Abstract
OBJECTIVES
To assess the food intake pattern and the nutritional status of children with cerebral palsy.
METHODS
Cross-sectional study with 90 children from two to 12.8 years with cerebral palsy in the following forms: hemiplegia, diplegia, and tetraplegia. Nutritional status was assessed by weight, height, and age data. Food intake was verified by the 24-hour recall and food frequency questionnaire. The ability to chew and/or swallowing, intestinal habits, and physical activity were also evaluated.
RESULTS
For 2-3 year-old age group, the mean energy intake followed the recommended range; in 4-6 year-old age group with hemiplegia and tetraplegia, energy intake was below the recommended limits. All children presented low intake of carbohydrates, adequate intake of proteins and high intake of lipids. The tetraplegia group had a higher prevalence of chewing (41%) and swallowing (12.8%) difficulties compared to 14.5 and 6.6% of children with hemiplegia, respectively. Most children of all groups had a daily intestinal habit. All children presented mild physical activity, while moderate activity was not practiced by any child of the tetraplegia group, which had a significantly lower height/age Z score than those with hemiplegia (-2.14 versus -1.05; p=0.003).
CONCLUSIONS
The children with cerebral palsy presented inadequate dietary pattern and impaired nutritional status, with special compromise of height. Tetraplegia imposes difficulties regarding chewing/swallowing and moderate physical activity practice.
Keywords: brain damage, chronic; cerebral palsy; nutritional status; child
Abstract
OBJETIVO
Evaluar el estándar alimentar y estado nutricional de niños con parálisis cerebral.
MÉTODOS
Estudio transversal con 90 niños de 2 a 12,8 años de edad, con parálisis cerebral de tipo hemiplejía, diplejía y tetraplejía. Se evaluaron el estado nutricional por medio de los datos de peso, altura y edad, el consumo alimentar por el Recordatorio de 24 horas y por el Cuestionario de Frecuencia Alimentar, la capacidad de masticar y/o deglutir, el hábito intestinal y la práctica de actividad física.
RESULTADOS
En el grupo de 2 a 3 años, el promedio de ingestión energética estaba conforme a la recomendación; en la franja de 4 a 6 años, los grupos con hemiplejía y con tetraplejía presentaban promedios inferiores al límite inferior de recomendación. El grupo como un todo presentó estándar dietético bajo en carbohidratos, adecuado en proteínas y alto en lípidos. El grupo con tetraplejía presentó mayor prevalencia de dificultad para masticación (41%) y deglución (12,8%), versus, respectivamente, 14,5 y 6,6% de los niños con hemiplejía. Se observó que la mayoría de los niños con cada tipo de parálisis cerebral presentaba hábito intestinal diario. Todos los niños estudiados tenían actividad física liviana, mientras que la actividad moderada no era practicada por ningún niño del grupo tetraplejía, que también presentó escore Z de -2,14 de la relación estatura/edad, significantemente menor respecto al grupo con hemiplejía (escore Z de -1,05; p=0,003).
CONCLUSIONES
Los niños presentaron estándar alimentar inadecuado, estado nutricional comprometido, principalmente la estatura. La tetraplejía impone dificultades de masticación/deglución y práctica de actividad física moderada.
Introduction
Cerebral palsy (CP), also called non-progressive static encephalopathy, is the set of non-progressive brain disorders caused by brain injury that occurred during fetal life or in the first years of life( 1 ). The diagnosis is wide-ranging and depends on the severity of the topographic distribution (affected members), clinical history, and motor dysfunction( 2 ).
A number of other symptoms may be associated to motor disorders: mental retardation, epilepsy, hearing, language, ocular/visual, and behavior disorders (3). According to Rotta( 4 ), the child with CP presents lower weight, and lower resistance to infections. Studies documented association between chewing and swallowing problems and nutritional impairment( 5 - 7 ). The chronic changes in swallowing can lead to malnutrition, dehydration, aspiration, and pneumonia( 8 ).
Studies have shown an association between chewing and swallowing difficulties and nutritional impairment( 7 , 9 ). In Brazil, Pires et al( 10 ), in a research involving children and adolescents with CP in São Paulo, found 63% prevalence of low birth weight in patients with tetraplegia. According to Santos and Serrano( 11 ), 20% of children treated at the Association of Parents and Friends of Exceptional Children (Associação de Pais e Amigos dos Excepcionais - Apae) from Vale do Aço, (metropolitan area in the state of Minas Gerais) were malnourished, 65% were at risk of malnutrition, and 50% presented iron deficiency anemia.
Given the importance of nutritional assessment, which can provide support to the most suitable individual treatment as well as to the planning of public health interventions, the present study aimed to assess the nutritional status, by anthropometry, and the dietary patterns of children with non-progressive chronic encephalopathy.
