Abstract
Aim: Compliance with infection control practices is the key to quality care and excellence in dentistry. Infection control remains one of the most cost-beneficial interventions available. However, implementing control procedures requires full compliance of the whole dental team. The aim of our study was to measure the compliance in daily clinical practice.
Methods: The compliance with infection control practices in dentistry by dental health care personnel (DHCP) in a German university dental clinic was observed during clinical work. In addition, a survey was conducted to assess the individual knowledge about infection control procedures. Contamination of the workplace during invasive dental procedures was tested, as well.
Results: A total of 58 invasive dental treatments implying close contacts between HCWs and patients were scrutinized. All HCWs (100%) wore gloves during dental work, but in some cases (female dentists: 14.3%; dental assistants: 28.6%) gloves were neither changed nor hands were disinfected between different activities or patient contacts (female dentists: 68.6%; male dentists: 60.9%; dental assistants: 93%). Only 31.4% of female and 39.1% of male dentists carried out adequate hygienic hand disinfection after removing gloves. Male dentists wore significantly more often (100%) protective eyewear compared to 77.1% of female dentists (p<0.05). In addition, most of female dentists (62.9%) and dental assistants (80.7%) wore jewelry during dental procedures.
Conclusion: Despite the knowledge of distinct hygiene procedures only a small percentage of dental staff performs hygiene practices according to recommended guidelines. Strict audit is clearly needed in the dental setting to ensure compliance with infection control guidelines to prevent transmission of pathogens. Our results provide insights for the development of a targeted education and training strategy to enhance compliance of dental staff especially of dental assistants with infection control procedures.
Keywords: infection control, guidelines, environmental contamination, compliance
Zusammenfassung
Ziel: Die Einhaltung von Hygienerichtlinien ist der Schlüssel zur Gewährleistung einer hohen Qualität und exzellenten Patientenversorgung in der Zahnheilkunde. Infektionskontrolle bleibt eine der kosteneffektivsten Interventionen die zur Verfügung stehen. Allerdings erfordert die erfolgreiche Implementierung von Hygienerichtlinien die vollständige Compliance des gesamten Praxisteams. Das Ziel unserer Studie war es, diese Compliance im täglichen klinischen Alltag zu messen.
Methoden: Die Compliance mit Hygienerichtlinien in der Zahnmedizin durch das zahnmedizinische Personal (ZP) in einer deutschen Universitätszahnklinik wurde während der klinischen Arbeit beobachtet. Zusätzlich wurde eine Umfrage durchgeführt, um das individuelle Wissen über Maßnahmen zur Infektionskontrolle zu erfassen. Des Weiteren wurde die mikrobiologische Umgebungskontamination des Arbeitsplatzes während der Durchführung von invasiven zahnärztlichen Eingriffen getestet.
Ergebnisse: Insgesamt wurden 58 invasive zahnärztliche Behandlungen, welche engen Kontakt zwischen ZP und Patienten erfordern, ausgewertet. Alle des ZP (100%) trugen Handschuhe während der zahnärztlichen Arbeit, aber in einigen Fällen (Zahnärztinnen: 14,3%; Zahnarzthelferinnen: 28,6%) wurden die Handschuhe weder gewechselt, noch die Hände zwischen den verschiedenen Tätigkeiten oder Patientenkontakten desinfiziert (Zahnärztinnen: 68,6%; Zahnärzte: 60,9%; Zahnarzthelferinnen: 93%). Nur 31,4% der weiblichen und 39,1% der männlichen Zahnärzte führten eine korrekte hygienische Händedesinfektion nach dem Ausziehen der Handschuhe durch. Männliche Zahnärzte trugen signifikant häufiger (100%) Schutzbrillen im Vergleich zu 77,1% der weiblichen Zahnärzte (p<0,05). Zudem trugen die meisten der weiblichen Zahnärzte (62,9%) und der Zahnarzthelferinnen (80,7%) Schmuck.
Fazit: Trotz Kenntnis von Hygienerichtlinien befolgt nur ein kleiner Prozentsatz des ZP die empfohlenen Richtlinien. Eine strenge Auditierung und fachliche Weiterbildung des ZP ist notwendig, um die Einhaltung von Hygienerichtlinien in der Zahnheilkunde zu gewährleisten und um die Übertragung von Krankheitserregern sicher zu verhindern. Unsere Ergebnisse liefern Erkenntnisse zur Entwicklung einer gezielten Fortbildungsstrategie, um die Compliance des ZP mit Hygienerichtlinien, vor allem von Zahnarzthelferinnen, zu verbessern.
