Abstract
Acute HIV infection (AHI) is a relatively brief period when individuals are highly infectious and the opportunity to intervene to prevent forward transmission is extremely limited. HPTN 062 partnered with CHAVI 001 to evaluate the feasibility and acceptability of a motivational interviewing (MI)-based counseling intervention to reduce HIV-transmission risk behaviors among individuals with acute and early HIV infection in Lilongwe, Malawi. Participants were randomized to receive either (1) brief education sessions about HIV and AHI; or (2) the same brief education sessions plus an MI-based counseling intervention called Uphungu Wanga. Although Uphungu Wanga was determined to be feasible and acceptable, few major differences existed between the two arms with regard to acceptability, feasibility, and self-reported sexual behaviors. We therefore conclude that an additional MI-based counseling intervention may not be needed during the short period of AHI. Instead, we recommend that individuals with AHI receive frequent, but brief, counseling immediately after diagnosis and then transition to receiving counseling at less frequent intervals until they can initiate antiretroviral therapy. Other recommendations are provided.
Keywords: Acute HIV infection, HIV prevention, Motivational Interviewing, counseling, Malawi
Introduction
Acute HIV infection (AHI) is the period just following HIV infection when, due to a lack of an immediate immune response, the viral burden is dramatically high before receding to a lower set point [1]. During AHI, the HIV-transmission risk is sharply elevated, and up to 40% of new HIV infections are attributed to transmission during this brief period of time [2]. Previous research has demonstrated that some individuals diagnosed with AHI continue to engage in sexual activity, including unprotected sex, suggesting that interventions beyond post-test counseling are needed to reduce forward transmission [3, 4]. Currently, no guidelines are available on the prevention of forward transmission of HIV during AHI and no behavioral interventions for individuals with AHI have been evaluated and published, to our knowledge.
HPTN 062 evaluated the feasibility and acceptability of a motivational interviewing (MI)-based intervention to reduce HIV-transmission risk behaviors among individuals with acute and early HIV infection in Lilongwe, Malawi. To be most effective, interventions to prevent forward transmission during AHI must be delivered immediately after an AHI diagnosis, while individuals are still highly infectious [5], yet identifying such individuals is time- and resource-intensive [6, 7]. We therefore partnered with the Center for HIV/AIDS Vaccine Immunology (CHAVI) 001 study to deliver the HPTN 062 intervention. CHAVI 001 was a prospective, non-intervention cohort study of individuals with AHI who were identified and enrolled for the evaluation of cellular, antibody, and mucosal responses during AHI [8]. Interventions designed to prevent the forward transmission of HIV during the period of AHI also require a different strategy from other “prevention-for-positives” interventions. Individuals with AHI are highly infectious, they likely are currently engaging in risky behavior since they were very recently infected, they are coping with a new diagnosis, and the period to intervene is extremely limited. Counselors must therefore quickly build rapport, and individuals with AHI must rapidly reduce their risk behaviors. Hence we designed our counseling intervention to consist of several sessions over a brief period immediately after an AHI diagnosis and to focus on short-term prevention goals.
In this article, we describe data related to the two primary objectives of HPTN 062: (1) to assess the feasibility of enrolling and delivering MI-based counseling to individuals in the acute and early phases of HIV infection; and (2) to evaluate the acceptability of the counseling among participants.
Methods
Study Population
Between February 2010 and December 2011, individuals who sought HIV testing at the Kamuzu Central Hospital’s sexually transmitted infections clinic and who were identified as having AHI were enrolled in CHAVI 001 and subsequently invited by CHAVI 001 staff to co-enroll in HPTN 062. To be eligible for participation in HPTN 062, participants had to be 18 years of age or older and have an acute or early HIV infection. AHI, per CHAVI protocol, was defined as having parallel sero-negative results with a positive nucleic acid test (NAT). Early HIV infection was defined as having a positive or discordant parallel serologic result, a positive NAT, and an evolving, negative, or indeterminate Western Blot.
Study Design
HPTN 062 was a single-site, two-arm, randomized pilot intervention study (Fig. 1). Upon AHI diagnosis, all participants received WHO standard-of-care (SOC) post-test counseling [9]. After providing written informed consent, participants were randomized in a 1:1 ratio to (1) Arm 1, brief education on HIV and AHI provided by CHAVI 001; or (2) Arm 2, the brief education plus the MI-counseling intervention called Uphungu Wanga, which means “my own counseling.”
Fig. 1.
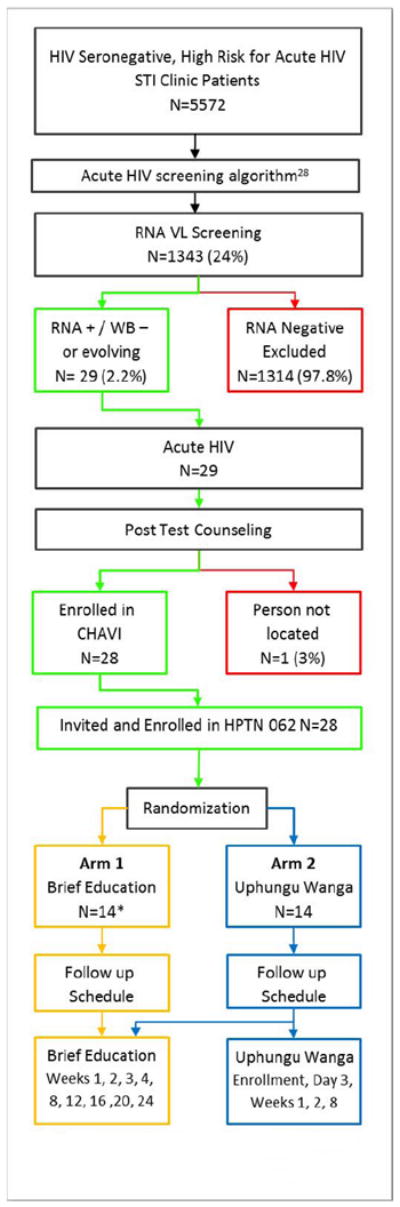
HPTN 062 Study flow; participants enrolled between February 2010 and December 2011.
*One participant was removed from analysis, false acute
Participants in both arms were followed for 24 weeks. The HPTN 062 study visits were conducted at weeks 1, 2, 3, 4, 8, 12, 16, 20, and 24 post-diagnosis, which coincided with the CHAVI 001 clinic visit schedule. As part of the CHAVI 001 study, all participants received the brief education at each visit. Participants in Arm 2 also received five Uphungu Wanga sessions: on the day of AHI diagnosis, 3 days later, and at the weeks 1, 2, and 8 visits post-diagnosis. At each study visit, participants in Arm 2 completed all the CHAVI 001 study procedures, including the brief education, before going to a separate location on the same hospital campus to proceed with the Uphungu Wanga counseling. Arm 2 participants met with the same Uphungu Wanga counselor during each visit. Per standard practice in Malawi, counselors and participants were not matched by gender in the brief education or in the Uphungu Wanga counseling sessions. Messages about AHI, developed by the study team (Table 1), were delivered during the brief education and during the Uphungu Wanga counseling.
