells were isolated from mice by density-gradient centrifugation with lymphocyte separation medium (mouse) (Solarbio, China). Cells were plated on culture dishes coated with mice vitronectin (Sigma) and cultured in phenol red–free endothelial-cell basal medium-2 (Lonza, Germany) supplemented with hydrocortisone, human fibroblast growth factor B, vascular endothelial growth factor (VEGF), R3 insulin-like growth factor 1, ascorbic acid, human endothelial growth factor, GA-1000, heparin and 5% fetal bovine serum. Cells were maintained at 37°C with 5% CO2 in a humidified atmosphere for 4 days, then non-adherent cells were removed by washing with PBS and new medium was added. The culture was maintained through day 7, when EPCs were recognized as attached spindle-shaped cells. Cells were extensively washed with PBS, and adherent cells were incubated with 2.4 µg/ml 1,1′-dioctadecyl-3,3,3′,3′-tetramethylindocarbocyanine perchlorate-acetylated low-density lipoprotein (DiI-Ac-LDL, Invitrogen) and stained with FITC-labelled Ulex europaeus agglutinin 1 (lectin, 10 µg/ml; Sigma) for EPCs. EPCs were also characterized by immunofluorescence staining for the expression of VEGF receptor 2 (Flk1, Abcam), platelet/endothelial cell adhesion molecule-1 (CD31, R&D), and CD34 (Abcam). The fluorescent images were recorded under a laser scanning confocal microscope.
In some experiments, 7-day EPCs from WT and per2−/− mice were incubated in a hypoxic condition (1% O2) for 24 hr.
EPC Migration and Tube Formation
Migration of EPCs was investigated under normoxic and hypoxic conditions with the modified Boyden chamber assay as described [26]. In brief, 2×104 EPCs were cultured in inlets (Costar, 8-µm pore size) placed in 24-well culture dishes containing 500 µl endothelial basal medium (Lonza, Germany) and 50 ng/ml VEGF (Prospec, Ness Zina, Israel). After 24 hr, migrated cells were fixed with 4% paraformaldehyde (Sigma) in PBS for 30 min, then wiped gently with a cotton ball to remove non-migratory cells and stained with 2% crystal violet in ethanol. Data are presented as mean number of migrated cells in 5 randomly selected fields at 200× magnification in every membrane (n = 6 in each group).
For tube-formation ability, we used the matrix gel tube formation assay. First, 50 µl matrix gel was added into every well of 96-well plates at 37°C for 1 hr. An amount of 2×104 EPCs supplemented with 50 µl EBM-2 with VEGF (50 ng/ml) was placed onto the matrix gel. The plate was placed under hypoxic conditions for 24 hr. Data are shown as the mean tube number of 5 randomly selected spaces at 400× magnification in each well. Every well was studied at least 3 times (n = 6 in each group).
Western Blot Analysis
Bone-marrow extracts or cell lysates from EPCs were mixed with sample loading buffer and separated under reducing conditions on 10% SDS-polyacrylamide gel, then incubated with the antibody rabbit anti-per2 (Santa Cruz Biotechnology), anti-PI3k, rabbit anti-Akt or anti-phosphorylated-Akt (p-Akt, pSer473), or rabbit anti-ERK or p-ERK (all Cell Signaling Technology). Protein and phosphorylation levels were normalized to that of β-actin (mouse-antiβ-actin, Kangchen Biotech) and baseline expression.
Statistical Analysis
Data are expressed as mean ± SEM. SPSS for Windows v16.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Comparisons between 2 groups involved Student's t test and more than 2 groups, one-way ANOVA, followed by least significant difference test (with equal variances assumed) or Dunnett's T3 test (with equal variances not assumed). P<0.05 was considered statistically significant.
Results
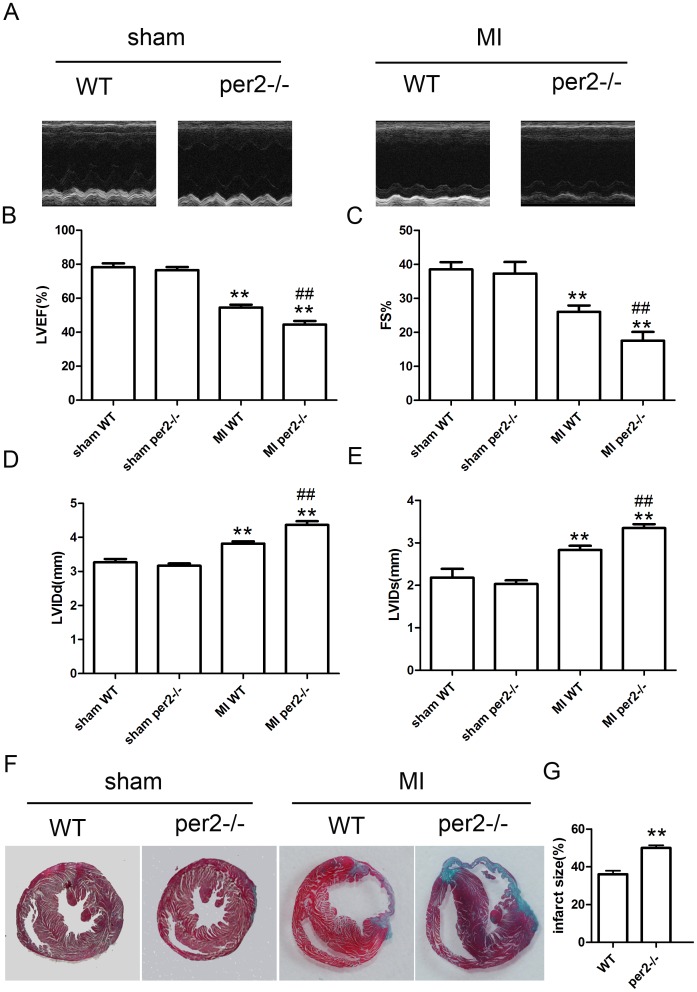
Per2 deficiency decreased cardiac function and increased infarct size in mice with MI
We surgically induced myocardial ischemia in per2−/− and background-matched WT mice. At 4 weeks after MI, mice showed decreased cardiac function (Fig. 1A–E), with cardiac function worse for per2−/− than WT mice. Infarct size was larger for per2−/− than WT mice (Fig. 1F–G).
