Abstract
Background:
The blockade of PD-1–PD-L1 pathway is emerging as an effective therapeutic strategy for several advanced cancers. But the immune regulatory role of PD-1–PD-L1 pathway is not clear in colorectal cancer (CRC) patients. This study aims to evaluate the role of PD-1–PD-L1 pathway in CD8+ T-cell functions in tumour-draining lymph nodes (TDLNs) and tumours of CRC patients.
Methods:
PD-1 expression on CD8+ T cells was examined by flow cytometry, and PD-L1 expression in TDLNs and tumour tissues were examined by immunohistochemistry. Production of IFN-γ, IL-2 and expression of granzyme B, perforin in CD8+ T cells were detected by intracellular staining.
Results:
PD-1 expression is markedly upregulated on CD8+ T cells in TDLNs and tumours compared with that in peripheral blood. PD-1-expressing CD8+ T cells are competent for production of cytokine (IL-2 and IFN-γ) and perforin in the tumour-free lymph nodes (TFLNs), but exhibit exhausted phenotypes in tumours. In addition, PD-L1 is highly expressed in tumours rather than TFLNs, which is closely correlated with the impairment of IFN-γ production of tumour-infiltrating PD-1+ CD8+ T cells.
Conclusions:
Our findings suggest a suppressive effect of PD-1 on CD8+ T-cell function in tumours, but not in TFLNs.
Keywords: PD-1, exhaustion, CD8+ T cell, draining lymph node, colorectal cancer
The programmed death 1 (PD-1, also known as CD279) is a co-inhibitory receptor that is inducibly expressed on T cells upon activation (Chen, 2004; Keir et al, 2008). PD-1 is rapidly upregulated on antigen-specific T cells responding to viral infection, but quickly downregulated upon removal of the antigen in acute viral infection (Barber et al, 2006). By contrast, during chronic infections such as LCMV in mice (Barber et al, 2006) and HIV (Day et al, 2006; Trautmann et al, 2006) or HCV in patients (Urbani et al, 2006; Golden-Mason et al, 2007; Nakamoto et al, 2008), virus-specific CD8 T cells show sustained expression of PD-1 that triggers T-cell dysfunction or exhaustion by interaction with its ligand PD-L1 (B7-H1). Blocking of PD-1–PD-L1 interactions can restore T-cell function to reverse the course of chronic infection.
The PD-1–PD-L1 pathway has also been implicated in T cell exhaustion in cancer. PD-1 is highly expressed on tumour-infiltrating CD8+ T cells in multiple solid tumours (Thompson et al, 2007; Ahmadzadeh et al, 2009; Lyford-Pike et al, 2013), particularly on tumour-specific CD8+ T cells. PD-1+ CD8+ T cells exhibit an exhausted phenotype as defined by impairment of proliferation, cytokine production and cytotoxicity. Meanwhile, PD-L1 is expressed in several different cancers, which is strongly associated with poor prognosis (Thompson et al, 2004; Ohigashi et al, 2005; Hamanishi et al, 2007; Keir et al, 2008). The interference with PD-1–PD-L pathway using blocking monoclonal antibodies (mAbs) against PD-1 or PD-L1 is emerging as an effective method for reversing cancer immunosuppression and thereby causing tumour regression in patients with advanced disease. Such treatments have shown promising clinical results not only for tumours classically considered to be immunogenic such as melanoma and renal cell carcinoma, but also for common epithelial malignancies such as non-small cell lung cancer, which has been considered to be non-immunogenic and poorly responsive to immune-based therapies (Brahmer et al, 2012; Topalian et al, 2012). But, in the same clinical trials, no objective responses were observed in patients with colorectal cancer (CRC). The reason for the different therapeutic effects of targeting PD-1–PD-L pathway between CRCs and other cancers is not known. It was reported that the presence of tumour-infiltrating lymphocytes (TILs) in primary CRC presages an improved clinical outcome (Ropponen et al, 1997; Naito et al, 1998). A high density of infiltrating memory and effector memory T cells (TEM) within CRCs was associated with decreased invasiveness, lower stage and improved survival. The type and density of T cells in CRCs were found to have stronger prognostic significance than conventional tumour–node–metastasis (TNM) staging (Pages et al, 2005; Galon et al, 2006). These studies provide clear evidence that anti-tumour T cell responses play an important role in determining the clinical outcome from CRC. However, the expression and regulatory effects of PD-1 on CD8+ TILs from CRC have not been reported, and the roles of PD-1–PD-L1 pathway in regulating T cell responses against CRC are not well studied. It was reported that PD-1 is expressed on T cells of peripheral blood and PD-L1 was detectable in epithelial cells of normal colonic mucosa and cancer cells in CRC patients (Arai et al, 2012; Droeser et al, 2013). But, PD-L1 expression is paradoxically associated with improved survival of CRC patients (Droeser et al, 2013).
The tumour-draining lymph node (TDLN) is the site in which tumour-specific CD8+ T cells are typically activated by antigen-presenting cells, and antitumor immune responses are initiated. Meanwhile, it is also the preferential site of initial tumour metastases. The local microenvironment in the TDLNs becomes a key determinant in setting the course of the subsequent immune response to the tumour (Kim et al, 2006). It was reported that a high density of CD45RO+ T cells in lymph node metastasis of CRC was associated with improved prognosis (Oberg et al, 2002). PD-1 is inducibly expressed on T cells upon activation, but the effect of PD-1 signalling in activated CD8+ T cells in TDLNs has not been reported.
In this study, we show that PD-1 is highly expressed on CD8+ T cells in tumour-free lymph nodes (TFLNs) and tumours. The functions of PD-1+ CD8+ T cells are intact in TFLNs, but impaired in tumours. PD-L1 is expressed in tumours and tumour-invaded lymph nodes (TILNs) rather than TFLNs. Moreover, expression of PD-L1 is closely associated with the function of PD-1+ CD8+ T cells in tumours. Our findings suggest that PD-1 signalling has no negative regulation on CD8+ T cells in TDLNs, but do severely inhibit functions of CD8+ T cells in tumours.
Materials and methods
Patient samples
Fresh tumour tissues, draining lymph nodes and blood samples were obtained from the CRC patients who underwent radical resection from 13 December 2011 to 28 August 2013 in a single group of the Cancer Hospital, Chinese Academy of Medical Science and Peking Union Medical College. The patients who were treated with radiation, chemotherapy or immunotherapy before operation, or had cancer history, hereditary CRC, autoimmune disease, inflammatory bowel disease, infectious diseases, and multi-primary cancer and CRC with emergency complications were excluded. The TNM stage was determined according to the seventh edition of the American Joint Committee on Cancer (AJCC) staging manual. The examination of regional lymph nodes was carried out by a single colorectal pathologist. The study and all protocols below were approved by the Ethics Committee of Cancer Hospital, Chinese Academy of Medical Science, and the Institutional Review Board of Institute of Biophysics, Chinese Academy of Sciences, Beijing, China. Patient written informed consent was obtained.