Table 1.
Main AHI messages.
The following messages were communicated to participants in both arms:
|
Arm 1 — Brief Education
The brief education was administered by male or female study nurses as part of a CHAVI 001 clinic visit. During each visit, participants were asked about any concerns they had in general, received the brief education, and completed all CHAVI 001 study visit clinical procedures, all in the same room with a single CHAVI 001 study staff member. The brief education consisted of providing all participants with information about (1) ways to live as health fully as possible with HIV, including information about good nutrition, exercise, spending time with loved ones, and seeking support in the community; (2) AHI (Table 1); and (3) safer sex. Participants’ psychosocial support needs were also informally explored.
Arm 2 — Brief Education plus Uphungu Wanga
Participants in Arm 2 received the brief education as part of their CHAVI 001 study visit, plus five Uphungu Wanga sessions (four within the first two weeks post-diagnosis and then a booster session at the week 8 visit). The Uphungu Wanga counseling sessions (Table 2) were primarily delivered by one of two experienced female counselors; a trained, male back-up counselor facilitated all five Uphungu Wanga sessions for two participants. The counseling program was informed by data from formative research conducted among CHAVI 001 participants [3] and developed through the adaptation and integration of aspects from two effective interventions to reduce risky sexual behaviors among people living with HIV — the Options Project [10] and Project Safe Talk [11-13]. Uphungu Wanga was based on the information—motivation—behavioral skills (IMB) model [14], and implemented using MI, a client-centered style of directed counseling that focuses on enhancing motivation for behavioral change [15-17]. The IMB model and MI were chosen for this intervention because they have been used in previous interventions shown to reduce sexual risk behaviors among people living with HIV [10, 12, 18, 19]. All Uphungu Wanga sessions incorporated the IMB framework; counselors assessed a participant’s knowledge of AHI and provided tailored additional explanation as needed, assessed motivation for behavior change, assessed self-efficacy to practice their chosen risk reduction strategy, and tailored counseling accordingly based on a standardized counseling guide.
Table 2.
Overview of Uphungu Wanga counseling sessions.
|
The HPTN 062 counselors participated in 5 days of training — facilitated by MI experts and informed by a step-by-step training manual — on MI counseling techniques and on the use of standardized session guides to deliver the intervention. The Uphungu Wanga counselors did not provide counseling to participants in Arm 1 or the brief education to participants in Arm 2; the nurses who provided the brief education were blinded to the HPTN 062 randomization. To help the counselors maintain fidelity to the protocol, they used quick reference guides — which outlined the key intervention steps of each session — during the counseling session.
Three core components formed the foundation of the Uphungu Wanga intervention:(1) facilitating understanding of AHI;(2) enhancing motivation and skills to maintain abstinence or 100% condom use during the period of AHI; and (3) supporting disclosure of one’s HIV status to current partners. We included the disclosure of one’s HIV status as a core component based on previous research, which suggested that not informing partners of one’s HIV diagnosis was a barrier to practicing risk-reduction behaviors during AHI[3].
The details of the Uphungu Wanga sessions are provided in Table 2. The first and second Uphungu Wanga sessions focused on two activities: ensuring that participants understood the implications of increased infectiousness and identifying individualized risk-reduction goals for participants to try in the few days following each session. In the third and fourth sessions, the counselor followed up on the goals that were previously identified for risk reduction and introduced a new topic, namely “disclosure of HIV status” in session 3 and “topic choice” in session 4. During “topic choice,” participants chose a topic of interest among a set menu of topics. The final session focused on transitioning from the acute to the established phase of HIV infection and planning for longer-term health management.
The National Health Science Research Committee in Malawi and the Protection of Human Subjects Committee (PHSC) at FHI 360 in the United States approved the study. The institutional review board at the University of North Carolina at Chapel Hill provided ongoing review of the study but deferred approval authority to the PHSC.
Measures and Data Collection
Acceptability Measures
We conducted a quantitative face-to-face interview with (1) participants in Arm 2 after each of the five Uphungu Wanga sessions and (2) participants in Arm 1 after the SOC counseling at enrollment and the brief education sessions at weeks 1, 2, and 8. The interviews were administered by staff members who did not facilitate the Uphungu Wanga counseling, brief education, or SOC counseling. The questions focused on the counseling format (e.g., length of sessions), content of the counseling (e.g., satisfaction with the session, whether the participant’s questions were adequately addressed), perceived effectiveness of the counseling, and the participant’s perceptions of her or his interactions with the counselors (e.g., comfort level, honesty). Participants in Arm 2 were asked to focus their answers on the Uphungu Wanga counseling rather than on the brief education and SOC counseling that they had also received. Additional quantitative questions about the format of the Uphungu Wanga intervention (e.g., acceptability of the number of sessions) and preference for the type of counseling, either Uphungu Wanga or the brief education, were asked of participants in Arm 2 at week 2.
We also conducted qualitative, semi-structured interviews (SSI) to explore the acceptability of the counseling interventions with participants in both arms at weeks 2 and 8. The SSIs were conducted by the same interviewer who conducted the quantitative interviews. Interviewers asked participants to describe the experiences that influenced their perceptions of the acceptability of the counseling that they had reported in the quantitative interview. Participants in Arm 2 were also asked to compare and contrast the brief education and the Uphungu Wanga counseling sessions. Interviews were audiotaped with the participant’s permission; detailed notes were taken when a participant preferred not to be audiotaped (n=1 at both weeks 2 and 8). All interviews were conducted in Chichewa, the local language.
Feasibility Measures
Feasibility was measured by (1) the proportion of participants in Arm 2 who had attended all four of the Uphungu Wanga sessions between enrollment and the week 2 visit; and (2) the proportion of participants in Arms 1 and 2 who had attended the brief education or the brief education plus all five of the Uphungu Wanga sessions, respectively, between enrollment and the week 8 visit.
Quality Assurance and Fidelity to the Uphungu Wanga Intervention
We assessed several intervention fidelity components recommended by the NIH Behavior Change Consortium [20] as well as observed counseling sessions to ensure the quality of the counseling was maintained. Each counselor was observed facilitating at least three of the five Uphungu Wanga sessions (the majority unannounced) by the site coordinator. The goal was to improve each counselor’s skills by providing feedback when needed and to determine whether the session was delivered as intended (e.g., with the main components discussed). Some flexibility in the session topics was expected to address the participants’ needs and to maintain rapport between the counselors and the participants. We also administered a questionnaire to the participants in Arm 1 after sessions 1 and 2 of the brief education and to the participants in Arm 2 after each Uphungu Wanga counseling session to document the topics that were discussed during the session. Uphungu Wanga counselors and CHAVI 001 providers also documented the topics that were discussed at each of their respective sessions. We also measured the “treatment dose” [20] — defined as the number of sessions, the frequency of the sessions, and the length of each session (through counselor documentation of the time of intervention start and end) in each study arm — cognizant that these measures would differ between the two study arms because of the intervention’s design.
