Abstract
Objective
This study aimed to understand the dyadic relationships between family communication and quality of life (QOL) and between coping and QOL in Chinese- and Korean-American breast cancer survivor (BCS)-family member dyads.
Methods
A cross-sectional survey design was used. A total of 32 Chinese- and Korean-American BCS-family member dyads were recruited from the California Cancer Surveillance Program and area hospitals in Los Angeles County, California, United States. The dyadic data were analyzed using a pooled regression actor-partner interdependence model.
Results
The study findings demonstrated that the survivors’ general communication and use of reframing coping positively predicted their own QOL. The survivors’ and family members’ general communication was also a strong predictor of the family members’ physical-related QOL score specifically. Meanwhile, each person’s use of mobilizing coping negatively predicted his or her partner’s QOL.
Conclusions
The study findings add important information to the scarce literature on the QOL of Asian-American survivors of breast cancer. The findings suggest that Chinese- and Korean-American BCS and their family members may benefit from interventions that enhance communication and coping within the family unit.
INTRODUCTION
The improved survival rate for breast cancer [1] has stimulated interest in quality of life (QOL) because breast cancer survivors (BCS) still suffer from physical and psychological concerns for an extended period [2, 3]. In the scarce literature on the QOL experiences of Asian-American BCS, previous studies documented that Chinese- and Korean-American BCS expressed lower QOL than European Americans [4-6]. Chinese- and Korean-Americans differ somewhat in culture, language, historical experiences, and immigration patterns [7]. Nevertheless, as the largest and fastest growing Asian-American subpopulations in the United States [8], these groups have considerable similarities in their immigration characteristics and cultural values. For example, the main reasons both groups reported for immigrating to the United States were to pursue a better life for themselves and their families [9, 10]. They also share similar cultural and family values arising from Confucianism and Familism [11-13]. Thus the current study combines these two groups to investigate the dyadic relationship of family communication and coping on quality of life (QOL) among BCS-family member dyads.
During the adjustment to breast cancer, family members may have a primary influence on the QOL of BCS [14]; thus cancer is frequently recognized as a family disease [15]. Communication and coping within the family specifically may influence how BCS or family members respond to emotional distress and concerns during the survivorship period; these responses, in turn, influence QOL [16-20]. Family communication is defined as messages that are typically sent with intent and that have consensually shared meaning among individuals who are related biologically, legally, or through marriage-like commitments [21]. Several studies have demonstrated that sharing information about their illness, its consequences, and their thoughts and feelings with family members is related to their positive adjustment, increased cohesion, lower mood disturbance, and better QOL [22-25]. Studies also have shown that cancer patients who hold back emotions and concerns report higher levels of psychological distress, lower emotional well-being, and lower QOL [26-29]. Generally, family coping refers to the set of cognitive and behavioral strategies used by family members to manage shared distress within the family [25]. Adaptive coping strategies (e.g., problem-solving) have been shown to be associated with decreased psychological distress, increased psychological and physical health, improved QOL, and positive health behavior changes [30-32], whereas maladaptive coping strategies (e.g., avoidance) are associated with higher levels of distress, poorer adjustment to diagnosis and treatment, and decreased QOL [33-35].
Chinese and Korean cultures might influence the communication and coping between BCS and their family members [36]. Belonging to cultures with a Confucianism tradition [37], Chinese and Koreans have learned that a person’s maturity is related to the ability to control one’s feelings or emotions [38]. Confucianism also teaches that “silence is golden.” This teaching suggests that many Chinese- and Korean-Americans may be comfortable with moments of prolonged silence throughout their chores and daily activities and may be discouraged from seeking help from outside the family [39, 40]. Individuals who do not have skills to communicate about and cope with cancer, however, may face increased risks for poor QOL and family instability [27, 41]. Furthermore, the mutual coping strategies and communication skills within the family may create interaction effects on everyone’s QOL given that the family members tend to react to disease as a unit [42]. In view of the tradition of Familism, all values are determined based on how things are favorable for the functioning of the family [43], such that an individual cannot become independent of the family due to the strongly tied family bond [44].
The current study aimed to understand the dyadic relationships between family communication and QOL and between family coping and QOL in Chinese- and Korean-American BCS-family member dyads. Because no studies have investigated whether Chinese-and Korean-American BCS’ and family members’ communication and coping abilities contribute to the survivors’ own and their partners’ QOL, this study utilized small samples for the purpose of exploring the dyadic associations as a pilot study. Based on the actor-partner interdependence model (APIM) [45], the current study analyzed dyadic data to test the following research questions:
Are the actor effects (i.e., the estimate of an individual’s impact on herself or himself) of family communication and coping on QOL significant?
Are the partner effects (i.e., the degree to which a person’s outcome is influenced by the partner’s score on the predictor variable) of family communication and coping on QOL significant?
METHODS
Study Design and Participants
The present study is a secondary analysis of data gathered for a descriptive and cross-sectional methodology with the use of both quantitative (157 survivors and 32 family members) and qualitative methods (32 dyads) [46, 47]. A total of 32 BCS-family member dyads who completed the survey section participated in this study. Preliminary analysis demonstrated that the selected BCS are not different from the total of 157 BCS in terms of demographic and medical characteristics [47]. Originally, BCS were included if they met the following criteria: 1) aged 18 years or older at diagnosis; 2) diagnosed with breast cancer (Stage I-III) within the previous 1-5 years; 3) completed active treatment; 4) received no diagnosis of another type of cancer; 5) self-identified as Chinese American or Korean American; and 6) were able to speak Chinese, Korean, and/or English. Eligible family members included adults who met the following criteria: 1) living with a BCS; 2) being either the husband/partner, adult child, parent, or close friend of BCS; and 3) not diagnosed with any type of cancer. The family members were nominated by the BCS as an individual in their families who provided significant support and help. Here, the term ‘family member’ refers to the family members or close friends who are living in their household, regardless of relationships by blood or marriage, and is thus based on emotional distance and relationship.
