Abstract
Background
The open abdomen is an increasingly used technique that is applied in a wide variety of clinical situations. The ABThera Open Abdomen Negative Pressure Therapy System is one of the most common and successful temporary closure systems, but it has limited ability to close the fascia in approximately 30% of patients. The abdominal reapproximation anchor system (ABRA) is a dynamic closure system that seems ideal to manage patients who may not achieve primary fascial closure with ABThera alone. We report on the use of the ABRA in conjunction with the ABThera in patients with an open abdomen.
Methods
We retrospectively analyzed patients with an open abdomen managed with the ABThera and ABRA between January 2007 and December 2012 at the Halifax Infirmary, QEII Health Science Centre, Halifax, Nova Scotia.
Results
Sixteen patients had combination therapy using the ABRA and ABThera systems for treatment of the open abdomen. After removing patients who died prior to closure, primary fascial closure was achieved in 12 of 13 patients (92%).
Conclusion
We observed a high rate of primary fascial closure in patients with an open abdomen managed with the ABThera system in conjuction with the ABRA. Applying mechanical traction in addition to the ABThera should be considered in patients predicted to be at high risk for failure to achieve primary fascial closure.
Abstract
Contexte
La laparotomie, ou « abdomen ouvert », est une technique de plus en plus employée dans une grande diversité de contextes cliniques. Le système ABThera (thérapie par pression négative pour abdomen ouvert) est l’un des systèmes de fermeture temporaire de l’abdomen les plus fréquemment utilisés et efficaces, mais sa capacité de refermer le fascia apparaît limitée chez environ 30 % des patients. Le système ABRA est un système de fermeture dynamique qui semble idéal pour la prise en charge des patients qui pourraient ne pas obtenir une fermeture primaire du fascia avec le système ABThera seul. Nous faisons rapport de l’utilisation du système ABRA en conjonction avec le système ABThera chez des patients soumis à une laparotomie.
Méthodes
Nous avons analysé rétrospectivement des patients soumis à une laparotomie et pris en charge au moyen des systèmes ABThera et ABRA entre janvier 2007 et décembre 2012 au Halifax Infirmary du Centre des sciences de la santé QEII d’Halifax, en Nouvelle-Écosse.
Résultats
Seize patients ont subi un traitement concomitant par les systèmes ABRA et ABThera pour leur laparotomie. Après exclusion des patients décédés avant l’obtention de la fermeture primaire du fascia, cette dernière a été réussie chez 12 patients sur 13 (92 %).
Conclusion
Nous avons observé un taux élevé de fermeture primaire du fascia chez les patients soumis à une laparotomie et traités au moyen du système ABThera en conjonction avec le système ABRA. L’application d’une traction mécanique en plus du système ABThera est à envisager chez les patients présumés à risque élevé d’échec de la fermeture primaire du fascia.
The open abdomen is an increasingly used technique that is applied in a wide variety of clinical situations, including treatment and prevention of abdominal compartment syndrome, damage control laparotomy and severe intra-abdominal sepsis.1 Once the abdominal fascia has been opened, the viscera must be contained by a temporary abdominal closure (TAC). The goals of TAC include protection of the viscera, prevention of adhesions of the viscera to the abdominal wall, removal of intra-abdominal fluid and prevention of fascial retraction.2 A variety of different techniques for TAC have been used in the past, including the Bagota bag, mesh, Wittmann patch and Barker vacuum pack. A systematic review and prospective observational trial have demonstrated that the ABThera Open Abdomen Negative Pressure Therapy System (KCI USA) may be the most effective TAC method.3,4
Although the ABThera system achieves all the goals of TAC, progressive loss of abdominal domain may still occur because of the ABThera’s limited ability to stabilize the fascia in some patients (Fig. 1). The ABThera, when used alone, fails to reapproximate the fascia in about 30% of patients with an open abdomen.2–4 Failure to close the fascia primarily results in an increased risk of enteroatmospheric fistula, requirement for skin grafting of the visceral mass and a large ventral hernia. Furthermore, early primary closure of the open abdomen has been associated with improved patient survival.5
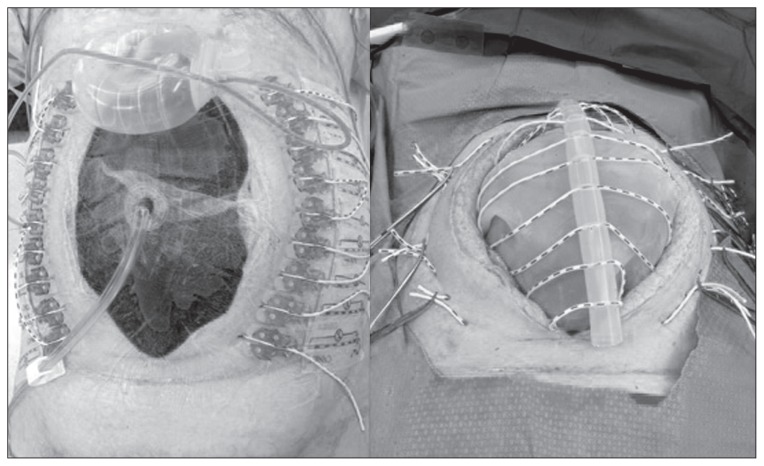
Fig. 1.