Method
This was an observational descriptive cross-sectional study, conducted by convenience sampling, involving 90 children of both genders, aged between two and 12.8 years, with CP followed at the Rehabilitation Center for Physical and Mental Disabilities (Centro de Reabilitação de Deficientes Físicos e Mentais) in the municipality of Santos, state of São Paulo. Data from January to May 2011 were collected. This study was approved by the Research Ethics Committee of Universidade Federal de São Paulo, and a previous written consent by parents or guardians was required.
The sample selection was conducted from the research in the medical records of all children and adolescents treated in that institution, which were signed by the neurologist on charge. Among the total of 232 records, there were 116 cases of CP. Children using nasogastric or gastrostomy feeding tube were excluded as were two others for frequent absences.
The classification by Rotta et al( 12 ) was used to classify the type of CP, with the use of topographic distribution and the extent of impairment. We classified the studied group in cases of hemiplegia, diplegia, and tetraplegia.
The dietary assessment with the parents was performed using the 24-hour recall method( 13 ) and the Food Frequency Questionnaire (FFQ)( 14 ). The intake of energy and macronutrients was calculated with the DietPro software, version 5.5i (Universidade Federal de Viçosa)( 15 ), with data from the 24-hour recall. The following percentages of total energy from macronutrients were considered adequate: 55-60% carbohydrates, 10-15% protein, and 25-30% lipids( 16 ). Values of energy and activity level were analyzed according to the American food guide( 17 ). It was necessary to stratify age for the analysis.
In the interview with parents, they were asked about the difficulty in chewing and/or swallowing solid foods; the number of meals/day (considering that four to five meals were appropriate); the practice of mild physical activity (only physiotherapy in the institution, once a week) and moderate physical activity (besides physiotherapy in the institution, 30 to 50 minutes of swimming, physical education or equine therapy); and bowel habit (daily, every other day, less than three times/week).
For height and weight measurements, the recommended techniques were employed. Estimates were used when the physical condition of the child did not allow the measurements. For estimated weight: the parents were weighed using only light clothing, without shoes; then they were weighed again with the child on their lap. The child's weight was obtained subtracting the values found. For estimated height, in centimeters, a bone caliper was used in order to measure knee length, to the calcaneus, with a 90° angle between the leg and the tight of the patient, and height was calculated according to the formula proposed by Stevenson( 18 ): [E(cm)=(2.69xCJ)+24.2, with a standard deviation of ±1.1].
The z score of body mass index-for-age (BMI/A) and height-for-age (H/A) of all participants was calculated. Specifically for children from 2 to 5 years, the z score of weight-for-age (W/A) was calculated. Nutritional status was calculated according to recommendations of the World Health Organization (WHO)( 19 ). Patients were classified as malnourished when z score values were ≤ -2.
In statistical analysis, Student t test, analysis of variance with one criterion, and Kruskal-Wallis test were used, according to the nature of the variables. Significance was established at p<0.05.
Results
The study sample consisted of 90 patients with chronic encephalopathy, from 2 to 12.8 years, of whom 52 were male and 38, female. The mean age was 6.2±3.3 years. Among the 90 children, 54% were classified with hemiplegia, 43% with tetraplegia, and 3% with diplegia.
Difficulty in chewing solid food was observed in 23 (26%) cases and, for swallowing, in eight (9%) cases. Children with diplegia had no difficulty in chewing and swallowing, while the quadriplegic children had a higher prevalence of chewing (41%) and swallowing (12.8%) problems, versus 14.5 and 6.6% of children with hemiplegia, respectively.
The percentage of total energy coming from macronutrients showed that for the group as a whole, there was a dietary pattern low in carbohydrates (52%), adequate in protein (53%), and high in lipids (43%). The analysis according to the type of CP showed, in the group with hemiplegia, high intake of fat (58%) and inadequate intake of carbohydrate and protein (50%). In the group with tetraplegia, 64% showed high fat intake, 62%, low carbohydrate intake and 46%, low protein intake.