Figure 1. Left ventricular remodeling and infarct size in wild-type (WT) and Period 2-deficient (per2−/−) mice after myocardial infarction (MI).
(A) Representative M-mode images of papillary muscles. (B–E) Systolic dysfunction 4 weeks after acute MI in mice (** p<0.01 vs sham-operated, ## p<0.01 vs MI WT). (F) Representative Masson's trichrome staining at 28 days after MI. (G) Quantitative analysis of infarct area (** p<0.01 vs WT). LVEF, left-ventricular ejection fracton; FS, fractional shortening; LVIDd, LV internal dimension diastolic; LVIDs, LV internal dimension systolic.
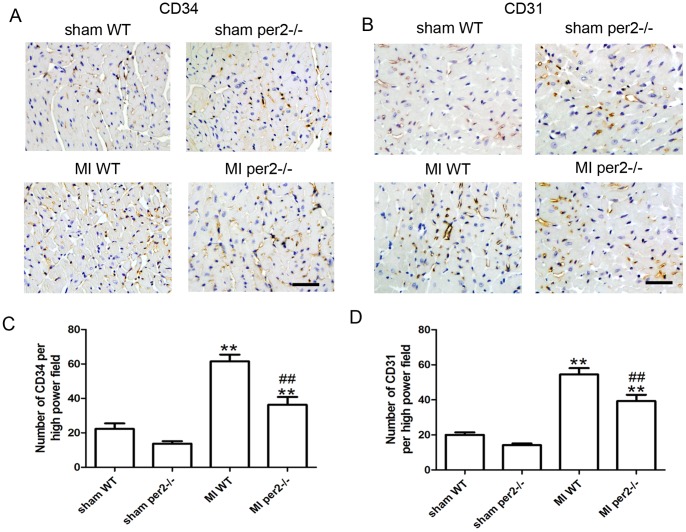
Per2 deficiency decreased the number of CD34+ cells and capillary density in the myocardium 4 weeks after MI
Because EPCs contribute to angiogenesis [1]–[4], we compared the number of CD34+ cells and capillary density in the ischemic heart in WT and per2−/− mice. CD34+ cells and capillary density was lower in per2−/− than WT mice at 4 weeks after MI (Fig. 2). Per2−/− increased the MI area and decreased heart function in part by decreasing EPC angiogenesis.
Figure 2. Per2−/− decreased the number of CD34+ progenitors and capillary density in mice.
(A) Representative immunostaining of CD34 to identify progenitors and (B) CD31 to identify capillaries. Original magnification: 400×. Quantitative analysis of (C) CD34+ cells and (D) capillary density (** p<0.01 vs sham-operated, ## p<0.01 vs MI WT).
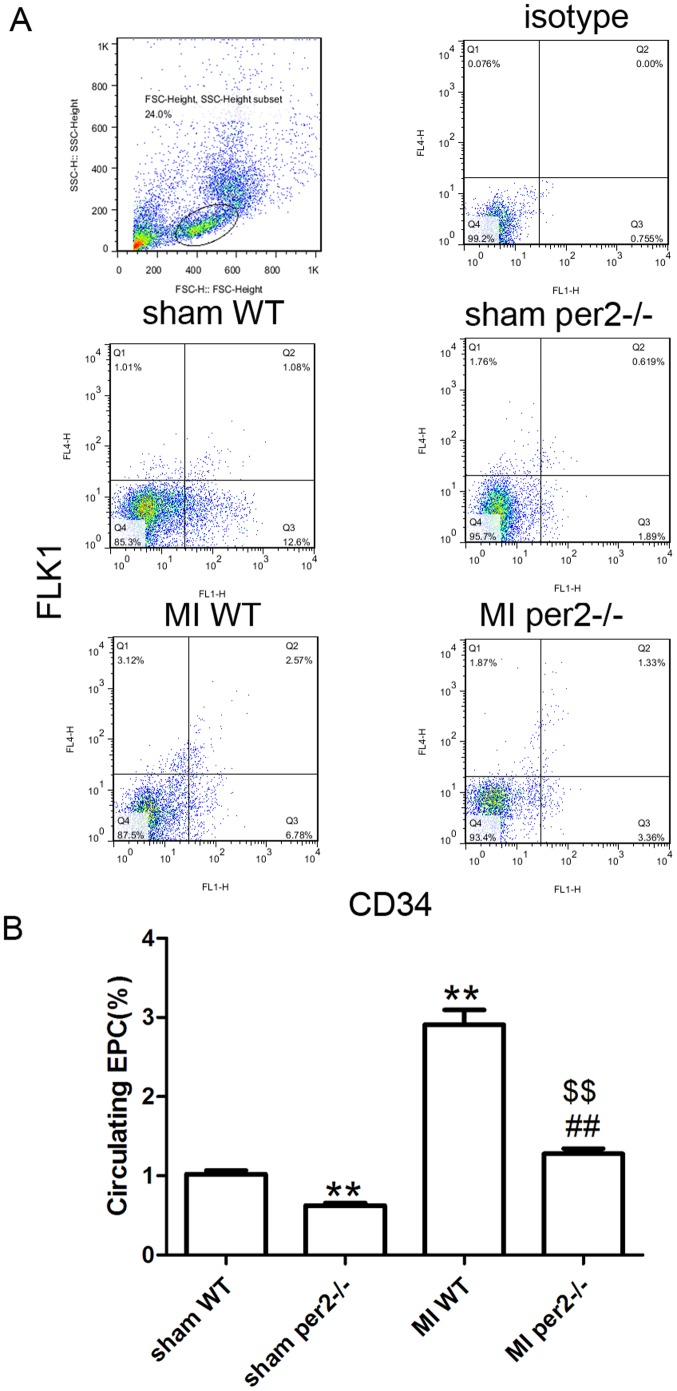
Per2 deficiency inhibits ischemia-induced EPC mobilization
