Abstract
Background
Subjects with neurological disease (ND) usually show impaired performance during sit-to-stand and stand-to-sit tasks, with a consequent reduction in their mobility levels.
Objective
To determine the measurement properties and feasibility previously investigated for clinical tests that evaluate sit-to-stand and stand-to-sit in subjects with ND.
Method
A systematic literature review following the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) protocol was performed. Systematic literature searches of databases (MEDLINE/SCIELO/LILACS/PEDro) were performed to identify relevant studies. In all studies, the following inclusion criteria were assessed: investigation of any measurement property or the feasibility of clinical tests that evaluate sit-to-stand and stand-to-sit tasks in subjects with ND published in any language through December 2012. The COSMIN checklist was used to evaluate the methodological quality of the included studies.
Results
Eleven studies were included. The measurement properties/feasibility were most commonly investigated for the five-repetition sit-to-stand test, which showed good test-retest reliability (Intraclass Correlation Coefficient:ICC=0.94-0.99) for subjects with stroke, cerebral palsy and dementia. The ICC values were higher for this test than for the number of repetitions in the 30-s test. The five-repetition sit-to-stand test also showed good inter/intra-rater reliabilities (ICC=0.97-0.99) for stroke and inter-rater reliability (ICC=0.99) for subjects with Parkinson disease and incomplete spinal cord injury. For this test, the criterion-related validity for subjects with stroke, cerebral palsy and incomplete spinal cord injury was, in general, moderate (correlation=0.40-0.77), and the feasibility and safety were good for subjects with Alzheimer's disease.
Conclusions
The five-repetition sit-to-stand test was used more often in subjects with ND, and most of the measurement properties were investigated and showed adequate results.
Keywords: rehabilitation, nervous system diseases, movement, reproducibility of results, clinical protocols, revision
Introduction
According to the World Health Organization1, neurological diseases (NDs) are conditions that affect the central or peripheral nervous system of humans. With the decrease in mortality rates, there are increasingly more individuals affected by ND who have major disabilities, such as limitations in daily activities2. Standing and sitting on a chair are among the most affected activities and are considered crucial for independence in the daily routine3. The inability to perform these actions may lead to disability4. Therefore, recovering or improving the performance of these activities is a major goal for rehabilitation teams4. To do so, practitioners need clinical tools that assess these activities5 with adequate measurement properties (such as validity and reliability)4,6.
In 1985, Czuka and McCarty7 proposed and documented the first standardized test to clinically assess the sit-to-stand movement, originally called timed-stands test. This test determined the time spent to perform 10 repetitions of the sit-to-stand movement7. Subsequent variations were developed, including the "20-second sit-to-stand test" (sit-to-stand test)8 and the "five-repetition sit-to-stand test" (five times sit-to-stand test)9. The latter has demonstrated good clinical feasibility in the elderly10 and good test-retest reliability in healthy individuals between 14 and 85 years of age11.
Considering that measurement and feasibility properties depend on the protocol used and are specific to the population studied12, the adequate results shown for some properties of the test in certain populations do not guarantee that these tests will be similarly suitable for individuals with ND. Thus, the present study aimed to determine the measurement or feasibility properties previously investigated in clinical trials that evaluated the sit-to-stand/stand-to-sit movement in individuals with ND.
Method
The present study is a systematic literature review conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol13,14. All stages were performed by two independent raters who, at the end of each stage, reached a consensus on the results obtained. A third rater was involved in case of disagreement between the first two raters13,14.
In the first stage, electronic searches were performed on the MEDLINE, SCIELO, LILACS and PEDro databases to identify studies, using a search strategy adequate for databases with combinations of terms relative to the tests of interest and measurement or feasibility properties (Appendix 1). Subsequently, the studies were assessed for the inclusion criteria: studies that investigated any measurement property or the feasibility of any clinical trial that assessed sit-to-stand and stand-to-sit tasks in individuals diagnosed with ND and studies that were published in any language through December 2012.
In the second stage, the titles of the studies were evaluated, and studies that clearly did not meet the inclusion criteria were excluded. The same procedure was used in the third stage, in which the abstracts of the studies included in the second stage were analyzed. In the fourth stage, all studies included in the third stage were fully read, and those that met the inclusion criteria were included. In the fifth stage, an active manual search was performed of all the references from the studies included in the electronic search, following the previously mentioned procedures13,14.
The sixth stage consisted of assessing the methodological quality of the studies using the Consensus-based standards for the selection of health Measurement Instruments (COSMIN)15-17, which features standardized criteria18 and allows the classification of the methodological quality of studies that investigate the measurement properties of an instrument15-18. COSMIN has been most commonly used to assess the methodological quality of questionnaire-based instruments and was developed for this purpose18-20. However, the tests investigated in the present study are performance-based. In the classification system proposed by Bloemendaal et al.19, the final score depends on the percentage of items scored in COSMIN, and this classification system had already been used in a systematic review of the measurement properties of other performance-based tests19. This classification system seemed adequate and was therefore used. Thus, the COSMIN criteria were used by two independent raters, who reached a consensus on the final classification of the methodological quality of the included studies, and a third rater was involved in case of disagreement19.