Cell preparation
Peripheral blood mononuclear cells were isolated by density-gradient centrifugation using Ficoll-Hypaque (Hao Yang Biological, Tianjin, China). Draining lymph nodes were minced and passed through sterile mesh to obtain cell suspension. Tumour tissues were sliced into small pieces, digested with a mixture of type IV collagenase (Life Technologies, Inc, Carlsbad, CA, USA), hyaluronidase and DNAse (Sigma-Aldrich, St Louis, MO, USA) in RPMI 1640 medium (GIBCO-BRL, Rockville, MD, USA) containing 2% fetal bovine serum (FBS) at 37°C for 2–3 h with gentle agitation, then passed through sterile mesh to obtain single-cell suspension. The digested tumour suspensions were washed twice in RPMI 1640 medium, and viable cells were isolated on a two-layer Ficoll gradient.
Antibodies and reagents
PerCP-Cy5.5-conjugated anti-CD3 (OKT3), anti-CD45RA (HI100), FITC-conjugated anti-PD-1 (MIH4), mouse IgG1 κ isotype control, PE-conjugated anti-CD8 (HIT8a), anti-perforin (B-D48), anti-granzyme B (GB11), APC-conjugated anti-CD8 (OKT8), anti-IFN-γ (4S.B3) and anti-IL-2 (MQ1-17H12) were purchased from eBioscience (San Diego, CA, USA).
Flow cytometry
Cells were resuspended in staining buffer (PBS containing 3% FBS) and blocked with human IgG (eBioscience). Then, the antibodies against surface antigens were added and incubated at 4°C for 30 min. For perforin and granzyme B staining, cells were subsequently washed twice, fixed and permeabilised using Cytofix/Cytoperm solution (BD Biosciences, San Jose, CA, USA) for 20 min on ice. After washing with 1 × Perm Wash Buffer (BD Biosciences), the cells were stained with labelled anti-perforin or granzyme B antibodies. Cells were acquired on FACS Calibur (BD Biosciences) and data were analysed with FlowJo software (Tree Star, Ashland, OR, USA).
Intracellular cytokine induction
Cells from tumour suspensions and draining lymph nodes were stimulated with phorbolmyristate acetate (PMA; 2 ng ml−1) and ionomycin (1 μg ml−1) in the presence of Brefeldin A (eBioscience) for 4 h at 37°C. Cells were subsequently collected and stained for surface markers followed by fixation with IC fixation Buffer (eBioscience) for 20 to 30 min at room temperature. Then, the cells were washed twice with 1 × Permeabilization Buffer (eBioscience) and stained with IL-2, IFN-γ antibody. After washing, cells were fixed with 1% PFA and stored at 4°C until acquisition.
Immunohistochemistry
Both tumour tissues and lymph nodes were fixed with formalin, and embedded in paraffin wax. Tissue sections were cut into 5-μm-thick consecutive sections and dried at 70°C for 30 min. Dried sections were deparraffinised in xylene and rehydrated through graded ethanol solutions to water. Antigens were retrieved by heating the tissue sections in citrate buffer (pH 6.0) by microwaves. To block endogenous peroxidase activity, all of the sections were treated with 100% methanol containing 0.3% H2O2 for 15 min. Non-specific binding was blocked with 10% normal goat serum (Life Technologies, Inc). The sections were incubated with mouse anti-PD-L1 mAbs (clone 27A2, MBL, Nagoya, Japan) or purified mouse IgG2b, κ isotype ctrl antibody (MCP-11, BioLegend, San Diego, CA, USA) overnight at 4°C. The sections were then incubated with HRP-labelled goat anti-mouse secondary antibody (Santa Cruz, Dallas, TX, USA). Diaminobenzene was used as the chromogen and haematoxylin as the nuclear counterstain.
Statistical analysis
Statistical analysis was done with GraphPad Prism 5 software (Graphpad, San Diego, CA, USA). Two-tailed t-test for paired or unpaired samples were applied to determine the significance. A correlation was tested for significance by the Spearman's rank correlation test. Data were considered statistically significant at P<0.05.
Results
Patient characteristics
Forty-nine patients (male 25, female 24) with CRC undergoing radical resection were enrolled into our study. The characteristics of patients are shown in Table 1. A total of 134 lymph nodes from 49 patients were investigated. Two patients had only one lymph node available. In total, 132 lymph nodes were individually analysed in 47 patients who had two or more lymph nodes.
Table 1. Clinicopathologic characteristics.
| Characteristics | All patients (n=49), n (%) |
|---|---|
|
Sex | |
| Male | 25 (51.0) |
| Female |
24 (49.0) |
|
Age, years | |
| Median | 55.5 |
| Range |
37–78 |
|
Tumour differentiation | |
| Good | 7 (14.3) |
| Moderate | 40 (81.6) |
| Poor |
2 (4.1) |
|
AJCC tumour stage | |
| I | 7 (14.3) |
| II | 13 (26.5) |
| III | 28 (57.1) |
| IV |
1 (2.0) |
|
M stage | |
| 0 | 48 (98.0) |
| 1 |
1 (2.0) |
|
pT stage | |
| 1 | 1 (2.0) |
| 2 | 6 (12.2) |
| 3 | 28 (57.1) |
| 4 |
14 (28.6) |
|
pN stage | |
| 0 | 20 (40.8) |
| 1 | 14 (28.6) |
| 2 | 15 (30.6) |
Abbreviation: AJCC=American Joint Committee on Cancer; M stage=metastasis stage; pT stage=primary tumour stage given by pathologic examination; pN stage=lymph nodes stage given by pathologic examination.
