Abstract
Objective
Inflammation is a mechanism of host response to infection which can be harmful when inappropriately modulated. Soluble ST2 (sST2) is a decoy receptor of interleukin (IL)-33, and this complex modulates the balance in the Th1/Th2 immune response. Moreover, sST2 inhibits the production of pro-inflammatory cytokines in cooperation with an anti-inflammatory cytokine, IL-10. The objectives of this study were to: 1) determine whether umbilical cord plasma sST2 concentration differ between comparing preterm neonates with and without funisitis and between those with and without the fetal inflammatory response syndrome (FIRS); and 2) evaluate the relationship between sST2 and IL-10 among neonates with funisitis and/or FIRS.
Methods
Umbilical cord plasma was collected from neonates delivered prematurely due to preterm labor or preterm prelabor rupture of membranes with (n=36), and without funisitis (n=30). FIRS (umbilical cord IL-6 concentration ≥17.5 pg/mL) was identified in 29 neonates. Plasma sST2 and IL-10 concentrations were determined by ELISA.
Results
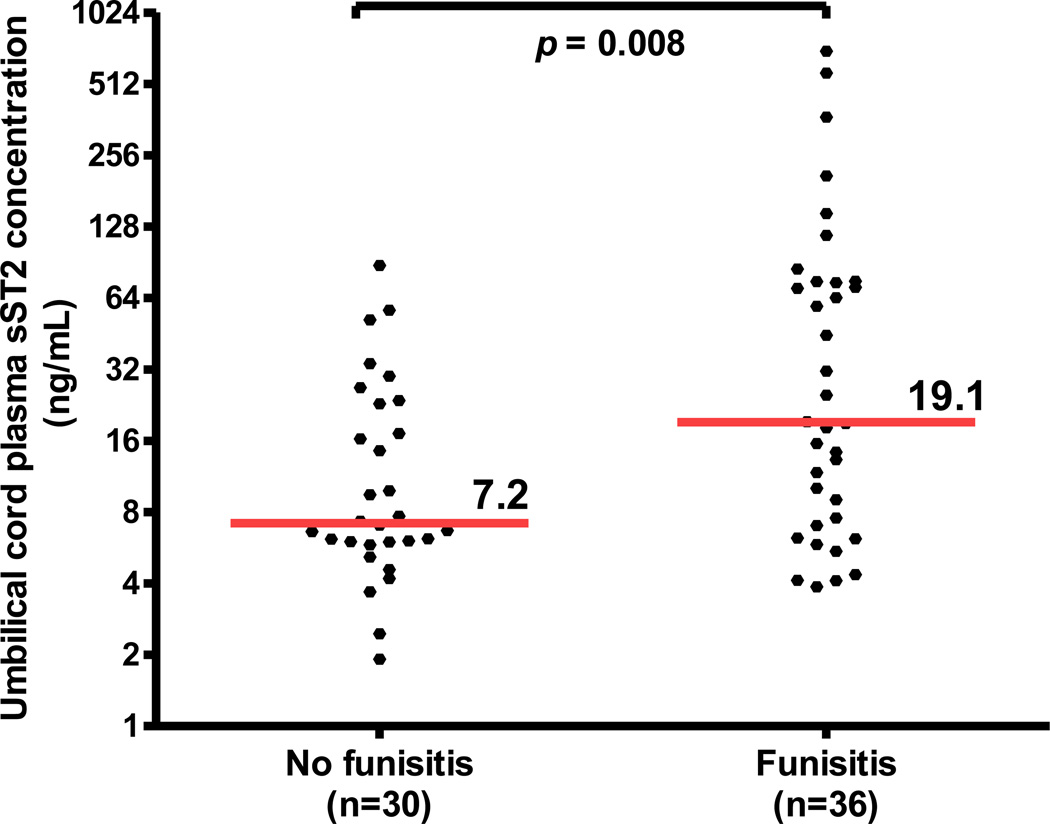
The median umbilical cord plasma sST2 concentration was 6.7-fold higher in neonates with FIRS than in those without FIRS (median 44.6 ng/mL, interquartile range [IQR] 13.8–80.3 ng/mL vs. median 6.7 ng/mL, IQR 5.6–20.1 ng/mL; p<0.0001). Similarly, the median umbilical cord plasma sST2 concentration was 2.6-fold higher in neonates with funisitis than in those without funisitis (median 19.1 ng/mL; IQR 7.1–75.0 ng/mL vs. median 7.2 ng/mL; IQR 5.9–23.1 ng/mL; p=0.008). There was a strong positive correlation between sST2 and IL-10 in neonates with funisitis and/or FIRS (Spearman’s Rho=0.7, p<0.0001).
Conclusions
FIRS and funisitis are associated with an elevation of umbilical cord plasma concentrations of soluble ST2. This protein represents an important mediator of the immune response in neonates diagnosed with fetal inflammatory response syndrome by promoting an anti-inflammatory effect in association with IL-10.
Keywords: funisitis, IL-10, intra-amniotic infection/inflammation, inflammation, preterm labor
Introduction
Intra-amniotic infection is associated with the spontaneous onset of labor [1–9] in patients with preterm labor (PTL) and intact membranes [10–27], and patients with preterm prelabor rupture of membranes (PROM) [28–38]. Moreover, this condition has been identified in a subset of patients with a short cervix [39–42], cervical insufficiency [43,44], and other conditions which confer increased risk for preterm delivery, such as an intrauterine device in pregnancy [45], vaginal bleeding [46], and placenta previa [47].
Microbial invasion of the amniotic cavity (MIAC) can lead to fetal infection [21,48–51]. Indeed, fetal bacteremia detected in blood obtained by cordocentesis has been reported in 30% of patients who have intra-amniotic infection [51], and one-fifth of preterm neonates born before 32 weeks of gestation have evidence of bacteremia in umbilical cord blood [52,53]. Subsequently, fetal microbial invasion may lead to a systemic inflammatory response, which we have termed the fetal inflammatory response syndrome (FIRS) [21,54]. This can be detected by the presence of elevated concentrations of cytokines, such as interleukin (IL) 6, in umbilical cord blood [21,55,56] or alternatively, by the presence of inflammation in the umbilical cord (funisitis) [55–58] or chorionic vasculitis [58].
FIRS is associated with the impending onset of labor [59], as well as multi-systemic involvement and high risk of short- and long-term complications [21,54,56,60]. The fetal organ systems involved include the skin [61–63], heart [64–66], lungs [67–74], eyes [75], kidneys [76], adrenal glands [77], hematologic system [78–80], thymus [81–83] and the central nervous system [84–97]. Although FIRS is frequently found in patients with intra-amniotic infection/inflammation (IAI), it can also be observed in fetuses with congenital viral infection [98–104] or alloimmunization [105].
Inflammation is a host defense mechanism elicited by insults such as infection [106], trauma [107], ischemia-reperfusion injury [108,109], necrosis [110], and tissue injury [111,112]. The innate immune system provides the first line of defense against infection through the engagement of pattern recognition receptors (i.e. Toll-like receptors, TLRs) [113–117], which recognize microbial products [118–120] and induce an inflammatory response [121–123] through the production of both chemokines and cytokines [123–125]. The crucial balance between pro- and anti-inflammatory responses is regulated, in part, by an inhibitory system activated by the anti-inflammatory limb of the immune response [126–129]. IL-10 is considered a key player in this process, serving as a major anti-inflammatory mediator, since it is produced mainly by monocytes and inhibits the transcription of pro-inflammatory cytokines [126,130,131]. Inappropriate modulation of this process may result in immunosuppression or an exaggerated inflammatory response; both can be harmful to the host, as shown in experimental and observational studies [56,67,132]. Indeed, a major cause of death in patients with sepsis is immunosuppression [133].
ST2 is a member of the IL-1 receptor super-family [134] and exists in four isoforms. The two best characterized isoforms are: 1) ST2L, a membrane receptor; and 2) soluble ST2 (sST2)[134,135]. The ligand for ST2L and sST2 is IL-33 [136]. Upon binding to ST2L, IL-33 is capable of stimulating the Th2 type immune response and cytokine production [137–139]. In contrast, sST2 acts as a decoy receptor for IL-33 and is thought to inhibit IL-33 function, thus favoring a shift towards the Th1 immune response [140–143]. Besides its regulatory properties on the type of the adaptive immune response, sST2 also plays a role in innate immunity [132,144–146]. Elevated sST2 production has been observed during inflammatory conditions, such as lipopolysaccharide (LPS)-induced inflammation [147,148] and ultraviolet light irradiation [149]. However, several studies have demonstrated that sST2 has anti-inflammatory properties [132,145,146]. This beneficial effect of sST2 is thought to be mediated by IL-10 [132]. During pregnancy, plasma sST2 concentrations were higher in women with preeclampsia than in those with uncomplicated pregnancies [150,151]. In contrast, among women with PTL, those with IAI had a lower median amniotic fluid sST2 concentration than those without IAI [152]. Interestingly, IL-33 expression was also found in macrophages of the chorioamniotic membranes in acute chorioamnionitis [153].
The objectives of this study were to: 1) determine whether umbilical cord plasma sST2 concentration differ between comparing preterm neonates with and without funisitis (the histologic counterpart of FIRS) and between those with and without FIRS (defined as umbilical cord IL-6 concentration ≥17.5 pg/mL); and 2) evaluate the relationship between sST2 and IL-10 in neonates with funisitis and/or FIRS.
Patients and methods
Study design and population
A retrospective cross-sectional study was conducted by searching the Detroit Medical Center/Wayne State University/Perinatology Research Branch (NICHD/NIH) clinical database and bank of biological samples. Sixty-six pregnant women with spontaneous preterm delivery (either PTL or preterm PROM) between 27 and 34 weeks of gestation with (n=36), and without (n=30) funisitis were included. Multiple gestations and pregnancies with fetal chromosomal and/or structural anomalies were excluded. Umbilical cord blood was collected immediately after birth. Placentas underwent histopathologic examination after delivery.
All women provided written informed consent before the collection of biological samples. The collection and utilization of the samples was approved by the IRB of Wayne State University and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NIH/DHHS). Many of these samples have been used in previous studies.
Clinical definitions
The diagnosis of PTL was made in the presence of regular uterine contractions (at least 3 in 30 minutes) and documented cervical change. Preterm PROM was diagnosed with sterile speculum examination by the combination of vaginal pooling, nitrazine and/or ferning test. Funisitis was diagnosed in the presence of neutrophil infiltration into the umbilical vessel wall or Wharton’s jelly, according to criteria previously described [58]. FIRS was defined as an umbilical cord blood IL-6 concentration ≥ 17.5 pg/mL [55,154].
Diagnosis of funisitis
Tissue sections for histopathologic evaluation included one chorioamniotic membrane roll, two full-thickness sections from the placental disc and one section of the umbilical cord. Tissues were fixed in 10% neutral buffered formalin, embedded in paraffin, and stained with hemotoxylin and eosin. Histopathologic examination was performed by a perinatal pathologist who was blinded to the clinical information.
Sample collection and determination of sST2 in umbilical cord plasma
Umbilical cord blood was collected immediately after birth into tubes containing EDTA. Blood was centrifuged at 1300 g for 10 minutes at 4°C. The samples were stored at −70 °C until analysis. Specific enzyme-linked immunoassays were used for the determination of umbilical cord plasma concentrations of sST2, IL-6 and IL-10 (R&D Systems, Minneapolis, MN, USA). The quantitative sandwich enzyme immunoassay was employed. The inter- and intra-assay coefficients of variation were: 1) sST2 4.6% and 3.9%, respectively; 2) IL-10 6.9% and 4.4%, respectively; and 3) IL-6 8.7% and 4.6%, respectively. The sensitivity was 17.5 pg/mL for sST2, 0.65 pg/mL for IL-10, and 0.09 pg/mL for IL-6.
