Abstract
The goal of postmastectomy breast reconstruction is to restore a woman’s body image and to satisfy her personal expectations regarding the results of surgery. Studies in other surgical areas have shown that unrecognized or unfulfilled expectations may predict dissatisfaction more strongly than even the technical success of the surgery. Patient expectations play an especially critical role in elective procedures, such as cancer reconstruction, where the patient’s primary motivation is improved health-related quality of life. In breast reconstruction, assessment of patient expectations is therefore vital to optimal patient care. This report summarizes the existing literature on patient expectations regarding breast reconstruction, and provides a viewpoint on how this field can evolve. Specifically, we consider how systematic measurement and management of patient expectations may improve patient education, shared medical decision-making and patient perception of outcomes.
Keywords: breast cancer, breast reconstruction, expectations, health-related quality of life, patient education, satisfaction
Currently, with the exception of skin malignancy, breast cancer is the most commonly diagnosed cancer among women. Over 250,000 women in the USA alone were diagnosed with breast cancer in 2009, with nearly 60,000 (or 25%) of these women undergoing mastectomy [1]. Increased awareness and changing attitudes toward breast reconstruction, among both patients and referring physicians, have led an increasing number of women to seek breast reconstruction after mastectomy.
The primary goal of breast reconstruction is to improve a woman’s body image and to fulfil her expectations regarding the appearance of her breasts following surgery. Research in other areas of surgery have demonstrated that unrecognized or unfulfilled expectations are more closely associated with dissatisfaction than is the technical success of the surgery [2]. In breast reconstruction, such expectations are particularly important, as surgery is directed toward a restoration or improvement in breast form as perceived by the patient [3]. Therefore, it is important that reconstructive surgeons fully appreciate and address individual patient expectations prior to surgery.
Exploring individual patients’ expectations may allow surgeons to recognize those patients who have unrealistic expectations, in order to address patients’ misconceptions preoperatively through improved patient education. When various surgical options exist, shared decision-making may be enhanced by a careful exploration of a patient’s expectations. Such delineation of appropriate expectations may also be helpful to further document the informed consent process [4]. While medical care experts advocate precise ascertainment of patient expectations [4], there have not previously been questionnaires available for breast reconstruction patients that can be used to systematically measure such expectations.
This special report describes the existing literature on the topic of patient expectations in breast reconstruction, and how research in the field may develop over time. More specifically, we consider how measuring patient expectations might provide information useful in the context of patient education and shared medical decision-making.
Expectancy theory
Expectations have long been recognized as an important predictor of health outcomes within psychosocial research. Expectations play a central role in several prominent theories of health behavior, including expectancy-value theories, such as Bandura’s social-cognitive theory [5] and the theories of reasoned action and planned behavior [6], as well as Kirsch’s response expectancy theory [7]. Expectancy-value theories are primarily concerned with how an individual’s beliefs influence behavior. Such beliefs include outcome expectancies and self-efficacy beliefs. By contrast, response expectancy theory is concerned with the influence of expectancies on nonvolitional outcomes, such as emotions, pain or pleasure, and has been used to explain phenomena such as placebo effects of medication and psychotherapy. Theories of expectations have also been developed within marketing and health services research, as expectations are believed to play a central role in determining patients’ perceptions of, and satisfaction with, health services. For example, the expectancy-disconfirmation theory contends that satisfaction is the result of a comparison between prior expectations and perceptions of the actual product or outcome [8], such that the greater the divergence between the two, the more apparent the (dis)satisfaction.
Thompson and Suñol outline four types of expectation: ideal expectations, which refer to the patients’ desired outcome; predicted expectations, which refer to the patients’ anticipated outcome; normative expectations, which represent what should or ought to be the outcome; and unformed expectations, which occur when patients are unwilling or unable to articulate expectations [8]. These authors have suggested an updated theory that integrates expectancy-disconfirmation theory with other theories of expectations, including Kirsch’s response expectancy theory [7], and elements of Festinger’s theory of cognitive dissonance [9], and accounts for the psychological adjustments people make in coming to terms with disconfirmed expectancies. Specifically, the authors suggest a ‘zone of tolerance’, in which objective outcomes will generally be perceived as satisfactory when they fall in the zone between normative and minimum predicted expectations. This is due to assimilation effects – the tendency for individuals to shift their perceptions towards their expectations when there is only a small difference between the two. Outside the zone of tolerance, when predicted expectations are well above the objective outcome dissatisfaction will be high, and when predicted expectations are well below objective outcomes satisfaction will be high. The model hypothesizes that maximum satisfaction occurs where ideal expectation levels are reached. Empirical data exist to support elements of this theory [10,11], but the complete integrated model still needs further empirical investigation. Although our current study will not test this theory, the model is used to guide the qualitative interviews and inform measurement development.
Marketing-based theories, such as expectancy-disconfirmation theory [8], are particularly helpful for understanding the importance of preoperative expectations among breast reconstruction patients as they contend that satisfaction is the result of a comparison between prior expectations and perceptions of the actual outcome [8]. When expectations are greater than the perception of the outcome, dissatisfaction is likely to occur, with greater divergence between the two leading to greater dissatisfaction. Thus, in the context of breast reconstruction, surgeons who create inappropriately high expectations for their patients, or who fail to modify unrealistic expectations that patients bring to the situation, may inadvertently set patients up for dissatisfaction. Although a divergence on the positive end – with the outcome exceeding expectations – is unlikely to create dissatisfaction, surgeons who set expectations too low may discourage patients from undergoing reconstructive surgery or may cause unnecessary anxiety.