Data Collection Procedures
BCS were drawn from the California Cancer Surveillance Program and area hospitals in Los Angeles County, California. After the invitation letters were mailed, initial telephone contacts with potential participants were conducted for eligibility screening. During the screening process, BCS were asked their opinions regarding family members’ study participation. Eligible participants were mailed a questionnaire and consent form in their preferred language.
After finalizing the recruitment of BCS, stratified random sampling was employed to select a certain number of family members for all BCS who agreed to the family member’s participation in a focus group study. As the stratification, BCS’ mean score on the family communication scale was used to evenly include subsamples that have open and closed communication patterns within the population. A recruitment letter was mailed to the nominated family members. If they were interested in participating in this study, a brief telephone screening was conducted to assess their eligibility. Family members who agreed to participate in both the survey and focus groups were included. The family members were asked to complete the questionnaire face-to-face prior to the focus group. A $40 grocery gift certificate was given to the participants as compensation. The recruitment procedures were approved by the Case Western Reserve University and the City of Hope Institutional Review Boards. In this paper, only the survey study is included.
Instruments
A rigorous “forward-backward” translation procedure was used to ensure that the English versions of the questionnaires were equivalent to the Chinese and Korean versions. Details regarding the instrument development, translation, and equivalency testing are reported elsewhere [47]. In this study, the internal consistency of the scales ranged from 0.67 to 0.97 for the Chinese version and from 0.72 to 0.97 for the Korean version, except for the passive appraisal subscale in the family coping (Table 2). The passive appraisal subscale was not reliable for Korean survivors specifically, indicating very low reliability (α=0.178). Hence, the passive appraisal subscale was dropped from further analyses. Preliminary analysis demonstrated no major differences in demographics, medical characteristics or outcomes as a result of the language of administration [47].
Table 2.
Differences in Variables between Survivors and Families
| Variables | Cronbach’s α | Range, Mean (SD) | F a | t b | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Chinese | Korean | Survivor | Family | |||
|
| ||||||
| Communication | ||||||
| General | 0.97 | 0.96 | 2-5, 3.8(0.9) | 1-5, 3.9(0.98) | 0 | −0.62 |
| Cancer-related | 0.97 | 0.97 | 1-5, 4.0(1.2) | 1-5, 3.8(1.15) | 0.1 | 0.89 |
|
| ||||||
| Family Coping | ||||||
| Social support | 0.81 | 0.91 | 10-42, 19.5(7.9) | 10-41, 22.7(7.9) | 0.27 | −2.09* |
| Mobilizing | 0.72 | 0.72 | 5-17, 9.4(3.5) | 4-20, 10.3(3.5) | 0.06 | −1.15 |
| Spiritual support | 0.87 | 0.85 | 3-20, 12.7(5.7) | 4-20, 13.4(4.5) | 3.91 | −0.76 |
| Reframing | 0.86 | 0.85 | 14-38, 26.0(7.0) | 13-40, 28.4(6.9) | 0.16 | −1.74 |
|
| ||||||
| Quality of Life | ||||||
| Physical Functioning | 0.92 | 0.86 | 8-100, 64.3 (29.8) | 8-100, 88.3(21.7) | 3.3 | −4.14*** |
| Role-Physical | 0.83 | 0.96 | 0-100, 48.4 (42.3) | 0-100, 79.8(36.8) | 1.57 | −3.03** |
| Pain | 0.81 | 0.86 | 23-100, 64.4 (22.5) | 10-100, 81.5(22.2) | 0.09 | −4.12*** |
| General Health | 0.7 | 0.8 | 15-100, 54.6 (19.8) | 10-100, 64.2(21.4) | 1.14 | −2.11* |
| Energy | 0.67 | 0.82 | 35-100, 59.0 (16.1) | 10-100, 53.3(22.6) | 3.29 | 1.02 |
| Social Functioning | 0.71 | 0.77 | 25-100, 66.4 (25.3) | 38-100, 80.1(21.0) | 2.24 | −3.09** |
| Role-Emotional | 0.83 | 0.89 | 0-100, 55.6 (45.8) | 0-100, 76.7(39.3) | 3.29 | −2.03 |
| Mental Health | 0.89 | 0.87 | 24-100, 69.2 (19.5) | 4-100, 55.5(25.7) | 2.66 | 2.48* |
| Physical QOL | - | - | 24-94, 57.9 (21.7) | 26-100, 78.1(21.2) | 0.4 | −4.32*** |
| Mental QOL | - | - | 27-100, 61.9 (21.2) | 27-100, 66.2(19.8) | 0.93 | −0.99 |
Note Levene’s test for equality of variance,
paired sample t-tests were conducted.
p<0.05,
p<0.01,
p<0.001
Quality of Life
The Medical Outcome Study (MOS) SF-36 was used to assess QOL for both BCS and family members [48]. This 36-item instrument contains eight multi-item subscales: 1) physical functioning, 2) physical role limitation, 3) pain, 4) general health, 5) vitality, 6) social functioning, 7) emotional role limitation, and 8) mental health. These eight subscales are comprised of two summary scores: the Physical Component Summary (PCS) and the Mental Component Summary (MCS). Subscale scores are computed by summing items in the same scale and then transforming raw scale scores to a range from 0 to 100. Each summary score was calculated by averaging the standardized scores of the corresponding subscales and used as outcomes in this study. Higher scores represent higher QOL.
Family Communication
Two communication scales addressing general communication and cancer-related communication were used to assess communication within the family. First, the Family Adaptability and Cohesion Evaluation Scales (FACES IV)–Family Communication Scale, which was designed to investigate ways to communicate with family members in daily life (i.e., listening, expression), was employed to assess general communication (referred to as general communication) [49]. This 10-item scale is rated on a 5-point Likert scale and computed by averaging all items. Higher scores indicate better general communication.
Cancer-related communication was assessed using the Family Avoidance of Communication About Cancer (FACC) Scale, which was developed to assess ways to communicate about the cancer experience with family members (i.e., discouraged, upset) and attitudes toward such communication (referred to as cancer-related communication) [50]. Five items are measured on a 5-point Likert scale. Each item was reverse scored and the total subscale score was computed by averaging the items. Higher scores reflect better cancer-related communication.