Results
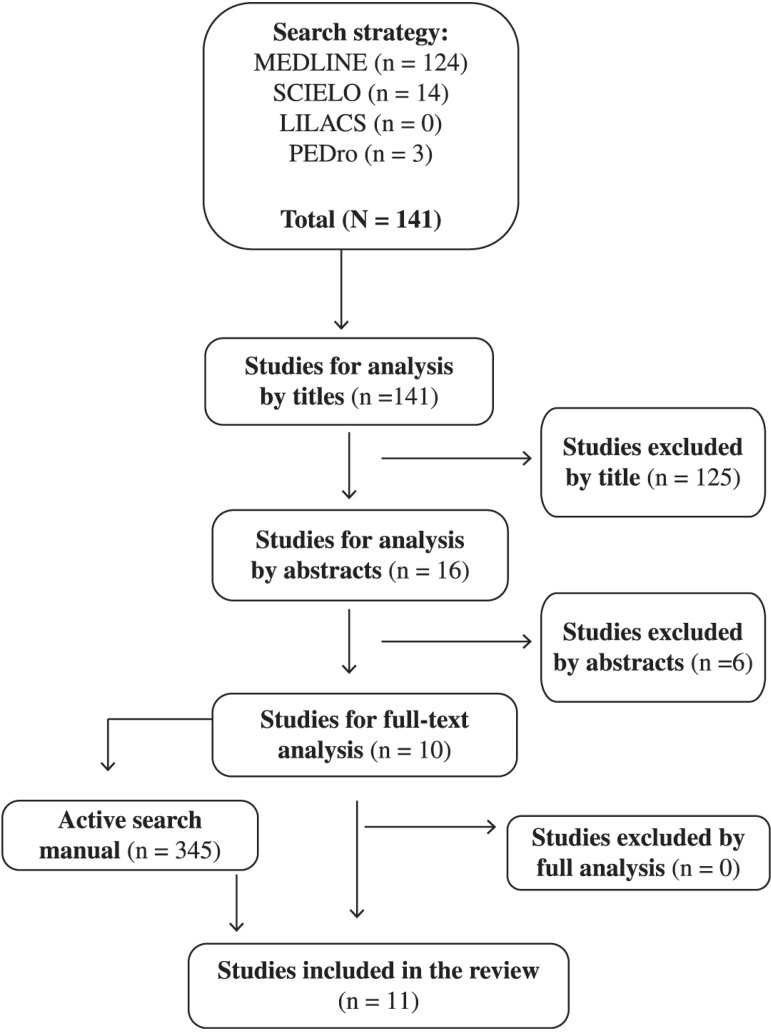
In total, 141 studies were found in the electronic search, 125 of which were excluded in the second stage of the analysis because they did not assess individuals with ND or were not related to clinical sit-to-stand and stand-to-sit tests. In the third stage, six studies were excluded because they did not refer to the population of interest or any test of interest or did not evaluate any property of the test used. In the fourth stage, all ten analyzed studies met the inclusion criteria and remained in the study. An active manual search was performed in these ten studies, which resulted in one more study being included, for a total of 11 studies (Figure 1). Considering the COSMIN classification system proposed by Bloemendaal et al.19, most of the studies included (96%)8,9,21-28 had a sufficient methodological quality, and one study (4%)29 had a good methodological quality (Table 1).
Figure 1.
Flow diagram of the literature search. n=number of studies.
Table 1.
Methodological quality assessment of the included studies according to COSMIN by Bloemendaal et al.19 (n=11).
| STUDY/TEST | PROPERTIES | COSMIN by Bloemendaal et al.19 |
|---|---|---|
| Pardo et al.24/T5R | ReliabilityT-RT and measurement error | Sufficient |
| Blankevoort et al.22/TNR30 | ReliabilityT-RT and measurement error | Sufficient |
| Moller et al.29/T5R | CCV | Good |
| Poncumhak et al.25/T5R | ReliabilityINTER and CCV | Sufficient |
| Wang et al.28/T5R | ReliabilityT-RT and measurement error | Sufficient |
| Reliability intrasession | Sufficient | |
| Convergent criterion-related validity | Sufficient | |
| Suttanon et al.26/T5R | ReliabilityT-RT and measurement error | Sufficient |
| Duncan et al.9/T5R | ReliabilityT-RT and INTER, and CV | Sufficient |
| Villamonte et al.8/TNR20 | ReliabilityT-RT | Sufficient |
| Mong et al.23/T5R | ReliabilityT-RT, INTER and INTRA, CCV and CV | Sufficient |
| Beninato et al.21/T5R | CV | Sufficient |
| Thomas et al.27/T5R | ReliabilityT-RT | Sufficient |
5RT: "five-repetition sit-to-stand test"; 30STST:"30-second sit-to-stand test"; 20STST: "20-second sit-to-stand test"; ReliabilityT-RT: testretest reliability; ReliabilityINTER: inter-rater reliability; CCV: concurrent criterion-related validity; CV: criterion-related validity (sensitivity/ specificity); ReliabilityINTRA: intra-rater reliability.
Three distinct tests were used to evaluate the sit-to-stand and stand-to-sit tasks: 82% of the studies (9/11)9,21,24-26,28 used the "five-repetition sit-to-stand test" (five times sit-to-stand test, 5-repetition sit-to-stand test23,29, sit-to-stand27), 9% of the studies (11/1)8 used the "20-second sit-to-stand test" (sit-to-stand test), and 9% (1/11)22 used the "30-second sit-to-stand test" (chair rise test) (Table 2).
Table 2.