Introduction
The oral cavity is a natural habitat for a large number of microorganisms. In dentistry, these microorganisms may pose a risk for cross-contamination and infection [1]. It is also important to consider that the pathways of contamination are bi-directional: Both patients and dental health care personnel (DHCP) may be exposed to a number of pathogens through exposure to blood and saliva [1]. In addition, the hands of DHCP may serve as a reservoir for pathogens [2], including multi-resistant strains [3]. Infection control forms an important part of practice for all health care professions and remains one of the most cost-beneficial medical interventions available [4], [5]. Professional dental associations and professional health agencies have advocated that universal precautions be applied to all patients, as their potential infectivity may not be known [6], [7], [8], [9].
The aim of this study was to assess the compliance with infection control recommendations of dentists and dental assistants and evaluate the risk of cross-contamination of the workplace due to aerosol formation during invasive dental procedures.
Methods
A prospective, observational study was carried out at the School of Dentistry of the University Hospital Freiburg, Germany. The study received an exemption from institutional review board, since only observational methods were applied. Dental hospital staff was observed during clinical work for their compliance with infection control procedures as recommended by the German Robert Koch Institute [9]. Compliance with infection control opportunities during ~60 dental treatments was investigated. In addition, a survey was conducted after the observation period to assess the individual knowledge of dental hospital staff about infection control procedures and official recommendations. All dentist and dental assistants working at the Department of operative Dentistry and Periodontology, Albert-Ludwigs-University, Freiburg, Germany, were eligible for participation in the study and the survey. Contamination of the workplace during 18 invasive dental procedures was tested by placing three Columbia 5% sheep blood (COS) agar plates (Heipha, Germany) in different angles each at a distance of 0.75 meters from the dental-hand pieces; the COS plates were then aerobically incubated for 48 h at 36°C. Microbiological growth was assessed in the microbiological laboratory.
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS 19.0, Chicago, USA). Descriptive statistics were used to explore data. Fisher’s exact test was used for the analysis of contingency tables. P-values of <0.05 were regarded as significant.
Results
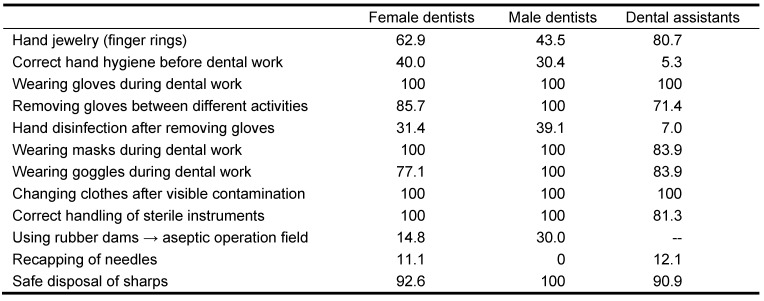
During the observational period, a total of 58 procedures were performed, 35 by female and 23 by male dentists. Results are shown in Table 1 (Tab. 1). All DHCP (100%) wore gloves during dental work, but in some cases (female dentists: 14.3%; dental assistants: 28.6%) gloves were neither changed nor hands were disinfected between aseptic activities (e.g. paperwork) or patients (female dentists: 68.6%; male dentists: 60.9%; dental assistants: 93%). Only 31.4% of female and 39.1% of male dentists carried out adequate hygienic hand disinfection after removing gloves, while dental assistants carried out adequate hand disinfection significantly less frequently (7.0%; p<0.005). Interestingly, 30% of all dental assistants stated in the survey that they would always perform correct hand disinfection after removal of gloves. All DHCP wore masks, however, 16% of all dental assistants masks were worn incorrectly covering only the mouth without the nose. All male dentists wore protective eyewear compared to 77.1% of female dentists and 62.5% of dental assistants (p<0.005). Recapping needles was observed in 11.1% of female and 0% of male dentists, and 12.1% of dental assistants. However, needle stick injuries in the last 12 months were reported in the questionnaire by 35% of all dentist and 42% of all dental assistants, respectively. Some female dentists (7.4%) and dental assistants (9.1%) did not follow safe practices when disposing sharps. Nearly half of all dentists (43%) stated in the questionnaire that they disinfect their hands correctly when entering and leaving the treatment area, while only 18% of dental assistants declared the same. Correct hand hygiene before dental work was really observed by female dentists, male dentists and dental assistants in 40%, 30.4%, and 5.3%, respectively.
