Abstract
Background:
Epithelial–mesenchymal transition (EMT) is characterised by the loss of cell-to-cell adhesion and gaining of mesenchymal phenotypes. Epithelial–mesenchymal transition is proposed to occur in various developmental processes and cancer progression. ‘Cadherin switch', a process in which cells shift to express different isoforms of the cadherin transmembrane protein and usually refers to a switch from the expression of E-cadherin to N-cadherin, is one aspect of EMT and can have a profound effect on tumour invasion/metastasis. The aim of this study was to investigate the clinicopathological significance of EMT-related proteins and cadherin switch in extrahepatic cholangiocarcinoma (EHCC).
Methods:
We investigated the association between altered expression of 12 EMT-related proteins and clinical outcomes in patients with EHCC (n=117) using immunohistochemistry on tissue microarrays.
Results:
Univariate and multivariate analyses revealed that, in addition to N classification (P=0.0420), the expression of E-cadherin (P=0.0208), N-cadherin (P=0.0038) and S100A4 (P=0.0157) was each an independent and a significant prognostic factor. We also demonstrated that cadherin switch was independently associated with poor prognosis (P=0.0143) in patients with EHCC.
Conclusions:
These results may provide novel information for selection of patients with EHCC who require adjuvant therapy and strict surveillance.
Keywords: EMT, extrahepatic cholangiocarcinoma, immunohistochemistry, tissue microarray, prognosis, survival, cadherin switch
Cholangiocarcinoma (CC) is a primary tumour originating from the bile duct epithelium and is classified as either intrahepatic or extrahepatic (Gandou et al, 2013; Aishima et al, 2014). As a result of the different embryological origins of extrahepatic and intrahepatic bile ducts, there may be the phenotypic diversity between extrahepatic and intrahepatic CC (Gandou et al, 2013). Extrahepatic CC (EHCC) is a highly malignant neoplasm, and the 5-year survival rate for patients who undergo surgical resection is reported to be only 20–40% (DeOliveira et al, 2007; Van der Gaag et al, 2012). Extrahepatic CC is a relatively uncommon disease with a reported incidence of 1–2 cases per 100 000 per year (Van der Gaag et al, 2012). The therapeutic gold standard for EHCC is complete resection of the tumour; however, local and distant recurrences occur in many patients after surgery (DeOliveira et al, 2007; Araki et al, 2011; Van der Gaag et al, 2012). Therefore, for such biologically aggressive EHCC, adjuvant therapy is often needed after surgical resection. For this reason, it is necessary to identify factors that can accurately predict outcomes in patients with EHCC.
Epithelial–mesenchymal transition (EMT) was first recognised as a central differentiation process in early embryogenic morphogenesis, and is characterised by loss of cell-to-cell junctions, specifically loss of epithelial phenotypes, and increased mobility due to cells gaining mesenchymal phenotypes (Thiery et al, 2009). The hallmark of EMT is downregulation of E-cadherin, an essential transmembrane protein for stable adherence junctions, and upregulation of mesenchymal molecules such as vimentin, fibronectin and N-cadherin (Thiery et al, 2009).
Epithelial–mesenchymal transition is also regulated by several transcription factors, such as Snail, Slug, Twist, Zeb1 and Zeb2 (Uchikado et al, 2005; Shioiri et al, 2006; Hotz et al, 2007; Wang et al, 2007; Usami et al, 2008; Sato et al, 2010; Gemmill et al, 2011; Kahlert et al, 2011; Ru et al, 2011; Sung et al, 2011; Dai et al, 2012; Kurahara et al, 2012). The functions of these factors are regulated by complex signalling networks present in the tumour microenvironment, such as transforming growth factor β, notch and Wnt pathways (Thiery et al, 2009; Sato et al, 2010; Kurahara et al, 2012).
It has recently become clear that EMT has an important role in tumour progression and metastasis (Thiery et al, 2009). In the gastrointestinal tract, many studies have shown that EMT is implicated in the progression and metastasis of cancers such as oesophageal (Usami et al, 2008; Sung et al, 2011), gastric (Kim et al, 2009; Ru et al, 2011; Dai et al, 2012; Ryu et al, 2012), colorectal (Shioiri et al, 2006; Kahlert et al, 2011) and pancreatic cancers (Hotz et al, 2007; Kurahara et al, 2012). Many EMT-related proteins including transcription factors have been investigated, and some of them have been shown to correlate with poor prognosis in some carcinomas (Thiery et al, 2009). Moreover, ‘cadherin switch', one aspect of EMT showing a loss of E-cadherin expression and a gain of N-cadherin expression, has a profound effect on tumour invasion/metastasis and is associated with unfavourable outcomes in several types of cancer (Gravdal et al, 2007; Wheelock et al, 2008; Jäger et al, 2010; Araki et al, 2011). Loss of E-cadherin expression and gain of N-cadherin expression is reminiscent of the cadherin switching that is seen during normal embryonic development and probably underpins many of the phenotypic changes in cancers. To our knowledge, only a few reported case series of EHCC have investigated a clinicopathological significance of EMT and cadherin switch in relation to tumour progression (Sato et al, 2010; Araki et al, 2011; Fabris et al, 2011). However, these studies were limited by the small numbers of cases and EMT-related proteins investigated, the prognostic significance of EMT and cadherin switch in EHCC has not yet been examined in detail.
The aim of this study was to investigate the clinicopathological significance of the expression of EMT-related proteins and cadherin switch in a large series of patients who underwent resection of EHCC.
Materials and methods
Cell lines
First of all, we need to validate antibodies used in this study, because many of the EMT-related proteins especially transcription factors have not been fully studied in actual surgically resected EHCC. The pancreatic adenocarcinoma cell lines Panc-1 and AsPc-1, the lung adenocarcinoma cell lines H1299 and H1650, and the breast carcinoma cell lines MDA-MB231, MCF7 and T47D were used for antibody validation (Hotz et al, 2007; Taube et al, 2010; Gemmill et al, 2011; Devarajan et al, 2012). Panc-1, H1299 and MDA-MB231 were cultured in D-MEM (Gibco BRL, Grand Island, NY, USA), and AsPc-1, H1650 and T47D were grown in RPMI-1640 (Sigma-Aldrich Japan, Tokyo, Japan), both of which were supplemented with 10% foetal bovine serum (FBS) and 1% penicillin/streptomycin. MCF7 was cultured in D-MEM supplemented with 10% FBS, 1% penicillin/streptomycin and 1% non-essential amino acids. All cell lines were maintained in a humidified incubator with 5% CO2 in air at 37 °C.