Subjects' characteristics and clinical tests used for the assessment of sit-to-stand and stand-to-sit tasks in the included studies (n=11).
| STUDY | n | Neurological disease | Age (years) | Sex (M/F) | Test |
|---|---|---|---|---|---|
| Pardo et al.24 | 19 | Chronic stroke | 53.4±12.3 | 9/10 | "Five times sit-to-stand test"* |
| Blankevoort et al.22 | 52 | Dementia | 82.47±5.31 | 17/41 | "Chair rise test" |
| Moller et al.29 | 11 | Multiple sclerosis | _____ | 7/4 | "5-repetition sit-to-stand test"* |
| Poncumhak et al.25 | 66(V) and 16 (R) | Incomplete spinal Cord injury | (V): 50.9±13.4 and 50.2±9.5 (R): 50.8±10.3 | _____ | "Five times sit-to-stand test"* |
| Wang et al.28 | 108(RIS) and 22(R T-RT) | Cerebral palsy | n=108: 8.1±1.8 | 65/43 | "Five times sit-to-stand test"* |
| Suttanon et al.26 | 14 | Alzheimer disease | 79.57 ± 6.19 | 7/7 | "Five times sit-to-stand test"* |
| Duncan et al.9 | 80(V) and 10 (R T-RT and R IE) | Parkinson disease | n=80: 67 ± 9.0 | 47/33 | "Five times sit-to-stand test"* |
| Villamonte et al.8 | 21 | Down syndrome | Between 5 and 31 | 10/11 | "Sit-to-stand test" |
| Mong et al.23 | 12 | Chronic stroke | 60 ± 4.8 | 6/6 | "5-repetition sit-to-stand test"* |
| Beninato et al.21 | 27 | Chronic stroke | 57.2 ± 12.4 | 12/15 | "Five times sit-to-stand test"* |
| Thomas et al.27 | 10 | Dementia | 80.5±6.2 | F | "Sit-to-stand"* |
n: number of subjects; M/F: male/female; V: validity; R: reliability; RIS: reliability intra-session; RT-RT: test-retest reliability; RIE: inter-rater reliability; _____: not described
related to the same test: "five-repetition sit-to-stand test"
The populations of the included studies ranged from children to the elderly, and the "five-repetition sit-to-stand test" was used by most studies on the following individuals: those with stroke, ambulating independently (3/11)21,23,24; those with dementia, ambulating independently (1/11)27; those with multiple sclerosis (MS) but without disabilities or ambulating with bilateral weight bearing (1/11)29; those with incomplete spinal cord injury, ambulating with moderate dependence or independently (1/11)25; those with Parkinson's disease (PD) with minimal dysfunctions (1/11)9; those with Alzheimer's disease (AD), ambulating independently26 and those with cerebral palsy (CP) whose functional level was not described28 (Table 2). Individuals with Down Syndrome ambulating independently were also evaluated with the "20-second sit-to-stand test"8, and individuals with dementia, whose functional level was not described, were also evaluated with the "30-second sit-to-stand test"22 (Table 2).
Among the studies that investigated the "five-repetition sit-to-stand test", 77% used chairs with a fixed seat height9,21,23,24,26,27,29, and 11% used a seat height adjustable to the individual's leg length8,28 (Table 3). Most of the studies (77%) reported that there were no arm rests on the chair8,9,23-25,28,29, and 66% used chairs with backrests9,23-25,27. No study that used this test allowed the use of the upper limbs9,21,23-25,27,29, and in 90% of the studies, the upper limbs of the individual were crossed23,26,27 over the chest9,21,28 or over the torso24,29. Approximately 33% of the studies gave the patients a test demonstration23,24,28, 55.5% reported the number of repetitions performed in the test23-25,28,29, and 88.8% reported the instructions provided21,23-29 (Table 2).
Table 3.
Chair characteristics, subjects positioning and clinical tests protocols described in the included studies (n=11).
| STUDY/TEST | CHARACTERISTICS OF THE CHAIR, POSITIONING SUBJECTS AND PROTOCOLS |
|---|---|
| Pardo et al.24/T5R | Chair: fixed height; UL crossed over the torso; familiarization: one rep.; test: three rep.; instruction; FS. |
| Blankevoort et al.22/TNR30 | Instruction; FS; allowed to use UL. |
| Moller et al.29/T5R | Chair: height of 45cm; UL crossed over the torso; feet parallel; test demonstration; test: two rep.; instruction; FS. |
| Poncumhak et al.25/T5R | UL on the side; feet 10cm behind kness; test: three rep.; instruction; FS; now allowed the use of the UL. |
| Wang et al.28/T5R | Chair: height adjustable to 90º hip flexion and 105º knees flexion; UL crossed over the chest; barefoot; familiarization: three rep.; test: three rep.; instruction; FS. |
| Suttanon et al.26/T5R | Chair: height of 45cm; UL crossed; instruction; FS. |
| Duncan et al.9/T5R | Chair: height of 43cm; UL crossed over the chest; test demonstration. |
| Villamonte et al.8/TNR20 | Chair: height adjustable to 30, 35, 41or 46cm; knees flexed (90º); fixed and flat feet during test; test: three rep. |
| Mong et al.23/T5R | Chair: height of 43cm; UL crossed; familiarization: two rep.; test: three rep.; instruction; FS. |
| Beninato et al.21/T5R | Chair: height of 45cm; UL crossed over the chest; instruction; FS. |
| Thomas et al.27/T5R | Chair: height of 45cm; UL crossed; instruction; FS. |
5RT: "five-repetition sit-to-stand test"; 30STST:"30-second sit-to-stand test"; 20STST: "20-second sit-to-stand test"; UL: upper limbs; rep.: repetition(s); FS: fast speed; cm: centimeter
Studies evaluating individuals with stroke21,23,24 included participants in the chronic phase, from both genders, with a mean age between 53.4 and 60 years (Table 2). These studies investigated some properties of the "five-repetition sit-to-stand test", such as reliability (test-retest23,24, inter-rater23 and intra-rater23), criterion validity (sensitivity and specificity21) and concurrent criterion validity23, all with adequate results (Table 4). For this same test used in individuals with MS (Table 2), the concurrent criterion validity was investigated, and moderate to good correlations were obtained between lower limb strength and body sway with eyes open (Table 4).