PD-1 expression is upregulated on CD8+ T cells in TDLNs and tumours of CRC patients
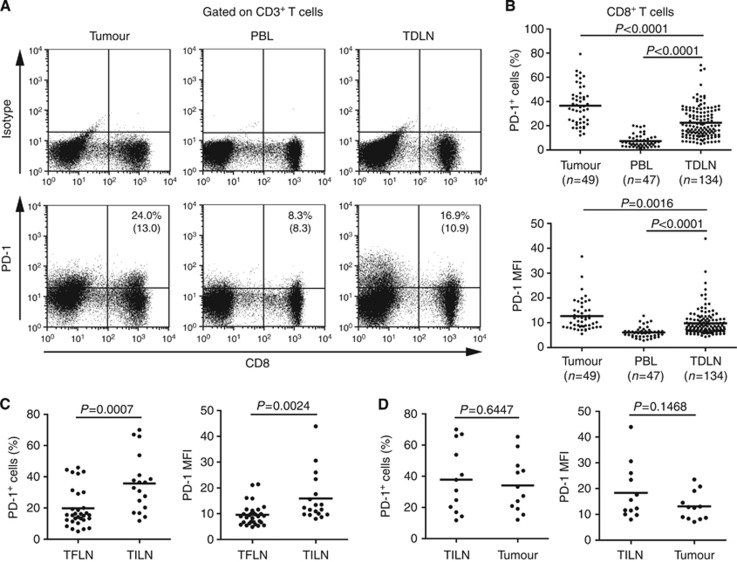
To explore the role of PD-1 signalling in regulating anti-tumour CD8+ T cell responses in CRC patients, we first assessed the expression of PD-1 on CD8+ T cells in tumour tissues, TDLNs and peripheral blood of the same patients. Single-cell suspensions of tumour digests, minced lymph node and PBLs were analysed directly by flow cytometry with anti-CD3, CD8 and PD-1 antibodies. The frequencies of PD-1+ cells among CD8 T cells were significantly higher in TDLNs (mean: 22.5%±12.9%) than those in PBLs (7.4%±5.2% P<0.0001), but remarkably lower than those in tumours (36.6%±15.7% P<0.0001). Similar observations were made when PD-1 expression was analysed as mean fluorescence intensity (MFI; Figure 1A and B).
Figure 1.
PD-1 expression on CD8+ T cells in TDLNs, tumours and peripheral blood (PBL) of CRC patients. Freshly isolated lymphocytes of TDLNs, tumour digests and PBL from the same patient were stained with CD3, CD8 and PD-1 antibody. (A) One representative patient was shown. The plots were gated on CD3+ lymphocytes. Quadrants were set based on mIgG isotype control. The percentage numbers in top right quadrant represent the fraction of PD-1+ cells in CD8+ T cells and the values in parentheses represent the mean fluorescence intensity (MFI) of PD-1+ cells in CD8+ T cells. (B) The percentage and MFI of PD-1+ cells in CD3+ CD8+ T cells in TILs, PBLs and DLNs from 49 patients with CRC are shown. (C) The overall frequency and MFI of PD-1+ cells in CD3+ CD8+ T cells in TFLN and TILN of stage III and IV CRC patients were shown. (D) Summary data showing the frequency and MFI of PD-1+ cells in CD3+ CD8+ T cells in TILN and tumour. P value was calculated using the unpaired t-test.
Tumour metastasis in draining lymph nodes was routinely examined by pathologists. The mean frequency of PD-1+ cells and the mean MFI of PD-1 expression were significantly higher for CD8+ T cells in TILNs than those in TFLNs (35.7%±18.2% vs 19.8%±12.4%, P=0.0007 and 15.9±9.4 vs 9.6±4.2, P=0.0024, respectively; Figure 1C). There was no difference in the expression of PD-1 on CD8+ T cells between TILNs and tumour tissues for both the percentage of PD-1+ cells (37.8%±21.6% vs 34.1%±17.3% P=0.6447) and the MFI of PD-1 expression (18.3±10.7 vs 13.1±5.4; P=0.1468; Figure 1D). Similar observation was also made between the lymph nodes from the same patients (data not shown). Collectively, our results demonstrated that PD-1 expression was upregulated on CD8+ T cells in TDLNs, although it was lower than that in tumour. Moreover, high-level expression of PD-1 was correlated with the presence of metastatic tumour cells.
PD-1+ CD8+ T cells are not functionally impaired in TFLNs, but dysfunctional in tumours
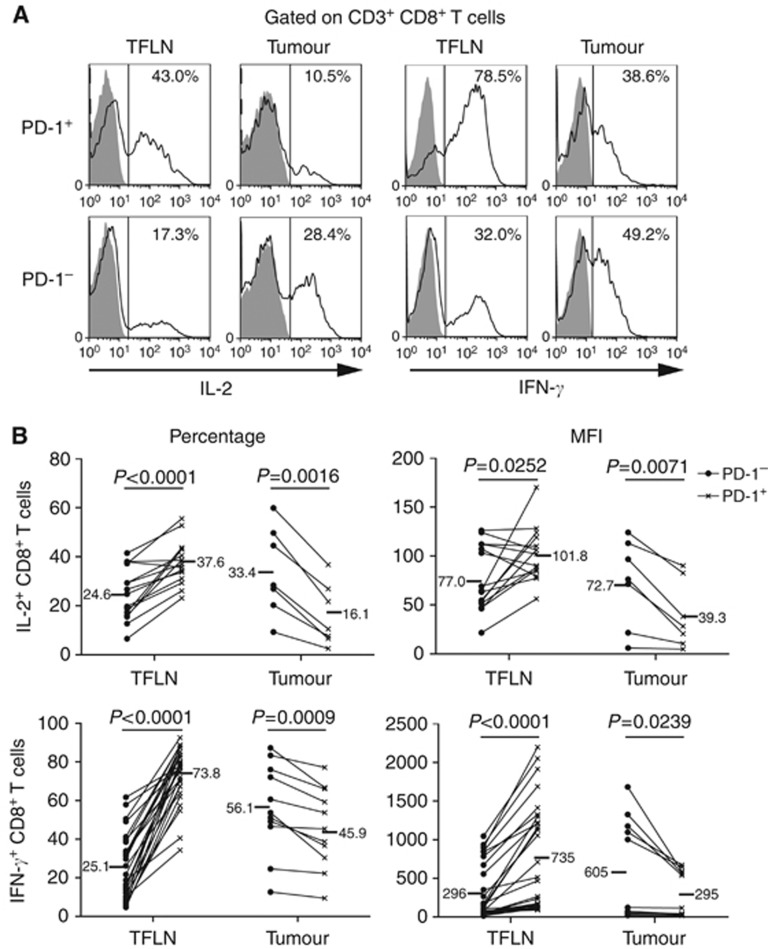
To compare the functions of PD-1+ and PD-1− CD8+ T cells, we first assessed cytokine production of CD8+ T cells in TDLNs and tumours from the same patients. Because tumour metastasis markedly decreased lymphocytes in lymph nodes (data not shown), which was not enough for studying their functions in vitro, the following functional studies were done with the lymphocytes of TFLNs. The freshly isolated lymphocytes were stimulated with PMA and ionomycin for 4 h, and intracellular cytokines were examined in gated CD3+ CD8+ T cells. As shown for one representative CRC patient in Figure 2A and for several CRC patients in Figure 2B, compared with PD-1− CD8+ TILs, PD-1+ CD8+ TILs not only exhibited markedly reduced percentages of IL-2- (16.1%±12.6% vs 33.4%±19.1%, P=0.0016; PD-1+ vs PD-1− CD8+ TIL) and IFN-γ-producing cells (45.9%±20.7% vs 56.1%±23.3, P=0.0009; PD-1+ vs PD-1− CD8+ TIL), but also expressed lower levels of IL-2 (39.3±33.9 vs 72.7±44.5, P=0.0071; PD-1+ vs PD-1− CD8+ TIL) and IFN-γ (295.2±288.9 vs 605.2±645.1, P=0.0239; PD-1+ vs PD-1− CD8+ TIL) quantified by MFI. These data are consistent with the previous findings that PD-1 upregulation is associated with the impairment of cytokine production of tumour-infiltrating CD8+ T cells upon ex vivo stimulation (Ahmadzadeh et al, 2009). In contrast, the percentage (IL-2: 37.6%±8.9% vs 24.6%±10.6%, P<0.0001; IFN-γ: 73.8%±13.9% vs 25.1%±16.7%, P<0.0001; PD-1+ vs PD-1−, respectively) and the amount (MFI; IL-2: 101.8±27.1 vs 77.0±33.4, P=0.0252; IFN-γ: 735.8±686.4 vs 296.7±346.2, P<0.0001; PD-1+ vs PD-1−, respectively) of IL-2 and IFN-γ production were increased in PD-1+ CD8+ T cells compared with PD-1− CD8+ T in TFLNs.