Reverse transcription-polymerase chain reaction
Total RNAs from the cell lines were extracted using Trizol reagent (Invitrogen Life Technologies, Carlsbad, CA, USA) and cDNA was synthesised with the Transcript First Strand cDNA Synthesis Kit (Roche, Indianapolis, IN, USA) in accordance with the manufacturer's protocols. The expression of EMT transcription factors was examined by reverse transcription polymerase chain reaction (RT–PCR) using the following primers (Hotz et al, 2007; Lindley and Briegel, 2010): Snail (557 bp) (forward) 5′-CAGACCCACTCAGATGTCAA-3′, (reverse) 5′-CATAGTTAGTCACACCTCGT-3′ Slug (182 bp) (forward) 5′-TGCGATGCCCAGTCTAGAAA-3′, (reverse) 5′-TTCTCCCCCGTGTGAGTTC-3′ Twist (196 bp) (forward) 5′-GTCCGCAGTCTTACGAGGAG-3′, (reverse) 5′-TGGAGGACCTGGTAGAGGAA-3′ Zeb1 (195 bp) (forward) 5′-CCTGTCCATATTGTGATAGAGGC-3′, (reverse) 5′-ACCCAGACTGCGTCACATGT-3′ Zeb2 (190 bp) (forward) 5′-AGGGACAGATCAGCACCAAA-3′, (reverse) 5′-GTGCGAACTGTAGGAACCAG-3′ GAPDH (150 bp) (forward) 5′-ATCAAGTGGGGCGATGCTG-3′, (reverse) 5′-ACCCATGACGAACATGGGG-3′.
GAPDH cDNA was amplified as a control. The PCR conditions were: initial denaturing at 94 °C for 5 min, followed by 30 cycles of denaturing at 94 °C for 30 s, annealing at 55 °C for 30 s and extension at 72 °C for 60 s. All PCR products were visualised by electrophoresis and ethidium bromide staining in 2% agarose gels.
Samples from patients
Surgical specimens of resected EHCC obtained between January 1995 and November 2006 at the Department of Gastroenterological Surgery II, Hokkaido University Graduate School of Medicine, were used in this study. A total of 117 specimens obtained from 92 males and 25 females (median age 71 years, range 44–87 years) were examined using the tissue microarray method. The median follow-up period was 26 months (range 0–151 months), and 89 patients (76.1%) died during follow-up. None of the patients received chemotherapy preoperatively. The tumour stage was classified according to the 7th TMN classification of the Union for International Cancer Control (Sobin et al, 2009). Extrahepatic CC was classified as a perihilar (n=74) or distal (n=43) on the basis of the location of the tumour epicentre or predominance of the main tumour (DeOliveira et al, 2007; Ebata et al, 2009). Macroscopically, the tumours were classified into three broad categories: papillary (n=18), nodular (n=79) and infiltrating (n=20). The latter two categories were grouped together as non-papillary tumours because the papillary form has specifically been associated with favourable survival outcomes (Jarnagin et al, 2005). Superficial spread was defined as extension of noninvasive carcinoma (carcinoma in situ) by >20 mm from the main tumour (Nakanishi et al, 2008). All informed consent processes for this study were conducted in accordance with the guidelines of the Hokkaido University Institutional Review Board.
Tissue microarray
Archival slides for all the cases were reviewed to select two representative areas (both the invasive front and bulk of tumour) and one representative area of non-neoplastic bile duct as an internal control. Tissue microarray blocks were then constructed using a manual tissue microarrayer (JF-4; Sakura Finetek Japan, Tokyo, Japan) with a 2.0-mm diameter needle. The finalised array blocks were sliced into 4-μm-thick sections and mounted on glass slides. To check the histopathological diagnosis and adequacy of tissue sampling, a section from each microarray was stained with haematoxylin and eosin and examined by an experienced pathologist (TM).
Immunohistochemical evaluation
Tissue sections were deparaffinised in xylene and rehydrated through a graded ethanol series. Heat-induced antigen retrieval was carried out in high-pH antigen retrieval buffer (Dako Cytomation, Glostrup, Denmark). Endogenous peroxidase was blocked by incubation in 3% H2O2 for 5 min. Details of the primary antibodies used are listed in Table 1. These sections were visualised by the HRP-labelled polymer method (Dako EnVision FLEX system) and an automated immunostaining system (Dako Autostainer Link). Immunostained sections were counterstained with haematoxylin, dehydrated in ethanol and cleared in xylene. Double immunostaining for N-cadherin and E-cadherin was performed using the HRP/DAB and ALP/Permanent red detection systems, respectively. After immunostaining for N-cadherin as described above, the sections were heat treated to strip the first step antibody in citrate-based buffer pH 6.0 (Dako Cytomation). The sections were immunostained for E-cadherin, and then visualised using the ALP-labelled LSAB method (Ventana iVIEW universal kit, Basel, Switzerland). Immunostained sections were counterstained with haematoxylin.
Table 1. Antibodies used for immunohistochemistry.
| Marker | Type | Source | Clone | Dilution | Antigen retrieval | Immunohistochemical patterns | Antibody validation control cell line (positive/negative) | Cutoff value of immunohistochemistry (%) |
|---|---|---|---|---|---|---|---|---|
| E-cadherin |
EM |
Invitrogen (Carlsbad, CA, USA) |
4A2C7 |
RTU |
Tris-EDTA |
Cytoplasmic membrane |
— |
43 |
| CK19 |
EM |
Novocastra (Newcastle-upon-Tyne, UK) |
b170 |
1 : 100 |
Tris-EDTA |
Cytoplasm |
— |
20 |
| Vimentin |
MM |
Ventana (Basel, Switzerland) |
V9 |
RTU |
Tris-EDTA |
Cytoplasm |
— |
43 |
| N-cadherin |
MM |
Dako (Carpinteria, CA, USA) |
6G11 |
1 : 50 |
Tris-EDTA |
Cytoplasmic membrane |
— |
35 |
| S100A4 |
MM |
Abcam (Cambridge, UK ) |
PAb (rabbit) |
1 : 200 |
Prot K |
Nuclear |
— |
50 |
|
α-SMA |
MM/CAFs |
Dako |
1A4 |
1 : 50 |
Tris-EDTA |
Cytoplasm |
— |
5a |
| Fibronectin |
MM |
Dako |
PAb (rabbit) |
1 : 2000 |
Prot K |
Cytoplasm |
— |
8 |
| Snail |
TF |
Abcam |
PAb (goat) |
1 : 500 |
Tris-EDTA |
Nuclear |
Panc1/H1299 |
60 |
| Slug |
TF |
Abcam |
PAb (rabbit) |
1 : 100 |
Tris-EDTA |
Nuclear |
MDA-MB231/T47D |
33 |
| Twist |
TF |
Abcam |
Twist2C1a |
1 : 20 |
Tris-EDTA |
Nuclear |
T47D/Panc1 |
15 |
| Zeb1 |
TF |
GenWay (San Diego, CA, USA) |
416A7H10 |
1 : 20 |
Tris-EDTA |
Nuclear |
MDA-MB231/MCF7 |
50 |
| Zeb2 |
TF |
Novus Biological (Littleton, CO, USA) |
PAb (rabbit) |
1 : 400 |
Tris-EDTA |
Cytoplasm |
H1299/MCF7 |
63 |
| Podoplanin |
CAFs |
Dako |
D2-40 |
RTU |
Tris-EDTA |
Stromal fibroblasts |
— |
30 |
| Ki67 | — | Dako | MIB-1 | 1 : 200 | Tris-EDTA | Nuclear | — | — |
Abbreviations: CAFs=cancer-associated fibroblasts marker; CK=cytokeratin; EM=epithelial marker; MM=mesenchymal marker; PAb=polyclonal antibody; Prot K=proteinase K solution; RTU=ready to use; α-SMA=α-smooth muscle actin; TF=transcription factor marker; Tris-EDTA=Tris-EDTA-based solution.