Table 4.
Results related to the measurement properties and feasibility of the clinical tests used in the included studies (n=11).
| STUDY/TEST | PROPERTIES |
|---|---|
| Pardo et al.24/T5R | Test-retest reliability (ICC=0.87) and measurement error (SEM=1.8 and MDC=5.0) |
| Blankevoort et al.22/TNR30 | Test-retest reliability (ICC=0.84) and measurement error (SEM=1.26 and MDC=3.49) |
| Moller et al.29/T5R | ValidityCC: IS kneema extensor (r=-0.77) and flexor (r=-0.60), and hipma flexor (r=-0.60); CS kneema extensor (r=-0.70) and flexor (r=-0.64), BS with eyes opened (r=0.69) |
| Poncumhak et al.25/T5R | Inter-rater reliability (ICC=0.99); ValidityCC: (rps=-0.59) FIM |
| Wang et al.28/T5R | Intra-session reliability (ICC=0.95), test-retest reliability (ICC=0.99), measurement error (SEM=0.02, MDC=0.06); convergent criterion-related validity: IS hip flexor (r/rs=0.78) and abductor (r/rs=0.76) |
| Suttanon et al.26/T5R | Test-retest reliability (ICC=0.79) and measurement error (SEM=1.39, MDC=2.73); safety/feasibility: 100% of the subjects did not have any fall and were able to perform the test. |
| Duncan et al.9/T5R | Inter-rater (ICC=0.99) and test-retest reliability (ICC=0.76); CV (SEN=75% and SPE=68%) |
| Villamonte et al.8/TNR20 | Test-retest reliability: men (ICC=0.54) and women (ICC=0.76) |
| Mong et al.23/T5R | Inter-rater (ICC=0.99), intra-rater (ICC=0.97/0.98) and test-retest reliability (ICC=0.99/1.0); ValidityCC: IS kneema (rs= -0.75) and NA (rs=-0.83); CV (SEN=83% and SPE=75%) |
| Beninato et al.21/T5R | CV (SEN=67%, SPE=72%, PLR=2.4 and NLR=0.46) |
| Thomas et al.27/T5R | Test-retest reliability (ICC=0.94) |
5RT: "five-repetition sit-to-stand test"; 30STST:"30-second sit-to-stand test"; 20STST: "20-second sit-to-stand test"; ICC: intraclass correlation coefficient; SEM: standard error of measurement; MDC: minimum detectable change; ValidityCC: concurrent criterion-related validity; FIM: Functional Independent Measurement; ma: most affected; rps: point biserial correlation coefficient; IS: isometric strength; CS: concentric strength; BS: body-sway; r: Pearson correlation coefficient; rs: spearman correlation coefficient; NA: not affected; CV: criterion-related validity; SEN: sensitivity; SPE: specificity; PLR: positive likelihood ratio; NLR: negative likelihood ratio
For the "five-repetition sit-to-stand test", the concurrent criterion validity was investigated with functional independence measures in individuals with incomplete spinal cord injury, using a point biserial correlation coefficient and obtaining a negative value of 0.59525 (Tables 2 and 4). In children with CP (Table 2), the convergent criterion validity was investigated, and Pearson's Correlation Coefficient values of 0.4 to 0.7828 were obtained (Table 4). For the population with dementia (Table 2), the test-retest reliability was assessed, and an intraclass correlation coefficient (ICC) value of 0.9427 (Table 4) was obtained. For individuals with AD (Table 2), the test was considered safe and with good clinical feasibility26 (Table 4).
The only study that used the "20-second sit-to-stand test" provided instructions regarding the pace of the test and allowed the participants to use their upper limbs (Table 3). Moreover, this study assessed the test-retest reliability in 21 individuals with Down Syndrome between five and 31 years from both genders who were ambulating independently (Table 2). Significant and at least moderate CCI values (0.54 to 0.76) (Table 4)8 were obtained. The only study that used the "30-second sit-to-stand test" used a chair with adjustable seat height, performed three repetitions of the test (Table 3) and assessed the test-retest reliability and measurement error in 52 subjects with mild to moderate dementia (Table 2). To investigate the measurement properties, intra-class correlation coefficients (ICC), standard measurement error and minimal detectable change were used, and values of 0.84, 1.26 and 3.49, respectively, were obtained (Table 4)22.
Discussion
The present study aimed to determine the measurement or feasibility properties of clinical trials that evaluated the sit-to-stand and stand-to-sit movements in individuals with ND. When assessing the methodological quality, many of the included studies obtained sufficient results by the classification system proposed by Bloemendaal et al.19. The lower scores were due to a small sample size and a lack of a description of the conditions of the individuals who performed the repeated measures, while the highest scores were related to the use of adequate statistical tests to assess the measurement properties.
Generally, the most commonly used test was the "five-repetition sit-to-stand test", and the most investigated property was the test-retest reliability. Other reliability measures were investigated, such as measurement error and criterion validity (convergent, concurrent, sensitivity/specificity), safety and clinical feasibility, most of which yielded adequate results. This test was performed in children, adults and the elderly, and individuals with stroke were those most commonly evaluated. The test-retest reliability and the measurement error of the "30-second sit-to-stand test" were also investigated in individuals with dementia, and the test-retest reliability of the "20-second sit-to-stand test" was assessed in individuals with Down syndrome, generally with adequate results. Other populations of individuals with ND and other properties were not investigated.