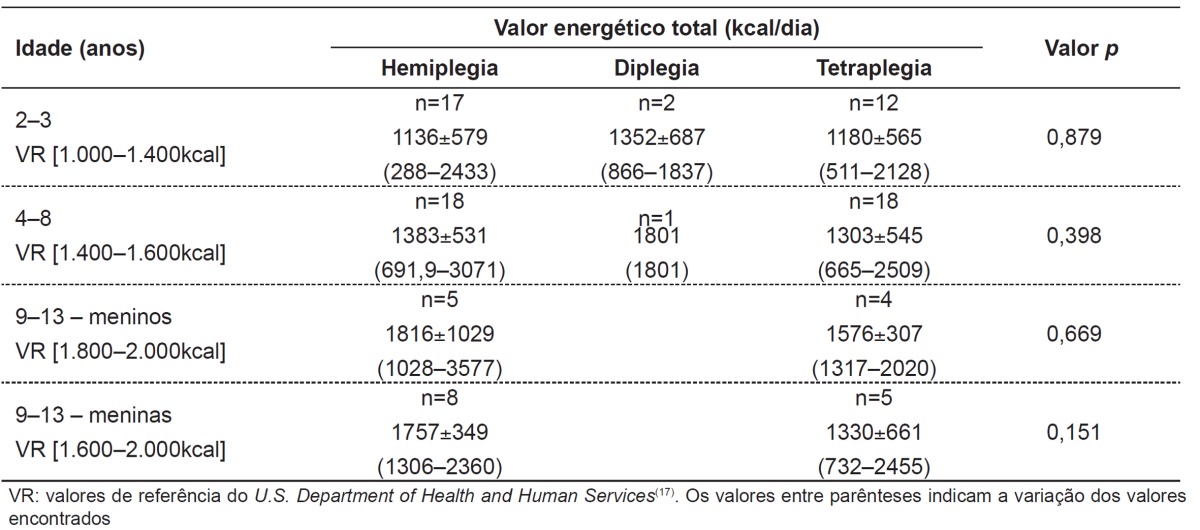
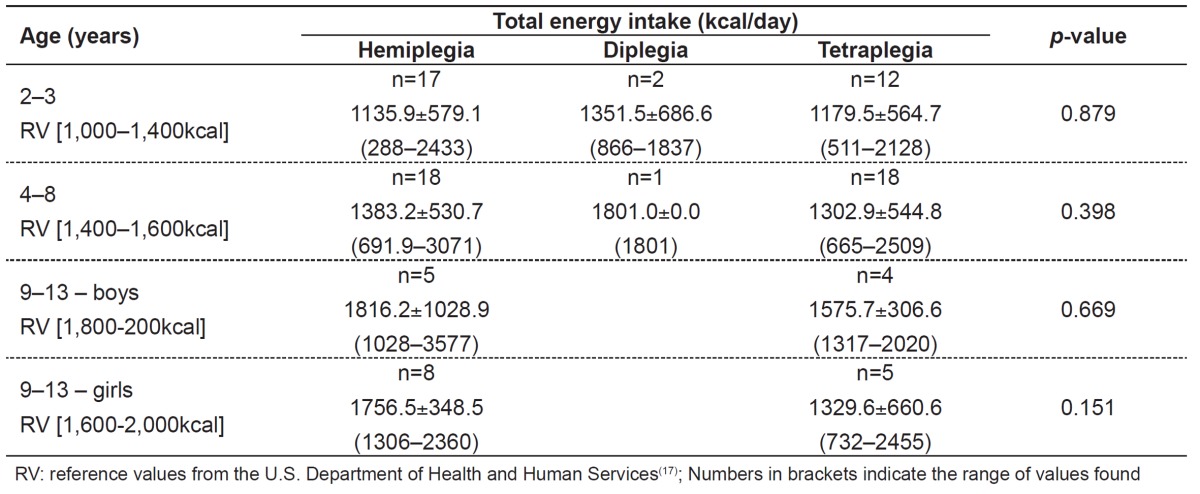
The average energy consumption showed no significant difference in children with the various types of CP, according to the age ranges. In the group of children from 2-3 years, the means were in agreement with the recommendation. In the age range of 4-6 years, the groups with hemiplegia and tetraplegia presented means below the lower limits of recommendation. In the age range from 9-13 years, both for boys and girls, the group with tetraplegia showed means of energy intake below the recommended (Table 1).
Table 1. Total energy consumption by children according to the type of cerebral palsy.