Family Coping
The Family Crisis Oriented Personal Evaluation Scales (F-COPES) was used to assess family coping [51]. The F-COPES is a self-report measure designed to identify coping strategies families use when they face problems or a crisis. This 29-item scale consists of five subscales: 1) acquiring social support (the family’s use of emotional and tangible support from extended family, friends, and neighbors; 9-item); 2) mobilizing the family to acquire and accept help (the family’s use of community resources to cope with their problems; 4-item); 3) seeking spiritual support (the family’s use participation in and emotional support acquired from their church; 4-item); 4) reframing (the family’s ability to redefine stress/situations; 8-item); and 5) passive appraisal (the family’s inactive coping style in managing problems; 4-item). The respondent rated the items on a 5-point Likert scale. The subscale scores were obtained by summing the responses to all items. Higher scores indicate more effective coping behavior.
Data Analyses
Exploratory data analyses were conducted to describe the participants’ characteristics. A chi-squared test was conducted to determine whether there were significant differences in demographic and medical characteristics between Chinese- and Korean-Americans to justify their combination in the analysis. The paired sample t-test was then conducted to investigate the mean differences in variables between survivors and family members. Pearson correlations among variables between BCS and family members were also conducted.
The type of survivor-family member dyads in this study was considered “distinguishable dyads,” in which members are distinguishable by a meaningful characteristic (i.e., survivor vs. family member). Generally, data from family members are considered non-independent because each family member is likely to influence the feelings, attitudes, and behaviors of the other family members. Given that traditional research methods (i.e., regression) are inadequate for dyadic data due to violations of independence assumptions and inaccurate statistics for non-independent data [35], the APIM [45, 52], which addresses many methodological problems related to dyadic data, was used for survivor-family member dyads as the unit of analysis.
The current study used a pooled regression APIM technique that is appropriate for smaller sample sizes [52]. Prior to major analyses, the homogeneity of variance across levels of the distinguishing variable was tested to examine whether the assumption of the pooled regression technique for distinguishable dyads was met. Using the pooled regression approach to estimate the APIM, two regression equations (one for the within-dyad effects of the predictor variable and the other for the between-dyad effects) are estimated, and the results are pooled together to obtain the actor effect, partner effect, and associated parameters for each predictor variable [45, 52]. Here, a variable related to the role (survivor or family member) and the interaction between the role variable and the other predictor was included in all of the analyses to explore potential role differences (survivors=1, family members=−1). The within-dyad and between-dyads regression equations are shown in Equations 1 and 2 [52], respectively.
| (1) |
| (2) |
Definition of Symbols:
DVdiff = the difference between each partner’s scores on the outcome variable
IVdiff = the difference between each partner’s scores on the predictor variable
Rdiff = the difference between each partner’s scores on the role (sick/caregiving role)
IVINdiff = the difference in the interaction between the predictor variable and role
DVavg = the dyad mean of the outcome variable
IVavg = the dyad mean of the predictor variable
IVINavg = the dyad average of the interaction between the predictor variable and role
bwn = unstandardized regression coefficients for the within-dyads regression
bbn = unstandardized regression coefficients for the between-dyads regression
Ewi = error term for the within-dyads regression
Ebi = error term for the between-dyads regression
The regression coefficients from these two equations were then used to estimate the actor and partner effects for each of the mixed predictor variables, as in Equation 3 [52].
| (3) |
Finally, t statistics with degrees of freedom were used to determine whether these actor and partner effects differed significantly from zero using the pooled standard errors. All analyses were conducted using SPSS 20.0 and computed manually. All hypotheses were tested with a p<0.05 criterion of significance for a two-sided test.
RESULTS
Sample Characteristics
A total of 32 BCS-family member dyads completed the survey. More Chinese-Americans (n=18) than Korean-Americans (n=14) participated in this study, but the Chinese- and Korean-American BCS did not differ significantly on any demographic or medical characteristics. For the family members, only the relationship with BCS varied significantly, indicating that more husbands of Korean-Americans participated than Chinese-Americans (see Table 1). Thus, this study combined Chinese- and Korean-Americans as one group in subsequent data analyses.
Table 1.