Analysis
Descriptive statistics were used to summarize the proportion of participants in each arm who attended the study visits and the frequency of responses to each quantitative acceptability question. Baseline participant characteristics and preferred time with counselors were compared between the two study arms using Fisher’s Exact test, and the length of the brief education and Uphungu Wanga sessions were compared using Wilcoxon Rank Sums test. The study was not powered to evaluate the efficacy of the intervention effect.
For the qualitative data, the audiotaped SSIs were transcribed and translated simultaneously from Chichewa into English by the bilingual interviewer; a standardized transcription protocol was followed [21]. For interviews not audiotaped, detailed notes were expanded immediately after the interview to capture as much of the content as possible. Two analysts applied structural codes [22] that were directly linked to the acceptability questions to the data using NVivo 9 [23]. Three rounds of coding review were conducted by the two analysts at different points throughout the analysis to confirm intercoder reliability. During each review, analysts selected transcripts that were complex or rich in data and coded the same transcripts independently. Codes were then reviewed by the analysts, discrepancies discussed, and the codebook revised and transcripts recoded as needed. Intercoder agreement was determined to be 90% or above at each review. Coding reports were produced for each of the acceptability codes, followed by data summaries that described the themes within each code and provided illustrative quotes.
Results
Study Participants
We enrolled 28 participants; 14 were randomly assigned to Arm 1 (brief education) and 14 to Arm 2 (brief education plus Uphungu Wanga). A participant in Arm 1 was removed from the analysis because of a false AHI diagnosis and therefore 13 participants were included in Arm 1 and 14 in Arm 2. More males were enrolled in Arm 1 (76.9%) compared to Arm 2 (57.1%), and fewer married participants were enrolled in Arm 1 (23.1%) compared to Arm 2 (42.9%). These differences, however, are not statistically significant and may be a result of the small sample size. Participants in the two arms also did not differ significantly by age, education, or employment status (Table 3).
Table 3.
Baseline characteristics of study participants.
| Arm 1 | Arm 2 | Total | p-value* | |
|---|---|---|---|---|
| Total Enrolled | 13 | 14 | 27 | |
| Age | ||||
| 18-20 | 2 (15.4%) | 2 (14.3%) | 4 (14.8%) | 0.22 |
| 21-25 | 2 (15.4%) | 7 (50.0%) | 9 (33.3%) | |
| 26-30 | 4 (30.8%) | 4 (28.6%) | 8 (29.6%) | |
| 31-35 | 2 (15.4%) | 1 (7.1%) | 3 (11.1%) | |
| 36-40 | 3 (23.1%) | 0 (0.0%) | 3 (11.1%) | |
| >40 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Mean (SD) | 29 (7.3) | 25 (4.1) | 27 (6.1) | |
| Gender | ||||
| Male | 10 (76.9%) | 8 (57.1%) | 18 (66.7%) | 0.42 |
| Female | 3 (23.1%) | 6 (42.9%) | 9 (33.3%) | |
| Education | ||||
| None | 0 (0.0%) | 1 (7.1%) | 1 (3.7%) | 0.56 |
| Some primary school | 4 (30.8%) | 5 (35.7%) | 9 (33.3%) | |
| Completed primary school | 2 (15.4%) | 2 (14.3%) | 4 (14.8%) | |
| Some secondary school | 3 (23.1%) | 3 (21.4%) | 6 (22.2%) | |
| Completed secondary school | 4 (30.8%) | 1 (7.1%) | 5 (18.5%) | |
| Any tertiary education | 0 (0.0%) | 2 (14.3%) | 2 (7.4%) | |
| Marital Status | ||||
| Never married | 6 (46.2%) | 4 (28.6%) | 10 (37.0%) | 0.33 |
| Married | 3 (23.1%) | 6 (42.9%) | 9 (33.3%) | |
| Separated | 2 (15.4%) | 0 (0.0%) | 2 (7.4%) | |
| Divorced | 2 (15.4%) | 4 (28.6%) | 6 (22.2%) | |
| Widowed | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Employment Status | ||||
| Daily wage earner | 6 (46.2%) | 5 (35.7%) | 11 (40.7%) | 0.85 |
| Salaried wage earner | 2 (15.4%) | 4 (28.6%) | 6 (22.2%) | |
| Student | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Not employed | 4 (30.8%) | 3 (21.4%) | 7 (25.9%) | |
| Other | 1 (7.7%) | 2 (14.3%) | 3 (11.1%) |
p-value was calculated by Fisher’s Exact test
No participant declined to participate in an SSI; only participants who missed a study visit were not interviewed at that time. At the week 2 interview, 25 participants were interviewed, 12 in Arm 1 and 13 in Arm 2. At the week 8 interview, 26 participants were interviewed: 12 in Arm 1 and 14 in Arm 2.
Fidelity to the Intervention
Fidelity to several key components of the Uphungu Wanga intervention was nearly 100% at each of the five sessions, as reported by counselors and participants (Table 4). These components included: (1) discussing each of the main AHI messages; (2) discussing strategies for behavior change; (3) setting a risk-reduction goal; (4) discussing the participants’ perception of the importance and confidence of their goals; and (5) discussing successes and challenges in reaching previous goals. Some optional components — such as the use of role-play — occurred less often.
Table 4.
Uphungu Wanga intervention fidelity: key topics addressed at each session.