Figure 2.
Cytokine production in PD-1+ and PD-1− CD3+ CD8+ T cells from TFLNs and tumours. Freshly isolated lymphocytes of TFLNs and tumour digests from same patients were stimulated with PMA/ionomycin for 4 h at 37°C in the presence of BFA. Cells were collected and stained with anti-CD3, CD8 and PD-1 antibodies, and then with anti-IL-2 or IFN-γ antibodies for intracellular staining. (A) Representative data from one patient showing expression of IL-2 and IFN-γ by PD-1+ and PD-1− CD3+ CD8+ T cell subsets. Open histograms indicate the staining of IFN-γ; filled histograms is the staining of isotype controls. (B) Matched PD-1+ (labelled as × ) and PD-1− (labelled as ●) CD8+ T cells from TFLNs (n=15) and tumours (n=7) were compared for the percentage and MFI of IL-2 (upper row) and IFN-γ (low row) expression. P values were calculated based on the paired t-test between PD-1+ and PD-1− subsets in TFLNs or tumours.
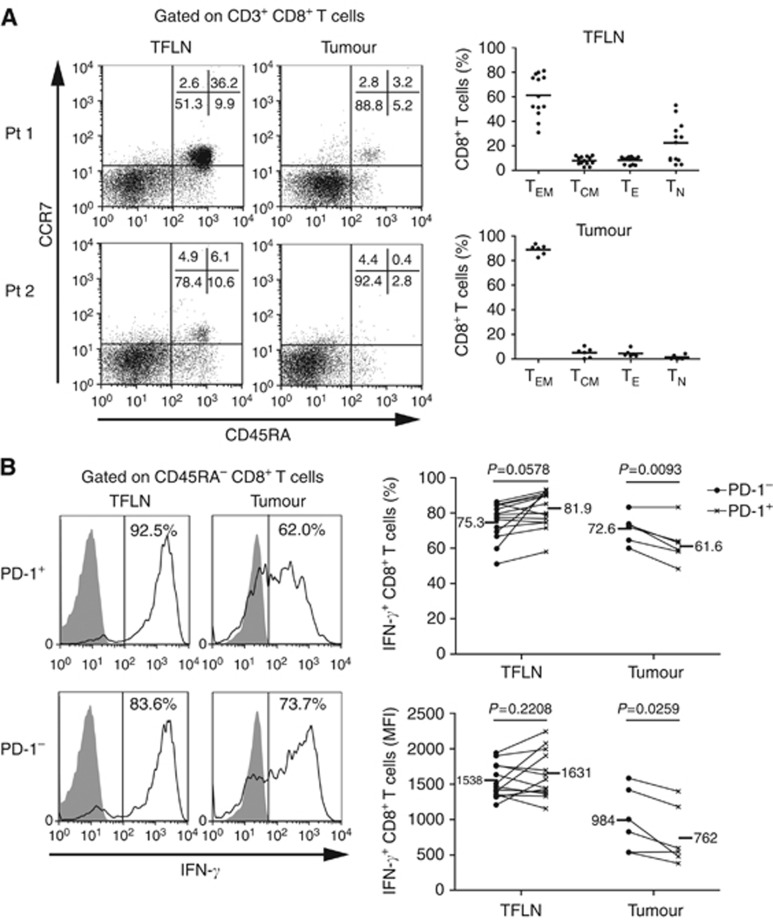
T-cell functions are associated with their differentiation/activation status, which could be identified by staining with CD45RA and CCR7. In tumour tissues, the majority of CD8+ T cells (88.9%±4.1%) fell into the subset of TEM (CD45RA− CCR7−), while naïve CD8+ T cells with CD45RA+ CCR7+ phenotype were rarely detected. However, some lymph nodes had much more naïve CD8+ T cells (22.5%±16.6%) besides the majority population of TEM cells (61.2%±17.2% Figure 3A). The frequencies of naïve cells were widely varied among individual lymph nodes with a range of 4.6% to 53.1%. Due to low frequency of CD8+ T effector cells (CD45RA+ CCR7−) in both tumours and lymph nodes, we excluded naïve cells by gating on CD45RA− CD8+ T cell populations comprised of the central memory cells (CD45RA− CCR7+) and TEM. Excluding CD45RA+ cell population markedly increased the percentage of IFN-γ-producing cells in PD-1− CD8+ T cell population in TFLNs (from 25.1%±16.7% in PD-1− CD8+ cells to 75.3%±10.5% in PD-1− CD45RA− CD8+ cells; Figures 2B and 3B). There was no significant difference of IFN-γ production in both percentage and MFI of IFN-γ-producing cells between PD-1+ and PD-1− CD45RA− CD8+ T cells in most TFLNs (Figure 3B). However, the low frequency of CD45RA+ CD8+ T cells had little influence on the percentage of IFN-γ-producing cells in tumour-infiltrating CD8+ T cells. PD-1+ cells still produced less IFN-γ in both percentage and MFI of IFN-γ-producing cells than PD-1− cells (percentage: 61.6%±11.5% vs 72.6%±8.1%, P=0.0093; MFI: 762±419 vs 984±441.1, P=0.0259) in the CD45RA− CD8+ T cell population of TILs (Figure 3B). These results indicated that the expression of PD-1 was inversely correlated with the ability of CD8+ T cells to produce IFN-γ in tumour, but had no significant effect on the cytokine production of CD8+ T cells in TFLNs.
Figure 3.