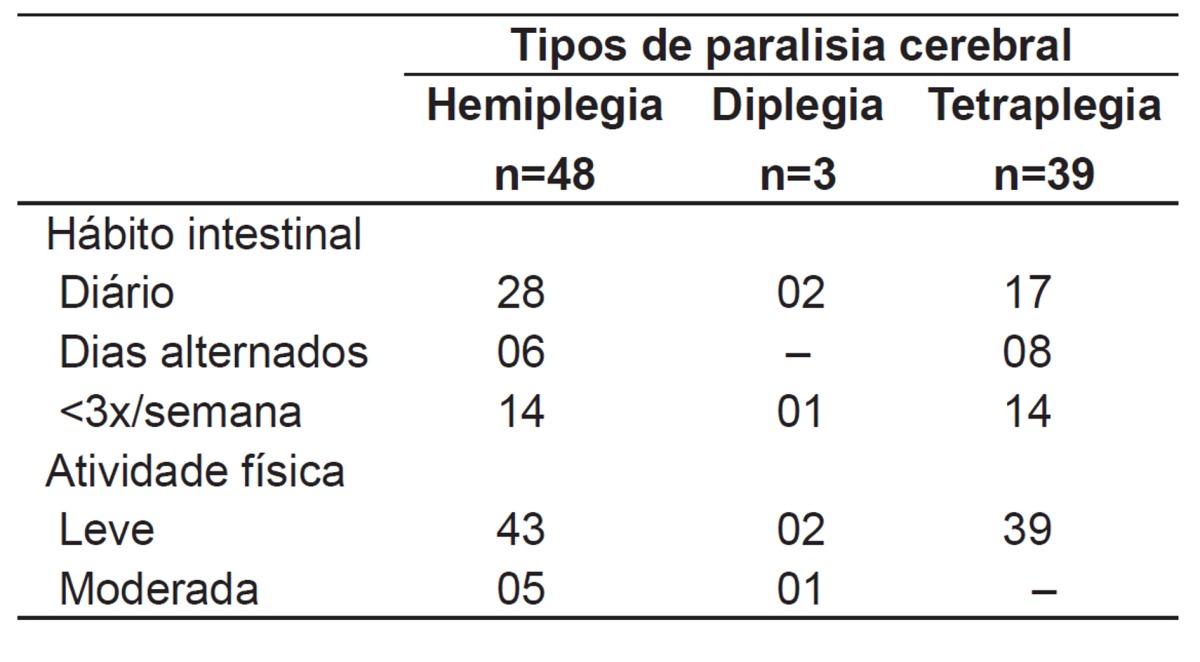
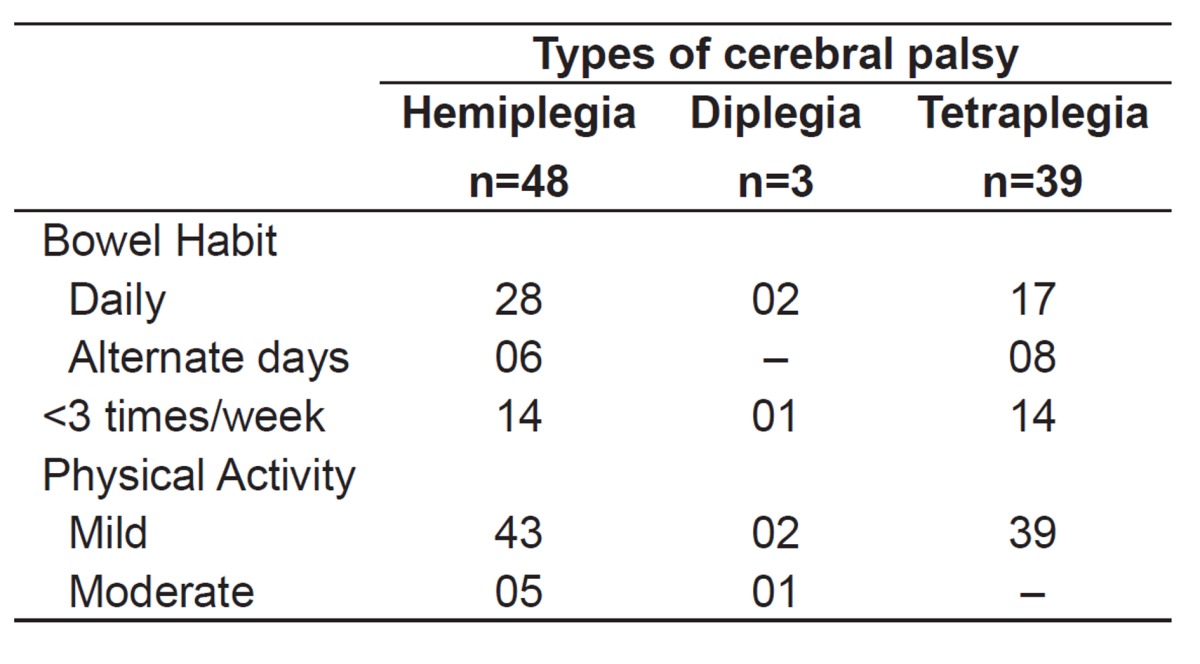
It was observed that most children with CP had daily bowel movements. The rest of each group showed predominantly less than three bowel movements a week, on alternate days. All children studied had mild physical activity. No children in the group with tetraplegia, five children in the group with hemiplegia, and one child in the group with diplegia reported moderate activity (Table 2).
Table 2. Distribution of the population according to the type of cerebral palsy and second bowel habits and level of physical activity.