Patient with an open abdomen demonstrating progressive fascial retraction and loss of abdominal domain during ABThera treatment.
The use of mechanical traction with sequential suturing and mesh imbrication in conjunction with the ABThera have been shown to significantly increase primary fascial closure rates to approximately 90%.2,6–9 The abdominal reapproximation anchor system (ABRA; Canica Design Inc.) is a dynamic closure system that uses elastomers through the full thickness of the abdominal wall that slowly pull the fascia together under continuous variable tension. It is easier to manage than mesh imbrication or sequential suturing and allows for the abdominal wall to oscillate with patient movement and breathing. Four case series have previously demonstrated the ABRA’s efficacy in achieving fascial closure in the open abdomen.10–13 Although combined therapy using the ABThera and the ABRA seems ideal to manage patients who may not achieve primary fascial closure with ABThera alone, this has not been previously described.
We report on the use of the ABRA in conjunction of the ABThera in patients with an open abdomen.
Methods
We conducted an insitution review board–approved, single-institution, retrospective analysis of patients with an open abdomen who were managed with the ABThera and ABRA systems between January 2007 and December 2012. Patients were identified from the Acute Care Surgery Surgical Log, which recorded all emergency surgical cases performed at the Halifax Infirmary, QEII Health Science Centre, Halifax, Nova Scotia, Canada. During this time period there was no protocol for the management of the open abdomen. The decision to use the open abdomen was at the discretion of the attending surgeon, as was the use and timing of the ABThera and ABRA.
The usual practice at our institution was to use an ABThera for TAC during the first operation in which an open abdomen technique was employed. ABThera installation involved placing the fenestrated plastic dressing with the incorporated polyurethane sponge over the viscera, under the fascia, down to the retroperitoneum posteriorly, the diaphragm superiorly and pelvis inferiorly. This prevented adherence of the viscera to the abdominal wall and allowed for mobilization of the fascia while preventing injury to the viscera. A granufoam sponge was then placed over the plastic sheet and the abdomen was sealed with an adherent plastic sheet to the skin. The ABThera was then placed to –125 mm Hg continuous suction. The ABThera dressing was changed every 3–5 days in the operating room.
The ABRA was added to the ABThera at the surgeon’s discretion. Typically, this was done when significant fascial retraction was observed, or when the fascia was failing to medialize over time. Installation of the ABRA involved placing elastomeres 5 cm from the fascial edge and 90° to the fascia through the skin and full thickness of the abdominal wall. The elastomeres were placed as close together as the skin anchor buttons would permit, approximately 3 cm apart. The elastomeres were placed over the ABThera fenestrated sheet and below the sponge (Fig. 2). If the fenestrated silicone sheet included with the ABRA kit was used, it was placed over the ABThera fenestrated sheet and below the granufoam sponges. An adhesive button tail was placed to the skin anchor buttons to prevent displacement and tilting. The ABRA elastomers were tightened daily to 1.5 times their tension-free length along with manual medialization of the fascia until primary closure was achieved. Primary closure was performed in the operating room when the fascia could be brought together under reasonable tension without causing physiologic compromise due to intra-abdominal hypertension. In some cases, intra-abdominal pressure was measured during closure. Fascial closure was performed using a running 1 polydioxanone suture.