| Enrollment | Day 3 | Week 1 | Week 2 | Week 8 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Topic | Participant (N=14) |
Counselor (N=14) |
Participant (N=13) |
Counselor (N=13) |
Participant (N=13) |
Counselor (N=13) |
Participant (N=13) |
Counselor (N=13) |
Participant (N=14) |
Counselor (N=14) |
||
| Questions answered by both the participant and the counselor | Goal review | 13 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | 13 (92.9%) | 14 (100.0%) | |||
| Successes and challenges in reaching goal | 13 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | 12 (92.3%) | 13 (100%) | 13 (92.9%) | 14 (100.0%) | ||||
| New sex partners | 11 (84.6%) | 13 (100%) | 12 (92.3%) | 13 (100%) | 12 (92.3%) | 13 (100%) | 12 (85.7%) | 14 (100.0%) | ||||
| Participant has high amount of HIV virus in body during AHI | 13 (92.9%) | 14 (100.0%) | 13 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | 11 (84.6%) | 13 (100%) | ||||
| There is a very high chance that participant will give partners HIV if has unprotected sex during AHI | 14 (100.0%) | 14 (100.0%) | 13 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | 12 (92.3%) | 13 (100%) | ||||
| Abstaining from sex during AHI | 12 (85.7%) | 14 (100.0%) | ||||||||||
| Using condoms during AHI | 14 (100.0%) | 14 (100.0%) | ||||||||||
| Importance of abstaining or using condoms during AHI for at least 3-4 months | 13 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | ||||||
| Action plan for longer-term safer sex behavior | 14 (100.0%) | 14 (100.0%) | ||||||||||
| Role plays | 4 (30.8%) | 5 (38.5) | 4 (30.8%) | 7 (58.3%) | 4 (28.6%) | 5 (35.7%) | ||||||
| Pros/cons of disclosing to others | 13 (100%) | 12 (92.3%) | ||||||||||
| Disclosure barriers/facilitators | 13 (100%) | 13 (100%) | ||||||||||
| Disclosure options: | Patient referral | 12 (92.3%) | 12 (92.3%) | |||||||||
| Provider referral | 12 (92.3%) | 9 (69.2%) | ||||||||||
| Contract referral with provider | 9 (69.2%) | 9 (69.2%) | ||||||||||
| Questions answered by the participant | How to use condoms | 13 (92.9%) | ||||||||||
| Ways to reduce HIV transmission to others (beyond abstinence and condom use) | 13 (92.9%) | 13 (100%) | ||||||||||
| Set risk-reduction goal until next visit | 13 (92.9%) | 13 (100%) | 13 (100%) | 13 (100%) | ||||||||
| Importance of goal | 13 (92.9%) | 12 (92.3%) | 13 (100%) | 13 (100%) | ||||||||
| Confidence in meeting goal | 13 (92.9%) | 13 (100%) | 13 (100%) | 13 (100%) | ||||||||
| Questions answered by the counselor | Participant’s emotional status | 14 (100.0%) | 13 (100%) | 13 (100%) | 13 (100%) | 14 (100.0%) | ||||||
| Identified specific behaviors for participants to change | 14 (100.0%) | 11 (84.6%) | 11 (84.6%) | 11 (84.6%) | 11 (78.6%) | |||||||
| Barriers to behavior change | 14 (100.0%) | 12 (92.3%) | 13 (100%) | 13 (100%) | 14 (100.0%) | |||||||
| Strategies for behavior change | 13 (92.9%) | 13 (100%) | 13 (100%) | 13 (100%) | 14 (100.0%) | |||||||
| Action plan | 14 (100.0%) | 13 (100%) | 12 (92.3%) | 13 (100%) | ||||||||
Feasibility
All individuals with AHI who were recruited to join HPTN 062 were enrolled. Retention among enrolled participants was exceptionally high. Ninety-three percent of participants (n=13) in Arm 2 attended all of the first four Uphungu Wanga counseling sessions between enrollment and the week 2 visit. Moreover, 92% (n=12) of participants in Arm 1 attended all of their brief education sessions and 93% of participants in Arm 2 (n=13) attended all of their brief education and Uphungu Wanga counseling sessions between enrollment and the week 8 visit. The participant in Arm 1 who did not attend all of her/his respective sessions attended only the enrollment visit, and the participant in Arm 2 who did not attend all sessions was present only at the enrollment and week 8 visits.
All of the Uphungu Wanga counseling sessions were longer than the brief education sessions (Table 5); the difference in median length was statistically significant at the week 1 session (Uphungu Wanga: 39 minutes; brief education: 19 minutes; p<0.001) and at the week 2 session (Uphungu Wanga: 45 minutes; brief education: 15 minutes; p<0.001).
Table 5.
Length of Sessions.
| Visit | Median minutes by study arm, (min, max) | Differences in median time by study arm | p-value* | |
|---|---|---|---|---|
| Brief Education | Uphungu Wanga | |||
| Enrollment | 30 (15,130) | 44 (34,62) | 14 | 0.84 |
| Day 3 | -- | 40 (25,70) | -- | -- |
| Week 1 | 19 (10,45) | 39 (20,50) | 20 | <0.001 |
| Week 2 | 15 (10,37) | 45 (32,88) | 30 | <0.001 |
| Week 8 | -- | 41 (32,65) | -- | -- |
p-value was calculated by Wilcoxon Rank Sums test.
Acceptability of the Uphungu Wanga Counseling
Uphungu Wanga Intervention Format
Key quantitative acceptability data for both study arms are located in Table 6. Of the participants who attended their week 2 visit (93%, n=13), all reported that it was acceptable to begin the counseling on the day of their AHI diagnosis or around that day. In the SSIs, participants reported that the counseling provided them with the behavioral guidance, information, and emotional support they needed at the time they received their AHI diagnosis. Specifically, almost all of the participants expressed the need for immediate guidance on “how to live with HIV in my life,” and many indicated the importance of receiving education to better understand AHI in general and HIV transmission during AHI. About half of the participants said the counseling provided comfort and helped them cope with their diagnosis, and several expressed a sense of urgency about receiving immediate counseling on behavioral change:
Table 6.
Key acceptability indicators.
| Measure | Topic | Enrollment | Day 3 | Week 1 | Week 2 | Week 8 | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Uphungu Wanga (N=14) |
Brief Education (N=13) |
Uphungu Wanga (N=13) |
Uphungu Wanga (N=13) |
Brief Education (N=12) |
Uphungu Wanga (N=13) |
Brief Education (N=12) |
Uphungu Wanga (N=14) |
Brief Education (N=12) |
||
| Counseling Format | Acceptability of initiation timing – “Acceptable” to start on day of AHI diagnosis | -- | -- | -- | -- | -- | 13 (100%) | -- | -- | -- |
| Acceptability of number of sessions – Number of sessions “just right” | -- | -- | -- | -- | -- | 11 (84.6%) | -- | -- | -- | |
| Acceptability of session length – Time with counselor “just right” | 12 (85.7%) | 7 (53.8%)1 | 12 (92.3%) | 11 (84.6%) | 11 (91.7%) | 12 (92.3%) | 7 (58.3%)2 | 14 (100%) | 10 (83.3%) | |
| Counseling Content | Perceived satisfaction – “Very satisfied” with each session | 13 (92.9%) | 11 (84.6%) | 13 (100%) | 13 (100%) | 12 (100%) | 13 (100%) | 12 (100%) | 14 (100%) | 12 (100%) |
| Perception of needs being met – Counselor addressed questions/problems/worries “very well” | 14 (100%) | 11 (84.6%) | 13 (100%) | 13 (100%) | 12 (100%) | 13 (100%) | 12 (100%) | 14 (100%) | 12 (100%) | |
| Counseling Effectiveness | Perceived helpfulness – Each session was “very helpful” | 14 (100%) | 13 (100%) | 13 (100%) | 13 (100%) | 12 (100%) | 13 (100%) | 12 (100%) | 14 (100%) | 12 (100%) |
| Counselor Interaction | Comfort level with counselor – “Very comfortable” | 13 (92.9%) | 10 (76.9%) | 13 (100%) | 13 (100%) | 10 (90.9%) | 13 (100%) | 12 (100%) | 14 (100%) | 11 (91.7%) |
| Honesty with counselor – “Completely honest” | 14 (100%) | 12 (92.3%) | 13 (100%) | 13 (100%) | 11 (91.7%) | 13 (100%) | 12 (100%) | 14 (100%) | 12 (100%) | |
| Overall Counseling Preference | Brief education | -- | -- | -- | -- | -- | 0 (0.0%) | -- | -- | -- |
| Uphungu Wanga | -- | -- | -- | -- | -- | 3 (23.1%) | -- | -- | -- | |
| Liked both the same | -- | -- | -- | -- | -- | 10 (76.9%) | -- | -- | -- | |
46.2% (n=6) preferred more time with the counselor
41.7% (n=5) preferred more time with the counselor
It was acceptable [to initiate counseling on the day of diagnosis] because if some one has been found with the virus, he needs to be counseled right away so that he knows how to live with the virus, to avoid spreading the virus and adding more of the virus that causes AIDS. (26-year-old never married male)
I liked to start the same day [of diagnosis] because I wanted to know what to do when the HIV has just entered the body…. I discovered that at the time the HIV has just entered the body it’s the time when it is easy to transmit to your partner that you have unprotected sex with. (24-year-old divorced female)
The number of Uphungu Wanga sessions — four in 2 weeks — was perceived to be “just right” for 85% of the participants (n=11) and “too many” for 15% (n=2). In the SSIs, the reasons for the “just right” perception varied, but primarily focused on the belief that they were able to learn the information and have their questions answered within the designated number of sessions provided. Participants also said that the spacing of the sessions allowed them to retain the information and provided them with ample time to put the information they learned into practice:
It was just right because I was able to understand very well whatever they were telling me, I was able to think as they were telling me. If there was a lag [between sessions] I would have been forgetting the previous sessions’ information. If it [the time period between sessions] was too short I wouldn’t be able to follow through. (26-year-old married male)
Another participant indicated that the frequency of the counseling sessions helped to curb negative behaviors:
It was just right because if I went home and did something bad, I would come back and learn. (20-year-old divorced female)
The amount of time spent with the counselor (i.e., session length) was perceived to be “just right” for each of the five sessions by a majority of the participants (range: 85% to 100%, n=11 to 14). As elaborated in the SSIs, all participants said they felt the time spent with the Uphungu Wanga counselors allowed them to understand the topics well and cover the content adequately.
Uphungu Wanga Content
All participants reported in the quantitative interview that the counselor addressed their questions, problems, or worries “very well” at each counseling session. All but one participant said that they were “very satisfied” with each session. In the SSIs, the most common reasons mentioned for their satisfaction with the Uphungu Wanga counseling was that the counseling helped them to avoid or minimize risky behaviors and to learn information that was relevant to people newly infected with HIV:
Because I now know what to do now that I have a high amount of HIV…how I can prevent spreading it to other people and also, how I should lead my life…like on the part of using condoms every time…had I not heard about the counseling, I would have been ignorant…because I was told using condoms every time in acute HIV infection is good. (28-year-old married female)
In the SSIs, almost all of the participants said that the counseling was easy to understand. A few participants, however, said some of the information was difficult to grasp at first:
Interviewer: Did you find it easy or hard to pay attention to information about acute HIV infection during your first counseling session?
Participant: Initially it was difficult to understand but after I had asked again, it was not difficult to understand I understood it very well.
Interviewer: What made it hard to understand at first?
Participant: It is because it is not what one thinks. You feel the virus is supposed to be in fewer numbers.
Interviewer: Meaning, that [people often believe that when] the virus has just entered the body then it has to be fewer in numbers, and they [counselors] explained that the virus is in a high amount?
Participant: Mmh. [Interviewer note: client nodding head in agreement](26-year-old never married male)
A few other participants said it was difficult to retain information about HIV that had been provided on the day of their AHI diagnosis because they were surprised by the diagnosis and they were consumed with adjusting to the fact that they had HIV:
At the very beginning, I was told that I was not well. Then I had a lot of thoughts. They were talking to me but I was not listening to what they were telling me, because of these thoughts…. Thoughts were going through my mind like, “So, I have been found with HIV at this time in my life, now what do I do, maybe I may die due to this!”They finished talking but I did not listen.(21-year-old never married male)
In response, several participants felt it was acceptable and helpful to repeat messages about AHI at subsequent counseling sessions because it reinforced their comprehension.
Perceived Effectiveness of Uphungu Wanga
In the quantitative interviews, all of the participants said that the time spent with the counselor was “very helpful.” In the SSIs, almost all of the participants said that discussions related to sexual behavior — specifically the instruction on the importance of safer sex and how to use condoms — were most helpful to them in reducing their chances of transmitting HIV. Some participants mentioned that the messages about AHI were particularly helpful:
Interviewer: In general, what have you found most helpful about the sessions, if any?
Participant: What helped me the most is the real counseling about how you can live with the virus and also how we can behave to avoid transmitting the virus…. It helped me abstain from sex, which prevents HIV transmission and reinfection.
Interviewer: Which parts of the counseling sessions tackled this?
Participant: The part which explained what happens when the virus just enters the body I was taught that when the virus just enters the body, the virus multiplies a lot, the three consecutive months.
Interviewer: How did that information help you reduce your chances of transmitting the virus?
Participant: It helped because if you have just acquired the virus, the chances are very high that you can easily pass on the virus to others and you can also acquire a different strain of virus, which can cause problems in the body.
Interviewer: What did you do to achieve that?
Participant: I achieved by abstaining [at times], having protected sex, and avoiding other ladies. (26-year-old never married male)
The messages on preventing the forward transmission of HIV and on exposure to additional HIV viruses were also said to be helpful:
I see it’s not good to transmit HIV to other people because the number of people with HIV will increase. (24-year-old divorced female)
It helped me very much because there were benefits I could gain when using condoms. The benefits like avoiding other infections because I might not know the status of my sex partner. (20-year-old divorced female)
In addition, several participants said they valued the counseling topics that focused on the future, especially how the counseling helped them to preserve, protect, and prolong their lives, as well as topics related to abstinence and disclosure:
Yes, like the topic on disclosure…. I like it because it helped me know how to go about disclosing my status to others, relatives, friends and the people that are close to me…. It did help me to disclose to relatives and also some of my friends I chat with…. After receiving the counseling, I was able to disclose my status [to my sex partners]. (26-year-old never married male)
Counselor Interaction in Uphungu Wanga Counseling
In the quantitative interviews, all of the participants reported that they were “completely honest” with the counselor. All but one participant reported that they were “very comfortable” with the counselor during each session. In the SSI, participants described several reasons why they were comfortable with the counselor: the information was helpful; the counselor was able to answer the participant’s questions; the participant was able to be open and honest with the counselors; the counselor’s manner was caring, welcoming and polite; the counselor was skilled; and the counselor made the participant feel good. As one participant said:
She was discussing with me in a loving manner, that is why I was comfortable with her and I was not feeling ashamed… She was not rude or harsh…. Yah, there are some people who, when talking to you, are harsh and shout at you, they face the other way or don’t smile at you and they don’t even tell you in the right way. (28-year-old married female)
Acceptability of the Brief Education
Brief Education Format and Content
During the quantitative interview at enrollment, 46% of the participants (n=6) in Arm 1 reported that they wanted more time with the counselor compared to 14% of participants (n=2) in Arm 2 who said they wanted more time with the Uphungu Wanga counselor (p=0.1). Similarly, 42% of the participants (n=5) in Arm 1 at the week 2 visit indicated that they wanted more time with the counselor compared to 8% (n=1) of Arm 2 participants who wanted more time with the Uphungu Wanga counselor (p=0.07). In the SSIs, participants in Arm 1 elaborated on their responses in the quantitative interview and several said they had desired more time with the counselor primarily because the counseling provided them with knowledge and encouragement that motivated them. Nevertheless, almost all of the Arm-1 participants reported in the quantitative interview that the counselors addressed their questions, problems and worries “very well;” and that they were “very satisfied” with the counseling they had received. According to the SSIs, the participants were satisfied primarily because: the counseling helped them avoid or minimize risky behaviors; they knew very little about HIV before counseling; and they understood the information discussed.