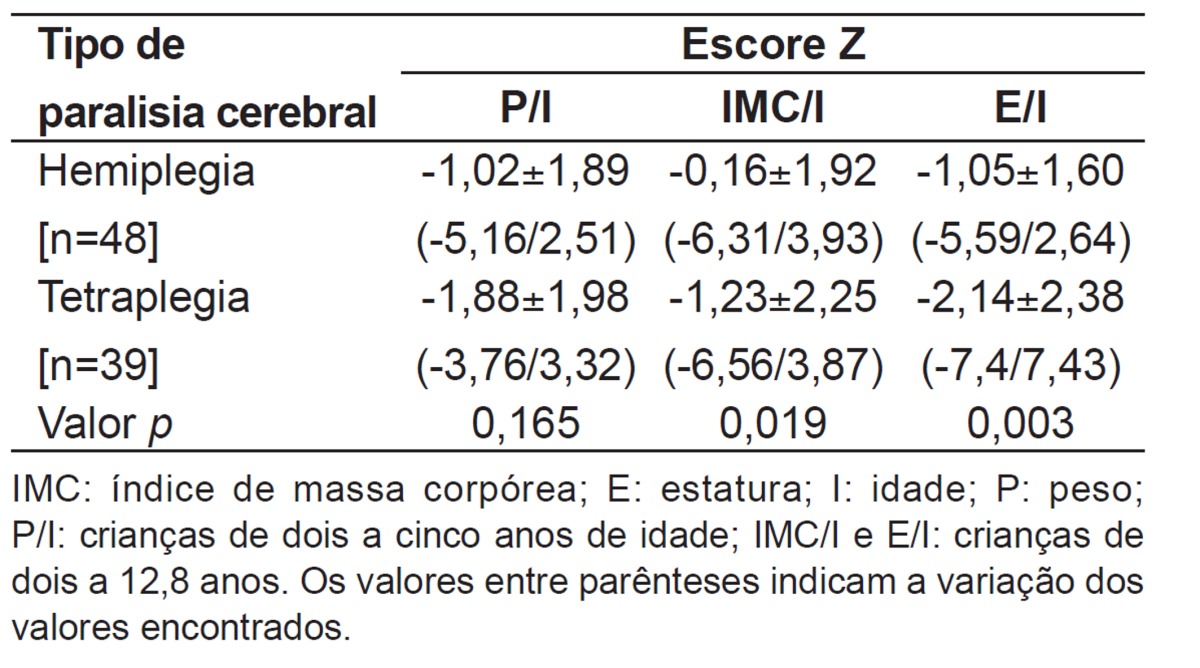
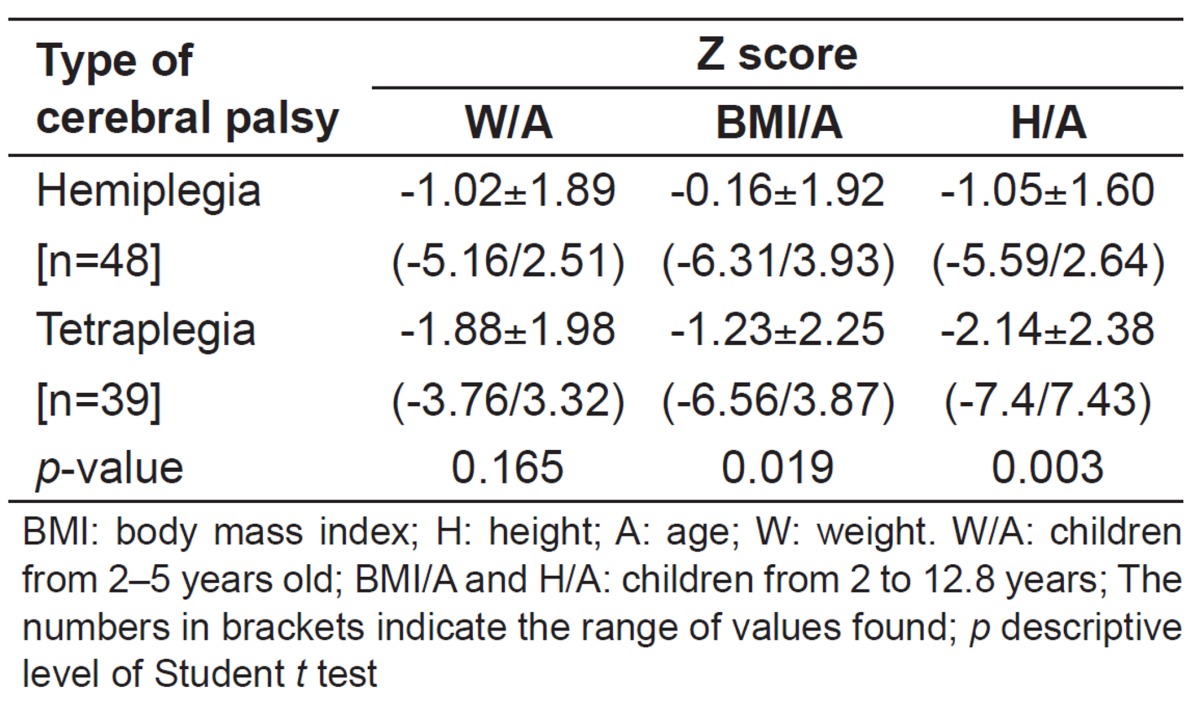
In the group with diplegia (not considered in the statistical analyses of anthropometric data), only one in three children showed a z score=-2.40 for H/A. On average, only the group with tetraplegia showed a z score for W/A near -2 (-1.88) and, as for the H/A z score, a value of -2.14, significantly lower than the group with hemiplegia (p=0.019 and p=0.003) was found. However, considering these two groups, 18/45 children, it was observed that they showed a z score <-2 for W/A; 20/87 for BMI/A, and 29/87 children for H/A z score (Table 3).
