Abstract
Objective:
To systematically review the literature on the telehealth initiatives in telerehabilitation practices in children and adolescents from zero to 18 years old.
Data sources:
Randomized and controlled clinical trials published in the past ten years (January 2002 to February 2012) in Medline/PubMed, Medline/BVS, PEDro and Cochrane Library databases. The descriptors "telemedicine", "rehabilitation" and "telehealth" were used in three different languages (English, Portuguese and Spanish).
Data synthesis:
From the 20 studies found in the literature, nine were included in this review. Most of the studies showed that telerehabilitation is able to produce better results in the treatment when compared to the traditional methods, providing less frequency of symptoms, better disease control, better quality of life and greater adherence to treatment.
Conclusions:
Telerehabilitation is a viable and effective strategy in the treatment of common diseases in children and adolescents. However, there are few studies on the subject in this age group. Although telehealth is already consolidated worldwide, there are no studies in Brazil that used the telerehabilitation in children and adolescents, which reinforces the need for more research and investments.
Keywords: telemedicine, rehabilitation, telenursing, remote consultation
Abstract
Objetivo:
Conocer las iniciativas de aplicación de la tele salud en las prácticas de tele-rehabilitación en niños y adolescentes de cero a 18 años, a partir de revisión sistemática de la literatura.
Fuentes de datos
: Ensayos clínicos controlados y aleatorios publicados los últimos diez años (enero de 2002 a febrero de 2012) en las bases Medline/PubMed, Medline/BVS, PEDro y Biblioteca Cochrane. Los descriptores "telemedicina", "rehabilitación" y tele salud fueron utilizados en tres distintos idiomas (portugués, inglés y español).
Síntesis de los datos:
De los 20 estudios encontrados en la literatura, nueve fueron incluidos en esta revisión. La mayoría de los estudios demostró que la tele-rehabilitación es capaz de producir mejores resultados en el tratamiento cuando comparada a los métodos de rehabilitación tradicionales, proporcionando reducción en la ocurrencia de síntomas, mejora en la calidad de vida, mayor control de las enfermedades y mayor adhesión al tratamiento.
Conclusiones:
La tele-rehabilitación es una estrategia viable y efectiva en el tratamiento de patologías frecuentes en niños y adolescentes. Sin embargo, hay pocos estudios sobre el uso de la tele-rehabilitación en esa franja de edad. Aunque la salud ya esté consolidada en nivel mundial, no se localizaron estudios realizados en Brasil que utilizaran la tele-rehabilitación en niños y adolescentes, lo que refuerza la necesidad de mayor número de investigaciones e inversiones.
Introduction
In recent years, contributions from technological development to projects in the area of health have increased, with a consequent increase in the sharing of knowledge and skills of health care offered to the population( 1 ). One of the successful initiatives of the incorporation of technology in health care is telemedicine or telehealth, defined by the World Health Organization (WHO) as the provision of health services in cases where distance is a critical factor. Telehealth emerges as a political and strategic instrument to plan and perform actions on health, allowing an exchange of important information for the diagnosis, prevention, and treatment of diseases. In addition, telehealth is used for continuing education of service providers, as well as for research and evaluation( 2 , 3 ).
Traditionally, heath care service occurs from a face-toface meeting. With the use of technological resources of telehealth, it is possible to conduct a "virtual meeting" between health professionals and patients and among health professionals themselves, whenever the distance or other factors prevent the contact in person. This peculiar feature, which escapes conventional standards, changes paradigms and has legal and ethical implications( 1 , 3 ). To ensure the secrecy and confidentiality of information, it is necessary, in addition to an appropriate location, to train all staff involved, once this is not composed only by health care professionals( 3 ). However, ethical and legal guidelines, provided they are taken into consideration, do not prevent patients and professionals from making use of telehealth.