Statistical analysis
The Shapiro-Wilk test was used to determine if the data were normally distributed. The Mann-Whitney U test was used to compare continuous non-parametric variables between groups. Comparison between proportions was performed using the Chi-square or Fisher’s exact tests. Correlation between two continuous variables was determined using Spearman’s rank correlation test. Multivariable general linear models including effect modification terms were constructed to examine whether the relationship between sST2 and IL-10 differed significantly as a function of either preterm PROM or gestational age at delivery. Plasma sST2 concentrations were log base 2 transformed to meet the assumptions of linear regression. A p value <0.05 was considered statistically significant. Analysis was performed with SPSS, version 19 (IBM Corp, Armonk, NY) and SAS version 9.3 (Cary, NC).
Results
Demographic and clinical characteristics of the study population
Demographic and clinical characteristics of the study population are presented in Table I. There were no significant differences in maternal age, gestational age at delivery, and birthweight between neonates with and without funisitis (Table I). The frequency of patients presenting with spontaneous PTL and intact membranes or preterm PROM was not significantly different between these groups (p=0.6; Table I). Similarly, when comparing neonates with and without FIRS, there were no significant differences in maternal age, gestational age at delivery, or birth weight (Table II). Neither umbilical cord plasma concentrations of sST2 nor IL-10 were correlated with gestational age at delivery (Spearman’s Rho −0.07, p=0.6 and 0.01, p=0.9, respectively). Two of 29 neonates with FIRS did not have funisitis.
Table I.
Demographic and clinical characteristics of the study population with and without funisitis.
| Without funisitis (n=30) |
With funisitis (n=36) |
p | |
|---|---|---|---|
| Maternal age (years) | 24 (19–29) | 24.5 (20–29) | 0.8 |
| GA at delivery (weeks) | 31.9 (30.5–33.4) | 31.9 (30.0–33.2) | 0.6 |
| Preterm PROM | 8 (26.7%) | 12 (33.3%) | 0.6 |
| PTL and intact membranes | 22 (73.3%) | 24 (66.7%) | 0.6 |
| FIRS | 2 (6.7%) | 27 (75%) | < 0.0001* |
| Birthweight (grams) | 1660 (1499–2127) | 1697 (1379–2090) | 0.8 |
Values are expressed as number (percent) or median (IQR).
p <0.05.
GA: gestational age; PTL: preterm labor; PROM: prelabor rupture of membranes; FIRS: fetal inflammatory response syndrome.
Table II.
Demographic and clinical characteristics of the study population with and without the fetal inflammatory response syndrome (FIRS).
| Without FIRS (n=37) |
With FIRS (n=29) |
p | |
|---|---|---|---|
| Maternal age (years) | 24 (19–29) | 24 (20–32) | 0.8 |
| GA at delivery (weeks) | 31.7 (30–33.3) | 32.1 (30–33.4) | 0.3 |
| Preterm PROM | 9 (24.3%) | 11 (37.9%) | 0.2 |
| PTL and intact membranes | 28 (75.7%) | 18 (62.1%) | 0.2 |
| Birthweight (grams) | 1625 (1307–2073) | 1745 (1502–2113) | 0.4 |
Values are expressed as number (percent) or median (IQR).
p<0.05.
FIRS: fetal inflammatory response syndrome; GA: gestational age; PTL: preterm labor; PROM: prelabor rupture of membranes.
Funisitis was associated with an increase in the umbilical cord plasma sST2 median concentration
Soluble ST2 was detected in all samples. The median umbilical cord plasma concentration of sST2 was 2.7-fold higher in neonates with funisitis than in those without funisitis (19.1 ng/mL; IQR 7.1–75.0 ng/mL vs. 7.2 ng/mL; IQR 5.9–23.1 ng/mL; p=0.008; Figure 1). IL-10 was below the detection limit of the assay in 16 patients; of these, three neonates had funisitis and none had FIRS. The median umbilical cord plasma concentration of IL-10 was also significantly greater in neonates with funisitis, than in those without funisitis (4.2 pg/mL; IQR 2.8–7.8 pg/mL vs. 1.9 pg/mL; IQR 0–2.7 pg/mL; p<0.0001).
Figure 1. Umbilical cord plasma sST2 concentrations in neonates with and without funisitis.
The median plasma concentration of sST2 in umbilical cord was greater in neonates with funisitis than in those without funisitis (median 19.1 ng/mL; IQR 7.1–75.0 ng/mL vs. median 7.2 ng/mL; IQR 5.9–23.1 ng/mL; p=0.008). The y axis is expressed as log2.
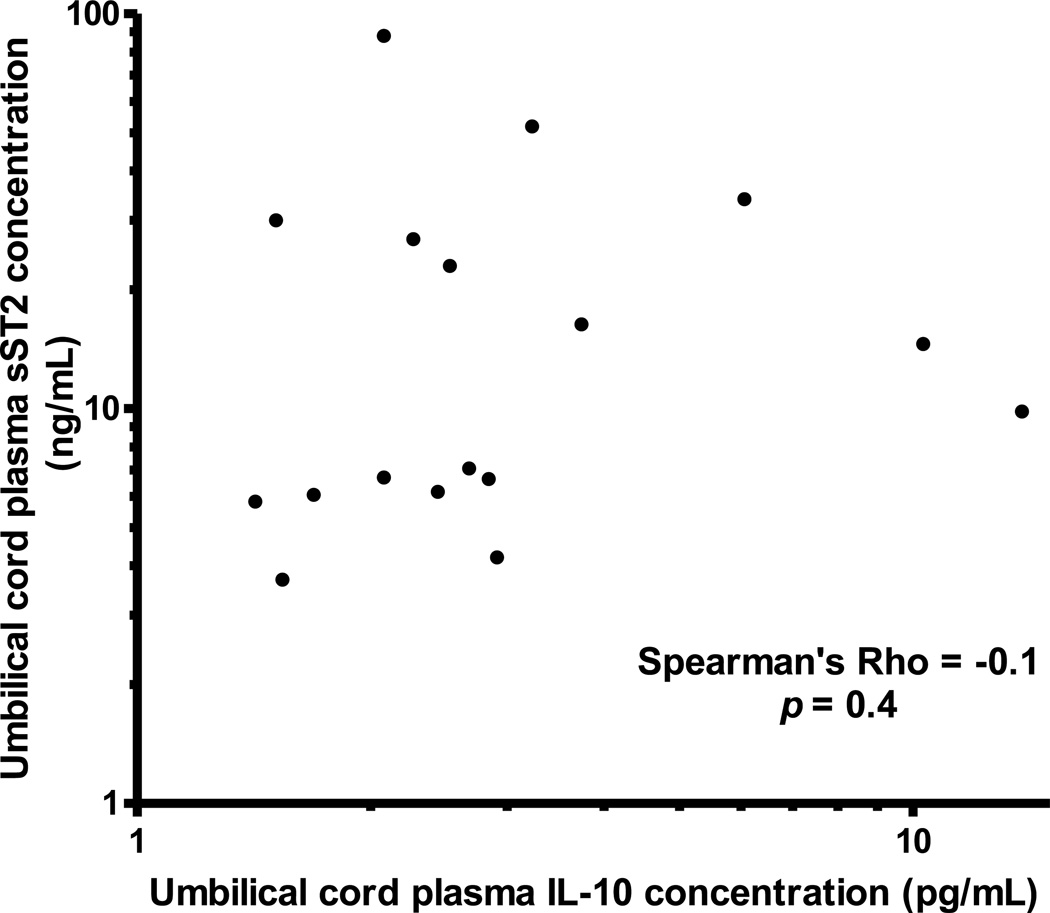
Among neonates with funisitis, there was a significant positive correlation between umbilical cord plasma concentrations of sST2 and IL-10 (Spearman’s Rho=0.7, p<0.0001; Figure 2). In contrast, there was no significant correlation between umbilical cord plasma concentrations of sST2 and IL-10 among neonates without funisitis (Spearman’s Rho=−0.1, p=0.4; Figure 3).
Figure 2. Correlation between umbilical cord plasma concentrations of sST2 and IL-10 in neonates with funisitis.
There was a significant positive correlation between umbilical cord plasma concentrations of sST2 and IL-10 (Spearman’s Rho=0.7, p<0.0001). The y and x axis are expressed as log10.
Figure 3. Correlation between umbilical cord plasma concentrations of sST2 and IL-10 in neonates without funisitis.
There was no significant correlation between umbilical cord plasma concentrations of sST2 and IL-10 (Spearman’s Rho=−0.1, p=0.4). The y and x axis are expressed as log10.
FIRS was associated with an increase in the umbilical cord plasma sST2 concentration
The median plasma concentration of sST2 in the umbilical cord was 6.7-fold higher in neonates with FIRS, than in those without FIRS (44.6 ng/mL; IQR 13.8–80.3 ng/mL vs. 6.7 ng/mL; IQR 5.6–20.1 ng/mL; p<0.0001; Figure 4). The median plasma IL-10 concentration in umbilical cord of neonates with FIRS was significantly greater than in those without FIRS (5.3 pg/mL; IQR 3.5–10.9 pg/mL vs. 2.5 pg/mL; IQR 2.1–3.6 pg/mL; p<0.0001)
Figure 4. Umbilical cord plasma sST2 concentrations in neonates with and without the fetal inflammatory response syndrome (FIRS).
The median plasma concentration of sST2 in umbilical cord was greater in neonates with FIRS than in those without FIRS (median 44.6 ng/mL; IQR 13.8–80.3 ng/mL vs. median 6.7 ng/mL; IQR 5.6–20.1 ng/mL; p<0.0001). The y axis is expressed as log2.
Among neonates with FIRS, a significant positive correlation between umbilical cord plasma concentrations of sST2 and IL-10 (Spearman’s Rho=0.7, p<0.0001) was observed. In contrast, among patients without FIRS, there was no correlation between umbilical cord plasma concentrations of sST2 and IL-10 (Spearman’s Rho=−0.2, p=0.1).
Use of a general linear models to examine whether the relation between IL-10 and sST2 differed as a function of preterm PROM revealed no evidence of effect modification, neither overall (p=0.27), in the presence of FIRS/funisitis (p=0.43), nor in the absence of FIRS/funisitis (p=0.32). Similarly, the relationship between FIRS/funisitis and sST2 did not vary as a function of preterm PROM (p=0.57).
DISCUSSION
Principal findings of the study
1) Preterm neonates with FIRS and/or funisitis had greater umbilical cord plasma concentrations of sST2 than neonates without FIRS and/or funisitis; 2) the median umbilical cord plasma sST2 concentration was 6.7-fold higher in FIRS and 2.7-fold higher in funisitis, compared to those without these conditions; and 3) there was a strong positive correlation between sST2 and IL-10 concentrations in the umbilical cord plasma in neonates with FIRS and/or funisitis, but not in neonates without these conditions.
The role of ST2 in infection/inflammation
ST2 has been intensively investigated to determine its involvement in the regulation of the Th1/Th2 adaptive immune response. Emerging evidence suggests that ST2 plays a role in regulating the innate limb of the immune response through inhibition of TLRs signaling [145,146,155]. TLRs are members of the Toll/IL-1R (TIR) superfamily, which also includes ST2 along with IL-1 and IL-18 [156]. TLR signaling can activate many genes identical to those induced by IL-1 [157], and, thus, are important for the initiation and development of the pro-inflammatory response. Nevertheless, a balance between activation and inhibition is required in order to avoid detrimental inflammation. Thus, negative regulators of TIR signaling are essential to achieve an immunological balance. Indeed, in contrast to other TIR family members which induce the inflammatory response through the activation of NF-κB, the TIR domain of the ST2 receptor activates mitogen-activated protein kinases [158]. Moreover, ST2 has been shown to sequester the adaptor proteins, myeloid differentiation primary response (MyD)88 and MyD88-adapter-like protein through its TIR domain, resulting in TLR4 down-regulation [146,155]. Similarly, another study has reported negative regulation of TLR2 by ST2, affecting the formation of TLR2-MyD88 and MyD88-IL-1R associated kinase immune-complexes [155].