Table 3. Nutritional status by anthropometry of children according to the types of hemiplegia and tetraplegia in cerebral palsy.
Discussion
In the review of food consumption and anthropometric measures, the group with diplegia showed results that were not considered for statistical analysis, since their sample size (3) was not representative. In groups with hemiplegia and tetraplegia, it was observed that, until 3 years of age, energy intake remained adequate. From 3 to 12.8 years, this consumption was below the recommended, with values, on average, lower in the group with tetraplegia. This fact can be explained by the difficulty in chewing and swallowing that these individuals might have, which is more significant in the group with tetraplegia, which may, perhaps, have been attenuated in the younger age groups due to food consistency of porridge and soups, more appropriate for this age group. The low energy intake is also reported by Sullivan et al( 7 ), when 90 children with CP were assessed, being 71% tetraplegic, and by Pereira Linhares( 20 ), who reports that this pattern of intake is independent of sex.
However, as important as energy intake, is the balance of macronutrients in the diet composition. In this sense, the studied population showed an unbalanced dietary pattern, high in fat and low in carbohydrates. Fat was represented mainly by weekly intake of cold cuts and sausages (cheese-salad, hot-dog, and fried sausage) in 58% and savory foods (potato chips, French fries, and garlic oil) in 62%. According to Abanto et al( 21 ), there is no significant difference in healthy children and adolescents with CP and normal ones on the preference for salty snacks. Similarly, the preference for fat instead of carbohydrates is described in healthy children and adolescents( 22 ), which may occur, among other possibilities, due to the higher palatability of fat, the influence of the media, the possibility of eating away from home, accompanying friends in the preference for fast food, and, especially, the family eating habits( 23 - 26 ). Therefore, the feeding patterns of children and adolescents is independent of health status, pointing to the need for nutrition education in general, and in particular for those with CP due to the lower amount of food intake and the need for change in consistency of food.
In this study, through the food frequency questionnaire, it was observed that there was an adequate number (four to five) of meals/day and, in addition to the high consumption of fatty foods, there was little daily consumption of vegetables, fruits and liquids, not exceeding three glasses daily of 200mL, represented mainly by industrialized juice powder and soda. This was consumed weekly by 54% of patients, and 19% used daily. Daily bowel movements were found in about 52% of the children studied. Accordingly, Castro(27) verified low consumption of foods that help bowel function (vegetables, leafy vegetables, fruit laxatives and increase of vegetable oils) in individuals with CP and observed that 94% of the sample presented low fluid intake (water, juice and tea). Among the complications associated with CP, constipation is a consequence of the low mobility of the body, difficulty in fluid intake, and inadequate food intake, due to dysphagia and low motility, because the abdominal muscles are always rigid, which contributes to slow peristalsis and the consequent drying of feces( 28 ).
Exercise may benefit children with CP, improving muscle strength, cardiovascular function, and motor performance( 29 ). It was observed that 93% of respondents were classified as insufficiently active for physical activity of at least 30 minutes, twice a week.
Anthropometric data showed that the group with tetraplegia showed greater nutritional loss and that the most affected ratio is the H/A. This confirms previous results of various authors, such as Pires et al( 10 ), who also identified low values of H/A in individuals with tetraplegia, Grammatikopoulou et al( 30 ), who reported in all studied sample a value <-2 for H/A, regardless of the gravity of the impairment, Dahlseng et al( 31 ), who observed that 20% of 661 diplegic and tetraplegic patients presented H/A and W/A <-2, and Caram et al( 32 ), who, analyzing all kinds of CP, reported that 51% had values below -2 for W/A and 39%, for H/A.
Interestingly, the group with tetraplegia had higher prevalence of difficulty in swallowing and chewing, as observed by other authors, confirming the importance of chewing and swallowing for nutritional status( 32 - 34 ). The difficulty in chewing and swallowing is probably the determining factor in the nutritional status of children with CP and an early identification would allow the monitoring by suitable professionals, assisting the preparation of a more adequate diet for this population. This fact was confirmed by Souza et al( 35 ), who assessed 20 children with CP who were treated at a rehabilitation center and accompanied by a multidisciplinary team. In this group, no impairment of BMI was observed, a fact that was also observed by Pereira Linhares( 20 ).