Because angiogenesis after MI depends in part on EPC mobilization, we investigated the effect of per2 on EPC mobilization in response to tissue ischemia by determining CD34+ Flk-1+ cells in peripheral blood by flow cytometry. Basal circulating EPC number was lower in per2−/− than WT mice (Fig. 3A and B). Consistent with previous findings that tissue ischemia can induce EPC mobilization [28], EPC mobilization was enhanced 3 days after MI in WT mice. In WT mice, the EPC level was increased nearly three-fold that in sham-operated mice after MI (Fig. 3A and B) but in per2−/− mice was increased two-fold that in sham-operated mice, which suggests that per2−/− inhibited bone-marrow EPC mobilization after MI.
Figure 3. Per2−/− decreased the number of CD34+ Flk-1+ progenitors in blood of mice before and after MI.
(A) Representative flow cytometry data of CD34+ Flk-1+ cells, considered EPCs, within the mononuclear cell population. (B) Quantitative evaluation of EPCs (** p<0.01 vs sham-operated WT, ## p<0.01 vs sham-operated per2−/−, $$ p<0.01 vs MI WT).
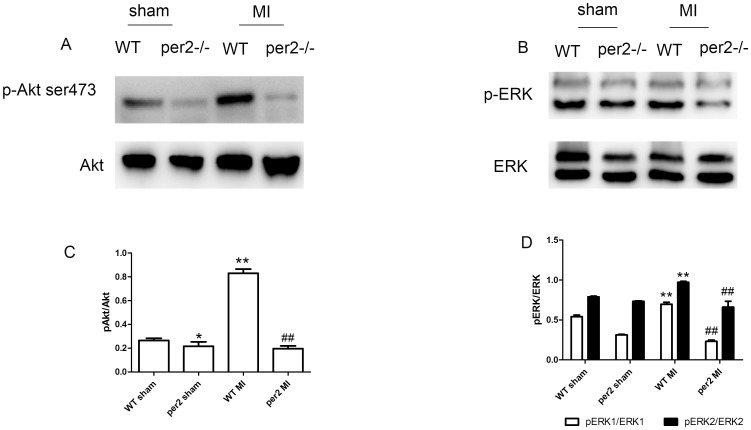
Per2 deficiency inhibited bone-marrow EPC mobilization 3 days after MI by inhibiting Akt and ERK signaling
We evaluated the possible mechanisms of per2 affecting bone-marrow EPC mobilization. At 3 days after MI, the bone-marrow environment was changed. Phosphorated Akt and ERK levels were increased both in WT and per2−/− mice, with weaker Akt and ERK phosphorylation in per2−/− bone marrow (Fig. 4A–D).
Figure 4. Effect of acute MI on expression of Akt and ERK in mouse bone marrow.
Western blot analysis of phosphorylated and total (A) Akt and (B) ERK levels. Quantitative analysis of (C) p-Akt (* p<0.05, ** p<0.01 vs WT sham-operated, ## p<0.01 vs WT MI) and (D) p-ERK (** p<0.01 vs WT sham-operated, ## p<0.01 vs WT MI).