This cutoff value of α-SMA is that for the mesenchymal marker (i.e., EMT-related marker). As for the immunohistochemical evaluation of α-SMA as a CAFs marker, refer to the main text.
In this study, we evaluated immunohistochemical staining in terms of both staining intensity and proportion of stained tumour cells in the TMA cores. We initially evaluated the staining intensities of tumour cells, based on the staining of the control normal bile duct epithelium. The staining of epithelial markers E-cadherin and CK19 were considered positive (high expression), if the staining intensity was equivalent to that in normal epithelium. The staining of mesenchymal and transcription factor markers were considered positive (high expression), if weak to strong positive staining was seen compared with normal epithelium. The proportions of tumour cells with recognised staining alteration compared with normal epithelium were quantified as a percentage of the total number of tumour cells for an each TMA core. The staining results of these 12 markers were finally evaluated based on the mean proportion of two EHCC cores in each case. As for the evaluation of podoplanin, stromal expression of podoplanin was defined as positive when over than 30% of stromal fibroblastic cells were stained, as previously reported (Shindo et al, 2013). Ki67-positive cells were evaluated after identifying the areas where the highest number of the nuclear-positive cells were detected or ‘hot spots'. In this study, we used α-smooth muscle actin (α-SMA) as markers for both mesenchymal (i.e., EMT-related) and cancer-associated fibroblasts (CAFs). As for the immunohistochemical evaluation of α-SMA as CAFs' marker, the staining in the fibroblasts within tumour stroma was qualitatively classified into four groups (grade 0, +1, +2 and +3), as previously reported (Chuaysri et al, 2009). For statistical analysis, the grades 0 and +1 were categorised as negative expression and grades +2 and +3 as positive expression.
Two researchers (TN and TM), who were blinded to the patients' clinical information, independently examined and scored each case. Differences in interpretation were resolved by consensus agreements of them.
Statistical analysis
To determine a suitable cutoff point for the proportion of tumour cells with recognised staining alteration and dichotomising the level of immunohistochemical staining into either high or low expression groups, we used a receiver operating characteristic (ROC) curve according to the previous report (Tripathi et al, 2012) with modifications. The values of the proportions of tumour cells with recognised staining alteration as a continuous variable and survival (alive or dead at the median follow-up time) as a binary variable were subjected to ROC analysis.
Statistical analysis of the immunohistochemical staining was performed using the χ2 test, Fisher's exact test and Mann–Whitney U-test. Overall patient survival was calculated from the date of surgery to the date of the last follow-up or patient death. Univariate survival analysis was performed according to the Kaplan–Meier method, and survival was compared using the log-rank test. Multivariate analysis was conducted using the Cox proportional hazards regression model. The level for significance was P<0.05 and the confidence interval (CI) was determined at the 95% level. Statistical analysis was performed using the JMP 10.0 software package (SAS Institute, Inc., Cary, NC, USA) for Windows.
Results
Antibody validation for immunohistochemistry of EMT transcription factors
We validated the antibodies against EMT transcription factors and optimised their staining conditions in formalin-fixed, paraffin-embedded (FFPE) materials because these antibodies are not generally used for routine histological diagnoses and less well characterised. Positive and negative control FFPE cell blocks were prepared on the basis of the results obtained by RT–PCR (Supplementary Data 1a). Representative immunohistochemical staining patterns for EMT transcription factors are shown in Supplementary Data 1b. These validation data are also incorporated in Table 1.
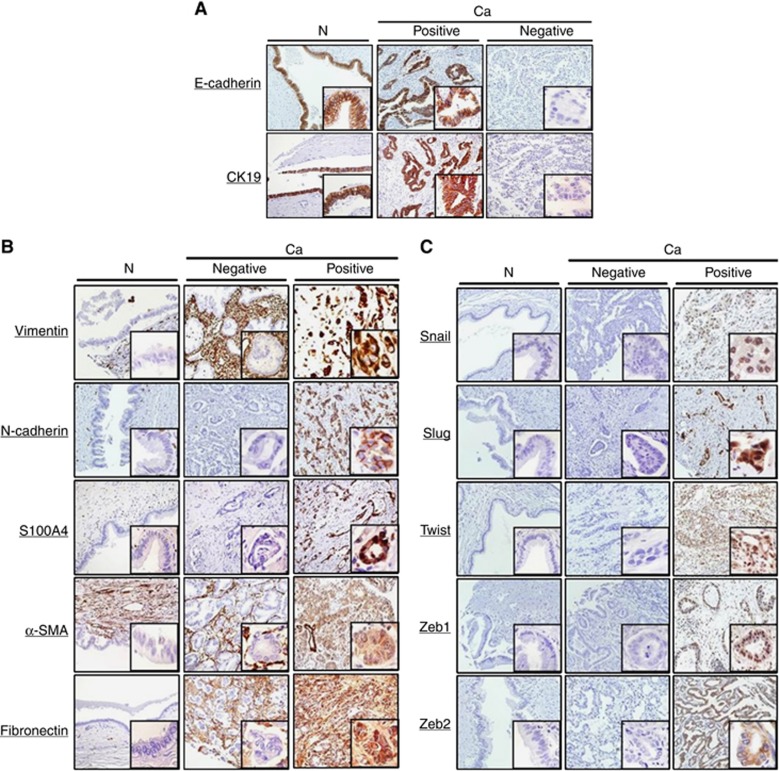
Expression of EMT-related proteins in EHCC
Figure 1A–C show representative immunohistochemical staining patterns from different cases for EMT-related proteins in the areas of carcinomas and non-neoplastic epithelia of the bile ducts. E-cadherin and N-cadherin showed a membranous staining pattern (Figure 1A and B). On the other hand, CK19, vimentin, α-SMA and fibronectin were detected in the cytoplasm (Figure 1A and B). Although S100A4 showed cytoplasmic and nuclear staining in cancer cells, nuclear S100A4 staining was considered to be positive because of its cytoplasmic expression in the non-neoplastic component that was induced by an epithelial reaction to damage (Fabris et al, 2011; Figure 1B). Immunohistochemical localisation of EMT transcription factors was consistent with cell block analysis (Figure 1C).
Figure 1.
Representative immunohistochemical staining patterns for 12 EMT-related markers are shown for carcinoma lesions (Ca) and non-neoplastic epithelium (N) of the bile duct. For each marker, positive and negative areas are from different patients. (A) epithelial markers, (B) mesenchymal markers and (C) transcription factor markers.