When comparing the results of several studies that evaluated the same property of the same test in populations with different NDs, the present review showed that the "five-repetition sit-to-stand test" showed a higher test-retest reliability in individuals with stroke23,24, dementia26 and CP28, although this property was also good for the other populations studied, PD9 and AD26. Regarding the inter-rater reliability of this same test, the results were adequate12 and similar in individuals with stroke23, incomplete spinal cord injury25 and PD9. In the population with stroke, this same test also showed adequate values12 of intra-rater reliability, similar to those obtained for inter-rater reliability23.
Some studies added informative value to the test-retest reliability measures by also assessing the measurement error by calculating the standard error of the mean and the minimum detectable change, which reflects the variability of the data in the sample12. However, this property was analyzed for more than one population group only for the "five-repetition sit-to-stand test", and the results indicated a lower variability in the measurements of this test in individuals with CP28, followed by individuals with AD26. For individuals with stroke24, the variability was considerably higher. Therefore, the possibility of this test providing more stable measurements with fewer errors is higher12 in individuals with CP. In individuals with stroke, the changes observed between assessments performed at different times (such as pre- and post-intervention) should not be related to the measurement error that may occur when using this test12.
The concurrent criterion validity of the "five-repetition sit-to-stand test" was assessed in individuals with stroke23, multiple sclerosis29, incomplete spinal cord injury25 and CP28. For individuals with stroke, significant correlations were obtained with isometric strength of the extensor muscles of both knees23, which were negative and with good magnitude12. For individuals with multiple sclerosis, the correlations found were significant, negative and moderate12 for lower limb strength and body sway with eyes open29. For individuals with incomplete spinal cord injury, significant, negative and moderate correlations12 with the Functional Independence Measure scores25 were reported. Finally, for children with CP, significant correlations were reported, which were positive and good12, for isometric muscle strength of hip flexors and abductors28. Therefore, this test showed better validity for the isometric strength of knee extensor muscles in individuals with stroke and hip flexors and abductors in individuals with CP.
Other measurement and feasibility properties were not studied for the same test in different populations, so comparisons similar to those previously performed could not be made. Conversely, a given property was investigated for different tests applied to the same population group. Two studies investigated the test-retest reliability for individuals with dementia, one investigated the "five-repetition sit-to-stand test"27 and one investigated the "30-second sit-to-stand test"22. In this comparison, the "five-repetition sit-to-stand test" showed higher ICC values when compared to the "30-second sit-to-stand test"12; thus, the former test seems to be the most adequate for individuals with dementia.
The "five-repetition sit-to-stand test" was the only test that showed any of the feasibility properties investigated, which were safety and clinical feasibility in individuals with AD. The results were similar to those reported by studies that investigated these measurement properties for this test in individuals without ND7,10. The test proved to be fast, was easy to perform, demanded little physical space and did not require special equipment. Further studies that clarify the feasibility of tests that assess the sit-to-stand movement in individuals with conditions other than NDs are still necessary.
Unlike already well-established clinical trials30, the protocols of the tests used to evaluate the sit-to-stand movement are still not completely standardized or clearly described by the studies. This limitation hinders the interpretation of the results and the reproduction of the tests in a clinical environment, given that parameters such as instructions, for example, may influence the results of performance-based tests31. In addition, in a literature review, Janssen et al.32 identified 19 determinants of the sit-to-stand movement, which have been clearly established and grouped into three categories related to the chair (such as seat height and the presence of arm and torso support), the individual (such as age, underlying disease and the use of shoes) and the strategy (such as speed and the positioning of the feet and upper limbs). These determinants influence the movement performed and may therefore influence the test results. Thus, ideally the sit-to-stand movement should be standardized, taking into consideration these determinants, including the characteristics of the individual32, so that the standardization would not compromise the clinical feasibility of the tests.
One of the determining factors for the sit-to-stand movement is the speed with which these activities are performed: when fast, the muscular demand imposed on the lower limbs of the individual is high32. Most likely, to require the maximum biomechanical performance, the test speed used in most studies was as high as possible21-29. Another determining factor for the sit-to-stand movement is the size of the chair and its other characteristics. The height of the chair has already been shown to interfere with the performance of the sit-to-stand movement32. One strategy already proposed for standardization is adjusting the chair height to the leg length of the individual, which was adopted only by two studies8,28. In most of the studies, the seat height was fixed9,21,23,24,26,27,29, and the results reflected the grouping of biomechanically favored and disadvantaged individuals according to the relationship between leg length and seat height.
Another determining factor for the sit-to-stand movement is the use of the upper limbs, which decreases the biomechanical demand for the individual, such as the muscular demand of the lower limbs32. Possibly for this reason, most studies did not allow the use of the upper limbs during the tests9,21,23-29. Conversely, not using the upper limbs during the test can hinder or prevent its application in individuals with greater motor impairment33, who are often a large portion of the population affected by ND34. These reasons may explain why a clear standardization regarding the positioning of the upper limbs was not observed among these studies, which on the one hand, increased the number of individuals able to perform the tests but on the other hand, created difficulty in comparing the results. Moreover, studies comparing the results of the different tests that assessed the sit-to-stand movement and considered the use of the upper limbs and their positioning were not found. We suggest the establishment of criteria or categories for the analysis that consider the functionality level of the individual when determining the best standardization for the upper limbs in these tests. This guideline would allow a greater proportion of individuals with ND to be included, as they are already included in studies that used the "five-repetition sit-to-stand test" in the elderly35.