There is also evidence that ST2 is an important selective negative regulator of the TIR domain containing receptor function [146]. Thus, it is not surprising that macrophages from ST2-deficient mice produce more pro-inflammatory cytokines in response to LPS or bacterial lipoprotein than wild-type mice. This leads to a sustained pro-inflammatory cytokine production by ST2 deficient macrophages [146]. On the other hand, sST2 has an inhibitory effect on pro-inflammatory cytokine production. Evidence in support of this is: 1) sST2 inhibits pro-inflammatory cytokine production from LPS-stimulated macrophages [145]; and 2) in animal models of sepsis and ischemia-reperfusion injury, the administration of sST2-Fc fusion protein suppresses the production of TNF-α, IL-6, and IL-12 [144,145], and increases survival [132].
ST2 is also involved in endotoxin tolerance [146]. Wild type mice remain healthy after priming with a sub-lethal dose of LPS, and subsequent challenging with a lethal dose of LPS; whereas ST2-deficient mice were unable to develop endotoxin tolerance, had an exaggerated inflammatory response, and died after the LPS challenge [146]. An increased susceptibility to polymicrobial infection with impaired bacterial clearance is associated with altered phagosome maturation and nitrogen oxide-2 derived production of reactive oxygen species in ST2-deficient mice [159].
Biology of IL-10
Traditionally, resolution of inflammation was thought to occur passively. However, it is now clear that resolution is an active process which consists mainly of a decreased production of pro-inflammatory components and removal of inflammatory cells. Both activation and resolution of the inflammatory response are of fundamental importance for survival. IL-10 is one of the most important anti-inflammatory cytokines, having a crucial role as a promoter of negative feedback in the inflammatory response [131,160,161]. IL-10 knock-out mice have an exaggerated Th1 immune activation in the presence of infection [162,163], and die quickly due to a massive and sustained inflammatory response [164,165]. The overproduction of IL-10 is associated with persistent infection [166–170]. Moreover, mice receiving IL-10 or transgenic mice over-expressing IL-10 have decreased production of pro-inflammatory cytokines [171,172]. IL-10 production can be stimulated by administration of pro-inflammatory cytokines such as IL-6, IL-12, IL-27, and transforming growth factor-β, which stimulate T-helper cells [173–177], or by endotoxin stimulation of macrophages and dendritic cells [178].
The anti-inflammatory action of IL-10 is elicited mainly through inhibition of pro-inflammatory cytokine synthesis through the direct effect on LPS-activated macrophages and/or down-regulation of T cells [130,131,179]. However, IL-10 also prevents the release of reactive oxygen intermediates from monocytes/macrophages [180,181]. IL-10 may also lead to down-regulation of major histocompatibility complex (MHC) class II antigens [182] and cell-adhesion molecules, such as intercellular adhesion molecule (ICAM)-1 on LPS-activated macrophages [183], resulting in the reduced production of pro-inflammatory cytokines.
The link between sST2 and IL-10
In an intestinal ischemic reperfusion model, the administration of soluble ST2-Fc fusion protein (before reperfusion) resulted in a reduced local and systemic inflammatory response (reduced neutrophil influx and cytokine production) and elevation of IL-10 concentration, leading to a reduction in the mortality rate of treated mice [132]. This protective effect of sST2 did not persist in IL-10 knock-out mice, suggesting that IL-10 is essential for the beneficial effect of sST2. The mechanisms and target cells on which sST2 exerts its action and induces IL-10 production remain to be elucidated, although T-regulatory cells [184] and direct action on macrophages have been proposed [145].
Preterm neonates with FIRS and/or funisitis have a higher median concentration of sST2 in umbilical cord plasma
We found that the median umbilical cord plasma concentration of sST2 in neonates with FIRS was 6.7-fold higher than in neonates without FIRS. Similarly, but to a lesser extent, the median umbilical cord plasma concentration of sST2 was 2.7-fold higher in neonates with funisitis than in those without funisitis. FIRS is associated with an increase in pro-inflammatory cytokines (e.g. IL-1β, TNF-α)[87], chemokine (IL-8)[54], and C-reactive protein [185] in umbilical cord blood, which may lead to short- and long-term complications in preterm neonates [21,55,57,58,67,86,87,89,185–191]. On the other hand, as confirmed by the study herein, FIRS is also associated with an increased umbilical cord plasma concentration of IL-10 [192,193]. The protective anti-inflammatory effect of IL-10 in pregnancy has been confirmed by several studies [194–198]. Elevated concentration of both sST2 and IL-10 have also been described among patients with sepsis [199]. Therefore, high plasma concentrations of sST2 and IL-10 in the umbilical cord of preterm neonates with FIRS and/or funisitis most likely reflect an anti-inflammatory host response mounted to counteract pro-inflammatory cytokines. The strong positive correlation between sST2 and IL-10 in neonates with FIRS, but not in those without FIRS, is consistent with the observation that sST2 exerts its action in cooperation with IL-10 [132,199]. On the other hand, a sustained elevation of serum sST2 concentration in septic patients is correlated with disease severity and mortality [200]. One possible explanation of this observation is that after the initial hyper-inflammatory phase, patients with sepsis can become immunosuppressed due to activation of the anti-inflammatory limb of the immune system [201–203]. Loss of delayed hypersensitivity, inability to clear infection, and predisposition to nosocomial infections can often be observed in these patients [203].
Strengths and limitations of the study
This is the first study to report the changes in umbilical cord plasma concentrations of sST2 and IL-10 in neonates with FIRS and/or funisitis. The diagnosis of FIRS was defined stringently by the IL-6 concentration in umbilical cord plasma. However, a limited sample size precluded analysis of an association between umbilical cord plasma sST2 concentration and adverse neonatal outcome. The cross-sectional nature of this study also precludes a clear determination of the temporal relationship between observed sST2 concentrations and the occurrence of FIRS and/or funisits.
Conclusions
The fetal inflammatory response syndrome is associated with an elevation of umbilical cord plasma concentrations of soluble ST2. This protein may represent an important mediator of the immune response in neonates diagnosed with this condition by promoting an anti-inflammatory response in cooperation with IL-10. Future studies examining the association between neonatal plasma sST2 concentration and adverse neonatal outcomes appear warranted.
Acknowledgments
Declaration of Interest
This project has been funded in whole or in part with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services, under Contract No. HHSN275201300006C.
References
- 1.Romero R, Sirtori M, Oyarzun E, Avila C, Mazor M, Callahan R, Sabo V, et al. Infection and labor. V. Prevalence, microbiology, and clinical significance of intraamniotic infection in women with preterm labor and intact membranes. Am J Obstet Gynecol. 1989;161:817–824. doi: 10.1016/0002-9378(89)90409-2. [DOI] [PubMed] [Google Scholar]
- 2.Romero R, Mazor M, Wu YK, Sirtori M, Oyarzun E, Mitchell MD, Hobbins JC. Infection in the pathogenesis of preterm labor. Semin Perinatol. 1988;12:262–279. [PubMed] [Google Scholar]
- 3.Cherouny PH, Pankuch GA, Romero R, Botti JJ, Kuhn DC, Demers LM, Appelbaum PC. Neutrophil attractant/activating peptide-1/interleukin-8: association with histologic chorioamnionitis, preterm delivery, and bioactive amniotic fluid leukoattractants. Am J Obstet Gynecol. 1993;169:1299–1303. doi: 10.1016/0002-9378(93)90297-v. [DOI] [PubMed] [Google Scholar]
- 4.Romero R, Gomez R, Chaiworapongsa T, Conoscenti G, Kim JC, Kim YM. The role of infection in preterm labour and delivery. Paediatric and perinatal epidemiology. 2001;15(Suppl 2):41–56. doi: 10.1046/j.1365-3016.2001.00007.x. [DOI] [PubMed] [Google Scholar]
- 5.Romero R, Brody DT, Oyarzun E, Mazor M, Wu YK, Hobbins JC, Durum SK. Infection and labor. III. Interleukin-1: a signal for the onset of parturition. Am J Obstet Gynecol. 1989;160:1117–1123. doi: 10.1016/0002-9378(89)90172-5. [DOI] [PubMed] [Google Scholar]
- 6.Newton ER. Preterm labor, preterm premature rupture of membranes, and chorioamnionitis. Clin Perinatol. 2005;32:571–600. doi: 10.1016/j.clp.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Romero R, Avila C, Santhanam U, Sehgal PB. Amniotic fluid interleukin 6 in preterm labor. Association with infection. J Clin Invest. 1990;85:1392–1400. doi: 10.1172/JCI114583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romero R, Sepulveda W, Kenney JS, Archer LE, Allison AC, Sehgal PB. Interleukin 6 determination in the detection of microbial invasion of the amniotic cavity. Ciba Found Symp. 1992;167:205–220. doi: 10.1002/9780470514269.ch13. discussion 220–203. [DOI] [PubMed] [Google Scholar]
- 9.Romero R, Manogue KR, Mitchell MD, Wu YK, Oyarzun E, Hobbins JC, Cerami A. Infection and labor. IV. Cachectin-tumor necrosis factor in the amniotic fluid of women with intraamniotic infection and preterm labor. Am J Obstet Gynecol. 1989;161:336–341. doi: 10.1016/0002-9378(89)90515-2. [DOI] [PubMed] [Google Scholar]
- 10.Bobitt JR, Hayslip CC, Damato JD. Amniotic fluid infection as determined by transabdominal amniocentesis in patients with intact membranes in premature labor. American journal of obstetrics and gynecology. 1981;140:947–952. doi: 10.1016/0002-9378(81)90090-9. [DOI] [PubMed] [Google Scholar]
- 11.Hameed C, Tejani N, Verma UL, Archbald F. Silent chorioamnionitis as a cause of preterm labor refractory to tocolytic therapy. American journal of obstetrics and gynecology. 1984;149:726–730. doi: 10.1016/0002-9378(84)90111-x. [DOI] [PubMed] [Google Scholar]