Rehabilitation is a comprehensive, dynamic, multi-professional process, which aims not only to recover, but also to reinstate the individual to society. It is concerned with the biopsychosocial well-being of the patient and its actions include multivariate and complementary fields, such as education, employment, welfare, and leisure( 4 , 5 ). Expanding and developing interfaces of rehabilitation with telerehabilitation can be an important strategy for increasing the effectiveness and efficiency of rehabilitation actions.
Telerehabilitation, defined as the method by which communication technologies are used to provide distance rehabilitation, although still underused, has been efficient and effective in comparison to conventional rehabilitation clinical practices( 6 ). In adult patients, there is a greater description in the literature on the use of telerehabilitation for cases of osteoarthritis( 7 ), cardiac rehabilitation( 8 ), chronic obstructive pulmonary disease( 9 ), dysarthria( 10 ), among others. However, when considering the juvenile population, the practice of telerehabilitation is scarce. Description of its use can be found in the treatment of asthmatic children with attention deficit disorder and hyperactivity, delayed oral language development, diabetes, and in controlling adolescent smokers( 11 , 12 ).
Considering the potential of telehealth practices for the successful treatment of patients in rehabilitation and the scarcity of studies in the literature on telerehabilitation in the juvenile population, a further clarification on the subject is necessary. It is believed in the importance of the use of telehealth in rehabilitation practice, and therefore, this study conducted a survey of the bibliographic production in the area, to provide health professionals with greater knowledge regarding the use of information and communication technologies for the success of rehabilitation practices. Therefore, this study aimed to investigate the initiatives of telehealth application in telerehabilitation practices in children and adolescents aged from zero to 18 years.
Method
This was a systematic review of the literature on randomized controlled trials about the use of telehealth in the rehabilitation of children and adolescents. The review was done according to the steps of the Cochrane Collaboration Library. The following items were predefined and limited: the topic of interest and the formulation of the guiding question; the search and selection strategies; the criteria for inclusion and exclusion; the assessment of the methodological quality of studies; and the development of a form for the presentation, analysis, and interpretation of data extracted from the studies. The guiding question that conducted this systematic review was: "how is the use of telehealth in telerehabilitation practices in children and adolescents from zero to 18 years?"
