Abstract
Oncology nurses are essential in all phases of cancer care; however, their role in survivorship care is unclear. To better understand the self-reported knowledge and educational needs on topics of survivorship care and oncology nurses’ learning preferences, an online survey was conducted. Respondents self-reported knowledge level for 31 care topics, identified areas of most interest, topics needed to assist patients and address patient questions, and reported participation in continuing education and preferred learning methods. Knowledge was rated highest for topics of fatigue, anxiety, and fear of recurrence and lowest for issues related to finance, employment, and insurance. Nurses were most interested in late and long-term physical effects of cancer or treatment, managing emotional issues, cancer screening and surveillance, and complementary and alternative therapies. Study findings suggest that online learning methods would be feasible and well accepted by nurses to meet continuing education needs related to cancer survivorship.
Keywords: Oncology nurses, Cancer survivorship, Nursing education
Introduction
Oncology nurses play a vital role in the day-to-day care of more than 1.5 million patients in the United States and 3.2 million patients in Europe who are newly diagnosed with cancer each year [1, 2]. Nurses are essential in every phase of patient care; however, their role is more clearly defined during acute/primary treatment. In addition to physical care of the patient, nurses provide well-defined patient and family education regarding treatment and much needed emotional and practical support in the early phase of cancer care [3, 4]. Knowledgeable nurses are essential to meet the challenge of managing millions of cancer survivors who are currently living with active disease or previously treated malignancies.
The role of the oncology nurse after primary treatment has been completed is still emerging because models for delivering specific elements of long-term survivorship care in primary care and oncology settings are still evolving. Essential components of survivorship care, as outlined by the Institute of Medicine in From Cancer Patient to Cancer Survivor: Lost in Transition [5] are: (1) prevention of recurrent and new cancers and of other late effects, (2) surveillance for cancer spread, recurrence, or second cancers and assessment of medical and psychosocial late effects, (3) intervention for later sequelae from cancer and its treatment, and (4) coordination of care between oncology specialists and primary care providers.
The oncology nurse is in a unique position to ensure that the patient’s needs are met by assessing the cancer survivor’s condition in physical, emotional, spiritual, and social domains. Nursing assessment identifies the patient education needed to address current issues and recommends cancer prevention strategies through healthier lifestyle and surveillance for cancer and any late effects of the malignancy or its treatment. Nurses can also play an important role in coordinating access to health care and community services as the patient transitions from primary cancer treatment to ongoing survivorship care [3, 4].
Unfortunately, most nurses receive limited exposure to cancer care over the course of their undergraduate training [4, 6–8]. The number of nursing schools in the United States that offered graduate training in oncology dropped from 45 in 1990 to 21 in 2006, and only 1% of advanced practice nurses specialize in oncology [3, 6, 9]. Due to a lack of formal training options, nurses working in the oncology field rely on learning within the workplace and participating in continuing nursing education programs to gain knowledge about acute cancer care and cancer survivorship issues. Oncology nursing textbooks and journals include content about providing survivorship care, although certain topics have received more attention than others [3]. Some continuing education programs focusing on cancer survivorship have been developed, such as a train-the-trainer model program that provided workshops and mentoring for 204 multidisciplinary teams [10, 11].
In order to better understand the continuing education needs of oncology nurses about specific survivorship issues and the scope of survivorship care they provide, the University of Kansas Cancer Center and the Oncology Nursing Society collaborated to conduct a survey among a broad sample of nurses in the United States [12]. Few nurses worked in settings with formal survivorship programs, and a number of the components of survivorship care recommended by the Institute of Medicine (IOM) [5] were inconsistently provided to patients. The current report provides the findings of the survey related to self-reported knowledge about key components of survivorship care and the respondents’ usual and preferred formats for receiving continuing education.
Methods
In this study, the term “cancer survivor,” referred to any individual living with cancer from the moment of diagnosis. An online survey was conducted after receiving Institutional Review Board approval at the University of Kansas School of Medicine (HSC# 220091266). The questionnaire included items for reporting self-assessed knowledge using a scale ranging from 0 to 5 (not at all knowledgeable to very knowledgeable, respectively). The 32 knowledge items were derived from consensus documents highlighting essential components of survivorship care. These included documents developed with stakeholder input by the IOM and the Lance Armstrong Foundation, as well as publications from those who are highly regarded in the field of cancer survivorship [3, 5, 8, 13, 14]. Two of the items addressed fatigue: one was worded “fatigue” and the other was worded “energy and fatigue management.” Internal consistency of responses to these items was very good (Pearsons’s correlation coefficient, .718, P<.001) so the responses for these items were averaged, leaving a total of 31 knowledge items for analysis. Other survey items asked participants to rank their educational needs for a list of 12 survivorship topics. Preferences for and access to continuing nursing education (21 items) were assessed as well as age, education, and characteristics of respondents’ work settings. The remaining questionnaire items, which have been reported previously [12], assessed the state of survivorship care provided within respondents’ work settings and perceived barriers to providing such care.