Like not using a condom, these are things that may happen to me. If there is no such counseling, I would say, “Ndafa kale ine!”[interviewer note: meaning “I am as good as dead already.”] I would be doing things carelessly so that many of us should be on that road to death, such things…but because I have come here and I am accessing counseling, I am able to avoid such things. (21-year-old never-married male)
In the SSIs, the participants mentioned several topics that they liked in the brief education. Most of these topics fell into three categories, two of which were similar to those identified in Uphungu Wanga: (1) a focus on the future, especially how the counseling will help them to preserve, protect, and prolong their lives; (2) general health promotion, such as guidance on nutrition, exercise, hygiene, keeping a clean home, and coping; and (3) risk reduction and sexual behaviors.
What I liked the most is the information on condom use. If I want to have sex, I must use a condom…. This information interested me very much because the virus cannot increase in your body and there is no way you can transmit the virus to the other person. (28-year-old male, separated from spouse)
A few participants said that too much information was given. One participant said the information was didactic and that no input was solicited from the participant. Even so, almost all of the participants in Arm 1 said that the brief education covered the main topics that interested them. When asked, the participants did not suggest any new topics that they thought should be added to future counseling interventions.
Perceived Effectiveness of the Brief Education
In the quantitative interviews, all of the Arm-1 participants reported that the brief education was “very helpful.” In the SSI, the participants identified two general categories of perceived helpfulness: (1) guidance on safer sexual behaviors; and (2) instruction on taking care of oneself (e.g., advice on curbing drinking and smoking, and improving nutrition and cleanliness). According to the participants, the most helpful messages about sexual behavior were messages related to condom use, preventing HIV transmission to others, and preventing exposure to additional HIV viruses. Several participants described achievements they had attained as a result of the brief education, such as increasing their ability to use condoms, and avoiding risky behaviors. Several Arm-1 participants also reported changes in non-sexual behavior, such as the cessation or reduction of smoking cigarettes and drinking alcohol, increased exercise, and maintaining a healthy diet.
Provider Interaction during the Brief Education
In the quantitative interviews, most participants in Arm 1 reported being comfortable and honest with the counselors at each session.
Comparing Uphungu Wanga and the Brief Education Formats among Participants in Arm 2
In the quantitative interview, a few participants in Arm 2 (n=3; 23%) reported that they preferred the Uphungu Wanga counseling to the brief education; though a majority of the participants (n=10, 77%) did not have a preference between the brief education and Uphungu Wanga counseling. Upon further reflection in the SSIs, however, a few participants who previously reported no preference between the two counseling formats stated that they in fact preferred the Uphungu Wanga counseling. Moreover, several participants, regardless of their overall counseling format preference, described additional benefits of Uphungu Wanga compared to the brief education. Descriptions of the added benefit of Uphungu Wanga primarily focused on the separation of counseling from other clinic procedures and the use of a more comprehensive, and client-centered, counseling approach that not only provided education on safe practices, but helped them consider what risk reduction changes would be realistic for them and how to achieve those behavior changes. For example, a participant said that CHAVI 001 sessions (including the brief education), focused on physical exams, whereas Uphungu Wanga taught the participants how to avoid risk:
I have learned a lot of things from here [Uphungu Wanga]. So, while as from there [brief education] they did not teach me to sleep with fewer people or that I have a lot of viruses but there they just examine me to see how my body is. While as for here [Uphungu Wanga], we see how to avoid friends who can pressurize you to go drinking beer. That’s why am seeing the difference. (28-year-old married male)
The same participant also mentioned that the “triggers” approach, used in Uphungu Wanga, was more helpful than the approaches used in the brief education:
We were able to learn that if a person wants to avoid transmitting to others, how can you prevent. And what can provoke…triggers which can attract you to restart [interviewer note: meaning to backslide]. To know how you can prevent, that is what I have learned more than I what I learned at CHAVI [brief education].”
Another participant said that engagement in the brief education was minimal compared to the Uphungu Wanga counseling:
Yes, I differentiate because there [brief education] the type of counseling is less, it is not as here [Uphungu Wanga]. One cannot grasp the essence of the counseling there, they just teach you a small bit, while here, we stay for some time explaining to you… here [Uphungu Wanga], you are more free to ask anything, but there [brief education], while talking to you, they are busy taking those bottles [specimens]. (20-year-old divorced female)
The same participant also preferred other aspects of the participant-centered approach used in Uphungu Wanga:
On abstaining, there [brief education], they would say, “Ah, you need to abstain,” while here [Uphungu Wanga], they would tell you to make your own choice of prevention of infection and then you would choose as an individual.
A different participant said she preferred Uphungu Wanga counseling because the counselors focused exclusively on counseling:
The difference is that when I am at [brief education], I am required to do a lot. It happens that the one who is giving the counseling has a lot of things to do, and it happens that whenever I have questions the person is busy. She wants to do other activities, and I feel they do not answer me appropriately. On the other hand the special counseling [Uphungu Wanga] counselor is safe, she only has that time special for counseling. (20-year-old divorced female)
Another participant liked the variety of topics discussed in Uphungu Wanga:
CHAVI [brief education] counseling is always the same; they just remind us every time while the special counseling [Uphungu Wanga] we discuss different issues from last week. (24-year-old divorced female)
Discussion
This is the first study to report findings about an intervention to prevent the forward transmission of HIV among individuals with AHI. The findings demonstrate that Uphungu Wanga —an MI-based counseling intervention initiated on the day of diagnosis with AHI— was feasible and acceptable among individuals with AHI. The partnership with CHAVI 001 had several benefits: We were able to intervene (1) when individuals were hyper-infectious, as documented by viral load data (not described here); (2) when the individuals were first notified of their AHI diagnosis; and (3) at a time when immediate behavioral change can have the most impact in preventing the forward transmission of HIV. In addition to their regular CHAVI 001 visits, the participants were willing to devote a considerable amount of time to attend four counseling sessions in the two weeks immediately following the diagnosis of AHI and a follow-up booster session at week 8. Many participants also described more positive aspects of the Uphungu Wanga counseling compared to the brief education sessions. The preference was primarily attributed to the separation of counseling from other clinic procedures and the comprehensive, client-centered approach which allowed them to receive guidance on identifying and selecting specific strategies to achieve their safer sex goals.