Fig. 2.
Installation of the ABRA system to the ABThera.
Results
During the study period, 78 patients underwent procedures using an open abdomen. Overall mortality was 24% (19 of 78). We identified 16 patients who had combination therapy using the ABRA and ABThera for treatment of the open abdomen (Table 1). The mean age of patients was 52.5 (range 33–66) years, and 10 patients (63%) were men. In patients managed without an ABRA, mortality was 26% (16 of 62), and primary closure failed in 13 of the remaining 46 patients (28%). Of those in whom primary closure failed, 8 were bridged with mesh and 5 were managed with a planned ventral hernia.
Table 1.
Patients with an open abdomen managed with both the ABThera and ABRA
| Group; age, yr | Sex | L1 to ABRA | Treatment | LOS ICU | LOS HOSP | Ostomy | Anastomosis | Diagnosis | Outcome | SAPS II | Bjorch classification |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ACS | |||||||||||
| 49 | M | 12 | 11 | 43 | 58 | N | N | Pancreatitis | Primary closure | 47 | 1A |
| 47 | M | 7 | 24 | 37 | 41 | N | Y | Pancreatitis | Primary closure | 41 | 1B |
| 53 | F | 7 | 16 | N/A | 79 | N | N | Pancreatitis | Primary closure | 46 | 1A |
| 66 | M | 4 | N/A | 16 | 16 | N | N | Ruptured AAA | Death from sepsis | 58 | 1B |
| 36 | F | 12 | 31 | 41 | 95 | N | Y | Post gastric sleeve | Primary closure | 63 | 1B |
| 40 | M | 0 | 5 | 12 | 27 | N | N | Post midgut volvulus | Primary closure | 51 | 1A |
| Trauma | |||||||||||
| 32 | M | 2 | 28 | 28 | 46 | N | Y | Damage control | Primary closure (Died) | 48 | 1B |
| 52 | F | 2 | 3 | 6 | 40 | N | Y | Damage control | Primary closure | 30 | 1B |
| 58 | M | 7 | 24 | 31 | 40 | Y | Y | Damage control | Closure with vicryl mesh | 39 | 1B |
| 33 | M | 4 | 17 | 5 | 27 | Y | Y | Damage control | Primary closure | 35 | 1B |
| GI | |||||||||||
| 62 | M | 3 | 4 | 29 | 46 | Y | N | Intraabdominal sepsis | Primary closure | 60 | 1B |
| 54 | M | 19 | 6 | 29 | 122 | Y | Y | Intraabdominal sepsis | Primary closure | 65 | 1B |
| 56 | M | 4 | 28 | 32 | 146 | N | Y | Intraabdominal sepsis | Primary closure | 79 | 1B |
| 38 | F | 15 | 3 | 15 | 28 | N | N | Intraabdominal sepsis | Primary closure | 97 | 1A |
| 65 | F | 7 | N/A | 31 | 31 | Y | N | Intraabdominal sepsis | Death from sepsis | 50 | 1B |
| 66 | F | 11 | N/A | 36 | 36 | Y | Y | Intraabdominal sepsis | Death from sepsis | 58 | 1A |
AAA = abdominal aortic aneurysm; ACS = abdominal compartment syndrome; F = female; GI = gastrointestinal; HOSP = hospital; ICU = intensive care unit; LOS = length of stay; M = male; N = no; N/A = not applicable; SAPS II = Simplified Acute Physiology Score; Y = yes.
In patients managed with an ABRA and ABThera, the most common reason for using an open abdomen was for the management of abdominal compartment syndrome (38%) and severe intra-abdominal sepsis (38%). Severe pancreatitis accounted for the majority of abdominal compartment syndrome cases. Damage control surgery, in the setting of trauma, accounted for 25% of cases.