Sample
A target sample size of approximately 10,000 nurses was selected to provide a sampling error of no greater than 5%, assuming a response rate of approximately 4% [15]. Among the approximately 37,000 Oncology Nursing Society members, a subset was identified from the membership database which had provided apparently valid email addresses and had indicated that they were working full- or part-time (n=27,561). Of these, 9,664 members were randomly selected. To this group, all 381 members of the Oncology Nursing Society’s Survivorship Quality of Life & Rehabilitation Special Interest Group were added. Any duplicates were removed, resulting in a total of 10,045 members. This group was sent an email invitation stating the survey purpose, providing a link to the survey, and assuring them that their responses would not be identified individually. The Magnetmail® system (Real Magnet, LLC, Bethesda, MD) was used to track email delivery, open rate, and number of recipients who followed the survey link. Email was successfully delivered to 9,415 (93.7%) of the original sample. The initial email occurred on July 23, 2009, a reminder was sent 2 weeks later, and the option to participate ended on August 30, 2009. The survey responses were collected using the Zarca® (Zarca Interactive, Inc., Herndon, VA) electronic survey system.
Statistical Analysis
Data analysis was completed with Predictive Analytics Software® (SPSS, Inc., Chicago, IL), version 18.0. All analyses were conducted with the full sample of 470 respondents although respondents chose not to answer certain questions, and this resulted in somewhat varying denominators for specific analyses. Related samples marginal homogeneity tests were used to assess whether self-reported knowledge levels differed when comparing two topics. Principal component analysis with varimax rotation was used to group the 31 knowledge items into five knowledge domains. Rotated component correlations of 0.460 or greater were used to define components. This analysis was conducted on a subset consisting of 415 questionnaires with no missing data for any of the knowledge items. The analysis had a Kaiser–Meyer–Olkin measure of sampling adequacy of .961 and P< .001 for Bartlett’s test of sphericity. Mean scores for each knowledge domain were then computed. For subgroup analyses (e.g., by work setting), proportions were compared by Pearson’s Chi-square tests or, when expected values in any cell were less than 5, with Fisher’s exact tests. Normally distributed continuous variables were compared using t tests or one-way analysis of variance. All statistical tests were two-tailed, and an alpha of 0.05 was used for all analyses.
Results
The response rate was 5.0% (470/9,415) among the emails that could be delivered and 31.6% (470/1,485) among the emails that were opened by the recipients. The respondents had worked in oncology for an average of 14.9+9.8 years (mean, standard deviation), and their oncology experience ranged from 0 to 40 years. Half (51.6%) of the respondents were >50 years of age, and about one third (34.7%) of respondents had received at least a master’s degree. Most (84.9%) of the respondents were employed in a work setting at which care was provided for cancer patients during extended survival (i.e., patients diagnosed one or more years previously). Other characteristics of the sample are provided in Table 1.
Table 1.
Characteristics of respondents
| Characteristic | n (%) |
|---|---|
| Age, years | |
| <40 | 83 (17.9) |
| 40–49 | 142 (30.6) |
| 50–54 | 94 (20.3) |
| >55 | 145 (31.3) |
| Highest degree completed in nursing | |
| Diploma | 38 (8.2) |
| Associate | 92 (19.9) |
| Bachelor’s | 172 (37.2) |
| Masters | 138 (29.9) |
| Doctorate | 22 (4.8) |
| Care provided for patients who are >1 year since diagnosisa | 399 (84.9) |
| Outpatient | 203 (44.2) |
| Inpatient | 108 (23.5) |
| Radiation therapy | 29 (6.3) |
| Other | 119 (25.9) |
| Primary functional area of work | |
| Patient care | 259 (57.0) |
| Education | 69 (15.2) |
| Administration | 57 (12.6) |
| Research | 36 (7.9) |
| Other | 33 (7.0) |
| Primary patient setting | |
| Adult only | 421 (89.6) |
| Adult and pediatric | 23 (4.9) |
| Pediatric only | 21 (4.5) |
Yes response to “In your work setting, do you see patients who are a year or more post initial treatment, whether or not they are continuing to receive any cancer treatment?”