Demographic and Medical Characteristics of Samples (32 Dyads)
| N (%) | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Variables | Survivors | Family | ||||
|
| ||||||
|
Chinese
(n=18) |
Korean
(n=14) |
Total |
Chinese
(n=18) |
Korean
(n=14) |
Total | |
|
| ||||||
| Relationshipa | ||||||
| Wife/Husband | 7(38.9) | 12(85.7) | 19(59.4) | 19(59.4) | 12(85.7) | 19(59.4) |
| Mother/Daughter | 4(22.2) | 2(14.3) | 6(18.8) | 6(18.8) | 2(14.3) | 6(18.8) |
| Others | 7(38.9) | 0 | 7(21.9) | 7(21.9) | 0 | 7(21.9) |
| Education | ||||||
| <High school | 4(22.2) | 0 | 4(12.5) | 2(11.1) | 2(11.1) | 3(9.4) |
| High school graduated | 3(16.7) | 1(7.1) | 4(12.5) | 2(11.1) | 2(11.1) | 6(18.8) |
| >High school | 11(61.1) | 13(92.9) | 24(75.0) | 14(77.8) | 14(77.8) | 23(71.9) |
| Household income | ||||||
| <25K | 8(60.0) | 4(28.6) | 12(37.5) | 5(33.3) | 1(7.7) | 6(18.8) |
| 25K–45K | 3(18.8) | 2(14.3) | 5(15.6) | 7(46.7) | 5(38.5) | 12(37.5) |
| 45K–75K | 3(18.8) | 5(35.7) | 8(25.0) | 0 | 4(30.8) | 4(12.6) |
| >75K | 2(12.5) | 3(21.4) | 5(15.6) | 3(20.0) | 3(23.1) | 6(18.8) |
| Marital Status | ||||||
| Married | 13(72.2) | 12(85.7) | 25(78.1) | 11(61.1) | 12(85.7) | 23(71.9) |
| Others | 5(27.8) | 2(14.3) | 7(21.9) | 7(38.9) | 2(14.3) | 9(28.1) |
| Employment Status | ||||||
| Employed | 8(50.0) | 8(57.1) | 16(53.3) | 12(80.0) | 14(100) | 26(89.6) |
| Un-employed | 8(50.0) | 6(42.9) | 14(46.7) | 3(20.0) | 0 | 3(10.3) |
| Primary language | ||||||
| Chinese/Korean | 17(94.4) | 14(100) | 31(96.9) | 17(94.4) | 11(91.7) | 30(93.8) |
| English | 1(5.6) | 0 | 1(3.1) | 1(5.6) | 1(7.7) | 2(6.2) |
| Cancer stage | ||||||
| 0 | 3(16.7) | 0 | 3(9.4) | |||
| I | 3(16.7) | 7(50.0) | 10(31.3) | |||
| II | 8(44.4) | 6(42.9) | 14(43.8) | |||
| III | 4(22.2) | 1(7.1) | 5(15.6) | |||
| Radiation(Yes) | 5(31.3) | 9(69.2) | 14(43.8) | |||
| Chemotherapy(yes) | 10(66.7) | 8(57.1) | 18(56.3) | |||
| Hormonal therapy(yes) | 11(68.8) | 7(50.0) | 18(56.3) | |||
|
| ||||||
| Mean(SD) | ||||||
|
| ||||||
| Age | 55.9(10.7) | 57.9(10.7) | 56.8(10.6) | 51.6(16.4) | 53.5(12.3) | 52.4(14.5) |
| Length of stay in the US | 19.3(10.5) | 23.1(7.9) | 20.9(9.5) | 17.1(8.9) | 24.2(7.5) | 20.4(8.9) |
| Years since diagnosis | 3.1(1.3) | 4.2(1.2) | 3.5(1.4) | |||
significant difference between Chinese and Korean survivors at p<0.05
As outlined in Table 1, the mean ages of BCS and family members were 57 (SD=10.6) and 52 years (SD=14.5), respectively. Nineteen husbands, six daughters, and seven others (siblings or friends) participated as family members. The majority of BCS and family members had completed either high school or college (87.5% of BCS and 90.7% of family members) and were married (78.1% of BCS and 71.9% of family members). Approximately 40% of survivors reported an annual household income of under $25,000. Nearly half of survivors were currently employed, whereas approximately 90% of family members were employed. Most respondents used their native language as a primary language. The length of residence in the United States for both BCS and family members was approximately 20 years. The average number of years since cancer diagnosis was 3.5 (SD=1.4), and approximately 40% of the participants were diagnosed with Stage II cancer (Table 1).
Preliminary Analyses
As shown in Table 2, BCS and family members did not show significant differences in variances of predictor and outcome variables, supporting the assumption of homogeneity of variance. The paired-sample t-test demonstrated that neither the general nor the cancer-related communication scores revealed significant differences between BCS and family members. Regarding family coping, the acquiring social support coping subscale showed significant differences between BCS and family members (t=−2.09, p<0.05); the family members were more likely than BCS to use acquiring social support. In the QOL, family members showed a better PCS score than did BCS (t=−4.32, p<0.001), whereas the MCS score did not show significant differences. Of the eight QOL subscales, six significantly varied between BCS and family members. This finding indicates that family members are more likely than BCS to have better PCS; however, on the mental health subscale, BCS expressed a better outcome than did their family members.
As indicated in Table 3, the bivariate correlations between BCS and family members were low for QOL and moderate for most predictors. The within-dyad correlation was relatively high for QOL compared with the correlations for predictors.
Table 3.
Pearson Correlations between Study Variables
| 1.PCS | 2.MCS | 3.general com | 4.cancer com |
5.FC-social support |
6.FC- mobilizing |
7.FC-spiritual support |
8.FC -reframing |
|
|---|---|---|---|---|---|---|---|---|
| 1 | .24 | .74*** | .40* | .05 | .07 | .19 | .33 | .36* |
| 2 | .74*** | .28 | .45** | .31 | .26 | .15 | .57** | .52** |
| 3 | .30 | .44* | .54** | .26 | .32 | .13 | .03 | .51** |
| 4 | .08 | .13 | .03 | .58** | −.15 | −.07 | .45** | .19 |
| 5 | −.16 | −.11 | .46** | −.27 | .45* | .69*** | .07 | .67*** |
| 6 | −.10 | −.21 | .40* | −.35 | .79*** | .27 | −.05 | .52** |
| 7 | .60 | .06 | .29 | .06 | .34 | .35 | .60*** | .41* |
| 8 | .40* | .40* | .44* | .07 | .30 | .40* | .60*** | .39* |
Note. Survivors above, families below, and between survivors and families along the diagonal;QOL=quality of life;com=communication;FC=family coping.
p<0.05,
p<0.01,
p<0.001.
Research Question 1: Actor Effects of Family Communication and Coping on QOL
The actor effects between general communication and PCS for both survivors (t=4.40, p<0.001) and family members (t=2.47, p<0.05) proved significant (Table 4). This indicates that the use of more effective communication within the family in daily life was related to an increase of one’s own PCS score for both BCS and family members. In the relationships between mobilizing (t=2.69, p<0.05) and reframing coping (t=2.34, p<0.05) and PCS, the actor effects were positive for survivors only, i.e., the increased use of own mobilizing or reframing coping strategy was associated with increasing their own physical-related QOL.
Table 4.