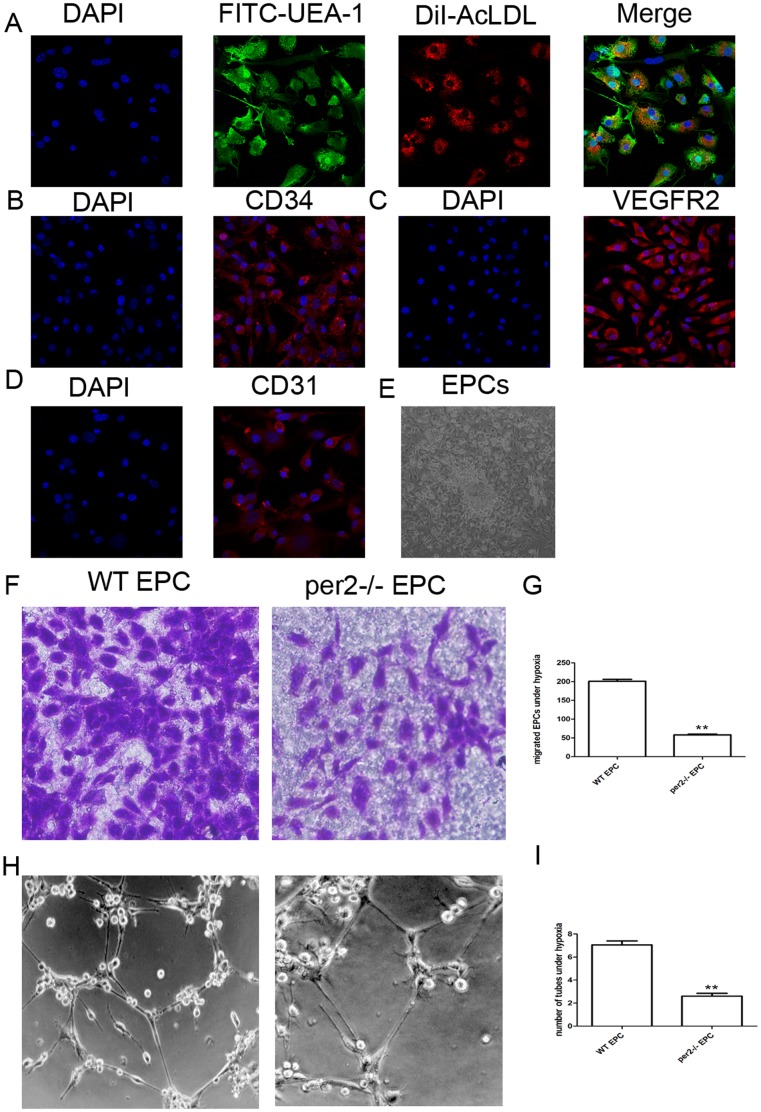
Characterization of bone-marrow–derived EPCs
Early EPCs were isolated from bone-marrow mononuclear cells of WT and per2−/− mice. In brief, after 7 days of culture in the presence of endothelial growth medium,>90% of cells were capable of cellular uptake of DiI-AcLDL and FITC-UEA-1 binding (Fig. 5A). Most of the cells expressed CD34 and Flk1 and some expressed CD31 (Fig. 5B–D). EPCs with phase contrast imaging is shown in Fig. 5E.
Figure 5. Characterization of cultured EPCs and the effect of per2 on EPC function under hypoxia.
(A) Fluorescence microscopy of adherent cells at day 7 after bone-marrow isolation with Dil-Ac-LDL staining and endothelial-specific lectin-FITC binding. (B) The expression of CD34, (C) vascular endothelial growth factor receptor 2 (Flk-1) and (D) CD31 in EPCs. (E) EPCs with phase-contrast imaging. (F) EPC migration evaluated by transwell assay under hypoxia. (G) Quantitative analysis of EPC migration (** p<0.01 s WT EPCs). (H) Tube formation of EPCs detected by matrigel tube-formation assay. (I) Quantitative analysis of EPC tube formation (** p<0.01 vs WT EPCs).
Per2 deficiency inhibited EPC function induced by hypoxia
WT or per2−/− EPCs were cultured under normal or hypoxia environment for 24 hr. Hypoxia upregulated EPC function. As compared with WT EPCs, per2−/− EPCs showed weaker migration and tube formation under hypoxia (Fig. 5F–I).
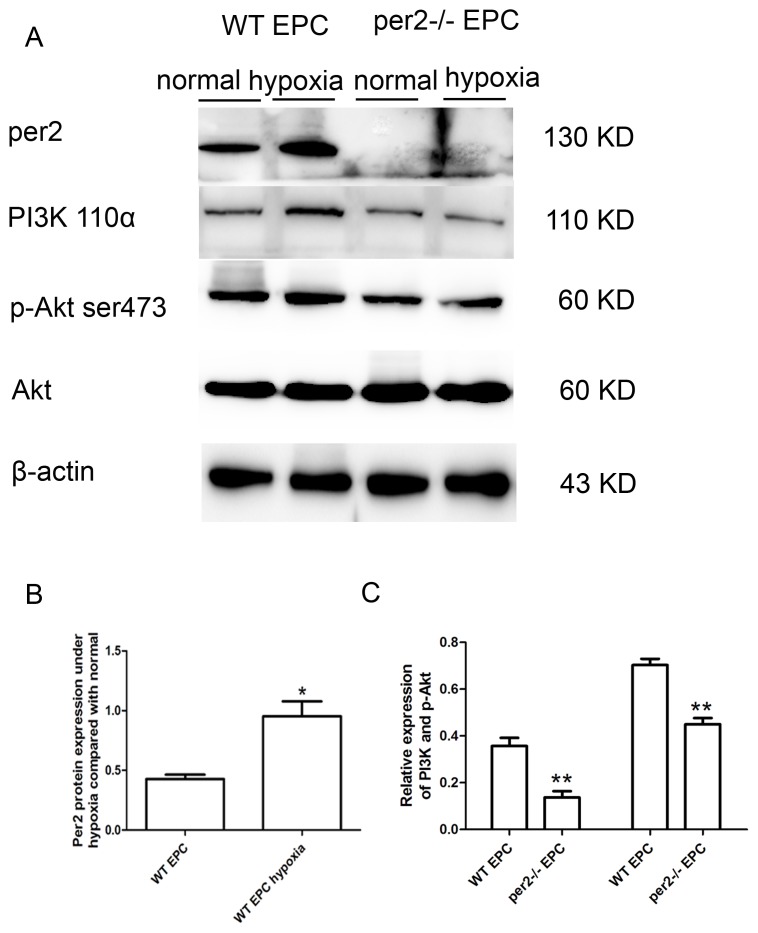
Per2 deficiency decreased PI3K and phosphorylated Akt levels induced by hypoxia in EPCs
To investigate the mechanism of per2 affecting EPC function under hypoxia, we studied per2 protein level in WT and per2−/− EPCs. In WT EPCs, per2 protein level was increased with hypoxia (Fig. 6A and B). We investigated EPC function-related signaling and found activated PI3K/Akt signaling in WT EPCs under hypoxia (Fig. 6A and C), with reduced signaling in per2−/− mice EPCs.