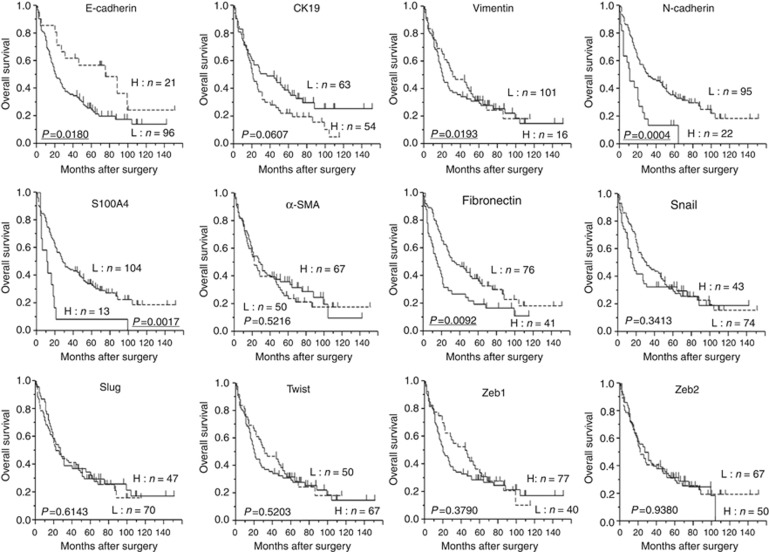
Survival analysis on the basis of EMT-related protein expression
Overall patient survival rates were determined using the log-rank test with respect to expression of the 12 EMT-related proteins. In terms of epithelial markers, low expression of E-cadherin (P=0.0180) was correlated with a poor outcome. High expression of vimentin (P=0.0193), N-cadherin (P=0.0004), S100A4 (P=0.0017) and fibronectin (P=0.0092) was each correlated with an unfavourable prognosis. However, no significant difference in patient outcome was found with respect to the expression status of the transcription factors, CK19 and α-SMA (Figure 2). In addition to EMT-related proteins, univariate analysis of overall survival using the log-rank test identified venous invasion (P=0.0020), histological classification (P=0.0291), T classification (P=0.0357), N classification (P=0.0010) and residual tumour (P=0.0471) as significant prognostic indicators. Moreover, multivariate analysis using the Cox regression model on the same set of patients was performed using the factors shown to be significant by univariate analysis. Those results showed that low expression of E-cadherin (hazard ratio (HR), 2.09; P=0.0208), high expression of N-cadherin (HR, 2.53; P=0.0038) and high expression of S100A4 (HR, 2.51; P=0.0157) was each an independent unfavourable prognostic factor, in addition to N classification (HR, 1.60; P=0.0420; Table 2).
Figure 2.
Kaplan–Meier survival curves with the log-rank test for expression of 12 EMT-related proteins. Abbreviations: H=high expression group; L=low expression group.
Table 2. Survival analysis.
| |
|
Survival (%) |
Univariate |
Multivariate |
||
|---|---|---|---|---|---|---|
| Variable | n | 3-Year | 5-Year | P-value | Relative risk (95% CI) | P-value |
|
Gender | ||||||
| Male | 92 | 41.7 | 32.1 | 0.4798 | ||
| Female |
25 |
36.0 |
24.0 |
|
|
|
|
Age | ||||||
| <71 | 56 | 40.0 | 29.1 | 0.4722 | ||
| ⩾71 |
61 |
40.9 |
33.5 |
|
|
|
|
Tumour size | ||||||
| <3 cm | 89 | 41.5 | 31.6 | 0.2027 | ||
| ⩾3 cm |
28 |
37.2 |
26.0 |
|
|
|
|
Location | ||||||
| Distal | 43 | 33.3 | 30.7 | 0.4266 | ||
| Perihilar |
74 |
44.5 |
30.0 |
|
|
|
|
Macroscopic type | ||||||
| Papillary | 18 | 50.0 | 37.5 | 0.5582 | ||
| Non-papillary |
99 |
38.7 |
29.0 |
|
|
|
|
Depth of tumour invasion | ||||||
| Within fm | 8 | 75.0 | 37.5 | 0.1633 | ||
| Beyond fm |
109 |
37.9 |
29.9 |
|
|
|
|
Invasion to the hepatic artery | ||||||
| Negative | 112 | 40.5 | 30.8 | 0.9620 | ||
| Positive |
5 |
40.0 |
20.0 |
|
|
|
|
Invasion to the portal vein | ||||||
| Negative | 91 | 43.3 | 35.0 | 0.1554 | ||
| Positive |
26 |
30.7 |
15.3 |
|
|
|
|
Lymphatic vessel invasion | ||||||
| Negative | 40 | 55.0 | 39.1 | 0.1322 | ||
| Positive |
77 |
32.9 |
25.4 |
|
|
|
|
Venous invasion | ||||||
| Negative | 52 | 57.6 | 45.4 | 0.0020 | 1.00 | 0.2002 |
| Positive |
65 |
26.5 |
18.2 |
|
1.37 (0.85–2.22) |
|
|
Perineural invasion | ||||||
| Negative | 15 | 46.6 | 33.3 | 0.5534 | ||
| Positive |
102 |
39.6 |
29.9 |
|
|
|
|
Superficial spread | ||||||
| Negative | 97 | 40.6 | 29.8 | 0.9510 | ||
| Positive |
20 |
40.0 |
33.3 |
|
|
|
|
Histopathological classification | ||||||
| Well+Pap | 37 | 59.4 | 45.1 | 0.0291 | 1.00 | 0.3528 |
| Mod+poor+others |
80 |
31.6 |
23.5 |
|
1.29 (0.75–2.26) |
|
|
pT | ||||||
| 1+2 | 62 | 48.3 | 39.8 | 0.0357 | 1.00 | 0.4162 |
| 3+4 |
55 |
31.5 |
19.8 |
|
1.22 (0.76–1.96) |
|
|
pN | ||||||
| 0 | 63 | 52.3 | 42.4 | 0.0010 | 1.00 | 0.0420 |
| 1 |
54 |
26.4 |
16.0 |
|
1.60 (1.02–2.54) |
|
|
pStage | ||||||
| I+II | 66 | 47.6 | 39.4 | 0.0607 | ||
| III+IV |
51 |
31.3 |
19.0 |
|
|
|
|
R | ||||||
| 0 | 95 | 44.7 | 33.5 | 0.0471 | 1.00 | 0.4475 |
| 1 |
22 |
22.7 |
17.1 |
|
1.27 (0.67–2.29) |
|
|
E-cadherin | ||||||
| High expression | 21 | 61.9 | 56.7 | 0.0180 | 1.00 | 0.0208 |
| Low expression |
96 |
35.8 |
24.4 |
|
2.09 (1.11–4.27) |
|
|
Vimentin | ||||||
| Low expression | 101 | 44.0 | 32.3 | 0.0193 | 1.00 | 0.5662 |
| High expression |
16 |
18.7 |
18.7 |
|
1.21 (0.61–2.25) |
|
|
N-cadherin | ||||||
| Low expression | 95 | 46.8 | 34.2 | 0.0004 | 1.00 | 0.0038 |
| High expression |
22 |
13.6 |
13.6 |
|
2.53 (1.36–4.54) |
|
|
S100A4 | ||||||
| Low expression | 104 | 44.2 | 32.8 | 0.0017 | 1.00 | 0.0157 |
| High expression |
13 |
8.3 |
8.3 |
|
2.51 (1.20–4.96) |
|
|
Fibronectin | ||||||
| Low expression | 76 | 48.0 | 36.2 | 0.0092 | 1.00 | 0.9093 |
| High expression | 41 | 26.8 | 19.5 | 1.08 (0.64–1.79) | ||
Abbreviation: CI=confidence interval. The bold and underlined entities indicate statistical significance (P<0.05).