Respondents self-reported their knowledge levels for 31 cancer care topics. Average responses by topic ranged from 2.25 to 3.54 on a scale of 0–5 (Table 2). Respondents thought their knowledge levels were highest for fatigue, anxiety, fear of recurrence, hope, and palliative care. Even for these topics, however, relatively few respondents thought their knowledge levels were in the “very knowledgeable” range. Knowledge about helping patients with anxiety, for example, was ranked as a 5 by only 17.4% of respondents, and as a 4 by only 32.3% of respondents. The mean overall knowledge score for all 31 items was 3.06 (Table 2).
Table 2.
Self-assessed knowledge
| Survivorship care components | Knowledge scorea mean (SD) |
|---|---|
| Individual topics | |
| Fatigue | 3.54 (1.0) |
| Anxiety | 3.49 (1.0) |
| Fear of recurrence | 3.48 (1.0) |
| Hope | 3.48 (1.1) |
| Palliative care | 3.47 (1.1) |
| Chronic painb | 3.44 (1.1) |
| Depression | 3.43 (1.0) |
| Body image | 3.38 (1.0) |
| Cancer surveillance and screening | 3.36 (1.1) |
| Grief and loss | 3.36 (1.1) |
| Smoking cessation and prevention | 3.32 (1.1) |
| Living with uncertainty | 3.31 (1.1) |
| Hormonal effects, including menopausal symptoms, osteoporosisb | 3.28 (1.2) |
| Neuropathyb | 3.27 (1.1) |
| Diet | 3.27 (1.0) |
| Lymphedemab | 3.20 (1.2) |
| Physical activity and rehabilitation | 3.18 (1.0) |
| Skin changes such as scarring, sun sensitivityb | 3.15 (1.1) |
| Cognitive and memory changesb | 3.12 (1.1) |
| Finding meaning | 3.06 (1.2) |
| Changes in bowel and bladder controlb | 3.04 (1.2) |
| Cardiac problemsb | 2.92 (1.2) |
| Post-traumatic stress | 2.75 (1.2) |
| Sexual dysfunction and sexual health | 2.74 (1.2) |
| Fertility issues | 2.71 (1.2) |
| Dental problemsb | 2.55 (1.2) |
| Health care access | 2.52 (1.4) |
| Ostomy managementb | 2.52 (1.4) |
| Employment issues | 2.31 (1.1) |
| Insurance issues | 2.24 (1.2) |
| Financial issues | 2.25 (1.1) |
| Knowledge domain scoresc | |
| Long-term cancer care and prevention | 3.35 (0.87) |
| Emotion-laden or spiritual topics | 3.19 (0.91) |
| Late effects of cancer or treatment | 3.08 (0.89) |
| Other nursing care | 3.00 (0.99) |
| Practical matters related to employment and finance | 2.33 (1.1) |
| All 31 knowledge items | 3.06 (0.79) |
SD standard deviation
Scores on a scale of 0–5 (not at all knowledgeable–very knowledgeable, respectively)
Question was worded to indicate these were related to late and long-term effects of cancer and treatment
See text for list of items comprising each score
Long-Term Cancer Care and Prevention
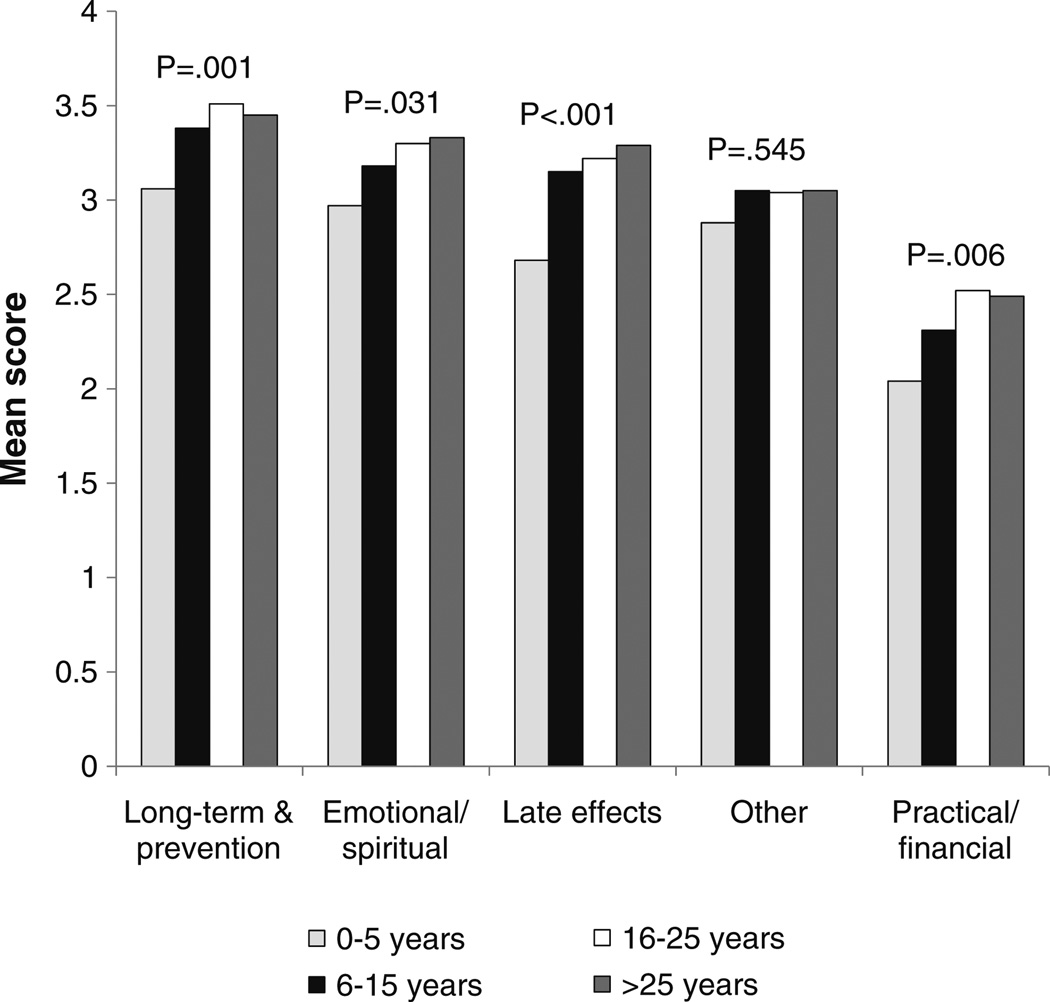