Searches were conducted in Medline/PubMed, Medline/ BVS, PEDro and Cochrane Library databases (Table 1), using the keywords: "telemedicine", "rehabilitation" and "telehealth", in Portuguese, English, and Spanish. In the search strategy, we delimited the search for papers published from January 2002 to February 2012.
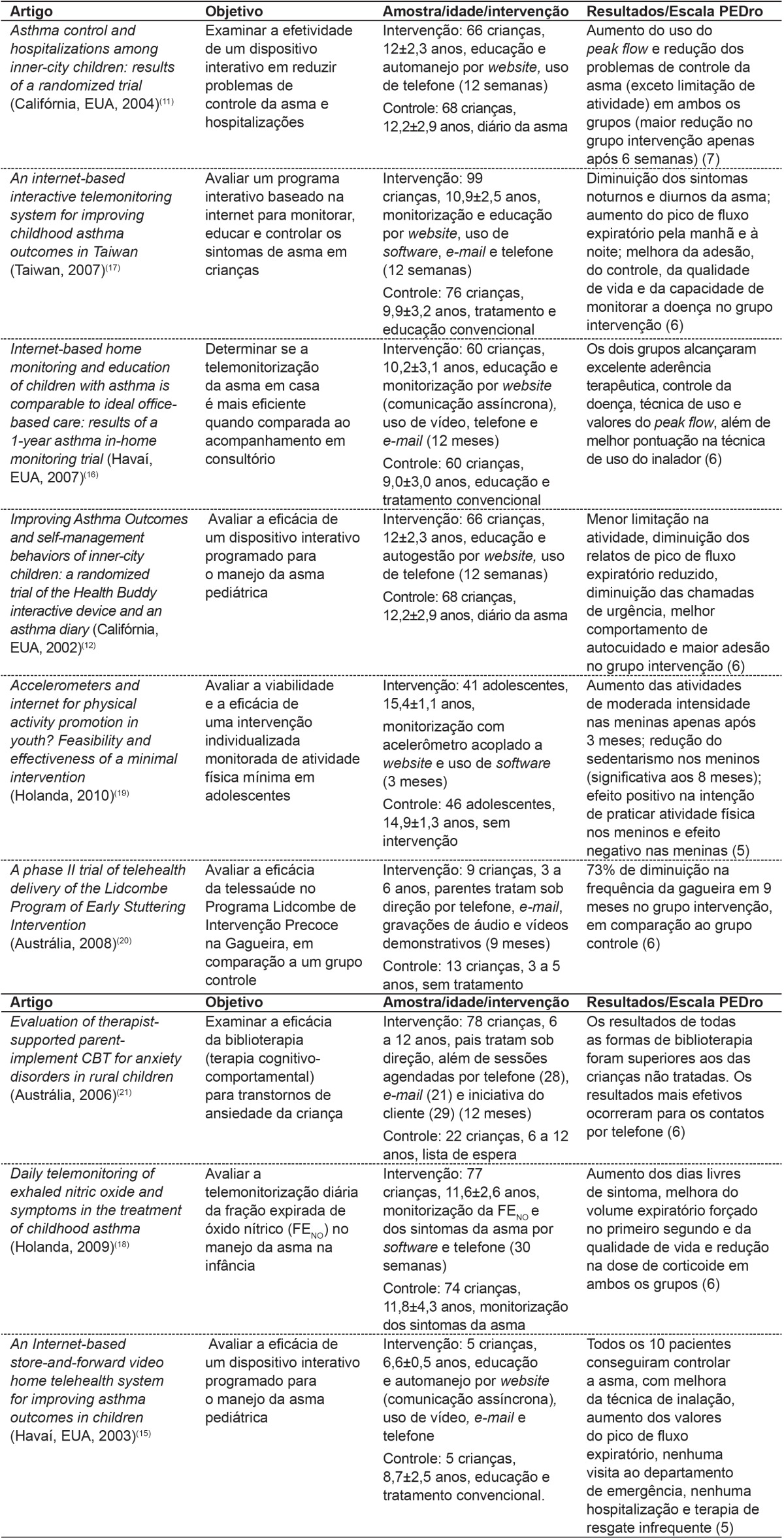
Table 1. Results and key findings from selected studies.

The study included only randomized controlled trials, available in full text, considering only studies with a target population of children and adolescents up to 18 years and that covered the topic of telerehabilitation. The following studies were excluded: those that were not randomized controlled trials, those not available in full, those whose participants were not exclusively under 19, and those whose theme was not telerehabilitation.
The articles were read in full and evaluated independently by two authors. The methodological quality of the studies was assessed with the PEDro scale, currently the most widely used in the area of rehabilitation( 13 ). This scale was developed by the Physiotherapy Evidence Database to be applied in experimental studies and has a total score of ten points, including assessment criteria for internal validity and presentation of statistical analysis employed. In case of discrepancy in scores between the two raters, a consensus was sought. When necessary, a third opinion was requested.
The PEDro scale consists of the following criteria: 1) specification of inclusion criteria; 2) random allocation; 3) concealed allocation; 4) similarity of the groups at baseline; 5) blinding of subjects; 6) blinding of therapists; and 7) blinding of assessors, 8) measures of at least one key outcome obtained from more than 85% of the subjects allocated, 9) intention to treat analysis; 10) between-group statistical comparisons reported for at least one key outcome; and 11) point measures and measures of variability for at least one key outcome ( 13 , 14 ). In this scale, when a defined criterion is clearly satisfied, a point is scored, except in the case of the first criterion (the only one not punctuated in the scale).