Comparison of IFN-γ production between PD-1+ and PD-1− CD45RA− CD8+ T cells in tumours and TFLNs. (A) Freshly isolated lymphocytes of TFLNs and tumour digests from the same patient were stained with anti-CD3, CD8 and CCR7, and CD45RA antibodies. The representative data of two CRC patients (left) and statistical results of six patients (right) showing percentage of different status of T cells indicated by CCR7 and CD45RA expression in TFLNs and tumours. (B) The freshly isolated lymphocytes were stimulated with PMA/ionomycin in the presence of BFA. IFN-γ production was examined by intracellular staining. Representative data from one patient showing percentage of IFN-γ-producing cells in PD-1+ (labelled as × ) and PD-1− (labelled as ●) CD45RA− CD8+ T cell subsets (left). Matched PD-1+ and PD-1− CD45RA− CD8+ T cells from TFLNs (n=13) and tumours (n=6) were compared for the percentage and MFI of IFN-γ expression (right). P values were calculated based on the paired t-test between PD-1+ and PD-1− subsets in TFLNs or tumours.
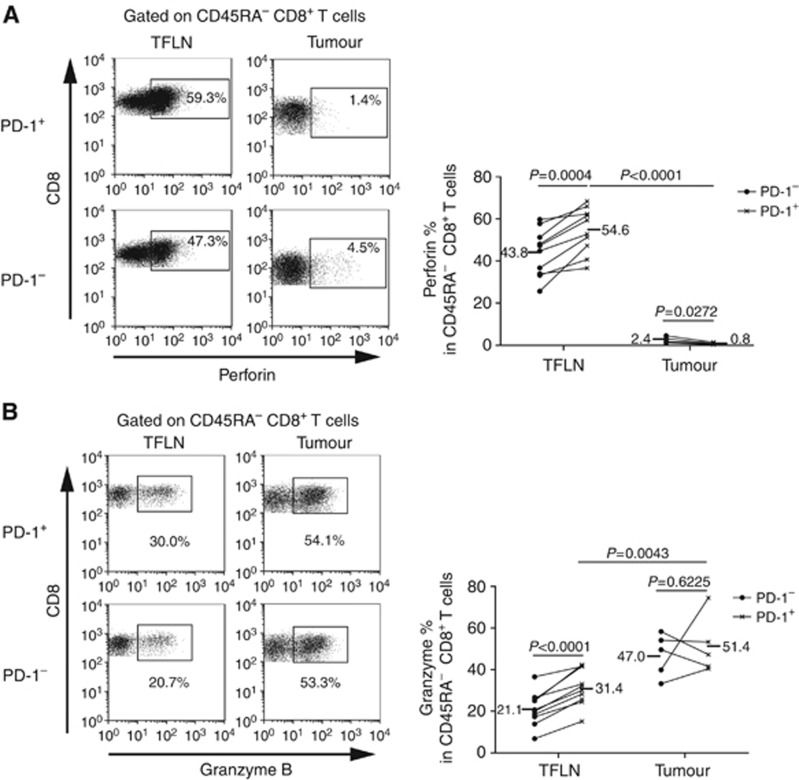
Next, we assessed the cytotoxicity of CD8+ T cells in TFLNs and tumours from the same patient by detecting the expression of granzyme B and perforin. PD-1+ CD45RA− CD8+ T cells expressed a higher level of perforin (range: 36.6–68.3%, mean: 54.6%) than PD-1− CD45RA− CD8+ T cells (range: 25.6–59.7%, mean: 43.8%) in TFLNs (Figure 4A; P=0.0004). Although a higher level of perforin was also measured in PD-1− (range: 1.2–4.5%, mean: 2.4%) than PD-1+ CD45RA− CD8+ TILs (range: 0.4–1.4%, mean: 0.8%, P=0.0272), antigen-experienced CD45RA− CD8+ T cells expressed extremely low level of perforin in tumours (Figure 4A). On the contrary, tumour-infiltrating CD45RA− CD8+ T cells expressed a higher level of granzyme B than that in TFLNs, and no significant difference in granzyme B expression was observed between PD-1+ and PD-1− CD8+ TILs (Figure 4B). While in draining lymph nodes, PD-1+ CD8 T cells still express a higher level of granzyme B (range: 15.2–42.3%, mean: 31.4%) than PD-1− CD45RA− CD8+ T cells (range: 6.8–36.6%, mean: 21.1%, P<0.0001; Figure 4B). These results demonstrated that CD8+ TILs in CRC had a serious defection in perforin expression, although they stored the highest amount of granzyme B, and upregulation of PD-1 even more impaired perforin production, which will lead to a defect of cytotoxicity. However, PD-1+ CD8+ T cells were competent for expression of granzyme B and perforin in TFLNs.
Figure 4.
Expression of perforin and granzyme B in PD-1+ and PD-1− CD45RA− CD8+ T cells from TFLNs and tumours. Freshly isolated lymphocytes of TFLNs and tumour digests from the same patients were stained with CD3, CD8 and PD-1, and then with anti-perforin or ganzyme B antibodies for intracellular staining. (A) A representative data showing percentage of perforin expression by PD-1+ (labelled as × ) and PD-1− (labelled as ●) CD8+ T cell subsets in TFLN and tumours (left). Matched PD-1+ and PD-1− CD8+ T cells from TFLNs (n=10) and tumours (n=5) were compared for the percentage of perforin expression. (B) A representative data showing percentage of granzyme B expression by PD-1+ (labelled as × ) and PD-1− (labelled as ●) CD8+ T cell subsets in TFLNs and tumours (left). Matched PD-1+ and PD-1− CD8+ T cells from DLNs (n=10) and tumours (n=5) were compared for the percentage of granzyme B expression. P values were calculated based on the paired t-test between PD-1+ and PD-1− subsets in TFLNs or tumours, but unpaired t-tests were used between PD-1+ subsets in TFLNs and tumours.