- 12.Wahbeh CJ, Hill GB, Eden RD, Gall SA. Intra-amniotic bacterial colonization in premature labor. American journal of obstetrics and gynecology. 1984;148:739–743. doi: 10.1016/0002-9378(84)90558-1. [DOI] [PubMed] [Google Scholar]
- 13.Leigh J, Garite TJ. Amniocentesis and the management of premature labor. Obstetrics and gynecology. 1986;67:500–506. [PubMed] [Google Scholar]
- 14.Gravett MG, Hummel D, Eschenbach DA, Holmes KK. Preterm labor associated with subclinical amniotic fluid infection and with bacterial vaginosis. Obstetrics and gynecology. 1986;67:229–237. doi: 10.1097/00006250-198602000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Skoll MA, Moretti ML, Sibai BM. The incidence of positive amniotic fluid cultures in patients preterm labor with intact membranes. American journal of obstetrics and gynecology. 1989;161:813–816. doi: 10.1016/0002-9378(89)90407-9. [DOI] [PubMed] [Google Scholar]
- 16.Watts DH, Krohn MA, Hillier SL, Eschenbach DA. The association of occult amniotic fluid infection with gestational age and neonatal outcome among women in preterm labor. Obstetrics and gynecology. 1992;79:351–357. doi: 10.1097/00006250-199203000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Romero R, Yoon BH, Mazor M, Gomez R, Diamond MP, Kenney JS, Ramirez M, et al. The diagnostic and prognostic value of amniotic fluid white blood cell count, glucose, interleukin-6, and gram stain in patients with preterm labor and intact membranes. American journal of obstetrics and gynecology. 1993;169:805–816. doi: 10.1016/0002-9378(93)90009-8. [DOI] [PubMed] [Google Scholar]
- 18.Coultrip LL, Lien JM, Gomez R, Kapernick P, Khoury A, Grossman JH. The value of amniotic fluid interleukin-6 determination in patients with preterm labor and intact membranes in the detection of microbial invasion of the amniotic cavity. American journal of obstetrics and gynecology. 1994;171:901–911. doi: 10.1016/s0002-9378(94)70057-5. [DOI] [PubMed] [Google Scholar]
- 19.Yoon BH, Yang SH, Jun JK, Park KH, Kim CJ, Romero R. Maternal blood C-reactive protein, white blood cell count, and temperature in preterm labor: a comparison with amniotic fluid white blood cell count. Obstetrics and gynecology. 1996;87:231–237. doi: 10.1016/0029-7844(95)00380-0. [DOI] [PubMed] [Google Scholar]
- 20.Markenson GR, Martin RK, Tillotson-Criss M, Foley KS, Stewart RS, Jr, Yancey M. The use of the polymerase chain reaction to detect bacteria in amniotic fluid in pregnancies complicated by preterm labor. American journal of obstetrics and gynecology. 1997;177:1471–1477. doi: 10.1016/s0002-9378(97)70093-0. [DOI] [PubMed] [Google Scholar]
- 21.Gomez R, Romero R, Ghezzi F, Yoon BH, Mazor M, Berry SM. The fetal inflammatory response syndrome. Am J Obstet Gynecol. 1998;179:194–202. doi: 10.1016/s0002-9378(98)70272-8. [DOI] [PubMed] [Google Scholar]
- 22.Kara M, Ozden S, Arioglu P, Cetin A. The significance of amniotic fluid interleukin-6 levels in preterm labour. The Australian & New Zealand journal of obstetrics & gynaecology. 1998;38:403–406. doi: 10.1111/j.1479-828x.1998.tb03097.x. [DOI] [PubMed] [Google Scholar]
- 23.Greci LS, Gilson GJ, Nevils B, Izquierdo LA, Qualls CR, Curet LB. Is amniotic fluid analysis the key to preterm labor? A model using interleukin-6 for predicting rapid delivery. American journal of obstetrics and gynecology. 1998;179:172–178. doi: 10.1016/s0002-9378(98)70269-8. [DOI] [PubMed] [Google Scholar]
- 24.Yoon BH, Chang JW, Romero R. Isolation of Ureaplasma urealyticum from the amniotic cavity and adverse outcome in preterm labor. Obstetrics and gynecology. 1998;92:77–82. doi: 10.1016/s0029-7844(98)00122-7. [DOI] [PubMed] [Google Scholar]
- 25.Gonzalez-Bosquet E, Cerqueira MJ, Dominguez C, Gasser I, Bermejo B, Cabero L. Amniotic fluid glucose and cytokines values in the early diagnosis of amniotic infection in patients with preterm labor and intact membranes. The Journal of maternal-fetal medicine. 1999;8:155–158. doi: 10.1002/(SICI)1520-6661(199907/08)8:4<155::AID-MFM3>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 26.Locksmith GJ, Clark P, Duff P, Schultz GS. Amniotic fluid matrix metalloproteinase-9 levels in women with preterm labor and suspected intra-amniotic infection. Obstetrics and gynecology. 1999;94:1–6. doi: 10.1016/s0029-7844(99)00011-3. [DOI] [PubMed] [Google Scholar]
- 27.Rizzo G, Capponi A, Vlachopoulou A, Angelini E, Grassi C, Romanini C. Ultrasonographic assessment of the uterine cervix and interleukin-8 concentrations in cervical secretions predict intrauterine infection in patients with preterm labor and intact membranes. Ultrasound Obstet Gynecol. 1998;12:86–92. doi: 10.1046/j.1469-0705.1998.12020086.x. [DOI] [PubMed] [Google Scholar]
- 28.Romero R, Quintero R, Oyarzun E, Wu YK, Sabo V, Mazor M, Hobbins JC. Intraamniotic infection and the onset of labor in preterm premature rupture of the membranes. Am J Obstet Gynecol. 1988;159:661–666. doi: 10.1016/s0002-9378(88)80030-9. [DOI] [PubMed] [Google Scholar]
- 29.Cotton DB, Hill LM, Strassner HT, Platt LD, Ledger WJ. Use of amniocentesis in preterm gestation with ruptured membranes. Obstetrics and gynecology. 1984;63:38–43. [PubMed] [Google Scholar]
- 30.Broekhuizen FF, Gilman M, Hamilton PR. Amniocentesis for gram stain and culture in preterm premature rupture of the membranes. Obstetrics and gynecology. 1985;66:316–321. [PubMed] [Google Scholar]
- 31.Vintzileos AM, Campbell WA, Nochimson DJ, Weinbaum PJ, Escoto DT, Mirochnick MH. Qualitative amniotic fluid volume versus amniocentesis in predicting infection in preterm premature rupture of the membranes. Obstetrics and gynecology. 1986;67:579–583. [PubMed] [Google Scholar]
- 32.Feinstein SJ, Vintzileos AM, Lodeiro JG, Campbell WA, Weinbaum PJ, Nochimson DJ. Amniocentesis with premature rupture of membranes. Obstetrics and gynecology. 1986;68:147–152. [PubMed] [Google Scholar]
- 33.Garite TJ, Freeman RK, Linzey EM, Braly P. The use of amniocentesis in patients with premature rupture of membranes. Obstetrics and gynecology. 1979;54:226–230. [PubMed] [Google Scholar]
- 34.Gauthier DW, Meyer WJ. Comparison of gram stain, leukocyte esterase activity, and amniotic fluid glucose concentration in predicting amniotic fluid culture results in preterm premature rupture of membranes. American journal of obstetrics and gynecology. 1992;167:1092–1095. doi: 10.1016/s0002-9378(12)80044-5. [DOI] [PubMed] [Google Scholar]
- 35.Romero R, Yoon BH, Mazor M, Gomez R, Gonzalez R, Diamond MP, Baumann P, et al. A comparative study of the diagnostic performance of amniotic fluid glucose, white blood cell count, interleukin-6, and gram stain in the detection of microbial invasion in patients with preterm premature rupture of membranes. American journal of obstetrics and gynecology. 1993;169:839–851. doi: 10.1016/0002-9378(93)90014-a. [DOI] [PubMed] [Google Scholar]
- 36.Font GE, Gauthier DW, Meyer WJ, Myles TD, Janda W, Bieniarz A. Catalase activity as a predictor of amniotic fluid culture results in preterm labor or premature rupture of membranes. Obstetrics and gynecology. 1995;85:656–658. doi: 10.1016/0029-7844(95)00026-n. [DOI] [PubMed] [Google Scholar]
- 37.Hussey MJ, Levy ES, Pombar X, Meyer P, Strassner HT. Evaluating rapid diagnostic tests of intra-amniotic infection: Gram stain, amniotic fluid glucose level, and amniotic fluid to serum glucose level ratio. American journal of obstetrics and gynecology. 1998;179:650–656. doi: 10.1016/s0002-9378(98)70059-6. [DOI] [PubMed] [Google Scholar]
- 38.Yoon BH, Romero R, Kim M, Kim EC, Kim T, Park JS, Jun JK. Clinical implications of detection of Ureaplasma urealyticum in the amniotic cavity with the polymerase chain reaction. American journal of obstetrics and gynecology. 2000;183:1130–1137. doi: 10.1067/mob.2000.109036. [DOI] [PubMed] [Google Scholar]
- 39.Gomez R, Romero R, Nien JK, et al. A short cervix in women with preterm labor and intact membranes: a risk factor for microbial invasion fo the amniotic cavity. Am J Obstet Gynecol. 2005;192:678–689. doi: 10.1016/j.ajog.2004.10.624. [DOI] [PubMed] [Google Scholar]
- 40.Hassan SS, Romero R, Hendler I, et al. A sonographic short cervix as the only clinical manifestation of intra-amniotic infection. J Perinat Med. 2006;34:13–19. doi: 10.1515/JPM.2006.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vaisbuch E, Romero R, Mazaki-Tovi S, Erez O, Kusanovic JP, Mittal P, Gotsch F, et al. The risk of impending preterm delivery in asymptomatic patients with a nonmeasurable cervical length in the second trimester. American journal of obstetrics and gynecology. 2010;203:446 e441–446 e449. doi: 10.1016/j.ajog.2010.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vaisbuch E, Hassan SS, Mazaki-Tovi S, Nhan-Chang CL, Kusanovic JP, Chaiworapongsa T, Dong Z, et al. Patients with an asymptomatic short cervix (<or=15 mm) have a high rate of subclinical intraamniotic inflammation: implications for patient counseling. American journal of obstetrics and gynecology. 2010;202:433 e431–433 e438. doi: 10.1016/j.ajog.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Romero R, Gonzalez R, Sepulveda W, Brandt F, Ramirez M, Sorokin Y, Mazor M, et al. Infection and labor. VIII. Microbial invasion of the amniotic cavity in patients with suspected cervical incompetence: prevalence and clinical significance. American journal of obstetrics and gynecology. 1992;167:1086–1091. doi: 10.1016/s0002-9378(12)80043-3. [DOI] [PubMed] [Google Scholar]
- 44.Lee SE, Romero R, Park CW, Jun JK, Yoon BH. The frequency and significance of intraamniotic inflammation in patients with cervical insufficiency. Am J Obstet Gynecol. 2008;198:633 e631–633 e638. doi: 10.1016/j.ajog.2007.11.047. [DOI] [PubMed] [Google Scholar]
- 45.Kim SK, Romero R, Kusanovic JP, Erez O, Vaisbuch E, Mazaki-Tovi S, Gotsch F, et al. The prognosis of pregnancy conceived despite the presence of an intrauterine device (IUD) Journal of perinatal medicine. 2010;38:45–53. doi: 10.1515/JPM.2009.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gomez R, Romero R, Nien JK, Medina L, Carstens M, Kim YM, Chaiworapongsa T, et al. Idiopathic vaginal bleeding during pregnancy as the only clinical manifestation of intrauterine infection. J Matern Fetal Neonatal Med. 2005;18:31–37. doi: 10.1080/14767050500217863. [DOI] [PubMed] [Google Scholar]