Figure 6. Per2−/− decreased the expression of PI3K and Akt in EPCs under hypoxia.
(A) Hypoxia induced the expression of per2 and per2−/− decreased the expression of PI3K and Akt under hypoxia. Quantitative analysis of (B) per2 (* p<0.05 vs WT EPCs), (C) PI3K and p-Akt expression under hypoxia (** p<0.01 vs WT EPCs).
Discussion
In this study, we focused on the role of the circadian gene per2 in mobilization and function of EPCs under hypoxia in vitro and after MI in mice. Per2−/− mice with MI showed attenuated heart function, increased MI area and decreased angiogenesis. In addition, per2−/− mice showed down regulated Akt and ERK expression in bone marrow, which reduced the mobilization of EPCs in response to acute ischemia. In vitro studies further demonstrated that per2−/− suppressed EPC migration and tube-forming capacity under a hypoxic microenvironment. Hypoxia increased the expression of per2 in WT EPCs, which activated PI3K/Akt signaling but was counteracted by per2 knockout. Per2 may play an important role in regulating EPC mobilization and EPC function activity after MI, which is important for recovery.
Ischemic tissue neovascularization requires not just angiogenesis but also circulating EPCs during vasculogenesis [27]. These circulating EPCs are derived from bone marrow and are mobilized in response to tissue ischemia [27]. An inadequate angiogenic response to ischemia in the myocardium of patients might result in poor collateral formation and severe organ damage [28]–[30].
EPCs were recognized to have dual profiles of immature cells, stem or progenitor cells and endothelial-lineage cells in terms of marker expression from peripheral blood or bone marrow mononuclear cells: CD34/Flk-1[31], Sca-1/Flk-1[32], CXCR4/Flk-1 [33], and Flk-1/VE-cadherin [34]. However, the cell-surface marker-based definition of EPCs is still controversial. Here, we analyzed CD34+ Flk1+ cells as a marker of circulating EPCs. Before and after MI, the number of CD34+ Flk1+ EPCs was lower in per2−/− than WT mouse blood. In our previous study [35], we found weaker proliferation of per2−/− than WT EPCs, which explains the decreased number of EPCs before MI.
Evidence from animal studies has been reproduced in studies of EPC mobilization in patients recovering from burns, coronary artery bypass graft surgery, or acute MI [36]. In addition, experiments performed in a mouse bone-marrow transplant model indicated that the incorporation of bone-marrow–derived EPCs into the foci of ocular neovascularization after corneal micropocket surgery was greater in mice with hind-limb ischemia than non-ischemic mice [34]. Thus, the mobilization of bonemarrowderived EPCs appears to be a natural response to tissue ischemia, and the mobilized cells become incorporated into sites of vessel growth.
Per2 has been found a regulator of EPC mobilization induced in hind-limb ischemia [37]. To investigate the reasons for the fewer number of EPCs after MI in per2−/− than WT mice, we studied the mechanisms of EPC mobilization after MI in WT and per2−/− mice. The number of circulating EPCs was linked to alterations in bone-marrow molecular pathways known to be involved in EPC mobilization. Phosphorylated ERK [38]–[41] and Akt [42] signaling plays important roles in bone-marrow EPC mobilization. Here we observed attenuated ERK and Akt signaling in per2−/− mouse bone marrow. The inhibition of ERK and Akt signaling in per2−/− mice led to decreased EPC mobilization.
After MI, bone-marrow derived EPCs incorporated into sites of neovascularization at the border of the infarct area [43] and neoangiogenesis after EPC transplantation improved myocardial blood flow, function and remodeling [44]. Therefore, reduced circulating EPCs early after MI by per2 deficiency likely contributed to decreased capillary density in the peri-infarct area, thus leading to impaired cardiac remodeling and function 28 days post-infarction. In our former investigation [35], DiI-labelled bone marrow derived WT and per2−/− EPCs cultured in vitro were injected into mouse myocardium after MI. At 4 weeks, the number of DiI-labelled per2−/− EPCs was lower than that of WT EPCs in the MI myocardium. Decreased number of CD34+ cells in the per2−/− myocardium combined with our former result also led to the weaker angiogenesis.