Table 1. Infection control compliance (in % by category of opportunity) of dental health care workers during dental procedures (n=58).
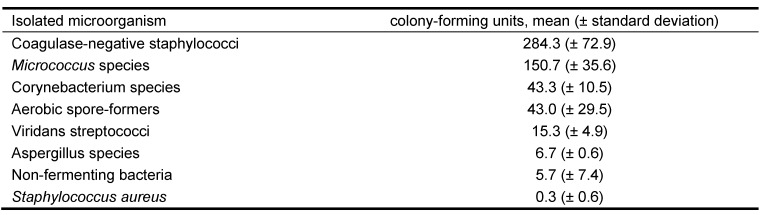
Contamination of the workplace due to evaporation and formation of aerosols by rotors and turbines of dental hand-pieces after invasive dental procedures was found in all cases (n=54). Within 0.75 meters all agar plates showed growth of oral flora, including non-fermenting bacteria, clinical relevant fungi (e.g. Aspergillus species), and oxacillin-sensitive Staphylococcus aureus (Table 2 (Tab. 2)).
Table 2. Isolated microorganisms around the workplace during invasive dental procedures (n=18).
Discussion
Dental practitioners are at high risk for infection by blood-borne pathogens, since they are continually exposed to blood and saliva mixed with blood, and may even suffer needle punctures [10], [11]. Emanation of pathogens through the spray of dental hand-pieces can also be considered an air-borne or water-born means of transmission, which may affect both the patient and the dental team [1]. Although, bacterial counts in dental rooms are not significantly higher than bacterial counts in public areas, the risk of transmission might be higher in a dental clinic compared to a public area due to the type of micro-organisms, host susceptibility and exposure time [12]. Data on transmission rates of viruses and bacteria in dental practice are scarce and real rates may even be underestimated [1]. In addition, the likelihood of health-care associated infections, particularly in dentistry, of being detected, reported, documented and published is small [13], [1]. The key to reduce or prevent the transmission of a variety of microorganisms to dental workers lays in a high compliance to infection control practices. Our study investigated dentist’s compliance with recommended infection control practices in a university hospital dental clinic in Germany. This study shows that most dental healthcare personnel are compliant with infection control practices according to their needs, however, not necessarily according to the real recommendations. Wearing of masks and gloves during dental work was observed in all cases, however, 16% of dental assistants wore mask incorrectly. Also changing of clothes after visible contamination was done in all cases, and goggles were worn in 77.1%, 100%, and 83.9% of all cases by female dentists, male dentists, and dental assistants, respectively. All of which aims at personal protection in the first place. Nevertheless, also the transmission of pathogens from the hands of dental personnel to patients is of major importance for infection control. Hand hygiene is considered the single most effective method for prevention and control of healthcare-associated infections. The hands of healthcare workers may serve as a reservoir for many pathogens [14], [2]. Thus, compliance with hand hygiene procedures is essential. In our study, however, compliance with hand hygiene procedures was very low. More than half of all dental workers failed to disinfect their hands correctly before dental work, and also after removing gloves adequate hand disinfection was carried out in 31.4% of female and 39.1% of male dentists, only (Table 1 (Tab. 1)). Dental assistants, however, showed even significantly less compliance rates (7.0%; p<0.005). Furthermore, female dental workers wore jewelry significantly more frequent than male dentists. Ring wearing, however, is associated with 10-fold higher median skin organism count, and the risk of contamination with any transient organism increases stepwise as the number of rings worn increases (odds ratio [OR] for 1 ring worn, 2.6; OR for >1 ring worn, 4.6) [15].
Transmission via aerosols, due to aerosol formation during invasive dental procedures, is a major concern in the dental setting. When working with hand-pieces bacterial aerosols including approximately 105 CFU are continuously generated [16]. Our study confirmed the contamination of the workplace with bacteria in an area of diameter of 0.75. Several infectious agents relevant to the dental setting can occur via direct or indirect airborne transmission, such as varicella-zoster virus or tuberculosis [17], [18]. However, also Hepatitis B virus (HBV) infection can, besides through percutaneous injuries, result from (in)direct blood or bloody fluid exposure through inoculation into cutaneous scratches, abrasions, burns or on mucosal surfaces [19], [1]. HBV has demonstrated the ability to survive and remain infectious in dried blood on environmental surfaces for at least 1 week and probably longer [1], [20]. Therefore, dental procedures can introduce oral pathogens into the bloodstream or lymphatic system via direct hematogenous spread or aspiration, thereby causing various medical conditions including bacteremia, pneumonia, or infective endocarditis [21], [3].