- 47.Madan I, Romero R, Kusanovic JP, Mittal P, Chaiworapongsa T, Dong Z, Mazaki-Tovi S, et al. The frequency and clinical significance of intra-amniotic infection and/or inflammation in women with placenta previa and vaginal bleeding: an unexpected observation. J Perinat Med. 2010;38:275–279. doi: 10.1515/JPM.2010.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carroll SG, Papaioannou S, Ntumazah IL, Philpott-Howard J, Nicolaides KH. Lower genital tract swabs in the prediction of intrauterine infection in preterm prelabour rupture of the membranes. British journal of obstetrics and gynaecology. 1996;103:54–59. doi: 10.1111/j.1471-0528.1996.tb09515.x. [DOI] [PubMed] [Google Scholar]
- 49.Ferrazzi E, Muggiasca ML, Fabbri E, Fontana P, Castoldi F, Lista G, Primerano L, et al. Assessment of fetal inflammatory syndrome by "classical" markers in the management of preterm labor: a possible lesson from metabolomics and system biology. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2012;25:54–61. doi: 10.3109/14767058.2012.716984. [DOI] [PubMed] [Google Scholar]
- 50.Novy MJ, Duffy L, Axthelm MK, et al. Ureaplasma parvum or Mycoplasma hominis as sole pathogens cause chorioamnionitis, preterm delivery, and fetal pneumonia in rhesus macaques. Reprod Sci. 2009;16:56–70. doi: 10.1177/1933719108325508. [DOI] [PubMed] [Google Scholar]
- 51.Carroll SG, Papioannou S, Ntumazah IL, Philpott-Howard J, Nicholaides KH. Lower genital tract swabs in the prediction of intrauterine infection in preerm prelabour rupture of membranes. Br J Obstet Gynaecol. 1996;103:54–59. doi: 10.1111/j.1471-0528.1996.tb09515.x. [DOI] [PubMed] [Google Scholar]
- 52.Goldenberg RL, Andrews WW, Goepfert AR, Faye-Peterson O, Cliver SP, Carlo WA, Hauth JC. The Alabama Pretrm Birth Study: umbilical cord Ureaplasma urealyticum and Mycoplasma hominis cultures in very preterm newborn infants. Am J Obstet Gynecol. 2008;198:43.e1–43.e5. doi: 10.1016/j.ajog.2007.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Romero R, Garite TJ. Twenty percent of very preterm neonates (23–32 weeks of gestation) are born with bacteremia caused by genital Mycoplasmas. American journal of obstetrics and gynecology. 2008;198:1–3. doi: 10.1016/j.ajog.2007.11.031. [DOI] [PubMed] [Google Scholar]
- 54.Gotsch F, Romero R, Kusanovic JP, Mazaki-Tovi S, Pineles BL, Erez O, Espinoza J, Hassan SS. The fetal inflammatory response syndrome. Clin Obstet Gynecol. 2007;50:652–683. doi: 10.1097/GRF.0b013e31811ebef6. [DOI] [PubMed] [Google Scholar]
- 55.Yoon BH, Romero R, Park JS, Kim M, Oh SY, Kim CJ, Jun JK. The relationship among inflammatory lesions of the umbilical cord (funisitis), umbilical cord plasma interleukin 6 concentration, amniotic fluid infection, and neonatal sepsis. Am J Obstet Gynecol. 2000;183:1124–1129. doi: 10.1067/mob.2000.109035. [DOI] [PubMed] [Google Scholar]
- 56.Murthy V, Kennea NL. Antenatal infection/inflammation and fetal tissue injury. Best Pract Res Clin Obstet Gynaecol. 2007;21:479–489. doi: 10.1016/j.bpobgyn.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 57.Kim CJ, Yoon BH, Park SS, Kim MH, Chi JG. Acute funisitis of preterm but not term placentas is associated with severe fetal inflammatory response. Hum Pathol. 2001;32:623–629. doi: 10.1053/hupa.2001.24992. [DOI] [PubMed] [Google Scholar]
- 58.Pacora P, Chaiworapongsa T, Maymon E, Kim YM, Gomez R, Yoon BH, Ghezzi F, et al. Funisitis and chorionic vasculitis: the histological counterpart of the fetal inflammatory response syndrome. J Matern Fetal Neonatal Med. 2002;11:18–25. doi: 10.1080/jmf.11.1.18.25. [DOI] [PubMed] [Google Scholar]
- 59.Romero R, Gomez R, Ghezzi F, Yoon BH, Mazor M, Edwin SS, Berry SM. A fetal systemic inflammatory response is followed by the spontaneous onset of preterm parturition. Am J Obstet Gynecol. 1998;179:186–193. doi: 10.1016/s0002-9378(98)70271-6. [DOI] [PubMed] [Google Scholar]
- 60.Arad I, Ergaz Z. The fetal inflammatory response syndrome and associated infant morbidity. Isr Med Assoc J. 2004;6:766–769. [PubMed] [Google Scholar]
- 61.Kim YM, Romero R, Chaiworapongsa T, Espinoza J, Mor G, Kim CJ. Dermatitis as a component of the fetal inflammatory response syndrome is associated with activation of Toll-like receptors in epidermal keratinocytes. Histopathology. 2006;49:506–514. doi: 10.1111/j.1365-2559.2006.02542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang L, Saito M, Jobe A, Kallapur SG, Newnham JP, Cox T, Kramer B, et al. Intra-Amniotic Administration of E coli Lipopolysaccharides Causes Sustained Inflammation of the Fetal Skin in Sheep. Reprod Sci. 2012;19:1181–1189. doi: 10.1177/1933719112446079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kemp MW, Saito M, Kallapur SG, Jobe AH, Keelan JA, Li S, Kramer B, et al. Inflammation of the fetal ovine skin following in utero exposure to Ureaplasma parvum. Reprod Sci. 2011;18:1128–1137. doi: 10.1177/1933719111408114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Romero R, Espinoza J, Goncalves LF, Gomez R, Medina L, Silva M, Chaiworapongsa T, et al. Fetal cardiac dysfunction in preterm premature rupture of membranes. J Matern Fetal Neonatal Med. 2004;16:146–157. doi: 10.1080/14767050400009279. [DOI] [PubMed] [Google Scholar]
- 65.Letti Muller AL, Barrios Pde M, Kliemann LM, Valerio EG, Gasnier R, Magalhaes JA. Tei index to assess fetal cardiac performance in fetuses at risk for fetal inflammatory response syndrome. Ultrasound Obstet Gynecol. 2010;36:26–31. doi: 10.1002/uog.7584. [DOI] [PubMed] [Google Scholar]
- 66.Yanowitz TD, Jordan JA, Gilmour CH, Towbin R, Bowen A, Roberts JM, Brozanski BS. Hemodynamic disturbances in premature infants born after chorioamnionitis: association with cord blood cytokine concentrations. Pediatric research. 2002;51:310–316. doi: 10.1203/00006450-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 67.Yoon BH, Romero R, Kim KS, Park JS, Ki SH, Kim BI, Jun JK. A systemic fetal inflammatory response and the development of bronchopulmonary dysplasia. Am J Obstet Gynecol. 1999;181:773–779. doi: 10.1016/s0002-9378(99)70299-1. [DOI] [PubMed] [Google Scholar]
- 68.Mittendorf R, Covert R, Montag AG, elMasri W, Muraskas J, Lee KS, Pryde PG. Special relationships between fetal inflammatory response syndrome and bronchopulmonary dysplasia in neonates. J Perinat Med. 2005;33:428–434. doi: 10.1515/JPM.2005.076. [DOI] [PubMed] [Google Scholar]
- 69.Speer CP. New insights into the pathogenesis of pulmonary inflammation in preterm infants. Biology of the neonate. 2001;79:205–209. doi: 10.1159/000047092. [DOI] [PubMed] [Google Scholar]
- 70.Watterberg KL, Demers LM, Scott SM, Murphy S. Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics. 1996;97:210–215. [PubMed] [Google Scholar]
- 71.Jobe AH. Antenatal associations with lung maturation and infection. Journal of perinatology : official journal of the California Perinatal Association. 2005;25(Suppl 2):S31–S35. doi: 10.1038/sj.jp.7211317. [DOI] [PubMed] [Google Scholar]
- 72.Ghezzi F, Gomez R, Romero R, Yoon BH, Edwin SS, David C, Janisse J, Mazor M. Elevated interleukin-8 concentrations in amniotic fluid of mothers whose neonates subsequently develop bronchopulmonary dysplasia. European journal of obstetrics, gynecology, and reproductive biology. 1998;78:5–10. doi: 10.1016/s0301-2115(97)00236-4. [DOI] [PubMed] [Google Scholar]
- 73.Jobe AH, Newnham JP, Willet KE, Sly P, Ervin MG, Bachurski C, Possmayer F, et al. Effects of antenatal endotoxin and glucocorticoids on the lungs of preterm lambs. American journal of obstetrics and gynecology. 2000;182:401–408. doi: 10.1016/s0002-9378(00)70231-6. [DOI] [PubMed] [Google Scholar]
- 74.Bry K, Lappalainen U, Hallman M. Intraamniotic interleukin-1 accelerates surfactant protein synthesis in fetal rabbits and improves lung stability after premature birth. The Journal of clinical investigation. 1997;99:2992–2999. doi: 10.1172/JCI119494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sood BG, Madan A, Saha S, Schendel D, Thorsen P, Skogstrand K, Hougaard D, et al. Perinatal systemic inflammatory response syndrome and retinopathy of prematurity. Pediatric research. 2010;67:394–400. doi: 10.1203/PDR.0b013e3181d01a36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yoon BH, Kim YA, Romero R, Kim JC, Park KH, Kim MH, Park JS. Association of oligohydramnios in women with preterm premature rupture of membranes with an inflammatory response in fetal, amniotic, and maternal compartments. Am J Obstet Gynecol. 1999;181:784–788. doi: 10.1016/s0002-9378(99)70301-7. [DOI] [PubMed] [Google Scholar]
- 77.Yoon BH, Romero R, Jun JK, Maymon E, Gomez R, Mazor M, Park JS. An increase in fetal plasma cortisol but not dehydroepiandrosterone sulfate is followed by the onset of preterm labor in patients with preterm premature rupture of the membranes. Am J Obstet Gynecol. 1998;179:1107–1114. doi: 10.1016/s0002-9378(98)70114-0. [DOI] [PubMed] [Google Scholar]
- 78.Romero R, Savasan ZA, Chaiworapongsa T, Berry SM, Kusanovic JP, Hassan SS, Yoon BH, et al. Hematologic profile of the fetus with systemic inflammatory response syndrome. J Perinat Med. 2011;40:19–32. doi: 10.1515/JPM.2011.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Berry SM, Romero R, Gomez R, Puder KS, Ghezzi F, Cotton DB, Bianchi DW. Premature parturition is characterized by in utero activation of the fetal immune system. Am J Obstet Gynecol. 1995;173:1315–1320. doi: 10.1016/0002-9378(95)91378-5. [DOI] [PubMed] [Google Scholar]
- 80.Chaiworapongsa T, Romero R, Berry SM, Hassan SS, Yoon BH, Edwin S, Mazor M. The role of granulocyte colony-stimulating factor in the neutrophilia observed in the fetal inflammatory response syndrome. J Perinat Med. 2011;39:653–666. doi: 10.1515/JPM.2011.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.De Felice C, Toti P, Santopietro R, Stumpo M, Pecciarini L, Bagnoli F. Small thymus in very low birth weight infants born to mothers with subclinical chorioamnionitis. The Journal of pediatrics. 1999;135:384–386. doi: 10.1016/s0022-3476(99)70140-x. [DOI] [PubMed] [Google Scholar]
- 82.Toti P, De Felice C, Stumpo M, Schurfeld K, Di Leo L, Vatti R, Bianciardi G, et al. Acute thymic involution in fetuses and neonates with chorioamnionitis. Human pathology. 2000;31:1121–1128. doi: 10.1053/hupa.2000.16676. [DOI] [PubMed] [Google Scholar]