Bone-marrow–derived adherent cells exhibiting endothelial characteristics such as acetylated low density lipoprotein uptake and lectin binding have been considered cultured EPCs [45]. These cells are positive for CD34, Flk1 and CD31. To study the effect of per2 on EPC function under hypoxia, we cultured EPCs in vitro and compared EPC function under hypoxia. Hypoxia for 24 hr increased the migration and tube formation of EPCs as compared with per2−/− EPCs. Our finding agrees with previous investigations [46]–[48]. In the Hoffmann et al. study, hypoxia could increase VEGF-A expression in endothelial cells, which led to enhanced tube formation, and similar results were found in EPCs. In the Kanzler et al. study, hypoxia upregulated CXCR4 and VEGF, thus improving EPC migration and tube formation. In the Yuyu et al. study, hypoxia induced phosphorylation of Akt in EPCs [49]. In the Tobias et al. study, PER2 transcript and protein levels were increased in cardiac tissue of patients with ischemic heart disease. Here, we found increased per2 protein level in EPCs under hypoxia.
Activation of PI3K/Akt signaling was regulated by per2, which was induced by ischemia. However, activation of PI3K/Akt signaling was inhibited in per2−/− EPCs. Therefore, per2 may be a regulator of activation of PI3K/Akt signaling in EPCs under hypoxia. The PI3K/Akt pathway is essential to EPC mobilization, migration, proliferation, and survival [50], so the altered EPC migration and tube formation under hypoxia may depend on activation of PI3K/Akt. In vitro hypoxic studies of EPCs are a good explanation for the weak angiogenesis in the per2−/− myocardium after MI.
In conclusion, per2 deficiency aggravates the MI may in part be through decreased EPC bone-marrow mobilization and inhibited EPC function activity.
Supporting Information
Western blot analysis (A) of per2 levels. (B) Quantitative analysis of per2 (** p<0.01 vs WT sham-operated). (C) Representative immunostaining of CD68 (macrophages, 1∶100) in the heart tissue.
(TIF)
Acknowledgments
This study was supported by the National 973 Basic Research Program of China (no. 2012CB518603), National Natural Science Foundation of China (nos. 30873325, 81100103, 81173251, 81302939), Natural Science Foundation of Shandong Province (nos. ZR2011HQ020, ZR2009CM049), postdoctoral special foundation for innovative projects of Shandong Province (no. 201103049) and promotive research fund for excellent young and middle-aged scientists of Shandong Province (no. BS2013YY015).
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by the National 973 Basic Research Program of China (no. 2012CB518603), National Natural Science Foundation of China (no's. 30873325, 81100103, 81173251, 81302939), Natural Science Foundation of Shandong Province (no's. ZR2011HQ020, ZR2009CM049), postdoctoral special foundation for innovative projects of Shandong Province (No. 201103049) and promotive research fund for excellent young and middle-aged scientists of Shandong Province (BS2013YY015). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Shintani S, Murohara T, Ikeda H, Ueno T, Honma T, et al. (2001) Mobilization of endothelial progenitor cells in patients with acute myocardial infarction. Circulation 103: 2776–2779. [DOI] [PubMed] [Google Scholar]
- 2. Brenner W, Aicher A, Eckey T, Massoudi S, Zuhayra M, et al. (2004) 111In-labeled CD34+ hematopoietic progenitor cells in a rat myocardial infarction model. J Nucl Med 45: 512–518. [PubMed] [Google Scholar]
- 3. Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, et al. (1999) Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res 85: 221–228. [DOI] [PubMed] [Google Scholar]
- 4. Li B, Sharpe EE, Maupin AB, Teleron AA, Pyle AL, et al. (2006) VEGF and PlGF promote adult vasculogenesis by enhancing EPC recruitment and vessel formation at the site of tumor neovascularization. FASEB J 20: 1495–1497. [DOI] [PubMed] [Google Scholar]
- 5. Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, et al. (1997) Isolation of putative progenitor endothelial cells for angiogenesis. Science 275: 964–967. [DOI] [PubMed] [Google Scholar]
- 6. Leone AM, Rutella S, Bonanno G, Abbate A, Rebuzzi AG, et al. (2005) Mobilization of bone marrow-derived stem cells after myocardial infarction and left ventricular function. Eur Heart J 26: 1196–1204. [DOI] [PubMed] [Google Scholar]
- 7. Prasad A, Stone GW, Stuckey TD, Costantini CO, Zimetbaum PJ, et al. (2005) Impact of diabetes mellitus on myocardial perfusion after primary angioplasty in patients with acute myocardial infarction. J Am Coll Cardiol 45: 508–514. [DOI] [PubMed] [Google Scholar]
- 8. Shantsila E, Watson T, Lip GY (2007) Endothelial progenitor cells in cardiovascular disorders. J Am Coll Cardiol 49: 741–752. [DOI] [PubMed] [Google Scholar]
- 9. Kissel CK, Lehmann R, Assmus B, Aicher A, Honold J, et al. (2007) Selective functional exhaustion of hematopoietic progenitor cells in the bone marrow of patients with postinfarction heart failure. J Am Coll Cardiol 49: 2341–2349. [DOI] [PubMed] [Google Scholar]