Appreciating individual patient expectations within such theoretical models allows surgeons to recognize patients who have unrealistic expectations and address their issues preoperatively. It is also important to note that patients can derive information from a variety of sources: the internet, television, literature, nurses, patient-care coordinators and other patients, to name a few. These sources can be misleading, however; for example, plastic surgeons who advertise heavily may exhibit photographs of their best postoperative results, setting unrealistically high expectations for patients. Subsequently, such pre-existing beliefs and conceptions about breast reconstruction may be very difficult to reconfigure. The impact of these ‘nontraditional information sources’ has recently been considered by Smith-McLallen and colleagues within the context of expectancy-value theory and an integrative model of behavior prediction [12]. For most patients, the most important source of knowledge remains their surgeon. Despite this, in a busy practice, most surgeons are forced to limit their patient consultations to discussions about surgical options and potential problems. Ironically, surgeons may find that their patients are less well-prepared for common events that constitute normal postoperative healing.
Patient expectations in healthcare
Outside of breast reconstruction, the relationship between patient expectations, satisfaction and health-related quality of life (HR-QoL) has been examined across a variety of patient populations. For example, in primary care, realistic patient expectations have been found to be associated with higher satisfaction with care and compliance with medical advice [13]. Similarly, in a study of cancer patients, those that expected to be cured were more likely to follow the treatment recommendations of their oncologist [14]. Interestingly, researchers have noted that expectations may vary by race. In a study of primary care patients, Guerra et al. found that in the USA, African–Americans were more likely than Caucasian patients to expect complete physical examinations, referral to a specialist and for the doctor to be familiar with their medical records [13]. The authors suggest that these differences in expectations may relate to patient factors such as knowledge about (e.g., cultural beliefs) and experience with symptoms and health conditions. They also consider when the differential treatment of African–Americans and other minorities by the medical profession may cause them to have higher expectations for their physicians to do more, because they assume that this is what white patients receive. In other words, African–Americans may develop and express higher expectations as a way of protecting themselves against past and potential discrimination.
Numerous studies in surgical areas substantiate the notion that preoperative expectations play an important role in patient assessment of results and are strongly predictive of both satisfaction and HR-QoL [2,15–25]. For example, in cardiac surgery, positive expectations about life after heart transplantation have been associated with better postoperative scores for mood, adjustment to illness and HR-QoL, even among patients who experienced health setbacks [26]. In patients who underwent a bone marrow transplant, discordance between preoperative expectations about how long it would take to return to normal activities and postoperative functional status has been associated with greater postoperative psychological distress [27]. In urology, men undergoing trans-urethral resection of the prostate, who had positive preoperative expectations, were more likely to report improvements in health 3 months after surgery [28]. Furthermore, in patients who underwent surgery for sciatica, those that had favorable expectations about surgery had better outcomes than patients with unfavorable expectations [20]. Across these various patient groups, the uniform finding has been that unfulfilled or unrecognized expectations were associated with postoperative dissatisfaction with the outcome. Conversely, appropriate positive preoperative expectations have been associated with higher postoperative satisfaction and HR-QoL outcomes.
Patient expectations play an especially critical role in elective surgical procedures where the patient’s primary motivation for surgery is improved HR-QoL. In the elective orthopedic surgery literature, patient expectations have been particularly well studied. A significant relationship has been demonstrated between expectations and satisfaction following knee surgery and total hip arthroplasty [15–18,29]. For example, a study of 88 patients who underwent total hip replacement found that while 86% of patients believed their operation was technically successful, only 55% felt that their preoperative expectations had been fulfilled. Interestingly, patients who believed that their expectations were fulfilled reported a higher HR-QoL than those with unfulfilled expectations. This finding suggests that fulfilled expectations may be more predictive of satisfaction than a successful operation [2]. In a 2009 study of 112 total knee arthroplasty patients, investigators noted several unrealistic expectations, including that patients significantly underestimating the time it would take to fully recover from surgery (expected 4.7 ± 2.8 months, recalled actual time 6.1 ± 3.7 months; p = 0.005) were overly optimistic about the likelihood of being pain free (85% expected it, 43% were; p < 0.05) and of not being limited in engagement in usual activities (52% expected it, 20% were; p < 0.05) [29]. The authors suggest that further attention should be paid preoperatively to patient expectations regarding postoperative pain and recovery.
The recognition in orthopedics that patient expectations are clinically important has led to the development of a number of patient assessment questionnaires. To be of value, such assessment questionnaires must be reliable and valid. van Hartingsveld and colleagues performed a systematic review of all questionnaires for use among patients with musculoskeletal disorders and evaluated their psychometric properties [30]. They identified 24 questionnaires, 12 specific to orthopedic problems, three for rheumatoid problems and three for chronic pain. Psychometric properties were found to be generally poor. Only two-thirds of questionnaires demonstrated construct validity, ten out of 24 reported analysis of convergent or discriminant validity, and only five of 24 reported questionnaire reliability. They conclude that there was limited evidence to support the reliability or validity of these instruments and strongly recommended further research to achieve this [30].
Another interesting study by a team in Boston (MA, USA) and Newcastle (UK) provided a cross-cultural comparison of patient expectations in knee surgery between the USA, UK and Australia [31]. These authors confirmed, as have other authors, that patient dissatisfaction may be secondary to having inappropriate preoperative expectations. The authors found that Australian patients had a greater expectation of being able to walk >3.2 km than patients in the UK and USA, and that patients in Australia and the USA were more likely than UK patients to expect not to require a walking aid at 12 months postsurgery. These expectations were seen to play a key role in the decision-making process of patients, as Australian patients were less likely than US and UK patients to undergo further total knee arthroplasty [31].