To extract data from the selected articles, an instrument that included the following variables was created: study identification (title and authors), year of publication, country of research, the issue addressed in telerehabilitation, age range, sample size, interventions, results/conclusions and PEDro score.
Results and Discussion
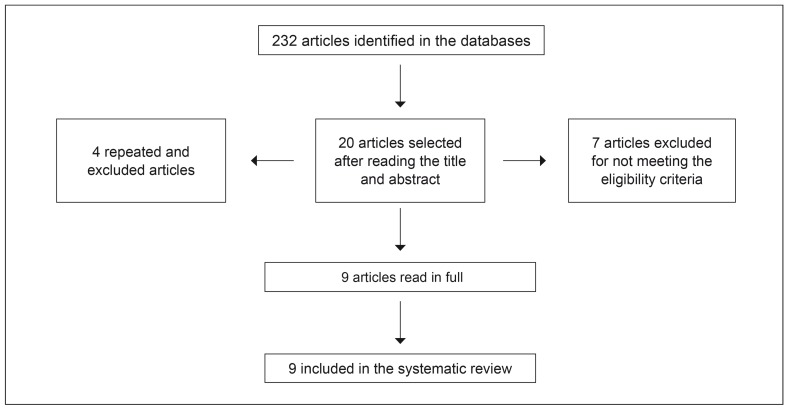
In the present search, 232 articles were found, 125 from the Cochrane Library, 38 from PEDro base, 35 from PubMed, and 34 from Medline. After reading the title and abstract of each article, 212 studies were discarded by repetition in different search bases or due to non-compliance with the eligibility criteria proposed, leaving only 20 articles for full review (four from the Cochrane Library, eight from PubMed, four from Medline, and from PEDro). Among these, seven were excluded because they did not fit the inclusion criteria, and three, because they were repeated in the databases (Figure 1), totaling nine articles for this review (Table 1). After the initial screening of articles, we performed the reading in full and the quality assessment of the nine selected papers. From the analyses of the texts, it was noticed that most (55.6%) of the included articles adopted, as an intervention methodology, the comparison between the traditional method of rehabilitation versus telerehabilitation( 11 , 12 , 15 - 17 ).
Figure 1. Flow chart of the different phases of the systematic review.
It was also verified that the United States( 11 , 12 , 15 , 16 ) (44.4%), followed by the Netherlands( 18 , 19 ) (22.2%), Australia(20,21) (22.2%), and Taiwan( 17 ) (11.1%), demonstrated a greater interest in investigating the issue of telerehabilitation in children and adolescents. Although telehealth is already consolidated worldwide, no studies were found in Brazil that used the methodology of telerehabilitation in children and adolescents. This finding allows us to affirm that this is a fairly unexplored area in the country, requiring further studies and investments. Moreover, in general, the access to technology is not yet a reality to the whole population, unlike developed countries where the studies took place.
The main theme explored by the analyzed studies was asthma( 11 , 12 , 15 - 18 ), the most prevalent chronic disease among children, which constitutes a serious public health problem( 22 ). This fact may explain the recurrence of the theme when studying the child population.
Most selected studies (88.9%) involved children aged from 6 years. Children have contact with the technological innovations increasingly early. Nowadays, this contact can be used as a strategy for education and motivation, from the use of playful actions that interest children. On several occasions, the child alone can get in touch with technology. However, in children younger than 6 years, a greater involvement of parents/family members is necessary, which may hinder the implementation of telerehabilitation. Only one study, among the selected ones, included children younger than 6 years, due to the need to initiate treatment for stuttering earlier, with constant parental involvement in the process( 21 ).