Principal component analysis revealed five knowledge domains. The domain with the highest overall knowledge score was long-term cancer care and prevention (mean score, 3.35; Table 2). The items in this domain were cancer surveillance and screening, smoking, diet, physical activity and rehabilitation, palliative care, and fatigue. On-the-job experience was associated with overall knowledge in this domain. The pattern of knowledge gain after progressively more years of oncology experience is shown in Fig. 1. Those who had worked 5 or fewer years in oncology had a mean knowledge score of 3.06 compared to a score of 3.44 for those having worked in oncology for more than 5 years (P<.001).
Fig. 1.
Self-reported knowledge according to quartile of years working in an oncology setting
Knowledge in the long-term cancer care and prevention domain was not associated with having obtained more training in the nursing field (mean domain scores for less than a bachelor’s degree, bachelor’s degree, and more than a bachelor’s degree were 3.29, 3.33, and 3.44, respectively, P=.324). The overall score in this domain was not associated with work setting. For items making up this domain, those working in outpatient settings had significantly more knowledge about cancer surveillance and screening (item score of 3.56 compared to 3.19 for all other work settings, P<.001) whereas working on an inpatient unit was associated with more knowledge about palliative care (item score of 3.73 compared to 3.38 for all other work settings, P=.003).
Emotion-Laden and Spiritual Topics
Items in this knowledge domain were the existential or spiritual items on hope, finding meaning, living with uncertainty and grief or loss, the emotional topics of anxiety, post-traumatic stress, fear of recurrence, and depression, and the emotion-laden items of body image, sexual dysfunction or sexual health, and fertility. Self-reported knowledge was significantly higher for anxiety than for post-traumatic stress related to cancer, sexual issues, or fertility (all P<.001, Table 2). Individuals 40 years of age or older had higher mean scores in this domain (mean scores of 3.26 compared to 2.84 among younger respondents, P<.001). There were no meaningful differences in the domain score or item scores by work setting. Respondents who had more experience in oncology reported higher knowledge levels for emotion-laden and spiritual topics (Fig. 1). Nurses with 0–5 years compared to 6 or more years of oncology experience rated their knowledge in this domain, with mean scores of 2.97 compared to 3.26, respectively (P=.007).