An anastomosis was present in 9 of 16 (56%) and an ostomy (i.e., colostomy, ileostomy, diverting ileostomy/ colostomy) was present in 6 (38%) patients. Four (25%) patients had both an anastomosis and an ostomy. There were no reported stoma complications related to the addition of the ABRA. None of the patients had a history of radiation treatment.
After the ABThera was installed, the addition of the ABRA system occurred at a median of 7 (range 0–19) days. Most patients had the ABRA system applied on the first or second ABThera dressing change. There was significant variability observed in the timing of ABRA installation, as it was at the discretion of the surgeon. The patient who had the ABRA placed on day 0 had a decompressive laparotomy for abdominal compartment syndrome. In this case, the elastomers were placed but not loaded under tension in an attempt to prevent fascial retraction in excess of what was required to relieve intra-abdominal hypertension.
All patients in whom the ABRA was used had a Bjorch Open Abdomen Classification System grade of 1A or 1B.14
After removing patients who died prior to closure, primary fascial closure was achieved in 12 of 13 patients (92%). The number of days required for fascial closure after the addition of the ABRA was a median of 17 (range 3–31) days. Fascial closure was not achieved in the remaining patient because the surgeon elected to remove the ABRA and bridge the fascial gap with a Vicryl mesh after 31 days with an open abdomen and 24 days of treatment with the ABRA and ABThera.
Skin breakdown at the ABRA button site was observed in 1 (6%) patient. Recurrent abdominal compartment syndrome was noted in 1 patient who was subsequently treated in the intensive care unit by decreasing the tension of the ABRA elastomers.
Overall survival in patients with an ABRA and ABThera was 75%, with 3 of the 4 deaths occurring before primary fascial closure was achieved. Sepsis and multisystem organ failure was the cause of death in all cases, including 1 patient who died from an anastamotic leak and ensuing sepsis after primary closure. The average Simplified Acute Physiology II Score (SAPS II) was 54 (range 41–97). The length of stay in the intensive care unit was a median of 30 (range 5–47) days. Excluding the 4 patients who died, the length of stay in hospital was a median of 43.5 (range 27–146) days.
Discussion
The use of the open abdomen, although a lifesaving technique, presents a clinical challenge that is associated with significant morbidity and mortality. Once the physiologic crisis necessitating the open abdomen has resolved, rapid primary closure of the fascia is required to prevent complications, such as fistula and loss of fluid, protein, heat and electrolytes. Failure to close the fascia results in a giant ventral hernia that requires a complex repair and has significant associated morbidity.4 Furthermore, delay in closure of the fascia is associated with increased mortality.
The ABThera open abdomen negative pressure therapy protects the viscera from adhering to the abdominal wall and effectively removes fluid from the entire abdominal cavity. This facilitates the safe mobilization of the native fascia and, compared with other types of TAC, improves the rate of primary fascial closure.3,15,16 However, the ABThera still fails to achieve primary closure in approximately 30% of patients with an open abdomen. In our experience as well as other authors’, it is usually apparent 4–7 days after placement of the ABThera that the fascia retracts further and will likely not close with the ABThera alone.10,17 Although the reason for using an ABRA in addition to the ABThera was not recorded in our series, surgeons typically choose to use the ABRA in patients in whom they feel the fascia is unlikely to close with the ABThera alone. Consequently, we hypothesize that if the ABThera had been used without the ABRA, a primary fascial closure rate of less than 70% would have been observed in these patients. In spite of this, the addition of the ABRA to the ABThera was associated with a successful primary fascial closure in 92% of patients in our study. In the 1 patient in whom primary fascial closure failed, the surgeon removed the ABRA and placed a vicryl mesh after 24 days of treatment with the ABRA. It is possible that primary fascial closure may have been possible in this patient as well if more time had been given with the ABRA, as successful closure has been reported at up to 31 days in our study and 62 days in other studies involving the ABRA.10–12 Achieving primary fascial closure avoids the morbidity of a ventral hernia and a second operation to repair it. However, the prolonged use of the ABRA to achieve primary closure comes at the cost of ongoing ABThera changes and increased length of stay in hospital. A cost analysis to determine the length of time after which attempting primary closure with the ABRA is no longer cost-effective could be a direction for future study.