- 83.Di Naro E, Cromi A, Ghezzi F, Raio L, Uccella S, D'Addario V, Loverro G. Fetal thymic involution: a sonographic marker of the fetal inflammatory response syndrome. American journal of obstetrics and gynecology. 2006;194:153–159. doi: 10.1016/j.ajog.2005.05.036. [DOI] [PubMed] [Google Scholar]
- 84.Yoon BH, Romero R, Park JS, Kim CJ, Kim SH, Choi JH, Han TR. Fetal exposure to an intra-amniotic inflammation and the development of cerebral palsy at the age of three years. Am J Obstet Gynecol. 2000;182:675–681. doi: 10.1067/mob.2000.104207. [DOI] [PubMed] [Google Scholar]
- 85.Andrews WW, Cliver SP, Biasini F, Peralta-Carcelen AM, Rector R, Alriksson-Schmidt AI, Faye-Petersen O, et al. Early preterm birth: association between in utero exposure to acute inflammation and severe neurodevelopmental disability at 6 years of age. Am J Obstet Gynecol. 2008;198:466.e1–466.e11. doi: 10.1016/j.ajog.2007.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mittendorf R, Montag AG, MacMillan W, Janeczek S, Pryde PG, Besinger RE, Gianopoulos JG, Roizen N. Components of the systemic fetal inflammatory response syndrome as predictors of impaired neurologic outcomes in children. Am J Obstet Gynecol. 2003;188:1438–1434. doi: 10.1067/mob.2003.380. discussion 1438–44. [DOI] [PubMed] [Google Scholar]
- 87.Yoon BH, Romero R, Yang SH, Jun JK, Kim IO, Choi JH, Syn HC. Interleukin-6 concentrations in umbilical cord plasma are elevated in neonates with white matter lesions associated with periventricular leukomalacia. Am J Obstet Gynecol. 1996;174:1433–1440. doi: 10.1016/s0002-9378(96)70585-9. [DOI] [PubMed] [Google Scholar]
- 88.Dammann O, Leviton A. Maternal intrauterine infection, cytokines, and brain damage in the preterm newborn. Pediatr Res. 1997;42:1–8. doi: 10.1203/00006450-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 89.Leviton A, Paneth N, Reuss ML, Susser M, Allred EN, Dammann O, Kuban K, et al. Maternal infection, fetal inflammatory response, and brain damage in very low birth weight infants. Developmental Epidemiology Network Investigators. Pediatr Res. 1999;46:566–575. doi: 10.1203/00006450-199911000-00013. [DOI] [PubMed] [Google Scholar]
- 90.Patrick LA, Smith GN. Proinflammatory cytokines: a link between chorioamnionitis and fetal brain injury. J Obstet Gynaecol Can. 2002;24:705–709. doi: 10.1016/s1701-2163(16)30325-5. [DOI] [PubMed] [Google Scholar]
- 91.Hagberg H, Mallard C, Jacobsson B. Role of cytokines in preterm labour and brain injury. BJOG. 2005;112(Suppl 1):16–18. doi: 10.1111/j.1471-0528.2005.00578.x. [DOI] [PubMed] [Google Scholar]
- 92.Bashiri A, Burstein E, Mazor M. Cerebral palsy and fetal inflammatory response syndrome: a review. J Perinat Med. 2006;34:5–12. doi: 10.1515/JPM.2006.001. [DOI] [PubMed] [Google Scholar]
- 93.Yoon BH, Park CW, Chaiworapongsa T. Intrauterine infection and the development of cerebral palsy. BJOG. 2003;110(Suppl 20):124–127. doi: 10.1016/s1470-0328(03)00063-6. [DOI] [PubMed] [Google Scholar]
- 94.Elovitz MA, Brown AG, Breen K, Anton L, Maubert M, Burd I. Intrauterine inflammation, insufficient to induce parturition, still evokes fetal and neonatal brain injury. Int J Dev Neurosci. 2011;29:663–671. doi: 10.1016/j.ijdevneu.2011.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Moon JB, Kim JC, Yoon BH, Romero R, Kim G, Oh SY, Kim M, Shim SS. Amniotic fluid matrix metalloproteinase-8 and the development of cerebral palsy. J Perinat Med. 2002;30:301–306. doi: 10.1515/JPM.2002.044. [DOI] [PubMed] [Google Scholar]
- 96.Yoon BH, Jun JK, Romero R, Park KH, Gomez R, Choi JH, Kim IO. Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1beta, and tumor necrosis factor-alpha), neonatal brain white matter lesions, and cerebral palsy. Am J Obstet Gynecol. 1997;177:19–26. doi: 10.1016/s0002-9378(97)70432-0. [DOI] [PubMed] [Google Scholar]
- 97.Yoon BH, Romero R, Kim CJ, Koo JN, Choe G, Syn HC, Chi JG. High expression of tumor necrosis factor-alpha and interleukin-6 in periventricular leukomalacia. Am J Obstet Gynecol. 1997;177:406–411. doi: 10.1016/s0002-9378(97)70206-0. [DOI] [PubMed] [Google Scholar]
- 98.Gabrielli L, Bonasoni MP, Lazzarotto T, Lega S, Santini D, Foschini MP, Guerra B, et al. Histological findings in foetuses congenitally infected by cytomegalovirus. J Clin Virol. 2009;46(Suppl 4):S16–S21. doi: 10.1016/j.jcv.2009.09.026. [DOI] [PubMed] [Google Scholar]
- 99.Cardenas I, Mor G, Aldo P, Lang SM, Stabach P, Sharp A, Romero R, et al. Placental viral infection sensitizes to endotoxin-induced pre-term labor: a double hit hypothesis. Am J Reprod Immunol. 2011;65:110–117. doi: 10.1111/j.1600-0897.2010.00908.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cardenas I, Means RE, Aldo P, Koga K, Lang SM, Booth CJ, Manzur A, et al. Viral infection of the placenta leads to fetal inflammation and sensitization to bacterial products predisposing to preterm labor. J Immunol. 2010;185:1248–1257. doi: 10.4049/jimmunol.1000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.McCarthy M, Auger D, Whittemore SR. Human cytomegalovirus causes productive infection and neuronal injury in differentiating fetal human central nervous system neuroepithelial precursor cells. J Hum Virol. 2000;3:215–228. [PubMed] [Google Scholar]
- 102.Von Herzen JL, Benirschke K. Unexpected disseminated herpes simplex infection in a newborn. Obstet Gynecol. 1977;50:728–730. [PubMed] [Google Scholar]
- 103.Hyde SR, Giacoia GP. Congenital herpes infection: placental and umbilical cord findings. Obstet Gynecol. 1993;81:852–855. [PubMed] [Google Scholar]
- 104.Heifetz SA, Bauman M. Necrotizing funisitis and herpes simplex infection of placental and decidual tissues: study of four cases. Hum Pathol. 1994;25:715–722. doi: 10.1016/0046-8177(94)90306-9. [DOI] [PubMed] [Google Scholar]
- 105.Vaisbuch E, Romero R, Gomez R, Kusanovic JP, Mazaki-Tovi S, Chaiworapongsa T, Hassan SS. An elevated fetal interleukin-6 concentration can be observed in fetuses with anemia due to Rh alloimmunization: implications for the understanding of the fetal inflammatory response syndrome. J Matern Fetal Neonatal Med. 2011;24:391–396. doi: 10.3109/14767058.2010.507294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bhatia M, He M, Zhang H, Moochhala S. Sepsis as a model of SIRS. Front Biosci. 2009;14:4703–4711. doi: 10.2741/3561. [DOI] [PubMed] [Google Scholar]
- 107.Lenz A, Franklin GA, Cheadle WG. Systemic inflammation after trauma. Injury. 2007;38:1336–1345. doi: 10.1016/j.injury.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 108.Carden DL, Granger DN. Pathophysiology of ischaemia-reperfusion injury. J Pathol. 2000;190:255–266. doi: 10.1002/(SICI)1096-9896(200002)190:3<255::AID-PATH526>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 109.Lefer AM, Lefer DJ. The role of nitric oxide and cell adhesion molecules on the microcirculation in ischaemia-reperfusion. Cardiovasc Res. 1996;32:743–751. [PubMed] [Google Scholar]
- 110.Franco-Pons N, Casas J, Fabrias G, Gea-Sorli S, de-Madaria E, Gelpi E, Closa D. Fat Necrosis Generates Proinflammatory Halogenated Lipids During Acute Pancreatitis. Ann Surg. 2012 doi: 10.1097/SLA.0b013e318269d536. [DOI] [PubMed] [Google Scholar]
- 111.Eming SA, Hammerschmidt M, Krieg T, Roers A. Interrelation of immunity and tissue repair or regeneration. Semin Cell Dev Biol. 2009;20:517–527. doi: 10.1016/j.semcdb.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 112.Nurden AT. Platelets, inflammation and tissue regeneration. Thromb Haemost. 2011;105(Suppl 1):S13–S33. doi: 10.1160/THS10-11-0720. [DOI] [PubMed] [Google Scholar]
- 113.Matzinger P. The danger model: a renewed sense of self. Science. 2002;296:301–305. doi: 10.1126/science.1071059. [DOI] [PubMed] [Google Scholar]
- 114.Hashimoto C, Hudson KL, Anderson KV. The Toll gene of Drosophila, required for dorsal-ventral embryonic polarity, appears to encode a transmembrane protein. Cell. 1988;52:269–279. doi: 10.1016/0092-8674(88)90516-8. [DOI] [PubMed] [Google Scholar]
- 115.Medzhitov R, Janeway C., Jr The Toll receptor family and microbial recognition. Trends in microbiology. 2000;8:452–456. doi: 10.1016/s0966-842x(00)01845-x. [DOI] [PubMed] [Google Scholar]
- 116.Hargreaves DC, Medzhitov R. Innate sensors of microbial infection. Journal of clinical immunology. 2005;25:503–510. doi: 10.1007/s10875-005-8065-4. [DOI] [PubMed] [Google Scholar]
- 117.Pasare C, Medzhitov R. Toll-like receptors: linking innate and adaptive immunity. Microbes and infection / Institut Pasteur. 2004;6:1382–1387. doi: 10.1016/j.micinf.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 118.Castellheim A, Brekke OL, Espevik T, Harboe M, Mollnes TE. Innate immune responses to danger signals in systemic inflammatory response syndrome and sepsis. Scand J Immunol. 2009;69:479–491. doi: 10.1111/j.1365-3083.2009.02255.x. [DOI] [PubMed] [Google Scholar]
- 119.Oberholzer A, Oberholzer C, Moldawer LL. Sepsis syndromes: understanding the role of innate and acquired immunity. Shock. 2001;16:83–96. doi: 10.1097/00024382-200116020-00001. [DOI] [PubMed] [Google Scholar]
- 120.Beutler B, Hoebe K, Du X, Ulevitch RJ. How we detect microbes and respond to them: the Toll-like receptors and their transducers. Journal of leukocyte biology. 2003;74:479–485. doi: 10.1189/jlb.0203082. [DOI] [PubMed] [Google Scholar]
- 121.Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005;365:63–78. doi: 10.1016/S0140-6736(04)17667-8. [DOI] [PubMed] [Google Scholar]
- 122.Beutler B, Poltorak A. Sepsis and evolution of the innate immune response. Critical care medicine. 2001;29:S2–S6. doi: 10.1097/00003246-200107001-00002. discussion S6–7. [DOI] [PubMed] [Google Scholar]
- 123.Beutler B. Science review: key inflammatory and stress pathways in critical illness - the central role of the Toll-like receptors. Crit Care. 2003;7:39–46. doi: 10.1186/cc1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Beutler B, Cerami A. Cachectin/tumor necrosis factor: an endogenous mediator of shock and inflammation. Immunologic research. 1986;5:281–293. doi: 10.1007/BF02935501. [DOI] [PubMed] [Google Scholar]