Late Effects of Cancer or Treatment
The items making up the domain related to late effects of cancer or its treatment were: cardiac, dental, cognitive, hormonal and osteoporosis, skin, neuropathy, and lym-phedema problems. Respondents reported only modest knowledge in this domain (mean score of 3.08; Table 2). The overall domain score was higher among those with more oncology experience (Fig. 1), and nurses with 0– 5 years compared to 6 or more years of oncology experience rated their knowledge in this domain with mean scores of 2.68 compared to 3.20, respectively (P<.001). Knowledge in this domain was not associated with the type of nursing degree. Those working in outpatient settings reported greater knowledge on several of the items, especially hormonal effects and osteoporosis (item score of 3.51 compared to 3.09 for other work settings, P<.001). Those working in radiation oncology had a much higher knowledge score for skin effects (item score of 4.07 compared to 3.10 for other work settings, P<.001).
Other Nursing Care
Nursing care for ostomy management, cancer-related bowel or bladder problems, and chronic cancer pain made up the domain of other nursing care. There was no relationship between duration of oncology experience and self-reported knowledge in this domain (Fig. 1), nor with age or nursing degree. Respondents from radiation oncology reported higher knowledge levels regarding bowel and bladder issues (item score of 3.59 compared to 3.01 for other work settings, P=.008). The mean knowledge scores for ostomy care were low in all work settings, although the ostomy care scores for those providing inpatient settings were the highest (item score of 2.91 compared to 2.39 for other work settings, P=.001).
Practical Matters Related to Finances
Of all the knowledge items on the survey, scores were lowest for access to care, employment, insurance, and financial issues related to cancer (Table 2). These four items made up the domain of practical matters related to finances, and this domain score was 2.33 for all respondents. The greatest knowledge gain in this domain occurred after 0–5 years of oncology nursing experience (mean domain scores of 2.04 compared to 2.42 for nurses with 0–5 years compared to 6 or more years of oncology experience, P=.002). Even though increased knowledge in this domain was associated with greater oncology experience (Fig. 1), the highest domain score at 16–25 years of experience was only 2.52. This knowledge domain and its individual items had no relationship to nursing degree or age, and there was poor self-reported knowledge for helping patients with these practical needs across all practice settings.
Educational Interests and Needs
For 12 survivorship topic areas, participants were asked to choose the three in which they were most interested (Table 3). They were also asked to indicate all those topics for which they need more information to assist their patients and those about which their patients asked the most questions. The topic area that was chosen most commonly in all three questions was physical late and long-term effects of cancer or treatment, such as cardiac problems, osteoporosis, cognitive changes, or bowel and bladder changes. High levels of educational need were revealed for managing emotional issues and cancer screening and surveillance, as well as complementary and alternative therapies such as vitamins, herbal supplements, massage, and relaxation therapy. Each of the 12 topic areas was chosen by at least one fourth of respondents as an area in which they needed more information in order to assist their patients (Table 3, column 2).
Table 3.
Number of respondents who ranked each topic among their educational interests or needs
| Survivorship care topics | Interested in topica | Need information to assist patientsb | Get questions from patientsb |
|---|---|---|---|
| Physical late and long-term effectsc | 278 | 271 | 235 |
| Managing emotional effects of cancer treatment | 200 | 220 | 226 |
| Cancer screening and surveillance for recurrence | 163 | 161 | 222 |
| Complementary and alternative therapiesd | 159 | 257 | 212 |
| Healthy behaviors such as diet, exercise | 140 | 145 | 206 |
| Dealing with partner and family relationships | 103 | 170 | 106 |
| Genetics | 83 | 197 | 83 |
| Sexual dysfunction and sexual health | 80 | 225 | 95 |
| Issues such as insurance, financial or legal concerns | 78 | 270 | 200 |
| Body image | 46 | 126 | 82 |
| Fertility preservation | 37 | 166 | 37 |
| Employment | 32 | 194 | 101 |
For this question, participants were required to select exactly three topics
For these questions, participants were not limited on the number of topics they could select
The question listed these examples: cardiac problems, osteoporosis, cognitive changes, bowel and bladder changes
The question listed these examples: vitamins or herbal supplements, massage, relaxation therapy
Even though emotional aspects of cancer received among the highest item scores for self-reported knowledge (Table 2), respondents were still highly interested in learning more about the topic area (Table 3). Employment issues were considered the least interesting even though patients commonly asked about these issues (Table 3), and self-reported knowledge about this knowledge domain was the lowest of all knowledge domains (Table 2). Patients commonly asked respondents questions about most of the topic areas, but even if they didn’t, respondents still believed they needed to know more. For example, only 37 respondents indicated that their patients commonly ask about fertility preservation, but 166 respondents indicated that fertility preservation was an area of education that they needed in order to assist patients (Table 3).