Despite the knowledge of distinct hygiene procedures only a small percentage of dental staff performs hygiene practices according to the recommended guidelines. Although compliance with other infection control practices was high, clearly improvements were desirable, as well. Considerably lower compliance with infection control procedures due to insufficient knowledge was found in dental assistants compared to dentists. Based on the results of this study a training program was initiated which was well accepted and appreciated by all DHCP, including dental assistants and dentists. Extending continuing education and strict audit is needed in the dental setting to ensure compliance with infection control guidelines and to provide enduring knowledge [22]. In addition, a high compliance with infection control procedures is the key to quality care and excellence in dentistry. Our results provide insights for the development of a targeted education and training strategy to enhance compliance of dental staff, especially of dental assistants, with infection control procedures.
Notes
Acknowledgements
Parts of the sections material and methods and results have been presented in a poster on the 52nd ICAAC in San Francisco, September, 2012.
Conflict of interest
All authors report no conflict of interest relevant to this article.
References
- 1.Laheij AM, Kistler JO, Belibasakis GN, Valimaa H, de Soet JJ European Oral Microbiology Workshop (EOMW) 2011. Healthcare-associated viral and bacterial infections in dentistry. J Oral Microbiol. 2012;4 doi: 10.3402/jom.v4i0.17659. Available from: http://dx.doi.org/10.3402/jom.v4i0.17659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cook HA, Cimiotti JP, Della-Latta P, Saiman L, Larson EL. Antimicrobial resistance patterns of colonizing flora on nurses' hands in the neonatal intensive care unit. Am J Infect Control. 2007 May;35(4):231–236. doi: 10.1016/j.ajic.2006.05.291. Available from: http://dx.doi.org/10.1016/j.ajic.2006.05.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Amorim-Finzi MB, Cury MV, Costa CR, Dos Santos AC, de Melo GB. Rate of Compliance with Hand Hygiene by Dental Healthcare Personnel (DHCP) within a Dentistry Healthcare First Aid Facility. Eur J Dent. 2010 Jul;4(3):233–237. [PMC free article] [PubMed] [Google Scholar]
- 4.Wenzel RP. The Lowbury Lecture. The economics of nosocomial infections. J Hosp Infect. 1995 Oct;31(2):79–87. doi: 10.1016/0195-6701(95)90162-0. Available from: http://dx.doi.org/10.1016/0195-6701(95)90162-0. [DOI] [PubMed] [Google Scholar]
- 5.Al-Omari MA, Al-Dwairi ZN. Compliance with infection control programs in private dental clinics in Jordan. J Dent Educ. 2005 Jun;69(6):693–698. [PubMed] [Google Scholar]
- 6.McCarthy GM, Koval JJ, John MA, MacDonald JK. Infection control practices across Canada: do dentists follow the recommendations? J Can Dent Assoc. 1999 Oct;65(9):506–511. [PubMed] [Google Scholar]
- 7.Recommended infection-control practices for dentistry, 1993. Centers for Disease Control and Prevention. MMWR Recomm Rep. 1993 May 28;42(RR-8):1–12. [PubMed] [Google Scholar]
- 8.Recommendations for infection control procedures. Canadian Dental Association. Board of Governors. J Can Dent Assoc. 1995 Jun;61(6):509. [PubMed] [Google Scholar]
- 9.Infektionsprävention in der Zahnheilkunde – Anforderungen an die Hygiene. Mitteilung der Kommission für Krankenhaushygiene und Infektionsprävention beim Robert Koch-Institut. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2006 Apr;49(4):375–394. doi: 10.1007/s00103-005-1219-y. Available from: http://dx.doi.org/10.1007/s00103-005-1219-y. [DOI] [Google Scholar]