While the relationship between expectations, satisfaction and HR-QoL has been relatively well examined in orthopedics and other areas of elective surgery, little research has been done among breast reconstruction patients. This is somewhat surprising, given that the primary goal of reconstruction is patient satisfaction and improved HR-QoL. Overall, the current literature on expectations for breast reconstruction largely reflects cross-sectional, quantitative studies. Notably, qualitative research and prospective studies are lacking. In a cross-sectional, single time-point survey, Alves et al. found that women undergoing mastectomy lacked knowledge about their surgeries and experienced fear and anxiety with what to expect before having surgery [32]. Brown and colleagues similarly looked at the satisfaction of early breast cancer patients in initial consultations with medical oncologists and found that patient expectations were generally not well met [33]. From a cross-cultural perspective, Guyomard et al. performed an audit comparing French and British patients’ and partners’ satisfaction after breast reconstruction surgery following mastectomy [34]. They found that, compared with British patients, French patients had higher expectations for the results of surgery and were more likely to be disappointed. In addition, the partners of French patients were more likely to be disappointed by breast symmetry, sensation and nipple reconstruction [34]. Most recently, a survey by Waljee et al. at the University of Michigan (MI, USA) revealed that preoperatively, women inaccurately predicted postoperative HR-QoL, and this was most significant for patients undergoing mastectomy alone [35]. Overall, women underestimated their expected HR-QoL and overestimated the stigma of surgery. The authors conclude that predicting HR-QoL and stigma following breast cancer surgery is challenging for patients and that identifying strategies to better inform patients of surgical outcomes may improve the decision-making process [35]. The authors specifically note the future requirement for qualitative research, along with high-quality longitudinal outcomes studies.
Qualitative research on patient expectations for breast reconstruction
Given the importance of expectations in breast reconstruction, and the paucity of research that has been done in this area to date, our team adopted a qualitative approach and performed in-depth interviews with patients before and after breast reconstruction surgery. This work was performed as the first step in a larger study to develop and validate a questionnaire to measure patient expectations for breast reconstruction surgery for use in real-time clinical care (grant number: NIH R03 CA128476-02) [36].
The advantage of qualitative research is that one is able to collect a level of rich descriptive detail from participants often not captured in survey studies. We took a grounded theory approach, which seeks to construct theory about issues of importance to people through a process of data collection that is inductive in nature [37]. A grounded theory approach is well suited to understanding concepts from the patient’s perspective, and to developing a conceptual framework that could be used in the development of a patient-reported outcome measure [38]. In this study, our immediate goal was to better understand the key themes and issues of importance to patients. This exploration of patient perspectives was also directed toward our longer-term goal, which was to develop a new questionnaire that could be used clinically to measure patient expectations for breast reconstruction preoperatively [39,40].
To begin, we obtained approval for our study from the research ethics board at the Memorial Sloan–Kettering Cancer Center (MSKCC; NY, USA). MSKCC is one of the largest cancer centers in the USA and performs approximately 500 breast reconstruction surgeries annually. Plastic surgeons working specifically with breast cancer patients at MSKCC were asked to consider their patient population and identify a sample of participants for qualitative interviews. Women who presented for consultation about breast reconstruction surgery, or had already undergone breast reconstruction surgery, were eligible to be interviewed. We specifically asked surgeons to recruit a maximum variation sample of women that differed in terms of the following patient characteristics: age, ethnicity, social class and phase of treatment. The research team was notified of any consenting women, who were followed up by telephone to set up a time and location for an interview. Sixty-four patients were invited to be interviewed, of whom 44 agreed to participate. Table 1 shows sample characteristics for the 44 patients interviewed. Our sampling strategy took an iterative approach. Patient interview data were analyzed concurrently with data collection and as new themes emerged, additional patients were interviewed among whom these themes could be explored. For example, patients who were undergoing prophylactic mastectomy were found to have different expectations to patients with invasive disease. Therefore, we sought to enrich our sample with additional prophylactic surgery patients, to ensure that data saturation was attained for this cohort. A limitation of our study is that while the interview sample was representative of breast cancer patients treated at MSKCC, patients were not necessarily representative of the greater US breast cancer population. Specifically, a high proportion of our patients were Caucasian, had college-level education and annual income greater than US$100,000. An additional limitation is that we used a surgeon-based sampling strategy, which could introduce bias if surgeons preferentially selected patients with clear and realistic expectations. Surgeons were, however, reminded to recruit patients across the widest possible spectrum, and to include any patients whom the clinician perceived might have particularly high, low or vague expectations.
Table 1.
Qualitative interviews: patient sample characteristics (n = 44, mean age 48 years).
| Patient characteristic | Percentage of patients (n) |
|---|---|
| Ethnicity | |
| Asian or Pacific Islander | 6.8 (3) |
| Black non-Hispanic | 11.4 (5) |
| Black Hispanic | 0 |
| White non-Hispanic | 54.5 (24) |
| White Hispanic | 11.4 (5) |
| Other | 4.5 (2) |
| Education level | |
| Some high school | 0 |
| High school diploma | 4.5 (2) |
| Some college/trade/university | 0 |
| College/trade/university degree | 45.5 (20) |
| Some master/doctoral degree | 4.5 (2) |
| Master/doctoral degree | 45.5 (20) |
| Annual household income (US$) | |
| <20,000 | 0 |
| 20,000–39,999 | 6.8 (3) |
| 40,000–59,999 | 2.3 (1) |
| 60,000–79,999 | 15.9 (7) |
| 80,000–99,999 | 13.6 (6) |
| >100,000 | 38.6 (17) |
| Type of reconstruction | |
| Implant reconstruction | 61.4 (27) |
| TRAM/DIEP | 29.6 (13) |
| LD with implant | 6.8 (3) |
| Other | 2.3 (1) |
| Interview timing | |
| Pre-reconstruction | 59.1 (26) |
| Post-reconstruction | 40.9 (18) |
| Reconstruction timing | |
| Delayed | 6.8 (3) |
| Immediate | 93.2 (41) |
DIEP: Deep inferior epigastric perforator; LD: Latissimus dorsi; TRAM: Transverse rectus abdominus myocutaneous.