A Pooled Regression Actor-Partner Interdependence Model
| Variables | Survivor Actor effect |
Family Actor effect |
Survivor Partner Effect |
Family Partner Effect |
|
|---|---|---|---|---|---|
|
|
|||||
| Unstandardized Estimates | |||||
| Physical QOL | |||||
|
| |||||
| General communication | 4.40*** | 2.47* | −1.88 | 2.84* | |
| Cancer communication | 0.06 | 1.10 | 0.44 | 2.35+ | |
| Social support | 0.76 | −0.26 | −0.50 | −0.98 | |
| Family coping |
Mobilizing | 2.69* | −0.40 | −1.86 | −2.65* |
| Spiritual support | 1.71 | −0.18 | 0.15 | −0.18 | |
| Reframing | 2.34* | −1.38 | 1.73 | −0.94 | |
|
| |||||
| Mental QOL | |||||
|
| |||||
| General communication | 4.43** | 1.26 | −0.91 | 1.39 | |
| Cancer communication | 0.88 | −0.20 | 2.18+ | 1.83 | |
| Family coping |
Social support | 2.63* | 0.38 | −1.21 | −0.54 |
| Mobilizing | 2.20+ | −0.12 | −2.41* | −2.65* | |
| Spiritual support | 3.87** | 0.39 | −0.44 | 0.25 | |
| Reframing | 4.03** | −1.21 | 1.10 | −1.16 | |
p<0.1,
p<0.05,
p<0.01,
p<0.001.
For MCS, general communication (t=4.43, p<0.01), as well as acquiring social support (t=2.63, p<0.05), seeking spiritual support (t=3.87, p<0.01), and reframing coping strategies (t=4.03, p<0.01) had positive actor effects for survivors. That is, survivors who had better scores for general communication or used acquiring social support, seeking spiritual support, or reframing coping strategy increased their own mental-related QOL. However, family member actor effects of family communication and coping on MCS were not observed. Thus, for research question 1, 8 out of a total of 24 possible relationships were significant in the expected direction.
Research Question 2: Partner Effects of Family Communication and Coping on QOL
The survivor-partner effect was not observed in PCS. For the family-partner effects, however, two relationships were significant: 1) general communication and PCS (t=2.84, p<0.05), and 2) mobilizing coping and PCS (t=−2.65, p<0.05). That is, survivors who had better scores for general communication increased their family members’ PCS. The survivors’ use of mobilizing coping was associated with the family members’ lower PCS score.
In terms of MCS, mobilizing coping showed both the survivor- (t=−2.41, p<0.05) and family-partner effects (t=−2.65, p<0.05). This indicates that the family members’ use of mobilizing coping was related to the survivors’ lower MCS score, and the survivors’ use of mobilizing coping was also associated with the family members’ lower mental-related QOL. Other predictors did not show any survivor- or family partner effects on mental QOL. Nevertheless, the survivor- and the family-partner effects of cancer-related communication on mental and physical QOL, respectively, were marginally significant; this finding indicates that individuals whose partners have better communication about the cancer experience within the family may have better physical or mental QOL. For research question 2, 4 out of a total of 24 possible relationships were significant in the expected direction.
DISCUSSION
The present study aimed to understand the dyadic relationships between family communication and coping and QOL for BCS-family member dyads within Chinese- and Korean-American cultural contexts. The study findings demonstrated that 1) the survivors’ general communication and use of reframing coping positively predicted their own QOL; 2) the survivors’ and family members’ general communication was a strong predictor of the family members’ PCS score specifically; and 3) each person’s use of mobilizing coping negatively predicted his or her partner’s QOL.
A pooled regression approach to the APIM is known to be an appropriate approach for analyzing dyadic data with smaller samples [52], although most types of dyadic analyses require large samples. The benefit of a pooled regression approach is that researchers can examine actor and partner effects while accounting for the interdependence between couples, resulting in accurate statistical inferences with small samples [45]. Considering that cancer survivorship studies targeting Asian-Americans tend to recruit small samples because of recruitment challenges [2], the use of this approach is meaningful in that researcher-practitioners may have an opportunity to learn more about Asian-American dyadic samples.
First, this study found that BCS’ and family members’ levels of general communication within the family were associated with their own QOL, consistent with the results of previous studies for mostly White populations [50, 53, 54]. This implies that individuals’ ability to effectively communicate and manage general concerns within the family can improve QOL for both those who are surviving breast cancer and their family members. Generally, it is known that Asian cultures tend to discourage discussing concerns in public and within the family [38, 46]. Nevertheless, we should not overlook the possibility that Chinese- and Korean-Americans’ values may be gradually changing to adjust to everyday life within their host country and adopting Western cultural norms. Thus, open communication within the family may be more beneficial to improving QOL than retaining such cultural values as closed communication. The current study suggests that the use of effective communication among family members may maximize QOL for Chinese- and Korean-American BCS and their family members.
The current study also confirmed that having positive thoughts and feelings when coping with family concerns may play a key role in improving QOL for Chinese- and Korean-American BCS, consistent with previous studies [55, 56]. This reflects that the collectivist values that Asian culture emphasizes (e.g., seeking harmony) are still at work when dealing with concerns and problems within the family. However, the family actor effect was not observed in the relationship between reframing coping and QOL, indicating that the family members’ positive thoughts and feelings are not helpful in improving their QOL. This may imply that positive thoughts do not offer any practical solutions to deal with their problems or distress for family members. Furthermore, in the current study, there was no evidence of actor effects in the relationship between family coping and QOL for family members. Generally, family members provide informal cancer care that meets the survivors’ multidimensional needs [57] such that they may have an additional burden, i.e., the obligation that they must meet the survivors’ demands. Hence, other survivor-related factors beyond the use of family members’ coping strategies may be necessary to influence family members’ QOL.
In terms of the partner effects, findings regarding the effect of mobilizing coping on QOL are not consistent with findings from other studies [21, 23]. That is, the use of active coping strategies produced favorable outcomes [21]. However, such previous findings might not be applicable to Asian culture. For example, people in Asian cultures may be reluctant to request and accept help from someone outside the family given the values associated with Confucianism [11, 13, 58] and Collectivism [59-61]. It is also possible that our samples did not have enough resources to request assistance in solving their problems because of limited social networks and cultural and language barriers [62]. Thus, mobilizing the family to acquire and accept help may cause side effects of repressing their emotions. Further investigation aimed at understanding the role of mobilizing coping on QOL within the Asian culture is needed.