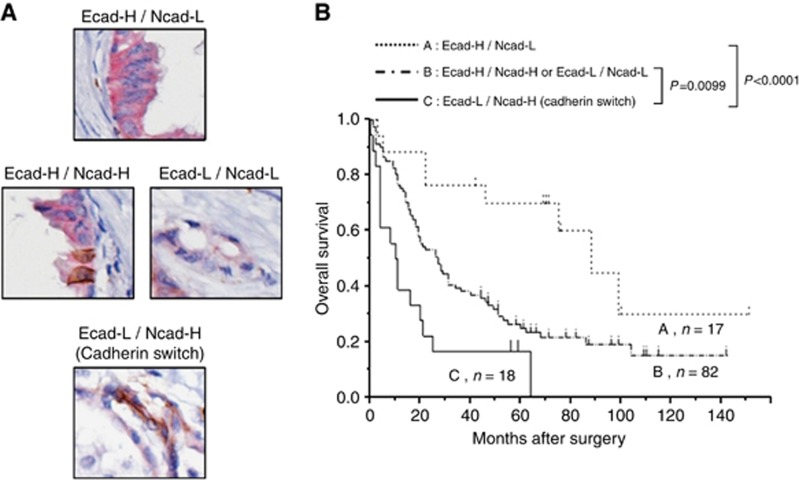
Relationships between patient survival and expression of E-cadherin and N-cadherin
We divided the 117 cases of EHCC into the following three subgroups: A, E-cadherin high expression and N-cadherin low expression phenotype (Ecad-H/Ncad-L); B, incomplete phenotype (Ecad-H/Ncad-H or Ecad-L/Ncad-L); and C, E-cadherin low expression and N-cadherin high expression phenotype (Ecad-L/Ncad-H). In this study, we defined subgroup C as the ‘cadherin switch' phenotype because this subgroup consistently showed downregulation of E-cadherin and upregulation of N-cadherin (Gravdal et al, 2007; Wheelock et al, 2008; Jäger et al, 2010; Araki et al, 2011). We showed the representative double immunohistochemical staining patterns for the cadherin switch in Figure 3A. In the immunohistochemical staining of the cell proliferation marker, Ki67, there was no significant differences of Ki67 labelling index between the cadherin switch-positive and -negative cases both in invasive front (P=0.9758) and bulk of tumour (P=0.6366; see Supplementary Data 2). In addition, to study whether the tumour reactive stroma was more expressed in specimens showing the cadherin switch, we immunohistochemically examined the expression of α-SMA and podoplanin, which have been reported to be the CAFs markers (Chuaysri et al, 2009; Vered et al, 2010; Pula et al, 2011; Neri et al, 2012; Herrera et al, 2013; Shindo et al, 2013), both in invasive front and bulk of tumour. As a result, no significant correlation was found between the presence of α-SMA/podoplanin-expressing CAFs and the expression of cadherin switch both in invasive front and bulk of tumour (see Supplementary Data 3).
Figure 3.
The 117 cases of EHCC are divided into three subgroups: A, E-cadherin high expression and N-cadherin low expression phenotype (Ecad-H/Ncad-L); B, incomplete phenotype (Ecad-H/Ncad-H or Ecad-L/Ncad-L); C, E-cadherin low expression and N-cadherin high expression phenotype (Ecad-L/Ncad-H). The subgroup C is defined as the ‘cadherin switch'. (A) Representative double immunohistochemical staining patterns for the cadherin switch. The expression of E-cadherin; red colour, the expression of N-cadherin; brown colour. (B) Kaplan–Meier survival curves with the log-rank test for combined E-cadherin and N-cadherin expression. The cadherin switch-positive group (subgroup C) was prognostically more unfavourable than the cadherin switch-negative group (subgroups A and B) (P<.0001, P=0.0099, respectively).
With regard to survival analysis, as shown in Figure 3B, the cadherin switch-positive group (subgroup C) was prognostically more unfavourable than the cadherin switch-negative group (subgroups A and B; P<.0001, P=0.0099, respectively). We then performed multivariate analysis to confirm the cadherin switch as an independent prognostic factor, and included the same set of significant factors derived from univariate analysis (excluding E-cadherin and N-cadherin). This analysis showed that the cadherin switch was an independent unfavourable prognostic factor (HR, 2.34; P=0.0143), in addition to S100A4 expression (HR, 2.29; P=0.0263) and N classification (HR, 1.65; P=0.0316; Table 3).
Table 3. Multivariate analysis including the cadherin switch.
| Characteristics | HR | 95% CI of relative risk | P-value |
|---|---|---|---|
| Venous invasion (negative vs positive) |
1.54 |
0.97–2.50 |
0.0681 |
| Histological classification (well+Pap vs mod+poor+others) |
1.14 |
0.67–1.98 |
0.6218 |
| T classification (1+2 vs T3+4) |
1.28 |
0.80–2.03 |
0.3024 |
| N classification (negative vs positive) |
1.65 |
1.05–2.62 |
0.0316 |
| Residual tumour (R0 vs R1/R2) |
1.21 |
0.65–2.16 |
0.5348 |
| Vimentin (low vs high expression) |
1.34 |
0.68–2.47 |
0.3819 |
| S100A4 (low vs high expression) |
2.29 |
1.11–4.45 |
0.0263 |
| Fibronectin (low vs high expression) |
1.06 |
0.64–1.74 |
0.8194 |
| Cadherin switch (negative vs positive) | 2.34 | 1.19–4.35 | 0.0143 |
Abbreviations: CI=confidence interval; HR=hazard ratio. The bold and underlined entities indicate statistical significance (P<0.05).
Discussion
Previous reports have analysed the relationship between expression of EMT-related proteins including cadherin switch and prognosis in EHCC (Sato et al, 2010; Araki et al, 2011; Fabris et al, 2011). However, those studies examined only a limited number of EMT-related proteins and small sample cohorts. To our knowledge, this is the first study to have investigated the correlation between the expression of multiple EMT-related proteins including representative transcription factors and clinicopathological outcomes in a large series of patients with EHCC. We confirmed that the results of immunohistochemistry performed on tissue microarrays paralleled those of the corresponding whole sections, based on the random selection of 10 cases. Among the 10 cases studied in whole sections, the staining localisation in tumour cells of each case was identical with the cores included in TMA, and the staining intensity was similar between invasive front and bulk of the tumours. According to the previous report (Kahlert et al, 2011), overexpression of Zeb2, one of the EMT-related transcriptional factors, in the invasive front correlated with patients' prognosis in colorectal cancer. On the other hand, in our pilot study, the expression of any transcriptional factor markers in the invasive front or bulk of tumour was not correlated with EHCC patients' prognosis. Therefore, we evaluated the staining results of TMA core based on the mean value of two tumour cores (both invasive front and bulk of tumour) in each case.