All consenting patients participated in a semi-structured interview with an experienced qualitative interviewer. Interviews lasted 60 min on average and involved the use of an interview guide with a series of open-ended questions and probes during which participants were encouraged to discuss their feelings and experiences in depth. All interviews were digitally recorded and transcribed verbatim with identifiable information removed. Interviewing continued until no new themes emerged. The software 6 QSR NVivo 7 was used to store, code and organize the data [41].
Data collection and analysis took place concurrently, which allowed the researchers to revise the interview guide to gather data to refine emerging categories. Analysis was inductive and involved line-by-line coding with codes and categories emerging from participants’ stories. The coding scheme was developed through ongoing discussions with members of the research team. Coding was performed by several members of the research team, who applied codes to patient statements and then used constant comparison to examine relationships within and across codes and categories in order to develop a preliminary conceptual framework for patient expectations (see Figure 1). Patient interviews revealed four key themes that formed the basis of our conceptual framework of patient expectation in breast reconstruction (Figure 1). Below we describe each theme, and illustrate each with examples from patient interviews.
Figure 1.
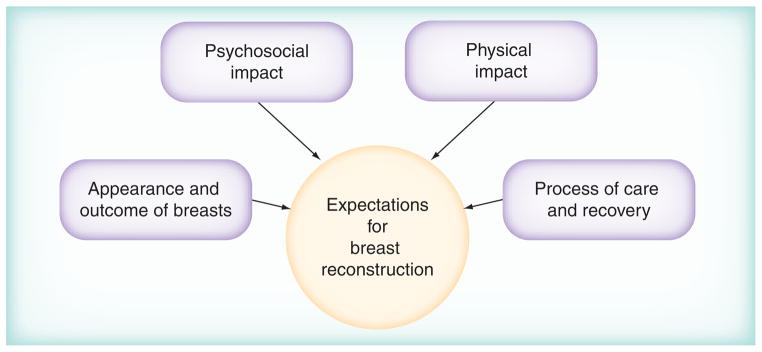
Conceptual framework for patient expectations.
Appearance & outcome of the breasts
This theme relates to women’s expectations about breast appearance and the outcome of breast reconstruction surgery. Comments showed a wide range of different expectations for how women thought their breasts would look after undergoing reconstructive surgery. For example, some comments reflected realistic expectations about how they would look:
“Your breasts aren’t going to be exactly the same anymore. You know, so, I mean, like I said, you really can’t set your expectations up too high” (age 45 years, preoperative immediate tissue expander/implant surgery).
On the other hand, other women expressed seemingly unrealistic expectations. For example, one woman expected her breasts to: “actually look better” following surgery (age 44 years, preoperative immediate tissue expander/implant surgery).
Psychosocial impact of reconstruction
Women talked in detail about the expected psychosocial impact of breast reconstruction. We identified three important subthemes: coping; feelings about oneself; and sexuality.
First, in terms of coping, women expressed a range of expectations for how they would cope with the process of breast reconstruction. It was not uncommon to hear women say they expected to take one step at a time: “So I just try to take it one day at a time” (age 45 years, preoperative immediate tissue expander/implant reconstruction).
Similarly, they also talked about how they expected things would get better “down the road” (age 45 years, post immediate tissue expander, pre implant reconstruction). Many women said they wanted to move on from the cancer and live life again, and expected the breast reconstruction would help them to do that:
“I’m hoping that, you know, like I said, I can move on with my life. I mean, I’m hoping that, like, right now this is just a detour on the road” (age 45 years, preoperative immediate tissue expander/implant reconstruction).
Second, women talked about how they expected to feel about themselves after breast reconstruction. A range of different expectations were identified here. For example, many women talked about the desire to feel whole again:
“‘Cause to me, you know, that’s going to make – it would make me feel whole” (age 49 years, pre-immediate tissue expander/implant reconstruction), and “I wanted to be whole again” (age 53 years, postoperative immediate tissue expander/implant reconstruction).
It was also common for women to express that they expected to feel normal following breast reconstruction surgery. Women also talked about expecting to feel more attractive and more feminine: “I’m going to feel more feminine and more, you know, positive about my body” (age 50 years, postoperative immediate tissue expander, pre-implant placement).
The final psychosocial theme related to sexuality. Women had different expectations in terms of this theme. Women made comments about engaging in sexual relations such as the following: “I would feel uncomfortable in the beginning but I think I’ll get accustomed to it” (age 47 years, preoperative immediate tissue expander/implant reconstruction).
Physical impact of reconstruction
Expectations regarding the physical impact of breast reconstruction included issues such as how much sensation (feeling) there would be in the breasts and reconstructed nipples following surgery. We found that women were sometimes surprised to have no feeling in their breasts, even if they were told this in advance:
“There was no sensation there and I wasn’t ready for that” (age 33 years, postoperative immediate tissue expander/implant reconstruction);
“I wasn’t expecting that when I would touch my skin I wouldn’t feel anything at all” (age 33 years, postoperative immediate tissue expander/implant reconstruction).
Women also talked about their expectations for how their breasts would feel to the touch. Expectations for feel to the touch varied, with some women saying things such as: “I imagine that they’ll be somewhat firmer than what I have” (age 39 years, pre-operative immediate tissue expander/implant reconstruction); “From what I’ve read, they’re going to feel hard” (age 49 years, preoperative immediate tissue expander/implant reconstruction).
The process of care & recovery
The final theme involved expectations regarding the process of care and recovery. Within this area, women talked about their expectations for the amount of information they would expect to receive before their breast reconstruction:
“I expected that I would receive a lot of information, and I didn’t” (age 46 years, prophylactic, postoperative immediate tissue expander, pre-implant placement);
“I’m not expecting them to hold your hand but I do think that there could be some more written information put out or something that would give – that would have made me feel better about the whole thing” (age 47 years, post immediate tissue expander/ implant reconstruction).