Meanwhile, the current study did not find significant relationships between the QOL of the BCS and their family members. Such a finding is inconsistent with previous studies for mostly White populations [22, 63, 64]. Although this finding is surprising in view of the Familism in Asian populations, the other finding regarding general communication and the Confucianism tradition may provide tips to better understand their relationships. One possible explanation is that family members do not openly discuss their concerns or stressors to keep the family in harmony, thus the extent to which survivors and family members perceive quality of life may be different. Additionally, methodological issues such as sample size, the extended definition of family members, and broad criteria of samples might influence outcomes. Future studies are required to further investigate dyadic relationships of QOL with large Asian populations.
Finally, this study observed no evidence that actor effects of cancer-related communication on QOL exist. However, individuals whose partners did not avoid talking about the cancer, although it was marginally significant, had better QOL, indicating a potential partner effect of cancer-related communication on QOL. This suggests that open communication about cancer within the family system may be associated with family stability, which, in turn, may influence partners’ QOL because the mutual understanding of cancer can help to improve both the survivor’s and the family’s adjustment to cancer [53]. Therefore, this finding implies that the development and implementation of cancer-related communication intervention within the family may be useful for improving QOL, especially when accompanied by psychosocial care to help BCS and family members develop effective communication practices.
Several limitations of this study should be noted. First, this study relied on a cross-sectional survey design; therefore, causality between variables should not be assumed. Additionally, the majority of the study questions were asked retrospectively using self-report instruments; concerns about definitive causal interpretations should be addressed with prospective longitudinal data. Second, this study is limited because of its small sample size. Although this study satisfied the recommended minimum sample size (n=28 dyads) for conducting a pooled regression approach [52], a potential reason that some effects were not statistically significant from zero may be related to the small sample size [52]. The results may also not be generalizable to Chinese- and Korean-American BCS or to other Asian-American populations. Future studies are needed with other Asian-American subpopulations. Finally, the eligibility criteria of survivors and family members were quite broad. Given that communication style and contents specifically can vary depending on whom one is communicating with, the results should be interpreted with caution. The effect of communication on QOL by relationships with each family member needs to be further investigated.
Despite these limitations, our investigation delivers important messages related to the positive roles of general and cancer-related communication and reframing coping and the negative role of mobilizing coping on improving QOL in Asian cultures. Our findings suggest that BCS and their family members may benefit from interventions that enhance communication and coping for Asian families. BCS and their family members who show maladjustment or poor QOL may also benefit from prompt psychosocial interventions at either the individual, dyadic, or family level, which can ultimately improve QOL for BCS-family member dyads.
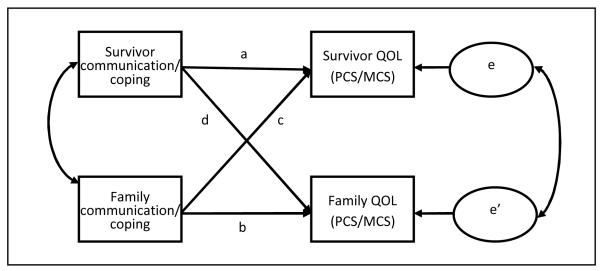
Figure 1. The Effects of Family Coping and Communication on QOL.
Note. a=survivor actor effect; b=family actor effect; c=survivor-partner effect; d=family-partner effect; PCS=Physical component summary; MCS=Mental component summary; predictors include communication (i.e., general and cancer-related communication) and family coping (i.e., acquiring social support, mobilizing the family to acquire and accept help, seeking spiritual support, and reframing).
Acknowledgements
Funding for this research was supported by a grant from the National Institutes of Health, National Cancer Institute (R03CA139941). The author also wishes to express gratitude for the support and assistance received from the following mentors, consultants, and assistants: Kimlin Ashing-Giwa, Kathleen Ell, Joseph Kim, Anjela Jo, Sophia Yeung, Okmi Baik, and Minso Paek.
REFERENCES
- 1.American Cancer Society . Breast Cancer Facts & Figures 2011-2012. American Cancer Society; Atlanta: 2011. [Google Scholar]
- 2.Ashing-Giwa KT, et al. Breast cancer survivorship in a multiethnic sample: Challenges in recruitment and measurement. Cancer. 2004;101(3):450–465. doi: 10.1002/cncr.20370. [DOI] [PubMed] [Google Scholar]
- 3.Ganz PA, et al. Quality of life in long-term, disease-free survivors of breast cancer: A follow-up study. Journal of the National Cancer Institute. 2002;94(1):39–49. doi: 10.1093/jnci/94.1.39. [DOI] [PubMed] [Google Scholar]
- 4.Ashing-Giwa KT, et al. Examining predictive models of HRQOL in a population-based, multiethnic sample of women with breast carcinoma Quality of Life Research. 2007;16(3):413–428. doi: 10.1007/s11136-006-9138-4. [DOI] [PubMed] [Google Scholar]
- 5.Lim J, Zebrack B. Different pathways in social support and quality of life between Korean American and Korean breast and gynecological cancer survivors. Quality of Life Research. 2008;17:679–689. doi: 10.1007/s11136-008-9343-4. [DOI] [PubMed] [Google Scholar]