It should be considered that this study is limited by the sample size, which resulted from selection by convenience. Thus, longitudinal studies are needed, with a representative sample, showing the positive influence of multidisciplinary guidance on the health status of this population, so that the public authority can be convinced that this procedure should become mandatory.
From the data collected and analyzed in the present study, it may be concluded that the children studied have inappropriate dietary patterns and impaired nutritional status, especially in relation to height. Tetraplegia imposes difficulty in chewing/ swallowing and in the practice of moderate physical activity.
Footnotes
Instituição: Centro de Reabilitação de Deficientes Físicos e Mentais do Município de Santos, Santos, SP, Brasil
References
- 1.Brouwer B, Ashby P. Altered corticospinal projections to lower limb motoneurons in subjects with cerebral palsy. Brain. 1991;114:1395–1407. doi: 10.1093/brain/114.3.1395. [DOI] [PubMed] [Google Scholar]
- 2.Piovesana AM, Val JA, Filho, Lima CL, Fonseca MS, Murer AP. Encefalopatia crônica: paralisia cerebral. In: Fonseca LF, Pianetti G, Xavier CC, editors. Compêndio de neurologia infantil. Rio de Janeiro: Medsi; 2002. pp. 826–837. [Google Scholar]
- 3.Low JA, Galbraith RS, Muir DW, Killen HL, Pater EA, Karchmar EJ. Factors associated with motor and cognitive deficits in children after intrapartum fetal hypoxia. Am J Obstet Gynecol. 1984;148:533–539. doi: 10.1016/0002-9378(84)90742-7. [DOI] [PubMed] [Google Scholar]
- 4.Rotta NT. Cerebral palsy, new therapeutic possibilities. J Pediatr (Rio J) 2002;78(Suppl 1):S48–S54. doi: 10.2223/jped.850. [DOI] [PubMed] [Google Scholar]
- 5.Gangil A, Patwari AK, Aneja S, Ahuja B, Anand VK. Feeding problems in children with cerebral palsy. Indian Pediatr. 2001;38:839–846. [PubMed] [Google Scholar]
- 6.Piccoli R, Gelio S, Fratucello A, Valletta E. Risk of low micronutrient intake in neurologically disabled children artificially fed. J Pediatr Gastroenterol Nutr. 2002;35:583–584. doi: 10.1097/00005176-200210000-00025. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan PB, Juszczak E, Lambert BR, Rose M, Ford-Adams ME, Johnson A. Impact of feeding problems on nutritional intake and growth: Oxford Feeding Study II. Dev Med Child Neurol. 2002;44:461–467. doi: 10.1017/s0012162201002365. [DOI] [PubMed] [Google Scholar]
- 8.Aurélio SR, Genaro KF, Macedo ED., Filho Comparative analysis of swallowing patterns between children with cerebral palsy and normal children. Rev Bras Otorrinolaringol. 2002;68:167–173. [Google Scholar]
- 9.Samson-Fang LJ, Stevenson RD. Identification of malnutrition in children with cerebral palsy: poor performance of weight-for-height centiles. Dev Med Child Neurol. 2000;42:162–168. doi: 10.1017/s0012162200000293. [DOI] [PubMed] [Google Scholar]
- 10.Pires PT, Matta DS, Rodrigues AM, Lopes AC, Costa RF, Gil KV. Medidas de peso e estatura de crianças e adolescentes com paralisia cerebral. Med Reabil. 2007;26:11–14. [Google Scholar]
- 11.Santos DC, Serrano HM. Nutritional diagnostic of children and adolescentes with cerebral paralysis helped in an Apae of Vale do Aço. Nutrir Gerais [serial on the Internet]; 2007. [2013 Jan 16]. Available from: http://www.unilestemg.br/nutrirgerais/downloads/artigos/diagnostico_nutricional.pdf. [Google Scholar]
- 12.Rotta NT, Drachler ML, Vaitses VD, Ohlweiler L, Lago IS. Paralisia cerebral: estudo de 100 casos. Rev HCPA. 1983;3:113–116. [Google Scholar]
- 13.Bonomo E. Como medir a ingestão alimentar? In: Dutra JE, editor. Obesidade, anemia carencial na adolescência. São Paulo: Instituto Danone; 2000. pp. 117–126. [Google Scholar]
- 14.Dwyer J, Picciano MF, Raiten DJ, Members of the Steering Committee National Health and Nutrition Examination Survey Estimation of usual intakes: what we eat in America-NHANES. J Nutr. 2003;133:609S–6023. doi: 10.1093/jn/133.2.609S. [DOI] [PubMed] [Google Scholar]