- 10.Su J, Deng XH, Sun Z. A 10-year survey of compliance with recommended procedures for infection control by dentists in Beijing. Int Dent J. 2012 Jun;62(3):148–153. doi: 10.1111/j.1875-595X.2011.00107.x. Available from: http://dx.doi.org/10.1111/j.1875-595X.2011.00107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Razak IA, Lind OP. Cross-infection control in Malaysian dental practice. Singapore Dent J. 1995 Jul;20(1):11–15. [PubMed] [Google Scholar]
- 12.Kimmerle H, Wiedmann-Al-Ahmad M, Pelz K, Wittmer A, Hellwig E, Al-Ahmad A. Airborne microbes in different dental environments in comparison to a public area. Arch Oral Biol. 2012 Jun;57(6):689–696. doi: 10.1016/j.archoralbio.2011.11.012. Available from: http://dx.doi.org/10.1016/j.archoralbio.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 13.Perry JL, Pearson RD, Jagger J. Infected health care workers and patient safety: a double standard. Am J Infect Control. 2006 Jun;34(5):313–319. doi: 10.1016/j.ajic.2006.01.004. Available from: http://dx.doi.org/10.1016/j.ajic.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Henderson DK. Managing methicillin-resistant staphylococci: a paradigm for preventing nosocomial transmission of resistant organisms. Am J Infect Control. 2006 Jun;34(5 Suppl 1:S46-54):discussion S64–discussion S73. doi: 10.1016/j.ajic.2006.05.228. Available from: http://dx.doi.org/10.1016/j.ajic.2006.05.228. [DOI] [PubMed] [Google Scholar]
- 15.Trick WE, Vernon MO, Hayes RA, Nathan C, Rice TW, Peterson BJ, Segreti J, Welbel SF, Solomon SL, Weinstein RA. Impact of ring wearing on hand contamination and comparison of hand hygiene agents in a hospital. Clin Infect Dis. 2003 Jun 1;36(11):1383–1390. doi: 10.1086/374852. Available from: http://dx.doi.org/10.1086/374852. [DOI] [PubMed] [Google Scholar]
- 16.Micik RE, Miller RL, Mazzarella MA, Ryge G. Studies on dental aerobiology. I. Bacterial aerosols generated during dental procedures. J Dent Res. 1969 Jan-Feb;48(1):49–56. doi: 10.1177/00220345690480012401. Available from: http://dx.doi.org/10.1177/00220345690480012401. [DOI] [PubMed] [Google Scholar]
- 17.Gershon AA, Gershon MD, Breuer J, Levin MJ, Oaklander AL, Griffiths PD. Advances in the understanding of the pathogenesis and epidemiology of herpes zoster. J Clin Virol. 2010 May;48 Suppl 1:S2–S7. doi: 10.1016/S1386-6532(10)70002-0. Available from: http://dx.doi.org/10.1016/S1386-6532(10)70002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carvalho AC, Migliori GB, Cirillo DM. Tuberculosis in Europe: a problem of drug resistance or much more? Expert Rev Respir Med. 2010 Apr;4(2):189–200. doi: 10.1586/ers.10.7. Available from: http://dx.doi.org/10.1586/ers.10.7. [DOI] [PubMed] [Google Scholar]
- 19.Lauer JL, VanDrunen NA, Washburn JW, Balfour HH., Jr Transmission of hepatitis B virus in clinical laboratory areas. J Infect Dis. 1979 Oct;140(4):513–516. doi: 10.1093/infdis/140.4.513. Available from: http://dx.doi.org/10.1093/infdis/140.4.513. [DOI] [PubMed] [Google Scholar]
- 20.Bond WW, Favero MS, Petersen NJ, Gravelle CR, Ebert JW, Maynard JE. Survival of hepatitis B virus after drying and storage for one week. Lancet. 1981 Mar;1(8219):550–551. doi: 10.1016/S0140-6736(81)92877-4. Available from: http://dx.doi.org/10.1016/S0140-6736(81)92877-4. [DOI] [PubMed] [Google Scholar]
- 21.Greco PM, Lai CH. A new method of assessing aerosolized bacteria generated during orthodontic debonding procedures. Am J Orthod Dentofacial Orthop. 2008 Apr;133(4 Suppl):S79–S87. doi: 10.1016/j.ajodo.2006.08.021. Available from: http://dx.doi.org/10.1016/j.ajodo.2006.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Milward MR, Cooper PR. Competency assessment for infection control in the undergraduate dental curriculum. Eur J Dent Educ. 2007 Aug;11(3):148–154. doi: 10.1111/j.1600-0579.2007.00439.x. Available from: http://dx.doi.org/10.1111/j.1600-0579.2007.00439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]