The positioning of the feet (symmetrical, asymmetrical, both in front of and behind the knees) may also modify the biomechanical demand and the strategy for performing the sit-to-stand movement32,36,37. Only two studies described this feature: the feet were positioned 10 cm behind the knees in individuals with incomplete spinal cord injury25 and parallel to each other in individuals with multiple sclerosis29. In the first case, the muscular demand of the lower limbs is lower, and therefore, the time spent on the test may be shorter. The parallel positioning may facilitate or hinder the test performance, depending on the population group. According to a study conducted on individuals with stroke36, the parallel positioning requires symmetry in the biomechanical demand of the lower limbs, which, in this population, could hinder the test performance. However, it is uncertain whether the same effect would apply to individuals with other NDs. Both studies that described the feet positioning used during the test investigated the criterion validity but for distinct constructs, which does not allow comparisons between them.
Final remarks
The clinical evaluation of the sit-to-stand movement in individuals with ND has been performed using three different tests. The "five-repetition sit-to-stand test" is the most widely used and investigated test, and it shows the best reliability in individuals with stroke, dementia and CP, as well as the best criterion validity in individuals with stroke and CP. This test was also considered the most adequate for individuals with dementia when compared to the "30-second sit-to-stand test" because it showed the best test-retest reliability values. The feasibility properties were investigated only for the "five-repetition sit-to-stand test" in individuals with AD, and good results were obtained. There are still not enough data on the main determining factors of the sit-to-stand movement to allow the adequate standardization of the test protocols, which hinders the investigation of measurement properties and intra- and inter-group comparisons. Furthermore, although adequate results were already found for measurement and feasibility properties when evaluating these clinical trials, properties that may better reflect the clinical usefulness of these tests have not yet been investigated, such as responsiveness, or were not thoroughly discussed, such as safety, clinical feasibility and inter- and intra-rater reliability in different NDs.
Acknowledgments
We thank the Minas Gerais Research Foundation (Fundação de Amparo à Pesquisa do Estado de Minas Gerais - FAPEMIG), the Brazilian Federal Agency for Support and Evaluation of Graduate Education (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - CAPES), the National Council for Scientific and Technological Development (Conselho Nacional de Desenvolvimento Científico e Tecnológico - CNPq) and the Dean of Research of the Federal University of Minas Gerais (Pró-reitoria de Pesquisa da Universidade Federal de Minas Gerais /Universidade Federal de Minas Gerais - PRPq / UFMG) for the financial support.
Appendix 1. Search strategy.
DATABASES: MEDLINE, SCIELO, LILACS e PEDro MEDLINE
50. "Five times sit-to-stand test"
51. Five times sit-to-stand
52. "Five-times-sit-to-stand test"
53. Five-times-stand-to-sit-test
54. 5-times-stand-to-sit-test
55. "Five repetition sit-to-stand test"
56. "Five-repetition sit-to-stand test"
57. Five-repetition-stand-to-sit-test
58. "5-repetition sit-to-stand test"
59. "5-repetition STS test"
60. Test-of-5-repetition-sit-to-stand
61. 5-repetition-stand-to-sit-test
62. Ten-repetition-sit-to-stand-test
63. "Sit-to-stand test"
64. "STS test"
65. "Sit to stand test"
66. "Sit-to-stand-to-sit test"
67. STST
68. "Chair-rise test"
69. "Chair-stand test"
70. "Chair-rising test"
71. "Timed-stands test"
72. Timed-sit-stand-test
73. Agreement
74. Consistency
75. "Internal consistency"
76. "Validity OR reliability"
77. "Ceiling effect*"
78. "Floor effect*"
79. Sensitivity
80. Specificity
81. Accuracy
82. Reproducibility
83. Repeatability
84. Applicability
85. Responsiveness
86. Responsivity
87. "Psychometric properties"
88. "Clinimetric properties"
89. "Psychometric data"
90. "Instrument psychometrics"
91. "Psychometric tests"
92. "Change score"
93. "Difference score"
94. Generalizability
95. "Minimal clinically important difference"
96. MCID
97. Feasibility
98. (1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24) AND (25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48)
SCIELO, LILACS and PEDro
43. "Five times sit-to-stand test" or Five times sit-to-stand
44. "Five-times-sit-to-stand test" or Five-times-stand-to-sit-test
45. 5-times-stand-to-sit-test or "Five repetition sit-to-stand test"
46. "Five-repetition sit-to-stand test" or Five-repetition-stand-to-sit-test
47. "5-repetition sit-to-stand test" or "5-repetition STS test"
48. Test-of-5-repetition-sit-to-stand or 5-repetition-stand-to-sit-test
49. Ten-repetition-sit-to-stand-test or "Sit-to-stand test"
50. "STS test" or "Sit to stand test"
51. "Sit-to-stand-to-sit test" or STST
52. "Chair-rise test" or "Chair-stand test" or "Chair-rising test"
53. "Timed-stands test" or Timed-sit-stand-test
54. Agreement
55. Consistency or "internal consistency"
56. "Validity OR reliability"
57. "Ceiling effect*"
58. "Floor effect*"
59. Sensitivity
60. Specificity
61. Accuracy
62. Reproducibility or Repeatability
63. Applicability
64. Responsiveness or Responsivity