The high rate of primary fascial closure observed in our series is consistent with that in other studies that have used the addition of mechanical traction to the ABThera system. Rasilainen and colleagues6 reported a primary fascial closure rate of 53% using the intra-abdominal vacuum-assisted closure (VAC) system alone, which increased to 93% primary closure when a mesh was sequentially imbricated over top. Similarly, sequential fascial suturing over the intra-abdominal VAC has increased rates of primary fascial closure to approximately 90%.8,9 Specific to the ABRA system, Verdam and colleagues11 reported primary fascial closure in 14 of 16 patients (88%), Salman and colleagues10 reported primary closure in 7 of 7 patients with an open abdomen, and Haddock and colleagues13 reported primary closure in 30 of 36 (83%) patients.
We speculate that early application of the ABRA may be important in achieving successful primary fascial closure. Early application prevents fascial retraction and can start pulling the fascia together while the tissues are relatively more dynamic. Preventing adhesions of the viscera to the abdominal wall is also important to allow for safe and unimpeded medialization of the fascia. This is highlighted in the study by Reimer and colleagues12 in which the ABRA was placed relatively later (average of 18 d) and in which primary closure was achieved in only 14 of 23 patients (61%). Success of primary fascial closure was associated with earlier application of the ABRA and having the fascia free of adhesions to the abdominal wall.12 Similar to us, Haddock and colleagues13 reported fascial closure in 83% of patients with an average time from first laparotomy to ABRA placement of 11.9 days. However, in their study, there appeared to be a longer median time from the first laparotomy to the placement of the ABRA in patients achieving primary fascial closure. They hypothesized that patients who had a more thorough decontamination of the abdomen with a longer duration of an open abdomen would be more amenable to closure.13 In our cohort, the ABRA was placed earlier in the trauma subgroup of patients relative to the gastrointestinal sepsis subgroup, highlighting the desire to create as clean an abdominal cavity as possible before placing the ABRA.
In previous studies, trauma patients had a higher rate of primary closure than those with septic abdomens.17,18 In our series, we observed an equally high rate of closure in patients with nontraumatic etiologies, possibly because we used the ABThera system, which allowed for suctioning of the pelvis, paracolic gutters and subdiaphragmatic spaces. The previous studies used a VAC system, which may not have been able to decontaminate the abdomen as readily and thereby prevented successful primary closure.
Our study demonstrates the severity of illness associated with patients managed with an open abdomen. The observed mortality of 25% is consistent with that of other cohorts of patients managed with an open abdomen.2,17,19 No deaths in our study were directly attributable to the ABRA device. Pressure sores related to the ABRA buttons have been reported as a complication of the ABRA, with the study by Verdam and colleagues11 reporting its occurrence in 12 of 18 patients. In our study, skin breakdown was observed in only 1 patient. The reason for this may be secondary to our practice of placing the ABRA buttons over the ABThera adherent dressing, which may have provided additional protection to the skin.
Limitations
This study has several weaknesses. First, it is uncontrolled and describes outcomes of a cohort of patients managed entirely at the surgeon’s discretion, with no protocol to guide therapy. The reasons the surgeon decided to add the ABRA were not specifically recorded for all patients. Second, as the study was not prospective, many pertinent data points, such as body mass index, were not available for all patients. This makes the generalization of our observations difficult.