The brief education sessions were also shown to be feasible and acceptable among participants in Arm 1. However, we should note some important differences in the acceptability between the two arms. First, some participants in the brief education arm wanted more time with the counselor, particularly during the enrollment and the week 2 visits, although the differences were not statistically significant. Second, in the SSIs, many Arm-2 participants described many more characteristics of the Uphungu Wanga counseling that they liked, found helpful, and that were related to sexual behavior compared to descriptions about the brief education provided by participants in Arm 1. Third, although almost all of the participants in both arms attended all of their respective brief education or Uphungu Wanga sessions, and reported similar perceptions in their quantitative interviews, participants in the Uphungu Wanga arm spent more time at the clinic undergoing counseling compared to those in the brief education arm. Thus, even though the time commitment to the two interventions differed considerably, the retention rates were equivalent. These findings, combined with participants’ other positive descriptions of the Uphungu Wanga counseling from the SSIs, suggest that Uphungu Wanga is highly feasible and acceptable from the participants’ perspective despite the added time. The findings also suggest that the participants were highly motivated to commit their time because the counseling was perceived to be useful. Ultimately, however, the participants in Arm 1 liked the brief education and found it helpful in changing their sexual behaviors after they were diagnosed with AHI. The participants in both study arms also reported substantial reductions in risky sexual behaviors (data to be described elsewhere).
It is important to note, however, that the brief education was a component of an intensive cohort study where contact with the participants was frequent and counseling was provided regularly. Outside of the research context, individuals diagnosed with AHI might not be offered such frequent clinic visits — so the comparison arm in this study was, in fact, enhanced. Greater differences in the acceptability and feasibility may have been seen if Uphungu Wanga had been compared to SOC counseling outside of the research context. The intervention was also evaluated within the context of the CHAVI 001 study, which required clinical visits and blood-sample collection together with counseling. In some instances, the integration of counseling and clinical procedures had a negative impact on the participants’ perceptions of the brief education.
One limitation of the study is that it was designed with a small sample size that restricted our ability to make statistical comparisons between the two arms on some measures. Although several participants preferred and described additional benefits of the Uphungu Wanga counseling, such as having more time with the counselors, it is unknown if these preferences would have led to significant differences between the groups if we had a larger sample size. Second, the acceptability of the interventions was measured through the participants’ self-reports and therefore subject to social-desirability bias. Third, the high enrollment and retention rates among participants in Uphungu Wanga may have been influenced by the reimbursement (US $5) the HPTN 062 participants received at each study visit, and by the tracing conducted by the study staff when a participant missed a study visit. Fourth, the numerous behavioral assessments may have influenced subsequent changes in the sexual behaviors of participants in both arms [24].
Recommendations
Feasibility studies are typically designed to determine whether large-scale studies should be subsequently conducted [25]. However, because identification of individuals with AHI is uncommon using current detection technologies, studies in the near future will probably be unable to obtain a sufficiently large sample population to detect statistically significant differences between different counseling interventions for individuals with AHI. We therefore offer recommendations for counseling individuals with AHI intended for HIV prevention and treatment programs. Our recommendations were informed by the quantitative and qualitative findings of this study, which together enabled us to develop a more complete picture of the participants’ experiences.
Because we found few major differences in the short-term between the two arms with regard to acceptability, feasibility, and self-reported sexual behaviors, our results suggest that an MI-based counseling intervention may not be needed during the brief period of AHI, even though the participants often preferred some of the unique features of Uphungu Wanga. Engaging a person immediately after an AHI diagnosis and continuing to engage the person in care, while providing brief counseling about HIV and AHI at each point of contact, was found to be highly needed by participants. Diagnosis with AHI may provide a “teachable moment” [26], where brief counseling may be sufficient to reduce risky behaviors and limit forward HIV transmission during this highly infectious period. Shorter counseling sessions, as implemented in the brief education arm, may also be more cost-efficient and feasible to implement, particularly when counselors are overburdened. We therefore recommend that:
Individuals with AHI receive frequent, but brief, counseling at several points, starting on the day of diagnosis and continuing in the short-term after diagnosis (e.g., at weeks 1 and 2 after diagnosis).
Extra time should be allocated during counseling on the day of diagnosis for individuals who may need more time to discuss and reflect upon the meaning of AHI.
An extra counseling session may be needed a few days after the AHI diagnosis (e.g. in between visits at weeks 1 and 2 after diagnosis) to re-emphasize messages about AHI because some individuals may not remember messages that were provided on the day of the diagnosis.
Follow-up counseling sessions should be provided at regular, but longer, intervals (e.g. monthly) after the first month following diagnosis to encourage on-going behavioral risk reduction to prevent forward transmission until individuals can initiate antiretroviral therapy (ART).
Focused messages should be provided on increased infectiousness and on the importance of abstaining from sex or using condoms 100% of the time during AHI as well as condom demonstrations and practice.
Topics should be included that focus on healthy living for the future and the influence of alcohol on sexual behaviors.
We would be remiss to disregard the participants’ preferences for many of the more personalized components of the Uphungu Wanga counseling, or the possibility that these advantages may have a greater impact on the participants’ long-term behavior. We therefore recommend that HIV-prevention programs:
Provide stand-alone counseling that is delivered separately from clinical assessments and by counselors who focus only on counseling.
Incorporate client-centered strategies into the brief education session — such as considering an individual’s context and aspirations, assessing an individual’s motivation to change risky behaviors, discussing specific behaviour-change strategies to try, and encouraging individuals to set risk-reduction goals.
Include counseling on options for serostatus disclosure to current sexual partners to facilitate the ability of individuals with AHI to make rapid behaviour change (i.e. to abstain or use condoms) during the critical AHI period.
While identification of individuals with AHI is difficult and resource-intensive with the technology currently available, future advances in rapid HIV viral testing are likely to result in more widespread detection of AHI. In the meantime, there is an urgent need and a unique opportunity to intervene in this early stage when acutely infected individuals are highly infectious. We have provided prevention messages and recommended practices that clinicians and other health-care providers and counselors can use with acutely infected individuals. Moreover, as global HIV-prevention efforts transition to early detection and treatment — known as “test and treat” [27] — it is unlikely that all individuals will be able to initiate ART on the day of diagnosis. A counseling package on the prevention of forward HIV transmission, when provided regularly to individuals diagnosed with HIV, may be an important component of the test-and-treat strategy to keep individuals motivated and engaged in care until ART is initiated and sustained.