We evaluated the prognostic significance of both E-cadherin and N-cadherin expression in EHCC patients as similar to that in many other carcinomas previously reported (Gravdal et al, 2007; Kim et al, 2009). In several types of carcinoma, the E- to N-cadherin switch that influences cell phenotype and behaviour as a major aspect of EMT, has found to be associated with patient prognosis (Gravdal et al, 2007; Wheelock et al, 2008; Jäger et al, 2010; Araki et al, 2011). In EHCC, Araki et al (2011) confirmed that the cadherin switch occurred in CC cells as a result of TGF-β-induced EMT in vitro, and that this cadherin switch was related to the migratory and invasive properties of CC cells. In an immunohistochemical study of 38 EHCC specimens, they also revealed that the cadherin switch was correlated with patients' survival (Araki et al, 2011). In this study, we demonstrated for the first time in the EHCC patients that the cadherin switch was a more significant factor associated with poor prognosis than either E-cadherin or N-cadherin alone. Multivariate analysis also showed that the cadherin switch was an independent prognostic factor. The reason why the cadherin switch is a more significant factor than altered expression of E-cadherin or N-cadherin alone is not clear. In our study, no significant difference in Ki67 labelling index was found between cadherin switch-positive and -negative groups.
Recently, it has been reported that interaction between cancer cells and surrounding CAFs has a pivotal role in cancer progression (Chuaysri et al, 2009; Vered et al, 2010; Pula et al, 2011; Neri et al, 2012; Herrera et al, 2013; Shindo et al, 2013). One of the most common CAFs' markers is α-SMA (Chuaysri et al, 2009; Vered et al, 2010; Herrera et al, 2013). Detection of α-SMA in tumour stroma has been studied in various carcinomas, and was proposed to have an association with an aggressive phenotype of cancer cells (Chuaysri et al, 2009; Vered et al, 2010; Herrera et al, 2013). Podoplanin, which is a representative lymphatic vessel marker (D2-40), have gained attention as a CAFs' marker, and the podoplanin-expressing CAFs has been reported to be associated with malignant potential in several types of cancer (Pula et al, 2011; Neri et al, 2012; Shindo et al, 2013). However, in this study, no significant correlation was found between the presence of α-SMA/podoplanin-expressing CAFs and the expression of cadherin switch both in invasive front and bulk of tumour. Although, in some reports, the contribution of the CAFs to the cancer progression has been found (Chuaysri et al, 2009; Vered et al, 2010; Pula et al, 2011; Neri et al, 2012; Herrera et al, 2013; Shindo et al, 2013), the exact role of CAFs in cancer is not fully understood and may have functional heterogeneity according to the types of cancer (Shindo et al, 2013). The malignant potential of the cadherin switch may be explained by the association between cadherins and the growth factor receptor signalling pathway (Wheelock et al, 2008). Growth factor receptors, such as the epidermal growth factor receptor and fibroblast growth factor receptor, regulate many aspects of tumour cell behaviour, including cell motility and invasion (Wheelock et al, 2008). It has been suggested that when epithelial tumour cells switch from E- to N-cadherin expression, they also gain the ability to activate growth factor receptor pathways to enhance cell growth and invasion (Wheelock et al, 2008). As for cadherin switch, it is also interesting to examine the correlation between the expression of more advanced mesenchymal markers showing complete EMT, such as α-SMA and fibronectin, and the cadherin switch in vitro study. Further insight into this aspect awaits future studies.
S100A4 is a member of the S100 family of Ca2+-binding proteins and is expressed in both mesenchymal cells and some malignant epithelial tumours (Helfman et al, 2005; Schneider et al, 2008; Fabris et al, 2011). S100A4 is involved in the regulation of a wide range of biological phenomena including cell motility, survival, differentiation, contractility, fibrosis and EMT (Schneider et al, 2008; Fabris et al, 2011). Moreover, S100A4 has been shown to be a candidate molecular marker of metastatic potential with high prognostic significance in several cancers (Helfman et al, 2005; Schneider et al, 2008; Fabris et al, 2011). Fabris et al (2011) reported that the expression of nuclear S100A4 was an independent predictor of survival in CC including both intrahepatic (n=55) and extrahepatic (n=31) types. They also demonstrated that the nuclear expression of S100A4 was associated with the enhanced metastatic potential of CC cell lines xenotransplanted into SCID mice, and that the silencing of S100A4 was associated with reduced motility, invasiveness and the expression of MMP9 in vitro (Fabris et al, 2011). In our large-scale study of EHCC, S100A4 was revealed to be an independent prognostic factor, being consistent with the previous study (Fabris et al, 2011).
Transcription factors that orchestrate EMT have been correlated with poor prognosis in several types of carcinoma. For example, in the gastrointestinal tract, expression of Snail, Slug, Twist, Zeb1 and Zeb2 has been associated with unfavourable survival outcomes in patients with oesophageal (Uchikado et al, 2005), gastric (Kim et al, 2009; Ru et al, 2011; Dai et al, 2012), colorectal (Shioiri et al, 2006; Kahlert et al, 2011) or pancreatic cancer (Kurahara et al, 2012). Sato et al (2010) reported that EHCC patients whose tumours showed marked immunohistochemical expression of Snail had a significantly poorer prognosis than those with tumours showing negative or mild-to-moderate expression. Although a large number of studies have suggested that these transcription factors may be useful as prognostic parameters, our present results indicated that none of the transcription factors investigated here were predictive of patient outcome. In addition to the pathways triggered by the transcription factors investigated in this study, many other molecules, such as Kruppel-like factor 8, Goosecoid and FoxC2, have recently been described as EMT inducers (Wang et al, 2007; Thiery et al, 2009). In EHCC, these other transcription factors may be key transcription factors inducing EMT. Moreover, a discrepancy between our results and those obtained by others may be also explained by the differences of case numbers, patients' characteristics, antibodies used in those studies, periods of follow-up, storage conditions and the methods of fixation for the specimens. In addition, the way of setting the cutoff point for immunohistochemistry may also be a cause of inconsistency.
In conclusion, we have demonstrated that the expression of E-cadherin, N-cadherin and S100A4 may each be a novel prognostic indicator reflecting the aggressiveness of EHCC. Furthermore, the cadherin switch may be a prognostic parameter for EHCC patients, showing a higher discriminative power than expression of E-cadherin or N-cadherin alone. Although the validation of these results with the same cutoffs in an independent patient cohort is necessary, these results may provide useful information for selecting the appropriate adjuvant therapy protocol and strict surveillance for EHCC patients.