65. "Psychometric properties"
66. "Clinimetric properties"
67. "Psychometric data"
68. "Instrument psychometrics"
69. "Psychometric tests"
70. "Change score" or "Difference score"
71. Generalizability
72. "Minimal clinically important difference" or MCID
73. Feasibility
74. (1) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
75. (2) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
76. (3) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
77. (4) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
78. (5) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
79. (6) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
80. (7) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
81. (8) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
82. (9) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
83. (10) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
84. (11) AND (12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31)
References
- 1.World Health Organization - WHO . What are neurological disorders? [online] Geneva: World Health Organization; 2007. [cited 2007]. Available from: www.who.int/features/qa/55/en/ [Google Scholar]
- 2.World Health Organization - WHO . Neurological disorders: public health challenges [online] Geneva: World Health Organization; 2006. [cited 2006]. Available from: www.who.int/mental_health/neurology/neurodiso/en/ [Google Scholar]
- 3.Lomaglio MJ, Eng JJ. Muscle strength and weight-bearing symmetry relate to sit-to-stand performance in individuals with stroke. Gait Posture. 2005;22:126–131. doi: 10.1016/j.gaitpost.2004.08.002. http://dx.doi.org/10.1016/j.gaitpost.2004.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ng SSM. Balance ability, not muscle strength and exercise endurance, determines the performance of hemiparetic subjects on the timed-sit-to-stand test. Am J Phys Med Rehabilitation. 2010;89:497–504. doi: 10.1097/PHM.0b013e3181d3e90a. http://dx.doi.org/10.1097/PHM.0b013e3181d3e90a [DOI] [PubMed] [Google Scholar]
- 5.Sim J, Arnell P. Measurement validity in physiscal therapy research. Phys Ther. 1993;73(2):48–61. doi: 10.1093/ptj/73.2.102. [DOI] [PubMed] [Google Scholar]
- 6.Tyson S, Connell L. The psychometric properties and clinical utility of measures of walking and mobility in neurological conditions: a systematic review. Clin Rehabil. 2009;23:1018–1033. doi: 10.1177/0269215509339004. http://dx.doi.org/10.1177/0269215509339004 [DOI] [PubMed] [Google Scholar]
- 7.Czuka M, McCarty DJ. Simple method for measurement of lower extremity muscle strenght. Am J Med. 1985;78:77–81. doi: 10.1016/0002-9343(85)90465-6. http://dx.doi.org/10.1016/0002-9343(85)90465-6 [DOI] [PubMed] [Google Scholar]
- 8.Villamonte R, Vehrs PR, Feland JB, Johnson AW, Seeley MK, Eggett D. Reliability of 16 balance tests in individuals with Down Syndrome. Percept Mot Skills. 2010;111(2):530–542. doi: 10.2466/03.10.15.25.PMS.111.5.530-542. http://dx.doi.org/10.2466/03.10.15.25.PMS.111.5.530-542 [DOI] [PubMed] [Google Scholar]
- 9.Duncan RP, Leddy AL, Earhart GM. Five times sit-to-stand test performance in Parkinson's Disease. Arch Phys Med Rehabil. 2011;92:1431–1436. doi: 10.1016/j.apmr.2011.04.008. http://dx.doi.org/10.1016/j.apmr.2011.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tiedemann A, Shimada H, Sherrington C, Murray S, Lord SR. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing. 2008;37:430–435. doi: 10.1093/ageing/afn100. http://dx.doi.org/10.1093/ageing/afn100 [DOI] [PubMed] [Google Scholar]
- 11.Bohannon RW, Bubela DJ, Magasi SR, Gershon RC. Relative reliability of three objectives tests of limb muscle strength. Isokinet Exerc Sci. 2011;19:77–81. doi: 10.3233/IES-2011-0400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. New Jersey: Prentice Hall; 2009. [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;339:332–336. [PMC free article] [PubMed] [Google Scholar]
- 14.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies tha evaluate health care interventions: explanation and elaboration. Ann Inter Med. 2009;151(4):65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. http://dx.doi.org/10.7326/0003-4819-151-4-200908180-00136 [DOI] [PubMed] [Google Scholar]
- 15.Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, et al. Protocol of the COSMIN study: COnsensus-based Standards for the selection of health Measurement INstruments. BMC Med Res Methodol. 2006;6:2. doi: 10.1186/1471-2288-6-2. http://dx.doi.org/10.1186/1471-2288-6-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balemans AC, Fragala-Pinkham MA, Lennon N, Thorpe D, Boyd RN, O'neil ME, et al. Systematic review of the clinimetric properties of laboratory-and field-based aerobic and anaerobic fitness measures in children with cerebral palsy. Arch Phys Med Rehabil. 2013;94:287–301. doi: 10.1016/j.apmr.2012.09.012. http://dx.doi.org/10.1016/j.apmr.2012.09.012 [DOI] [PubMed] [Google Scholar]
- 17.Dobson F, Hinman RS, Terwee CB, Ross EM, Bennell KL. Measurement properties of performance-based measures to assess physical function in hip and knee osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2012;20:1548–1562. doi: 10.1016/j.joca.2012.08.015. http://dx.doi.org/10.1016/j.joca.2012.08.015 [DOI] [PubMed] [Google Scholar]