PD-L1 expression is related with functional impairment of CD8+ T cells in tumours rather than TFLNs
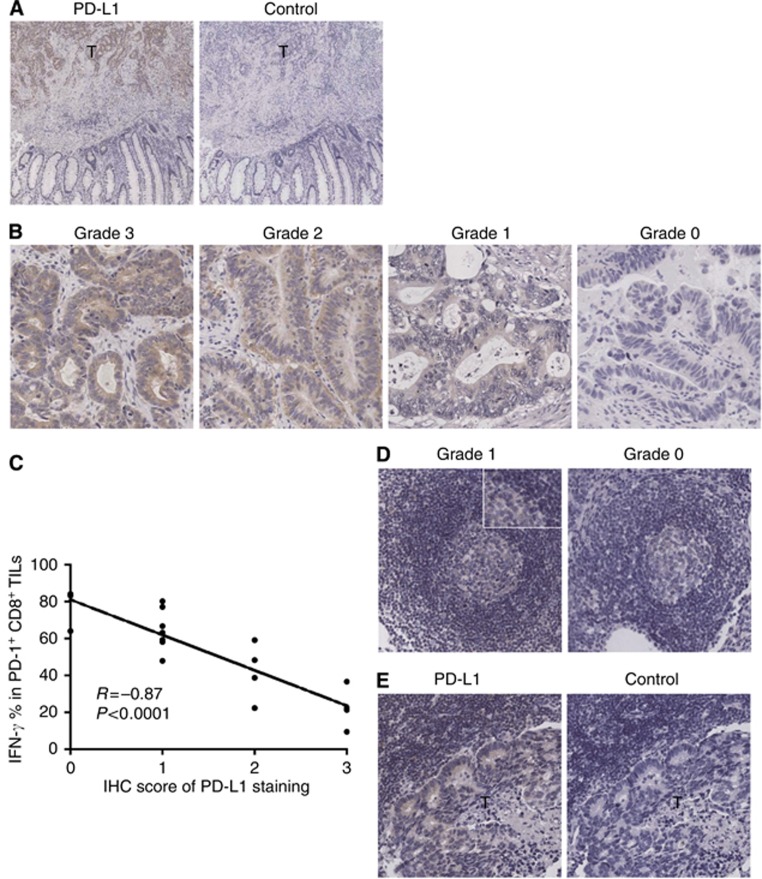
To evaluate the relation of PD-L1 expression to the functions of PD-1+ CD8+ T cell in TFLNs and tumours, we examined PD-L1 expression by immunohistochemistry. PD-L1 was clearly expressed in tumours, not in adjacent tissues (Figure 5A). The expression of PD-L1 was greatly varied in tumour tissues from different patients, which was scored as 0, 1, 2 and 3 grades in 4 (22.2%), 4 (22.2%), 7 (38.9%) and 3 (16.7%) cases, respectively (Figure 5B). More importantly, the expression level of PD-L1 was closely correlated with the impairment of cytokine production of PD-1+ CD8+ T cells in tumour (R=−0.87, P<0.0001; Figure 5C).
Figure 5.
Immunohistochemical staining of TDLNs and tumour tissues for PD-L1 expression. (A) Tumour tissues were stained with a PD-L1-specific antibody (left) or mouse IgG2b isotype control (right). (B) Representative patterns of PD-L1 expression with grade 3, grade 2, grade 1 and grade 0 are shown. (C) Plot of the scores of PD-L1 expression vs the percentages of IFN-γ-expressing cells in PD-1+ CD8+ T cells in tumour tissues. (D) Representative staining of PD-L1 expression in TFLNs is shown. (E) TILNs were stained with a PD-L1-specific antibody (left) or isotype control (right). T indicates tumour region. Original magnification × 50 (A), × 200 (B, D and E) and × 400 (inset in panel D). P value was determined by Spearman's rank correlation test.
TFLNs had no or very low-level expression of PD-L1. Moreover, PD-L1 expression in TFLNs was observed in the germinal follicles, not in T-cell-dependent paracortical areas (Figure 5D), suggesting that PD-1+ CD8+ T cells has no PD-L1 binding in TFLNs. But, PD-L1 was moderately expressed in tumour nests of TILNs, which was consistent with the higher expression of PD-1 on CD8+ T cells in TILNs (Figure 5E). These results suggested that the functions of PD-1+ CD8+ T cells should be impaired in TILNs.
Discussion
In the present study, we have systemically examined the expression of the inhibitory receptor PD-1 on CD8+ T cells in tumour, TDLNs and peripheral blood, and found that PD-1 is markedly expressed on CD8+ T cells in both tumour and TFLNs compared with that in peripheral blood, although the expression of PD-1 on CD8+ T cells in TFLNs is lower than that in tumours. The functional studies of CD8+ T cells show that PD-1+ CD8+ T cells have intact functions for expression of cytokine and perforin in TFLNs, but are dysfunctional in tumours. The functional difference of CD8+ T cells in TFLNs and tumours is related with the expression of PD-L1, one of the ligands of PD-1.
PD-1 has been found to be expressed on a large proportion of TILs from many different tumour types (Thompson et al, 2007; Ahmadzadeh et al, 2009; Lyford-Pike et al, 2013). Increased PD-1 expression on CD8+ TILs may either reflect an anergic or exhausted state, as has been suggested by decreased cytokine production by PD-1+ compared with PD-1− TILs (Ahmadzadeh et al, 2009). However, the expression pattern of PD-1 and its relation with T-cell functions in TDLNs have rarely been studied. Here, we examined PD-1 expression on CD8+ T cells in TDLNs and contrasted its functional profile with CD8+ T cells in tumours. We found that even in TFLNs, PD-1 expression is markedly upregulated on CD8+ T cells compared with that in peripheral blood, although CD8+ T cells of TFLNs express lower level of PD-1 than CD8+ TILs. However, in contrast with the dysfunction of PD-1+ CD8+ TILs, PD-1+ CD8+ T cells in TFLNs are functionally intact. They even express higher granzyme B and perforin than antigen-experienced PD-1− CD8+ T cells of TFLNs, suggesting a stronger anti-tumour cytotoxicity. PD-1 has been considered as a primary marker for exhausted T cells. However, PD-1 expression on T cells is not always associated with exhausted phenotype (Fourcade et al, 2009). Our data show that PD-1+ CD8+ T cells are bona fide effector T cells in TFLNs, while their functions are impaired in tumours. The remarkable disparity of PD-1+ CD8+ T-cell function between TFLNs and tumours cannot be explained by the expression level of PD-1 on CD8+ T cells, because PD-1+ CD8+ T cells express more granzyme B and perforin than antigen-experienced PD-1− CD8+ T cells in TFLNs. But they are closely related with the expression of PD-L1 in TFLNs and tumours. Moreover, the level of PD-L1 in tumours is negatively correlated with IFN-γ production of PD-1+ CD8+ TILs. These results demonstrate that PD-1 upregulation, which is induced by T-cell priming or reactivation in TDLNs, alone has no direct effect on the functionality of activated CD8+ T cells. Without ligand binding in the TDLN, PD-1 may just be an activation marker of T cells. Once activated PD-1+ CD8+ T cells migrate into tumour, the binding of PD-1 with PD-L1 inhibit cytokine production and the cytolytic activity of CD8+ T cells, leading to exhaustion or dysfunction of T cells.
Human CRCs with a high density of infiltrating memory and effector memory (CD45RO+) T cells were less likely to disseminate to lymphovascular and perineural structures and to regional lymph nodes (Pages et al, 2005). The frequency of CD45RO+ T cells in TILNs of CRC was also associated with improved prognosis (Oberg et al, 2002). We previously showed that CD45RO+ CD8+ T cells were major IFN-γ-producing cells compared with CD45RO− CD8+ T cells in TDLNs (Deng et al, 2010). In the present study, we further identify the differentiation/activation statue of CD8+ T cells in tumour and TDLNs of CRC by flow cytometry and to show that the majority of antigen-experienced CD8+ T cells in both locations are effector memory phenotype (CD45RA− CCR7−) and highly express PD-1. However, their functions are completely opposite. These results suggest that TFLNs may be a major provider for competent anti-tumour CD8+ T cells. Although they are severely inhibited by various suppressive signalling, such as PD-1-PD-L1 pathway, once infiltrating into tumours, they still play important roles in tumour progression.