Another area of expectation related to the likeliness that they would experience a complication following breast reconstruction surgery. In addition, women talked about their expectations for the physical recovery, including pain. Finally, expectations about the amount of support women would receive from the medical team was an important concern, with postoperative patients commenting: “Don’t be surprised by how little time the plastic surgeons have to spend with you. I didn’t understand that going in” (age 47 years, postoperative immediate tissue expander/implant reconstruction).
Conclusion
Given the mounting demands on surgical practice and concern over medicolegal issues, patient education about breast reconstruction is heavily directed towards complications data. This means that patients may consent for surgery knowing clearly what to expect if something goes wrong, but having very little insight as to what to expect if all goes well. Understanding how patient expectations for breast reconstruction may impact on their perceived outcome is critically important to providing high-quality care. Systematic, efficient measurement and management of expectations may improve patient education, shared medical decision-making and, importantly, long-term quality of life and satisfaction.
Expert commentary: systematic assessment of patient expectations to improve patient education, shared medical decision-making & outcomes
The central value of understanding expectations among breast reconstruction patients lies in opportunities for enhanced patient education and improved shared medical decision-making. Women who seek breast reconstructive surgery do so based on a certain set of personal expectations. When their expectations about the outcome are greater than their actual perceived outcome, disappointment and dissatisfaction may occur. By measuring individual patient expectations in a systematic and reliable way, surgeons may be able to recognize patients with unrealistic expectations preoperatively. They may also identify patients with inappropriately low expectations who might, for example, decide against surgery. Given that expectations play such a key role in patient decision-making and postoperative satisfaction, it is vital that the clinical team address expectations preoperatively through high-quality, individualized patient education.
Improving patient education
For most patients considering breast reconstruction, an important source of information comes from their surgeon during face-to-face discussions. Despite this, most surgeons with a busy clinical practice are forced to limit their patient consultations to discussions about procedural information and potential complications. Ironically, by focusing on potential problems, surgeons often find that their patients are well informed about uncommon adverse events, but do not know what to expect when all goes well. For example, unilateral implant reconstruction patients may be disconcerted to discover that breast symmetry may only be achieved when wearing a bra. Similarly, a patient may look forward to nipple reconstruction without realizing that sensation will not be restored. In addition, patients derive supplemental information from external sources – including the internet and television – that can be inaccurate and misleading, and may reinforce misconceptions about reconstructive surgery. For example, plastic surgeons who advertise heavily on the internet may selectively exhibit photographs of their best postoperative results, setting unrealistically high expectations for patients. These pre-existing beliefs and misconceptions about breast reconstruction may subsequently be very difficult to reconfigure.
Mancuso et al. attempted to evaluate whether, in fact, patients’ preoperative expectations could be successfully modified prior to a surgical intervention [42]. Their team performed two randomized controlled trials, one in hip arthroplasty patients and the other in knee arthroplasty patients. Control patients in each study received standard teaching, while intervention patients received the standard teaching and a specific module designed to address patient expectations for long-term recovery. Before and after receiving the educational module, patients completed either a hip-specific or knee-specific validated expectation questionnaire. The authors concluded that patients’ preoperative expectations about postoperative recovery could indeed be successfully modified.
In light of these findings, our team is developing an interactive, multimedia educational program designed to specifically address patient expectations about breast reconstruction. Our intent is to develop a web-based program that can easily be incorporated into routine clinical practice in order to systematically address individual patients’ preoperative expectations. By employing innovative technology to engage and immerse patients in an interactive learning environment, patient comprehension can be optimized [43]. For example, prior research in the area of patient comprehension suggests that the way information is presented has a profound effect on a patient’s ability to understand and use it. Consistent with this research, in a study of breast reconstruction patients, those who expressed dissatisfaction with preoperative information were most dissatisfied with information presented in printed words [44]. By contrast, others have shown that interactive, multimedia software can play a key and unique role in patient education. For example, the results of a recent randomized controlled trial performed by Shaw et al. demonstrated that the use of a multimodality patient education program can have a positive impact on the delivery of information and, ultimately, on patient satisfaction [45].
Our team’s educational program is being developed directly from the rich qualitative data provided in our patient interview study. The program is structured around the four key themes we identified: appearance and outcome of the breasts; psychosocial impact of reconstruction; physical impact of reconstruction; and the process of care and recovery. Whenever possible, patient-derived language is being used to guide the text; additionally, patients have reviewed the program at every stage to ensure that language and content are appropriate and easy to understand. Illustrations, animations, patient photographs and audio clips of patient interviews are being incorporated to enhance comprehension and engage the learner. Interactive questions with relevant, error-contingent feedback are being introduced into the script. The end result will be a program that allows the patient to browse the information at her own pace and repeat select portions of the interactive program to maximize learning. By including realistic graphics and photographs, the transfer of knowledge from the virtual environment to reality will be optimized. In addition, by periodically challenging the learner with questions, integration of information into long-term memory will be facilitated [46]. This multimedia education program is in the final phases of development and will be available for use by Spring 2012.
Optimizing shared decision-making
Contemporary surgical techniques provide numerous options for breast reconstruction (e.g., the use of an implant or one’s own tissues). Procedure selection is generally based on a range of patient variables, including pre-existing health conditions, availability of donor tissues for reconstruction and, most importantly, patient preference. By engaging a woman in the process of shared decision-making, the surgeon and patient can make a mutually agreeable choice that reflects the patient’s individual values and health preferences.
In the clinical setting, shared decision-making may be promoted by a careful inventory of expectations; such documentation of appropriate expectations may also be helpful to further delineate the informed consent process. To guide this process, reliable outcomes data are an essential element. Such data will not only provide an accurate estimation of predicted outcomes but also assist in defining realistic postoperative expectations for patients. In the preoperative encounter, clinicians should endeavor to systematically discuss evidence from existing studies on patient-reported outcomes. For example, we recently set out to identify predictors of patient satisfaction with breast appearance, including implant type, in a large sample of women who had breast reconstruction surgery using implants. The results of our study suggest that patients who receive silicone breast implants report higher satisfaction with their reconstructed breasts compared with those who receive saline implants [47]. For breast cancer survivors who plan to undergo implant-based breast reconstruction, this information can now be used to provide a more accurate estimation of predicted outcomes and may assist in individualizing treatment options. Other authors have similarly examined long-term patient satisfaction comparing autogenous reconstruction to implant reconstruction [48]. These authors note that long-term satisfaction is significantly higher when reconstruction is performed using a woman’s own tissue. While this study does not suggest that all women should undergo autogenous reconstruction, the findings can help to guide appropriate expectations for patients considering each of these techniques.