Acknowledgments
We appreciate the contributions of Jun Moriya, Tomohiro Shimizu and Sanae Mochizuki for their technical support in the Department of Surgical Pathology.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Material
References
- Aishima S, Kubo Y, Tanaka Y, Oda Y. Histological features of precancerous and early cancerous lesions of biliary tract carcinoma. J Hepatobiliary Pancreat Sci. 2014;21 (7:448–452. doi: 10.1002/jhbp.71. [DOI] [PubMed] [Google Scholar]
- Araki K, Shimura T, Suzuki H, Tsutsumi S, Wada W, Yajima T, Kobayahi T, Kubo N, Kuwano H. E/N-cadherin switch mediates cancer progression via TGF-β-induced epithelial-to-mesenchymal transition in extrahepatic cholangiocarcinoma. Br J Cancer. 2011;105 (12:1885–1893. doi: 10.1038/bjc.2011.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuaysri C, Thuwajit P, Paupairoj A, Chau-In S, Suthiphongchai T, Thuwajit C. Alpha-smooth muscle actin-positive fibroblasts promote biliary cell proliferation and correlate with poor survival in cholangiocarcinoma. Oncol Rep. 2009;21 (4:957–969. doi: 10.3892/or_00000309. [DOI] [PubMed] [Google Scholar]
- Dai YH, Tang YP, Zhu HY, Lv L, Chu Y, Zhou YQ, Huo JR. ZEB2 promotes the metastasis of gastric cancer and modulates epithelial mesenchymal transition of gastric cancer cells. Dig Dis Sci. 2012;57 (5:1253–1260. doi: 10.1007/s10620-012-2042-6. [DOI] [PubMed] [Google Scholar]
- DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, Choti MA, Yeo CJ, Schulick RD. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245 (5:755–762. doi: 10.1097/01.sla.0000251366.62632.d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devarajan E, Song YH, Krishnappa S, Alt E. Epithelial-mesenchymal transition in breast cancer lines is mediated through PDGF-D released by tissue-resident stem cells. Int J Cancer. 2012;131 (5:1023–1031. doi: 10.1002/ijc.26493. [DOI] [PubMed] [Google Scholar]
- Ebata T, Kamiya J, Nishio H, Nagasaka T, Nimura Y, Nagino M. The concept of perihilar cholangiocarcinoma is valid. Br J Surg. 2009;96 (8:926–934. doi: 10.1002/bjs.6655. [DOI] [PubMed] [Google Scholar]
- Fabris L, Cadamuro M, Moserle L, Dziura J, Cong X, Sambado L, Nardo G, Sonzogni A, Colledan M, Furlanetto A, Bassi N, Massani M, Cillo U, Mescoli C, Indraccolo S, Rugge M, Okolicsanyi L, Strazzabosco M. Nuclear expression of S100A4 calcium-binding protein increases cholangiocarcinoma invasiveness and metastasization. Hepatology. 2011;54 (3:890–899. doi: 10.1002/hep.24466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandou C, Harada K, Sato Y, Igarashi S, Sasaki M, Ikeda H, Nakanuma Y. Hilar cholangiocarcinoma and pancreatic ductal adenocarcinoma share similar histopathologies, immunophenotypes, and development-related molecules. Hum Pathol. 2013;44 (5:811–821. doi: 10.1016/j.humpath.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Gemmill RM, Roche J, Potiron VA, Nasarre P, Mitas M, Coldren CD, Helfrich BA, Garrett-Mayer E, Bunn PA, Drabkin HA. ZEB1-responsive genes in non-small cell lung cancer. Cancer Lett. 2011;300 (1:66–78. doi: 10.1016/j.canlet.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravdal K, Halvorsen OJ, Haukaas SA, Akslen LA. A switch from E-cadherin to N-cadherin expression indicates epithelial to mesenchymal transition and is of strong and independent importance for the progress of prostate cancer. Clin Cancer Res. 2007;13 (23:7003–7011. doi: 10.1158/1078-0432.CCR-07-1263. [DOI] [PubMed] [Google Scholar]
- Helfman DM, Kim EJ, Lukanidin E, Grigorian M. The metastasis associated protein S100A4: role in tumour progression and metastasis. Br J Cancer. 2005;92 (11:1955–1958. doi: 10.1038/sj.bjc.6602613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrera M, Herrera A, Dominguez G, Silva J, Garcia V, Garcia JM, Gomez I, Soldevilla B, Munoz C, Provencio M, Campos-Martin Y, Garcia de Herreros A, Casal I, Bonilla F, Pena C. Cancer-associated fibroblast and M2 macrophage markers together predict outcome in colorectal cancer patients. Cancer Sci. 2013;104 (4:437–444. doi: 10.1111/cas.12096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotz B, Arndt M, Dullat S, Bhargava S, Buhr HJ, Hotz HG. Epithelial to mesenchymal transition: expression of the regulators snail, slug, and twist in pancreatic cancer. Clin Cancer Res. 2007;13 (16:4769–4776. doi: 10.1158/1078-0432.CCR-06-2926. [DOI] [PubMed] [Google Scholar]
- Jarnagin WR, Bowne W, Klimstra DS, Ben-Porat L, Roggin K, Cymes K, Fong Y, DeMatteo RP, D'Angelica M, Koea J, Blumgart LH.2005Papillary phenotype confers improved survival after resection of hilar cholangiocarcinoma Ann Surg 241(5703–712.; discussion 712-714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jäger T, Becker M, Eisenhardt A, Tilki D, Tötsch M, Schmid KW, Romics I, Rübben H, Ergün S, Szarvas T. The prognostic value of cadherin switch in bladder cancer. Oncol Rep. 2010;23 (4:1125–1132. doi: 10.3892/or_00000741. [DOI] [PubMed] [Google Scholar]
- Kahlert C, Lahes S, Radhakrishnan P, Dutta S, Mogler C, Herpel E, Brand K, Steinert G, Schneider M, Mollenhauer M, Reissfelder C, Klupp F, Fritzmann J, Wunder C, Benner A, Kloor M, Huth C, Contin P, Ulrich A, Koch M, Weitz J. Overexpression of ZEB2 at the invasion front of colorectal cancer is an independent prognostic marker and regulates tumor invasion in vitro. Clin Cancer Res. 2011;17 (24:7654–7663. doi: 10.1158/1078-0432.CCR-10-2816. [DOI] [PubMed] [Google Scholar]
- Kim MA, Lee HS, Lee HE, Kim JH, Yang HK, Kim WH. Prognostic importance of epithelial-mesenchymal transition-related protein expression in gastric carcinoma. Histopathology. 2009;54 (4:442–451. doi: 10.1111/j.1365-2559.2009.03247.x. [DOI] [PubMed] [Google Scholar]
- Kurahara H, Takao S, Maemura K, Mataki Y, Kuwahata T, Maeda K, Ding Q, Sakoda M, Iino S, Ishigami S, Ueno S, Shinchi H, Natsugoe S. Epithelial-mesenchymal transition and mesenchymal-epithelial transition via regulation of ZEB-1 and ZEB-2 expression in pancreatic cancer. J Surg Oncol. 2012;105 (7:655–661. doi: 10.1002/jso.23020. [DOI] [PubMed] [Google Scholar]