Acknowledgments
We are grateful to the individuals who participated in this study. We also appreciate the efforts of the following organizations, teams, and individuals: CHAVI, HPTN 062, the UNC Project, and the Kamuzu Central Hospital staff members who contributed to the implementation of this study; Niasha Brown Michele Demers, and Caleb Parker, who assisted with the design of the intervention; and Kate Clouse who assisted with the design of the study instruments.
Funding
Research reported in this publication was supported by the National Institute of Allergy And Infectious Diseases of the National Institutes of Health under Award Number UM1 AI068619 and the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Pilcher CD, Joaki G, Hoffman IF, Martinson FE, Mapanje C, Stewart PW, et al. Amplified transmission of HIV-1: comparison of HIV-1 concentrations in semen and blood during acute and chronic infection. AIDS. 2007;21(13):1723–30. doi: 10.1097/QAD.0b013e3281532c82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Powers KA, Ghani AC, Miller WC, Hoffman IF, Pettifor AE, Kamanga G, et al. The role of acute and early HIV infection in the spread of HIV and implications for transmission prevention strategies in Lilongwe, Malawi: a modelling study. Lancet. 2011;378(9787):256–68. doi: 10.1016/S0140-6736(11)60842-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pettifor A, MacPhail C, Corneli A, Sibeko J, Kamanga G, Rosenberg N, et al. Continued high risk sexual behavior following diagnosis with acute HIV infection in South Africa and Malawi: implications for prevention. AIDS Behav. 2011;15(6):1243–50. doi: 10.1007/s10461-010-9839-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steward WT, Remien RH, Higgins JA, Dubrow R, Pinkerton SD, Sikkema KJ, et al. Behavior change following diagnosis with acute/early HIV infection-a move to serosorting with other HIV-infected individuals. The NIMH Multisite Acute HIV Infection Study: III. AIDS Behav. 2009;13(6):1054–60. doi: 10.1007/s10461-009-9582-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly JA, Morin SF, Remien RH, Steward WT, Higgins JA, Seal DW, et al. Lessons learned about behavioral science and acute/early HIV infection. The NIMH Multisite Acute HIV Infection Study: V. AIDS Behav. 2009;13(6):1068–74. doi: 10.1007/s10461-009-9579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crowe S, Turnbull S, Oelrichs R, Dunne A. Monitoring of human immunodeficiency virus infection in resource-constrained countries. Clin Infect Dis. 2003;37(Suppl 1):S25–35. doi: 10.1086/375369. [DOI] [PubMed] [Google Scholar]
- 7.Pilcher CD, Eron JJ, Jr, Galvin S, Gay C, Cohen MS. Acute HIV revisited: new opportunities for treatment and prevention. J Clin Invest. 2004;113(7):937–45. doi: 10.1172/JCI21540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen MS. CHAVI 001: Acute HIV-1 Infection Prospective Cohort Study Protocol. A Study of the Center for HIV/AIDS Vaccine Immunology (CHAVI) Final Version 2.0. 2007 Apr 14; [Google Scholar]
- 9.UN World Health Organization. Guidance on Provider-Initiated HIV Testing and Counselling in Health Facilities. 2007 Available from: http://www.who.int/hiv/pub/vct/pitc2007/en/
- 10.Fisher JD, Fisher WA, Cornman DH, Amico RK, Bryan A, Friedland GH. Clinician-delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. J Acquir Immune Defic Syndr. 2006;41(1):44–52. doi: 10.1097/01.qai.0000192000.15777.5c. [DOI] [PubMed] [Google Scholar]
- 11.Golin CE, Patel S, Tiller K, Quinlivan EB, Grodensky CA, Boland M. Start Talking About Risks: development of a Motivational Interviewing-based safer sex program for people living with HIV. AIDS Behav. 2007;11(5 Suppl):S72–83. doi: 10.1007/s10461-007-9256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Golin CE, Earp JA, Grodensky CA, Patel SN, Suchindran C, Parikh M, et al. Longitudinal effects of Safe Talk, a motivational interviewing-based program to improve safer sex practices among people living with HIV/AIDS. AIDS Behav. 2012;16(5):1182–91. doi: 10.1007/s10461-011-0025-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Golin CE, Davis RA, Przybyla SM, Fowler B, Parker S, Earp JA, et al. Safe Talk, a multi component, motivational interviewing-based, safer sex counseling program for people living with HIV/AIDS: a qualitative assessment of patients’ views. AIDS Patient Care STDS. 2010;24(4):237–45. doi: 10.1089/apc.2009.0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–74. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 15.Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med. 2001;20(1):68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 16.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York: Guildford; 1991. [Google Scholar]
- 17.Rollnick S, Miller WR. What is Motivational Interviewing? Behavioural and Cognitive Psychotherapy. 1995;23:325–34. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- 18.Cornman DH, Kiene SM, Christie S, Fisher WA, Shuper PA, Pillay S, et al. Clinic-based intervention reduces unprotected sexual behavior among HIV-infected patients in KwaZulu-Natal, South Africa: results of a pilot study. J Acquir Immune Defic Syndr. 2008;48(5):553–60. doi: 10.1097/QAI.0b013e31817bebd7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson ES, Wagstaff DA, Heckman TG, Winett RA, Roffman RA, Solomon LJ, et al. Information-Motivation-Behavioral Skills (IMB) Model: testing direct and mediated treatment effects on condom use among women in low-income housing. Ann Behav Med. 2006;31(1):70–9. doi: 10.1207/s15324796abm3101_11. [DOI] [PubMed] [Google Scholar]
- 20.Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–51. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 21.McLellan E, MacQueen KM, Niedig J. Beyond the Qualitative Interview: Data Preparation and Transcription. Field Methods. 2003;15:63–84. [Google Scholar]
- 22.Saldaña J. The Coding Manual for Qualitative Researchers. Los Angeles: Sage Publications; 2009. [Google Scholar]
- 23.NVivo Qualitative Data Analysis Software. Version 9.2. QSR International Pty Ltd; 2010. [Google Scholar]
- 24.Sprott DE, Spangenberg ER, Block LG, Fitzsimons GJ, Morwitz VG, Williams P. The question-behavior effect: What we know and where we go from here. Social Influence. 2006;1(2):128–37. [Google Scholar]
- 25.Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–7. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18(2):156–70. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 27.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 28.Powers KA, Miller WC, Pilcher CD, Mapanje C, Martinson FE, Fiscus SA, et al. Improved detection of acute HIV-1 infection in sub-Saharan Africa: development of a risk score algorithm. AIDS. 2007;21(16):2237–42. doi: 10.1097/QAD.0b013e3282f08b4d. [DOI] [PMC free article] [PubMed] [Google Scholar]