Improving patient satisfaction & HR-QoL outcomes
Building on the key themes identified in our qualitative study, our team has recently developed a new questionnaire to provide reliable and valid measurement of patient expectations for breast reconstruction. The questionnaire that we are developing to measure expectations for reconstruction is designed as a module within the BREAST-Q©. The BREAST-Q is patient-reported outcome measure developed by our group to measure multiple aspects of HR-QoL (i.e., psychosocial, sexual and physical wellbeing) as well as patient satisfaction (i.e., satisfaction, with overall outcome and information and care provided) among breast surgery patients [49]. The BREAST-Q scales are brief and designed for administration before and after surgery. The BREAST-Q has now been translated and linguistically validated in 14 languages, and is being used extensively around the world. For example, it was recently used as an outcome metric in the UK’s NHS Breast Surgery Audit involving over 8000 breast cancer surgery patients [50,101].
Five-year view
This questionnaire is now available for use by researchers and healthcare providers (Table 2). Further details regarding the psychometric development of this questionnaire are to be published separately. We anticipate that over the next 5 years, systematic measurement of patient expectations using this questionnaire may become routine in clinical practice. Building upon this, we also envision new and innovative ways to enhance patient education, shared medical decision-making and outcomes.
Table 2.
BREAST-Q: expectations for reconstruction example question.
| Response | Code for response |
|---|---|
| Imagine yourself 1 year after your surgery. What do you expect the shape of your reconstructed breast to be like? | |
| A very different shape from my natural breast(s) | 1 |
| A similar shape to my natural breast(s) | 2 |
| Exactly the same shape as my natural breast(s) | 3 |
| I don’t know | dk |
| How similar (symmetric) do you expect your breasts to look when you are unclothed? | |
| My breasts will look very different from each other | 1 |
| My breasts will look similar to each other | 2 |
| My breasts will look exactly the same | 3 |
| I don’t know | dk |
We hypothesize that by systematically assessing and addressing patient expectations, it may be possible to improve satisfaction and HR-QoL outcomes among breast reconstruction patients. Using the core BREAST-Q outcome scales in combination with the Expectations for Reconstruction Module, future research can be conducted to better elucidate the relationship between patient expectations prior to surgery and satisfaction and HR-QoL after surgery. From a research perspective, a long-term goal would be to design and conduct prospective studies to: determine variations in expectations related to patient characteristics; identify patients at risk of dissatisfaction; and evaluate how systematic assessment and modification of preoperative expectations may contribute to improved long-term postoperative satisfaction and HR-QoL.
Key issues.
By assessing individual patient expectations in a reliable way, surgeons may recognize patients who have unrealistic expectations before they undergo surgery, and take steps to address these misconceptions preoperatively.
Shared medical decision-making may be complemented by a careful exploration and measurement of a woman’s expectations, along with her individual values and health preferences.
Given the role that patient expectations play in decision-making and postoperative satisfaction, it is vital that the clinical team monitor patient expectations preoperatively through high-quality, individualized patient education.
The assessment of individual patient expectations and steps taken to modify or manage these expectations may be helpful to document the informed consent process.
The BREAST-Q Expectations module was developed to address the need for a qualitatively grounded assessment tool to measure pre-operative expectations among breast reconstruction patients.
The conceptual framework of the BREAST-Q Expectations module consists of four main themes: appearance and outcome of the breasts; psychosocial impact of reconstruction; physical impact of reconstruction; and the process of care and recovery.
By systematically addressing patient expectations, it may be possible to improve patient education, shared medical decision-making, satisfaction and health-related quality-of-life outcomes among breast reconstruction patients.