- 125.Beutler B. Innate immune sensing of microbial infection: the mechanism and the therapeutic challenge. Wien Med Wochenschr. 2002;152:547–551. doi: 10.1046/j.1563-258x.2002.02097.x. [DOI] [PubMed] [Google Scholar]
- 126.Keel M, Ungethum U, Steckholzer U, Niederer E, Hartung T, Trentz O, Ertel W. Interleukin-10 counterregulates proinflammatory cytokine-induced inhibition of neutrophil apoptosis during severe sepsis. Blood. 1997;90:3356–3363. [PubMed] [Google Scholar]
- 127.Neidhardt R, Keel M, Steckholzer U, Safret A, Ungethuem U, Trentz O, Ertel W. Relationship of interleukin-10 plasma levels to severity of injury and clinical outcome in injured patients. J Trauma. 1997;42:863–870. doi: 10.1097/00005373-199705000-00017. discussion 870-861. [DOI] [PubMed] [Google Scholar]
- 128.Ouyang W, Rutz S, Crellin NK, Valdez PA, Hymowitz SG. Regulation and functions of the IL-10 family of cytokines in inflammation and disease. Annu Rev Immunol. 2011;29:71–109. doi: 10.1146/annurev-immunol-031210-101312. [DOI] [PubMed] [Google Scholar]
- 129.Scumpia PO, Moldawer LL. Biology of interleukin-10 and its regulatory roles in sepsis syndromes. Crit Care Med. 2005;33:S468–S471. doi: 10.1097/01.ccm.0000186268.53799.67. [DOI] [PubMed] [Google Scholar]
- 130.Fiorentino DF, Zlotnik A, Mosmann TR, Howard M, O'Garra A. IL-10 inhibits cytokine production by activated macrophages. J Immunol. 1991;147:3815–3822. [PubMed] [Google Scholar]
- 131.Moore KW, O'Garra A, de Waal Malefyt R, Vieira P, Mosmann TR. Interleukin-10. Annu Rev Immunol. 1993;11:165–190. doi: 10.1146/annurev.iy.11.040193.001121. [DOI] [PubMed] [Google Scholar]
- 132.Fagundes CT, Amaral FA, Souza AL, Vieira AT, Xu D, Liew FY, Souza DG, Teixeira MM. ST2, an IL-1R family member, attenuates inflammation and lethality after intestinal ischemia and reperfusion. J Leukoc Biol. 2007;81:492–499. doi: 10.1189/jlb.0606422. [DOI] [PubMed] [Google Scholar]
- 133.Reddy RC, Chen GH, Tekchandani PK, Standiford TJ. Sepsis-induced immunosuppression: from bad to worse. Immunol Res. 2001;24:273–287. doi: 10.1385/IR:24:3:273. [DOI] [PubMed] [Google Scholar]
- 134.Tominaga S. A putative protein of a growth specific cDNA from BALB/c-3T3 cells is highly similar to the extracellular portion of mouse interleukin 1 receptor. FEBS Lett. 1989;258:301–304. doi: 10.1016/0014-5793(89)81679-5. [DOI] [PubMed] [Google Scholar]
- 135.Takagi T, Yanagisawa K, Tsukamoto T, Tetsuka T, Nagata S, Tominaga S. Identification of the product of the murine ST2 gene. Biochim Biophys Acta. 1993;1178:194–200. doi: 10.1016/0167-4889(93)90009-e. [DOI] [PubMed] [Google Scholar]
- 136.Schmitz J, Owyang A, Oldham E, Song Y, Murphy E, McClanahan TK, Zurawski G, et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23:479–490. doi: 10.1016/j.immuni.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 137.Allakhverdi Z, Smith DE, Comeau MR, Delespesse G. Cutting edge: The ST2 ligand IL-33 potently activates and drives maturation of human mast cells. J Immunol. 2007;179:2051–2054. doi: 10.4049/jimmunol.179.4.2051. [DOI] [PubMed] [Google Scholar]
- 138.Pecaric-Petkovic T, Didichenko SA, Kaempfer S, Spiegl N, Dahinden CA. Human basophils and eosinophils are the direct target leukocytes of the novel IL-1 family member IL-33. Blood. 2009;113:1526–1534. doi: 10.1182/blood-2008-05-157818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bourgeois E, Van LP, Samson M, Diem S, Barra A, Roga S, Gombert JM, et al. The pro-Th2 cytokine IL-33 directly interacts with invariant NKT and NK cells to induce IFN-gamma production. Eur J Immunol. 2009;39:1046–1055. doi: 10.1002/eji.200838575. [DOI] [PubMed] [Google Scholar]
- 140.Xu D, Chan WL, Leung BP, Huang F, Wheeler R, Piedrafita D, Robinson JH, Liew FY. Selective expression of a stable cell surface molecule on type 2 but not type 1 helper T cells. J Exp Med. 1998;187:787–794. doi: 10.1084/jem.187.5.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lohning M, Stroehmann A, Coyle AJ, Grogan JL, Lin S, Gutierrez-Ramos JC, Levinson D, et al. T1/ST2 is preferentially expressed on murine Th2 cells, independent of interleukin 4, interleukin 5, and interleukin 10, and important for Th2 effector function. Proc Natl Acad Sci U S A. 1998;95:6930–6935. doi: 10.1073/pnas.95.12.6930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Coyle AJ, Lloyd C, Tian J, Nguyen T, Erikkson C, Wang L, Ottoson P, et al. Crucial role of the interleukin 1 receptor family member T1/ST2 in T helper cell type 2-mediated lung mucosal immune responses. J Exp Med. 1999;190:895–902. doi: 10.1084/jem.190.7.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Townsend MJ, Fallon PG, Matthews DJ, Jolin HE, McKenzie AN. T1/ST2-deficient mice demonstrate the importance of T1/ST2 in developing primary T helper cell type 2 responses. J Exp Med. 2000;191:1069–1076. doi: 10.1084/jem.191.6.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Leung BP, Xu D, Culshaw S, McInnes IB, Liew FY. A novel therapy of murine collagen-induced arthritis with soluble T1/ST2. J Immunol. 2004;173:145–150. doi: 10.4049/jimmunol.173.1.145. [DOI] [PubMed] [Google Scholar]
- 145.Sweet MJ, Leung BP, Kang D, Sogaard M, Schulz K, Trajkovic V, Campbell CC, et al. A novel pathway regulating lipopolysaccharide-induced shock by ST2/T1 via inhibition of Toll-like receptor 4 expression. J Immunol. 2001;166:6633–6639. doi: 10.4049/jimmunol.166.11.6633. [DOI] [PubMed] [Google Scholar]
- 146.Brint EK, Xu D, Liu H, Dunne A, McKenzie AN, O'Neill LA, Liew FY. ST2 is an inhibitor of interleukin 1 receptor and Toll-like receptor 4 signaling and maintains endotoxin tolerance. Nat Immunol. 2004;5:373–379. doi: 10.1038/ni1050. [DOI] [PubMed] [Google Scholar]
- 147.Saccani S, Polentarutti N, Penton-Rol G, Sims JE, Mantovani A. Divergent effects of LPS on expression of IL-1 receptor family members in mononuclear phagocytes in vitro and in vivo. Cytokine. 1998;10:773–780. doi: 10.1006/cyto.1998.0359. [DOI] [PubMed] [Google Scholar]
- 148.Mildner M, Storka A, Lichtenauer M, Mlitz V, Ghannadan M, Hoetzenecker K, Nickl S, et al. Primary sources and immunological prerequisites for sST2 secretion in humans. Cardiovasc Res. 2010;87:769–777. doi: 10.1093/cvr/cvq104. [DOI] [PubMed] [Google Scholar]
- 149.Kumar S, Tzimas MN, Griswold DE, Young PR. Expression of ST2, an interleukin-1 receptor homologue, is induced by proinflammatory stimuli. Biochem Biophys Res Commun. 1997;235:474–478. doi: 10.1006/bbrc.1997.6810. [DOI] [PubMed] [Google Scholar]
- 150. <Drake school pic spring 2013 2.pdf>. [Google Scholar]
- 151.Stampalija TCT, Chaemsaithong P, Korzeniewski S, Schwartz A, Ferrazzi E, Dong Z, Hassan S, Romero R. Maternal plasma concentrations of sST2 and angiogenic/anti-angiogenic factors in preeclampsia. The Journal of Maternal-Fetal & Neonatal Medicine. 2013 doi: 10.3109/14767058.2013.784256. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Stampalija TCT, Romero R, Tarca AL, Bhatti G, Chiang PJ, Than NG, Ferrazzi E, Hassan S, Yeo L. Soluble ST2, a modulator of the inflammatory response, in preterm and term labor. The Journal of Maternal-Fetal & Neonatal Medicine Submitted. 2013 doi: 10.3109/14767058.2013.806894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Topping V, Romero R, Than NG, Tarca AL, Xu Z, Kim SY, Wang B, et al. Interleukin-33 in the human placenta. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2013;26:327–338. doi: 10.3109/14767058.2012.735724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Savasan ZA, Chaiworapongsa T, Romero R, et al. Interleukin-19 in fetal systemtic inflammation. J Matern Fetal Neonatal Med. 2012;25:995–1005. doi: 10.3109/14767058.2011.605917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Liu J, Buckley JM, Redmond HP, Wang JH. ST2 negatively regulates TLR2 signaling, but is not required for bacterial lipoprotein-induced tolerance. J Immunol. 2010;184:5802–5808. doi: 10.4049/jimmunol.0904127. [DOI] [PubMed] [Google Scholar]
- 156.Dunne A, O'Neill LA. The interleukin-1 receptor/Toll-like receptor superfamily: signal transduction during inflammation and host defense. Sci STKE. 2003;2003:re3. doi: 10.1126/stke.2003.171.re3. [DOI] [PubMed] [Google Scholar]
- 157.O'Neill LA, Dinarello CA. The IL-1 receptor/toll-like receptor superfamily: crucial receptors for inflammation and host defense. Immunol Today. 2000;21:206–209. doi: 10.1016/s0167-5699(00)01611-x. [DOI] [PubMed] [Google Scholar]
- 158.Brint EK, Fitzgerald KA, Smith P, Coyle AJ, Gutierrez-Ramos JC, Fallon PG, O'Neill LA. Characterization of signaling pathways activated by the interleukin 1 (IL-1) receptor homologue T1/ST2. A role for Jun N-terminal kinase in IL-4 induction. J Biol Chem. 2002;277:49205–49211. doi: 10.1074/jbc.M209685200. [DOI] [PubMed] [Google Scholar]
- 159.Buckley JM, Liu JH, Li CH, Blankson S, Wu QD, Jiang Y, Redmond HP, Wang JH. Increased susceptibility of ST2-deficient mice to polymicrobial sepsis is associated with an impaired bactericidal function. J Immunol. 2011;187:4293–4299. doi: 10.4049/jimmunol.1003872. [DOI] [PubMed] [Google Scholar]
- 160.Moore KW, de Waal Malefyt R, Coffman RL, O'Garra A. Interleukin-10 and the interleukin-10 receptor. Annu Rev Immunol. 2001;19:683–765. doi: 10.1146/annurev.immunol.19.1.683. [DOI] [PubMed] [Google Scholar]
- 161.Trinchieri G. Interleukin-10 production by effector T cells: Th1 cells show self control. J Exp Med. 2007;204:239–243. doi: 10.1084/jem.20070104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Li C, Corraliza I, Langhorne J. A defect in interleukin-10 leads to enhanced malarial disease in Plasmodium chabaudi chabaudi infection in mice. Infect Immun. 1999;67:4435–4442. doi: 10.1128/iai.67.9.4435-4442.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Deckert M, Soltek S, Geginat G, Lutjen S, Montesinos-Rongen M, Hof H, Schluter D. Endogenous interleukin-10 is required for prevention of a hyperinflammatory intracerebral immune response in Listeria monocytogenes meningoencephalitis. Infect Immun. 2001;69:4561–4571. doi: 10.1128/IAI.69.7.4561-4571.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gazzinelli RT, Wysocka M, Hieny S, Scharton-Kersten T, Cheever A, Kuhn R, Muller W, et al. In the absence of endogenous IL-10, mice acutely infected with Toxoplasma gondii succumb to a lethal immune response dependent on CD4+ T cells and accompanied by overproduction of IL-12, IFN-gamma and TNF-alpha. J Immunol. 1996;157:798–805. [PubMed] [Google Scholar]