PD-L1 is expressed at high levels in several different cancers, and high expression of PD-L1 on tumours is usually strongly associated with poor prognosis. But the clinical significance of PD-L1 expression in CRC is still not clear. Droeser et al (2013) recently analysed the expression of PD-L1 in CRC by using a tissue microarray and found that PD-L1 expression is paradoxically associated with improved survival in DNA mismatch repair-proficient rather than -deficient CRC. They also found that strong PD-L1 expression in CRC appeared to be correlated with high numbers of CD8+ TILs, which did not express the PD-1 and did not measure the functions of CD8+ TILs. The mechanism underlying the favourable effect of PD-L1 overexpression in CRC was not clear. Our study showed that PD-L1 expression in CRC was inversely associated with the ability of PD-1+ CD8+ TILs to produce IFN-γ, and PD-1 was markedly upregulated on CD8+ TILs, which was also associated with the impairment of cytokine and perforin production of CD8+ TILs. However, it should be noted that the functional difference between PD-1+ and PD-1− CD8+ TILs is not very big, and the expression of perforin in PD-1− CD8+ TILs is already extremely low in CRC. In addition, no objective responses have been observed in CRC patients in the phase I clinical trial with anti-PD-1 or PD-L1 antibody (Brahmer et al, 2012; Topalian et al, 2012). These results suggest that other molecules and inhibitory pathways are likely involved in T-cell exhaustion of CRC. It has been recently reported that the inhibitory receptors LAG-3, Tim-3 and BTLA were co-expressed with PD-1 on CD8+ TILs or tumour-specific CD8+ T cells, which impair the functions of tumour-specific T cells (Matsuzaki et al, 2010; Sakuishi et al, 2010; Fourcade et al, 2012). Thus, it will be intriguing to identify the dominant inhibitory receptor for T-cell dysfunction in CRC.
In summary, we report that PD-1 expression is upregulated on CD8+ T cells in both TDLNs and tumours. PD-1+ CD8+ T cells are competent for production of cytokines and perforin in TFLNs in which PD-L1 is not expressed, but exhibits less effector functions than PD-1− CD8+ T cells in tumours in which PD-L1 is highly expressed. These results support a role of PD-1 pathway to suppress T-cell effector functions in tumours, not in TFLNs.
Acknowledgments
This work was supported by grants from National Basic Research Program of China (973 program; 2012CB917101), National Natural Science Foundation of China (81272769, 81000920) and the capital health research and development of special (2011-4002-04).
The authors declare no conflict of interest.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
References
- Ahmadzadeh M, Johnson LA, Heemskerk B, Wunderlich JR, Dudley ME, White DE, Rosenberg SA. Tumor antigen-specific CD8 T cells infiltrating the tumor express high levels of PD-1 and are functionally impaired. Blood. 2009;114 (8:1537–1544. doi: 10.1182/blood-2008-12-195792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arai Y, Saito H, Ikeguchi M. Upregulation of TIM-3 and PD-1 on CD4+ and CD8+ T cells associated with dysfunction of cell-mediated immunity after colorectal cancer Operation. Yonago Acta Med. 2012;55 (1:1–9. [PMC free article] [PubMed] [Google Scholar]
- Barber DL, Wherry EJ, Masopust D, Zhu B, Allison JP, Sharpe AH, Freeman GJ, Ahmed R. Restoring function in exhausted CD8 T cells during chronic viral infection. Nature. 2006;439 (7077:682–687. doi: 10.1038/nature04444. [DOI] [PubMed] [Google Scholar]
- Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, Pitot HC, Hamid O, Bhatia S, Martins R, Eaton K, Chen S, Salay TM, Alaparthy S, Grosso JF, Korman AJ, Parker SM, Agrawal S, Goldberg SM, Pardoll DM, Gupta A, Wigginton JM. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366 (26:2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L. Co-inhibitory molecules of the B7-CD28 family in the control of T-cell immunity. Nat Rev Immunol. 2004;4 (5:336–347. doi: 10.1038/nri1349. [DOI] [PubMed] [Google Scholar]
- Day CL, Kaufmann DE, Kiepiela P, Brown JA, Moodley ES, Reddy S, Mackey EW, Miller JD, Leslie AJ, DePierres C, Mncube Z, Duraiswamy J, Zhu B, Eichbaum Q, Altfeld M, Wherry EJ, Coovadia HM, Goulder PJ, Klenerman P, Ahmed R, Freeman GJ, Walker BD. PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature. 2006;443 (7109:350–354. doi: 10.1038/nature05115. [DOI] [PubMed] [Google Scholar]
- Deng L, Zhang H, Luan Y, Zhang J, Xing Q, Dong S, Wu X, Liu M, Wang S. Accumulation of foxp3+ T regulatory cells in draining lymph nodes correlates with disease progression and immune suppression in colorectal cancer patients. Clin Cancer Res. 2010;16 (16:4105–4112. doi: 10.1158/1078-0432.CCR-10-1073. [DOI] [PubMed] [Google Scholar]
- Droeser RA, Hirt C, Viehl CT, Frey DM, Nebiker C, Huber X, Zlobec I, Eppenberger-Castori S, Tzankov A, Rosso R, Zuber M, Muraro MG, Amicarella F, Cremonesi E, Heberer M, Iezzi G, Lugli A, Terracciano L, Sconocchia G, Oertli D, Spagnoli GC, Tornillo L. Clinical impact of programmed cell death ligand 1 expression in colorectal cancer. Eur J Cancer. 2013;49 (9:2233–2242. doi: 10.1016/j.ejca.2013.02.015. [DOI] [PubMed] [Google Scholar]
- Fourcade J, Kudela P, Sun Z, Shen H, Land SR, Lenzner D, Guillaume P, Luescher IF, Sander C, Ferrone S, Kirkwood JM, Zarour HM. PD-1 is a regulator of NY-ESO-1-specific CD8+ T cell expansion in melanoma patients. J Immunol. 2009;182 (9:5240–5249. doi: 10.4049/jimmunol.0803245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fourcade J, Sun Z, Pagliano O, Guillaume P, Luescher IF, Sander C, Kirkwood JM, Olive D, Kuchroo V, Zarour HM. CD8(+) T cells specific for tumor antigens can be rendered dysfunctional by the tumor microenvironment through upregulation of the inhibitory receptors BTLA and PD-1. Cancer Res. 2012;72 (4:887–896. doi: 10.1158/0008-5472.CAN-11-2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pages C, Tosolini M, Camus M, Berger A, Wind P, Zinzindohoue F, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Pages F. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313 (5795:1960–1964. doi: 10.1126/science.1129139. [DOI] [PubMed] [Google Scholar]