- 10. Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, et al. (2003) Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med 348: 593–600. [DOI] [PubMed] [Google Scholar]
- 11. Chironi G, Walch L, Pernollet MG, Gariepy J, Levenson J, et al. (2007) Decreased number of circulating CD34+KDR+ cells in asymptomatic subjects with preclinical atherosclerosis. Atherosclerosis 191: 115–120. [DOI] [PubMed] [Google Scholar]
- 12. Kocher AA, Schuster MD, Szabolcs MJ, Takuma S, Burkhoff D, et al. (2001) Neovascularization of ischemic myocardium by human bonemarrow- derived angioblasts prevents cardiomyocyte apoptosis, reduces remodeling and improves cardiac function. Nat Med 7: 430–436. [DOI] [PubMed] [Google Scholar]
- 13. Loomans CJ, de Koning EJ, Staal FJ, Rookmaaker MB, Verseyden C, et al. (2004) Endothelial progenitor cell dysfunction: a novel concept in the pathogenesis of vascular complications of type 1 diabetes. Diabetes 53: 195–199. [DOI] [PubMed] [Google Scholar]
- 14. Hansen J, Lassen CF (2014) Shift work and risk of cancer and coronary heart diseases. Ugeskr Laeger 176: 146–149. [PubMed] [Google Scholar]
- 15. Sato M, Matsuo T, Atmore H, Akashi M (2014) Possible contribution of chronobiology to cardiovascular health. Front Physiol 4: 409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Maemura K (2013) Circadian rhythm and ischemic heart disease. Nihon Rinsho 71: 2124–2129.. [PubMed] [Google Scholar]
- 17. Pan X, Jiang XC, Hussain MM (2013) Impaired cholesterol metabolism and enhanced atherosclerosis in clock mutant mice. Circulation 128: 1758–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Muller JE (1999) Circadian variation and triggering of acute coronary events. Am Heart J 137: S1–S8. [DOI] [PubMed] [Google Scholar]
- 19. Lamont EW, James FO, Boivin DB, Cermakian N (2007) From circadian clock gene expression to pathologies. Sleep Med 8: 547–556. [DOI] [PubMed] [Google Scholar]
- 20. Yue X, Yu H, Lin X, Liu K, Wang X, et al. (2013) Investigation into the optimal surgical conditions for coronary artery ligation for establishing a myocardial infarction model in mice. Exp Ther Med 6: 341–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kido M, Du L, Sullivan CC, Li X, Deutsch R, et al. (2005) Hypoxia-inducible factor 1-alpha reduces infarction and attenuates progression of cardiac dysfunction after myocardial infarction in the mouse. J Am Coll Cardiol 46: 2116–2124. [DOI] [PubMed] [Google Scholar]
- 22. Eirin A, Zhu XY, Woollard JR, Herrmann SM, Gloviczki ML, et al. (2013) Increased circulating inflammatory endothelial cells in blacks with essential hypertension. Hypertension 62: 585–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Riegersperger M, Plischke M, Steiner S, Seidinger D, Sengoelge G, et al. (2013) Effect of conversion from ciclosporin to tacrolimus on endothelial progenitor cells in stable long-term kidney transplant recipients. Transplantation 95: 1338–1345. [DOI] [PubMed] [Google Scholar]
- 24. Massot A, Navarro-Sobrino M, Penalba A, Arenillas JF, Giralt D, et al. (2013) Decreased levels of angiogenic growth factors in intracranial atherosclerotic disease despite severity-related increase in endothelial progenitor cell counts. Cerebrovasc Dis 35: 81–88. [DOI] [PubMed] [Google Scholar]
- 25. Krishnamurthy P, Thal M, Verma S, Hoxha E, Lambers E, et al. (2011) Interleukin-10 deficiency impairs bone marrow-derived endothelial progenitor cell survival and function in ischemic myocardium. Circ Res 109: 1280–1289.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Heeschen C, Aicher A, Lehmann R, Fichtlscherer S, Vasa M, et al. (2003) Erythropoietin is a potent physiologic stimulus for endothelial progenitor cell mobilization. Blood 102: 1340–1346. [DOI] [PubMed] [Google Scholar]
- 27. Murayama T, Tepper OM, Silver M, Ma H, Losordo DW, et al. (2002) Determination of bone marrow-derived endothelial progenitor cell significance in angiogenic growth factor-induced neovascularization in vivo. Exp Hematol 30: 967–972. [DOI] [PubMed] [Google Scholar]
- 28. Kuliczkowski W, Derzhko R, Prajs I, Podolak-Dawidziak M, Serebruany VL (2012) Endothelial progenitor cells and left ventricle function in patients with acute myocardial infarction: potential therapeutic considertions. Am J Ther 19: 44–50. [DOI] [PubMed] [Google Scholar]
- 29. António N, Fernandes R, Soares A, Soares F, Lopes A, et al. (2014) Reduced levels of circulating endothelial progenitor cells in acute myocardial infarction patients with diabetes or pre-diabetes: accompanying the glycemic continuum. Cardiovasc Diabetol 13: 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Porto I, De Maria GL, Leone AM, Dato I, D'Amario D, et al. (2013) Endothelial progenitor cells, microvascular obstruction, and left ventricular remodeling in patients with ST elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol 112: 782–791. [DOI] [PubMed] [Google Scholar]
- 31. Iwakura A, Luedemann C, Shastry S, Hanley A, Kearney M, et al. (2003) Estrogen-mediated, endothelial nitric oxide synthase-dependent mobilization of bone marrow-derived endothelial progenitor cells contributes to reendothelialization after arterial injury. Circulation 108: 3115–3121. [DOI] [PubMed] [Google Scholar]