- 165.Hunter CA, Ellis-Neyes LA, Slifer T, Kanaly S, Grunig G, Fort M, Rennick D, Araujo FG. IL-10 is required to prevent immune hyperactivity during infection with Trypanosoma cruzi. J Immunol. 1997;158:3311–3316. [PubMed] [Google Scholar]
- 166.Nylen S, Sacks D. Interleukin-10 and the pathogenesis of human visceral leishmaniasis. Trends Immunol. 2007;28:378–384. doi: 10.1016/j.it.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 167.Lilic D, Gravenor I, Robson N, Lammas DA, Drysdale P, Calvert JE, Cant AJ, Abinun M. Deregulated production of protective cytokines in response to Candida albicans infection in patients with chronic mucocutaneous candidiasis. Infect Immun. 2003;71:5690–5699. doi: 10.1128/IAI.71.10.5690-5699.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mancilla-Diaz JM, Escartin-Perez RE, Lopez-Alonso VE, Floran-Garduno B, Romano-Camacho JB. Role of 5-HT1A and 5-HT1B receptors in the hypophagic effect of 5-HT on the structure of feeding behavior. Med Sci Monit. 2005;11:BR74–BR79. [PubMed] [Google Scholar]
- 169.Pagliari C, Fernandes ER, Guedes F, Alves C, Sotto MN. Role of mast cells as IL10 producing cells in paracoccidioidomycosis skin lesions. Mycopathologia. 2006;162:331–335. doi: 10.1007/s11046-006-0069-y. [DOI] [PubMed] [Google Scholar]
- 170.Fornari MC, Bava AJ, Guereno MT, Berardi VE, Silaf MR, Negroni R, Diez RA. High serum interleukin-10 and tumor necrosis factor alpha levels in chronic paracoccidioidomycosis. Clin Diagn Lab Immunol. 2001;8:1036–1038. doi: 10.1128/CDLI.8.5.1036-1038.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Howard M, Muchamuel T, Andrade S, Menon S. Interleukin 10 protects mice from lethal endotoxemia. J Exp Med. 1993;177:1205–1208. doi: 10.1084/jem.177.4.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Lang R, Rutschman RL, Greaves DR, Murray PJ. Autocrine deactivation of macrophages in transgenic mice constitutively overexpressing IL-10 under control of the human CD68 promoter. J Immunol. 2002;168:3402–3411. doi: 10.4049/jimmunol.168.7.3402. [DOI] [PubMed] [Google Scholar]
- 173.Jankovic D, Trinchieri G. IL-10 or not IL-10: that is the question. Nat Immunol. 2007;8:1281–1283. doi: 10.1038/ni1207-1281. [DOI] [PubMed] [Google Scholar]
- 174.Fitzgerald DC, Zhang GX, El-Behi M, Fonseca-Kelly Z, Li H, Yu S, Saris CJ, et al. Suppression of autoimmune inflammation of the central nervous system by interleukin 10 secreted by interleukin 27-stimulated T cells. Nat Immunol. 2007;8:1372–1379. doi: 10.1038/ni1540. [DOI] [PubMed] [Google Scholar]
- 175.Awasthi A, Carrier Y, Peron JP, Bettelli E, Kamanaka M, Flavell RA, Kuchroo VK, et al. A dominant function for interleukin 27 in generating interleukin 10-producing anti-inflammatory T cells. Nat Immunol. 2007;8:1380–1389. doi: 10.1038/ni1541. [DOI] [PubMed] [Google Scholar]
- 176.Stumhofer JS, Silver JS, Laurence A, Porrett PM, Harris TH, Turka LA, Ernst M, et al. Interleukins 27 and 6 induce STAT3-mediated T cell production of interleukin 10. Nat Immunol. 2007;8:1363–1371. doi: 10.1038/ni1537. [DOI] [PubMed] [Google Scholar]
- 177.McGeachy MJ, Bak-Jensen KS, Chen Y, Tato CM, Blumenschein W, McClanahan T, Cua DJ. TGF-beta and IL-6 drive the production of IL-17 and IL-10 by T cells and restrain T(H)-17 cell-mediated pathology. Nat Immunol. 2007;8:1390–1397. doi: 10.1038/ni1539. [DOI] [PubMed] [Google Scholar]
- 178.Murray PJ. Understanding and exploiting the endogenous interleukin-10/STAT3-mediated anti-inflammatory response. Curr Opin Pharmacol. 2006;6:379–386. doi: 10.1016/j.coph.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 179.Fiorentino DF, Zlotnik A, Vieira P, Mosmann TR, Howard M, Moore KW, O'Garra A. IL-10 acts on the antigen-presenting cell to inhibit cytokine production by Th1 cells. J Immunol. 1991;146:3444–3451. [PubMed] [Google Scholar]
- 180.Fiorentino DF, Bond MW, Mosmann TR. Two types of mouse T helper cell. IV. Th2 clones secrete a factor that inhibits cytokine production by Th1 clones. J Exp Med. 1989;170:2081–2095. doi: 10.1084/jem.170.6.2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Bogdan C, Vodovotz Y, Nathan C. Macrophage deactivation by interleukin 10. J Exp Med. 1991;174:1549–1555. doi: 10.1084/jem.174.6.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.de Waal Malefyt R, Abrams J, Bennett B, Figdor CG, de Vries JE. Interleukin 10(IL-10) inhibits cytokine synthesis by human monocytes: an autoregulatory role of IL-10 produced by monocytes. J Exp Med. 1991;174:1209–1220. doi: 10.1084/jem.174.5.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Willems F, Marchant A, Delville JP, Gerard C, Delvaux A, Velu T, de Boer M, Goldman M. Interleukin-10 inhibits B7 and intercellular adhesion molecule-1 expression on human monocytes. Eur J Immunol. 1994;24:1007–1009. doi: 10.1002/eji.1830240435. [DOI] [PubMed] [Google Scholar]
- 184.Sakaguchi S. Naturally arising CD4+ regulatory t cells for immunologic self-tolerance and negative control of immune responses. Annu Rev Immunol. 2004;22:531–562. doi: 10.1146/annurev.immunol.21.120601.141122. [DOI] [PubMed] [Google Scholar]
- 185.Yoon BH, Romero R, Shim JY, Shim SS, Kim CJ, Jun JK. C-reactive protein in umbilical cord blood: a simple and widely available clinical method to assess the risk of amniotic fluid infection and funisitis. J Matern Fetal Neonatal Med. 2003;14:85–90. doi: 10.1080/jmf.14.2.85.90. [DOI] [PubMed] [Google Scholar]
- 186.Santana C, Guindeo MC, Gonzalez G, Garcia-Munoz F, Saavedra P, Domenech E. Cord blood levels of cytokines as predictors of early neonatal sepsis. Acta Paediatr. 2001;90:1176–1181. doi: 10.1080/080352501317061602. [DOI] [PubMed] [Google Scholar]
- 187.Nishimaki S, Sato M, An H, Shima Y, Akaike T, Yokoyama U, Yokota S. Comparison of markers for fetal inflammatory response syndrome: fetal blood interleukin-6 and neonatal urinary beta(2)-microglobulin. J Obstet Gynaecol Res. 2009;35:472–476. doi: 10.1111/j.1447-0756.2008.00988.x. [DOI] [PubMed] [Google Scholar]
- 188.Romero R, Gomez R, Galasso M, Mazor M, Berry SM, Quintero RA, Cotton DB. The natural interleukin-1 receptor antagonist in the fetal, maternal, and amniotic fluid compartments: the effect of gestational age, fetal gender, and intrauterine infection. Am J Obstet Gynecol. 1994;171:912–921. doi: 10.1016/s0002-9378(94)70058-3. [DOI] [PubMed] [Google Scholar]
- 189.Romero R, Ceska M, Avila C, Mazor M, Behnke E, Lindley I. Neutrophil attractant/activating peptide-1/interleukin-8 in term and preterm parturition. Am J Obstet Gynecol. 1991;165:813–820. doi: 10.1016/0002-9378(91)90422-n. [DOI] [PubMed] [Google Scholar]
- 190.Paananen R, Husa AK, Vuolteenaho R, Herva R, Kaukola T, Hallman M. Blood cytokines during the perinatal period in very preterm infants: relationship of inflammatory response and bronchopulmonary dysplasia. J Pediatr. 2009;154:39–43 e33. doi: 10.1016/j.jpeds.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 191.Chaiworapongsa T, Romero R, Kim JC, Kim YM, Blackwell SC, Yoon BH, Gomez R. Evidence for fetal involvement in the pathologic process of clinical chorioamnionitis. Am J Obstet Gynecol. 2002;186:1178–1182. doi: 10.1067/mob.2002.124042. [DOI] [PubMed] [Google Scholar]
- 192.Savasan ZA, Chaiworapongsa T, Romero R, Hussein Y, Kusanovic JP, Xu Y, Dong Z, et al. Interleukin-19 in fetal systemic inflammation. J Matern Fetal Neonatal Med. 2012;25:995–1005. doi: 10.3109/14767058.2011.605917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Wirbelauer J, Seidenspinner S, Thomas W, Kunzmann S, Speer CP. Funisitis is associated with increased interleukin-10 gene expression in cord blood mononuclear cells in preterm infants</=32 weeks of gestation. Eur J Obstet Gynecol Reprod Biol. 2011;155:31–35. doi: 10.1016/j.ejogrb.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 194.Robertson SA, Skinner RJ, Care AS. Essential role for IL-10 in resistance to lipopolysaccharide-induced preterm labor in mice. J Immunol. 2006;177:4888–4896. doi: 10.4049/jimmunol.177.7.4888. [DOI] [PubMed] [Google Scholar]
- 195.Terrone DA, Rinehart BK, Granger JP, Barrilleaux PS, Martin JN, Jr, Bennett WA. Interleukin-10 administration and bacterial endotoxin-induced preterm birth in a rat model. Obstet Gynecol. 2001;98:476–480. doi: 10.1016/s0029-7844(01)01424-7. [DOI] [PubMed] [Google Scholar]
- 196.Fortunato SJ, Menon R, Swan KF, Lombardi SJ. Interleukin-10 inhibition of interleukin-6 in human amniochorionic membrane: transcriptional regulation. Am J Obstet Gynecol. 1996;175:1057–1065. doi: 10.1016/s0002-9378(96)80053-6. [DOI] [PubMed] [Google Scholar]
- 197.Froen JF, Munkeby BH, Stray-Pedersen B, Saugstad OD. Interleukin-10 reverses acute detrimental effects of endotoxin-induced inflammation on perinatal cerebral hypoxia-ischemia. Brain Res. 2002;942:87–94. doi: 10.1016/s0006-8993(02)02700-2. [DOI] [PubMed] [Google Scholar]
- 198.Meyer U, Murray PJ, Urwyler A, Yee BK, Schedlowski M, Feldon J. Adult behavioral and pharmacological dysfunctions following disruption of the fetal brain balance between pro-inflammatory and IL-10-mediated anti-inflammatory signaling. Mol Psychiatry. 2008;13:208–221. doi: 10.1038/sj.mp.4002042. [DOI] [PubMed] [Google Scholar]
- 199.Brunner M, Krenn C, Roth G, Moser B, Dworschak M, Jensen-Jarolim E, Spittler A, et al. Increased levels of soluble ST2 protein and IgG1 production in patients with sepsis and trauma. Intensive Care Med. 2004;30:1468–1473. doi: 10.1007/s00134-004-2184-x. [DOI] [PubMed] [Google Scholar]
- 200.Hoogerwerf JJ, Tanck MW, van Zoelen MA, Wittebole X, Laterre PF, van der Poll T. Soluble ST2 plasma concentrations predict mortality in severe sepsis. Intensive Care Med. 2010;36:630–637. doi: 10.1007/s00134-010-1773-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003;348:138–150. doi: 10.1056/NEJMra021333. [DOI] [PubMed] [Google Scholar]
- 202.van der Poll T, Opal SM. Host-pathogen interactions in sepsis. Lancet Infect Dis. 2008;8:32–43. doi: 10.1016/S1473-3099(07)70265-7. [DOI] [PubMed] [Google Scholar]
- 203.Volk HD, Reinke P, Docke WD. Clinical aspects: from systemic inflammation to 'immunoparalysis'. Chem Immunol. 2000;74:162–177. doi: 10.1159/000058753. [DOI] [PubMed] [Google Scholar]