Footnotes
For reprint orders, please contact reprints@expert-reviews.com
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
Financial & competing interests disclosure
Grant funding for the development of the BREAST-Q: Expectations for Reconstruction Module was provided by the National Endowment for Plastic Surgery and the NIH (R03 CA128476-01). The BREAST-Q is jointly owned by the Memorial Sloan–Kettering Cancer Center and the University of British Columbia. A Pusic, A Klassen and S Cano are codevelopers of the BREAST-Q and, as such, receive a share of any license revenues based on the inventor sharing policies of these two institutions. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
• of interest
- 1.Breast Cancer Facts & Figures 2011. American Cancer Society; GA, USA: 2011. [Google Scholar]
- 2.Burton KE, Wright V, Richards J. Patients’ expectations in relation to outcome of total hip replacement surgery. Ann Rheum Dis. 1979;38:471–474. doi: 10.1136/ard.38.5.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarwer DB, Whitaker LA, Pertschuk MJ, Wadden TA. Body image concerns of reconstructive surgery patients: an underrecognized problem. Ann Plast Surg. 1998;40(4):403–407. doi: 10.1097/00000637-199804000-00014. [DOI] [PubMed] [Google Scholar]
- 4•.Kravitz RL, Callahan EJ, Paterniti D, et al. Prevalence and sources of patients’ unmet expectations for care. Ann Intern Med. 1996;125:730–737. doi: 10.7326/0003-4819-125-9-199611010-00004. Qualitative study of patients who reported an omission in their medical care. The study is an exploration of the source of the patients’ expectations and perceptions of the care they received. [DOI] [PubMed] [Google Scholar]
- 5.Bandura A. Social Foundation of Thought and Human Action. Prentice-Hall; NJ, USA: 1986. [Google Scholar]
- 6.Ajzen I. Attitudes, Personality, and Behavior. Open University Press; Milton-Keynes, UK: 1988. [Google Scholar]
- 7.Kirsch I. Response expectancy as a determinant of experience and behavior. American Psychologist. 1985;40:1189–1202. [Google Scholar]
- 8•.Thompson AG, Suñol R. Expectations as determinants of patient satisfaction: concepts, theory, and evidence. Int J Qual Health Care. 1995;7(2):127–141. doi: 10.1093/intqhc/7.2.127. Review of the literature between 1973 and 1995 surrounding expectations and satisfaction with a special emphasis on healthcare. [DOI] [PubMed] [Google Scholar]
- 9.Festinger L. A Theory of Cognitive Dissonance. Harper and Row; NY, USA: 1957. [Google Scholar]
- 10.Parasuraman A, Berry LL, Zeithaml VA. Understanding customer expectations of service. Sloan Management Review. 1991;32(3):39–48. [Google Scholar]
- 11.Oliver RL. Cognitive, affect, and attribute bases of the satisfaction response. J Consumer Res. 1993;20:418–430. [Google Scholar]
- 12.Smith-McLallen A, Fishbein M, Hornik RC. Psychosocial determinants of cancer-related information seeking among cancer patients. J Health Comm. 2011;16:212–225. doi: 10.1080/10810730.2010.522227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guerra CE, McDonald VJ, Ravenell KL, et al. Effect of race on patient expectations regarding their primary care physicians. Fam Pract. 2008;25:49–55. doi: 10.1093/fampra/cmn005. [DOI] [PubMed] [Google Scholar]
- 14.Gleason ME, Harper FW, Eggly S, et al. The influence of patient expectations regarding cure on treatment decisions. Patient Educ Couns. 2009;75:263–269. doi: 10.1016/j.pec.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mancuso CA, Sculco TP, Wickiewicz TL, et al. Patients’ expectations of knee surgery. J Bone Joint Surg Am. 2001;83-A:1005–1012. doi: 10.2106/00004623-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Mancuso CA, Salvati EA. Patients’ satisfaction with the process of total hip arthroplasty. J Healthcare Qual. 2003;25:12–18. doi: 10.1111/j.1945-1474.2003.tb01039.x. quiz 18–19. [DOI] [PubMed] [Google Scholar]
- 17.Mancuso CA, Salvati EA, Johanson NA, et al. Patients’ expectations and satisfaction with total hip arthroplasty. J Arthroplasty. 1997;12:387–396. doi: 10.1016/s0883-5403(97)90194-7. [DOI] [PubMed] [Google Scholar]
- 18.Mancuso CA, Sculco TP, Salvati EA. Patients with poor preoperative functional status have high expectations of total hip arthroplasty. J Arthroplasty. 2003;18:872–878. doi: 10.1016/s0883-5403(03)00276-6. [DOI] [PubMed] [Google Scholar]
- 19.Iversen MD, Daltroy LH, Fossel AH, et al. The prognostic importance of patient pre-operative expectations of surgery for lumbar spinal stenosis. Patient Educ Couns. 1998;34:169–178. doi: 10.1016/s0738-3991(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 20.Lutz GK, Butzlaff ME, Atlas SJ, et al. The relation between expectations and outcomes in surgery for sciatica. J Gen Intern Med. 1999;14:740–744. doi: 10.1046/j.1525-1497.1999.10417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kiyak HA, Vitaliano PP, Crinean J. Patients’ expectations as predictors of orthognathic surgery outcomes. Health Psychol. 1988;7:251–268. doi: 10.1037//0278-6133.7.3.251. [DOI] [PubMed] [Google Scholar]
- 22.Flood AB, Lorence DP, Ding J, et al. The role of expectations in patients’ reports of post-operative outcomes and improvement following therapy. Med Care. 1993;31:1043–1056. doi: 10.1097/00005650-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 23•.Hudak PL, Hogg-Johnson S, Bombardier C, et al. Testing a new theory of patient satisfaction with treatment outcome. Med Care. 2004;42:726–739. doi: 10.1097/01.mlr.0000132394.09032.81. Cohort study testing a new patient satisfaction theory of embodiment compared with seven other satisfaction theories in a population of elective hand surgery patients. [DOI] [PubMed] [Google Scholar]
- 24.Mahomed NN, Liang MH, Cook EF, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273–1279. [PubMed] [Google Scholar]
- 25.O’Malley KJ, Roddey TS, Gartsman GM, et al. Outcome expectancies, functional outcomes, and expectancy fulfillment for patients with shoulder problems. Med Care. 2004;42:139–146. doi: 10.1097/01.mlr.0000108766.00294.92. [DOI] [PubMed] [Google Scholar]
- 26.Leedham B, Meyerowitz BE, Muirhead J, et al. Positive expectations predict health after heart transplantation. Health Psychol. 1995;14:74–79. doi: 10.1037//0278-6133.14.1.74. [DOI] [PubMed] [Google Scholar]