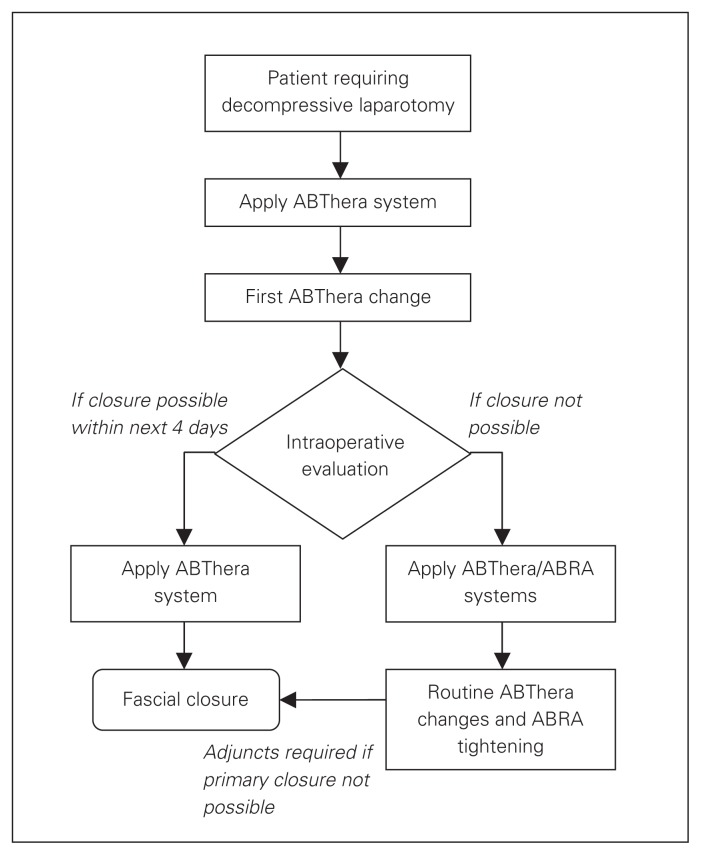
Based on the experience gained from this cohort, and in context of other studies using the ABThera, we have proposed a treatment algorithm of the open abdomen that recommends early use of mechanical traction in addition to the ABThera (Fig. 3). This recommendation has been made by other authors as well.2 The ABThera is essential for removing fluid and contamination from the abdomen and prevents adhesions between the visceral mass and the abdominal wall. If the fascia is failing to medialize by the first dressing change on day 3–5, we suggest the addition of mechanical traction to the fascia in order to increase the rate of primary fascial closure. The options for this include sequential suturing of the fascia, progressive imbrication of mesh sutured to the fascia and the ABRA system. We prefer the ABRA system, as in our experience it takes less time to manage than mesh imbrication or sequential suturing, and tightening can be done daily at the bedside without disrupting the ABThera. Although not specifically recorded, a typical time to install the ABRA is about 10 minutes. The ABRA does not impede the changing of the ABThera, as the elastomers are easily loosened and retracted. The only extra time added to the ABThera change is the time required to tighten the elastomers, which typically takes less than 5 minutes. The ABRA system also leaves the edges of the native fascia undisturbed, which is an attractive advantage at the time of definitive closure.
Fig. 3.
Proposal for management of the open abdomen.
Conclusion
We observed a high rate of primary fascial closure in patients with an open abdomen managed with the ABThera in conjuction with the ABRA. Consideration should be ginen to applying mechanical traction in addition to the ABThera in patients predicted to be at high risk for failure to achieve primary fascial closure.
Footnotes
Presented at the Canadian Critical Care Forum, November 2013.
Competing interests: S. Minor has received an honorarium from KCI to provide an educational talk on temporary abdominal closure. This occurred 3 times over the past 3 years. Each honorarium was approximately $1000. The talk was not specific to the ABThera product, but it did discuss its use. None declared for A. Mukhi.
Contributors: Both authors designed the study, acquired and analyzed the data, wrote and reviewed the article, and approved the final version for publication.