Participation in Continuing Education
Respondents reported regular participation in continuing education, and the 50th percentile for time spent in continuing education was 45–50 h per year. Most hours were acquired by attending conferences or lectures; 57.3% acquired 6–25 h per year and 32.9% acquired >25 h per year in person. Half of respondents commonly used print materials or online resources for continuing education (47.9% and 52.3%, respectively, acquired 6–25 continuing education hours in these ways annually). A few respondents did not regularly use conferences and lectures for continuing education (only 8.8% of respondents acquired 0–5 h in person annually), but a substantial minority spent a few hours per year obtaining continuing education from print materials or online resources (24.7% and 35.5%, respectively).
Preferences for and Access to Online Nursing Education
Almost all respondents reported having access to the internet at home and at work, 97.4% and 96.5%, respectively. Most respondents (67.2%) could do web-based education at work. If not, the main barriers to completing online education at work were lack of time and lack of support from administration to use work time for this activity (47.4% and 32.5% of respondents, respectively). The majority of respondents reported being proficient in online learning and endorsed the importance of access to online learning (76.6% and 84.5%, respectively gave responses of 8–11 on a scale of 1–11, where 11 was extremely comfortable or extremely important).
Among those who did not report being proficient in online learning (109 individual who gave responses of 0–7 on the scale), the most common barriers to using internet continuing education were lack of time (54.1%), preference for other educational methods (37.6%), the format of existing internet educational materials (26.6%), lack of comfort with computers (23.9%), cost (16.5%), and uninteresting topics (15.6%). Despite these barriers, 50.9% of the nonproficient group rated access to online learning as important (responses of 8–11 on the 11-point scale).
Among the respondent group as a whole, nearly half (46.0%) would prefer completing web-based learning at home, 31.7% would like the option of accessing this education either at home or at work, 20.9% would prefer completing online learning only at work, and 1.5% did not want to use such education at either location. Nearly all (88.3%) respondents reported that online self-study modules should include continuing education credit. Most (71.7%) reported that their ideal amount of time to spend on a single continuing education session was 30–60 min.
Discussion
Over the past 30 years, the number of cancer survivors in the United States has risen from 3.2 million to over 12 million, and a parallel trend has been seen in Europe [1, 2]. Although the number of cancer survivors continues to grow, there has not been a similar increase in training about cancer survivorship care within nursing degree programs [6–8]. Because of this, it is important to develop high-quality continuing nursing education to help nurses develop and maintain competency in cancer survivorship care. This study has helped to identify those topic areas for which nurses have an interest and need for continuing education.
In the present study, there was no association between knowledge deficits and level of formal nursing training. However, years of experience in oncology nursing was associated with most knowledge domains. Knowledge levels were lowest among those with 5 or fewer years of oncology experience. These findings are consistent with learning occurring through on-the-job training. The relatively low levels of self-reported knowledge and the high level of interest in topic areas such as the late and long-term effects of cancer and its treatment underscore the need for continuing nursing education programs that address cancer survivorship.
In most topic areas, as shown in Table 3, respondent interest, perceived need for information to assist patients, and getting questions from patients were well aligned in terms of the number of respondents who selected the topics. There were, however, three notable exceptions to this alignment: genetics, sexual dysfunction and sexual health, and insurance, financial and legal issues. These topic areas were associated with lower interest despite relatively high need for information to assist patients. Employment issues generated questions from patients and respondents indicated that they need information about these issues to help patients, but this topic was least frequently chosen as an area of interest. These contrasting responses to selected topic areas suggest that these issues may lie outside perceived roles during nursing practice (and, thus, nurses do not have a high interest in their own education in the topic), but nurses do see the need for resources in these areas to make available to their patients.
Many expert groups have called for expanding the oncology nursing workforce to improve care for patients during extended cancer survivorship and to coordinate care between oncology specialty and primary care settings [3–6, 13]. Traditional, face-to-face continuing education opportunities are being provided for nurses by organizations such as the European Oncology Nursing Society, the International Society of Nurses in Cancer Care, the Oncology Nursing Society and its Survivorship Quality of Life & Rehabilitation Special Interest Group in the United States and others. Many nurses do not have the financial resources to attend large conferences, however. The distant location of many professional meetings, the high cost of travel and lodging, and the difficulty in taking time away from work and family prohibit in-person attendance. Travel to participate in high-quality, educational conferences is even more difficult when poor economic times impact the nurse as well as the employer.