When observing the interventions reported in telerehabilitation, it was verified the use of the most varied forms of technology to implement the new treatment programs. The internet, with the use of websites, software, and email for communication, was a strategy present in all analyzed studies. Besides the internet, other resources were employed to implement the programs of telerehabilitation, such as telephone (88.9%)( 11 , 12 , 15 - 18 , 21 , 22 ), videos (33.3%)( 15 , 16 , 20 ), and audio recordings (11.1%)( 20 ). This reality can be justified by the facility of use of computers by children and adolescents in the present day. Currently, computers and the internet are no longer barriers to the acquisition of knowledge, being attractive to the young public( 23 ). Moreover, in the countries where the studies were carried out, access to technology is a reality for most of the population, facilitating the implementation of programs of telerehabilitation mediated through the Internet.
When observing the interventions reported in telerehabilitation, it was verified that all interventions proposed by the included studies were conducted with the focus on the treatment of diseases already present, especially asthma. Only one study using the accelerometer as a methodology for increasing physical activity in adolescents( 19 ) focused on health promotion and disease prevention. Moreover, some of the interventions of telerehabilitation proposed required a minimum period of time to achieve the results( 11 , 12 , 17 , 19 ). The use of technologies, especially those able to motivate and attract children and adolescents, may have been a potentiating factor for the positive findings, when compared to traditional rehabilitation therapies( 12 , 17 ).
The quality of the studies was determined from the score on the PEDro scale. Due to the impossibility to conduct a randomized controlled trial in the area of telerehabilitation with blinding of therapists or subjects, the maximum PEDro score achievable for the studies analyzed was of 8 in 10. Most of the selected studies in this systematic review presented high methodological quality, i.e., a score ≥6 (75% of the maximum possible score), as shown in Table 1.
It should be mentioned that this review presented some limitations, such as the small number of studies that met the criteria and the heterogeneity of the selected studies in several aspects: topic covered, age range, sample size, type of technology used, duration of intervention, and follow-up. These limitations prevented quantitative analysis or deeper inferences about the effectiveness of telerehabilitation. It was also observed that only 66.7% of the articles( 11 , 12 , 16 - 19 ) performed the sample calculation to define the sample and the study power. It is known that proper sizing of the sample and the appropriate analysis of error of method is an important step in validating the data obtained in a particular scientific study( 24 ).
In general, most studies have demonstrated that the inclusion of telerehabilitation is able to produce superior results( 11 , 12 , 17 ) or similar( 15 , 16 ), when treatment is compared to traditional methods of rehabilitation. Among the studies that show superior results, it was observed a decrease in the occurrence of symptoms( 11 , 12 , 17 ), improvement in quality of life( 17 ), grater control of the diseases( 11 , 17 ), greater treatment adherence( 11 , 12 , 17 ), and greater practice of physical exercise( 12 , 17 ).
Furthermore, distant rehabilitation appears to be a safe intervention, because there was virtually no reporting of adverse events in the studies listed, as the absence of feedback from participants, poor adherence, or loss of confidentiality of records and errors on data transmission or interpretation of information( 3 ). Only one study had fewer visits to the website and a high dropout rate, perhaps because it is the only one that evaluated healthy participants, what may explain the lack of interest in the approach( 19 ). This result indicates that by using technology in rehabilitation, there should be some care so that adverse events do not occur. It is necessary that the educational material used is appropriate to the audience and that the strategies used are able to promote adherence to treatment, providing satisfactory results.
Only two studies evaluated the cost of telerehabilitation compared to conventional treatment( 16 , 20 ) and results shown were contradictory. While one of them observed reduction in costs by half compared to the conventional treatment( 16 ), the other reported a 3-fold increase in the intervention group( 20 ). The final study compared measures of treatment time recorded in the intervention group (the distance version of the conventional model of rehabilitation of stuttering) with measures of treatment time program offered in the conventional manner, which were not evaluated in this study.