- Golden-Mason L, Palmer B, Klarquist J, Mengshol JA, Castelblanco N, Rosen HR. Upregulation of PD-1 expression on circulating and intrahepatic hepatitis C virus-specific CD8+ T cells associated with reversible immune dysfunction. J Virol. 2007;81 (17:9249–9258. doi: 10.1128/JVI.00409-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamanishi J, Mandai M, Iwasaki M, Okazaki T, Tanaka Y, Yamaguchi K, Higuchi T, Yagi H, Takakura K, Minato N, Honjo T, Fujii S. Programmed cell death 1 ligand 1 and tumor-infiltrating CD8+ T lymphocytes are prognostic factors of human ovarian cancer. Proc Natl Acad Sci USA. 2007;104 (9:3360–3365. doi: 10.1073/pnas.0611533104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol. 2008;26:677–704. doi: 10.1146/annurev.immunol.26.021607.090331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim R, Emi M, Tanabe K, Arihiro K. Immunobiology of the sentinel lymph node and its potential role for antitumour immunity. Lancet Oncol. 2006;7 (12:1006–1016. doi: 10.1016/S1470-2045(06)70975-5. [DOI] [PubMed] [Google Scholar]
- Lyford-Pike S, Peng S, Young GD, Taube JM, Westra WH, Akpeng B, Bruno TC, Richmon JD, Wang H, Bishop JA, Chen L, Drake CG, Topalian SL, Pardoll DM, Pai SI. Evidence for a role of the PD-1:PD-L1 pathway in immune resistance of HPV-associated head and neck squamous cell carcinoma. Cancer Res. 2013;73 (6:1733–1741. doi: 10.1158/0008-5472.CAN-12-2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuzaki J, Gnjatic S, Mhawech-Fauceglia P, Beck A, Miller A, Tsuji T, Eppolito C, Qian F, Lele S, Shrikant P, Old LJ, Odunsi K. Tumor-infiltrating NY-ESO-1-specific CD8+ T cells are negatively regulated by LAG-3 and PD-1 in human ovarian cancer. Proc Natl Acad Sci USA. 2010;107 (17:7875–7880. doi: 10.1073/pnas.1003345107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naito Y, Saito K, Shiiba K, Ohuchi A, Saigenji K, Nagura H, Ohtani H. CD8+ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Res. 1998;58 (16:3491–3494. [PubMed] [Google Scholar]
- Nakamoto N, Kaplan DE, Coleclough J, Li Y, Valiga ME, Kaminski M, Shaked A, Olthoff K, Gostick E, Price DA, Freeman GJ, Wherry EJ, Chang KM.2008Functional restoration of HCV-specific CD8 T cells by PD-1 blockade is defined by PD-1 expression and compartmentalization Gastroenterology 134(71927–1937.1937. e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberg A, Samii S, Stenling R, Lindmark G. Different occurrence of CD8+, CD45R0+, and CD68+ immune cells in regional lymph node metastases from colorectal cancer as potential prognostic predictors. Int J Colorectal Dis. 2002;17 (1:25–29. doi: 10.1007/s003840100337. [DOI] [PubMed] [Google Scholar]
- Ohigashi Y, Sho M, Yamada Y, Tsurui Y, Hamada K, Ikeda N, Mizuno T, Yoriki R, Kashizuka H, Yane K, Tsushima F, Otsuki N, Yagita H, Azuma M, Nakajima Y. Clinical significance of programmed death-1 ligand-1 and programmed death-1 ligand-2 expression in human esophageal cancer. Clin Cancer Res. 2005;11 (8:2947–2953. doi: 10.1158/1078-0432.CCR-04-1469. [DOI] [PubMed] [Google Scholar]
- Pages F, Berger A, Camus M, Sanchez-Cabo F, Costes A, Molidor R, Mlecnik B, Kirilovsky A, Nilsson M, Damotte D, Meatchi T, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Galon J. Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med. 2005;353 (25:2654–2666. doi: 10.1056/NEJMoa051424. [DOI] [PubMed] [Google Scholar]
- Ropponen KM, Eskelinen MJ, Lipponen PK, Alhava E, Kosma VM. Prognostic value of tumour-infiltrating lymphocytes (TILs) in colorectal cancer. J Pathol. 1997;182 (3:318–324. doi: 10.1002/(SICI)1096-9896(199707)182:3<318::AID-PATH862>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- Sakuishi K, Apetoh L, Sullivan JM, Blazar BR, Kuchroo VK, Anderson AC. Targeting Tim-3 and PD-1 pathways to reverse T cell exhaustion and restore anti-tumor immunity. J Exp Med. 2010;207 (10:2187–2194. doi: 10.1084/jem.20100643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RH, Dong H, Lohse CM, Leibovich BC, Blute ML, Cheville JC, Kwon ED. PD-1 is expressed by tumor-infiltrating immune cells and is associated with poor outcome for patients with renal cell carcinoma. Clin Cancer Res. 2007;13 (6:1757–1761. doi: 10.1158/1078-0432.CCR-06-2599. [DOI] [PubMed] [Google Scholar]
- Thompson RH, Gillett MD, Cheville JC, Lohse CM, Dong H, Webster WS, Krejci KG, Lobo JR, Sengupta S, Chen L, Zincke H, Blute ML, Strome SE, Leibovich BC, Kwon ED. Costimulatory B7-H1 in renal cell carcinoma patients: indicator of tumor aggressiveness and potential therapeutic target. Proc Natl Acad Sci USA. 2004;101 (49:17174–17179. doi: 10.1073/pnas.0406351101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, Leming PD, Spigel DR, Antonia SJ, Horn L, Drake CG, Pardoll DM, Chen L, Sharfman WH, Anders RA, Taube JM, McMiller TL, Xu H, Korman AJ, Jure-Kunkel M, Agrawal S, McDonald D, Kollia GD, Gupta A, Wigginton JM, Sznol M. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366 (26:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trautmann L, Janbazian L, Chomont N, Said EA, Gimmig S, Bessette B, Boulassel MR, Delwart E, Sepulveda H, Balderas RS, Routy JP, Haddad EK, Sekaly RP. Upregulation of PD-1 expression on HIV-specific CD8+ T cells leads to reversible immune dysfunction. Nat Med. 2006;12 (10:1198–1202. doi: 10.1038/nm1482. [DOI] [PubMed] [Google Scholar]
- Urbani S, Amadei B, Tola D, Massari M, Schivazappa S, Missale G, Ferrari C. PD-1 expression in acute hepatitis C virus (HCV) infection is associated with HCV-specific CD8 exhaustion. J Virol. 2006;80 (22:11398–11403. doi: 10.1128/JVI.01177-06. [DOI] [PMC free article] [PubMed] [Google Scholar]