- 15.Dietpro . Dietpro 5.5i Professional: tecnologia para nutrição [CD-ROM] Viçosa: A.S. Sistemas; 2008. [Google Scholar]
- 16.World Health Organization . Diet, nutrition, and the prevention of chronic diseases.Report of a WHO Study Group. Geneva: WHO; 1990. Report of a WHO Study Group. [WHO Technical Report Series 797] [PubMed] [Google Scholar]
- 17.U.S. Department of Health and Human Services; U.S. Department of Agriculture. Dietary guidelines for Americans 2005. Washington: National Academy Press; 2005. [Google Scholar]
- 18.Stevenson RD. Use of segmental measures to estimate stature in children with cerebral palsy. Arch Pediatr Adolesc Med. 1995;149:658–662. doi: 10.1001/archpedi.1995.02170190068012. [DOI] [PubMed] [Google Scholar]
- 19.De Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pereira Linhares FM. Avaliação do estado nutricional de crianças com disfagia por paralisia cerebral. Santa Maria, RS: UFSM; 2004. [Google Scholar]
- 21.Abanto J, Bortolotti R, Carvalho TS, Alves FB, Raggio DP, Ciamponi AL. Assessment of dietary habits of dental interest in children with cerebral palsy. Rev Inst Cienc Saude. 2009;27:244–248. [Google Scholar]
- 22.Silva JV, Timóteo AK, Santos CD, Fontes G, Rocha EM. Food consumption of children and adolescents living in an area of invasion in Maceio, Alagoas, Brazil. Rev Bras Epidemiol. 2010;13:83–93. doi: 10.1590/s1415-790x2010000100008. [DOI] [PubMed] [Google Scholar]
- 23.Mcdonald LA, Wearring GA, Moase O. Factors affecting the dietary quality of adolescent girls. J Am Diet Assoc. 1983;82:260–263. [PubMed] [Google Scholar]
- 24.Woodward DR. What influences adolescent food intakes. Hum Nutr Appl Nutr. 1986;40:185–194. [PubMed] [Google Scholar]
- 25.Rees JM. The overall impact of recently developed foods on the dietary habits of adolescents. J Adolesc Health. 1992;13:389–391. doi: 10.1016/1054-139x(92)90035-a. [DOI] [PubMed] [Google Scholar]
- 26.Tojo R, Leis R, Pavon P. Nutritional needs in adolescence. Risk factors. An Esp Pediatr. 1992;36(Suppl 49):80–85. [PubMed] [Google Scholar]
- 27.Castro FF. Constipação intestinal em pacientes com paralisia cerebral: avaliação dos resultados das internações de enfermagem. Belo Horizonte, MG: UFMG; 2009. [Google Scholar]
- 28.Böhmer CJ, Taminiau JA, Klinkenberg-Knol EC, Meuwissen SG. The prevalence of constipation in institutionalized people with intellectual disability. J Intellect Disabil Res. 2001;45:212–218. doi: 10.1046/j.1365-2788.2001.00300.x. [DOI] [PubMed] [Google Scholar]
- 29.Kelly M, Darrah J. Aquatic exercise for children with cerebral palsy. Dev Med Child Neurol. 2005;47:838–842. doi: 10.1017/S0012162205001775. [DOI] [PubMed] [Google Scholar]
- 30.Grammatikopoulou MG, Daskalou E, Tsigga M. Diet, feeding practices, and anthropometry of children and adolescents with cerebral palsy and their siblings. Nutrition. 2009;25:620–626. doi: 10.1016/j.nut.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 31.Dahlseng MO, Finbråten AK, Júlíusson PB, Skranes J, Andersen G, Vik T. Feeding problems, growth and nutritional status in children with cerebral palsy. Acta Paediatr. 2012;101:92–98. doi: 10.1111/j.1651-2227.2011.02412.x. [DOI] [PubMed] [Google Scholar]
- 32.Caram AL, Morcillo AM, Pinto EA. Nutritional status of children with cerebral palsy. Rev Nutr. 2010;23:211–219. [Google Scholar]
- 33.Sleigh G, Brocklehurst P. Gastrostomy feeding in cerebral palsy: a systematic review. Arch Dis Child. 2004;89:534–539. [PMC free article] [PubMed] [Google Scholar]
- 34.Sullivan PB, Juszczak E, Bachlet AM, Thomas AG, Lambert B, Vernon-Roberts A, et al. Impact of gastrostomy tube feeding on the quality of life of carers of children with cerebral palsy. Dev Med Child Neurol. 2004;46:796–800. doi: 10.1017/s0012162204001392. [DOI] [PubMed] [Google Scholar]
- 35.Souza KE, Sankako AN, Carvalho SM, Braccialli LM. Classification of gross motor function injury and body mass index in children with cerebral palsy. Rev Bras Crescimento Desenvolvimento Hum. 2011;21:11–20. [Google Scholar]