For the telerehabilitation to be effective, a high initial investment is necessary for the purchase of equipment, for professional training, and for the production of technological resources that meet the developmental stages of children and adolescents. However, as stated earlier, it not yet possible to say whether the initial costs is offset by the benefits from the practice, which, once implemented, requires maintenance and technological upgrades. The lack of evaluation of the resources used for telerehabilitation is observed in most studies, but it appears that the costs may change over time( 6 ). It is known that dealing with new technologies is an undeniable need and new concepts are being incorporated by the area of health. However, some issues raise concerns on the part of managers and health professionals. Technology should be a means of connection between patient and professional. By using telerehabilitation, the professional will not be close to the patient to provide the feedback it needs. Therefore, in cases where the telerehabilitation is indicated and feasible, the training and the constant improvement of professionals, parental monitoring regarding the treatment of children, and the availability of pedagogic resources that facilitate the approach are needed. These practices must be conceived as ways of stimulating motivation, to ensure adherence, providing better results and prognostics in rehabilitation.
Conclusions
Telerehabilitation is a possible, effective and secure strategy for the treatment of common diseases in children and adolescents, according to the high-quality studies analyzed. However, there were few studies available, and they were heterogeneous with regard to the use of telerehabilitation in this age range. There is yet no evidence of the cost or even cost-benefit of this new therapeutic modality, which reinforces the need for more research and careful investments in the area of telerehabilitation. It is noteworthy that this treatment does not come with the intention of replacing the traditional practices of rehabilitation, and should be considered as an alternative to be associated with conventional treatment, improving it.
Acknowledgements
We are thankful to Professor Maria do Carmo Melo, for giving us the opportunity to learn about telerehabilitation and telehealth.
Footnotes
Instituição: Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brasil
References
- 1.Santos AF, Souza C, Alves HJ, Santos SF. Telessaúde: um instrumento de suporte assistencial e educação permanente. Belo Horizonte: UFMG; 2006. [Google Scholar]
- 2.Organização Mundial da Saúde [cited 2012 Mar 20];[homepage on the Internet]. Telemedicine. 2012 a Available from: Available from: http://www.who.int/goe/publications/ goe_telemedicine_2010.pdf.
- 3.Rezende EJ, Melo MC, Tavares EC, Santos AF, Souza C. Ética e telessaúde: reflexões para uma prática segura. Rev Panam Salud Publica. 2010;28:58–65. doi: 10.1590/s1020-49892010000700009. [DOI] [PubMed] [Google Scholar]
- 4.Portugal - Ministério da Saúde . Direcção-Geral da Saúde - Direcção de Serviços de Planeamento.Rede de referenciação hospitalar de medicina física e de reabilitação. Lisboa: Direcção-Geral da Saúde; 2003. [Google Scholar]
- 5.Brasil - Conselho Federal de Fisioterapia e Terapia Ocupacional . Resolução nº 80, de 9 de maio de 1987.Dispõe sobre a atuação do Fisioterapeuta como auditor e dá outras providências. Brasília: Diário Oficial da União; 1987. [Google Scholar]
- 6.Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, health care utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31:427–447. doi: 10.1080/09638280802062553. [DOI] [PubMed] [Google Scholar]
- 7.Blixen CE, Bramstedt KA, Hammel JP, Tilley BC. A pilot study of health education via a nurse-run telephone self-management programme for elderly people with osteoarthritis. J Telemed Telecare. 2004;10:44–49. doi: 10.1258/135763304322764194. [DOI] [PubMed] [Google Scholar]
