Summary
Morel-Lavallée lesions are a closed internal degloving, and open débridement can damage the only remaining blood supply to the skin. We performed percutaneous draining and débridement to treat 8 patients in whom the diagnosis of Morel-Lavallée lesions was delayed more than 1 week. Here we discuss our treatment procedures and the outcomes in these 8 patients. We consider percutaneous drainage to be an effective treatment for patients with delayed diagnosis of Morel-Lavallée lesions.
Morel-Lavallée lesions are a closed internal degloving that occurs most commonly over the greater trochanter region, but can also occur in other regions, such as the knee.1 The injury is typically caused by a vertical shearing force over soft tissue that abruptly separates skin and subcutaneous tissue from the underlying fascia, thus creating a dead space that becomes filled with hematoma and necrotic fat.1 The condition generally takes several days to develop, and delayed diagnosis has been reported to occur in one-third of cases or more.1 The condition is typically treated with open débridement of the degloved areas and complete removal of hematoma and necrotic tissue.2,3 However, the vertical blood vessel branches from the underlying muscle and deep fascia have been separated from the degloved skin by the injury, and open débridement may jeopardize the subdermal arterial plexus, the only remaining blood supply to the skin in the area of the lesion.
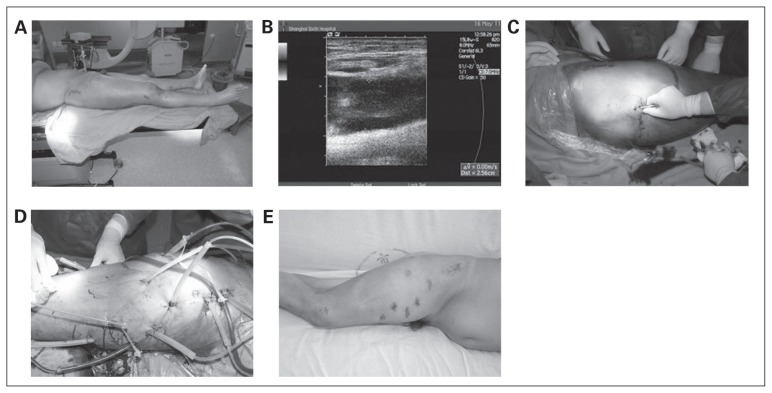
We performed percutaneous drainage to treat 3 men and 5 women with a delayed diagnosis of Morel-Lavallée lesions and found the procedure to be effective; it was associated with minimal morbidity as well as preservation of the remaining blood supply to the skin. The mean age of our 8 patients was 41.9 years, and the mean time from injury to diagnosis was 11.9 (range 8–17) days. The criteria for diagnosis were a local fluctuant area with skin mobility and systemic symptoms, such as fever and hyperleukocytosis (Fig. 1A), and imaging evidence on ultrasound (Fig. 1B) or computed tomography scan. All patients were treated within 1 day after diagnosis.
Fig. 1.
(A) A 53-year-old man with a femoral shaft fracture treated with closed intramedullary nailing. Local swelling appeared with gradual development of fluctuance and skin hypermobility. (B) Ultrasound showing a fluid collection in the subcutaneous tissue adjacent to the fascia lata, confirming a Morel-Lavallée lesion. (C) Percutaneous drainage was performed through a 2-cm incision with suction tips. (D) Several incisions were made for débridement, and double-lumen catheters were placed for suction drainage. (E) Three months postoperatively the soft tissue had healed without complications.
Ultrasonography was performed to detect the location and area of the lesion and to determine the location of the operative incisions. Several 2-cm incisions were made and suction tips inserted through the incisions into the lesion (Fig. 1C). Suction was then applied to remove hemorrhagic fluid and necrotic and liquefied tissue. In some patients, necrotic fascia were scraped out through the incision using a plastic brush. A planer tool used in arthroscopy was also used and effectively removed necrotic adipose tissue. After fluid and necrotic tissue were removed, extensive irrigation was performed. Finally, abdominal double-lumen catheters were placed subcutaneously, and continuous suction was applied (Fig. 1D).
We administered cefuroxime intravenously each day until bacterial culture results were available. If the catheters became obstructed, another operation was performed for percutaneous drainage, débridement and catheter replacement. When the drainage was under 30 mL for a 24-hour period, all catheters were removed, the incisions were sutured, and elastic bandages were used to apply pressure to the degloved skin. Healing of the lesion was defined as disappearance of the fluctuant lesion and loss of excessive skin mobility upon manual examination (Fig. 1E).
Percutaneous drainage was performed successfully without complications in all patients, and systemic inflammatory response syndrome scores all decreased to 0 by the third postoperative day. Because of catheter obstruction, 6 patients received a second débridement, and 2 received a third procedure. Complete healing of the soft tissue and skin occurred in 6 patients. Skin necrosis occurred in 2 patients and was treated by skin grafting. The mean soft tissue healing time was 3.25 weeks. There were no reoccurrences of the lesions and no deep infections or other complications during the 1-year follow-up period.
While Harma and colleagues4 advocated that Morel-Lavallée lesions in the pelvic and gluteal regions can be managed conservatively when the overlying skin is intact and the fluid accumulation is not excessive, open débridement is generally recommended to evacuate any hematoma and remove necrotic tissue once an injury is identified because neglected lesions can become infected.2,3 Nonetheless, open débridement may violate the blood supply of the injured skin and introduces a risk of infection.
Percutaneous management of Morel-Lavallée lesions was introduced by Tseng and Tornetta5 in order to preserve the subdermal arterial plexus. In their series of 19 patients, percutaneous drainage with débridement, irrigation and suction drainage was performed through 2 small incisions in the skin, and all patients achieved soft tissue healing without recurrence or infection. There are some differences between our method and theirs. First, we made more incisions for complete débridement and to enable insertion of double-lumen catheters to provide circulation for postoperative drainage. Second, we used continuous suction.
Percutaneous drainage is an effective treatment for patients with a delayed diagnosis of Morel-Lavallée lesions. The procedure is associated with minimal morbidity and preserves the remaining blood supply to the skin. Percutaneous treatment may be more complex and last longer than open surgery, but the benefits outweigh these factors.
Footnotes
Competing interests: None declared.
Contributors: All authors contributed substantially to writing and revising and to the conception and design of the manuscript and approved the final version submitted for publication.
References
- 1.Powers ML, Halem SF, Sundaram M. Diagnosis: Morel-Lavalee lesion. Orthopedics. 2007;30:322–3. doi: 10.3928/01477447-20070401-10. [DOI] [PubMed] [Google Scholar]
- 2.Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: the Morel-Lavallee lesion. J Trauma. 1997;42:1046–51. doi: 10.1097/00005373-199706000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Carlson DA, Smmons J, Sando W, et al. Morel-Lavalee lesions treated with debridement and meticulous dead space closure: surgical technique. J Orthop Trauma. 2007;21:140–4. doi: 10.1097/BOT.0b013e31802f19ca. [DOI] [PubMed] [Google Scholar]
- 4.Harma A, Inan M, Ertem K. The Morel-Lavallée lesion: a conservative approach to closed degloving injuries. Acta Orthop Traumatol Turc. 2004;38:270–3. [PubMed] [Google Scholar]
- 5.Tseng S, Tornetta P., III Percutaneous management of Morel-Lavallee lesions. J Bone Joint Surg Am. 2006;88:92–6. doi: 10.2106/JBJS.E.00021. [DOI] [PubMed] [Google Scholar]