Online education provides the means to fulfill nurses’ responsibility to engage in life-long learning by removing barriers of location and excessive cost. Some web-based education programs are being offered by the oncology nursing societies in the United States and Europe to meet these needs. Respondents in our study acknowledged comfort with online educational tools and have ready access to the internet both at work and at home. These and other findings in this study suggest that the online route is a viable method for reaching oncology nurses interested in cancer survivorship education.
Limitations
This survey was conducted among members of the Oncology Nursing Society, most of whom are located in the United States. Because of this, the findings may not generalize perfectly to other countries. However, other data suggest that the training needs of the cancer nursing workforce in the United States have many similarities with the training needs in Canada and Europe [3–7]. Competency in cancer survivorship nursing care is needed not only in the field of oncology nursing but also among primary care nurses since most cancer survivors are cared for in both specialty and primary care settings. Further research is needed to identify the specific educational needs of primary care nurses so that they can more effectively collaborate with oncology specialty practices to deliver optimal care for cancer survivors.
The survey addressed self-reported knowledge, which may not reflect actual knowledge or patient care skills. Many studies, however, have shown that gains in self-reported knowledge are associated with positive behavior changes and can be useful for designing continuing education [16]. An advantage of the online survey method was better compliance with the survey instructions [17]. In this study, respondents were required to enter exactly three choices for the questions about their educational needs and interests, and this allowed the comparisons shown in Table 3 to be made.
This study had low response rate (5% overall and 31.6% among the emails that were opened by the recipients). This response rate is consistent with other reports of online surveys among health professionals [17–19]. In another study of email survey response behaviors, 32 non-profit organizations reported an average response rate of 4.5– 4.8% for surveys and advocacy email communications [20]. Compared to the overall membership of ONS [12], the respondents in this study were more likely to have at least a master’s degree (20.0% compared to 34.7%, respectively) and to work in education or administration (14.0% compared to 27.8%, respectively). This may have occurred because conducting the survey online provided a pool of respondents with a higher level of comfort with and interest in online education compared with those who did not respond. The online survey method, however, identified perceived barriers to using online courses from 109 individuals who reported that their level of comfort with online learning was relatively low, and these barriers can be addressed in future online education programs. An advantage of online education is that it is available to nurses regardless of geographic location and can reach nurses who may have limited access to local or national cancer education programs.
Conclusions
This study has identified areas for continuing nursing education related to cancer survivorship care based upon respondents’ level of current knowledge, interest, need to assist patients, and questions received from patients. Based on these findings, potential areas for priority education include physical late and long-term effects, managing emotional effects of cancer treatment, cancer screening and surveillance, and complementary and alternative therapies. For genetic issues, sexual dysfunction and sexual health, and practical issues such as employment, insurance, financial and legal concerns, some nurses want to learn how to help patients directly, and others may feel they can best address patient needs with referrals to multidiciplinary resources. Respondents indicated current capability and comfort level with online education, suggesting that this is a viable approach for disseminating education on survivorship care to nurses who are working with cancer patients.
Footnotes
Opinions expressed herein do not indicate or imply endorsement from the Oncology Nursing Society.
Conflicts of interest The authors declare no conflicts of interest.
Contributor Information
Jennifer R. Klemp, Email: jklemp@kumc.edu, Breast Cancer Survivorship Center, University of Kansas Cancer Center, University of Kansas School of Medicine, Cancer Center and Medical Pavilion, 2330 Shawnee Mission Parkway, Suite 1105, Westwood, KS 66205, USA.
Linda M. Frazier, Department of Obstetrics and Gynecology, University of Kansas School of Medicine-Wichita, Wichita, USA
Catherine Glennon, Department of Nursing, Cancer Center, University of Kansas Hospital Cancer Center, Kansas, USA.
Jill Trunecek, Breast Cancer Survivorship Center, University of Kansas Cancer Center, University of Kansas School of Medicine, Cancer Center and Medical Pavilion, 2330 Shawnee Mission Parkway, Suite 1105, Westwood, KS 66205, USA.
Margaret Irwin, Oncology Nursing Society, Kansas, USA.
References
- 1.American Cancer Society. [Accessed 09 Nov 2010];Cancer facts & figures, 2010. 2010 http://www.cancer.org/Research/CancerFactsFigures/index.