References
- 1.Navsaria P, Nicol A, Hudson D, et al. Negative pressure wound therapy management of the “open abdomen” following trauma: a prospective study and systematic review. World J Emerg Surg. 2013;8:4. doi: 10.1186/1749-7922-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Regner JL, Kobayashi L, Coimbra R. Surgical strategies for management of the abdomen. World J Surg. 2012;36:497–510. doi: 10.1007/s00268-011-1203-7. [DOI] [PubMed] [Google Scholar]
- 3.Roberts DJ, Zygun DA, Grendar J, et al. Negative-pressure wound therapy for critically ill adults with open abdominal wounds: a systematic review. J Trauma Acute Care Surg. 2012;73:629–39. doi: 10.1097/TA.0b013e31825c130e. [DOI] [PubMed] [Google Scholar]
- 4.Cheatham ML, Demetrios D, Fabian TC, et al. Prospective study examining clinical outcomes. World J Surg. 2013;37:2018–30. doi: 10.1007/s00268-013-2080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheatham ML, Safcsak K. Is the evolving management of intra-abdominal hypertension and abdominal compartment syndrome improving survival? Crit Care Med. 2010;38:402–7. doi: 10.1097/ccm.0b013e3181b9e9b1. [DOI] [PubMed] [Google Scholar]
- 6.Rasilainen SK, Mentula PJ, Leppaniemi AK. Vacuum and mesh-mediated fascial traction for primary closure of the open abdomen in critically ill surgical patients. Br J Surg. 2012;99:1725–32. doi: 10.1002/bjs.8914. [DOI] [PubMed] [Google Scholar]
- 7.Cothren CC, Moore EE, Johnson JL, et al. One hundred percent fascial approximation with sequential abdominal closure of the open abdomen. Am J Surg. 2006;192:238–42. doi: 10.1016/j.amjsurg.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Suliburk JW, Ware DN, Balogh Z, et al. Vacuum-assisted wound closure achieves early fascial closure of open abdomens after severe trauma. J Trauma. 2003;55:1155–60. doi: 10.1097/01.TA.0000100218.03754.6A. [DOI] [PubMed] [Google Scholar]
- 9.Miller PR, Meredith JW, Johnson JC, et al. Prospective evaluation of vacuum-assisted fascial closure after open abdomen: planned ventral hernia rate is substantially reduced. Ann Surg. 2004;239:608–14. doi: 10.1097/01.sla.0000124291.09032.bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salman AE, Yetisir F, Aksoy M, et al. Use of dynamic closure system in conjunction with vacuum-assisted closure therapy in delayed closure of open abdomen. Hernia. 2014;18:99–104. doi: 10.1007/s10029-012-1008-0. [DOI] [PubMed] [Google Scholar]
- 11.Verdam FJ, Dolmans DE, Loos MJ, et al. Delayed primary closure of the septic abdomen with a dynamic closure system. World J Surg. 2011;35:2348–55. doi: 10.1007/s00268-011-1210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reimer MW, Yelle YD, Reitsma B, et al. Management of open abdominal wounds using a dynamic fascial closure system. Can J Surg. 2008;51:209–14. [PMC free article] [PubMed] [Google Scholar]
- 13.Haddock C, Konkin DE, Blair NP. Management of the open abdomen with the Abdominal Reapproximation Anchor dynamic fascial closure system. Am J Surg. 2013;205:528–33. doi: 10.1016/j.amjsurg.2013.01.028. [DOI] [PubMed] [Google Scholar]
- 14.Björck M, Bruhin A, Cheatham M, et al. Classification, an important step to improve the management of patients with an open abdomen. World J Surg. 2009;33:1154–7. doi: 10.1007/s00268-009-9996-3. [DOI] [PubMed] [Google Scholar]
- 15.Frazee RC, Abernathy SW, Jupiter DC, et al. Are commercial negative pressure systems worth the cost in the open abdomen management? J Am Coll Surg. 2013;216:730–3. doi: 10.1016/j.jamcollsurg.2012.12.035. [DOI] [PubMed] [Google Scholar]
- 16.Boele van Hensbroek P, Wind J, Dijkgraaf MG, et al. Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg. 2009;33:199–207. doi: 10.1007/s00268-008-9867-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goussous N, Kim BD, Jenkins DH, et al. Factors affecting primary fascial closure of the open abdomen in the non-trauma patient. Surgery. 2012;152:777–83. doi: 10.1016/j.surg.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 18.Mentula P. Non-traumatic causes and the management of the open abdomen. Minerva Chir. 2011;66:153–63. [PubMed] [Google Scholar]
- 19.de Costa A. Making a virtue of necessity: managing the open abdomen. ANZ J Surg. 2006;76:356–63. doi: 10.1111/j.1445-2197.2006.03638.x. [DOI] [PubMed] [Google Scholar]