- 6.Sun A, et al. Quality of life in Chinese patients with breast cancer. Cancer supplement. 2005;104(12):2952–2954. doi: 10.1002/cncr.21516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Srinivasan S, Guillermo T. Toward improved health: disaggregating Asian American and Native Hawaiian/Pacific Islander data. American Journal of Public Health. 2000;90(11):1731–1734. doi: 10.2105/ajph.90.11.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnes JS, Bennett CE. The Asian population: 2000. Census. 2000 brief, 2002. [Google Scholar]
- 9.Hurh W. The Korean-Americans. Greenwood Press; Westport, CT: 1998. [Google Scholar]
- 10.Lobo AP, Salvo JJ. Changing U.S. Immigration Law and the Occupational Selectivity of Asian Immigrants. International Migration Review. 1998;32(3):737–760. [PubMed] [Google Scholar]
- 11.Park M, Chesla C. Revisiting Confucianism as a conceptual framework for Asian family study. Journal of Family Nursing. 2007;13(3):293–311. doi: 10.1177/1074840707304400. [DOI] [PubMed] [Google Scholar]
- 12.Lee E. Chinese American families. Guilford; New York: 1997. Working with Asian Americans: A guide for clinicians; pp. 46–78. [Google Scholar]
- 13.Hyun KJ. Sociocultural change and traditional values: Confucian values among Koreans and Korean Americans. International Journal of Intercultural Relations. 2001;25(2):203–229. [Google Scholar]
- 14.Ashing-Giwa KT, et al. Understanding the breast cancer experience of Asian American women. Psycho-Oncology. 2003;12(1):38–58. doi: 10.1002/pon.632. [DOI] [PubMed] [Google Scholar]
- 15.Masten AS. Resilience in individual development: Successful adaption despite risk and adversity. In: Wang MC, Gorden EW, editors. Educational resilience in inner-city America. Hillsdale, NJ; Erlbaum: 1994. pp. 3–25. [Google Scholar]
- 16.Helgeson VS, Snyder P, Seltman H. Psychological and physical adjustment to breast cancer over 4 years: identifying distinct trajectories of change Health Psychology. 2004;23:3–15. doi: 10.1037/0278-6133.23.1.3. [DOI] [PubMed] [Google Scholar]
- 17.Stanton AL, Danof-Burg S, Huggins ME. The first year after breast cancer diagnosis: hope and coping strategies as predictors of adjustment. Psychooncology. 2002;11:93–102. doi: 10.1002/pon.574. [DOI] [PubMed] [Google Scholar]
- 18.Boyle DA. Survivorship. Clinical Journal of Oncology Nursing. 2006;10:407–416. [Google Scholar]
- 19.Sammarco A. Psychosocial stages and quality of life of women with breast cancer. Cancer Nursing. 2001;24:272–277. doi: 10.1097/00002820-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Friedman L, et al. Optimism, social support and psychosocial functioning among women with breast cancer. Psycho-Oncology. 2006;15(7):595–603. doi: 10.1002/pon.992. [DOI] [PubMed] [Google Scholar]
- 21.Kim J, et al. The role of social support and coping strategies in predicting breast cancer patients’ emotional well-being. Journal of Health Psychology. 2010;15(4):543–552. doi: 10.1177/1359105309355338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Giese-Davis J, et al. Quality of couples’ relationship and adjustment to metastatic breast cancer. Journal of Family Psychology. 2000;14:251–266. doi: 10.1037//0893-3200.14.2.251. [DOI] [PubMed] [Google Scholar]
- 23.Manne SL, et al. Cancer-related relationship communication in couples coping with early stage breast cancer. Psycho-Oncology. 2006;15:234–247. doi: 10.1002/pon.941. [DOI] [PubMed] [Google Scholar]
- 24.Manne SL, et al. Couples’ support-related communication, psychological distress, and relationship satisfaction among Women with early stage breast cancer. Journal of Consulting and Clinical Psychology. 2004;72(4):660–670. doi: 10.1037/0022-006X.72.4.660. [DOI] [PubMed] [Google Scholar]
- 25.Folkman S, Moskowitz JT. Coping: pitfalls and promise. Annual Review of Psychology. 2004;55:745–774. doi: 10.1146/annurev.psych.55.090902.141456. [DOI] [PubMed] [Google Scholar]
- 26.Ko C, et al. Problem-solving and distress in prostate cancer patients and their spousal caregivers. Supportive Care in Cancer. 2005;13(6):367–374. doi: 10.1007/s00520-004-0748-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Manne SL, Ostroff JS, Norton TR. Cancer-related relationship communication in couples coping with early stage breast cancer. Psychooncology. 2005;15:234–247. doi: 10.1002/pon.941. [DOI] [PubMed] [Google Scholar]
- 28.Mellon S, Northouse LL. Family survivorship and quality of life following a cancer diagnosis. Research in Nursing and Health. 2001;24(6):446–459. doi: 10.1002/nur.10004. [DOI] [PubMed] [Google Scholar]
- 29.Figueiredo MI, Fries E, Ingram KM. The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psychooncology. 2004;13:96–105. doi: 10.1002/pon.717. [DOI] [PubMed] [Google Scholar]
- 30.David D, Montgomery GH, Bovbjerg DH. Relations between coping responses and optimism-pessimism in predicting anticipatory psychological distress in surgical breast cancer patients. Pers Individ Dif. 2006;40(2):203–213. doi: 10.1016/j.paid.2005.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bellizzi KM, et al. Health behaviors of cancer survivors: Examining opportunities for cancer control interventions. Journal of clinical Oncology. 2005;23:8884–8893. doi: 10.1200/JCO.2005.02.2343. [DOI] [PubMed] [Google Scholar]
- 32.Stanton AL, et al. Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. Journal of Consulting and Clinical Psychology. 2000;68(5):875–882. [PubMed] [Google Scholar]
- 33.Roesch SC, et al. Coping with prostate cancer: A meta-analytic review. Journal of Behavioral Medicine. 2005;28:281–293. doi: 10.1007/s10865-005-4664-z. [DOI] [PubMed] [Google Scholar]
- 34.Wagner CD, Bigatti SM, Storniolo AM. Quality of life of husbands of women with breast cancer. psycho-Oncology. 2006;15:109–120. doi: 10.1002/pon.928. [DOI] [PubMed] [Google Scholar]
- 35.Cook WL, Kenny DA. The actor-partner interdependence model: a model of bidirectional effects in developmental studies. International Journal of Behavioral Development. 2005;29:101–109. [Google Scholar]