- 27.Andrykowski MA, Brady MJ, Greiner CB, et al. ‘Returning to normal’ following bone marrow transplantation: outcomes, expectations and informed consent. Bone Marrow Transplant. 1995;15:573–581. [PubMed] [Google Scholar]
- 28.Marschall-Kehrel D, Roberts RG, Brubaker L. Patient-reported outcomes in overactive bladder: the influence of perception of condition and expectation for treatment benefit. Urology. 2006;68:29–37. doi: 10.1016/j.urology.2006.02.046. [DOI] [PubMed] [Google Scholar]
- 29.Mannion AF, Kämpfen S, Munzinger U, Kramers-de Quervain I. The role of patient expectations in predicting outcome after total knee arthroplasty. Arthritis Res Ther. 2009;11:R139. doi: 10.1186/ar2811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30•.van Hartingsveld F, Ostelo RW, Cuijpers P, et al. Treatment-related and patient-related expectations of patients with musculoskeletal disorders: a systematic review of published measurement tools. Clin J Pain. 2010;26:470–488. doi: 10.1097/AJP.0b013e3181e0ffd3. Systematic review of measurement instruments to assess expectations of patients with musculoskeletal disorders. The instruments reviewed were noted to have generally weak psychometric properties. [DOI] [PubMed] [Google Scholar]
- 31.Lingard EA, Sledge CB, Learmonth ID. Patient expectations regarding total knee arthroplasty: differences among the United States, United Kingdom, and Australia. J Bone Joint Surg Am. 2006;88:1201–1207. doi: 10.2106/JBJS.E.00147. [DOI] [PubMed] [Google Scholar]
- 32.Alves PC, Silva AP, Santos MC, et al. Knowledge and expectations of women in the preoperative mastectomy. Rev Esc Enferm USP. 2010;44:989–995. doi: 10.1590/s0080-62342010000400019. [DOI] [PubMed] [Google Scholar]
- 33.Brown RF, Hill C, Burant CJ, et al. Satisfaction of early breast cancer patients with discussions during initial oncology consultations with a medical oncologist. Psychooncology. 2009;18:42–49. doi: 10.1002/pon.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guyomard V, Leinster S, Wilkinson M, et al. A Franco–British patients’ and partners’ satisfaction audit of breast reconstruction. J Plast Reconstr Aesthet Surg. 2009;62:782–789. doi: 10.1016/j.bjps.2007.09.054. [DOI] [PubMed] [Google Scholar]
- 35.Waljee JF, Ubel PA, Atisha DM, et al. The choice for breast cancer surgery: can women accurately predict postoperative quality of life and disease-related stigma? Ann Surg Oncol. 2011;18:2477–2482. doi: 10.1245/s10434-011-1582-x. [DOI] [PubMed] [Google Scholar]
- 36.Snell L, Pusic A, Klassen A, et al. Clarifying expectations for breast reconstruction: developing a new patient assessment tool. Plast Reconstr Surg. 2010;125(6 Suppl):102. doi: 10.1097/PRS.0b013e3181f44580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strauss AC, Corbin JM. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Sage Publications; CA, USA: 1990. [Google Scholar]
- 38.Streiner DL, Norman G. Health Measurement Scales: A Practical Guide to Their Development and Use. Oxford University Press; Oxford, UK: 1995. [Google Scholar]
- 39•.Snell L, McCarthy C, Klassen A, et al. Clarifying the expectations of patients undergoing implant breast reconstruction: a qualitative study. Plast Reconstr Surg. 2010;126:1825–1830. doi: 10.1097/PRS.0b013e3181f44580. Exploration of patient expectations regarding implant-based breast reconstruction following standard teaching. Unclear expectations were found to correspond with postoperative dissatisfaction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40•.Spector D, Mayer D, Knafl K, Pusic A. Not what I expected: informational needs of women undergoing breast surgery. Plast Surg Nurs. 2010;30:70–74. doi: 10.1097/PSN.0b013e3181dee9a4. Qualitative study outlining the informational needs of women who underwent breast augmentation, reduction or reconstruction surgery. [DOI] [PubMed] [Google Scholar]
- 41.NVivo qualitative data analysis software. Version 7. Qualitative Solutions Research International; Australia: 2006. [Google Scholar]
- 42•.Mancuso CA, Graziano S, Briskie LM, et al. Randomized trials to modify patients’ preoperative expectations of hip and knee arthroplasties. Clin Orthop Relat Res. 2008;466:424–431. doi: 10.1007/s11999-007-0052-z. Randomized clinical trial showing that patients’ preoperative expectations of their recovery from knee or hip arthroplasty could be modified through the intervention of preoperative education. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Giloth B. What makes a patient education program effective? Promot Health. 1983;4:6–8. [PubMed] [Google Scholar]
- 44.Sheehan J, Sherman KA, Lam T, et al. Association of information satisfaction, psychological distress and monitoring coping style with post-decision regret following breast reconstruction. Psychooncology. 2007;16:342–351. doi: 10.1002/pon.1067. [DOI] [PubMed] [Google Scholar]
- 45.Shaw MJ, Beebe TJ, Tomshine PA, et al. A randomized, controlled trial of interactive, multimedia software for patient colonoscopy education. J Clin Gastroenterol. 2001;32:142–147. doi: 10.1097/00004836-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 46.Clark R. Web-Based Learning: What Do We Know? Where Do We Go? Information Age Publishing; CT, USA: 2003. Research on web-based learning: a half-full glass. [Google Scholar]
- 47•.McCarthy CM, Klassen AF, Cano SJ, et al. Patient satisfaction with postmastectomy breast reconstruction: a comparison of saline and silicone implants. Cancer. 2010;116:5584–5591. doi: 10.1002/cncr.25552. Multicenter, cross-sectional study suggesting that patient satisfaction was higher (p = 0.016) in women who received a silicone compared with saline implant for postmastectomy breast reconstruction. [DOI] [PubMed] [Google Scholar]
- 48.Hu ES, Pusic AL, Waljee JF, et al. Patient-reported aesthetic satisfaction with breast reconstruction during the long-term survivorship period. Plast Reconstr Surg. 2009;124:1–8. doi: 10.1097/PRS.0b013e3181ab10b2. [DOI] [PubMed] [Google Scholar]
- 49.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–353. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]
- 50.Jeevan R, Cromwell D, Browne J, et al. Third Annual Report of the National Mastectomy and Breast Reconstruction Audit 2009. The NHS Information Centre; Leeds, UK: 2010. [Google Scholar]
Website
- 101.National Clinical Audit Support Programme – Mastectomy and Breast Reconstruction. www.ic.nhs.uk/mbr.