- 2.Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010;46(4):765–781. doi: 10.1016/j.ejca.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Ferrell BR, Virani R, Smith S, Juarez G. The role of oncology nursing to ensure quality care for cancer survivors: a report commissioned by the National Cancer Policy Board and Institute of Medicine. Oncol Nurs Forum. 2003;30(1):E1–E11. doi: 10.1188/03.ONF.E1-E11. [DOI] [PubMed] [Google Scholar]
- 4.Faithfull SE, Milly L, Haagedoorn Lecture EACE. Developing oncology nurse education and training across Europe. J Cancer Educ. 2006;21(4):212–215. doi: 10.1080/08858190701347697. [DOI] [PubMed] [Google Scholar]
- 5.Hewitt M, Greenfield S, Stovall E, editors. National Cancer Policy Board (NCPB) From cancer patient to cancer survivor—lost in transition. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 6.Patlak M, Levit L. Ensuring quality cancer care through the oncology workforce: sustaining care in the 21st century: workshop summary. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 7.Cheung WY, Fishman PN, Verma S. Oncology education in Canadian undergraduate and postgraduate training programs. J Cancer Educ. 2009;24(4):284–290. doi: 10.1080/08858190902973143. [DOI] [PubMed] [Google Scholar]
- 8.Ferrell BR, Winn R. Medical and nursing education and training opportunities to improve survivorship care. J Clin Oncol. 2006;10(24):5442–5148. doi: 10.1200/JCO.2006.06.0970. [DOI] [PubMed] [Google Scholar]
- 9.Anonymous. [Accessed 09 Nov 2010];Graduate programs in oncology nursing. http://ons.org/media/ons/docs/education/grad-onc-programs-list.pdf.
- 10.Grant M, Economou D, Ferrell B, Bhatia S. Preparing professional staff to care for cancer survivors. J Cancer Surviv. 2007;1(1):98–106. doi: 10.1007/s11764-007-0008-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grant M, Economou DD. Survivorship education for quality cancer care: update. Oncol Issues. 2010;25(3):48–49. [Google Scholar]
- 12.Irwin M, Klemp JR, Glennon C, Frazier LM. Oncology nurses’ perspectives on the state of cancer survivorship care: current practice and barriers to implementation. Oncol Nurs Forum. 2011;38(1):E11–E19. doi: 10.1188/11.ONF.E11-E19. [DOI] [PubMed] [Google Scholar]
- 13.Lance Armstrong Foundation, Centers for Disease Control and Prevention. A national action plan for cancer survivorship: advancing public health strategies. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2004. [Google Scholar]
- 14.2009–2013 Oncology Nursing Society Research Agenda Team. Berger AM, Cochrane B, Mitchell SA. The 2009–2013 research agenda for oncology nursing. Oncol Nurs Forum. 2009;36(5):E274–E82. doi: 10.1188/09.ONF.E274-E282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dillman DA. The tailored design method. 2nd edn. Hoboken: Wiley; 2007. Mail and internet surveys. [Google Scholar]
- 16.Institute of Medicine. Redesigning continuing education in the health professions. Washington, DC: The National Academies Press; 2010. [PubMed] [Google Scholar]
- 17.Kongsved SM, Basnov M, Hiolm-Christensen K, Hjollund NH. Response rate and completeness of questionnaires: a randomized study of Internet versus paper-and-pencil versions. J Med Internet Res. 2007;9(3):e25. doi: 10.2196/jmir.9.3.e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brogger J, Nystad W, Cappelen I, Bakke P. No increase in response rate by adding a web response option to a postal population survey: a randomized trial. J Med Internet Res. 2007;9(5):e40. doi: 10.2196/jmir.9.5.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buscaglia JM, Shin EJ, Giday SA, Kapoor S, Dunbar KB, Eloubeidi MA, Canto MI, Jagannath SB. Awareness of guidelines and trends in the management of suspected pancreatic cystic neoplasms: survey results among general gastroenterologists and EUS specialists. Gastrointest Endosc. 2009;69(4):813–820. doi: 10.1016/j.gie.2008.05.036. [DOI] [PubMed] [Google Scholar]
- 20.Matheson K, Ruben M, Ross H. [Accessed 25 Jan 2011];2009 eNonprofit benchmark study: an analysis of online messaging, fundraising and advocacy metrics for nonprofit organizations. 2009 http://www.ebenchmarksstudy.com/pubs/2009_eNonprofit_Benchmarks_Study.pdf.