- Lindley LE, Briegel KJ. Molecular characterization of TGF beta-induced epithelial-mesenchymal transition in normal finite lifespan human mammary epithelial cells. Biochem Biophys Res Commun. 2010;399 (4:659–664. doi: 10.1016/j.bbrc.2010.07.138. [DOI] [PubMed] [Google Scholar]
- Nakanishi Y, Zen Y, Kawakami H, Kubota K, Itoh T, Hirano S, Tanaka E, Nakanuma Y, Kondo S. Extrahepatic bile duct carcinoma with extensive intraepithelial spread: a clinicopathological study of 21 cases. Mod Pathol. 2008;21 (7:807–816. doi: 10.1038/modpathol.2008.65. [DOI] [PubMed] [Google Scholar]
- Neri S, Ishii G, Taira T, Hishida T, Yoshida J, Nishimura M, Nagai K, Ochiai A. Recruitment of podoplanin positive cancer-associated fibroblasts in metastatic lymph nodes predicts poor prognosis in pathological N2 stage III lung adenocarcinoma. Ann Surg Oncol. 2012;19 (12:3953–3962. doi: 10.1245/s10434-012-2421-4. [DOI] [PubMed] [Google Scholar]
- Pula B, Jethon A, Piotrowska A, Gomulkiewicz A, Owczarek T, Calik J, Wojnar A, Witkiewicz W, Rys J, Ugorski M, Dziegiel P, Podhorska-Okolow M. Podoplanin expression by cancer-associated fibroblasts predicts poor outcome in invasive ductal breast carcinoma. Histopathology. 2011;59 (6:1249–1260. doi: 10.1111/j.1365-2559.2011.04060.x. [DOI] [PubMed] [Google Scholar]
- Ru GQ, Wang HJ, Xu WJ, Zhao ZS. Upregulation of Twist in gastric carcinoma associated with tumor invasion and poor prognosis. Pathol Oncol Res. 2011;17 (2:341–347. doi: 10.1007/s12253-010-9332-0. [DOI] [PubMed] [Google Scholar]
- Ryu HS, Park DJ, Kim HH, Kim WH, Lee HS. Combination of epithelial-mesenchymal transition and cancer stem cell-like phenotypes has independent prognostic value in gastric cancer. Hum Pathol. 2012;43 (4:520–528. doi: 10.1016/j.humpath.2011.07.003. [DOI] [PubMed] [Google Scholar]
- Sato Y, Harada K, Itatsu K, Ikeda H, Kakuda Y, Shimomura S, Shan Ren X, Yoneda N, Sasaki M, Nakanuma Y. Epithelial-mesenchymal transition induced by transforming growth factor-{beta}1/Snail activation aggravates invasive growth of cholangiocarcinoma. Am J Pathol. 2010;177 (1:141–152. doi: 10.2353/ajpath.2010.090747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider M, Hansen JL, Sheikh SP. S100A4: a common mediator of epithelial-mesenchymal transition, fibrosis and regeneration in diseases. J Mol Med (Berl) 2008;86 (5:507–522. doi: 10.1007/s00109-007-0301-3. [DOI] [PubMed] [Google Scholar]
- Shioiri M, Shida T, Koda K, Oda K, Seike K, Nishimura M, Takano S, Miyazaki M. Slug expression is an independent prognostic parameter for poor survival in colorectal carcinoma patients. Br J Cancer. 2006;94 (12:1816–1822. doi: 10.1038/sj.bjc.6603193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shindo K, Aishima S, Ohuchida K, Fujiwara K, Fujino M, Mizuuchi Y, Hattori M, Mizumoto K, Tanaka M, Oda Y. Podoplanin expression in cancer-associated fibroblasts enhances tumor progression of invasive ductal carcinoma of the pancreas. Mol Cancer. 2013;12 (1:168–184. doi: 10.1186/1476-4598-12-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobin LH, Gospodarowicz MK, Wittekind Ch.eds) (2009TNM Classification of Malignant Tumours7th edn.Wiley-Blackwell: Oxford; 122–128. [Google Scholar]
- Sung CO, Park CK, Kim SH. Classification of epithelial-mesenchymal transition phenotypes in esophageal squamous cell carcinoma is strongly associated with patient prognosis. Mod Pathol. 2011;24 (8:1060–1068. doi: 10.1038/modpathol.2011.59. [DOI] [PubMed] [Google Scholar]
- Taube JH, Herschkowitz JI, Komurov K, Zhou AY, Gupta S, Yang J, Hartwell K, Onder TT, Gupta PB, Evans KW, Hollier BG, Ram PT, Lander ES, Rosen JM, Weinberg RA, Mani SA. Core epithelial-to-mesenchymal transition interactome gene-expression signature is associated with claudin-low and metaplastic breast cancer subtypes. Proc Natl Acad Sci USA. 2010;107 (35:15449–15454. doi: 10.1073/pnas.1004900107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139 (5:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Tripathi SC, Kaur J, Matta A, Gao X, Sun B, Chauhan SS, Thakar A, Shukla NK, Duggal R, Choudhary AR, DattaGupta S, Sharma MC, Ralhan R, Siu KW. Loss of DLC1 is an independent prognostic factor in patients with oral squamous cell carcinoma. Mod Pathol. 2012;25 (1:14–25. doi: 10.1038/modpathol.2011.145. [DOI] [PubMed] [Google Scholar]
- Uchikado Y, Natsugoe S, Okumura H, Setoyama T, Matsumoto M, Ishigami S, Aikou T. Slug Expression in the E-cadherin preserved tumors is related to prognosis in patients with esophageal squamous cell carcinoma. Clin Cancer Res. 2005;11 (3:1174–1180. [PubMed] [Google Scholar]
- Usami Y, Satake S, Nakayama F, Matsumoto M, Ohnuma K, Komori T, Semba S, Ito A, Yokozaki H. Snail-associated epithelial-mesenchymal transition promotes oesophageal squamous cell carcinoma motility and progression. J Pathol. 2008;215 (3:330–339. doi: 10.1002/path.2365. [DOI] [PubMed] [Google Scholar]
- Van der Gaag NA, Kloek JJ, de Bakker JK, Musters B, Geskus RB, Busch OR, Bosma A, Gouma DJ, van Gulik TM. Survival analysis and prognostic nomogram for patients undergoing resection of extrahepatic cholangiocarcinoma. Ann Oncol. 2012;23 (10:2642–2649. doi: 10.1093/annonc/mds077. [DOI] [PubMed] [Google Scholar]
- Vered M, Dayan D, Yahalom R, Dobriyan A, Barshack I, Bello IO, Kantola S, Salo T. Cancer-associated fibroblasts and epithelial-mesenchymal transition in metastatic oral tongue squamous cell carcinoma. Int J Cancer. 2010;127 (6:1356–1362. doi: 10.1002/ijc.25358. [DOI] [PubMed] [Google Scholar]
- Wang X, Zheng M, Liu G, Xia W, McKeown-Longo PJ, Hung MC, Zhao J. Krüppel-like factor 8 induces epithelial to mesenchymal transition and epithelial cell invasion. Cancer Res. 2007;67 (15:7184–7193. doi: 10.1158/0008-5472.CAN-06-4729. [DOI] [PubMed] [Google Scholar]
- Wheelock MJ, Shintani Y, Maeda M, Fukumoto Y, Johnson KR. Cadherin switching. J Cell Sci. 2008;121 (Pt 6:727–735. doi: 10.1242/jcs.000455. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.