- 36.Liu J, Mok E, Wong T. Perceptions of supportive communication in Chinese patients with cancer: experiences and expectations. Journal of Advanced Nursing. 2005;52(3):262–270. doi: 10.1111/j.1365-2648.2005.03583.x. [DOI] [PubMed] [Google Scholar]
- 37.Chen GM, Starosta WI. Intercultural communication competence: A synthesis. Communication Yearbook. 1996;19:353–384. [Google Scholar]
- 38.Ritsner M, et al. Somatization in an immigrant population in Israel: a community survey of prevalence, risk factors, and help-seeking behavior. American Journal of Psychiatry. 2000;157(3):385–392. doi: 10.1176/appi.ajp.157.3.385. [DOI] [PubMed] [Google Scholar]
- 39.Kim MT. Cultural influences of depression experiences among Korean Americans. Journal of Psychosocial Nursing. 1995;33(2):13–18. doi: 10.3928/0279-3695-19950201-04. [DOI] [PubMed] [Google Scholar]
- 40.McCollaum B, Lester D. Locus of control, depression and suicidality in Korean workers. Psychological Reports. 1997;80:1282. doi: 10.2466/pr0.1997.80.3c.1282. [DOI] [PubMed] [Google Scholar]
- 41.Lewis FM. The effects of cancer survivorship on families and caregivers. American Journal of Nursing. 2006;106:20–21. doi: 10.1097/00000446-200603003-00008. [DOI] [PubMed] [Google Scholar]
- 42.Pakenham KI. Couple coping and adjustment to multiple sclerosis in care receiver– carer dyads. Family Relations: An Interdisciplinary Journal of Applied Family Studies. 1998;47(3):269–277. [Google Scholar]
- 43.Kulp D. Community life in South China. MacMillan; NY: 1929. [Google Scholar]
- 44.Lim JW, O’Keefe M. Social problems and service needs in a Korean American community: Perceptions of residents and community leaders. Journal of Ethnic and Cultural Diversity in Social Work. 2009;18(2) [Google Scholar]
- 45.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. Guilford Press; New York, NY: 2006. [Google Scholar]
- 46.Lim JW, Ashing-Giwa K. Is family functioning and communication associated with health-related quality of life for Chinese- and Korean-American breast cancer survivors? Quality of Life Research. 2012 doi: 10.1007/s11136-012-0247-y. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lim JW, Townsend A. Cross-ethnicity measurement equivalence of family coping for breast cancer survivors. Research on Social Work Practice. 2012 in press. [Google Scholar]
- 48.Ware JE, et al. SF-36 health survey: manual and interpretation guide. Health Institute, New England Medical Center; Boston: 1993. [Google Scholar]
- 49.Olson DH, Gorall DM, Tiesel JW. FACES IV Package. Life Innovations; Minneapolis, MN: 2004. [Google Scholar]
- 50.Mallinger JB, Griggs JJ, Shields CG. Family communication and mental health after breast cancer. European Journal of Cancer. 2006;15:355–361. doi: 10.1111/j.1365-2354.2006.00666.x. [DOI] [PubMed] [Google Scholar]
- 51.McCubbin HI, Larsen A, Olson DH. Family crisis orientated personal evaluation scales (F COPES) In: McCubbin HI, Thompson AI, editors. Family assessment inventories for research and practice. University of Wisconsin-Madison; Madison, WI: 1987. pp. 193–207. [Google Scholar]
- 52.Tambling RB, Johnson SK, Johnson LN. Analyzing dyadic data from small samples: a pooled regression actor-partner interdependence model approach. Counseling Outcome Research and Evaluation. 2011;2(2):101–114. [Google Scholar]
- 53.Zhang AY, Siminoff LA. Silence and cancer: why do families and patients fail to communicate? Health Communication. 2003;15(4):415–429. doi: 10.1207/S15327027HC1504_03. [DOI] [PubMed] [Google Scholar]
- 54.Bodenmann G. Dyadic coping and its significant for marital functioning. In: Revenson T, Kayser K, Bodenmann G, editors. Couples coping with stress: emerging perspectives on dyadic coping. American Psychological Association; Washington DC: 2005. pp. 33–50. [Google Scholar]
- 55.Coutu D. How resilience works. Harvard Business Review. 2002 May;:46–55. [PubMed] [Google Scholar]
- 56.Everall R, Altrows J, Paulson B. Creating a future: A study of resilience in suicidal female adolescents. Journal of Counselling and Development. 2006;84:461–470. [Google Scholar]
- 57.Hodgkinson K, et al. Life after cancer: couples’ and partners’ psychological adjustment and supportive care needs. Support Care Cancer. 2007;15(4):405–15. doi: 10.1007/s00520-006-0148-0. [DOI] [PubMed] [Google Scholar]
- 58.Suen H, Cheung S, Mondejar R. Managing ethical behaviour in construction organizations in Asia: How do the teachings of Confucianism, Taoism and Buddhism and Globalization influence ethics management? International Journal of Project Management. 2007;25(3):257–265. [Google Scholar]
- 59.Leung K, Koch PT, Lu L. A Dualistic Model of Harmony and its Implications for Conflict Management in Asia. Asia Pacific Journal of Management. 2002;19(2):201–220. [Google Scholar]
- 60.Merkin RS. Cross-cultural communication patterns: Korean and American communication. Journal of Intercultural Communication Research. 2009:20. [Google Scholar]
- 61.Hara K, Kim M. The effect of self-construals on conversational indirectness. International Journal of Intercultural Relations. 2004;28(1):1–18. [Google Scholar]
- 62.Lim J, Yi J, Zebrack B. Acculturation, social support, and quality of life for Korean immigrant breast and gynecological cancer survivors. Ethnicity & Health. 2008;13(5):1–18. doi: 10.1080/13557850802009488. [DOI] [PubMed] [Google Scholar]
- 63.Mellon S, Northouse L, Weiss LK. A population-based study of the Quality of Life of cancer survivors and their family caregivers. Cancer Nursing. 2006;29(2):120–131. doi: 10.1097/00002820-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 64.Northouse L, Templin T, Mood D. Couples’ adjustment to breast disease during the first year following diagnosis. J Behav Med. 2001;24:115–136. doi: 10.1023/a:1010772913717. [DOI] [PubMed] [Google Scholar]