- 8.Johansson T, Wild C. Telerehabilitation in stroke care - a systematic review. J Telemed Telecare. 2011;17:1–6. doi: 10.1258/jtt.2010.100105. [DOI] [PubMed] [Google Scholar]
- 9.McLean S, Nurmatov U, Liu JL, Pagliari C, Car J, Sheikh A. Telehealthcare for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;(7):CD007718–CD007718. doi: 10.1002/14651858.CD007718.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hill AJ, Theodoros DG, Russell TG, Ward EC. The redesign and re-evaluation of an internet-based telerehabilitation system for the assessment of dysarthria in adults. Telemed J E Health. 2009;15:840–850. doi: 10.1089/tmj.2009.0015. [DOI] [PubMed] [Google Scholar]
- 11.Guendelman S, Meade K, Chen YQ, Benson M. Asthma control and hospitalizations among inner-city children: results of a randomized trial. Telemed J E Health. 2004;10(2):S6–14. [PubMed] [Google Scholar]
- 12.Guendelman S, Meade K, Benson M, Chen YQ. Improving asthma outcomes and self-management behaviors of inner-city children: a randomized trial of the Health Buddy interactive device and an asthma diary. Arch Pediatr Adolesc Med. 2002;156:114–120. doi: 10.1001/archpedi.156.2.114. [DOI] [PubMed] [Google Scholar]
- 13.Sampaio RF, Mancini MC. Sytematic review studies: a guide for carefull synthesis of the scientific evidence. Rev Bras Fisioter. 2007;11:83–89. [Google Scholar]
- 14.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 15.Chan DS, Callahan CW, Sheets SJ, Moreno CN, Malone FJ. An Internet-based store-and-forward video home telehealth system for improving asthma outcomes in children. Am J Health Syst Pharm. 2003;60:1976–1981. doi: 10.1093/ajhp/60.19.1976. [DOI] [PubMed] [Google Scholar]
- 16.Chan DS, Callahan CW, Hatch-Pigott VB, Lawless A, Proffitt HL, Manning NE, et al. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: results of a 1-year asthma in-home monitoring trial. Pediatrics. 2007;119:569–578. doi: 10.1542/peds.2006-1884. [DOI] [PubMed] [Google Scholar]
- 17.Jan RL, Wang JY, Huang MC, Tseng SM, Su HJ, Liu LF. An internet-based interactive telemonitoring system for improving childhood asthma outcomes in Taiwan. Telemed J E Health. 2007;13:257–268. doi: 10.1089/tmj.2006.0053. [DOI] [PubMed] [Google Scholar]
- 18.De Jongste JC, Carraro S, Hop WC, CHARISM Study Group. . Baraldi E. Daily telemonitoring of exhaled nitric oxide and symptoms in the treatment of childhood asthma. Am J Respir Crit Care Med. 2009;179:93–97. doi: 10.1164/rccm.200807-1010OC. [DOI] [PubMed] [Google Scholar]
- 19.Slootmaker SM, Chinapaw MJ, Seidell JC, van Mechelen W, Schuit AJ. Accelerometers and Internet for physical activity promotion in youth? Feasibility and effectiveness of a minimal intervention. Prev Med. 2010;51:31–36. doi: 10.1016/j.ypmed.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 20.Lewis C, Packman A, Onslow M, Simpson JM, Jones M. A phase II trial of telehealth delivery of the Lidcombe Program of Early Stuttering Intervention. Am J Speech Lang Pathol. 2008;17:139–149. doi: 10.1044/1058-0360(2008/014). [DOI] [PubMed] [Google Scholar]
- 21.Lyneham HJ, Rapee RM. Evaluation of therapist-supported parent-implement CBT for anxiety disorders in rural children. Behav Res Ther. 2006;44:1287–1300. doi: 10.1016/j.brat.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 22.Chatkin MN, Menezes AM. Prevalence and risk factors for asthma in schoolchildren in Southern Brazil. J Pediatr (Rio J) 2005;81:411–416. doi: 10.2223/JPED.1393. [DOI] [PubMed] [Google Scholar]
- 23.Araújo MJ. O jogo, a internet e o mundo das crianças. Proceedings of the VI Congresso Português de Sociologia - mundos sociais: saberes e práticas; - 2008. [Google Scholar]
- 24.Normando D, Almeida MA, Quintão CC. Analysis of the use of sample size calculation and error of method in researches published in Brazilian and international orthodontic journals. Dental Press J Orthod. 2011;16:33–35. [Google Scholar]