- 18.Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality os studies on measurement properties of healty status measurement instruments: an international Delphi study. Qual Life Res. 2010;19:539–549. doi: 10.1007/s11136-010-9606-8. http://dx.doi.org/10.1007/s11136-010-9606-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bloemendaal M, Water ATM, Port IGL. Walking tests for stroke survivors: a systematic review of their measurement properties. Disabil Rehabil. 2012;34(26):2207–2221. doi: 10.3109/09638288.2012.680649. http://dx.doi.org/10.3109/09638288.2012.680649 [DOI] [PubMed] [Google Scholar]
- 20.Terwee CB, Mokkink LB, Knol DL, Ostelo RWJG, Bouter LM, Vet HCW. Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual Life Res. 2012;21:651–657. doi: 10.1007/s11136-011-9960-1. http://dx.doi.org/10.1007/s11136-011-9960-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beninato M, Portney LG, Sullivan PE. Using the International Classification of Functioning, Disability and Health as a framework to examine the association between falls and clinical assessment tools in people with stroke. Phys Ther. 2009;89(8):816–828. doi: 10.2522/ptj.20080160. http://dx.doi.org/10.2522/ptj.20080160 [DOI] [PubMed] [Google Scholar]
- 22.Blankevoort CG, Heuvelen MJG, Scherder EJA. Reliability of six physical performance tests in older people with dementia. Phys Ther. 2012;93:69–78. doi: 10.2522/ptj.20110164. http://dx.doi.org/10.2522/ptj.20110164 [DOI] [PubMed] [Google Scholar]
- 23.Mong Y, Teo TW, Ng SS. 5-repetition sit-to-stand in subjects with chronic stoke: reliability and validity. Arch Phys Med Rehabil. 2010;91:407–413. doi: 10.1016/j.apmr.2009.10.030. http://dx.doi.org/10.1016/j.apmr.2009.10.030 [DOI] [PubMed] [Google Scholar]
- 24.Pardo V, Knuth D, McDermott B, Powell J, Goldberg A. Validity, reliability and minimum detectable change of the maximum step length test in people with stroke. J Neurol Sci. 2013;325:74–78. doi: 10.1016/j.jns.2012.11.021. http://dx.doi.org/10.1016/j.jns.2012.11.021 [DOI] [PubMed] [Google Scholar]
- 25.Poncumhak P, Saengsuwan J, Kumruecha W, Amatachaya S. Reliability and validity of three functional tests in ambulatory patients with spinal cord injury. Spinal Cord. 2013;51(3):214–217. doi: 10.1038/sc.2012.126. http://dx.doi.org/10.1038/sc.2012.126 [DOI] [PubMed] [Google Scholar]
- 26.Suttanon P, Hill KD, Dodd KJ, Said CM. Retest reliability of balance and mobility measurements in people with mild to moderate Alzheimer's disease. Int Psychogeriatr. 2011;23(7):1152–1159. doi: 10.1017/S1041610211000639. http://dx.doi.org/10.1017/S1041610211000639 [DOI] [PubMed] [Google Scholar]
- 27.Thomas VS, Hageman PA. A preliminary study on the reliability of physical performance measures in older day-care center clients with dementia. Int Psychogeriatr. 2002;14(01):17–23. doi: 10.1017/s1041610202008244. http://dx.doi.org/10.1017/S1041610202008244 [DOI] [PubMed] [Google Scholar]
- 28.Wang TH, Liao HF, Peng YC. Reliability and validity of the five-repetition sit-to-stand test for children with cerebral palsy. Clin Rehabil. 2011;26(7):664–671. doi: 10.1177/0269215511426889. http://dx.doi.org/10.1177/0269215511426889 [DOI] [PubMed] [Google Scholar]
- 29.Moller AB, Bibby BM, Skjerbaek AG, Jensen E, Sorensen H, Stenager E, et al. Validity and variability of the 5-repetition sit-to-stand test in patients with multiple sclerosis. Disabil Rehabil. 2012;34(26):2251–2258. doi: 10.3109/09638288.2012.683479. http://dx.doi.org/10.3109/09638288.2012.683479 [DOI] [PubMed] [Google Scholar]
- 30.Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008;88(5):559–566. doi: 10.2522/ptj.20070205. http://dx.doi.org/10.2522/ptj.20070205 [DOI] [PubMed] [Google Scholar]
- 31.Nascimento LR, Caetano LCG, Freitas DCMA, Morais TM, Polese JC, Teixeira-Salmela LF. Different instructions during the ten-meter walking test determined significant increases in maximum gait speed in individuals with chronic hemiparesis. Rev Bras Fisioter. 2012;16(2):122–127. doi: 10.1590/s1413-35552012005000008. http://dx.doi.org/10.1590/S1413-35552012005000008 [DOI] [PubMed] [Google Scholar]
- 32.Janssen WGM, Bussmann HBJ, Stam HJ. Determinants of sit-to-stand movement: a review. Phys Ther. 2002;82(9):866–879. [PubMed] [Google Scholar]
- 33.Bohannon RW. Five-repetition sit-to-stand test: usefulness for older patients in a home-care setting. Percept Mot Skills. 2011;112(3):803–306. doi: 10.2466/15.26.PMS.112.3.803-806. http://dx.doi.org/10.2466/15.26.PMS.112.3.803-806 [DOI] [PubMed] [Google Scholar]
- 34.Teixeira-Salmela LF, Oliveira ESG, Santana EGS, Resende GP. Fortalecimento muscular e condicionamento físico em hemiplégicos. Acta Fisiátrica. 2000;7(3):108–118. [Google Scholar]
- 35.Cesari M, Onder G, Zamboni V, Manini T, Shorr RI, Russo A, et al. Physical function and self-rated health status as predictors of mortality: results from longitudinal analysis in the ilSIRENTE strudy. BMC Geriatr. 2008;8(34):1–9. doi: 10.1186/1471-2318-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lecours J, Nadeau S, Gravel D, Teixeira-Salmela LF. Interactions between foot placement, trunk frontal position, weight-bearing and knee moment asymmetry at seat-off during rising from a chair in healthy controls and persons with hemiparesis. J Rehabil Med. 2008;40:200–207. doi: 10.2340/16501977-0155. http://dx.doi.org/10.2340/16501977-0155 [DOI] [PubMed] [Google Scholar]
- 37.Roy G, Nadeau S, Gravel D, Malouin F, McFadyen BJ, Piotte F. The effect of foot placement and chair height on the asymmetry of vertical forces during sit-to-stand and stand-to-sit tasks in individuals with hemiparesis. Clin Biomech. 2006;21:585–593. doi: 10.1016/j.clinbiomech.2006.01.007. http://dx.doi.org/10.1016/j.clinbiomech.2006.01.007 [DOI] [PubMed] [Google Scholar]