- 32. Gallagher KA, Liu ZJ, Xiao M, Chen H, Goldstein LJ, et al. (2007) Diabetic impairments in NO-mediated endothelial progenitor cell mobilization and homing are reversed by hyperoxia and SDF-1 alpha. J Clin Invest 117: 1249–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nakajima M, Ogawa M, Shimoda Y, Hiraoka S, Iida M, et al. (2006) Presenilin-1 controls the growth and differentiation of endothelial progenitor cells through its beta-catenin-binding region. Cell Biol Int 30: 239–243. [DOI] [PubMed] [Google Scholar]
- 34. Takahashi T, Kalka C, Masuda H, Chen D, Silver M, et al. (1999) Ischemia and cytokine-induced mobilization of bone marrow-derived endothelial progenitor cells for neovascularization. Nat Med 5: 434–438. [DOI] [PubMed] [Google Scholar]
- 35. Sun YY, Bai WW, Wang B, Lu XT, Xing YF, et al. (2014) Period 2 is essential to maintain early endothelial progenitor cell function in vitro and angiogenesis after myocardial infarction in mice. J Cell Mol Med 18: 907–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shintani S, Murohara T, Ikeda H, Ueno T, Honma T, et al. (2001) Mobilization of endothelial progenitor cells in patients with acute myocardial infarction. Circulation 103: 2776–2779. [DOI] [PubMed] [Google Scholar]
- 37. Wang CY, Wen MS, Wang HW, Hsieh IC, Li Y, et al. (2008) Increased vascular senescence and impaired endothelial progenitor cell function mediated by mutation of circadian gene Per2. circulation 118: 2166–2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Heissig B, Hattori K, Dias S, Friedrich M, Ferris B, et al. (2002) Recruitment of stem and progenitor cells from the bone marrow niche requires MMP-9 mediated release of kit-ligand. Cell 109: 625–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Moon SK, Cha BY, Kim CH (2004) ERK1/2 mediates TNF-alpha-induced matrix metalloproteinase-9 expression in human vascular smooth muscle cells via the regulation of NF-kappaB and AP-1: involvement of the ras dependent pathway. J Cell Physiol 198: 417–427. [DOI] [PubMed] [Google Scholar]
- 40. Chung TW, Lee YC, Kim CH (2004) Hepatitis B viral HBx induces matrix metalloproteinase-9 gene expression through activation of ERK and PI-3K/AKT pathways: involvement of invasive potential. FASEB J 18: 1123–1125. [DOI] [PubMed] [Google Scholar]
- 41. Tanimura S, Asato K, Fujishiro SH, Kohno M (2003) Specific blockade of the ERK pathway inhibits the invasiveness of tumor cells: down- regulation of matrix metalloproteinase-3/-9/-14 and CD44. Biochem Biophys Res Commun 304: 801–806. [DOI] [PubMed] [Google Scholar]
- 42. Zhou J, Cheng M, Liao YH, Hu Y, Wu M, et al. (2013) Rosuvastatin enhances angiogenesis via eNOS-dependent mobilization of endothelial progenitor cells. PLoS One 8: e63126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, et al. (1999) Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological revascularization. Circ Res 85: 221–228. [DOI] [PubMed] [Google Scholar]
- 44. Kocher AA, Schuster MD, Szabolcs MJ, Takuma S, Burkhoff D, et al. (2001) Neovascularization of ischemic myocardium by human bone-marrow-derived angioblasts prevents cardiomyocyte apoptosis, reduces remodeling and improves cardiac function. Nat Med 7: 430–436. [DOI] [PubMed] [Google Scholar]
- 45. Huang Po-Hsun, Chen Yung-Hsiang, Wang Chao-Hung, Chen Jia-Shiong, Tsai Hsiao-Ya (2009) Matrix Metalloproteinase-9 Is Essential for Ischemia-Induced Neovascularization by Modulating Bone Marrow -Derived Endothelial Progenitor Cells. Arterioscler Thromb Vasc Biol 29: 1179–1184. [DOI] [PubMed] [Google Scholar]
- 46. Hoffmann BR, Wagner JR, Prisco AR, Janiak A, Greene AS (2013) Vascular endothelial growth factor-A signaling in bone marrow-derived endothelial progenitor cells exposed to hypoxia stress. Physiol Genomics 45: 1021–1034.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kanzler I, Tuchscheerer N, Steffens G, Simsekyilmaz S, Konschalla S, et al. (2013) Differential role of angiogenic chemokines in endothelial progenitor cell-induced angiogenesis. Basic Res Cardiol 108: 310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yao Y, Sheng Z, Li Y, Yan F, Fu C, et al. (2012) Tissue Kallikrein Promotes Cardiac Neovascularization by Enhancing Endothelial Progenitor Cell Functional Capacity. HUMAN GENE THERAPY 23: 859–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Eckle T, Hartmann K, Bonney S, Reithel S, Mittelbronn M, et al. (2012) Adora2b-elicited Per2 stabilization promotes a HIF-dependent metabolic switch critical for myocardial adaptation to ischemia. Nat Med 18: 774–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Llevadot J, Murasawa S, Kureishi Y, Uchida S, Masuda H, et al. (2001) HMG- CoA reductase inhibitor mobilizes bone marrow–derived endothelial progenitor cells. J Clin Invest 108: 399–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Western blot analysis (A) of per2 levels. (B) Quantitative analysis of per2 (** p<0.01 vs WT sham-operated). (C) Representative immunostaining of CD68 (macrophages, 1∶100) in the heart tissue.
(TIF)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.